Abstract
Background:
Theory of mind (ToM) is a social-cognitive skill that involves the ability to understand the thoughts and feelings of others. Evidence is mixed regarding the extent of ToM ability in individuals with depression.
Methods:
We conducted a meta-analysis of 43 studies to investigate the strength of the association between ToM and depression.
Results:
Results indicated significant, small- to moderate impairment in ToM with a medium overall effect size (g = −.398) in individuals with depression. Moderator analyses compared effect sizes across groups for the following variables: ToM content, process, and sample type. Additionally, meta-regression analyses tested age and gender as continuous moderators.
Limitations:
The cross-sectional nature of included studies limits this meta-analysis from clarifying temporal or bidirectional relations.
Conclusions:
We discuss findings in the context of the extant developmental, cognitive, social, and clinical literatures. We also suggest several possible explanations for these findings and offer implications for intervention.
Keywords: theory of mind, depression, meta-analysis
Theory of mind (ToM) is a social-cognitive ability that allows individuals to understand the thoughts and feelings of others (Premack & Woodruff, 1978). ToM emerges in various capacities throughout childhood (e.g., Leslie, 1987), adolescence (e.g., Shamay-Tsoory et al., 2010), and young adulthood (e.g., Bernstein et al., 2011), is relevant to cognitive processes of decoding and reasoning (e.g., Sabbagh, 2004), and is differentially associated with various clinical presentations (e.g., Brune & Brune-Cohrs, 2006). Recent work has investigated associations between ToM ability and psychiatric disorders, particularly depression, but this literature reveals varied and inconsistent findings. In individuals with depression, studies have shown ToM to be impaired (e.g., Nejati et al., 2012), comparable (e.g., Caputi & Schoenborn, 2018; Corcoran et al., 2008), and even heightened (e.g., Harkness et al., 2005), as compared to healthy controls. The current meta-analytic review had the following aims: (a) to review the literature relevant to ToM and depression and (b) to investigate ToM ability in individuals with depression using meta-analyses to allow us to calculate the strength of the association between ToM and depression.
ToM
ToM is the knowledge and awareness of mental states in oneself and others (Premack & Woodruff, 1978), and involves the ability to “put oneself in another’s shoes” (Flavell et al., 1968). The social-cognitive literature includes varied and related terms for ToM. In the current review, we use the term ToM to encompass cognitive and affective facets of perspective-taking and mentalizing, but we do not consider empathy to be equivalent to ToM (Dvash & Shamay-Tsoory, 2014; Davis, 1983; Eslinger, 1998).
In early development, studies of looking times suggest that infants as young as 15-months begin to exhibit an understanding of the beliefs of others (Onishi & Baillargeon, 2005). During the preschool years, ToM ability frequently is assessed via a false belief task, which requires children to infer that another person does not have the same knowledge that they have and to acknowledge that another person can hold a belief that is inaccurate or false (Wimmer & Perner, 1983). Typically, children between the ages of 3- and 5-years-old achieve this basic level of cognitive ability (Sullivan & Winner, 1993).
Higher-order ToM abilities continue to develop throughout childhood, adolescence, and into adulthood (Blakemore, 2008; Meinhardt‐Injac et al., 2020). Two constituent parts, which codevelop in varied and interrelated ways (e.g., Pons et al., 2004; Sebastian et al., 2011; Shamay-Tsoory et al., 2010), comprise advanced ToM: affective (i.e., understanding the feelings and emotions of others) and cognitive (i.e., mentalization or understanding the thoughts, beliefs, and intentions of others) (Brothers & Ring, 1992; Shamay-Tsoory & Aharon-Peretz, 2007). Generally, affective ToM relies more heavily on skills relevant to the decoding of others’ emotions (e.g., identifying what a person is experiencing by seeing their eyes only), whereas cognitive ToM relies more on reasoning skills (e.g., understanding how a person might perceive a complex social situation). fMRI studies have revealed that affective and cognitive ToM are associated with activating neural responses in traditional ToM networks (bilateral superior temporal sulcus/temporoparietal junction). Additionally, affective ToM activates neural responses in separate networks (medial prefrontal cortex/ventromedial prefrontal cortex), suggesting that cognitive and affective ToM may represent distinct neural processes (Sebastian et al., 2011).
Methodological variation exists in the assessment of ToM. Most measures of ToM are task-based, requiring individuals to perform instantaneous identification of mental states of others (e.g., Reading the Mind in the Eyes Test [RMET; Baron-Cohen et al., 2001a]) or to explain properly why an individual might experience a certain thought or feeling (e.g., Movie for the Assessment of Social Cognition [MASC; Dziobek et al., 2006]). Importantly, most tasks aimed at assessing affective ToM require decoding processes whereas most tasks aimed at assessing cognitive ToM require reasoning processes. Although the literature largely reflects these affective/decoding and cognitive/reasoning associations in measurement, conceptually, these constructs remain distinct and should not be conflated (e.g., Sabbagh, 2004; Sabbagh & Bowman, 2018). Other measures of ToM are self-report (e.g., Interpersonal Reactivity Index – Perspective Taking [IRI-PT; Davis, 1983]), and as such, they rely on people’s perceptions of their tendencies and abilities to understand the thoughts and feelings of others. Due to small associations between performance of ToM tasks and self-report questionnaires (e.g., Murphy & Lilienfeld, 2019), the current review focused solely on ToM tasks. (See Appendix A, however, for post hoc analyses of self-report measures of ToM.)
Prior research has recognized and documented dysfunction in ToM as a feature of several clinical disorders, particularly schizophrenia and autism spectrum disorder (ASD) (for reviews, see Bora et al., 2009; Sprong et al., 2007; Baron-Cohen, 2000; Mathersul et al., 2013). Far fewer studies have assessed ToM in individuals with depression, although research in this area has been growing over the last decade (e.g., Bora & Berk, 2015, Berecz et al., 2016, Washburn et al., 2016). The goal of the current meta-analytic review was to document the extent to which ToM is impaired, comparable, or heightened in individuals with depression.
ToM and Depression
Depression is one of the most prevalent and debilitating mental disorders in the world (Baxter et al., 2013) and the leading cause of years lived with disability worldwide (Ferrari et al., 2013). In addition to its high prevalence, depression can be episodic and recurrent (American Psychological Association [APA], 2000). Depression also accounts for significant impairment in terms of productivity, interpersonal relationships, and well-being, and is associated with suicide and substance use disorders (Clark et al., 2016; Hawton et al., 2013; Swendsen & Merikangas, 2000; Zlotnick et al., 2000; Wells et al., 1989).
A recent, seminal meta-analysis of 18 studies measuring ToM in adults with task-based measures (Bora & Berk, 2015) found that those with a clinical diagnosis of major depressive disorder (MDD) significantly underperformed (d = −.58) on measures of ToM compared to healthy controls. Additionally, more severe depression was associated with greater deficits in ToM performance. These impairments were evident for tasks measuring cognitive and affective ToM, and for tasks specifically measuring decoding (e.g., RMET; Baron-Cohen et al., 2001a) and reasoning processes of ToM (e.g., MASC; Dziobek et al., 2006). Neither age nor gender significantly moderated differences between adults with depression and healthy controls on measures of ToM. Similarly, in a narrower investigation, Richman and Unoka (2015) conducted a meta-analysis on 8 studies of RMET performance in adults with depression compared to healthy controls and found a significant, large deficit (d = −.75) in ToM for adults with depression. Again, neither age nor gender significantly moderated differences between adults with depression and healthy controls.
Not all evidence, however, indicates a general deficit in ToM for individuals with depression. In a comprehensive though qualitative review of the literature, Berecz and colleagues (2016) examined a wider range of studies, including those that compared mild and unspecified depression to healthy controls. They found that depressed individuals did not consistently underperform on ToM tasks as compared to healthy controls. In fact, several studies found no significant differences between depressed individuals and healthy controls on measures of ToM, although some trends emerged depending upon which ToM component was assessed and which measurement method was used. For example, several studies found that depression was associated with deficits in affective ToM as assessed on the RMET, a test of mental state identification from viewing only a person’s eyes, which requires skills in decoding more than reasoning, (Harkness, Washburn, Theriault, Lee, & Sabbagh, 2011; Lee, Harkness, Sabbagh, & Jacobson, 2005; Nejati et al., 2012). In contrast, Lee et al. (2005) identified ToM deficits only in individuals with severe depression, but not in those with mild/moderate depression.
These mixed results regarding ToM and depression have been found for both cognitive and affective ToM, indicating no specific content-pattern of results. For example, individuals with depression performed comparably to healthy controls on tasks of cognitive ToM relying on reasoning abilities, including those measuring the characters’ intentions, faux pas detection, and awareness of nuanced social situations (for a review, see Berecz et al., 2016). Other studies, however, found ToM impairments in individuals with depression on similar types of tasks (Ladegaard et al., 2014; Thoma et al., 2015; Uekermann et al., 2008). Thus, performance based on ToM content may not be uniformly impaired in individuals with depression. Rather, mixed findings emerge, depending on depression symptom severity and the specific complexity of the affective or cognitive demand of the ToM assessment method. Heterogeneity of ToM measures as well as the heterogeneity of depression presentations may contribute to the lack of consistent differences between individuals with depression and healthy controls.
A few studies have shown that depressive symptoms are associated with more accurate or heightened ToM. For example, Harkness and colleagues (2005) reported that individuals with dysphoria, assessed by a self-report depressive symptom count, had more accurate affective ToM than did nondysphoric individuals. In a sample of 40 women with nonclinical levels of depressive symptoms, Poletti and colleagues (2014) found that mild symptoms were associated with greater accuracy in an assessment of affective ToM. Perhaps, at certain levels of low mood affective ToM is enhanced, or some levels of depressive symptoms may be characterized by hyper social sensitivity. The theory of orientation to social information (e.g., Weary & Edwards, 1994, see Harkness et al., 2011) may be relevant here. Specifically, individuals with subthreshold depression might become increasingly oriented to the social world around them as a way to regain control in the midst of their symptoms. This increased orientation toward the social cues of others might improve the emotion detection skills inherent to affective ToM. No study, however, has reported similar results regarding the reasoning aspects of cognitive ToM.
Another instance of heightened affective ToM was found in adolescent males with MDD who exhibited more accurate affective-state decoding compared to healthy male controls (Mellick & Sharp, 2016). Thus, subgroups of individuals for whom depressive symptoms are associated with more adaptive ToM might exist. In fact, increased fear of social disapproval, often associated with depressive disorders (Gilbert & Miles, 2000), might motivate greater attunement to the thoughts and feelings of others, thereby leading to enhanced ToM in individuals with depression. Relatively few studies, however, have examined the link between ToM and depression as a function of demographic characteristics such as gender and age, particularly in children and adolescents; this highlights a gap in the literature regarding the connection between depression and ToM.
The review by Berecz and colleagues (2016) examined studies of individuals with less severe levels of depression, but only included investigations of individuals with diagnoses of a depressive disorder rather than studies using dimensional measures of depression. Additionally, both the recent review (Berecz et al., 2016) and meta-analyses (Bora & Berk, 2015; Richman & Unoka, 2015) predominantly focused on adult samples, rarely examining ToM in depressed children and adolescents. As such, these reviews might have overlooked an important age-related lens of depression and ToM. For example, studies of children might be underrepresented in meta-analyses because children may be more likely than adults to report subclinical levels of depression but not meet full diagnostic criteria for MDD (Dekker et al., 2007).
