Abstract
Environmental health research can be oriented across a continuum of effects ranging from adverse to cobenefits to salutogenic. We argue that the salutogenic end of the continuum is insufficiently represented in research and as a basis for environmental protection, even though there is growing evidence that the natural environment plays a critical role in blunting adverse effects and promoting human health and well-being. Thus, we advocate for advancing environmental health research through environmental epidemiology that more fully and directly accounts for the salutogenic effects of the natural environment on individual well-being by (1) defining “natural environments” broadly, from pristine natural areas to urban green infrastructure; (2) considering exposure comprehensively to encompass residential, occupational, and recreational settings, local and distant, day-to-day and occasional; (3) doing individual-level assessments that include both health and well-being outcomes and one’s experience of nature, including potential mediation by connectedness to nature and individual perceptions and preferences, as well as sociocultural and demographic effect modifiers; and (4) collecting longitudinal and nationally representative data.
Graphical Abstract
We can only be healthy if the environment in which we live is also healthy.
Jerald L. Schnoor, Environmental Science & Technology, July 13 2011
As recognized in the above quote, our health and the environment are intertwined. Still, this relationship is most often viewed from a perspective of the adverse health effects resulting from contaminants in the environment. Although we recognize “healthy” as more than the absence of disease, our understanding of the benefits of the natural environment to human health and well-being is not nearly as developed. However, this has begun to change. The natural environment as a “salutogenic context” is increasingly recognized as crucial to our physical and mental health and to our subjective well-being.1 Since 2010, ES&T has published several papers on the benefits of exposure to nearby natural environments and on “green exercise” (e.g., refs 2–7). There is a strong rationale for environmental health research to consider salutary factors associated with exposure to natural environments, as has been championed by H. Frumkin and others (e.g., refs 2 and 8–14).
In the late 20th century, A. Antonovsky introduced the salutogenic model to provide a theoretical foundation for health promotion as envisioned in the World Health Organization charter, which states that “Health is a state of optimal physical, mental and social well-being, and not merely the absence of disease and infirmity.” Thus, instead of solely a “pathogenic orientation” (keeping risk factors for disease low), health promotion should have a “salutogenic orientation” (actively promote health by focusing on salutogenesis—the origins of health—and the enhancement of salutary or health-promoting factors).15 The natural environment is one of the external conditions (together with the built, sociocultural, and institutional environments) that influence individual well-being, along with personal attributes, such as genetics and personality traits, past experiences, education and skills, etc.
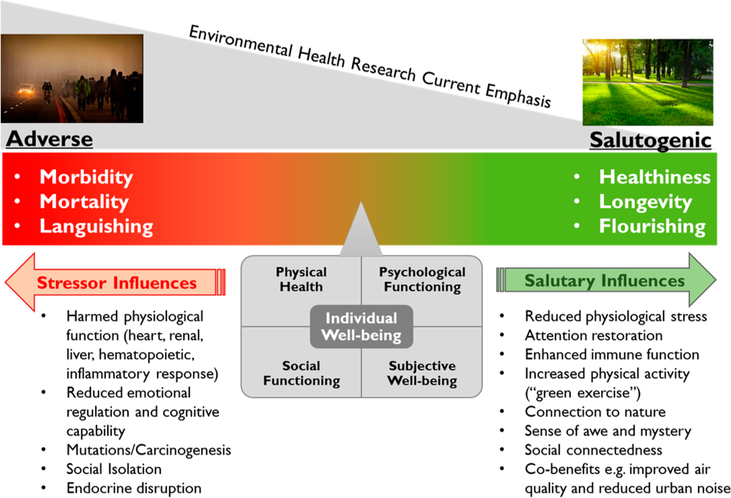
The influence of the environment on human health and well-being can be viewed over a continuum (Figure 1). On the adverse side of the continuum, the focus is on how physical, chemical, or biological contaminants are associated with, contribute to, or cause disease, morbidity, and mortality. On the salutogenic end of the continuum, environmental salutary influences are not only associated with the absence of disease but contribute to improved health, happiness, vitality, sense of purpose, and satisfaction with life. In the context of mental health, Keys termed this continuum from languishing to flourishing.16 Although the tradition of environmental health sciences and current research is more heavily oriented toward harmful agents and adverse effects, there is growing interest in the salutogenic end of the continuum. These salutary influences range from mitigation of environmental contaminants (e.g., roadside vegetative barriers reducing traffic noise and airborne particles), which translates into health cobenefits, extending to providing beneficial experiences (e.g., increased physical activity and social contact) that lead to improved well-being. Our focus here relates to the latter, recognizing that in the environmental health literature, the salutogenic influence of the environment, beyond cobenefits, is relatively understudied with respect to disease prevention (e.g., enhanced cardiovascular and immune function) or improved well-being (e.g., happiness) (ref 12 and references therein).
Figure 1.
Continuum of environmental health research: from adverse to salutogenic. The green arrow depicts the influence of salutary factors that pull individual well-being toward the salutogenic outcomes, while the red arrow depicts the influence of environmental stressors that pull individual well-being toward adverse outcomes. Developed from refs 12 and 13.
Available evidence suggests that the positive influence of the natural environment on human well-being occurs through different pathways: environmental psychology, enhanced immune function, promotion of healthy behaviors, and improvement of environmental quality.12 Within the first pathway, environmental psychology, two main theories describe the restorative effects of exposure to natural environments (e.g., refs 17–19): stress reduction theory (SRT20), focused on improved emotional and physiological responses to life stressors, and attention restoration theory (ART21), centered on refocused attention and improved cognition resulting from contact with nature. A third theory (preferences for nature) leans on the biophilia hypothesis,22 which claims that all human beings experience a love for nature and feelings of awe and mystery in the presence of nature, and suggests that the benefits derived from exposure to natural environments and the effect of sense of belonging on subjective well-being (SWB) may be mediated by different degrees of “nature-relatedness”23 or “connectedness to nature”,24 that is, “the extent to which an individual includes nature within his/her cognitive representation of self”.25 The second pathway, enhanced immune function, has been proposed to play a central role on the nature-health relationship, since it may underlie many beneficial effects on health and well-being that have been found.26 The third pathway involves the positive effects of natural environments on healthy behaviors—increases in both physical activity, including green exercise,4,27 and social interaction (e.g., ref 28 and 29)—which are supported by existing research, although several factors, including urban sprawl, lifestyle, and perceived safety, influence those effects and results are mixed across studies.2,4,11,30–33 Finally, the presence of natural elements translates into benefits to environmental quality, which reflect positively on individual well-being (e.g., ref 12); notably, there are cobenefits associated with improved air quality, heat and humidity regulation, stormwater management, noise reduction, and biodiversity, although the role of the latter is not yet conclusive.34 Through these interactive pathways, exposure to natural environments can lead to enhanced individual well-being and increased social cohesion. There is evidence of benefits for physical health and physiological markers of mental health,19,33,35,36 psychological and social functioning,2,18,19,33,37 and SWB19,38,39 from everyday exposure to natural environments. Additionally, since Ulrich’s seminal work on the role of views of nature to help patient recovery,40 a number of studies have focused on providing natural environments in health care settings to improve health outcomes and reduce healthcare costs (e.g., refs 41 and 42). The evidence described above predominantly comes from developed countries so relevance to populations in developing countries is unclear.13
Although in many ways this evidence is extensive and compelling, there are some important limitations. A few very recent review studies (e.g., refs 12–14) examine methodological issues and a broad range of outcomes, providing comprehensive summaries of the state of the science and critical research needs and priorities. Thus, we do not present a systematic review of the literature but rather a brief overview of the existing body of knowledge and research gaps, taking into account the above-mentioned broad scope reviews and additional focused reviews. Our goal is to provide context and suggest strategies for advancing environmental epidemiology research oriented toward the salutogenic influence of the natural environment on human well-being. Specifically, building on Frumkin and colleagues,12 we advocate for using multidimensional measurements in nationwide population surveys and longitudinal studies to capture both objective and subjective factors that may influence the benefits derived from exposure to natural environments, at the individual level. We recognize that there are established drivers of environmental health research including such considerations as funding sources, regulation, and established study sections. However, it is outside the scope of this paper to discuss the drivers of research focus along the continuum of environmental health research (Figure 1).
