Abstract
Objectives. To examine changes in prevalence of cannabis use and of cannabis use disorder symptomatology among young adults from 2014 to 2019 in Washington State, where nonmedical (or “recreational”) cannabis was legalized in 2012 and retail stores opened in July 2014.
Methods. We used 6 years of cross-sectional data collected annually from 2014 (premarket opening) to 2019 from 12 963 (∼2000 per year) young adults aged 18 to 25 years residing in Washington. Logistic regression models estimated yearly change in prevalence of cannabis use at different margins and related outcomes.
Results. Prevalence of past-year, at least monthly, at least weekly, and daily use of cannabis increased for young adults, although increases were driven by changes among those aged 21 to 25 years. There was also a statistically significant increase in prevalence of endorsing at least 2 of 5 possible symptoms associated with cannabis use disorder.
Conclusions. Among young adults in Washington, particularly those of legal age, prevalences of cannabis use and cannabis use disorder symptomatology have increased since legalization. This trend may require continued monitoring as the nonmedical cannabis market continues to evolve. (Am J Public Health. 2022;112(4):638–645. https://doi.org/10.2105/AJPH.2021.306641)
Over the past 2 decades, cannabis use prevalence has increased among young adults in the United States. Data from the National Survey on Drug Use and Health (NSDUH) showed an increase in the prevalence of any past-year cannabis use among young adults aged 18 to 25 years from 29.8% in 2002 to 35.4% in 2019.1 This increase is concerning because cannabis use among young adults is associated with adverse short- and long-term consequences, including cognitive deficits,2 poorer academic outcomes,3–6 impaired driving,7 worse mental health,8 and addiction.9 In 2019, 5.8% of those aged 18 to 25 years met diagnostic criteria for past-year cannabis use disorder (CUD).9
As of August 2021, 18 states and Washington, DC, have legalized cannabis for nonmedical (or “recreational”) use, and, in November 2012, Washington State was 1 of the first 2 states to legalize it.10 Although cannabis use and possession for people older than 21 years were permitted 30 days after the election, the first state-licensed retail cannabis stores did not open until July 2014. Thus, there was a period of 19 months when use and possession were legal, but there were no legal means of buying or selling nonmedical cannabis. In addition to the illicit market, there was access through weakly regulated medical dispensaries.11,12 It was not until 2015 that strong state-level regulation phased out the original medical cannabis dispensaries and incorporated the medical market into the regulated system.13 Initially, even after July 2014, the number of nonmedical (or “retail”) stores was small and prices could not compete with the illegal and medical cannabis markets.14 Prices of pretax cannabis flower in retail stores dropped, however, from as high as $30 per gram in 2014 to less than $7 per gram in late 2017.15 Along with dropping prices, the number of retail outlets in the state increased.13 Also, the variety of cannabis products increased, with a larger proportion of sales in the form of edibles, tinctures, and concentrates used in vaping.14,16
The inception and growth of the nonmedical cannabis market may have led to increased cannabis use and related problems, although studies comparing states with and without legalized nonmedical cannabis have yielded mixed results. In an examination of 2008–2018 data from a survey of undergraduate 4-year college students, 1 study found that prevalence of both “any” and “frequent” past-month cannabis use increased among students in states with legal nonmedical cannabis compared with use among students in other states.17 A study using 2008–2016 NSDUH data reported that legalization was associated with statistically significant increases in “any” and “frequent” cannabis use and meeting criteria for CUD among adults 26 years and older, but not among young adults aged 18 to 25 years.18 Differences between young adults younger or older than 21 years were not assessed, and the absence of legal access for those 18 to 20 years may partially account for the lack of evidence of increase in those aged 18 to 25 years. Evidence on changes in cannabis use among adolescents has been mixed,18–21 including from studies that have specifically examined changes in adolescent cannabis use among Washington State high school students.20,21
We assessed changes from 2014 to 2019 in cannabis use among young adults in Washington State using repeated statewide cross-sectional data. We analyzed change across these cohorts in past-year use, at least monthly use, at least weekly use, and daily use of cannabis and changes in prevalence of 2 or more symptoms typically associated with cannabis dependence or CUD. In addition, we examined whether trends in these cannabis-related outcomes differed by whether young adults were aged 21 years and older or younger than 21 years.