Reviews of the relations between depressive symptoms and ToM ability should include studies of children and adolescents for several reasons. First, a significant percentage (i.e., 20–25%) of depressive episodes onset before 19 years of age (Kessler et al., 2005). Excluding studies of the relations between depression and ToM in youth might limit conclusions about their association. Second, interpersonal relationships become more salient during the transition from childhood to adolescence, and social competence and psychosocial adjustment become increasingly linked during this time (Steinberg & Morris, 2001). Therefore, ToM capabilities (i.e., understanding the thoughts and feelings of the self and others) might be particularly relevant during this developmental window.
Third, neurobiologically, ToM substrates (e.g., mPFC/vmPFC) continue to develop throughout adolescence and into young adulthood (Blakemore, 2008). This continued growth highlights the importance of clarifying the potential transactional and temporal relations between depressive symptoms and ToM abilities as they emerge prior to adulthood. That is, whether ToM abilities are a precursor to depressive symptoms or depressive symptoms precede changes in ToM abilities remains an important area of investigation in future longitudinal studies.
Fourth, moderator analyses of the link between ToM and depression have been scarce. Therefore, a primary aim of the current meta-analytic review was to further clarify the extent of ToM abilities in individuals with depression across the lifespan. Examining when and for whom changes in ToM ability in relation to depression are most consequential may be useful for targeted interventions. Further, we included studies of all age groups as well as correlational studies of individuals with varying levels of depressive symptoms, not simply diagnostic groups. A secondary aim was to test specific moderators (e.g., demographic variables, assessment methods, ToM aspects) of associations between ToM and depression.
Heterogeneity of prior findings and varied aspects of ToM motivated our selection of moderators. Specifically, we assessed ToM content (i.e., affective vs. cognitive) and process (i.e., decoding vs. reasoning). Given prior work that suggests distinct neural substrates and temporal relations between affective ToM and cognitive ToM (Sebastian et al., 2011; Shamay-Tsoory et al., 2010), we explored whether ToM content moderated the relations between ToM and depression. Next, because extensive variability exists between ToM measures of decoding and reasoning processes, we explored whether one process of ToM was more challenging than the other for those with depression.
Finally, with respect to demographic variables, we tested the potential moderators of sample type, age, and gender. With respect to sample type, we were interested in replicating Bora and Berk’s (2015) finding that severity of depression was significantly associated with ToM impairment in depression. Therefore, we tested whether relations between ToM and depression differed based on clinical versus nonclinical/community samples of those with depression. Also, because we included an expansive age range in this meta-analysis, particularly child and adolescent samples, we explored whether age moderated the relation between ToM and depression. Also, we tested whether the relation between ToM and depression varied by gender. As mentioned, prior work has found that some subgroups (e.g., adolescent males with MDD) exhibit heightened affective ToM improvements (Mellick & Sharp, 2016). Moreover, some researchers have suggested that women possess better emotion identification skills than men (Baron-Cohen, 2010). Therefore, we tested gender as a moderator to clarify further the associations between ToM and depression.
Current Study
In the current meta-analysis, we investigated the associations between ToM and depression, and tested possible moderators of these associations (e.g., ToM content, process, sample type, age, and gender). In so doing, we broadened the approach of prior meta-analytic work that has focused solely on adults (i.e., Bora & Berk, 2015; Richman & Unoka, 2015), on one specific ToM task (i.e., Richman & Unoka, 2015), and exclusively on categorical measures of depression (i.e., Bora & Berk, 2015; Richman & Unoka, 2015).
Methods
Study Selection
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for this meta-analysis (Moher et al., 2009; see Figure 1), and we conducted a review of the literature using the PsycINFO database to identify relevant studies (Jan 1988 to March 2021) applying the following search string: (“theory of mind” OR mentalizing OR “social cognition” OR “perspective taking”) AND (depress* OR mood). Search results were included if they were (a) English-language publications and (b) peer-reviewed. This search strategy yielded a total of 717 articles, excluding duplicate reports. Authors identified additional records (n = 32) via Google Scholar and reference lists of published reports. Two coders (BAN, SS) independently reviewed the abstract of each search result to determine eligibility. In cases (n = 4) when coders made discrepant conclusions about article eligibility, they reached consensus by discussion. Coders examined full texts of articles when eligibility could not be deduced by the title and abstract alone.
Figure 1.
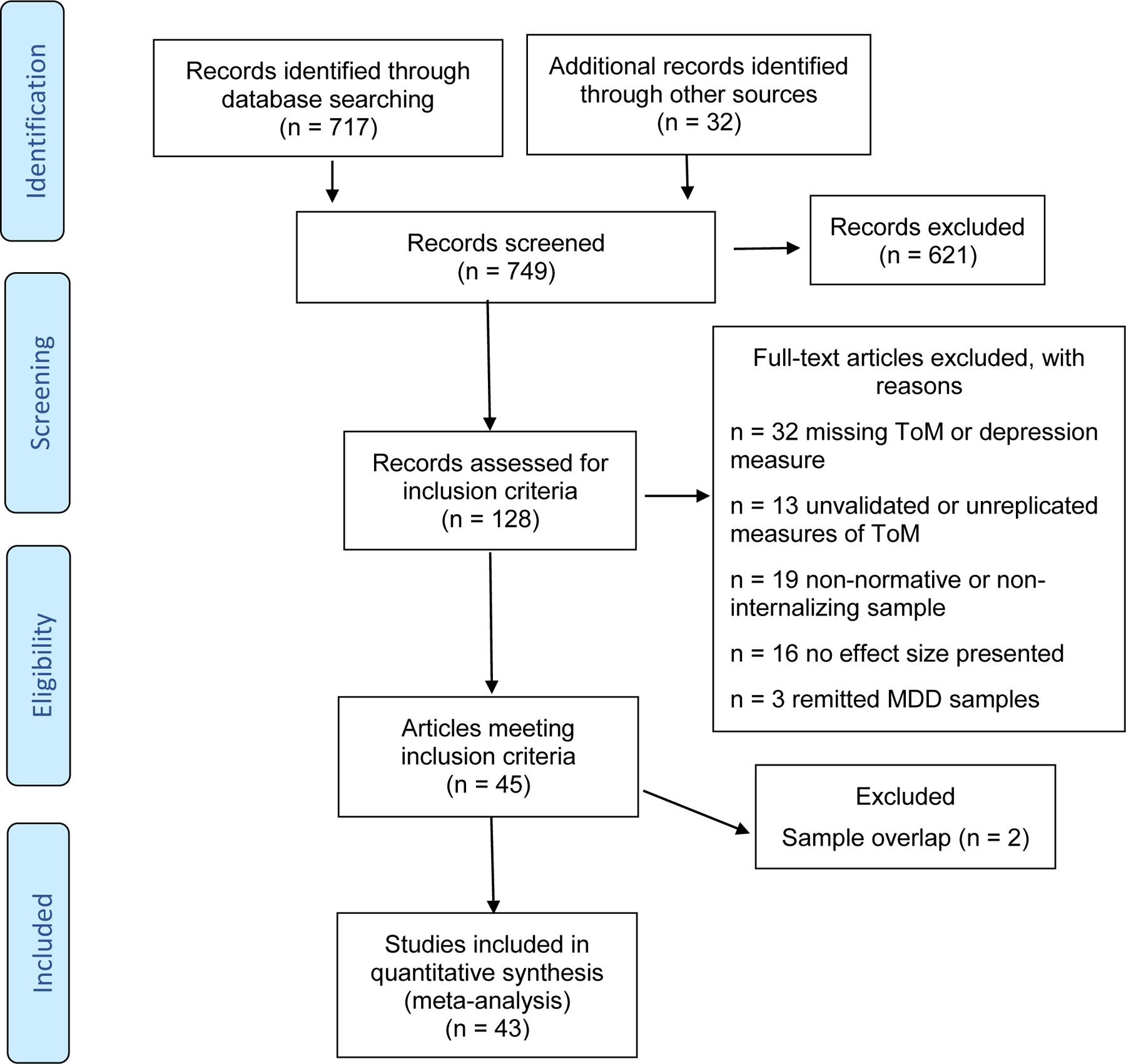
Flow Diagram for Meta-Analysis of ToM in Depression
Inclusion criteria were (a) studies that compared ToM performance of depressed individuals versus that of healthy controls; (b) studies that reported sufficient data to calculate effect size and standard error of the ToM measure or provided correlational data between ToM performance and dimensional measures of depression. Screening of abstracts identified 621 records for exclusion. We assessed the full texts of the remaining studies (n = 128) for inclusion criteria. Of these, we excluded 83 studies based on their ToM measure, participant sample, lack of reported effect sizes, or lack of relevant measures completed at baseline (for studies with multiple time points). If studies did not provide sufficient data for effect sizes to be calculated from reported findings (n= 16), we contacted authors via email. Ultimately, 43 studies met inclusion criteria. Interrater reliability across all inclusion variables was 93% or greater.
Measures of ToM
Studies used various measures of ToM including RMET (Baron-Cohen et al., 2001a) and age relevant versions (i.e., Child Eyes Test; CET; Baron-Cohen et al., 2001b), MASC (Dziobek et al., 2006), faux pas recognition tests (e.g., see McKinnon & Moscovitch, 2007), False Belief tests (e.g., see Sullivan et al., 1994), Strange Stories (Happe, 1994), The Awareness of Social Inference Test (TASIT; McDonald et al., 2003), Frith-Happe animations (Abell et al., 2000), Yoni’s task (Shamay-Tsoory & Aharon-Peretz, 2007), cartoons (Brune, 2003), ToM Tests (Muris et al., 1999), Metacognition Assessment Scale (Lysaker et al., 2005), and Mentalistic Interpretation Task (Thoma et al., 2015). Studies were only included if their measure of ToM was determined to be valid based on a review of the relevant literatures. Significant heterogeneity of ToM measures was present in the literature; therefore, the following criteria were used to determine eligibility for inclusion: 1) the measure has been used or validated previously in the literature, and 2) the measure assesses understanding of thoughts or feelings of others.
Measures of Depression
Different measures of depression were used across studies. Depression-group status was determined by a semi-structured diagnostic interview (e.g., Structured Clinical Interview for DSM-III to 5 Disorders; SCID; First et al., 1995), Diagnostic Interview Schedule for Children (DISC-IV; Shaffer et al., 2000), DSM-III to 5 criteria (American Psychiatric Association, 1987, 1994, 2013), or scores on versions of the Hamilton Rating Scale for Depression (HRSD; Hamilton, 1986) or the Hospital Anxiety and Depression Scale (HADS; Snaith, 2003). Correlational studies measured depressive symptoms with relevant versions of the Beck Depression Inventory (BDI; Beck et al., 1961), Child Depression Inventory (CDI; Kovacs, 1992), Montgomery Asberg Depression Rating Scale (MADRS; Montgomery & Asberg, 1979), Geriatric Depression Scale-30 (Sheikh & Yesavage, 1986), the HRSD, Inventory of Depressive Symptomatology (IDS; Rush et al.,1996), Quick Inventory of Depressive Symptomatology (QIDS; Rush et al., 2003), Profile of Mood States (POMS; McNair et al., 1981), Depression Anxiety Stress Scales (DASS; Lovibond & Lovibond, 1995), and versions of the Center for Epidemiological Studies Depression Scale (CESD; Radloff, 1977).
