Abstract
Objectives. To compare fine particulate matter (PM2.5) concentrations in American Indian (AI)-populated with those in non–AI-populated counties over time (2000–2018) in the contiguous United States.
Methods. We used a multicriteria approach to classify counties as AI- or non--AI-populated. We ran linear mixed effects models to estimate the difference in countywide annual PM2.5 concentrations from well-validated prediction models and monitoring sites (modeled and measured PM2.5, respectively) in AI- versus non–AI-populated counties.
Results. On average, adjusted modeled PM2.5 concentrations in AI-populated counties were 0.38 micrograms per cubic meter (95% confidence interval [CI] = 0.23, 0.54) lower than in non–AI-populated counties. However, this difference was not constant over time: in 2000, modeled concentrations in AI-populated counties were 1.46 micrograms per cubic meter (95% CI = 1.25, 1.68) lower, and by 2018, they were 0.66 micrograms per cubic meter (95% CI = 0.45, 0.87) higher. Over the study period, adjusted modeled PM2.5 mean concentrations decreased by 2.13 micrograms per cubic meter in AI-populated counties versus 4.26 micrograms per cubic meter in non–AI-populated counties. Results were similar for measured PM2.5.
Conclusions. This study highlights disparities in PM2.5 trends between AI- and non–AI-populated counties over time, underscoring the need to strengthen air pollution regulations and prevention implementation in tribal territories and areas where AI populations live. (Am J Public Health. 2022;112(4): 615–623. https://doi.org/10.2105/AJPH.2021.306650)
Short- and long-term exposure to particulate matter of aerodynamic diameter 2.5 micrometers or less (PM2.5) increases the risk of cardiovascular and respiratory disease, among other health outcomes.1–3 In the United States, socioeconomically disadvantaged communities are often exposed to higher PM2.5 exposure levels and bear a disproportionate burden of disease, even at levels well below air quality standards set by the US Environmental Protection Agency (EPA).4,5
American Indian (AI) and Alaska Native communities may be particularly vulnerable to the health effects of air pollution.6,7 These communities already face a large disease burden attributable to environmental pollution owing, for instance, to extensive mining and water contamination on reservations.8,9 The decline in nitrogen dioxide, another criteria air pollutant, was larger in both absolute and relative terms in White versus AI populations between 2000 and 2010.10 Little is known, however, about the extent of particulate air pollution exposure and its potential health effects among rural Native American communities, as most US studies of air pollution have been conducted in urban settings. In a cohort of all Medicare beneficiaries in the continental United States, increasing annual PM2.5 exposure was associated with increases in all-cause mortality from 2000 through 2012, and this effect was higher among participants identified as Native Americans than the overall Medicare population.11 These findings suggest that Native Americans may be more susceptible to adverse health effects from PM2.5 exposure than the overall Medicare population but are limited by wide confidence intervals (CIs). Conclusions may not be generalizable to Native Americans not on Medicare, as Medicare coverage for AI and Alaska Natives is incomplete, especially on reservations and in rural communities.11
Monitoring data sparsity may contribute to gaps in air pollution regulation. As federal air quality monitors tend to be placed in areas of higher population density,12 insight into PM2.5 exposure burdens in AI and Alaskan Native communities is limited, in turn contributing to the paucity of air pollution epidemiological studies that include this population. In the contiguous United States, AI people live predominantly in the West and often reside in sparsely populated areas, including reservations, small towns, and rural areas. Limited data on ambient air pollution levels are currently available in these communities. The use of well-validated models with comprehensive spatial coverage may allow the assessment of possible disparities in PM2.5 concentrations in areas lacking monitoring data.
We aimed to compare ambient PM2.5 average concentrations and trends in AI-populated versus non–AI-populated counties in the contiguous United States from 2000 to 2018. To do so, we compared annual PM2.5 levels predicted by a satellite-based chemical transport model, because of sparse data coverage via the monitoring networks. We also compared monitored PM2.5 concentrations in counties with available monitoring data.
METHODS
We conducted our analysis at the county level, which serves as the most relevant unit of analysis to inform regulatory action. Public policies can be enacted at the county level, but implementation is not feasible at finer resolutions, such as the census tract or zip code level. There is currently no formal definition for AI counties. Thus, we used various sources to inform 3 classification schemes to characterize counties and county equivalents (henceforth referred to collectively as “counties”) with a substantial AI population. We classified counties as “AI-populated” if they fit at least 1 of the following criteria: (1) had greater than 5% population that self-identified as AI or Alaska Native alone in the 2010 Census (“census” classification)13; (2) contained at least 20% of their areas in a federally recognized tribal entity, defined as federally recognized reservations, off-reservation trust lands, and Census Oklahoma Tribal Statistical Areas (“Tribal entity” classification)14; or (3) were previously classified as a rural AI county in a cluster analysis of US counties using k-means clustering (“rural cluster” classification).15
We included this binary AI county type classification (yes/no) as the primary predictor variable of interest in all models. Details on the number of AI- and non–AI-populated counties by classification are provided in Table A (available as a supplement to the online version of this article at http://www.ajph.org). We restricted our main analysis to the 48 contiguous states and the District of Columbia, totaling 3108 study counties.