METHODS
We collected data as part of the Washington Young Adult Health Survey, a project funded by the Division of Behavioral Health & Recovery in Washington State’s Health Care Authority, to evaluate impacts of alcohol privatization and cannabis legalization among young adults in Washington. We administered 6 annual cross-sectional surveys, each with approximately 2000 respondents, between 2014 and 2019. We recruited participants from across Washington, with all geographic regions of the state represented. We recruited a new sample of study participants in each year through direct mail and online advertising. Although we did not separately track source of recruitment for cohorts 1 to 3, the proportion of participants coming from the direct mail to known Washington residents was similar across time (e.g., we recruited 59.0% of participants in cohort 4 from direct mail, 56.9% of participants in cohort 5, and 59.4% of participants in cohort 6).
The direct mail outreach was facilitated through access to Washington State Department of Licensing contact information, and a random sample of licensed drivers aged 18 to 25 years received a letter inviting their participation for each cohort. Online advertising strategies included using social media sites such as Facebook and Instagram, other online sites such as Craigslist, and a dedicated study Web site. Participants who responded to the online advertisements completed a screening survey to determine whether they met inclusion criteria of age (18–25 years) and residence in Washington State.
Participants provided digital consent and completed an online screening survey. Study staff then verified eligibility and identity through a follow-up telephone call, after which we directed them to the online baseline survey. In 2014, we collected data between late April and early August, with 69.3% of data completely collected before the opening of the first cannabis retail outlets in July. Although the remaining 30.7% were completed after stores had opened, the impact of stores opening likely did not change how most remaining participants accessed cannabis. Only 18 retail outlets opened statewide during July 2014, and only 31 had opened by August. By comparison, in July 2015 there were 163 retail outlets. Field periods in 2015 to 2019 were roughly the same length and generally launched in June and closed by November each year (except 2019, which launched in August and closed in December). The Web-based surveys contained questions on substance use, related risk factors, attitudes and acceptability, perceived norms, and health behaviors. The survey took approximately 20 minutes to complete, and participants received a $10 e-gift card as compensation.
The analytic sample consisted of 12 963 individuals who completed the survey for the first time in 2014 through 2019, provided information on sociodemographic covariates, and provided data on at least 1 of the prevalence outcomes examined. The number of participants at each survey wave ranged from 1675 in 2015 to 2493 in 2016. Geographic distribution and sociodemographic characteristics of the sample are shown in Table 1.
TABLE 1—
Weighted and Unweighted Distribution of Study Participant Characteristics: Washington State, 2014–2019
| Characteristic | Weighted, % or Mean ±SD | Unweighted, No. (%) or Mean ±SD |
| Female sex | 48.6 | 8715 (67.2) |
| Race/ethnicity | ||
| Non-Hispanic White | 66.5 | 8359 (64.5) |
| Non-Hispanic Asian | 7.7 | 1470 (11.3) |
| Non-Hispanic other race | 15.0 | 1376 (10.6) |
| Hispanic, any race | 10.8 | 1758 (13.6) |
| Geographic region | ||
| East | 24.9 | 2749 (21.2) |
| Northwest | 44.8 | 6718 (51.8) |
| Southwest | 30.3 | 3496 (27.0) |
| Age, y | 21.5 ±2.3 | 21.6 ±2.3 |
| Attending 4-y college | 30.5 | 4116 (31.9) |
| Employed full-time | 36.0 | 4432 (34.9) |
| Study year | ||
| 2014 | . . . | 2101 (16.2) |
| 2015 | . . . | 1675 (12.9) |
| 2016 | . . . | 2493 (19.2) |
| 2017 | . . . | 2341 (18.1) |
| 2018 | . . . | 2412 (18.6) |
| 2019 | . . . | 1941 (15.0) |
Note. The study population was n = 12 963.