Data Extraction
Of the 45 studies meeting eligibility criteria, 2 studies had overlapping samples, so redundant findings were excluded to reduce bias, leaving a complete final sample of 43 studies. All effect sizes in the current meta-analysis were extracted from cross-sectional data. To assess for potential moderators, we extracted data for 5 study characteristics: (1) content of ToM assessment (i.e., cognitive ToM versus affective ToM); (2) process of ToM ability, (i.e., decoding versus reasoning); (3) type of sample, (i.e., nonclinical/community versus clinical); (4) mean age of whole sample; and (5) gender (i.e., percentage of sample reported as female). Except for mean age of the sample and gender (i.e., percent female), which were considered continuous variables, all other moderators were categorical. (We also identified 15 studies that used only self-report measures of ToM (i.e., Interpersonal Reactivity Index – Perspective Taking; IRI-PT; Davis, 1983; Interpersonal Emotion Regulation Questionnaire – Perspective Taking; IERQ-PT; Hofmann et al., 2016; reflective-functioning questionnaires (RFQ; Fonagy et al., 2016), which we included in a supplemental analysis in Appendix A.)
Data Analysis Plan
For studies that reported more than one ToM task, we calculated pooled effect sizes and standard error values. This was only done when the ToM measures were assessing the same content (i.e., in a given study, effect sizes of only affective ToM measures were pooled or effect sizes of only cognitive ToM measures were pooled). If studies reported more than one ToM task from dissimilar ToM content groups, then single outcomes were selected to balance randomly the number of measures assessing affective ToM and the number of measures assessing cognitive ToM. Other than the outcome of total ToM score, we calculated separate effect sizes based on the three categorical moderators of interest: content (“Affective” and “Cognitive”), process (“Decoding” and “Reasoning”), and type of sample ( “Nonclinical/Community” and “Clinical”).
When categorical groups exhibited significant heterogeneity, potential moderators were evaluated with the Q-statistic to determine whether significant between-study variability existed. We tested categorical moderators with a two-tailed significance level set at p < .05. Meta-regression analyses were conducted to test the two continuous moderators (i.e., mean age of sample and percentage of sample that was female) with a random-effects model and a two-tailed significance level set at p < .05.
We followed guidelines presented in prior work (e.g., Bora & Berk, 2015) to characterize ToM tasks based on content and process. Specifically, if measures were described to primarily assess identification or understand of feelings or emotions, we deemed them to be affective assessments. If measures were described to assess primarily thoughts, beliefs, or intentions, we deemed them to be cognitive measures. As such, we classified tasks that emphasized the understanding of emotional states of others (i.e., RMET, some items of the MASC, certain affective versions of False Belief tests) as assessments of affective ToM. We then considered all other tasks and items primarily to be assessments of cognitive ToM.
Only one task (RMET) included in the studies reviewed in this meta-analysis tested the decoding process of ToM. Thus, we considered all other measures to be assessments of the reasoning process of ToM. If studies included a clinical group (i.e., participants meeting clinical criteria for MDD), we categorized the sample as “Clinical.” Conversely, we determined studies to be “Nonclinical/Community,” if the sample included participants not assessed for a diagnosis or not meeting criteria for a disorder.
We conducted all analyses with Comprehensive Meta-Analysis Version 3 (Borenstein et al., 2015), which calculated Hedges’ g from reported means and standard deviations, t-statistics, p-values, or correlations. Confidence intervals and z-values of the effect sizes were used to assess statistical significance. Similar to Cohen’s d, Hedges’ g effect sizes indicate small (g = .2), medium (g = .5), or large (g > .8) magnitudes. Random-effects models were used as the distributions of effect sizes were heterogenous for the number of variables. Homogeneity of the distribution of weighted effect sizes were tested with I-squared and Q-tests. Tau-squared, an estimate of between study variance, was used as a measure of heterogeneity in the random-effects model. Table 1 presents characteristics of included studies.
Table 1.
Characteristics of Included Studies
| Study | ToM Measure | Content | Process | Sample Type | Depression Measure | Age in Years | % Female | N | Country |
|---|---|---|---|---|---|---|---|---|---|
| Al Ain et al., 2013 | RMET | Aff. | Decoding | Comm. | BDI | 24 | 59 | 107 | France |
| Augustin et al., 2020 | FHA | Cog. | Reasoning | Comm. | BDI | 42 | 40 | 40 | Germany |
| Bertoux et al., 2012 | faux pas | Cog. | Reasoning | Clinical | MADRS | 63 | 51 | 49 | France |
| Camodeca et al., 2020 | RMET | Aff. | Decoding | Comm. | DASS | 20 | 55 | 143 | USA |
| Cao et al., 2013 | RMET | Aff. | Decoding | Clinical | BDI-II | 49 | n.p. | 127 | China |
| Caputi & Schoenborn, 2018 | Strange stories | Cog. | Reasoning | Comm. | CDI | 11 | 49 | 326 | Italy |
| Caputi et al., 2017 | Strange stories | Cog. | Reasoning | Comm. | CDI | 11 | 51 | 368 | Italy |
| Corcoran et al., 2008 | false belief | Cog. | Reasoning | Clinical | DSM | 43 | 50 | 60 | England |
| Cusi et al., 2013 | faux pas | Cog. | Reasoning | Clinical | HDRS | 47 | 70 | 40 | Canada |
| Demers & Koven, 2015 | RMET | Aff. | Decoding | Comm. | POMS | 19 | 66 | 86 | USA |
| Ellement et al., 2021 | false belief | Cog. | Reasoning | Comm. | HADS | 56 | 87 | 45 | Canada |
| Harkness et al., 2005 | RMET | Aff. | Decoding | Comm. | BDI | 20 | 70 | 81 | Canada |
| Harkness et al., 2012 | RMET | Aff. | Decoding | Comm. | BDI-II | 18 | 100 | 95 | Canada |
| Hentze et al., 2016 | false belief | Aff. | Reasoning | Clinical | MADRS | 42 | 64 | 25 | Germany |
| Kessels et al., 2020 | false belief | Cog. | Reasoning | Clinical | GDS-30 | 72 | 51 | 45 | Netherlands |
| Kettle et al., 2008 | RMET | Aff. | Decoding | Clinical | CESD | 19 | 63 | 30 | Australia |
| Kilic et al., 2020 | RMET | Aff. | Decoding | Comm. | BDI | 26 | 100 | 35 | Turkey |
| Kilincel et al., 2020 | RMET | Aff. | Decoding | Clinical | CDI | 13 | 64 | 61 | Turkey |
| Ladegaard et al., 2014 | FHA, TASIT | Cog. | Reasoning | Clinical | HDRS | 33 | 75 | 44 | Denmark |
| Ladegaard et al., 2016 | FHA, MAS | Cog. | Reasoning | Clinical | HDRS | 33 | 79 | 29 | Denmark |
| Lannoy et al., 2020 | Yoni Task | Aff. | Reasoning | Comm. | BDI | 17 | 62 | 202 | France |
| Lee et al., 2020 | RMET | Aff. | Decoding | Clinical | CESD | 77 | 62 | 676 | USA |
| Maleki et al., 2020 | faux pas | Cog. | Reasoning | Clinical | BDI | 28 | 52 | 72 | Iran |
| Manstead et al., 2013 | RMET | Aff. | Decoding | Clinical | BDI-II | 22 | 84 | 164 | England |
| Mattern et al., 2015 | false belief | Aff. | Reasoning | Clinical | IDS-SR | 41 | 58 | 52 | Germany |
| Mellick & Sharp, 2016 | CET | Aff. | Decoding | Clinical | DISC | 14 | 0 | 117 | USA |
| Monteleone et al., 2020 | MASC | Cog. | Reasoning | Clinical | DASS | 27 | 100 | 77 | Italy |
| Nejati et al., 2012 | RMET | Aff. | Decoding | Clinical | DSM | 28 | 59 | 95 | Iran |
| Rothschild-Yakar et al., 2019 | RMET | Aff. | Decoding | Clinical | SCID/BDI | 17 | 100 | 73 | Israel |
| Samson et al., 2012 | false belief | Cog. | Reasoning | Comm. | BDI | 24 | 50 | 52 | Austria |
| Sarfati et al., 1999 | Cartoons | Cog. | Reasoning | Clinical | DSM | 27 | 42 | 26 | France |
| Scaini et al., 2020 | Strange stories | Cog. | Reasoning | Comm. | CDI | 11 | 50 | 337 | Italy |
| Simon et al., 2019 | RMET | Aff. | Decoding | Clinical | HDRS | 33 | 67 | 92 | Hungary |
| Szanto et al., 2012 | RMET | Aff. | Decoding | Clinical | SCID | 69 | 56 | 90 | USA |
| Szily & Keri, 2009 | RMET | Aff. | Decoding | Clinical | SCID | 20 | 63 | 70 | Hungary |
| Thoma et al., 2015 | MI | Cog. | Reasoning | Clinical | HDRS | 41 | 58 | 56 | Germany |
| Wang et al., 2008 | faux pas | Cog. | Reasoning | Clinical | BDI | 28 | 57 | 86 | China |
| Washburn et al., 2016 | MASC | Cog. | Reasoning | Clinical | BDI | 19 | 68 | 83 | Canada |
| Wilbertz et al., 2010 | MASC | Cog. | Reasoning | Clinical | BDI | 44 | 50 | 32 | Germany |
| Wolkenstein et al., 2011 | MASC | Cog. | Reasoning | Clinical | QIDS | 36 | 57 | 44 | Germany |
| Zahavi et al., 2016 | RMET | Aff. | Decoding | Clinical | BDI | 23 | 72 | 96 | Canada |
| Zobel et al., 2010 | Cartoons | Cog. | Reasoning | Clinical | IDS-SR | 47 | 55 | 60 | Germany |
| Zwick & Wolkenstein, 2017 | MASC | Cog. | Reasoning | Clinical | HDRS | 43 | 65 | 81 | Germany |
Note. Aff = Affective; BDI = Beck Depression Inventory; CDI = Child Depression Inventory; CESD = Center for Epidemiological Studies Depression Scale; CET = Child Eyes Test; Cog = Cognitive; Comm = Nonclinical/Community; DASS = Depression Anxiety Stress Scale; DISC = Diagnostic Interview Schedule for Children; DSM = Diagnostic and Statistical Manual of Mental Disorders; FHA = Frith-Happe Animations; GDS-30 = Geriatric Depression Scale-30; HADS = Hospital Anxiety and Depression Scale; HDRS = Hamilton Depression Rating Scale, IDS-SR = Inventory of Depressive Symptomatology; MADRS = Montgomery Asberg Depression Rating Scale; MASC, Movie for Assessment of Social Cognition; MIT = Mentalistic Interpretation Task; POMS = Profile of Mood States; QIDS = Quick Inventory of Depressive Symptomatology; RMET, Reading the Mind in the Eyes Test; SCID = Structured Clinical Interview for DSM; TASIT = The Awareness of Social Inference Test.
Results
ToM and Depression
This analysis of effect sizes included 29 studies that tested differences in ToM performance in individuals with depression versus healthy controls, and 14 studies that directly tested the relations between ToM and depression (i.e. the continuous symptom measures). Analysis revealed a moderate effect size (Hedges’ g = −0.398, 95% CI [−.540, −.255]) for the relations between ToM and depression, indicating impaired ToM in individuals with depression. Significant heterogeneity (tau-squared = .166, I-squared = 78.966) emerged for the distribution of effect sizes in the random-effects model. Given that the variability in effect sizes across studies differed more than sampling error alone, we conducted analyses of the moderator variables.