Air Pollution Data
We estimated the PM2.5 concentrations used in this analysis at the county level from both a satellite-based model and ground-monitoring data. Using PM2.5 monitoring data allows researchers to capture ground truth concentrations where data are available, whereas modeled PM2.5 provides more comprehensive spatial coverage across the entirety of the contiguous United States. We estimated annual county-level PM2.5 from a satellite-based surface PM2.5 model (henceforth referred to as “modeled PM2.5”), which provided comprehensive nationwide annual mean concentrations at approximately a 1 kilometer 1 kilometer grid resolution.16 The model interprets satellite retrievals of aerosol optical depth using its geophysical relationship to PM2.5, as simulated by the GEOS-Chem chemical transport model. The resulting geophysical PM2.5 surface is then calibrated using ground-based monitors via a geographically weighted regression.16,17 We estimated county-level modeled PM2.5 concentrations for every study year by averaging the PM2.5 concentrations in all grids with their centers contained in each US county.
To gain insights into PM2.5 concentrations in counties with adequate monitoring, we obtained annual PM2.5 concentrations measured by all available monitors (henceforth referred to as “measured PM2.5”); to do so, we used a federal reference method or a federal equivalent method from the EPA Air Quality System Database and Interagency Monitoring of Protected Visual Environments Rural Monitoring program between 2000 and 2018. These monitors collected data on a daily, 3-day, or 6-day schedule. We excluded PM2.5 monitors from analyses that had valid measurements for less than 75% of annually scheduled sampling days in our eligibility criteria when estimating county-level average measured PM2.5. We assessed measured PM2.5 in counties with more than 1 monitor by averaging the concentrations of all available monitors in the county boundaries for each study year.
Covariates
We obtained population density and median household income at the county level from the 2010 decennial US Census. We used these variables to estimate differences in air pollution estimates between AI- and non–AI-populated counties that were independent of how populated the counties were and their socioeconomic status. Given the highly skewed distribution of these variables (population density and income) across US counties, we used deciles of their distribution as categorical variables in the regression models.
Statistical Analysis
We used linear mixed effects regression to compare mean annual PM2.5 concentrations in AI- versus non–AI-populated counties. Our main analysis included 2 regression models, with either modeled or measured PM2.5 as the response variable. Both models included random intercepts for each state to account for potential within-state correlation of monitoring sites and nested random intercepts for counties in states to account for potential correlation of observations over time in counties.
We adjusted for covariates in a staggered manner. First, we included only year as a categorical predictor variable to account for possible nonlinear time trends in PM2.5 concentrations, together with random intercepts by county and state in the model (model 1). We further adjusted for population density in model 2 and additionally for median household income in model 3. Finally, we additionally included interaction terms between county type and each year indicator in model 4. To test for the presence of significant interaction between county type and year, indicating changes in annual PM2.5 trends over time by county type, we compared the model fit of models 3 and 4 and examined whether the interaction term for the factor year (df = 18) was statistically significant at a significance level of .05.
We conducted all statistical analyses using the R Statistical Software, version 3.6.3.18 All data and code to run analyses are publicly available and can be accessed here: https://github.com/maggie-mengyuan-li/native-air-pollution.git.
Sensitivity Analyses
To evaluate the robustness of our results, we conducted several sensitivity analyses. Because other factors beyond income might be needed to account for differences in socioeconomic factors across counties more comprehensively, we adjusted for the Area Deprivation Index (ADI)—a marker of socioeconomic differences widely used in health care research—instead of household income, in models 3 and 4.19,20 ADI uses 17 indicators of social and material conditions reflecting educational attainment, income and poverty, household composition, and vehicle and utilities access; higher values indicate greater neighborhood socioeconomic disadvantage.21 We estimated mean ADI per county by aggregating from block group ADI national percentile rankings. We excluded counties in the Northeastern United States in model 3, specifically EPA regions22 1, 2, and 3, as this region included only 2 AI-populated counties in the main analysis (Table B, a [available as a supplement to the online version of this article at http://www.ajph.org]).