Measures
Cannabis use
We adapted survey items regarding cannabis use from the Monitoring the Future survey and the Drinking Norms Rating Form.22 Respondents were asked a question about frequency of recreational cannabis use in the past year. Response options ranged from 0 for never to 9 for every day. We based 4 binary measures of cannabis use prevalence on the answer to the past-year recreational use item: any use, at least monthly use, at least weekly use, and daily use.
Cannabis use disorder symptomatology
As we were creating the survey, terminology associated with substance use disorders changed from separate diagnostic criteria for “cannabis dependence” and “cannabis abuse” in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision23 to “cannabis use disorder” in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).24 The NSDUH assesses symptomatology with 18 items, historically split into 12 items that address “dependence” and 6 items that assess “abuse.”25 Participants in this study responded to 9 items adapted from the 12 questions associated with what was previously “cannabis dependence.” We used the 9 items to assess the presence of 5 symptoms in the past 12 months:
spending considerable time obtaining, using, or getting over the effects of cannabis (1 item);
attempting to set limits on use (2 items);
increased tolerance (1 item);
affects emotional or psychological and physical health and whether use continued despite these effects (3 items); and
wanting or trying to reduce or stop use (2 items).
For analyses, we categorized individuals as having either 2 or more symptoms (1) or none or 1 (0). Although we did not capture the full range of CUD symptoms, given that DSM-5 criteria require the presence of at least 2 of 11 symptoms, those with 2 or more symptoms in this study would likely have elevated symptomatology, aligning with what is considered a “mild” disorder per DSM-5 criteria.
Covariates
Demographic characteristics that we used for analyses included covariates for biological sex (0 = male, 1 = female), age in years, region of the state (east, northwest, southwest), race/ethnicity (4 categories: non-Hispanic White, non-Hispanic Asian, Hispanic, and non-Hispanic other [including American Indian/Alaska Native, Native Hawaiian/Pacific Islander, Black/African American, and multiracial]), whether participants were attending a 4-year college, and whether they were employed full-time.
Analytic Plan
To examine changes in prevalence of cannabis use and related outcomes, which were all dichotomized, we used logistic regression models. Models included data from a total of 12 689 participants with nonmissing covariate or outcome data (97.9% of the total sample). We included survey year as the primary covariate of interest and specified it in separate models (1) as a linear term to assess a linear trend from 2014 to 2019, and (2) using indicator variables to test how prevalence for a given year differed compared with 2014. All models included covariates for biological sex, indicator variables for race/ethnicity (White [reference], Asian, other race, Hispanic any race), indicator variables for geographic region (east [reference], northwest, southwest), age, attending 4-year college, and full-time employment status. To examine whether changes over time varied by age, we used the Wald test to assess interaction terms for survey year × age, where age was dichotomized as younger than 21 years (0) or 21 years or older (1).