MEASURING EXPOSURE
Defining Natural Environments.
Clearly defining natural environments is critical to measuring exposure and well-being effects.11 A wide range of definitions have been reported and often “green space” (e.g., ref 33) and “blue space” (e.g., refs 43 and 44) are considered separately. We suggest the adoption of a broad definition of “natural environments” that encompasses one’s every day experience.4,18,45,46 This definition includes any outdoor spaces that retain noticeable elements of nature, ranging from pristine or seminatural areas to urban green or blue spaces, including green infrastructure. Thus, natural environments represent a spectrum of spaces: not only national/state parks, wildlife parks, forests and wetlands but also beaches and the coast, farmland, rangeland, reservoirs, ponds, rivers, lakes, and creeks, as well as golf courses, urban parks, community gardens, tree-lined streets, lawns and backyards, and roof gardens. The goal is to capture the full range of human exposure to outdoor nature both by using this broader definition and by accounting for individual differences in “experience of nature” and the subjective factors that determine them, as detailed next.
Characterizing Exposure to Natural Environments at the Individual Level.
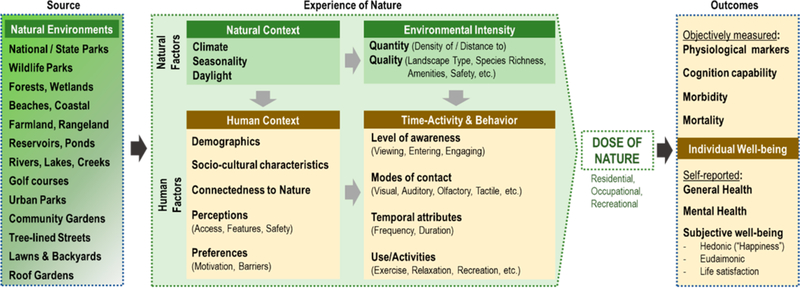
Exposure to natural environments is often defined as the distance to the nearest green or blue space or as the density of greenness in the neighborhood.46 Given the influence that subjective factors may have on the benefits derived from “exposure to” natural environments, we argue that this should be framed as “experience of” natural environments or “experience of nature”, following the early work of Kaplan and Kaplan47 and subsequent research (e.g., ref 18). Although the natural environment has an objective impact on human beings related to the provision of life-supporting “essential ecosystem services (water, air, food, and biodiversity)”,48 there are additional effects dependent on subjective factors, including individual behavior and social context.11,13,18 Thus, when measuring “exposure” there is a need to go beyond the presence of natural environments in the immediate surroundings (e.g., neighborhood greenness, distance to the nearest park or beach) or distant locations (e.g., wilderness areas, tropical forest, etc.). These measurements ignore one’s experience of nature and provide an incomplete assessment of exposure at the individual level (e.g., refs 11–13, 18, 28, 49, and 50). Additional natural and human factors determine “dose” of nature51 and may impact health and well-being outcomes differently (Figure 2).
Figure 2.
Experience of nature (e.g., refs 18 and 47) and individual well-being: Grounding the benefits of natural environments to individual wellbeing on exposure science52 and the concept of dose of nature.51
As noted by Shanahan et al.51 and consistent with the National Research Council’s exposure science report,52 when estimating dose of nature, environmental intensity (or nature intensity) is considered by accounting for quantity (density of/distance to) and quality (landscape type, species richness, amenities, safety, etc.) of natural environments present in each individual’s life. In parallel, time-activity and behavior factors also determine dose of nature:12,13,49–51 (a) level of awareness of nature, which ranges from viewing natural environments through a window or media (e.g., book, video, etc.) or experiencing them through virtual reality, entering nature (e.g., walk in an urban park), or engaging with nature (e.g., observing wildlife, gardening, hiking in a nature trail, etc.); (b) modes of contact (visual, auditory, olfactory, tactile, etc.); (c) temporal attributes (frequency, duration); and (d) uses or types of activities conducted in natural environments, such as exercise, relaxation, recreation (e.g., fishing, hunting, wildlife viewing, social contact, etc.). Moreover, natural context (e.g., climate, seasonality, daylight) and human context (see Assessing the Influence of Individual-Level Factors on Well-Being section) may modify our experience of nature. Also, exposure metrics should be standardized to facilitate comparison of results across studies,32,53 although this presents a number of challenges, including specific focus of different disciplines.54 Finally, to fully characterize total exposure, not only residential metrics but also measurements of exposure in occupational (school, work) and recreational settings (local and distant) need to be considered,13 as well as exposure through the life course.54–57
Measuring Outcome: Individual Well-Being.