Given the lack of an official definition denoting AI-populated areas, we ran 3 separate versions of model 3 using each of the 3 criteria to classify AI-populated counties, 1 separate version for AI-populated counties defined only by the intersection of all 3 classification schemes, and 1 separate version denoting AI-populated counties that included all study counties in our main analysis and additional counties with any overlap with a federally recognized tribal entity. We ran a restricted version of model 4 that excluded adjustment for median household income and population density. We additionally adjusted for US climate region as defined by the National Oceanic and Atmospheric Administration in models 3 and 4 to account for potential confounding by geographic area. We restricted analyses using models 3 and 4 to rural counties, defined as micropolitan and noncore counties by the National Center for Health Statistics, as 82% of AI-populated counties were classified like this in the main analysis (Table A, a).23 Finally, given the spatial autocorrelation of PM2.5 across counties, we conducted sensitivity analyses including a spatial lag term in models 3 and 4 using a queen contiguity-based spatial weights matrix.
RESULTS
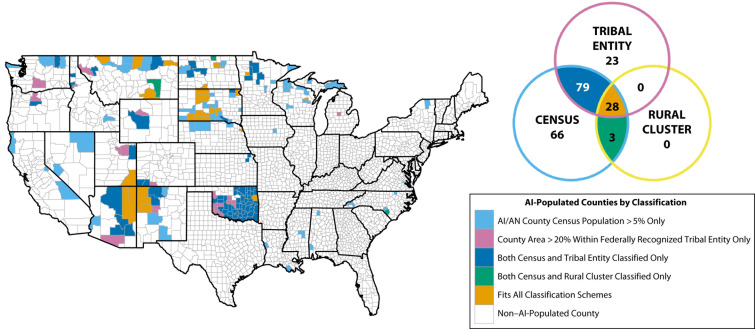
Using the classification criteria previously defined, we defined 6.4% (n = 199) of the 3108 total study counties as AI populated and the remaining 93.6% as non–AI populated (Table 1). Counties classified as AI populated were primarily located in the Midwestern, Southwestern, and Northwestern United States, with the remaining 14 in the Southeast and Northeast (Figure 1). Of the 199 counties classified as AI populated, 11.5% fulfilled the federally recognized tribal entity criteria exclusively, 33.2% fulfilled the census criteria exclusively, 14.1% fulfilled all 3 classification criteria, 1.5% fulfilled both the rural cluster and census criteria, and 39.7% fulfilled the census and federally recognized tribal entity criteria (Figure 1).
TABLE 1—
Descriptive Statistics for American Indian (AI)- and Non–AI-Populated Counties Overall and Among Those With Monitors: United States, 2000–2018
| Characteristic | All Counties | Counties With Monitorsa | ||
| AI | Non-AI | AI | Non-AI | |
| All counties | ||||
| No. of counties | 199 | 2909 | 71 | 766 |
| % AI population, mean (SD) | 18.2 (19.9) | 0.6 (0.6) | 16.0 (15.1) | 0.7 (0.8) |
| Modeled PM2.5 concentration, µg/m3, mean (SD) | 6.3 (2.1) | 8.4 (2.2) | 6.0 (2.2) | 8.6 (2.5) |
| Measured PM2.5 concentration,b µg/m3, mean (SD) | . . . | . . . | 7.0 (2.7) | 9.6 (2.8) |
| Population density, per mi2, mean (SD) | 41 (116) | 276 (1790) | 69 (180) | 787 (3400) |
| Median annual household income,$1000, mean (SD) | 40.4 (7.6) | 44.4 (11.6) | 42.0 (7.2) | 49.1 (12.6) |
| ADI,d 25th, 75th percentiles | 60.5, 83.3 | 56.7, 79.4 | 50.9, 77.3 | 44.5, 70.9 |
| Rural countiesc | ||||
| No. of counties | 163 | 1785 | 51 | 245 |
| % AI population, mean (SD) | 19.7 (20.7) | 0.6 (0.8) | 18.5 (16.3) | 0.9 (1.0) |
| Modeled PM2.5 concentration, µg/m3, mean (SD) | 6.2 (2.0) | 8.0 (2.3) | 5.8 (2.1) | 7.2 (2.5) |
| Measured PM2.5 concentrationb, µg/m3, mean (SD) | . . . | . . . | 6.5 (2.9) | 8.3 (3.1) |
| Population density, per mi2, mean (SD) | 19 (24) | 45 (99) | 25 (28) | 51 (51) |
| Median annual household income, $1000, mean (SD) | 39.1 (7.3) | 40.0 (8.1) | 40.3 (7.1) | 42.5 (9.6) |
| ADI, 25th, 75th percentilesd | 64.1, 84.2 | 65.7, 82.5 | 49.5, 78.1 | 52.7, 78.0 |
Note. ADI = Area Deprivation Index; PM2.5 = fine particulate matter.
aCounties with at least 1 year with monitored PM2.5 data over the study period.
bMeasured PM2.5 concentrations were only assessed in counties with monitors. Analyses involving measured PM2.5 included only counties with monitors during the study period, whereas modeled PM2.5 analyses included all counties.
cMicropolitan and noncore counties defined by the Centers for Disease Control and Prevention National Center for Health Statistics (i.e., nonmetropolitan counties).
dHigher values indicate higher levels of neighborhood disadvantage.