Because of overrepresentation in the study sample of women, those of non-Hispanic Asian and Hispanic race/ethnicity, and those living in the northwest region of the state (where the Seattle metropolitan region is located) relative to the general young adult population in Washington State, we created poststratification weights that we applied to all analyses. We created strata according to sex, geographic region, and race/ethnicity. We derived weights by dividing the proportion of young adults in Washington State in that stratum according to 2010 US Census data by the proportion of young adults in the study sample in that stratum. Thus, we gave less weight to strata that were overrepresented in this sample relative to the general population and more weight to strata that were underrepresented. We used R version 3.6 (R Foundation for Statistical Computing, Vienna, Austria) for analyses using the survey package for applying poststratification weights26 and the ggplot2 package for data visualization.27
RESULTS
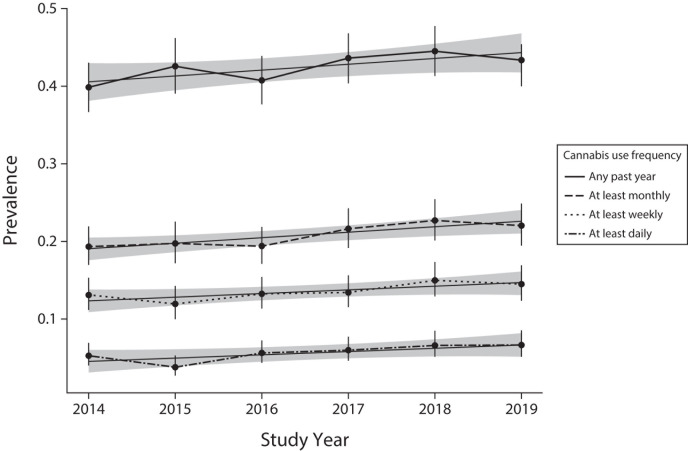
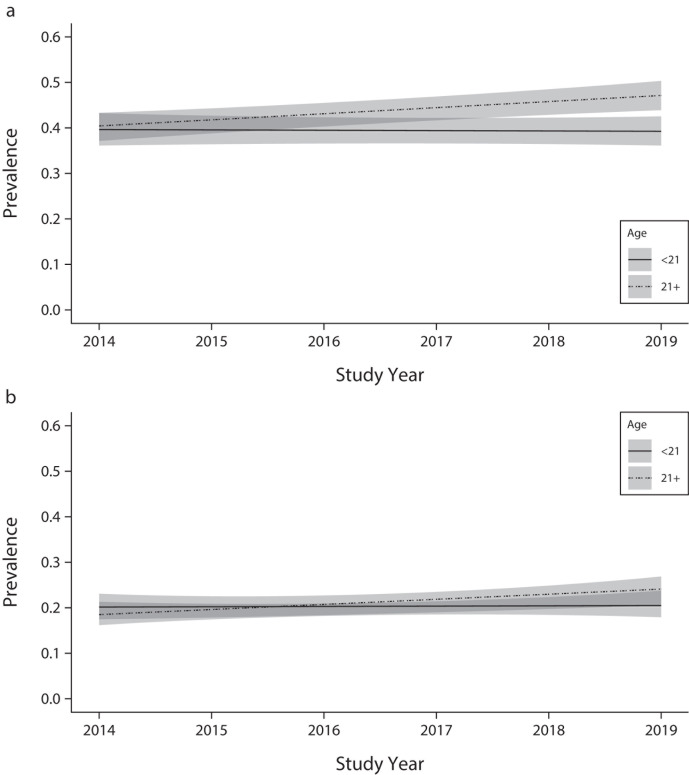
Table 1 shows weighted and unweighted demographic characteristics of the study sample. When examining the changes in prevalence of any past-year, at least monthly, at least weekly, and daily cannabis use, we observed a statistically significant increasing linear trend from 2014 to 2019 for each category of cannabis use frequency (all Ps ≤ .021 for linear trend for study year; Figure 1). Based on models including indicator variables for year, the model-predicted prevalence of any past-year use of cannabis increased from 39.8% in 2014 to 43.3% in 2019, and prevalence of at least monthly use increased from 19.3% to 22.0%. Model-based odds ratios (ORs) for yearly change in the odds for each outcome and unadjusted weighted prevalence estimates by year are available in Tables A–C (available as a supplement to the online version of this article at http://www.ajph.org). We observed a statistically significant cohort × age interaction for any past-year (F1,12 688 = 5.48; P = .019) and at least monthly (F1,12 688 = 4.71; P = .030) use, such that the increasing trend was restricted to those aged 21 years or older (Figure 2).