Publication Bias
We examined the funnel plot for our meta-analytic model, and we assessed the likelihood of the existence of publication bias with three statistical methods: Begg and Mazumdar rank correlation test (Begg & Mazumdar, 1994), Egger’s test of the intercept (Egger et al., 1997), and trim and fill analyses (Duval & Tweedie, 2000). Figure 2a presents the funnel plot for the meta-analysis of the associations between ToM and depression. Non-significant Begg and Mazumdar rank correlation (p = .252, one-tailed) and Egger (p = .321, one-tailed) tests do not indicate publication bias. Trim and fill analyses revealed that 12 values be added to the left of the mean to create a symmetrical funnel plot, and that the adjusted effect size remained significant, and was greater in magnitude, after this imputation (g = −.607, 95% CI [−.760, −.454]). Together, these tests do not reveal evidence of publication bias in this set of studies. Figure 2b depicts a forest plot of effect sizes for depression studies included in this model.
Figure 2a.
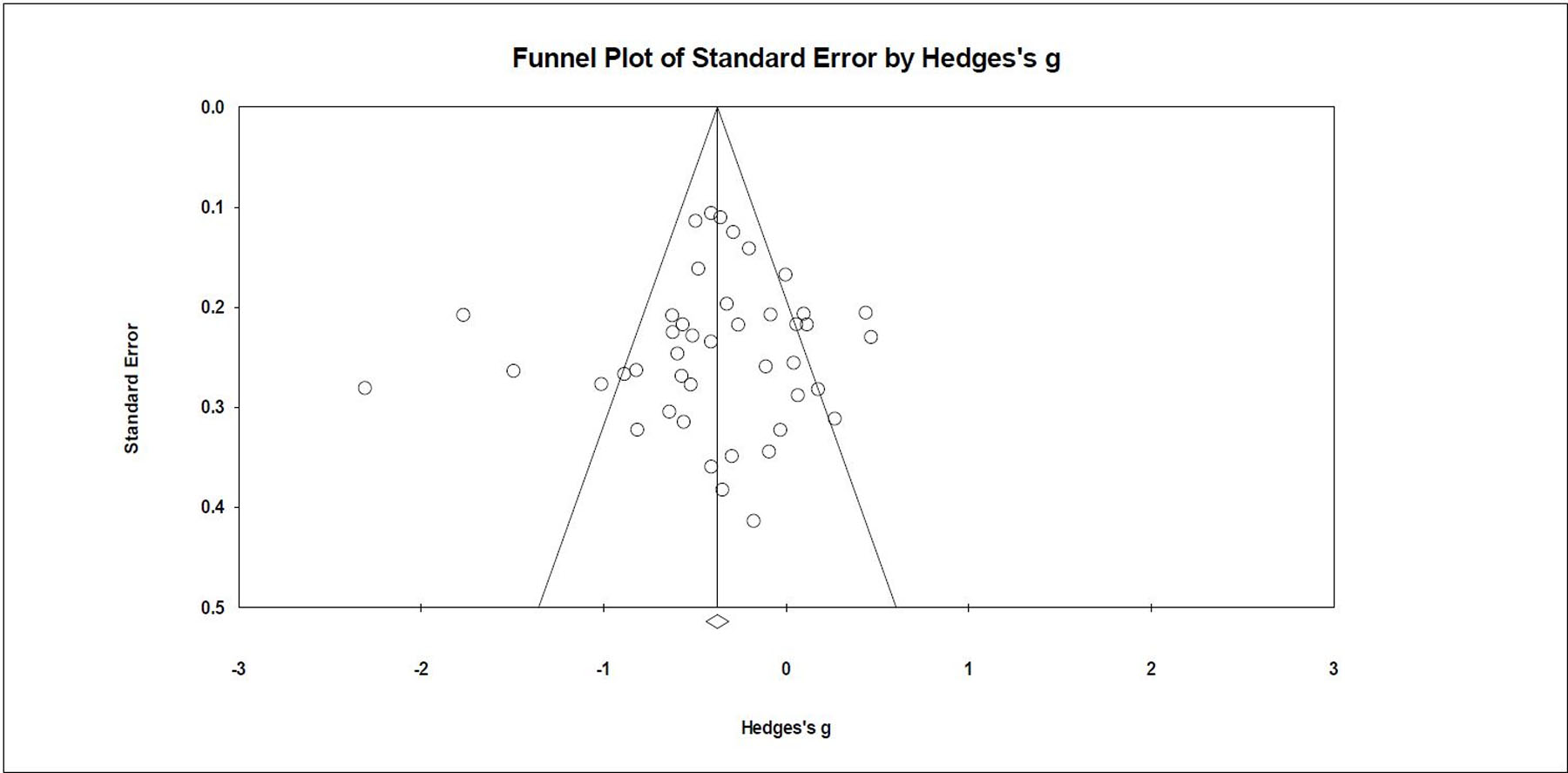
Funnel Plot for Associations between ToM and Depression
Note. ToM = Theory of Mind
Figure 2b.
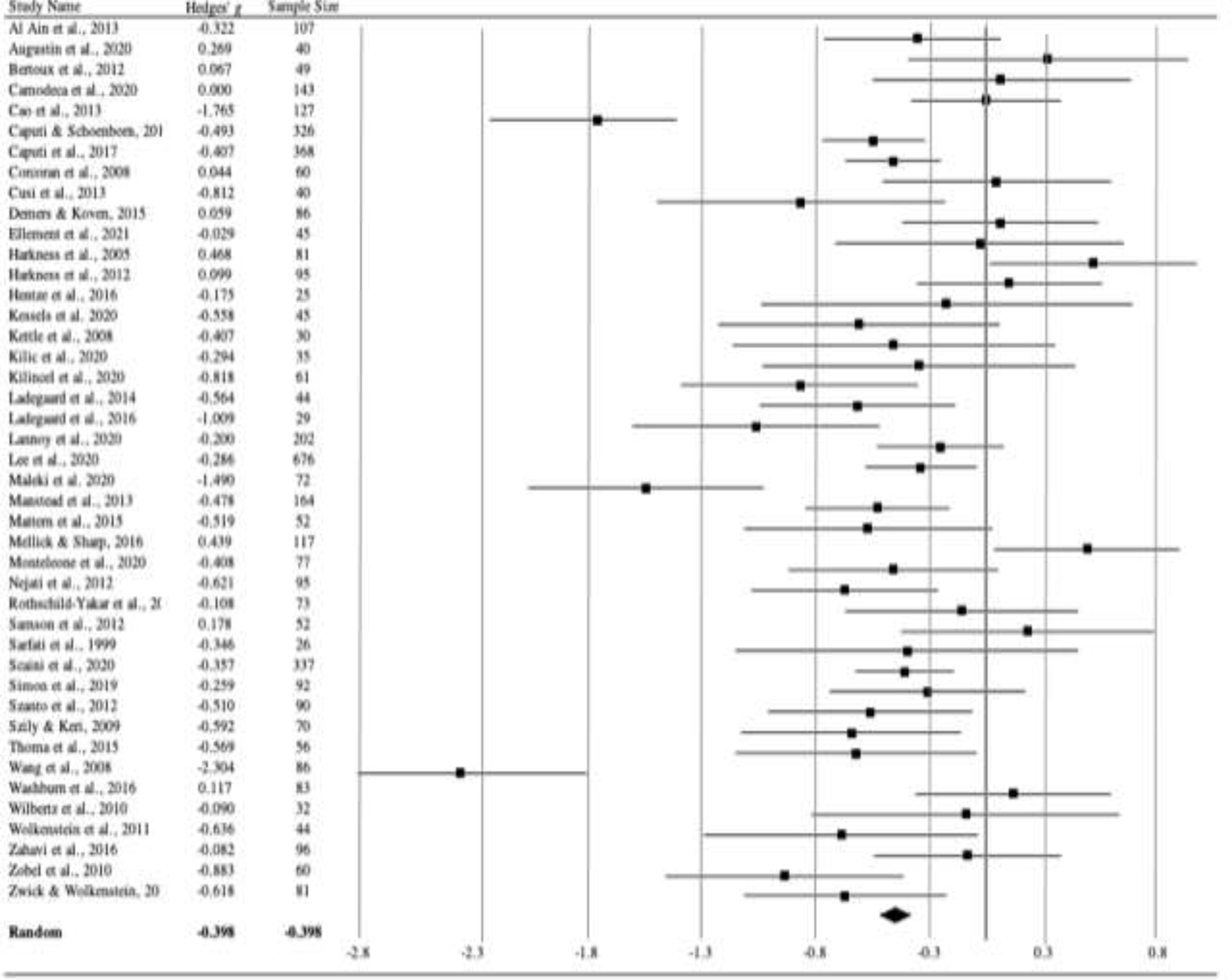
Forest Plot for Associations between ToM and Depression
Note. ToM = Theory of Mind
Moderator Analyses
We conducted three moderator analyses to compare effect sizes across various types of potential moderators. These included content (i.e., affective versus cognitive), process (i.e., decoding versus reasoning), and sample type (i.e., clinical versus nonclinical/community). We used meta-regressions to test two demographic moderators (i.e., mean age and percentage of sample that was female). Table 2 includes categorical moderator results.
Table 2.
Meta-analysis of ToM and Depression
| 95% Confidence Interval | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| k | G | Lower | Upper | Q | p | I 2 | T 2 | pEgger | |
| Depression Total | 43 | −.398 | −.540 | −.255 | 78.966 | .166 | .321 | ||
| Content | 1.82 | 0.177 | |||||||
| Affective | 21 | −.300 | −.501 | −.100 | |||||
| Cognitive | 22 | −.496 | −.699 | −.294 | |||||
| Process | 1.322 | 0.25 | |||||||
| Decoding | 18 | −.301 | −.532 | −.070 | |||||
| Reasoning | 25 | −.473 | −.654 | −.292 | |||||
| Sample Type | 9.656 | .002 | |||||||
| Clinical | 30 | −.540 | −.740 | −.341 | |||||
| Community | 13 | −.137 | −.295 | −.021 | |||||
Note. ToM = Theory of Mind; Nonclin/Comm = Nonclinical/Community
Content.
Twenty-one studies assessed affective ToM, and 22 studies assessed cognitive ToM. The relations between ToM and depression were significant for both affective (g = −.300, 95% CI [−.501, −.100]) and cognitive (g = −.496, 95% CI [−.699, −.294]) content. The difference between effect sizes by content was not significant (Q(1) = 1.820, p = .177).
Process.
Eighteen studies assessed decoding processes, and 25 studies assessed reasoning processes. The relations between ToM and depression were significant for both decoding (g = −.301, 95% CI [−.532, −.070]) and reasoning (g = −.473, 95% CI [−.654, −.292]) processes. The difference between effect sizes by ToM process was not significant (Q(1) = 1.322, p = .250).
Sample Type.
Thirty studies assessed clinical samples, and 13 studies assessed nonclinical/community samples. The relations between ToM and depression were significant for clinical (g = −.540, 95% CI [−.740, −.341]) but not for nonclinical/community (g = −.137, 95% CI [−.295, .021]) samples. The difference between effect sizes between these two groups was significant (Q(1) = 9.656, p = .002).
Age and Gender.
Mean age of sample did not significantly moderate the relations between ToM and depression (Z = −1.03, p = .303). Gender, as indexed by the percentage of sample that was female, also did not significantly moderate the relations between ToM and depression (Z = −0.42, p = .673).