FIGURE 1—
Map and Venn Diagram of American Indian (AI)-Populated Counties Across the United States: 2000–2018
Note. AN = Alaska Native.
Most counties included in our analysis were rural (Table 1). Of the 199 US counties classified as AI populated, 163 (82%) were rural, and of the 2909 US counties classified as non–AI populated 1785 (61%) were rural. On average, in counties classified as AI populated, 18.2% of the population was AI versus 0.6% in non–AI-populated counties. The mean modeled PM2.5 concentrations for 2000 through 2018 were 6.3 micrograms per cubic meter and 8.4 micrograms per cubic meter for AI-populated counties and non–AI-populated counties, respectively, whereas the corresponding measured PM2.5 concentrations were 7.0 micrograms per cubic meter and 9.6 micrograms per cubic meter, respectively (Table 1). Distributions for population density, household income, and ADI by AI-populated county type and rurality are provided in Table 1.
Using linear mixed effects regression models, we observed significantly lower modeled and measured mean PM2.5 concentrations in AI- versus non–AI-populated counties on average across the study period (Table 2). In our fully adjusted model with main effects only (model 3), modeled PM2.5 was on average 0.38 (95% CI = 0.23, 0.54) micrograms per cubic meter lower, and measured PM2.5 was on average 0.79 (95% CI = 0.33, 1.26) micrograms per cubic meter lower in AI- than in non–AI-populated counties (Table 2).
TABLE 2—
Mean Difference in Modeled and Measured PM2.5 Concentrations (μg/m3) in American Indian (AI)-Populated vs Non–AI-Populated Counties: United States, 2000–2018
| Model 1,a Mean Difference (95% CI) | Model 2,b Mean Difference (95% CI) | Model 3,c Mean Difference (95% CI) | |
| Modeled PM2.5 | −0.56 (−0.74, −0.38) | −0.36 (−0.52, −0.21) | −0.38 (−0.54, −0.23) |
| Measured PM2.5 | −1.65 (−2.18, −1.13) | −0.70 (−1.17, −0.22) | −0.79 (−1.26, −0.33) |
Note. CI = confidence interval; PM2.5 = fine particulate matter.
aAdjusted only for year and random intercepts for counties in states.
bAdditionally adjusted for population density.
cAdditionally adjusted for population density and median household income.
Overall, we observed that modeled and measured mean PM2.5 concentrations decreased in all states over time, with high variability in the rate of decline across states (Figure A, light-colored thin lines [available as a supplement to the online version of this article at http://www.ajph.org]). Over the study period, PM2.5 concentrations decreased more in non–AI-populated than in AI-populated counties across all states for both modeled and measured PM2.5 (Figure A, bold dashed lines). When we compared models 3 and 4, we detected the presence of a statistically significant interaction between county type and year (P < .001). We visually compared modeled and measured PM2.5 levels using estimated values from model 4 across county types for a hypothetical county with a fixed population density and median annual household income (Figure A, bold solid lines). Using all input data and model 4, we predicted that across the study period, PM2.5 concentrations in AI-populated counties decreased by 2.13 and 2.37 micrograms per cubic meter (22.7% and 23.3% relative decline) on average for modeled and measured PM2.5, respectively; in non–AI-populated counties, the corresponding declines were 4.26 and 5.05 micrograms per cubic meter (39.2% and 42.0%), respectively (Figure A).