Individual well-being is defined to include physical health, psychological and social functioning, and SWB. By definition, SWB which “refers to how people experience and evaluate their lives and specific domains and activities in their lives”58 is the most elusive dimension of individual well-being. Several authors identify SWB as “happiness” and restrict it to its hedonic (emotional) aspects, that is, the presence of positive affect and absence of negative affect. Other authors use broader definitions that include not only happiness but also eudaimonic components related with meaningfulness, vitality, and growth, as well as satisfaction with life. It should be noted that SWB itself contributes to health and longevity and, at the societal level, the size of this contribution is considerable.59
Although some components of individual well-being can be assessed by objective measures (physical health, physiological markers of mental health, and psychological functioning), the subjective component requires the use of subjective measures.60 Self-reported health has been shown to have a strong association with objective measures of overall health,61 and it is a “strong predictor of mortality”.62 In the context of the U.S. Department of Health and Human Services’ Healthy People 2020 initiative (https://www.healthypeople.gov/2020/topics-objectives/topic/health-related-quality-of-life-well-being), health-related quality of life was included in the 2010 U.S. National Health Interview Survey and is planned to be measured every five years using the 10-item PROMIS Global Health Scale.63,64 Also, in spite of the inherent difficulty in quantifying subjective factors, there are a number of well-validated scales that focus on or include SWB, such as WHO-5 Well-being Index (65 and references therein), GHQ-12,66 and the 5-item Satisfaction with Life Scale.67,68 Additionally, the Third European Quality of Life Survey included questions that directly assess all dimensions of SWB and were synthesized into three overall measures: WHO-5 Mental Well-Being Index, Hedonic Well-being Index and Overall [Subjective] Well-being Index.69 Finally, the International Well-being Group developed the Personal Wellbeing Index (PWI), which measures satisfaction with life in eight domains.70
Notwithstanding the focus in this article on positive effects, we acknowledge that exposure to natural environments, particularly when we enter or engage with them, can lead to adverse effects on individual well-being because of perceived (biophobia) or real threats from different natural elements (e.g., wild animal attacks, mosquito and tick bites, plant allergens, etc.), as well as perceived or real lack of safety in some spaces (refs 18 and 48 and references therein). There can also be a complicating interplay between the adverse and salutogenic effects. For example, the beneficial effects of physical activity enabled by natural environments can have adverse lung function effects if the environment is also polluted.71
Assessing the Influence of Individual-Level Factors on Well-Being.
The effect of exposure to natural environments on human health and well-being may be influenced by personal and cultural factors. Specifically, the impact of the natural environment on SWB is affected by individual-level factors, both objective—age and gender, socioeconomic status, race/ethnicity, and sociocultural characteristics—and subjective. Subjective factors related to exposure to natural environments include connectedness to nature, personal preferences associated with personality traits, past experiences, and sociocultural context, which influence the motivation and barriers for exposure, as well as individual perception of access, features, and safety of natural environments.11–13,31,38,39,49,72–74 Both subjective and objective individual-level data will enable investigation of environmental justice considerations that are likely to be significant,73,75,76 as has been well established on the adverse end of the environmental health continuum. A survey instrument is an appropriate tool to acquire data on self-reported health and SWB and on individual-level factors underlying human exposure to the environment.
A few large national surveys have evaluated subjective well-being, for example Gallup World Poll77 and the Third European Quality of Life Survey.69 However, these surveys lack information about one’s experience of nature. Conversely, large population surveys on experience of nature, like UK’s Monitoring Engagement with the Natural Environment (MENE),78 have only occasionally included questions on SWB.79 Accordingly, only very limited analysis of individual level influence of exposure to natural environments has been possible at a large scale. Research that has been done at an individual level has been dominated by experimental and small observational studies.4 Several large observational studies have been conducted, particularly in the UK, northern Europe and Australia, but focused on single aspects of individual well-being (e.g., physical activity, stress, etc.). This is also the case for the US, where, to the best of our knowledge, except for ref 80 (focused on women aged 35–74, physical activity, and obesity), studies have not included nationwide representative samples or have been limited by spatial misalignment or aggregation of measures of the natural environment (e.g., sleep81), which may lead to ecological fallacy. Therefore, the magnitude of any positive effects, as well as the mediators and modifiers that influence the association between exposure to natural environments and individual well-being, need to be better characterized, measured, and analyzed (e.g., refs 2, 11–13, 19, 31, 49, 56, and 82–84).
Collecting individual-level data on exposure to natural environments (time-activity and behavior component), outcome (individual well-being, including SWB), and factors that influence the relationship between exposure and outcome (including demographic and sociocultural factors, connectedness to nature, perceptions, and preferences) allows for exposure and outcome to be linked at the individual level in order to quantify directly any significant associations. Such topics (see Table 1) should be systematically included in representative nationwide population surveys. In the US, a number of ongoing surveys could provide a suitable platform for the proposed research (see next section, Table 2a). These surveys already capture outcome variables of interest, including self-reported health and/or subjective well-being. The incorporation of additional questions within these surveys would provide means for an assessment of how the natural environment is experienced at the individual level. Also, using such a questionnaire in ongoing nationwide health-related longitudinal studies (see next section, Table 2b) and new studies (that collect individual residential address and detailed health, occupational and lifestyle data) would make it possible to analyze life course effects and determine causal relationships between exposure and outcome, as well as evaluate the role of the natural environment on mental health and chronic disease later in life.7,13,55,56 Inclusion of this questionnaire in adequately sized experimental studies together with objective measures of environmental intensity, and of physical and mental health, would improve our understanding of (a) total positive effects on different components of individual well-being, (b) whether or not there is a threshold for the relationship between exposure to natural environments and effect on individual well-being, and (c) the temporal persistence of any salutogenic effects. Strengthening the evidence in these ways will further a salutogenic orientation to environmental protection, provide a more complete accounting of the cost to benefit ratio, and be more protective of public health.
Table 1.
Examples of Topics to Include in the Questionnaire
| topic | description | references |
|---|---|---|
| measuring exposure | ||
| time–activity and behavior | level of awareness (viewing, entering, engaging) | 13, 18 and references therein, and 49–51 |
| mode of contact (visual, auditory, olfactory, tactile, etc.) | ||
| temporal attributes (frequency, duration) | ||
| use/activities (exercise, relaxation, recreation, etc.) | ||
| measuring outcome | ||
| self-reported health | respondent’s self-rating of own health, in general | 61 and 62 |
| subjective well-being | respondent’s self-rating of different components of subjective well-being | 63–70 and 85 |
| measuring factors influencing relationship between exposure and outcome (human context) | ||
| demographic and sociocultural factors | age | 11 and 78 |
| sex | ||
| race/ethnicity | ||
| education | ||
| household income | ||
| social interaction (e.g., social contacts with neighbors, involvement in community projects) | ||
| urban, suburban, or rural living environment | ||
| dog ownership | ||
| access to car | ||
| connectedness to nature | respondent’s self-rating of different dimensions of connectedness to nature | 23–25 and 86 |
| perceptions regarding natural environments | access | 78, 87, and 88 |
| features | ||
| safety | ||
| preferences related to experience of nature | motivations barriers |
74, 87, and 88 |
| overall satisfaction with experience of nature | respondent’s overall satisfaction with own experience of nature in everyday life | |
Table 2.
