Abstract
Objectives. To estimate differences in breastfeeding initiation (BFI) rates between African Americans and Black immigrants enrolled in the District of Columbia Special Supplemental Nutrition Program for Women, Infants and Children (WIC) between 2007 and 2019.
Methods. We used data collected as part of routine WIC program activities for first-time mothers (n = 38 142). Using multivariable logistic regression models, we identified determinants of BFI for African Americans, Black immigrants, non-Hispanic Whites, and Hispanics. To assess the trend in BFI over time, we calculated the average of the annual percentage changes.
Results. Compared with African Americans, Black immigrants had a 2.7-fold higher prevalence and Hispanics had a 5.8-fold higher prevalence of BFI. The average of the annual percentage changes was 0.85 for Hispanics, 3.44 for Black immigrants, 4.40 for Non-Hispanic Whites, and 4.40 for African Americans. African Americans had the only statistically significant change (P < .05). Disparities in BFI persisted over the study period, with African Americans demonstrating the lowest rates each year.
Conclusions. Significant differences exist in BFI between Black immigrants and African Americans. Combining African Americans and Black immigrants masks important differences, overestimates rates among African Americans, and may lead to missed opportunities for targeting interventions and policies to improve breastfeeding. (Am J Public Health. 2022;112(4):671–674. https://doi.org/10.2105/AJPH.2021.306652)
Breastfeeding reduces the risk for sudden infant death syndrome, infectious diseases, asthma, obesity, and type 2 diabetes in infants and children, and for breast and ovarian cancer in women who breastfed, all of which disproportionately affect African American populations.1 Healthy People 2020’s target for breastfeeding initiation (BFI; 81.9%) was met nationally by the year 2014, but not by all racial/ethnic groups.2 Persistent disparities by race/ethnicity remain; the Centers for Disease Control and Prevention’s most recently reported data show that BFI is lowest among non-Hispanic Blacks, which, at 73.7%, falls short of the Healthy People 2020 target.3
However, current federal race/ethnicity classifications are problematic because they may mask potentially important differences in health behaviors and outcomes among the Black American population.4 For example, a recent systematic review of breastfeeding practices of Black immigrants residing in high-income countries provides evidence of high BFI (90%).5 Others report statistically greater odds of BFI among Black immigrants than among nonimmigrant Blacks in the United States.6–8 Without detailed data by race/ethnicity, the potential for poorly targeted interventions and policies exists, and opportunities to improve breastfeeding may be missed. We did not find any literature estimating BFI differences between Black American subgroups of women in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). Our objective was to estimate BFI rate differences between African Americans and Black immigrants enrolled in the District of Columbia WIC program over time.
METHODS
We conducted a secondary analysis of de-identified data collected as part of routine WIC program activities in the District of Columbia WIC program. We extracted data for all mothers who gave birth to a first child, singleton infant between January 1, 2007 and December 31, 2019 (n = 38 142). The final models consisted of all women with breastfeeding behavior data specified and no missing responses for the independent variables included (n = 35 108).
Outcome
We determined the outcome, BFI (yes or no), using WIC food package issuance data, a valid indicator for breastfeeding behavior.9 At the first WIC site visit following the infant’s birth, WIC staff collect breastfeeding behavioral data to determine eligibility for WIC benefit issuance (i.e., receipt of food package for the mother, formula, or both).
Determinants
We based selected sociodemographic and other potential determinants on a literature review, which included maternal age (aged ≤ 20, 21–30, 31–45, or ≥ 46 years), education (< high school, high school graduate or equivalent, and > high school education), maternal marital status (married or unmarried), household size (1–2, 3–4, 5–6, or ≥ 7), low birth weight status (yes or no), year of participation (continuous variable), and race/ethnicity (non-Hispanic White, Hispanic, and Black, which included 2 subgroups: African American and Black immigrants). We defined African Americans as those self-reporting as African American, not Hispanic, and speaking English only. We defined Black immigrants as those self-reporting as African American, not Hispanic, and speaking a language other than English.10
Statistical Analysis
We conducted bivariate analyses between the outcome (BFI) and each of the potential determinants, and between pairs of sociodemographic variables to assess their relation and multicollinearity. We included variables associated with BFI in the bivariate analysis (P < .05) or that we found important from the literature in the final models. Using a multivariable logistic regression model, we estimated adjusted odds ratios (AORs) and 95% confidence intervals (CIs) between BFI and potential determinants. To assess the trend over time in BFI, we calculated the average of the annual percentage changes (AAPC). We tested the hypothesis of whether the true average was greater than zero based on a 2-sided t test. We conducted all analyses with Stata version 16 (StataCorp, LP, College Station, TX).