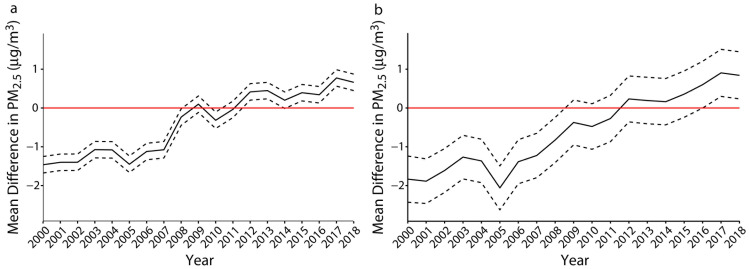
Given the observed interaction, modeled and measured PM2.5 (both estimated and observed annual means) were significantly lower in AI- than in non–AI-populated counties at the beginning of the study period, but this difference decreased in magnitude over time (Figure A). Adjusted mean concentrations were 1.46 (95% CI = 1.25, 1.68) micrograms per cubic meter lower for modeled PM2.5, and 1.83 (95% CI = 1.24, 2.43) micrograms per cubic meter lower for measured PM2.5 in AI-populated counties versus non–AI-populated counties in 2000 (Figure 2). Partway through the study period, mean PM2.5 concentrations in AI-populated counties became significantly higher than in non–AI-populated counties after 2012 for modeled PM2.5 and 2016 for measured PM2.5 (Figure 2). By 2018, adjusted modeled concentrations were on average 0.66 (95% CI = 0.45, 0.87) micrograms per cubic meter higher, and adjusted measured concentrations were on average 0.84 (95% CI = 0.24, 1.45) micrograms per cubic meter higher in AI-populated counties than in non–AI-populated counties (Figure 2).
FIGURE 2—
Adjusted Mean Difference in PM2.5 Concentrations Between American Indian (AI)- and Non–AI-Populated Counties That Are (a) Modeled, and (b) Measured: 2000–2018
Note. PM2.5 = fine particulate matter. The solid line shows the effect estimates (county type coefficient + interaction coefficient with time) of being classified as an AI-populated county over the study period. The dashed lines show the 95% confidence intervals from model 4. The red line represents no difference in adjusted average PM2.5 concentrations between AI and non–AI-populated counties.
Overall, our findings comparing PM2.5 concentrations averaged over time in AI- versus non–AI-populated counties did not change considerably when we adjusted for ADI instead of household income, excluded counties in the Northeast, defined AI-populated counties using each criteria separately and the intersection of all 3 criteria, included additional counties with any overlap with federally recognized tribal entities in our definition of AI-populated counties, additionally adjusted for climate region, and restricted analyses to rural counties (Table C [available as a supplement to the online version of this article at http://www.ajph.org]). Our findings comparing PM2.5 trends over time in model 4 remained consistent when we adjusted for ADI instead of household income and excluded household income and population density, additionally adjusted for climate region, and restricted to rural counties (Figure B [available as a supplement to the online version of this article at http://www.ajph.org]). When including a spatial lag in models 3 and 4, modeled PM2.5 was on average much lower in AI-populated counties compared with our main analysis results (Table C). Mean concentrations were substantially lower in AI- than in non–AI-populated counties at the beginning of the study period, but the mean difference by county type was attenuated over time, with no difference or even a potential increase in annual PM2.5 levels in AI- versus non–AI-populated counties by the end of the study period (Figure B).
DISCUSSION
We compared differences in modeled and measured PM2.5 concentrations between AI- and non–AI-populated US counties from 2000 to 2018. Although we observed that PM2.5 concentrations were lower in AI-populated counties at baseline and on average across the study period, this gap between AI- and non–AI-populated counties decreased over time. We observed higher PM2.5 concentrations in AI-populated counties than in non–AI-populated counties after approximately 2015. In sensitivity analyses using spatial lag linear mixed models, we observed substantially lower PM2.5 levels on average across the study period in AI-populated counties. Trends over time also showed lower concentrations in AI-populated counties near the beginning of our study period, although this difference was attenuated by the end of the study period.
We observed a larger difference on average over the study period in annual PM2.5 concentrations between AI- and non–AI-populated counties for measured versus modeled PM2.5. EPA monitors are not uniformly distributed and tend to be in more populous counties and more densely populated areas in a county, which also tend to have higher pollution levels than other areas in the same county; thus, the measured PM2.5 analysis may not fully represent capturing true differences in county-level average PM2.5 concentrations by AI-populated county type. The model, by contrast, provided PM2.5-predicted concentrations at a uniform spatial resolution, consistent with lower countywide average PM2.5 compared with measured concentrations at monitoring stations. Modeled data, however, can also be affected by measurement error, if the model yields less accurate predictions in areas where fewer monitors are available.
The varying trend in mean PM2.5 concentrations over time between AI-populated and non–AI-populated counties may reflect the spatial heterogeneity of changing PM2.5 levels across the continental United States in the past several decades. One study ranked US Census tracts by PM2.5 concentrations in 1981 and 2016 and found that census tracts in states bordering the Great Lakes and the Northeastern United States dropped in PM2.5 percentile rank relative to other areas; meanwhile, the Central and Imperial valleys of California, southwestern Arizona, and areas of Oklahoma, Arkansas, and Texas experienced increases in the relative ranking of PM2.5 between 1981 and 2016.24 However, we found similar results after adjusting for climate regions; future analyses restricted to specific regions should be considered to understand drivers of within–climate region differential PM2.5 trends in AI- versus non–AI-populated counties.