Selected Nationwide Population Surveys and Long-Term Health Studies
| (a) population surveys | |
| survey characterization | comments |
| American Time Use Survey (ATUS) | |
| Institutions: Sponsored by the Bureau of Labor Statistics and conducted by the U.S. Census Bureau | Nationally representative. Large sample sizea. Allows modules sponsored by other federal agencies b. Restricted access to respondents’ substate area location down to county, depending on population size. |
| Focus: Amount of time people spend doing various activities, such as paid work, childcare, volunteering, and socializing | |
| Target population: Individuals aged 15 and older | |
| Freq./Start/Latest Release: Annual/2005/2016 | |
| Source: https://www.bls.gov/tus/ | |
| Behavioral Risk Factor Surveillance System (BRFSS) | |
| Institution: Administered by the Centers for Disease Control and Prevention (CDC) | Very large sample size. Allows questions sponsored by other federal agencies, but states select which modules to field, so deployment is not standard nationwide. Restricted access to respondents’ substate area location down to county, depending on population size. |
| Focus: Health status and risk-related behaviors | |
| Target population: Adults | |
| Freq./Start/Latest Release: Annual/All states since 1994/2016 | |
| Source: https://www.cdc.gov/brfss/index.html | |
| General Social Survey (GSS) | |
| Institutions: Funded by the National Science Foundation and administered by NORC at University of Chicago | Nationally representative. Medium-sized sample. Allows modulesc sponsored by federal agencies and others. Long-term trend analyses possible for core questions (including self-reported general health and happiness). Restricted access to respondents’ residential Census Tract. |
| Focus: Social characteristics, attitudes, and behaviors | |
| Target population: Adults | |
| Freq./Start/Latest Release: Biennial/1972/2016 Source: http://www.gss.norc.org/ |
|
| National Health and Nutrition Examination Survey (NHANES) | |
| Institution: Administered by CDC Focus: Health and nutritional status; environmental exposures |
Nationally representative. Medium-sized sample. Includes interviews, physical examinations, laboratory tests, nutritional assessment and DNA repository; ongoing small longitudinal study. Restricted on-site access to residential location is granted through National Center for Health Statistics’ Research Data Center (RDC). |
| Target population: Adults and children | |
| Freq./Start/Latest Release: Biennial/1999–2000/2015–2016 Source: https://www.cdc.gov/nchs/nhanes/index.htm |
|
| National Health Interview Survey (NHIS) | |
| Institutions: Conducted by U.S. Census Bureau and administered by CDC | Nationally representative. Large sample size. Includes leisure-time physical activity. Restricted access to geocoded residential address. |
| Focus: Health status, conditions, and behaviors; health care access and utilization. | |
| Target population: Adults and children | |
| Freq./Start/Latest Release: Annual/1957/2017 | |
| Source: https://www.cdc.gov/nchs/nhis/index.htm | |
| Youth Risk Behavior Surveillance System (YRBSS) | |
| Institution: Administered by CDC Focus: Health risk behaviors and prevalence of obesity and asthma |
National survey conducted by CDC and state, territorial, tribal, and local education and health agencies and tribal governments. Allows for school-based analysis. |
| Target population: 9th through 12th grade students in public and private schools | |
| Freq./Start/Latest Release: Biennial/1991/2017 | |
| Source: https://www.cdc.gov/healthyyouth/data/yrbs/index.htm | |
| (b) long-term nationwide health studies | |
| study characterization | comments |
| “All of Us” Research Program | |
| Institution: National Institutes of Health Focus: Precision medicine Cohort: Target: 1 million + individuals Source: https://allofus.nih.gov/ |
Launched in May 2018. Open for enrollment. Aims to accelerate research and improve health, taking into account individual differences in lifestyle, environment, and biology. |
| Cancer Prevention Studies | |
| Institution: American Cancer Society | Newest cohort recruited in 2013 (over 304,000 participants). |
| Focus: Cancer prevention | |
| Cohort: Men and women between the ages of 30 and 65 years who had no personal history of cancer | |
| Source: https://www.cancer.org/research/we-conduct-cancer-research/epidemiology.html | |
| Health and Retirement Study (HRS) | |
| Institution: National Institute on Aging and the Social Security Administration | Biennial follow-up (since 1992), optional modules have included well-being. |
| Focus: Aging | |
| Cohort: Approximately 20 000 adults aged 50+ | |
| Source: https://hs.isr.umich.edu/ | |
| National Longitudinal Study of Adolescent to Adult Health (Add Health) | |
| Institution: Carolina Population Center | Ongoing Wave V follow-up from 2016 to 2018 collects social, environmental, behavioral, and biological data. |
| Focus: How social environments and behaviors in adolescence are linked to health and achievement outcomes in young adulthood and life-course health trajectories | |
| Cohort: Nationally representative sample of adolescents in grades 7–12 in the United States during the 1994–95 school year | |
| Source: http://www.cpc.unc.edu/projects/addhealth | |
| Nurses’ Health Studies | |
| Institutions: Brigham and Women’s Hospital, Harvard Medical School, Harvard T. H. Chan School of Public Health | Started in 1976. Biennial follow-ups. Third generation studies ongoing. |
| Focus: Risk factors for major chronic diseases in women | |
| Cohort: Over 275 000 male and female nurses (still enrolling participants) | |
| Source: http://www.nurseshealthstudy.org/ | |
| Sister Study | |
| Institution: National Institute of Environmental Health Sciences Focus: Environmental and genetic risk factors for breast cancer |
Annual and biennial follow-ups collect detailed health and environmental exposures information. |
| Cohort: 50 000 women across the US and Puerto Rico, who were between ages 35–74 during recruitment (2003–2009) and whose sister had breast cancer | |
| Source: https://sisterstudy.niehs.nih.gov/ | |
| Women’s Health Initiative (WHI) and extension studies | |
| Institutions: Sponsored by the National Institutes of Health (NIH), National Heart, Lung, and Blood Institute (NHLBI) Focus: Heart disease, breast, and colorectal cancer, osteoporotic fractures in postmenopausal women, and aging |
The Observational Study, which tracks the medical events and health habits of 93 676 women, examines the relationship between lifestyle, health and risk factors, and disease outcomes. |
| Cohort: Originally enrolled 161 808 women aged 50–79 between 1993 and 1998. | |
| Source: https://www.whi.org/ | |
Sample sizes: Small (less than 1000), medium (1000–10 000), large (10 000–100 000), and very large (over 100 000).
For example, Eating & Health module (2006–2008, 2014–2016) sponsored by U.S. Department of Agriculture’s Economic Research Service; Well-Being module (2010, 2012, 2013) sponsored by the National Institute on Aging.
For example, Environment module (1993, 2000, 2010); U.S. Environmental Protection Agency-sponsored questions deployed in 2012.