Discussion
The current meta-analytic review investigated ToM abilities in individuals with depression. Specifically, we explored the extent to which ToM abilities were impaired, comparable, or heightened in individuals with depression as compared to healthy controls. The results revealed that there were significant ToM deficits with medium effect sizes in depression, indicating that individuals with depression have significant difficulties in this aspect of social cognition.
Our results revealed that individuals with depression show significant impairment in ToM. The moderate magnitude of ToM impairment in depression was comparable to the medium effect size previously reported in the 18-study meta-analysis of ToM abilities in adults with MDD versus healthy controls (Bora & Berk, 2015), but it was considerably smaller than the large effect size reported in the meta-analysis of ToM abilities based on only one measure (i.e., RMET) in adults with MDD versus healthy controls (Richman & Unoka, 2015). The current analysis expanded upon these earlier reviews by updating with studies since 2015 and including a more comprehensive set of relevant studies (i.e., samples of varied ages with both diagnostic and dimensional depressive symptoms and varied measures of ToM). These features enabled us to draw conclusions based on a broader representation of studies across a larger age range for both clinical and nonclinical samples.
Several factors may contribute to impairment in ToM in individuals with depression. First, depression often is characterized by negative self-focused attention or self-absorption (for review, see Ingram, 1990; Mor & Winquist, 2002). This inward, internal bias toward negative thinking or rumination about the self and personal thoughts and feelings might diminish or compromise natural curiosity, concern, and engagement with the mental and emotional states of others. For example, individuals with depression might be so consumed by their own negative thoughts (e.g., “I never do anything right.”) that they fail to attend to the cognitive and affective experiences of those around them.
Similarly, those with depression might experience the world around them as aversive due to their own negative biases. As such, individuals with depression might typically misidentify the mental states of others because they view them through a negative lens. That is, individuals with depression might notice the thoughts and feelings of others, but inaccurately identify such thoughts and feelings due to their generally negative outlook. This view is consistent with previous research that has found that depressed individuals display a biased negative perception of others’ facial expressions (Raes et al., 2006).
Another possibility is that individuals with depression withdraw socially from others, whether due to intense low mood, anhedonia, fatigue, or other depressive symptoms (for review, see Porcelli et al., 2019). In states of social withdrawal, social-emotional motivation is impaired often leading to a reduced frequency of interpersonal interactions. Individuals with depression may become less skilled at identifying the thoughts and feelings of others because they are out of practice engaging in effective social interactions. Findings from studies of young children and ToM indicate that children who spend more time observing social interactions exhibit better ToM performance (Moore et al., 2011). Perhaps, exposure to social interactions, even in the absence of engagement in these interactions, improves an individual’s understanding of the thoughts and feelings of others. Therefore, with respect to depression, social withdrawal from engagement with and from observation of social interactions may contribute to diminished ToM skill.
Yet another important explanation of impaired ToM in depressed individuals may be related to neural abnormalities in substrates implicated in ToM networks within the brain. The prefrontal lobe emerges as necessary for ToM performance (Stuss et al., 2001), and in depressed patients, previous research has identified impairments both structurally and functionally in ventromedial prefrontal regions (Bora et al., 2012; Disner et al., 2011). On a neurobiological level, depressed individuals might not show the same responses to the thoughts and feelings of others. In youth with depression, prior research has found dysfunction in networks that support emotion processing (Kerestes et al., 2014), which may be foundational to ToM. These include medial prefrontal cortical networks and connections to limbic regions (i.e., specifically, the amygdala; Kerestes et al., 2014). Additionally, in a review of social cognition in adults with mood disorders, Cusi and colleagues (2012) found lower activation in prefrontal areas and increased activation in subcortical and limbic regions, suggesting that alterations of neural activation might be associated with differences in ToM performance in mood disorders. Further work is needed to clarify the neurobiological aspects of ToM-specific deficits in depression.
Moderator analyses revealed additional specific findings that advance our understanding of ToM impairments in individuals with depression. Consistent with Bora and Berk’s (2015) results, our moderator analyses revealed significant impairment in both cognitive and affective ToM content, and in both decoding and reasoning process domains. The similar finding in content and process domains likely reflects the substantial overlap between affective content and decoding processes versus cognitive content and reasoning processes. Although the constructs of content and process are theoretically similar, they also are distinct. Most ToM measures that assess affective content rely on instantaneous decoding processes (e.g., the RMET, which was the most frequently used measure of decoding and affective ToM used in studies in this review). Similarly, most ToM measures of cognitive content rely on more deliberative reasoning processes (e.g., false belief tasks requiring inferences about the knowledge of others). Few ToM measures violate this affective/decoding and cognitive/reasoning association, although some do. Tasks such as the affective versions of faux pas tests require participants to reason about the emotional states of others (Mattern et al., 2015). Therefore, due to fewer tasks testing specific affective/reasoning and cognitive/decoding skills, the moderator findings in content and process domains could be redundant.
Another important moderator was sample type. Depression related impairments in ToM were significant only for clinical samples, not for nonclinical/community samples. This finding is consistent with other studies showing that greater severity of depression is significantly associated with greater ToM impairment (Bora & Berk, 2015). Whether the intensity of depression leads to such ToM deficits, or whether ToM deficits lead to more severe presentations of depression remains an important question that needs to be tested. Our finding that nonclinical/community samples did not display a ToM deficit may relate generally to a previous finding indicating an association between dysphoria and superior ToM (e.g., Harkness et al., 2005), though we did not observe superior ToM in the nonclinical samples reviewed here.
What might explain these mixed findings? Very few studies have specifically assessed dysphoria and ToM. Although our meta-analysis included both nonclinical and clinical samples, dysphoric participants may be particularly understudied. Individuals with dysphoria may be excluded from studies of individuals meeting full criteria for MDD because their depressive symptoms are not severe enough, and they also may be excluded from studies examining normative samples because their depressive symptoms are too severe. Future work should seek to replicate this interesting finding by Harkness and colleagues (2005) by specifically selecting samples of dysphoric individuals.
Additionally, in the meta-regression, we found that age did not significantly moderate the relations between ToM and depression. Nonlinear relations, however, between ToM and age in depression also should be examined. Future studies should compare individuals across the lifespan on ToM abilities using the same measures of both ToM and depression to clarify specific age differences over time.
Finally, no significant moderation effect emerged for gender on the relations between ToM and depression. Although theoretical work suggests that women might be more disposed to empathy than men (Baron-Cohen, 2010), the current analyses did not find differences on ToM between males versus females with depression. Nonsignificant age and gender moderating effects are consistent with prior meta-analytic findings (e.g., Bora & Berk, 2015).
Clinical Implications
The results of this meta-analytic review may be relevant to the development of interventions for depression as targeting ToM in the treatment of depression may improve outcomes for individuals with ToM deficits. In a meta-analysis of 32 intervention studies, Hofmann and colleagues (2016) found that ToM training interventions, even in brief administrations, significantly improved children’s ToM as compared to control interventions. ToM improvements occurred in typically developing children, those with hearing impairments, and those with ASD. Thus, such ToM interventions might be suitable for individuals with diverse abilities and presentations.
In the adult literature, ToM interventions for nonclinical populations are scarce. One study of older adults (ages 60–85) found that a targeted intervention improved ToM as compared to an active control group (Rosi et al., 2016). To our knowledge, no other interventions targeting ToM in adult healthy controls exist. In contrast, interventions for improving ToM in adults with ASD or schizophrenia are quite effective (for a review, see Fletcher-Watson et al., 2014; Bechi et al., 2013; 2015). Evidence is less conclusive, however, regarding the e enduring effects of these interventions on ToM performance or on symptoms of ASD or schizophrenia.
To date, no intervention exists that specifically targets ToM in individuals with depression. Tailoring such interventions according to type of ToM errors common in depression might be particularly useful. A randomized controlled trial is currently under way that is testing the efficacy of a ToM-focused CBT intervention, compared to a standard CBT intervention, for adolescents with depression (Garber, 2018). For individuals with depression, interventions that target and improve ToM might focus on appropriately identifying the thoughts and feelings of others as one way to strengthen social relationships.
Individuals with depression also might benefit from practicing more positive ToM strategies. For example, to counteract the potential negative bias of ToM in depression, an intervention might teach depressed individuals to apply a more positive lens to the thoughts and feelings of those around them. Bolstering this understanding of others could be a particularly important treatment target for individuals with depression because deficits in ToM in remitted adults have been shown to be a vulnerability for recurrence of a subsequent depressive episode (Inoue et al., 2006). If interventions could enhance ToM in individuals with depression, recurrence may be less likely.
A curvilinear relation between depression and ToM also should be considered. At one end of the curve, depressed individuals might show deficits in their ability to take another’s perspective, which is the typical pattern found for depressed individuals. On the other hand, some individuals with depression might “over mentalize,” such that they still misinterpret the thoughts and feelings of others, but they attribute more intense thoughts or feelings to them. Thus, at both ends of the curve, they would exhibit wrong ToM, although in quite different ways. Future work should explore the possibility of such curvilinear relations between depression and ToM performance and its implications for intervention. If we can identify optimal points on a curve where ToM performance is at its best or worst, we can use this information to target both clinical symptoms and ToM skills.
Strengths, Limitations, and Conclusions
A strength of this meta-analysis was its broad relevance and contribution to clinical, developmental, and social-cognitive literatures. Additionally, this comprehensive meta-analysis included studies that used a wide variety of research designs. Most prior meta-analytic work in this area investigated only studies that tested differences between clinical groups (i.e., those with a diagnosis of depression) and healthy controls in adult samples (e.g., Bora & Berk, 2015; Richman & Unoka, 2015). In contrast, the current review extended findings by incorporating studies that examined associations between dimensional measures of depression and ToM performance in normative samples. Beyond adults, we also included child, adolescent, and young adult samples. As such, we are able to draw broader conclusions about ToM ability in relation to depression, for clinical diagnoses, subclinical constellations of symptoms, and varying age groups. Moreover, the current meta-analysis examined multiple potential moderators that provide valuable information about ToM as a construct, clinical or nonclinical status of depression, and age and gender. The studies in this meta-analysis included samples from a wide range of geographic regions, thus expanding the scope and diversity of these research findings (see Table 1).
Limitations of this review also should be noted. First, as with all meta-analytic work, results must be considered in the context of potential publication bias as unpublished studies may have had smaller effects than published studies. Second, results of meta-analyses can provide only an aggregate, summary statistic (i.e., one effect size) per study. As such, findings of specificity greater than the main outcomes investigated here could not be represented in this meta-analysis, and context and quality of individual studies cannot be captured. Still, inclusion of our extensive moderator variables affords some increased contextual precision.
Third, the small to moderate deficits observed in ToM may overlap considerably with similar deficits observed in depression for other executive functions and social-cognitive facets (e.g., Snyder 2013; Weightman et al., 2014). Nevertheless, the observed findings hold specific promise for clinical intervention because prior work shows ToM’s potential for change through intervention. Fourth, our meta-analysis was limited by the fact that all included studies were cross-sectional, preventing us from determine the temporal and possible bidirectional relations between depression and ToM.