Given that exposure to PM2.5 is a modifiable risk factor for cardiovascular disorders and other adverse health outcomes even at levels below the current national ambient air quality standards,25 it is important to characterize exposure patterning over space, particularly in areas with socioeconomically disadvantaged populations. The history of US settler colonialism has contributed to the displacement of tribes and forced acculturation of Native children to Western educational and sociocultural systems.26,27 These factors have exacerbated levels of poverty, poor health, and chronic diseases in this population.28 To this day, access to quality health care is still a challenge for AI people. Most rely on Indian Health Services as their primary health care provider. Lack of funding has forced Indian Health Services to regularly operate in a “state of emergency,” with a per capita spending on personal health care at half the national average expenditure.29 With potentially higher estimated PM2.5 concentrations in AI-populated counties than in other counties observed in recent years, or at least diminished differences by county type over time, it is imperative to recognize that these trends may further increase health disparities between AI people and other populations.
Cardiovascular disease, one of the outcomes positively associated with exposure to PM2.5, is the leading cause of death in AI populations and occurs at significantly higher rates than in White populations.30,31 Studies in the Strong Heart Study cohort—the largest and longest-running longitudinal study assessing cardiovascular outcomes and their risk factors in AI communities in Arizona, Oklahoma, and North and South Dakota—showcase the high burden of cardiovascular disease, which is associated with a high prevalence of diabetes and obesity.32–35 Because the role of air pollution in the cardiovascular health of AI people, to our knowledge, has not yet been evaluated, using the Strong Heart Study and similar cohorts can serve as invaluable resources for future investigations of health impacts associated with air pollution in AI populations.
Limitations
There are a few limitations to this analysis. Given the many modes of defining AI populations,7 demarcating AI- or non–AI-populated counties can only estimate, but not fully capture, the extent of where AI people reside. We adjusted for population density and median household income and ADI as indicators of socioeconomic status to characterize differences in PM2.5 levels in AI- versus non–AI-populated counties independently of these factors. However, we cannot exclude the possibility of potential residual confounding. The lack of PM2.5 monitors in the sparsely populated rural United States restricts our ability to assess measured PM2.5 in most AI- and non–AI-populated counties. These monitors are not uniformly distributed in space, and the somewhat arbitrary delineation of county boundaries makes the measured PM2.5 analysis prone to bias because of zonation effects of the modifiable areal unit problem.36 Although the use of PM2.5 models provides comprehensive spatial coverage across the United States, there is likely some error associated with these predictions. Future studies should incorporate different prediction models to perform analyses that can further validate these findings. By aggregating PM2.5 estimates and conducting our analyses at the county level, we cannot generalize our findings to differences in individual exposure levels between AI- and non-AI people.
Our study was limited to the contiguous United States, notably excluding Hawaii and Alaska. Native Hawaii and Alaska Native populations tend to be more uniformly distributed across these states,37,38 as opposed to AI communities being relatively concentrated geographically in the lower 48 states. This difference between these 2 states and the rest of the United States requires a separate analysis. Potentially, future studies at finer spatial resolutions in these areas may be able to elucidate the pollution disparities between these Alaska Natives and Native Hawaiians and non-Native communities. Finally, our study assessed only total PM2.5; future studies should evaluate potential differences in concentrations of PM2.5 components and other pollutants in AI- versus non–AI-populated counties.
Conclusions
The differential rates of PM2.5 decline and attenuated PM2.5 differences over time between AI- and non–AI-populated counties necessitates further investigation. Our findings suggest that socioeconomically disadvantaged communities experience disproportionate burdens of environmental hazards, such as ambient air pollution, contributing to adverse downstream health effects.39 The substantially larger decrease in PM2.5 concentrations in non–AI- versus AI-populated counties highlights a need to enhance enforcement of air quality regulations and restrictions to PM2.5 emissions on tribal territories, surrounding regions, and other areas with large populations of AI people. Given current research gaps, AI populations are likely underrepresented when the EPA is considering national ambient air quality standards. Greater resources should be allocated to creating mutual learning opportunities among researchers, federal and state agencies, and local tribal governments to spur further research to ensure that the national ambient air quality standards are indeed protecting everyone. Efforts should also prioritize the establishment of more permanent funding streams and institutional infrastructure to promote developments of successful long-term regulatory efforts in tribal communities.
ACKNOWLEDGMENTS
Support for this work was provided by the National Institute of Environmental Health Sciences, National Institutes of Health (NIH; grants T32 ES007322, P30 ES09089, R01 ES030616, and P42 ES010349).