Placing survey observations in context of both reported and verifiable landscape features (environmental intensity) will increase our understanding of individuals’ experience of nature. Thus, it is important to collect respondents’ location data at finer resolution than census region or even zip code or county, as most often done in existing nationwide surveys. Although requiring stricter data storage and management policies to ensure protection of participant privacy, collection of residential address, occupational, and recreational locations allows for individually reported survey responses to be linked with high resolution land cover information. For example, the U.S. Environmental Protection Agency’s geospatial online tool, EnviroAtlas89 can serve as an objective measure of various facets of nature for evaluation against well-being outcomes. EnviroAtlas provides a wealth of geospatial environmental and socioeconomic data, including many quantitative indicators of the potential benefits humans derive from the natural environment for the nation (e.g., tree buffer near roadways, percentage of natural land cover, percentage of forest) and, at very fine resolution (1 m), for selected communities (e.g., access to parks and coastal areas, view of trees, view of water, green space per capita).
As has been noted by others (e.g., refs 12 and 54), research with an experience of nature perspective and consideration of the complex array of natural and human factors (e.g., see Figure 2) will require diverse capability and expertise. Specifically, meaningful research and discovery will require interdisciplinary teams represented by exposure science, landscape ecology, environmental psychology, epidemiology, public health, geography, landscape architecture, urban and regional planning, survey methodology, statistics, economics, etc.
Candidate Population Surveys and Long-Term Health Studies in the U.S.
As mentioned above, we advocate for a nationwide assessment of experience of nature and its influence on health and well-being outcomes with inclusion of both topics in representative nationwide population surveys and long-term health studies. In Table 2, we summarize ongoing surveys and studies in the U.S. that would be likely candidates for this purpose.
Part a of Table 2 includes publicly administered surveys that target civilian noninstitutionalized population and allow (restricted) access to individual-level data. In general, researchers are required to submit a proposal detailing intended use for the data and data management policies and procedures to ensure confidentiality of responses and participants’ privacy. Part b of Table 2 includes ongoing long-term nationwide health studies that could potentially incorporate experience of nature in their questionnaire sets.
We considered other publicly administered nationwide surveys, but they were not deemed feasible because of expected cost or lack of access to individual-level data.
The largest population survey in the U.S., the Decennial Census of Population and Housing (https://www.census.gov/programs-surveys/decennial-census.html), and its companion, the annual American Community Survey (ACS) (https://www.census.gov/programs-surveys/acs/), administered and financed by the U.S. Census Bureau, do not release individual-level data; for ACS estimates are provided at state, county, place, and metro/micropolitan area with population 20 000 or over. Additionally, given the cost associated with their deployment, these would not be feasible instruments to consider.
The National Survey of Fishing, Hunting, & Wildlife-Associated Recreation (FHWAR), conducted by the U.S. Census Bureau every five years (2001, 2006, 2011, 2016) and sponsored by the U.S. Fish and Wildlife Service (https://www.census.gov/programs-surveys/fhwar.html), provides information on individuals involved in fishing, hunting, and other wildlife-associated recreation (observation, photography, feeding) in residential areas (within a one mile radius of home) and at least one mile from home. This survey targets participation and expenditures of persons 16 years of age and older and includes visits to public parks and publicly orprivately owned natural areas, expenses in books, equipment, etc., as well as land leasing and ownership. Although it would be a likely candidate for inclusion of self-reported health and well-being questions and a few additional questions on experience of nature (including connectedness to nature), this survey does not release individual-level data but only estimates for nine Census Divisions.
The annual National Survey of Children’s Health (NSCH), conducted by the U.S. Census Bureau and sponsored and funded by the Maternal and Child Health Bureau of the Health Resources and Services Administration, targets the physical and emotional health of children ages 0–17 years of age (https://mchb.hrsa.gov/data/national-surveys/data-user). Although this survey allows for inclusion of questions from other federal agencies (e.g., CDC and USDA), it only releases national and state-level estimates, so it would not be appropriate for the intended use.
Several ongoing nationwide health surveys have specific scopes and are not likely candidates either (e.g., National Study on Drug Use and Health, National Survey on Family Growth, and Surveillance Epidemiology and End Results (SEER) on cancer incidence).
Additionally, a few private institutions conduct nationwide surveys regularly (e.g., Gallup, Kaiser Permanente, Pew Research Center, etc.) that could be considered for inclusion of a module on experience of nature coupled with health and well-being questions. Besides cost and data ownership/release issues, an important aspect to consider would be accessing individual-level location data other than the usually collected zip code or county.
CONCLUSIONS
We suggest environmental health research should place greater emphasis on the salutogenic effects of the natural environment. First, these effects are not well accounted for. Wolf et al.,54 using a life course approach and accounting for potential cost savings, avoided health care costs and increased income, quantify the benefits from exposure to natural environments in urban areas to be between $2.7 and $6.8 billion annually focusing on six outcomes (birth weight, attention deficit hyperactivity disorder (ADHD), school performance, crime, cardiovascular disease, and Alzheimer’s disease). This is likely a considerable underestimate of total benefits for individual well-being and does not include any positive effects on SWB. As noted by Wolf and colleagues, additional research is needed in order to improve valuation of these benefits. One of the reasons that the salutogenic effects of the environment are not accounted for is the lack of methods of measurement as reflected in the adage “if it can’t be measured, it is as though it doesn’t exist.” In contrast, we have very sophisticated methods for measuring and therefore accounting for adverse effects of the environment on human health (e.g., chemical pollutants, noise, etc.). Several years after Barton and Petty2 and Thompson Coon and colleagues4 published their reviews, there is still a need for a more comprehensive evaluation of the magnitude of the salutogenic effects of the natural environment, as well as the factors that influence those effects. As synthesized in refs 12 and 13, besides improving the metrics and measurements of objective exposure to natural environments, we need to measure how subjective factors affect our experience of nature and how exposure to natural environments impacts all aspects of individual well-being, including SWB. Here, we foster the use of a standard survey instrument to collect data on individuals’ experience of nature coupled with health and well-being outcomes, from nationally representative samples, to provide a more complete picture of the salutogenic effect of the natural environment on individual well-being in the US. Nonetheless, we acknowledge that different types of studies (e.g., ethnographic research, activity tracking using Global Positioning Systems (GPS) and accelerometers, experience sampling, social network analysis, etc.) will allow the collection of data at an individual level that may not be captured by more traditional instruments.
