Abstract
COVID-19 has led to massive disruptions in societal, economic and healthcare systems globally. While COVID-19 has sparked a surge and expansion of new digital business models in different industries, healthcare has been slower to adapt to digital solutions. The majority of ophthalmology clinical practices are still operating through a traditional model of ‘brick-and-mortar’ facilities and ‘face-to-face’ patient–physician interaction. In the current climate of COVID-19, there is a need to fuel implementation of digital health models for ophthalmology. In this article, we highlight the current limitations in traditional clinical models as we confront COVID-19, review the current lack of digital initiatives in ophthalmology sphere despite the presence of COVID-19, propose new digital models of care for ophthalmology and discuss potential barriers that need to be considered for sustainable transformation to take place.
Keywords: telemedicine, public health, vision, Covid-19, diagnostic tests/investigation
COVID-19 has led to massive disruptions in societal, economic and healthcare systems globally. It is unlikely that clinical care can simply revert to ‘old norms’ after the COVID-19 pandemic. To prepare for a post-COVID-19 ‘new normal’, healthcare providers must shift from a current reactive mode to a proactive reimagining future-planning state with innovative new models of care, including digital and telemedicine solutions.1
Limitations in current eye care model during the COVID-19 pandemic
While COVID-19 has sparked a surge and expansion of new digital solutions and innovative business models in different industries,2 healthcare has been slower to adapt to digital solutions.1 3 4 The majority of ophthalmology clinical practices are still operating through a traditional model of ‘brick-and-mortar’ facilities and ‘face-to-face’ patient–physician interaction.3 5 This traditional ‘physical’ model is not suited for the COVID-19 pandemic and the postpandemic ‘new normal’.6
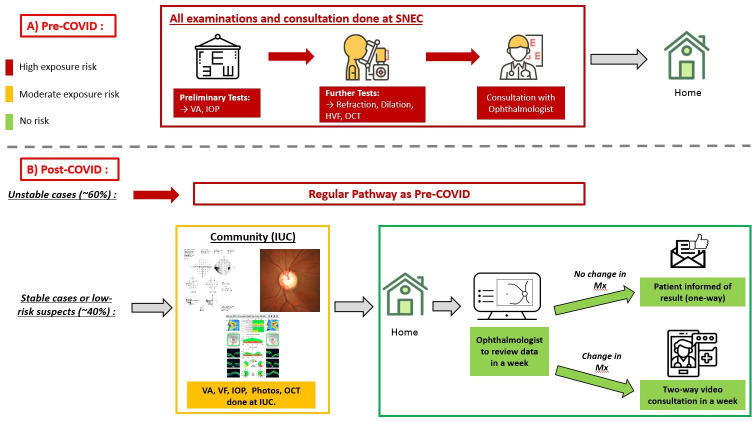
First, as illustrated in figure 1, in the traditional model, new patients from the community and primary care setting typically have to go through long and convoluted journey before eventually ‘arriving’ at tertiary eye hospitals. Furthermore, on eventual arrival at tertiary eye clinics, patients would typically further encounter a complicated clinical workflow with long waiting times and multiple preliminary and confirmatory investigations (eg, visual acuity (VA), intraocular pressure (IOP), scans such as optical coherence tomography (OCT) and visual fields (VFs)), resulting in multiple ‘touch points’ and interactions with different providers (ie, optometrists, ophthalmic technicians, nurses, doctors, pharmacists), before being diagnosed and given a management plan. All these factors increase exposure and thus the risk of contracting COVID-19, which is now known to spread through asymptomatic carriers (both patients and healthcare providers).7 8
Figure 1.
Illustrations of patient journey in the traditional model, its limitations and proposed new digital solutions to alleviate these limitations. (Image icons extracted and modified from Flaticon.com, performed by YCT.) AI, artificial intelligence; IOP, intraocular pressure; VA, visual acuity.