We propose three key design strategies to address this issue: longitudinal designs, at-risk samples, and samples with remitted depression. First, we suggest using broad longitudinal designs to understand directional relations between ToM and depression to guide intervention targets and timing. Do ToM deficits precede the onset of depression? Does depression precede deficits in ToM? Does some third variable (e.g., temperament, intelligence, social competence) predict both depression and ToM deficits? Second, we recommend identifying at-risk samples (e.g., offspring of depressed parents or individuals already showing impairment in ToM ability) and conducting prospective evaluations to determine the subsequent onset of depression. Third, we suggest assessment of individuals with remitted depression to determine whether ToM impairments persist even when individuals are not in a current episode or having current symptoms. Results of studies of those with remitted depression have been mixed, with some studies showing lingering ToM deficits in remission (Inoue et al., 2004; Inoue et al., 2006; Ladegaard et al., 2016), other studies finding no differences (Air et al., 2015; Purcell et al., 2013), and still others revealing enhanced ToM in remission (Harkness et al., 2010).
Despite these limitations, the current meta-analysis provides important findings about the relation between ToM and depression. Our results demonstrated significant and moderate impairment in ToM in individuals with depression, with additional specific moderator findings. More work is needed to determine the direction of these associations, changes in these relations over the course of development, and the efficacy of interventions aimed at reducing and preventing deficits in ToM for those currently experiencing or at-risk for depression.
Supplementary Material
Highlights.
Meta-analysis of depression and theory of mind (ToM) or the ability to understand the thoughts and feelings of others
Small-moderate ToM deficits (g = −.398) observed in individuals with depression across the lifespan
Intervention and prevention work should target this specific ability in conjunction with depressive symptoms
Funding Sources:
This work was supported in part from National Institute of Mental Health grants (R01MH100258; R61MH115125) and training grant (T32 MH018921).
We have no acknowledgements to report.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
The other authors declare no conflicts of interest.
References
- Abell F, Happe F, & Frith U (2000). Do triangles play tricks? Attribution of mental states to animated shapes in normal and abnormal development. Cognitive Development, 15(1), 1–16. [Google Scholar]
- Air T, Weightman MJ, & Baune BT (2015). Symptom severity of depressive symptoms impact on social cognition performance in current but not remitted major depressive disorder. Frontiers in Psychology, 6, 1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Aïn S, Carré A, Fantini-Hauwel C, Baudouin JY, & Besche-Richard C (2013). What is the emotional core of the multidimensional Machiavellian personality trait? Frontiers in Psychology, 4, 454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (1987). Diagnostic and statistical manual of mental disorders (3rd ed., text rev.). Washington, DC: Author. [Google Scholar]
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author. [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. [Google Scholar]
- Augustin M, Eichhammer P, Haas J, Schiekofer S, & Busch V (2020). Increased Alexithymia But No Profound Emotion Processing Disorder in Burnout Syndrome. The Journal of Nervous and Mental Disease, 208(10), 794–802. [DOI] [PubMed] [Google Scholar]
- Baron-Cohen S (2000). Theory of mind and autism: A fifteen year review. Understanding other minds: Perspectives from Developmental Cognitive Neuroscience, 2, 3–20. [Google Scholar]
- Baron-Cohen S (2010). Empathizing, systemizing, and the extreme male brain theory of autism. In Progress in Brain Research (Vol. 186, pp. 167–175). Elsevier. [DOI] [PubMed] [Google Scholar]
- Baron-Cohen S, Wheelwright S, Hill J, Raste Y, & Plumb I (2001a). The “Reading the Mind in the Eyes” Test revised version: a study with normal adults, and adults with Asperger syndrome or high-functioning autism. The Journal of Child Psychology and Psychiatry and Allied Disciplines, 42(2), 241–251. [PubMed] [Google Scholar]
- Baron-Cohen S, Wheelwright S, Spong A, Scahill V, & Lawson J (2001b). Are intuitive physics and intuitive psychology independent? A test with children with Asperger Syndrome. Journal of Developmental and Learning Disorders, 5(1), 47–78. [Google Scholar]
- Baxter AJ, Patton G, Scott KM, Degenhardt L, & Whiteford HA (2013). Global epidemiology of mental disorders: what are we missing? PloS One, 8(6), e65514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bechi M, Spangaro M, Bosia M, Zanoletti A, Fresi F, Buonocore M, … & Cavallaro R (2013). Theory of Mind intervention for outpatients with schizophrenia. Neuropsychological Rehabilitation, 23(3), 383–400. [DOI] [PubMed] [Google Scholar]
- Bechi M, Bosia M, Spangaro M, Buonocore M, Cocchi F, Pigoni A, … & Cavallaro R (2015). Combined social cognitive and neurocognitive rehabilitation strategies in schizophrenia: neuropsychological and psychopathological influences on Theory of Mind improvement. Psychological Medicine, 45(15), 3147–3157. [DOI] [PubMed] [Google Scholar]
- Beck AT (1991). Cognitive therapy: A 30-year retrospective. American Psychologist, 46, 368–375. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward C, Mendelson M, Mock J, & Erbaugh J (1961). Beck Depression Inventory (BDI). Archives of General Psychiatry, 4(6), 561–571. [DOI] [PubMed] [Google Scholar]
- Begg CB, & Mazumdar M (1994). Operating characteristics of a rank correlation test for publication bias. Biometrics, 1088–1101. [PubMed]
- Berecz H, Tényi T, & Herold R (2016). Theory of mind in depressive disorders: a review of the literature. Psychopathology, 49(3), 125–134. [DOI] [PubMed] [Google Scholar]
- Bernstein DM, Thornton WL, & Sommerville JA (2011). Theory of mind through the ages: Older and middle-aged adults exhibit more errors than do younger adults on a continuous false belief task. Experimental Aging Research, 37(5), 481–502. [DOI] [PubMed] [Google Scholar]
- Bertoux M, Delavest M, de Souza LC, Funkiewiez A, Lépine JP, Fossati P, … & Sarazin M (2012). Social cognition and emotional assessment differentiate frontotemporal dementia from depression. Journal of Neurology, Neurosurgery, and Psychiatry, 83(4), 411–416. [DOI] [PubMed] [Google Scholar]
- Blakemore SJ (2008). The social brain in adolescence. Nature Reviews Neuroscience, 9(4), 267–77. [DOI] [PubMed] [Google Scholar]
- Bora E, & Berk M (2015). Theory of mind in major depressive disorder: A meta-analysis. Journal of Affective Disorders, 191, 49–55. [DOI] [PubMed] [Google Scholar]
- Bora E, Fornito A, Pantelis C, & Yücel M (2012). Gray matter abnormalities in major depressive disorder: a meta-analysis of voxel based morphometry studies. Journal of Affective Disorders, 138(1–2), 9–18. [DOI] [PubMed] [Google Scholar]
- Bora E, Yucel M, & Pantelis C (2009). Cognitive functioning in schizophrenia, schizoaffective disorder and affective psychoses: meta-analytic study. The British Journal of Psychiatry, 195(6), 475–482. [DOI] [PubMed] [Google Scholar]
- Borenstein M, Hedges L, Higgins J, & Rothstein H (2015). Regression in meta-analysis. Comprehensive Meta-Analysis Version 3, Biostat, Englewood, NJ. [Google Scholar]
- Brothers L, & Ring B (1992). A neuroethological framework for the representation of minds. Journal of Cognitive Neuroscience, 4(2), 107–118. [DOI] [PubMed] [Google Scholar]
- Brüne M (2003). Theory of mind and the role of IQ in chronic disorganized schizophrenia. Schizophrenia Research, 60(1), 57–64. [DOI] [PubMed] [Google Scholar]
- Brüne M, & Brüne-Cohrs U (2006). Theory of mind—evolution, ontogeny, brain mechanisms and psychopathology. Neuroscience & Biobehavioral Reviews, 30(4), 437–455. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, & Thisted RA (2010). Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychology and Aging, 25(2), 453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camodeca A, Walcott K, Hosack A, & Todd KQ (2020). Preliminary evidence for the Emotion Word Fluency Test as a unique semantic fluency measure. Psychological Assessment [DOI] [PubMed]
- Cao Y, Zhao QD, Hu LJ, Sun ZQ, Sun SP, Yun WW, & Yuan YG (2013). Theory of mind deficits in patients with esophageal cancer combined with depression. World Journal of Gastroenterology: WJG, 19(19), 2969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caputi M, Pantaleo G, & Scaini S (2017). Do feelings of loneliness mediate the relationship between sociocognitive understanding and depressive symptoms during late childhood and early adolescence? The Journal of Genetic Psychology, 178(4), 207–216. [DOI] [PubMed] [Google Scholar]
- Caputi M, & Schoenborn H (2018). Theory of mind and internalizing symptoms during middle childhood and early adolescence: The mediating role of coping strategies. Cogent Psychology, 5(1), 1487270. [Google Scholar]
- Clark M, DiBenedetti D, & Perez V (2016). Cognitive dysfunction and work productivity in major depressive disorder. Expert Review of Pharmacoeconomics & Outcomes Research, 16(4), 455–463. [DOI] [PubMed] [Google Scholar]
- Corcoran R, Rowse G, Moore R, Blackwood N, Kinderman P, Howard R, … & Bentall RP (2008). A transdiagnostic investigation of ‘theory of mind’ and ‘jumping to conclusions’ in patients with persecutory delusions. Psychological Medicine, 38(11), 1577–1583. [DOI] [PubMed] [Google Scholar]
- Cusi AM, Nazarov A, Holshausen K, MacQueen GM, & McKinnon MC (2012). Systematic review of the neural basis of social cognition in patients with mood disorders. Journal of Psychiatry & Neuroscience 37(3), 154–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cusi AM, Nazarov A, MacQueen GM, & McKinnon MC (2013). Theory of mind deficits in patients with mild symptoms of major depressive disorder. Psychiatry Research, 210(2), 672–674. [DOI] [PubMed] [Google Scholar]
- Davis MH (1983). The effects of dispositional empathy on emotional reactions and helping: A multidimensional approach. Journal of Personality, 51(2), 167–184. [Google Scholar]
- Dekker MC, Ferdinand RF, Van Lang ND, Bongers IL, Van Der Ende J, & Verhulst FC (2007). Developmental trajectories of depressive symptoms from early childhood to late adolescence: gender differences and adult outcome. Journal of Child Psychology and Psychiatry, 48(7), 657–666. [DOI] [PubMed] [Google Scholar]
- Demers LA, & Koven NS (2015). The relation of alexithymic traits to affective theory of mind. The American Journal of Psychology, 128(1), 31–42. [DOI] [PubMed] [Google Scholar]
- Disner SG, Beevers CG, Haigh EA, & Beck AT (2011). Neural mechanisms of the cognitive model of depression. Nature Reviews Neuroscience, 12(8), 467–477. [DOI] [PubMed] [Google Scholar]
- Duval S, & Tweedie R (2000). Trim and fill: a simple funnel‐plot–based method of testing and adjusting for publication bias in meta‐analysis. Biometrics, 56(2), 455–463. [DOI] [PubMed] [Google Scholar]