We suggest that a parallel track for environmental protection based on its salutogenic effects and individual well-being will significantly improve efforts to protect public health and the environment. Although the ecological public health paradigm has captured the importance of the natural environment for human health, this is not fully reflected in current environmental health science and practice.10 For example, although health impact assessments of community projects increasingly detail beneficial effects for health and well-being related to the natural environment, these benefits are not usually quantified. Potential benefits from community projects aiming at increasing access to natural environments may not be realized due to subjective barriers (e.g., perception of limited benefits) or can be enhanced if subjective enablers are fostered (e.g., motivation for active living). There is a need for communities and public health practitioners to assess those barriers and enablers and to promote education or outreach programs to address them (e.g., refs 37 and 74). Also, evidence-based decision making would greatly benefit from the inclusion of these salutogenic effects in cumulative risk assessments. The development of methods to measure specific and individual-level salutogenic effects of the natural environment through the life course will provide a necessary initial and enabling step toward a full accounting of the importance of the environment for public health and well-being. Our suggested approach is aligned with several authors (e.g., refs 10, 12, and 54) who note that to maximize the salutogenic effects of the natural environment we need to address the existing research gaps and promote collaboration between environmental health scientists and professionals from many other disciplines.
ACKNOWLEDGMENTS
We thank Ferdouz Cochran, Anne Neale, and Steven Prince for enriching dialogues that helped shape this article and conceptualize Figures 1 and 2. We are grateful to EPA internal reviewers and journal peer-reviewers for their insightful reviews that greatly improved the paper.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
The authors declare no competing financial interest.
The U.S. Environmental Protection Agency, through its Office of Research and Development, has provided administrative review of this article and approved it for publication.
REFERENCES
- (1).Ward Thompson C Linking landscape and health: The recurring theme. Landscape Urban Plan 2011, 99, 187–195. [Google Scholar]
- (2).Barton J; Pretty J What is the best dose of nature and green exercise for improving mental health? A multi-study analysis. Environ. Sci. Technol. 2010, 44 (10), 3947–3955. [DOI] [PubMed] [Google Scholar]
- (3).Depledge MH; et al. Can natural and virtual environments be used to promote improved human health and wellbeing? Environ. Sci. Technol. 2011, 45 (11), 4660–4665. [DOI] [PubMed] [Google Scholar]
- (4).Thompson Coon J; Boddy K; Stein K; Whear R; Barton J; Depledge MH Does participating in physical activity in outdoor natural environments have a greater effect on physical and mental well-being than physical activity indoors? A systematic review. Environ. Sci. Technol. 2011, 45, 1761–1772. [DOI] [PubMed] [Google Scholar]
- (5).Akers A; et al. Visual color perception in green exercise: positive effects on mood and perceived exertion. Environ. Sci. Technol. 2012, 46 (16), 8661–8666. [DOI] [PubMed] [Google Scholar]
- (6).Brown D; et al. Viewing nature scenes positively affects recovery of autonomic function following acute-mental stress. Environ. Sci. Technol. 2013, 47 (11), 5562–5569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (7).Alcock I; et al. Longitudinal effects on mental health of moving to greener and less green urban areas. Environ. Sci. Technol. 2014, 48 (2), 1247–1255. [DOI] [PubMed] [Google Scholar]
- (8).Frumkin H Beyong toxicity: Human health and the natural environment. Am. J. Prev. Med. 2001, 20 (3), 234–240. [DOI] [PubMed] [Google Scholar]
- (9).McCurdy LE; Winterbottom KE; Mehta SS; Roberts JR Using Nature and Outdoor Activity to Improve Children’s Health. Curr. Probl. Pediatr. Adolesc. Health Care 2010, 40, 102–117. [DOI] [PubMed] [Google Scholar]
- (10).Coutts C; Forkink A; Weiner J The portrayal of natural environment in the evolution of the ecological public health paradigm. Int. J. Environ. Res. Public Health 2014, 11, 1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (11).Hartig T; Mitchell R; De Vries S; Frumkin H Nature and health. Annu. Rev. Public Health 2014, 35, 207–228. [DOI] [PubMed] [Google Scholar]
- (12).Frumkin H; et al. Nature Contact and Human Health: A Research Agenda. Environ. Health Perspect. 2017, 125 (7), 075001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (13).Markevych.; et al. Exploring pathways linking greenspace to health: Theoretical and methodological guidance. Environ. Res. 2017, 158, 301–317. [DOI] [PubMed] [Google Scholar]
- (14).van den Bosch M; Ode Sang A Urban natural environments as nature-based solutions for improved public health - A systematic review of reviews. Environ. Res. 2017, 158, 373–384. [DOI] [PubMed] [Google Scholar]
- (15).Antonovsky A The salutogenic model as a theory to guide health promotion. Health Promot. Int. 1996, 11 (1), 11–18. [Google Scholar]
- (16).Keyes CLM The Mental Health Continuum: From Languishing to Flourishing in Life. Journal of Health and Social Behavior 2002, 43 (2), 207–222. [PubMed] [Google Scholar]
- (17).Berto R The role of nature in coping with psychophysiological stress: A literature review on restorativeness. Behav. Sci. 2014, 4 (4), 394–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (18).Bratman GN; Hamilton J; Daily GC The impacts of nature experience on human cognitive function and mental health. Ann. N. Y. Acad. Sci. 2012, 1249, 118–136. [DOI] [PubMed] [Google Scholar]
- (19).Beute F; de Kort YA Salutogenic effects of the environment: Review of health protective effects of nature and daylight. Appl. Psychol. Health Well Being 2014, 6, 67–95. [DOI] [PubMed] [Google Scholar]
- (20).Ulrich RS; Simons RF; Losito BD; Fiorito E; Miles M; Zelson M Stress recovery during exposure to natural and urban environments. J. Environ. Psychol. 1991, 11, 201–230. [Google Scholar]
- (21).Kaplan S The restorative benefits of nature: Toward an integrative framework. J. Environ. Psychol. 1995, 15, 169–182. [Google Scholar]
- (22).Wilson EO Biophilia; Harvard University Press: Cambridge, MA, 1984. [Google Scholar]
- (23).Nisbet EK; Zelenski JM; Murphy SA The nature relatedness scale: Linking individuals’ connection with nature to environmental concern and behavior. Environment and Behavior 2009, 41, 715–740. [Google Scholar]
- (24).Mayer FS; Frantz CM The connectedness to nature scale: A measure of individuals’ feeling in community with nature. J. Environ. Psychol 2004, 24, 503–515. [Google Scholar]