Second, many patients need not be seen at tertiary eye centres. New case referrals and follow-up appointments at these eye centres may not be considered urgent or essential during the COVID-19 pandemic and even immediately in the early phases of ‘reopening’. However, the typical referral of new patients from primary care setting is based on self-reported symptoms or suboptimal VA level measured by the Snellen test, which is known to have higher false-positive rates.9 In fact, prior to COVID-19, a large number of new referral cases to tertiary eye centres are attributed to visually insignificant cataracts, dry eyes or even refractive error (which merely requires provision of spectacles).10–12 Similarly, a large proportion of follow-up appointments (eg, stable cataract and glaucoma, postcataract surgery or stable retinal diseases) in many eye centres could be deferred and postponed.13 Thus, during and after the COVID-19 pandemic, it is important to reduce non-urgent referrals and non-urgent follow-ups to eye centres. This will also reduce non-essential human movement in the community.
Principle considerations in the post-COVID-19 pandemic ‘new normal’
Based on WHO directives on social distancing and reduced movements, eye clinics need to sustainably adopt the three following ‘reduce’ (3Rs) principles: (1) reduce number of patients coming to one site, (2) reduce patient’s visit time at any site and (3) reduce the contact time between healthcare staff and patient. In the current climate of COVID-19, implementation of these ‘3Rs’ while maintaining high standard of care for patients calls for innovative digital solutions.
Ophthalmology is unique among medical specialties in that the requisite ocular examinations are heavily dependent on investigations and visualisation of ocular images. This makes it ideal for new care models where the traditional consultations and ocular examinations can be replaced with investigations (eg, retinal photographs or OCT) outside of the eye clinic, leveraging on digital tools and infrastructure. Results from these investigations can largely be reviewed remotely and securely by an ophthalmologist, thus reducing physical contact between the patient and the physician. In Singapore, during the national lockdown period (7 April till 1 June 2020), 80% of appointments in Singapore National Eye Centre (SNEC) were postponed/rescheduled. After lockdown, gradual and calibrated reopening measures ensued, with ‘resumption of operation’ priority given to essential services such as healthcare. Nevertheless, as the world is still grappled with COVID-19, there is still a potential risk of community transmission; thus, it is still important to continue reducing face-to-face consultations as much as possible.
Nevertheless, based on a preliminary literature review (search terms and results described in online supplemental appendix A), since the start of the COVID-19 pandemic, only a handful of countries (eg, USA, UK, India, Hong Kong, Singapore)14–18 had reported adoption of teleconsultations in ophthalmology thus far. These currently reported adoptions were mainly limited to subspecialties of medical retina,17 neuro-ophthalmology19 20 and paediatric ophthalmology.21 This further highlights the need to fuel wider implementation of telemedicine and digital health models for ophthalmology in the current climate of COVID-19. There is enormous room for growth in this regard to improve delivery of eye care services.
bjophthalmol-2020-317683supp001.pdf (28.2KB, pdf)
Here, we proposed a new digital model of care with three core components: the deployment of ‘investigation units in the community (IUCs)’ with teleconsultation, the use of a specially designed all-in-one app and effective triaging.
IUC, coupled with teleconsultation
In this model, multiple IUCs will be set up in the community to allow easy access to eye care services for patients. IUCs are stand-alone units, staffed by trained ophthalmic technicians to perform VA measurement, IOP measurement, anterior and posterior segment photography, OCTs and VF. Existing follow-up patients with stable eye conditions such as low-risk glaucoma suspect (ie, ocular hypertension with open angle), stable early glaucoma, stable diabetic retinopathy (DR), early age-related macular degeneration (AMD) or non-complicated postcataract surgery cases can be enrolled into this model. Briefly, these patients will first undergo the necessary investigations (as indicated by the attending ophthalmologist, from the last management plan) during their routine follow-up visits at the IUCs instead of tertiary eye hospital. Within a week after the examination at IUCs, the ophthalmologist will review the investigation results remotely. Communication of investigation results could be a one-way to the patient (text message/email, if all results remain stable and optimal) or a two-way audio/video teleconsultation when further elaborations on the investigation results are required. Worsening of the patient’s condition, when noticed along the pathway in this model, would trigger a consultation appointment back at the tertiary eye centre. Furthermore, in the event where recurrent medications need to be dispensed to patients, the required medications will be couriered to the patient.