FIGURE 1—
Model-Predicted Prevalence of Cannabis Use With Linear Trend Lines at Different Margins Among Young Adults: Washington State, 2014–2019
FIGURE 2—
Model-Predicted Linear Trend in (a) Any Past-Year Cannabis Use, and (b) at Least Monthly Use by Age: Washington State, 2014–2019
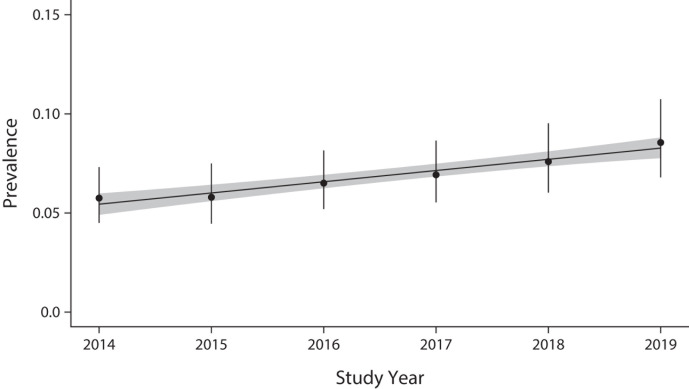
The prevalence of endorsing at least 2 of 5 possible CUD symptoms also increased over time (Figure 3; Tables A–C present the ORs). The model-predicted prevalence estimates of endorsing at least 2 disorder symptoms were 5.7% in 2014 and 8.6% in 2019. There was no statistically significant cohort × age interaction (F1,12 633 = 1.54; P = .22).
FIGURE 3—
Model-Predicted Prevalence With Linear Trend Line of at Least 2 Past-Year Cannabis Use Disorder Symptoms Among Young Adults: Washington State, 2014–2019
DISCUSSION
We have provided an initial examination of trends in cannabis use prevalence among young adults aged 18 to 25 years following legalization of nonmedical cannabis use for adults aged 21 years or older in Washington State. Five years of data after retail outlets opened showed that the prevalence of any past-year, at least monthly, at least weekly, and daily cannabis use has increased among young adults aged 18 to 25 years. Unlike national data, the data showing this trend showed no signs of plateauing during the study period (2014–2019). A significant cohort × age interaction suggested that the increase was primarily driven by those older than 21 years.
These findings highlight the potential importance of prevention efforts accompanying changes to the legal status of cannabis. For example, our results suggest that cannabis use among young adults older than 21 years has increased after legalization, so prevention and intervention efforts could be needed in this changing legal climate. Furthermore, future studies could explore community-level influences on prevalence of use, such as the increasing presence of cannabis retail outlets as well as the economic shifts (e.g., the decreasing prices of legal cannabis products) and changes in illegal markets over time.
Generally, we saw less change in cannabis use among younger adults (i.e., those aged 18–20 years), who may have been less affected by the expansion and evolution of the retail market after 2014 because of the inability to legally purchase nonmedical cannabis in stores. In fact, with the clear regulations of the medical market that arrived in 2015 and that included a state-regulated system of medical cannabis patients,11 access to medical cannabis became more challenging for people younger than 21 years. Among high school seniors who participated in Washington’s Healthy Youth Survey,28,29 the percentage who said cannabis would be “very easy” to get declined from 2012 (42.2%) to 2018 (37.8%), which may have been related to the shutdown of Washington’s previously poorly regulated medical market in 2016.11
Additionally, after the legalization of nonmedical cannabis (i.e., Initiative 502) was enacted, coalitions (e.g., the Washington Healthy Youth Coalition), prevention professionals, and state organizations (e.g., Office of Superintendent of Public Instruction) implemented or supported implementation of prevention programs that intended to reduce youth cannabis use. Moreover, many college campuses incorporated cannabis prevention content with incoming first-year students, and cannabis prevention was the focus of many presentations and trainings statewide. Although we did not assess the impact of these prevention efforts, it is possible that the absence of an increase by those younger than 21 years could have been the result of these intensive (and intentional) prevention efforts.