- (25).Schultz PW Inclusion with nature: Understanding the psychology of human-nature interactions. In The Psychology of Sustainable Development; Schmuck P, Schultz PW. Eds.; Kluwer: New York, 2002; pp 61–78. [Google Scholar]
- (26).Kuo M How might contact with nature promote human health? Promising mechanisms and a possible central pathway. Front. Psychol. 2015, 6, 1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (27).Hunter RF; Christian H; Veitch J; Astell-Burt T; Hipp JA; Schipperijn J The impact of interventions to promote physical activity in urban green space: A systematic review and recommendations for future research. Soc. Sci. Med. 2015, 124, 246–256. [DOI] [PubMed] [Google Scholar]
- (28).Fan Y; Das KV; Chen Q Neighborhood green, social support, physical activity, and stress: Assessing the cumulative impact. Health & Place 2011, 17 (6), 1202–1211. [DOI] [PubMed] [Google Scholar]
- (29).Dadvand P; Bartoll X; Basagaña X; Dalmau-Bueno A; Martinez D; Ambros A; et al. Green spaces and General Health: Roles of mental health status, social support, and physical activity. Environ. Int. 2016, 91, 161–167. [DOI] [PubMed] [Google Scholar]
- (30).Bowler DE; Buyung-Ali LM; Knight TM; Pullin AS A systematic review of evidence for the added benefits to health of exposure to natural environments. BMC Public Health 2010, 10, 456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (31).Lee AC; Maheswaran R The health benefits of urban green spaces: A review of the evidence. Journal of Public Health (Oxford, England) 2011, 33, 212–222. [DOI] [PubMed] [Google Scholar]
- (32).Bancroft C; Joshi S; Rundle A; Hutson M; Chong C; Weiss CC; et al. Association of proximity and density of parks and objectively measured physical activity in the United States: A systematic review. Soc. Sci. Med. 2015, 138, 22–30. [DOI] [PubMed] [Google Scholar]
- (33).James P; Banay RF; Hart JE; Laden F A review of the health benefits of greenness. Curr. Epidemiol. Rep. 2015, 2, 131–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (34).Lovell R; Wheeler BW; Higgins SL; Irvine KN; Depledge MH A systematic review of the health and well-being benefits of biodiverse environments. J. Toxicol. Environ. Health, Part B 2014, 17, 1. [DOI] [PubMed] [Google Scholar]
- (35).Haluza D; Schönbauer R; Cervinka R Green Perspectives for Public Health: A Narrative Review on the Physiological Effects of Experiencing Outdoor Nature. Int. J. Environ. Res. Public Health 2014, 11, 5445–5461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (36).Gray C; Gibbons R; Larouche R; Sandseter EB; Bienenstock A; Brussoni M; et al. What is the relationship between outdoor time and physical activity, sedentary behaviour, and physical fitness in children? A systematic review. Int. J. Environ. Res. Public Health 2015, 12 (6), 6455–6474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (37).McCormick R Does Access to Green Space Impact the Mental Well-being of Children: A Systematic Review. Journal of Pediatric Nursing 2017, 37, 3–7. [DOI] [PubMed] [Google Scholar]
- (38).Cervinka R; Roderer K; Hefler E Are nature lovers happy? On various indicators of well-being and connectedness to nature. J. Health Psychol. 2012, 17, 379–388. [DOI] [PubMed] [Google Scholar]
- (39).Capaldi CA; Dopko RL; Zelenski JM The relationship between nature connectedness and happiness: A meta-analysis. Front. Psychol. 2014, DOI: 10.3389/fpsyg.2014.00976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (40).Ulrich RS View through a window may influence recovery from surgery. Science 1984, 224 (4647), 420–421. [DOI] [PubMed] [Google Scholar]
- (41).Horowitz S Therapeutic Gardens and Horticultural Therapy. Alternative and Complementary Therapies 2012, 18 (2), 78. [Google Scholar]
- (42).Cervinka R; Röderer K; Hämmerle I Evaluation of Hospital Gardens and Implications for Design: Benefits from Environmental Psychology for Architecture and Landscape Planning. Journal of Architecture and Planning Research 2014, 31 (1), 43–56. [Google Scholar]
- (43).Volker S; Kistemann T The impact of blue space on human health and well-being - salutogenetic health effects of inland surface waters: A review. Int. J. Hyg. Environ. Health 2011, 214, 449–460. [DOI] [PubMed] [Google Scholar]
- (44).White MP; Pahl S; Wheeler BW; Fleming LEF; Depledge MH The ’blue gym’: What can blue space do for you and what can you do for blue space? J. Mar. Biol. Assoc. U. K 2016, 96, 5–12. [Google Scholar]
- (45).Nieuwenhuijsen MJ; Kruize H; Gidlow C; et al. Positive health effects of the natural outdoor environment in typical populations in different regions in Europe (PHENOTYPE): a study programme protocol. BMJ. Open 2014, 4, No. e004951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (46).Lachowycz K; Jones AP Towards a better understanding of the relationship between greenspace and health: Development of a theoretical framework. Landscape Urban Plan 2013, 118, 62–69. [Google Scholar]
- (47).Kaplan R; Kaplan S The Experience of Nature—A Psychological Perspective; Cambridge University Press, 1995. [Google Scholar]
- (48).Coutts C Green Infrastructure and Public Health; Routledge: Oxon, UK, 2016. [Google Scholar]
- (49).Keniger LE; Gaston KJ; Irvine KN; Fuller RA What are the benefits of interacting with nature? Int. J. Environ. Res. Public Health 2013, 10, 913–935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (50).Franco LS; Shanahan DF; Fuller RA A Review of the Benefits of Nature Experiences: More Than Meets the Eye. Int. J. Environ. Res. Public Health 2017, 14, 864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (51).Shanahan DF; Fuller RA; Bush R; Lin BB; Gaston KJ The Health Benefits of Urban Nature: How Much Do We Need? BioScience 2015, 65 (5), 476–485. [Google Scholar]
- (52).National Research Council (NRC). Exposure Science in the 21st Century: A Vision and a Strategy; The National Academies Press: Washington, DC, 2012. [PubMed] [Google Scholar]
- (53).Ekkel ED; de Vries S Nearby green space and human health: Evaluating accessibility metrics. Landscape and Urban Planning 2017, 157, 214–220. [Google Scholar]
- (54).Wolf KL; Measells MK; Grado SC; Robbins AST Economic values of metro nature health benefits: A life course approach. Urban For. Urban Gree. 2015, 14, 694–701. [Google Scholar]
- (55).Astell-Burt T; Mitchell R; Hartig T The association between green space and mental health varies across the life course. A longitudinal study. J. Epidemiol. Community Health 2014, 68, 578–583. [DOI] [PubMed] [Google Scholar]