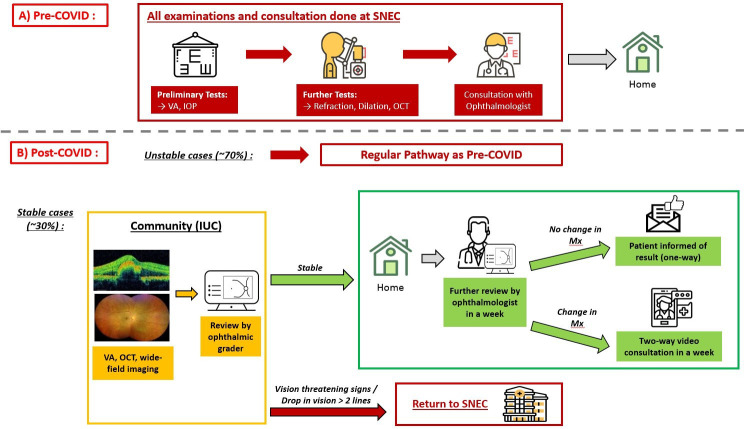
As an example, at the SNEC’s glaucoma clinic, approximately 40% of patients are stable glaucoma cases. The traditional model requires all patients (regardless of the disease severity) to go through examinations and consultations at the SNEC. If this model is still implemented in the current pandemic situation, it would continue exposing patients to higher risk of COVID-19 (figure 2A). Alternatively, stable glaucoma cases or new glaucoma suspect cases could instead be enrolled into a new proposed model (figure 2B), in which patients will first undergo investigative tests (ie, VA, IOP, OCT, VF) at the IUCs and return home right after. The glaucoma specialist will review the examination results within a week. If all is stable with no change in the management plan, the patient will be informed of the outcome via SMS or email (one-way teleconsultation). On the contrary, if a change in management is deemed necessary by the glaucoma specialist, then a two-way video consultation will further take place to explain the next action plan to patient.
Figure 2.
New IUC with teleconsultation model for stable glaucoma or low-risk glaucoma suspects. Red box denotes high exposure risk to COVID-19, orange box denotes moderate risk and green box denotes low risk. (Image icons extracted and modified from Flaticon.com, performed by YCT.) HVF, Humphrey visual field; IOP, intraocular pressure; IUC, investigative unit in community; OCT, optical coherence tomography; SNEC, Singapore National Eye Centre; VA, visual acuity; VF, visual field.
During our pilot trial of this new model, we conducted a preliminary satisfaction survey on 214 patients with glaucoma/glaucoma suspect (mean age of 62.7 years, 61.7% women) enrolled in this new model of care (table 1). About 90% of them either ‘agree or strongly agree’ that the new model of care helps to save time, and the outcomes were explained clearly and timely. Furthermore, 94.8% either ‘agree or strongly agree’ that the medical care received was satisfactory. Finally, 94.4% rated the overall experience in the new model as being ‘excellent’, and the remaining 5.6% rated as ‘good’. Overall, the survey results indicated good patient acceptance of this new model of care among enrolled patients with glaucoma/glaucoma suspect.
Table 1.
Survey on satisfaction towards the new IUC with teleconsultation model of care among 214 enrolled patients with glaucoma/glaucoma suspect
| Survey items | Strongly agree | Agree | Neutral | Disagree | Strongly disagree |
| ‘I spend less time in this new IUC model with teleconsultation compared with the conventional outpatient specialist clinic’. | 123 (57.5%) | 70 (32.7%) | 20 (9.3%) | 1 (0.5%) | 0 |
| ‘The outcome of the clinic visit is explained clearly to me’. | 123 (57.5%) | 69 (32.2%) | 19 (8.9%) | 3 (1.4%) | 0 |
| ‘The outcome was communicated to me timely (ie, within a week)’. | 128 (59.6%) | 68 (31.9%) | 16 (7.5%) | 1 (0.5%) | 1 (0.5%) |
| ‘I am satisfied with the medical care I've received’. | 124 (57.9%) | 79 (36.9%) | 10 (4.7%) | 1 (0.5%) | 0 |
IUC, investigative unit in community.