Importantly, the prevalence of CUD symptomatology has also increased since legalization was implemented. Given the association between CUD-related symptoms and increased frequency of use,2 the increases in prevalence of CUD symptomatology that we saw are not surprising when examined alongside the increased prevalence of frequent use. Indeed, it should be noted that the prevalence of frequent use (daily or weekly) was high among both age groups at all time points, and the prevalence of daily use among those aged 21 years or older had risen from 6.3% in 2014 to 10.2% in 2019.
Another explanatory factor could be the increasing THC (tetrahydrocannabinol, the main psychoactive compound in cannabis) potency of cannabis products sold in the legal market,16,30 including increasing market share of manufactured cannabis products such as concentrates, edibles, and vaping products, which are often higher in THC.14 In addition, the potency of cannabis flower (the product that still accounts for the majority of sales) has increased over time nationwide,31 and even more so in Washington State,30 and more than 92% of all flower sales are of strains with more than 15% THC.16 Greater THC potency may increase the risk of CUD symptoms beyond the frequency of use, and this could be examined in future studies.9
Furthermore, the “approachability” of more novel dab pens and vape pens could provide more convenient ways to use cannabis, and future studies could explore the degree to which these products play a part in changes in cannabis use. Collectively, the increased availability, lower price, and greater potency of cannabis may have led to increased cannabis use and related problems, and future studies can continue to explore the possible relationships among these variables.
Limitations of this study include examining trends in only 1 state where cannabis has been legalized for nonmedical use. We were unable to make comparisons with cannabis use trends in states where cannabis has not been legalized. Some of the general trends we see in our data are similar to trends in national data reviewed earlier and may have less to do with legalization and implementation of the retail cannabis market and more to do with national trends rooted in greater tolerance of cannabis use. Another limitation is that although recruitment strategies were similar across years, our recruitment approach may not have yielded a representative sample relative to Washington State. For example, women were overrepresented in this study. However, our analyses applied poststratification weighting to make distribution of key demographic characteristics similar to the general young adult population in Washington.
Because the survey’s space constraints meant we could not use many full measures, we adapted the assessment of symptomatology associated with CUD from the items of the NSDUH, and future studies could use a more thorough assessment that addresses all potential criteria associated with CUD. Additionally, it would have been helpful to have data from 2012 (when Initiative 502 was being considered) and 2013 (when legalization had been enacted but stores had not yet opened), and it is a limitation that conclusions are constrained to the window following 2014. Finally, although many of our items are self-reports of past-year behavior, the length and timing of the assessment periods across cohorts were not constant over time.
Despite limitations, our findings point to an increasing prevalence of cannabis use, including daily use, among young adults older than 21 years following the legalization of cannabis. For many young adults, this was not solely an increase in frequency, given the increase in endorsing symptomatology that can be associated with CUD. Based on these findings, we encourage continued monitoring of cannabis use and misuse, prevention efforts to reduce harmful misuse of cannabis, and making treatment readily available for young adults whose cannabis use reaches the point of a substance use disorder. Screening could be 1 strategy to identify high-risk or hazardous use in this age group, and brief interventions have been shown to reduce use, time spent high, and consequences.32 Particularly if referral to treatment is warranted or even requested, this could have an impact on young adults who may be struggling with cannabis use and any unwanted effects.
ACKNOWLEDGMENTS
This research was supported by National Institute on Drug Abuse, the National Institutes of Health ([NIH] grant R01DA047996; principal investigator [PI] K. Guttmannova) and the Division of Behavioral Health and Recovery, Washington State Health Care Authority ([HCA] contract 1265-62496; PI: J. R. Kilmer). B. A. Hultgren’s time working on this article was supported by National Institute on Alcohol Abuse and Alcoholism (NIAAA), NIH (grant K01AA027771; PI: B. A. Hultgren). Part of M. S. Gilson’s contribution was supported by the NIAAA (training grant T32AA007455; PI: M. E. Larimer).