Note. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
CONFLICTS OF INTEREST
The authors declare no potential or actual conflicts of interest.
HUMAN PARTICIPANT PROTECTION
No protocol approval was necessary because data were obtained from secondary sources.
REFERENCES
- 1.Feng S, Gao D, Liao F, Zhou F, Wang X. The health effects of ambient PM2.5 and potential mechanisms. Ecotoxicol Environ Saf. 2016;128:67–74. doi: 10.1016/j.ecoenv.2016.01.030. [DOI] [PubMed] [Google Scholar]
- 2.Kappos AD, Bruckmann P, Eikmann T, et al. Health effects of particles in ambient air. Int J Hyg Environ Health. 2004;207(4):399–407. doi: 10.1078/1438-4639-00306. [DOI] [PubMed] [Google Scholar]
- 3.Lu F, Xu D, Cheng Y, et al. Systematic review and meta-analysis of the adverse health effects of ambient PM2.5 and PM10 pollution in the Chinese population. Environ Res. 2015;136:196–204. doi: 10.1016/j.envres.2014.06.029. [DOI] [PubMed] [Google Scholar]
- 4.Bowe B, Xie Y, Yan Y, Al-Aly Z. Burden of cause-specific mortality associated with PM2.5 air pollution in the United States. JAMA Netw Open. 2019;2(11):e1915834. doi: 10.1001/jamanetworkopen.2019.15834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miranda ML, Edwards SE, Keating MH, Paul CJ. Making the environmental justice grade: the relative burden of air pollution exposure in the United States. Int J Environ Res Public Health. 2011;8(6):1755–1771. doi: 10.3390/ijerph8061755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jacobs-Wingo JL,, Espey DK, Groom AV, Phillips LE, Haverkamp DS. Causes and disparities in death rates among urban American Indian and Alaska Native populations, 1999–2009. Am J Public Health. 2016;106(5):906–914. doi: 10.2105/AJPH.2015.303033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vickery J, Hunter LM. Native Americans: where in environmental justice research? Soc Nat Resour. 2016;29(1):36–52. doi: 10.1080/08941920.2015.1045644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jones DS. The persistence of American Indian health disparities. Am J Public Health. 2006;96(12):2122–2134. doi: 10.2105/AJPH.2004.054262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lewis J, Hoover J, MacKenzie D. Mining and environmental health disparities in Native American communities. Curr Environ Health Rep. 2017;4(2):130–141. doi: 10.1007/s40572-017-0140-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clark LP, Millet DB, Marshall JD. Changes in transportation-related air pollution exposures by race-ethnicity and socioeconomic status: outdoor nitrogen dioxide in the United States in 2000 and 2010. Environ Health Perspect. 2017;125(9):097012. doi: 10.1289/EHP959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Di Q, Wang Y, Zanobetti A, et al. Air pollution and mortality in the Medicare population. N Engl J Med. 2017;376(26):2513–2522. doi: 10.1056/NEJMoa1702747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Watson JG, Chow JC, DuBois D, Green M, Frank N, Pitchford M. Guidance for network design and optimum site exposure for PM2.5 and PM10. December 15, 1997. Available at: https://www3.epa.gov/ttnamti1/files/ambient/pm25/network/r-99-022.pdf2022
- 13.Census Data API. Variables in /data/2010/dec/sf1/variables. 2021. https://api.census.gov/data/2010/dec/sf1/variables.html
- 14.Data.gov. 2017. https://catalog.data.gov/dataset/tiger-line-shapefile-2017-nation-u-s-current-american-indian-tribal-subdivision-aits-national
- 15.Wallace M, Sharfstein JM, Kaminsky J, Lessler J. Comparison of US county-level public health performance rankings with county cluster and national rankings: assessment based on prevalence rates of smoking and obesity and motor vehicle crash death rates. JAMA Netw Open. 2019;2(1):e186816. doi: 10.1001/jamanetworkopen.2018.6816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Donkelaar A, Martin RV, Li C, Burnett RT. Regional estimates of chemical composition of fine particulate matter using a combined geoscience-statistical method with information from satellites, models, and monitors. Environ Sci Technol. 2019;53(5):2595–2611. doi: 10.1021/acs.est.8b06392. [DOI] [PubMed] [Google Scholar]
- 17.Hammer MS, van Donkelaar A, Li C, et al. Global estimates and long-term trends of fine particulate matter concentrations (1998–2018) Environ Sci Technol. 2020;54(13):7879–7890. doi: 10.1021/acs.est.0c01764. [DOI] [PubMed] [Google Scholar]
- 18.R Core Team. 2022. https://www.R-project.org