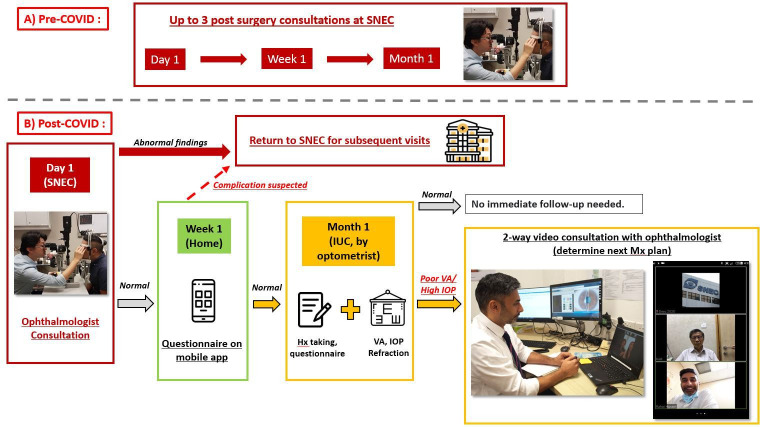
Similarly, in retinal clinic, the traditional model would continue exposing patients to higher risk of COVID-19 (figure 3A). On the contrary, applying the new digital model for stable retinal diseases (such as early AMD, stable DR or epiretinal membrane) could save approximately 30% of consultation visits to SNEC’s retinal clinics (figure 3B). Appropriate patients would also first undergo investigative tests (ie, VA, OCT, wide-field retinal imaging) at the IUCs (figure 3B), and in slight contrast to the glaucoma model described above, the investigations at IUC would first be reviewed by trained ophthalmic graders. If there was a drop in vision (best-corrected visual acuity (BCVA) >2 lines) or vision threatening retinal signs are observed by the grader, the patient would be referred back to SNEC. Conversely, if the condition is assessed as stable by the grader, the patient would return home after the session at IUC. Thereafter, a retinal specialist would still further review the examination results in a week as a ‘double confirmation’ process. If all is indeed stable, the patient would receive the notification via SMS or email, whereas if a change in management is warranted, a two-way video teleconsultation would take place.
Figure 3.
New IUC with teleconsultation model for stable retinal diseases. (Image icons extracted and modified from Flaticon.com, performed by YCT.) IUC, investigative unit in community; OCT, optical coherence tomography; VA, visual acuity; SNEC, Singapore National Eye Centre.
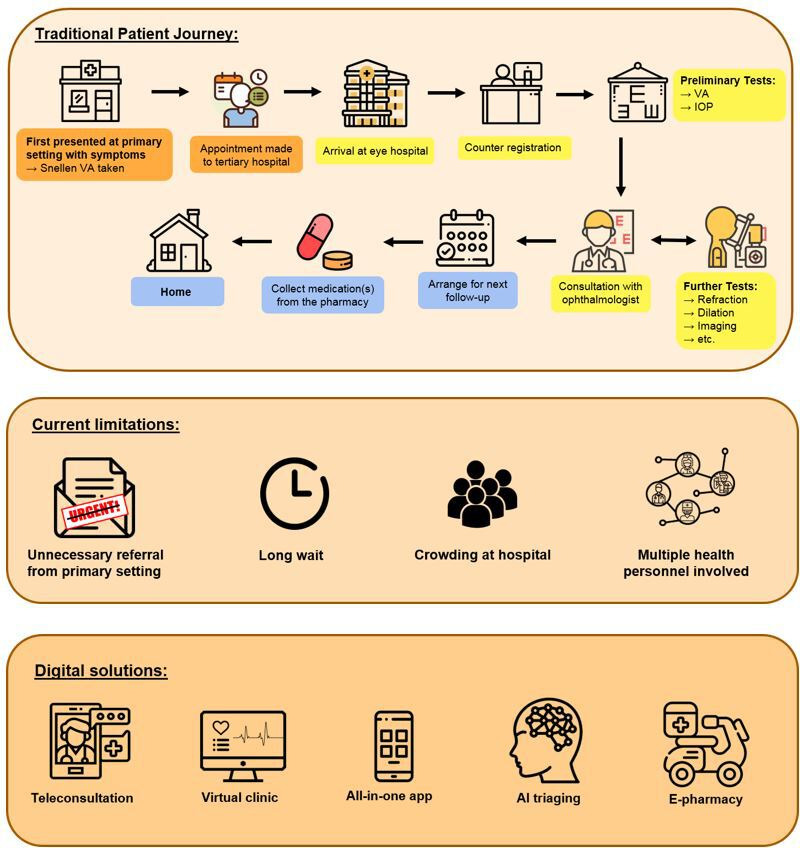
At SNEC, approximately 15 000 cataract surgeries are performed yearly. The traditional model (pre-COVID) involves up to three postcataract surgery eye clinic visits (day 1, week 1 and month 1), thus amounting to 45 000 visits per annum at SNEC (figure 4A). In the proposed new model (figure 4B), on day 1 after surgery, the patient would still be seen by the clinician in the clinic, but if all is normal, the subsequent week 1 and month 1 visits can be replaced with home-based self-monitoring (via mobile app) and community optometrists. For the week 1 visit, the patient would answer a series of questions designed to detect postcataract surgery complications (eg, endophthalmitis) using the specially designed mobile phone app. Based on patient’s responses, if complication is suspected, the patient would be asked to return to SNEC. On the contrary, if all is normal, the patient would proceed to month 1 visit with a designated community optometrist. The optometrist would again ask a series of questions and perform VA, refraction and IOP measurements (non-contact tonometry). In the event where the optometrist determines that the BCVA is worse than expected or the IOP is high, a two-way video call with the ophthalmologist would ensue immediately to determine whether the patient needs to be brought back to SNEC for further assessment.