General trends from the Young Adult Health Survey (particularly rates of past-year prevalence) have been presented to coalitions, stakeholders and partners in Washington State, and young adults (when discussing perceived and actual norms).
We thank Sarah Mariani, Sandy Salivaras, and Washington’s Division of Behavioral Health and Recovery for their support of the Young Adult Health Survey.
Note. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Washington State HCA.
CONFLICTS OF INTEREST
The authors report no potential or actual conflicts of interest from funding or affiliation-related activities.
HUMAN PARTICIPANT PROTECTION
All initial measures and procedures, as well as all modifications that followed, were reviewed and approved by the University of Washington institutional review board.
REFERENCES
- 1.Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results From the 2019 National Survey on Drug Use and Health. Rockville: MD; 2020. [Google Scholar]
- 2.Volkow ND, Baler RD, Compton WM, Weiss SR. Adverse health effects of marijuana use. N Engl J Med. 2014;370(23):2219–2227. doi: 10.1056/NEJMra1402309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arria AM, Caldeira KM, Bugbee BA, Vincent KB, O’Grady KE. The academic consequences of marijuana use during college. Psychol Addict Behav. 2015;29(3):564–575. doi: 10.1037/adb0000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arria AM, Caldeira KM, Vincent KB, Winick ER, Baron RA, O’Grady KE. Discontinuous college enrollment: associations with substance use and mental health. Psychiatr Serv. 2013;64(2):165–172. doi: 10.1176/appi.ps.201200106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meda SA, Gueorguieva RV, Pittman B, et al. Longitudinal influence of alcohol and marijuana use on academic performance in college students. PLoS One. 2017;12(3):e0172213. doi: 10.1371/journal.pone.0172213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Suerken CK, Reboussin BA, Egan KL, et al. Marijuana use trajectories and academic outcomes among college students. Drug Alcohol Depend. 2016;162:137–145. doi: 10.1016/j.drugalcdep.2016.02.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fischer B, Russell C, Sabioni P, et al. Lower-risk cannabis use guidelines: a comprehensive update of evidence and recommendations. Am J Public Health. 2017;107(8):e1–e12. doi: 10.2105/AJPH.2017.303818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Di Forti M, Quattrone D, Freeman TP, et al. The contribution of cannabis use to variation in the incidence of psychotic disorder across Europe (EU-GEI): a multicentre case–control study. Lancet Psychiatry. 2019;6(5):427–436. doi: 10.1016/S2215-0366(19)30048-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hines LA, Freeman TP, Gage SH, et al. Association of high-potency cannabis use with mental health and substance use in adolescence. JAMA Psychiatry. 2020;77(10):1044–1051. doi: 10.1001/jamapsychiatry.2020.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Washington Secretary of State. Election results. 2022. https://results.vote.wa.gov/results/20121106/measures.html
- 11.Cambron C, Guttmannova K, Fleming CB. State and national contexts in evaluating cannabis laws: a case study of Washington State. J Drug Issues. 2017;47(1):74–90. doi: 10.1177/0022042616678607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kleiman M, Davenport S, Rowe B, et al. Estimating the Size of the Medical Cannabis Market in Washington State. Woodland Hills, CA: BOTEC Analysis; 2015. [Google Scholar]
- 13.Darnell AJ, Bitney K.I-502 Evaluation and Benefit–Cost Analysis: Second Required Report. Olympia: Washington State Institute for Public Policy; 2017 [Google Scholar]