- Dvash J, & Shamay-Tsoory SG (2014). Theory of mind and empathy as multidimensional constructs: Neurological foundations. Topics in Language Disorders, 34(4), 282–295. [Google Scholar]
- Dziobek I, Fleck S, Kalbe E, Rogers K, Hassenstab J, Brand M, … & Convit A (2006). Introducing MASC: a movie for the assessment of social cognition. Journal of Autism and Developmental Disorders, 36(5), 623–636. [DOI] [PubMed] [Google Scholar]
- Egger M, Smith GD, Schneider M, & Minder C (1997). Bias in meta-analysis detected by a simple, graphical test. British Medical Journal, 315(7109), 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellement B, Jasaui Y, Kathol K, Nosratmirshekarlou E, Pringsheim T, Sarna J, … & Martino D (2021). Social cognition in cervical dystonia: phenotype and relationship to anxiety and depression. European Journal of Neurology, 28(1), 98–107. [DOI] [PubMed] [Google Scholar]
- Eslinger PJ (1998). Neurological and neuropsychological bases of empathy. European Neurology, 39(4), 193–199. [DOI] [PubMed] [Google Scholar]
- Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, Murray CJ, Vos T, & Whiteford HA (2013). Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Medicine, 10(11), e1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JB (1995). Structured clinical interview for DSM-IV axis I disorders-patient edition (SCID-I/P, Version 2.0) New York: Biometrics Research Department, New York State Psychiatric Institute, 722. [Google Scholar]
- Flavell JH, Botkin P, Fry C, Wright J, & Jarvis P (1968). The development of role-taking and communications skills in children (Vol. 10). New York: Wiley. [Google Scholar]
- Fletcher‐Watson S, McConnell F, Manola E, & McConachie H (2014). Interventions based on the Theory of Mind cognitive model for autism spectrum disorder (ASD). Cochrane Database of Systematic Reviews, (3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fonagy P, Luyten P, Moulton-Perkins A, Lee YW, Warren F, Howard S, … & Lowyck B (2016). Development and validation of a self-report measure of mentalizing: The Reflective Functioning Questionnaire. PLoS One 11(7): e0158678. 10.1371/journal.pone.0158678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber J (2018). Social cognitive training to enhance the efficacy of CBT for depression in youth: A developmental approach National Institute of Mental Health. NIH/NIMH 1R61MH115125. [Google Scholar]
- Gilbert P, & Miles JN (2000). Sensitivity to Social Put-Down: it’s relationship to perceptions of social rank, shame, social anxiety, depression, anger and self-other blame. Personality and Individual Differences, 29(4), 757–774. [Google Scholar]
- Hamilton M (1986). The Hamilton rating scale for depression. In Assessment of Depression (pp. 143–152). Springer, Berlin, Heidelberg. [Google Scholar]
- Happé FG (1994). An advanced test of theory of mind: Understanding of story characters’ thoughts and feelings by able autistic, mentally handicapped, and normal children and adults. Journal of Autism and Developmental Disorders, 24(2), 129–154. [DOI] [PubMed] [Google Scholar]
- Happé F, Cook JL, & Bird G (2017). The structure of social cognition: In (ter) dependence of socio-cognitive processes. Annual Review of Psychology, 68, 243–267. [DOI] [PubMed] [Google Scholar]
- Harkness K, Sabbagh M, Jacobson J, Chowdrey N, & Chen T (2005). Enhanced accuracy of mental state decoding in dysphoric college students. Cognition & Emotion, 19(7), 999–1025. [Google Scholar]
- Harkness KL, Jacobson JA, Duong D, & Sabbagh MA (2010). Mental state decoding in past major depression: Effect of sad versus happy mood induction. Cognition and Emotion, 24(3), 497–513. [Google Scholar]
- Harkness KL, Washburn D, Theriault JE, Lee L, & Sabbagh MA (2011). Maternal history of depression is associated with enhanced theory of mind in depressed and nondepressed adult women. Psychiatry Research, 189(1), 91–96. [DOI] [PubMed] [Google Scholar]
- Harkness KL, Jacobson JA, Sinclair B, Chan E, & Sabbagh MA (2012). For love or money? What motivates people to know the minds of others? Cognition & Emotion, 26(3), 541–549. [DOI] [PubMed] [Google Scholar]
- Hawton K, I Comabella CC, Haw C, & Saunders K (2013). Risk factors for suicide in individuals with depression: a systematic review. Journal of Affective Disorders, 147(1–3), 17–28. [DOI] [PubMed] [Google Scholar]
- Hentze C, Walter H, Schramm E, Drost S, Schoepf D, Fangmeier T, … & Schnell K (2016). Functional correlates of childhood maltreatment and symptom severity during affective theory of mind tasks in chronic depression. Psychiatry Research: Neuroimaging, 250, 1–11. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Carpenter JK, & Curtiss J (2016). Interpersonal emotion regulation questionnaire (IERQ): Scale development and psychometric characteristics. Cognitive Therapy and Research, 40(3), 341–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Doan SN, Sprung M, Wilson A, Ebesutani C, Andrews LA, … & Harris PL (2016). Training children’s theory-of-mind: A meta-analysis of controlled studies. Cognition, 150, 200–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingram RE (1990). Self-focused attention in clinical disorders: review and a conceptual model. Psychological Bulletin, 107(2), 156. [DOI] [PubMed] [Google Scholar]
- Inoue Y, Tonooka Y, Yamada K, & Kanba S (2004). Deficiency of theory of mind in patients with remitted mood disorder. Journal of Affective Disorders, 82(3), 403–409. [DOI] [PubMed] [Google Scholar]
- Inoue Y, Yamada K, Kanba S (2006). Deficit in theory of mind is a risk for relapse of major depression. Journal of Affective Disorders, 95, 125–127. [DOI] [PubMed] [Google Scholar]
- Kerestes R, Davey CG, Stephanou K, Whittle S, & Harrison BJ (2014). Functional brain imaging studies of youth depression: a systematic review. NeuroImage: Clinical, 4, 209–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessels RP, Waanders‐Oude Elferink M, & van Tilborg I (2020). Social cognition and social functioning in patients with amnestic mild cognitive impairment or Alzheimer’s dementia. Journal of Neuropsychology [DOI] [PMC free article] [PubMed]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. [DOI] [PubMed] [Google Scholar]
- Kettle JW, O’Brien-Simpson L, & Allen NB (2008). Impaired theory of mind in first-episode schizophrenia: comparison with community, university and depressed controls. Schizophrenia Research, 99(1–3), 96–102. [DOI] [PubMed] [Google Scholar]
- Kiliç F, Demirdas A, Isik Ü, Akkus M, Atay IM, & Kuzugüdenlioglu D (2020). Empathy, Alexithymia, and Theory of Mind in Borderline Personality Disorder. The Journal of Nervous and Mental Disease, 208(9), 736–741. [DOI] [PubMed] [Google Scholar]
- Kilincel Ş, Vural AP, & Kilincel O (2020). Theory of mind deficit in adolescents with major depressive disorder. Anatolian Journal of Psychiatry/Anadolu Psikiyatri Dergisi, 21(2). [Google Scholar]
- Kovacs M (1992). Children’s depression inventory North Tonawanda, NY: Multi-Health Systems. [Google Scholar]
- Ladegaard N, Larsen ER, Videbech P, & Lysaker PH (2014). Higher-order social cognition in first-episode major depression. Psychiatry Research, 216(1), 37–43. [DOI] [PubMed] [Google Scholar]
- Ladegaard N, Videbech P, Lysaker PH, & Larsen ER (2016). The course of social cognitive and metacognitive ability in depression: Deficit are only partially normalized after full remission of first episode major depression. British Journal of Clinical Psychology, 55(3), 269–286. [DOI] [PubMed] [Google Scholar]
- Lannoy S, Gilles F, Benzerouk F, Henry A, Oker A, Raucher-Chéné D, … & Gierski F (2020). Disentangling the role of social cognition processes at early steps of alcohol abuse: The influence of affective theory of mind. Addictive Behaviors, 102, 106187. [DOI] [PubMed] [Google Scholar]
- Lee L, Harkness KL, Sabbagh MA, & Jacobson JA (2005). Mental state decoding abilities in clinical depression. Journal of Affective Disorders, 86(2–3), 247–258. [DOI] [PubMed] [Google Scholar]
- Lee S, Jacobsen EP, Jia Y, Snitz BE, Chang CCH, & Ganguli M (2020). Reading the Mind in the Eyes: A Population-Based Study of Social Cognition in Older Adults. The American Journal of Geriatric Psychiatry, S1064–7481. [DOI] [PMC free article] [PubMed]
- Leslie AM (1987). Pretense and representation: The origins of “theory of mind.” Psychological Review, 94(4), 412. [Google Scholar]
- Lovibond PF, & Lovibond SH (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33(3), 335343. [DOI] [PubMed] [Google Scholar]
- Lysaker PH, Carcione A, Dimaggio G, Johannesen JK, Nicolò G, Procacci M, & Semerari A (2005). Metacognition amidst narratives of self and illness in schizophrenia: associations with neurocognition, symptoms, insight and quality of life. Acta Psychiatrica Scandinavica, 112(1), 64–71. [DOI] [PubMed] [Google Scholar]
- Maleki G, Zabihzadeh A, Richman MJ, Demetrovics Z, & Mohammadnejad F (2020). Decoding and reasoning mental states in major depression and social anxiety disorder. BMC psychiatry, 20(1), 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manstead AS, Dosmukhambetova D, Shearn J, & Clifton A (2013). The influence of dysphoria and depression on mental state decoding. Journal of Social and Clinical Psychology, 32(1), 116–133. [Google Scholar]
- Mathersul D, McDonald S, & Rushby JA (2013). Understanding advanced theory of mind and empathy in high-functioning adults with autism spectrum disorder. Journal of Clinical and Experimental Neuropsychology, 35(6), 655–668. [DOI] [PubMed] [Google Scholar]
- Mattern M, Walter H, Hentze C, Schramm E, Drost S, Schoepf D, … & Schnell K (2015). Behavioral evidence for an impairment of affective theory of mind capabilities in chronic depression. Psychopathology, 48(4), 240–250. [DOI] [PubMed] [Google Scholar]
- McDonald S, Flanagan S, Rollins J, & Kinch J (2003). TASIT: A new clinical tool for assessing social perception after traumatic brain injury. The Journal of Head Trauma Rehabilitation, 18(3), 219–238. [DOI] [PubMed] [Google Scholar]
- McNair DM, Loor M, & Droppleman LF (1981). Profile of mood states San Diego, CA: Educational and Industrial Testing Service. [Google Scholar]
- Meinhardt‐Injac B, Daum MM, & Meinhardt G (2020). Theory of mind development from adolescence to adulthood: Testing the two‐component model. British Journal of Developmental Psychology [DOI] [PubMed]
- Mellick W, & Sharp C (2016). Mental state decoding in adolescent boys with major depressive disorder versus sex-matched healthy controls. Psychopathology, 49(1), 53–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, & Altman DG (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of Internal Medicine, 151(4), 264–269. [DOI] [PubMed] [Google Scholar]
- Monteleone AM, Corsi E, Cascino G, Ruzzi V, Ricca V, Ashworth R, … & Cardi V (2020). The Interaction Between Mentalizing, Empathy and Symptoms in People with Eating Disorders: A Network Analysis Integrating Experimentally Induced and Self-report Measures. Cognitive Therapy and Research, 44(6), 1140–1149. [Google Scholar]
- Montgomery SA, & Åsberg MARIE (1979). A new depression scale designed to be sensitive to change. The British Journal of Psychiatry, 134(4), 382–389. [DOI] [PubMed] [Google Scholar]