Figure 4.
New home-based monitoring and teleconsultation model for management of postcataract surgery cases. (Image icons extracted and modified from Flaticon.com, performed by YCT.) IOP, intraocular pressure; IUC, investigative unit in community; VA, visual acuity; SNEC, Singapore National Eye Centre.
Altogether, this proposed model of IUC with teleconsultation removes the need to be seen at the tertiary eye hospital and substantially reduces the ‘footprint’ of a patient’s journey compared with traditional models, thus greatly reducing the exposure risk to COVID-19. This concept of decoupling investigations from clinical decision-making/management plan (which depends on ophthalmologist’s discretion) can potentially be adopted in other countries as well so as to further ‘free up’ ophthalmologists’ load and the burden at tertiary eye centres. In particular, for large countries with less ideal accessibility to tertiary eye centres, the proposed investigations units can be potentially located in communities or partnering optometry practices where they are more accessible to patients. Table 2 further summarises the differences between conventional care models and these new proposed models.
Table 2.
Comparison between conventional care model and proposed model of investigation units in community (IUCs) with teleconsultation.
| Conventional model | Proposed model | |
| Requirement of physical visit at tertiary eye care centre: | ||
| Stable glaucoma cases | All examinations and consultations done at tertiary eye care centre | Nil |
| Stable retinal disease cases | All examinations and consultations done at tertiary eye care centre | Nil (unless drop in vision >2 lines/vision-threatening signs detected at IUC) |
| Postcataract surgery cases | All three postsurgery consultations done at tertiary eye care centre (ie, day 1, week 1, month 1 visits) | Only needed on day 1 (if stable/uneventful in subsequent visits) |
| Involvement of ophthalmologists: | ||
| Stable glaucoma and retinal disease cases | Ophthalmologist needed to perform physical examinations and face-to-face consultations | Remote review of investigational results, followed by teleconsultation. No physical examinations required |
| Postcataract surgery cases | Ophthalmologist needed to perform physical examinations and face-to-face consultations for all three postsurgery evaluations (ie, day 1, week 1, month 1 visits) | Physical examination by ophthalmologists only needed on day 1 |
| Use of digital means/telemedicine: | SMS/text reminder for appointments. |
|
‘All-in-one’ mobile device application
To empower patients take coresponsibility of their conditions, we have designed an all-in-one eye care mobile device app. This app will serve several purposes. First, it will help to better manage the logistics of visit attendances by performing ‘smart scheduling’, which automatically identifies available appointment slot, thus doing away the conventional arduous process of manual scheduling by clinic receptionist. Second, it will provide a secured and user-friendly platform for teleconsultations in the IUC model described above. Third, it will securely store individual management plans and treatment outcomes, allowing for a quasi-medical record that may be shared with other physicians. Patients will also be able to track their own progress and treatment outcomes for chronic eye conditions. Finally, this app will provide education on eye conditions for patients and carers, and interactive appointment or medication reminders with an overall aim of enhancing patients’ outcomes by improving adherence, knowledge and awareness. To better facilitate digital onboarding, we will also deploy staff as ‘digital ambassadors’ in the clinic to assist/guide elderly patients on the usage of the mobile app.