- 14.Firth CL, Davenport S, Smart R, Dilley JA. How high: differences in the developments of cannabis markets in two legalized states. Int J Drug Policy. 2020;75:102611. doi: 10.1016/j.drugpo.2019.102611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Darnell AJ, Hirsch M, Wanner P. Suppressing Illicit Cannabis Markets After State Marijuana Legalization. Olympia, WA: Washington State Institute for Public Policy; 2019. [Google Scholar]
- 16.Smart R, Caulkins JP, Kilmer B, Davenport S, Midgette G. Variation in cannabis potency and prices in a newly legal market: evidence from 30 million cannabis sales in Washington State. Addiction. 2017;112(12):2167–2177. doi: 10.1111/add.13886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bae H, Kerr DCR. Marijuana use trends among college students in states with and without legalization of recreational use: initial and longer-term changes from. Addiction. 2020. 2008;115(6):1115–1124. doi: 10.1111/add.14939. [DOI] [PubMed] [Google Scholar]
- 18.Cerdá M, Mauro C, Hamilton A, et al. Association between recreational marijuana legalization in the United States and changes in marijuana use and cannabis use disorder from 2008 to 2016. JAMA Psychiatry. 2020;77(2):165–171. doi: 10.1001/jamapsychiatry.2019.3254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anderson DM, Hansen B, Rees DI, Sabia JJ. Association of marijuana laws with teen marijuana use: new estimates from the Youth Risk Behavior Surveys. JAMA Pediatr. 2019;173(9):879–881. doi: 10.1001/jamapediatrics.2019.1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cerdá M, Wall M, Feng T, et al. Association of state recreational marijuana laws with adolescent marijuana use. JAMA Pediatr. 2017;171(2):142–149. doi: 10.1001/jamapediatrics.2016.3624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dilley JA, Richardson SM, Kilmer B, Pacula RL, Segawa MB, Cerdá M. Prevalence of cannabis use in youths after legalization in Washington State. JAMA Pediatr. 2019;173(2):192–193. doi: 10.1001/jamapediatrics.2018.4458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baer JS, Stacy A, Larimer M. Biases in the perception of drinking norms among college students. J Stud Alcohol. 1991;52(6):580–586. doi: 10.15288/jsa.1991.52.580. [DOI] [PubMed] [Google Scholar]
- 23.Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association; 2000
- 24. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition . 2013.
- 25.Compton WM, Han B, Jones CM, Blanco C. Cannabis use disorders among adults in the United States during a time of increasing use of cannabis. Drug Alcohol Depend. 2019;204:107468. doi: 10.1016/j.drugalcdep.2019.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lumley T. Analysis of complex survey samples. J Stat Softw. 2004;9(8):1–19. doi: 10.18637/jss.v009.i08. [DOI] [Google Scholar]
- 27.Wickham H. ggplot2: Elegant Graphics for Data Analysis. 2nd ed. New York, NY: Springer; 2016. [Google Scholar]
- 28.Washington State Department of Social and Health Services. 2022. https://www.askhys.net/library/2012/StatewideGr12.pdf
- 29.Washington State Department of Social and Health Services. 2022. https://www.askhys.net/library/2018/StateGr12.pdf
- 30.Northwest High Intensity Drug Trafficking Area. Washington State Marijuana Impact Report: Northwest High Intensity Drug Trafficking Area. Volume 2. August 2017. Available at: https://hidtanmidotorg.files.wordpress.com/2017/09/nwhidta-marijuana-impact-report-volume-2_august-2017.pdf2022
- 31.ElSohly MA, Mehmedic Z, Foster S, Gon C, Chandra S, Church JC. Changes in cannabis potency over the last 2 decades (1995–2014): analysis of current data in the United States. Biol Psychiatry. 2016;79(7):613–619. doi: 10.1016/j.biopsych.2016.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee CM, Kilmer JR, Neighbors C, et al. Indicated prevention for college student marijuana use: a randomized controlled trial. J Consult Clin Psychol. 2013;81(4):702–709. doi: 10.1037/a0033285. [DOI] [PMC free article] [PubMed] [Google Scholar]