- Moore C, Bosacki SL, & Macgillivray S (2011). Theory of mind and social interest in zero‐ acquaintance play situations. Child Development, 82(4), 1163–1172. [DOI] [PubMed] [Google Scholar]
- Mor N, & Winquist J (2002). Self-focused attention and negative affect: a meta-analysis. Psychological Bulletin, 128(4), 638. [DOI] [PubMed] [Google Scholar]
- Muris P, Steerneman P, Meesters C, Merckelbach H, Horselenberg R, van den Hogen T, & van Dongen L (1999). The TOM test: A new instrument for assessing theory of mind in normal children and children with pervasive developmental disorders. Journal of Autism and Developmental Disorders, 29(1), 67–80. [DOI] [PubMed] [Google Scholar]
- Murphy BA, & Lilienfeld SO (2019). Are self-report cognitive empathy ratings valid proxies for cognitive empathy ability? Negligible meta-analytic relations with behavioral task performance. Psychological Assessment, 31(8), 1062. [DOI] [PubMed] [Google Scholar]
- Nejati V, Zabihzadeh A, Maleki G, & Tehranchi A (2012). Mind reading and mindfulness deficits in patients with major depression disorder. Procedia-Social and Behavioral Sciences, 32, 431–437. [Google Scholar]
- Onishi KH, & Baillargeon R (2005). Do 15-month-old infants understand false beliefs?. Science, 308(5719), 255–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poletti M, Sonnoli A, & Bonuccelli U (2014). Mild depressive symptoms are associated with enhanced affective theory of mind in nonclinical adult women. Journal of Neuropsychiatry and Clinical Neurosciences, 26(2), E63–E64. [DOI] [PubMed] [Google Scholar]
- Pons F, Harris PL, & de Rosnay M (2004). Emotion comprehension between 3 and 11 years: Developmental periods and hierarchical organization. European Journal of Developmental Psychology, 1(2), 127–152. [Google Scholar]
- Porcelli S, Van Der Wee N, van der Werff S, Aghajani M, Glennon JC, van Heukelum S, … & Posadas M (2019). Social brain, social dysfunction and social withdrawal. Neuroscience & Biobehavioral Reviews, 97, 10–33. [DOI] [PubMed] [Google Scholar]
- Premack D, & Woodruff G (1978). Does the chimpanzee have a theory of mind? Behavior and Brain Science, 1, 515–526. [Google Scholar]
- Purcell AL, Phillips M, & Gruber J (2013). In your eyes: does theory of mind predict impaired life functioning in bipolar disorder? Journal of Affective Disorders, 151 (3), 1113–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. [Google Scholar]
- Raes F, Hermans D, & Williams JMG (2006). Negative bias in the perception of others’ facial emotional expressions in major depression: The role of depressive rumination. The Journal of Nervous and Mental Disease, 194(10), 796–799. [DOI] [PubMed] [Google Scholar]
- Rosi A, Cavallini E, Bottiroli S, Bianco F, & Lecce S (2016). Promoting theory of mind in older adults: does age play a role?. Aging & Mental Health, 20(1), 22–28. [DOI] [PubMed] [Google Scholar]
- Richman MJ, & Unoka Z (2015). Mental state decoding impairment in major depression and borderline personality disorder: meta-analysis. The British Journal of Psychiatry, 207(6), 483–489. [DOI] [PubMed] [Google Scholar]
- Rothschild-Yakar L, Stein D, Goshen D, Shoval G, Yacobi A, Eger G, … & Gur E (2019). Mentalizing Self and Other and Affect Regulation Patterns in Anorexia and Depression. Frontiers in Psychology, 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, … & Thase ME (2003). The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biological Psychiatry, 54(5), 573–583. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Gullion CM, Basco MR, Jarrett RB, & Trivedi MH (1996). The inventory of depressive symptomatology (IDS): psychometric properties. Psychological Medicine, 26(3), 477–486. [DOI] [PubMed] [Google Scholar]
- Sabbagh MA (2004). Understanding orbitofrontal contributions to theory-of-mind reasoning: implications for autism. Brain and Cognition, 55(1), 209–219. [DOI] [PubMed] [Google Scholar]
- Sabbagh MA, & Bowman LC (2018). Theory of mind. Stevens’ Handbook of Experimental Psychology and Cognitive Neuroscience, 4, 1–39. [Google Scholar]
- Samson AC, Lackner HK, Weiss EM, & Papousek I (2012). Perception of other people’s mental states affects humor in social anxiety. Journal of Behavior Therapy and Experimental Psychiatry, 43(1), 625–631. [DOI] [PubMed] [Google Scholar]
- Sarfati Y, Hardy-Baylé MC, Brunet E, & Widlöcher D (1999). Investigating theory of mind in schizophrenia: influence of verbalization in disorganized and non-disorganized patients. Schizophrenia Research, 37(2), 183–190. [DOI] [PubMed] [Google Scholar]
- Scaini S, Caputi M, Ogliari A, & Oppo A (2020). The Relationship Among Attributional Style, Mentalization, and Five Anxiety Phenotypes in School-Age Children. Journal of Research in Childhood Education, 34(4), 551–565. [Google Scholar]
- Sebastian CL, Fontaine NM, Bird G, Blakemore SJ, De Brito SA, McCrory EJ, & Viding E (2011). Neural processing associated with cognitive and affective Theory of Mind in adolescents and adults. Social Cognitive and Affective Neuroscience, 7(1), 53–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, & Schwab-Stone ME (2000). NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry, 39(1), 28–38. [DOI] [PubMed] [Google Scholar]
- Shamay-Tsoory SG, & Aharon-Peretz J (2007). Dissociable prefrontal networks for cognitive and affective theory of mind: a lesion study. Neuropsychologia, 45(13), 3054–3067. [DOI] [PubMed] [Google Scholar]
- Shamay-Tsoory SG, Harari H, Aharon-Peretz J, & Levkovitz Y (2010). The role of the orbitofrontal cortex in affective theory of mind deficits in criminal offenders with psychopathic tendencies. Cortex, 46(5), 668–677. [DOI] [PubMed] [Google Scholar]
- Sheikh JI, & Yesavage JA (1986). Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clinical Gerontologist: The Journal of Aging and Mental Health
- Simon M, Németh N, Gálber M, Lakner E, Csernela E, Tényi T, & Czéh B (2019). Childhood adversity impairs theory of mind abilities in adult patients with major depressive disorder. Frontiers in Psychiatry, 10, 867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snaith RP (2003). The hospital anxiety and depression scale. Health and Quality of Life Outcomes, 1(1), 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR (2013). Major depressive disorder is associated with broad impairments on neuropsychological measures of executive function: a meta-analysis and review. Psychological Bulletin, 139(1), 81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprong M, Schothorst P, Vos E, Hox J, & Van Engeland H (2007). Theory of mind in schizophrenia: meta-analysis. The British Journal of Psychiatry, 191(1), 5–13. [DOI] [PubMed] [Google Scholar]
- Steinberg L, & Morris AS (2001). Adolescent development. Annual Review of Psychology, 52(1), 83–110. [DOI] [PubMed] [Google Scholar]
- Stuss DT, Gallup GG Jr, & Alexander MP (2001). The frontal lobes are necessary for theory of mind’. Brain, 124(2), 279–286. [DOI] [PubMed] [Google Scholar]
- Sullivan K, & Winner E (1993). Three-year-olds′ understanding of mental states: The influence of trickery. Journal of experimental child psychology, 56(2), 135–148. [DOI] [PubMed] [Google Scholar]
- Sullivan K, Zaitchik D, & Tager-Flusberg H (1994). Preschoolers can attribute second-order beliefs. Developmental Psychology, 30(3), 395. [Google Scholar]
- Swendsen JD, & Merikangas KR (2000). The comorbidity of depression and substance use disorders. Clinical Psychology Review, 20(2), 173–189. [DOI] [PubMed] [Google Scholar]
- Szanto K, Dombrovski AY, Sahakian BJ, Mulsant BH, Houck PR, Reynolds CF III, & Clark L (2012). Social emotion recognition, social functioning, and attempted suicide in late-life depression. The American Journal of Geriatric Psychiatry, 20(3), 257–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szily E, & Kéri S (2009). Anomalous subjective experience and psychosis risk in young depressed patients. Psychopathology, 42(4), 229–235. [DOI] [PubMed] [Google Scholar]
- Thoma P, Schmidt T, Juckel G, Norra C, & Suchan B (2015). Nice or effective? Social problem solving strategies in patients with major depressive disorder. Psychiatry Research, 228(3), 835–842. [DOI] [PubMed] [Google Scholar]
- Uekermann J, Channon S, Lehmkämper C, Abdel-Hamid M, Vollmoeller W, & Daum I (2008). Executive function, mentalizing and humor in major depression. Journal of the International Neuropsychological society, 14(1), 55–62. [DOI] [PubMed] [Google Scholar]
- Wang YG, Wang YQ, Chen SL, Zhu CY, & Wang K (2008). Theory of mind disability in major depression with or without psychotic symptoms: a componential view. Psychiatry Research, 161(2), 153–161. [DOI] [PubMed] [Google Scholar]
- Washburn D, Wilson G, Roes M, Rnic K, & Harkness KL (2016). Theory of mind in social anxiety disorder, depression, and comorbid conditions. Journal of Anxiety Disorders, 37, 71–77. [DOI] [PubMed] [Google Scholar]
- Weary G, & Edwards JA (1994). Social cognition and clinical psychology: Anxiety, depression, and the processing of social information. In Wyer RS Jr. & Srull TK (Eds.) Handbook of social cognition (pp. 289–338). Hillsdale, NJ: Erlbaum. [Google Scholar]
- Weightman MJ, Air TM, & Baune BT (2014). A review of the role of social cognition in major depressive disorder. Frontiers in Psychiatry, 5, 179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells KB, Stewart A, Hays RD, Burnam MA, Rogers W, Daniels M, … & Ware J (1989). The functioning and well-being of depressed patients: results from the Medical Outcomes Study. Journal of the American Medical Association, 262(7), 914–919. [PubMed] [Google Scholar]
- Wilbertz G, Brakemeier EL, Zobel I, Härter M, & Schramm E (2010). Exploring preoperational features in chronic depression. Journal of Affective Disorders, 124(3), 262–269. [DOI] [PubMed] [Google Scholar]
- Wimmer H, & Perner J (1983). Beliefs about beliefs: Representation and constraining function of wrong beliefs in young children’s understanding of deception. Cognition, 13(1), 103–128. [DOI] [PubMed] [Google Scholar]
- Wolkenstein L, Schönenberg M, Schirm E, & Hautzinger M (2011). I can see what you feel, but I can’t deal with it: Impaired theory of mind in depression. Journal of Affective Disorders, 132(1–2), 104–111. [DOI] [PubMed] [Google Scholar]
- Zahavi AY, Sabbagh MA, Washburn D, Mazurka R, Bagby RM, Strauss J, … & Harkness KL (2016). Serotonin and dopamine gene variation and theory of mind decoding accuracy in major depression: A preliminary investigation. PloS One, 11(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zlotnick C, Kohn R, Keitner G, & Della Grotta SA (2000). The relationship between quality of interpersonal relationships and major depressive disorder: findings from the National Comorbidity Survey. Journal of Affective Disorders, 59(3), 205–215. [DOI] [PubMed] [Google Scholar]
- Zobel I, Werden D, Linster H, Dykierek P, Drieling T, Berger M, & Schramm E (2010). Theory of mind deficits in chronically depressed patients. Depression and Anxiety, 27(9), 821–828. [DOI] [PubMed] [Google Scholar]
- Zwick JC, & Wolkenstein L (2017). Facial emotion recognition, theory of mind and the role of facial mimicry in depression. Journal of Affective Disorders, 210, 90–99. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