Chatbot and artificial intelligence to enhance triaging of urgent cases
Third, referral and scheduling of non-urgent cases (eg, dry eyes and stable cataract) should only resume after the pandemic situation improves. Furthermore, because of post-COVID-19 ‘backlog’ of appointments, priority should first be assigned to urgent cases. The current referral pathway from primary care to tertiary eye care cannot effectively triage urgent cases as risk stratification typically requires decision-making from ophthalmologists or highly trained ophthalmic nurses and not primary care physicians.
To address this gap, we are designing a medical chatbot to determine the urgency of referral based on patients’ self-reported symptoms. In addition, retinal photograph-based artificial intelligence algorithm could be developed to help better triage referral cases from primary care settings into non-urgent and urgent.
Potential barriers to sustained adoption of new digital models
For sustained adoptions of these new digital models during and beyond COVID-19, several potential barriers ought to be considered. First, information technology (IT) infrastructure, internet connectivity (ie, between devices and networks) and cybersecurity are key enablers for these new digital solutions. Subpar performances in these infrastructure will reduce patient’s user experience and assurance, and thus discourage patients to continue in this new care model. Hence, to further cater to the demands of new digital solutions, tandem effort to further build up these IT capabilities within the health system is needed.22 Second, lack of access to internet-enabled devices among elderly patients or lack of comfort and familiarity to operate technology independently (thus relying on caregivers to maintain enrolment in these digital models) may also dampen patient’s acceptance to these new models. To address this, during the initial stages of enrolment, greater in-person engagement to educate, guide and encourage elderly patients (and caregivers) on the benefits and usage of the new digital solutions would be needed. Finally, to further justify the deployment of these new models in the long run, implementation evaluation in the aspects of operational efficiency (eg, time, patient volume), cost-effectiveness, patient compliance (ie, adherence to subsequent follow-ups under the new models), safety and risk needs to be further conducted.
Conclusion
The current COVID-19 pandemic has catalysed the use of new digital solutions to enable continuation of eye care for patients.23 This digital trajectory will only accelerate and is unlikely to reverse. Hence, it is imperative for healthcare providers to embrace new digital models of care in the post-COVID-19 ‘new normal’. However, to ensure sustained adoption, it is equally important to robustly evaluate the effectiveness, feasibility, cost, risks and patient acceptance of these digital models.
Acknowledgments
We thank SNEC’s Singapore Ocular Reading Centre and Ms Sarah Shwu Huey Tan for the assistance in figure preparations.
Footnotes
Y-CT and RH contributed equally.
GSWT and TYW contributed equally.
Contributors: YCT, RH, GSWT and TYW conceived and designed the study. YCT, RH, KYCT, ACST, ACYC and CYC collected data. YCT, RH, KYCT, ACST and ACYC analysed and interpreted the data. YCT, RH and TYW wrote the manuscript. KYCT, ACST, DSWT, CYC, GSWT and TYW reviewed the manuscript. All authors approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not required.