- (56).Wu YT; Prina AM; Jones AP; Barnes LE; Matthews FE; Brayne C Community environment, cognitive impairment and dementia in later life: results from the Cognitive Function and Ageing Study. Age Ageing 2015, 44, 1005–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (57).Pearce J; Shortt N; Rind E; Mitchell R Life Course, Green Space and Health: Incorporating Place into Life Course Epidemiology. Int. J. Environ. Res. Public Health 2016, 13, 331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (58).National Research Council (NRC). Subjective Well-Being: Measuring Happiness, Suffering, and Other Dimensions of Experience: Panel on Measuring Subjective Well-Being in a Policy-Relevant Framework; Stone AA, Mackie C, Eds.; Committee on National Statistics, Division of Behavioral and Social Sciences and Education, The National Academies Press: Washington, DC, 2013. [PubMed] [Google Scholar]
- (59).Diener E; Chan MY Happy people live longer: Subjective well-being contributes to health and longevity. Applied Psychology: Health and Well-Being 2011, 3 (1), 1–43. [Google Scholar]
- (60).Michaelson J; Mahony S; Schifferes J Measuring Well-Being—A Guide for Practitioners; The New Economics Foundation: London, UK, 2012. [Google Scholar]
- (61).Gallagher JE; Wilkie AA; Cordner A; Hudgens EE; Ghio AJ; Birch RJ; Wade TJ Factors associated with self-reported health: implications for screening level community-based health and environmental studies. BMC Public Health 2016, 16, 640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (62).Schnittker J; Bacak V The increasing predictive validity of self-rated health. PLoS One 2014, 9, No. e84933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (63).Ader DN Developing the Patient-Reported Outcomes Measurement Information System (PROMIS). Medical Care 2007, 45, S1–S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (64).Hays RD; Bjorner JB; Revicki DA; Spritzer KL; Cella D Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Qual. Life Res. 2009, 18, 873–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (65).Topp CW; Ostergaard SD; Sondergaard S; Bech P The WHO-5 Well-Being Index: A systematic review of the literature. Psychother. Psychosom. 2015, 84 (3), 167–76. [DOI] [PubMed] [Google Scholar]
- (66).Golderberg D; Williams P A User’s Guide to the General Health Questionnaire; NFER-Nelson: Windsor, UK, 1988. [Google Scholar]
- (67).Diener E; Emmons R; Larsen J; Griffin S The Satisfaction with Life scale. Journal of Personality Assessment 1985, 49, 71–75. [DOI] [PubMed] [Google Scholar]
- (68).Kobau R; Sniezek J; Zack MM; Lucas RE; Burns A Wellbeing assessment: An evaluation of wellbeing scales for public health and population estimates of wellbeing among US adults. Applied Psychology: Health and Well-being 2010, 2 (3), 272–297. [Google Scholar]
- (69).Eurofound Third European Quality of Life Survey—Quality of Life in Europe: Subjective Well-Being; Publications Office of the European Union: Luxembourg, 2013. [Google Scholar]
- (70).Personal Wellbeing Index-Adult (PWI-A), 5th ed.; International Wellbeing Group, 2013. [Google Scholar]
- (71).Laeremanns M; Dons E; Avila-Palencia L; Carrasco-Turigas G; Orjuela-Mendoza JP; Anaya-Boig E Black carbon reduces beneficial effect of physical activity on lung function. Med. Sci. Sports Exerc. 2018, DOI: 10.1249/MSS.0000000000001632. [DOI] [PubMed] [Google Scholar]
- (72).Bell SL; Phoenix C; Lovell R; Wheeler BW Green space, health and wellbeing: Making space for individual agency. Health & Place 2014, 30, 287–292. [DOI] [PubMed] [Google Scholar]
- (73).Floyd M Race, ethnicity and use of the national park system. Social Science Research Review 1999, 1 (2), 1–24. [Google Scholar]
- (74).Calogiuri G; Chroni S The impact of the natural environment on the promotion of active living: An integrative systematic review. BMC Public Health 2014, 14, 873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (75).Rigolon A A complex landscape of inequity in access to urban parks: A literature review. Landscape and Urban Planning 2016, 153, 160–169. [Google Scholar]
- (76).Jennings V; Larson L; Yun J Advancing sustainability through urban green space: Cultural ecosystem services, equity, and social determinants of health. Int. J. Environ. Res. Public Health 2016, 13 (2), 196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (77).Diener E; Tay L Subjective well-being and human welfare around the world as reflected in the Gallup World Poll. International Journal of Psychology 2015, 50 (2), 135–149. [DOI] [PubMed] [Google Scholar]
- (78).TNS Monitor of Engagement with the Natural Environment (MENE)—Technical Report from the 2013–14 survey, Natural England Joint Report JP010, 2015. http://publications.naturalengland.org.uk/publication/4750201384337408 (accessed 22 Jul 2016).
- (79).White MP; Pahl S; Wheeler BW; Depledge MH; Fleming LEF Natural environments and subjective wellbeing: Different types of exposure are associated with different aspects of wellbeing. Health & Place 2017, 45, 77–84. [DOI] [PubMed] [Google Scholar]
- (80).Villeneuve PJ; et al. Association of residential greenness with obesity and physical activity in a US cohort of women. Environ. Res. 2018, 160, 372–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (81).Grigsby-Toussaint DS; et al. Sleep insufficiency and the natural environment: Results from the US Behavioral Risk Factor Surveillance System survey. Prev. Med. 2015, 78, 78–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (82).Bogar S; Beyer KM Green space, violence, and crime: A systematic review. Trauma Violence Abuse 2016, 17, 160–171. [DOI] [PubMed] [Google Scholar]
- (83).Gascon M; Triguero-Mas M; Martínez D; Dadvand P; Forns J; Plaséncia A; et al. Mental health benefits of long-term exposure to residential green and blue spaces: A systematic review. Int. J. Environ. Res. Public Health 2015, 12, 4354–4379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (84).Hunter AJ; Luck GW Defining and measuring the social-ecological quality of urban greenspace: A semi-systematic review. Urban Ecosystems 2015, 18, 1139–1163. [Google Scholar]
- (85).Stewart-Brown S; Tennant A; Tennant R; Platt S; Parkinson J; Weich S Internal construct validity of the Warwick-Edinburgh Mental Well-being Scale (WEMWBS): a Rasch analysis using data from the Scottish Health Education Population Survey. Health and Quality of Life Outcomes 2009, 7, 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (86).Nisbet EK; Zelenski JM The NR-6: A new brief measure of nature relatedness. Front. Psychol. 2013, 4, 813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (87).Saelens BE; Sallis JF; Black JB; Chen D Neighborhood-based differences in physical activity: An environment scale evaluation. Am. J. Public Health 2003, 93 (9), 1552–1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (88).Grahn P; Stigsdotter UA Landscape planning and stress. Urban For. Urban Gree. 2003, 2 (1), 1–18. [Google Scholar]
- (89).Pickard BR; Daniel J; Mehaffey M; Jackson LE; Neale A EnviroAtlas: A new geospatial tool to foster ecosystem services science and resource management. Ecosystem Services 2015, 14, 45–55. [Google Scholar]