- 19.Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible—the Neighborhood Atlas. N Engl J Med. 2018;378(26):2456–2458. doi: 10.1056/NEJMp1802313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.University of Wisconsin School of Medicine and Public Health. 2021. https://www.neighborhoodatlas.medicine.wisc.edu
- 21.Singh GK. Area deprivation and widening inequalities in US mortality, 1969–1998. Am J Public Health. 2003;93(7):1137–1143. doi: 10.2105/ajph.93.7.1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.US Environmental Protection Agency. 2020. https://www.epa.gov/aboutepa/regional-and-geographic-offices [PubMed]
- 23.Rothwell CJ, Madans JH, Arispe IE. 2013 NCHS urban–rural classification scheme for counties. Vital Health Stat 2. 2014;(166) https://www.cdc.gov/nchs/data/series/sr_02/sr02_166.pdf [PubMed] [Google Scholar]
- 24.Colmer J, Hardman I, Shimshack J, Voorheis J. Disparities in PM2.5 air pollution in the United States. Science. 2020;369(6503):575–578. doi: 10.1126/science.aaz9353. [DOI] [PubMed] [Google Scholar]
- 25.Papadogeorgou G, Kioumourtzoglou M-A, Braun D, Zanobetti A. Low levels of air pollution and health: effect estimates, methodological challenges, and future directions. Curr Environ Health Rep. 2019;6(3):105–115. doi: 10.1007/s40572-019-00235-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Edgerly CC, Laing SS, Day A-VG, et al. Strategies for implementing health promotion programs in multiple American Indian communities. Health Promot Pract. 2009;10(2 suppl):109S–117S. doi: 10.1177/1524839908331270. [DOI] [PubMed] [Google Scholar]
- 27.Evans-Campbell T. Historical trauma in American Indian/Native Alaska communities: a multilevel framework for exploring impacts on individuals, families, and communities. J Interpers Violence. 2008;23(3):316–338. doi: 10.1177/0886260507312290. [DOI] [PubMed] [Google Scholar]
- 28.Lowe AA, Bender B, Liu AH, et al. Environmental concerns for children with asthma on the Navajo Nation. Ann Am Thorac Soc. 2018;15(6):745–753. doi: 10.1513/AnnalsATS.201708-674PS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Merewood A. Baby-friendly and the Indian Health Service: a new standard of care. J Hum Lact. 2015;31(2):207–208. doi: 10.1177/0890334415570029. [DOI] [PubMed] [Google Scholar]
- 30.Breathett K, Mario S, Marie G, et al. Cardiovascular health in American Indians and Alaska Natives: a scientific statement from the American Heart Association. Circulation. 2020;141(25):e948–e959. doi: 10.1161/CIR.0000000000000773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Espey DK, Jim MA, Cobb N, et al. Leading causes of death and all-cause mortality in American Indians and Alaska Natives. Am J Public Health. 2014;104(S3, suppl 3):):S303–S311. doi: 10.2105/AJPH.2013.301798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Capaldo B, Di Bonito P, Iaccarino M, et al. Cardiovascular characteristics in subjects with increasing levels of abnormal glucose regulation: the Strong Heart Study. Diabetes Care. 2013;36(4):992–997. doi: 10.2337/dc12-1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Eilat-Adar S, Mete M, Fretts A, et al. Dietary patterns and their association with cardiovascular risk factors in a population undergoing lifestyle changes: the Strong Heart Study. Nutr Metab Cardiovasc Dis. 2013;23(6):528–535. doi: 10.1016/j.numecd.2011.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moon KA, Guallar E, Umans JG, et al. Association between exposure to low to moderate arsenic levels and incident cardiovascular disease. A prospective cohort study. Ann Intern Med. 2013;159(10):649–659. doi: 10.7326/0003-4819-159-10-201311190-00719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tellez-Plaza M, Guallar E, Howard BV, et al. Cadmium exposure and incident cardiovascular disease. Epidemiology. 2013;24(3):421–429. doi: 10.1097/EDE.0b013e31828b0631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Openshaw S. The Modifiable Areal Unit Problem. Norwich, UK: Geobooks; 1984. [Google Scholar]
- 37.State of Hawaii Research and Economic Analysis Division. Hawaii population characteristics 2019. 2021. https://census.hawaii.gov/wp-content/uploads/2020/06/Hawaii-Population-Characteristics-2019.pdf
- 38.Walker B, Drygas H, Robinson D, Hunsinger E, Howell D, Sandberg E.2021. https://live.laborstats.alaska.gov/pop/estimates/pub/13popover.pdf
- 39.Mohai P, Pellow D, Roberts JT. Environmental justice. Annu Rev Environ Resour. 2009;34:405–430. doi: 10.1146/annurev-environ-082508-094348. [DOI] [Google Scholar]