References
- 1. Hollander JE, Carr BG. Virtually perfect? telemedicine for Covid-19. N Engl J Med Overseas Ed 2020;382:1679–81. 10.1056/NEJMp2003539 [DOI] [PubMed] [Google Scholar]
- 2. Ting DSW, Carin L, Dzau V, et al. Digital technology and COVID-19. Nat Med 2020;26:459–61. 10.1038/s41591-020-0824-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Keesara S, Jonas A, Schulman K. Covid-19 and Health Care’s Digital Revolution. N Engl J Med Overseas Ed 2020;382:e82. 10.1056/NEJMp2005835 [DOI] [PubMed] [Google Scholar]
- 4. Greenhalgh T, Wherton J, Shaw S, et al. Video consultations for covid-19. BMJ 2020;368:m998. 10.1136/bmj.m998 [DOI] [PubMed] [Google Scholar]
- 5. Olivia Li J-P, Shantha J, Wong TY, et al. Preparedness among ophthalmologists: during and beyond the COVID-19 pandemic. Ophthalmology 2020;127:569–72. 10.1016/j.ophtha.2020.03.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Webster P. Virtual health care in the era of COVID-19. The Lancet 2020;395:1180–1. 10.1016/S0140-6736(20)30818-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bai Y, Yao L, Wei T, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA 2020;323:1406–7. 10.1001/jama.2020.2565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Arons MM, Hatfield KM, Reddy SC, et al. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med Overseas Ed 2020;382:2081–90. 10.1056/NEJMoa2008457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Falkenstein IA, Cochran DE, Azen SP, et al. Comparison of visual acuity in macular degeneration patients measured with Snellen and early treatment diabetic retinopathy study charts. Ophthalmology 2008;115:319–23. 10.1016/j.ophtha.2007.05.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Davey CJ, Green C, Elliott DB. Assessment of referrals to the hospital eye service by optometrists and GPs in Bradford and Airedale. Ophthalmic Physiol Opt 2011;31:23–8. 10.1111/j.1475-1313.2010.00797.x [DOI] [PubMed] [Google Scholar]
- 11. Pierscionek TJ, Moore JE, Pierscionek BK. Referrals to ophthalmology: optometric and general practice comparison. Ophthalmic Physiol Opt 2009;29:32–40. 10.1111/j.1475-1313.2008.00614.x [DOI] [PubMed] [Google Scholar]
- 12. Kern C, Fu DJ, Kortuem K, et al. Implementation of a cloud-based referral platform in ophthalmology: making telemedicine services a reality in eye care. Br J Ophthalmol 2020;104:312–7. 10.1136/bjophthalmol-2019-314161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Meltzer ME, Congdon N, Kymes SM. Cost and expected visual effect of interventions to improve follow-up after cataract surgery: prospective review of early cataract outcomes and grading (PRECOG) study. JAMA Ophthalmology 2017;135:85–94. [DOI] [PubMed] [Google Scholar]
- 14. Parikh D, Armstrong G, Liou V, et al. Advances in telemedicine in ophthalmology. Semin Ophthalmol 2020;35:210–5. 10.1080/08820538.2020.1789675 [DOI] [PubMed] [Google Scholar]
- 15. Jayadev C, Mahendradas P, Vinekar A, et al. Tele-consultations in the wake of COVID-19 – suggested guidelines for clinical ophthalmology. Indian J Ophthalmol 2020;68:1316–27. 10.4103/ijo.IJO_1509_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wong JKW, Shih KC, Chan JCH, et al. Tele-Ophthalmology amid COVID-19 pandemic—Hong Kong experience. Graefes Arch Clin Exp Ophthalmol 2020:1. 10.1007/s00417-020-04753-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Saedon H, Gould G, Begum M, et al. Video Conferencing in the intravitreal injection clinic in response to the COVID-19 pandemic. Ophthalmol Ther 2020;9:1–6. 10.1007/s40123-020-00262-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Khor WB, Yip L, Zhao P, et al. Evolving practice patterns in Singapore's public sector ophthalmology centers during the COVID-19 pandemic. Asia Pac J Ophthalmol 2020;9:285–90. 10.1097/APO.0000000000000306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Moss HE, Lai KE, Ko MW. Survey of telehealth adoption by Neuro-ophthalmologists during the COVID-19 pandemic: benefits, barriers, and utility. J Neuroophthalmol 2020;40:346–55. 10.1097/WNO.0000000000001051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ko MW, Busis NA. Tele-Neuro-Ophthalmology: vision for 20/20 and beyond. J Neuroophthalmol 2020;40:378–84. 10.1097/WNO.0000000000001038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Deshmukh AV, Badakere A, Sheth J, et al. Pivoting to teleconsultation for paediatric ophthalmology and strabismus: our experience during COVID-19 times. Indian J Ophthalmol 2020;68:1387–91. 10.4103/ijo.IJO_1675_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wong MYZ, Gunasekeran DV, Nusinovici S, et al. Telehealth demand trends during the COVID-19 pandemic in the top 50 most affected countries: Infodemiological evaluation. JMIR Public Health Surveill 2021;7:e24445. 10.2196/24445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gunasekeran DV, Tham Y-C, Ting DSW, et al. Digital health during COVID-19: lessons from operationalising new models of care in ophthalmology. Lancet Digit Health 2021;3:e124–34. 10.1016/S2589-7500(20)30287-9 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bjophthalmol-2020-317683supp001.pdf (28.2KB, pdf)