RESULTS
Almost half of the sample was aged 21 to 30 years (50.4%), possessed a high school degree or equivalent (45.0%), and lived in a household of 3 to 4 people (46.7%). Most were unmarried (89.2%) and 10.0% gave birth to a low birth weight baby. The number of women enrolled in WIC each year decreased over time, from 2426 in 2007 to 2210 in 2019. The largest racial/ethnic group was the Black subgroup of African American (74.8%), followed by Hispanic (16.9%), the Black subgroup of Black immigrant (6.0%), and non-Hispanic White (2.0%).
The average BFI rate was 48.6%. It was highest among Hispanics (77.7%), followed by Black immigrants (69.6%), non-Hispanic Whites (60.9%), and finally African Americans (39.9%). In the multivariable analysis, married compared with unmarried recipients and recipients with more than a high school education compared with those with less education had a significantly higher prevalence of BFI (Table A, available as a supplement to the online version of this article at http://www.ajph.org). Recipients in the youngest and oldest age groups had a significantly lower prevalence of BFI than did those aged 21 to 45 years. Those who gave birth to a low birth weight baby and recipients who lived in households with 7 or more people compared with smaller households had a significantly lower prevalence of BFI.
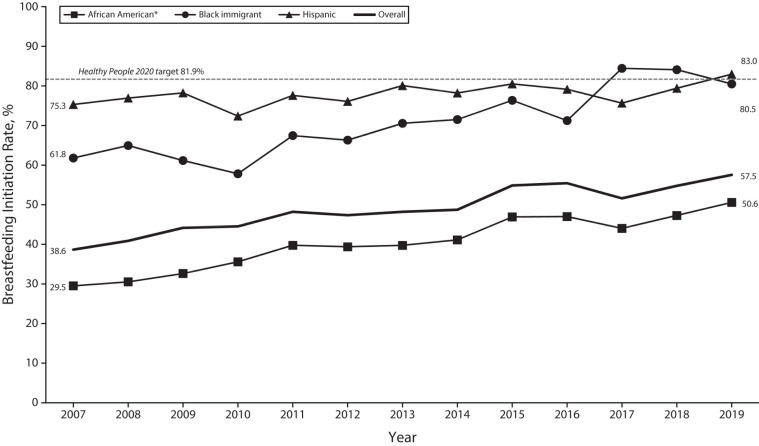
A significant increase in BFI occurred over the 13-year study period (AOR = 1.06; 95% CI = 1.05, 1.06). Race/ethnicity demonstrated the strongest association with the outcome. Compared with African Americans, Hispanics had a 5.8-fold higher prevalence of BFI and Black immigrants had a 2.7-fold higher prevalence. The AAPC was 0.85 for Hispanics, 3.44 for Black immigrants, 4.40 for non-Hispanic Whites, and 4.40 for African Americans; the last group was the only one with a statistically significant change (P < .05; Figure 1). Disparities in BFI persisted over the study period, with African Americans demonstrating the lowest rates each year (Figure 1).
FIGURE 1—
Breastfeeding Initiation Rate (%) by Race/Ethnicity With Black Subgroups in the District of Columbia Special Supplemental Nutrition Program for Women, Infants and Children (WIC) population: 2007–2019
Note. AAPC = average annual percentage change. The sample size was n = 36 015. AAPC in rate, 2007–2019: Hispanic = 0.92; Black immigrant = 2.78; and African American = 4.51 (P < .05). Non-Hispanic Whites not shown because of low numbers.
DISCUSSION
We uncovered significant differences in BFI between Black immigrants and African Americans enrolled in the District of Columbia WIC program. These results align with the literature, with findings of higher BFI for Black immigrants than for African Americans.6–8 Overall, BFI increased significantly over time in the study population, mirroring the national temporal trend,2 but at lower prevalence rates. This is similar to national data on WIC recipients compared with the general US population.3 Differentiating between African Americans and Black immigrants showed a significant annual increase in BFI among African Americans but a modest, statistically nonsignificant increase in all other groups.
As with most program data, inherent limitations exist. WIC data are collected to evaluate program impact on breastfeeding and other health and nutrition outcomes and to adjust the issuance of WIC benefits recipients receive (i.e., not for research purposes). Potential self-report bias may include underreporting breastfeeding behavior to obtain formula vouchers or overreporting to receive additional maternal food package issuance. Using primary language spoken at home to identify Black immigrants may underestimate this population, particularly in the District of Columbia, where some Black immigrants may come from English-language countries.10
Differentiating Black American WIC recipients by primary language spoken at home allowed us to conduct this study of WIC recipients. Our findings add to the literature on the importance of differentiating between racial/ethnic subgroups when evaluating behaviors, health, and development outcomes.4,7,11,12 This is the first study, to our knowledge, to examine Black American subgroups enrolled in WIC. WIC and other federal programs can employ similar methods to evaluate the reach and impact of their programs using readily available data that may include language spoken at home or place of birth.
PUBLIC HEALTH IMPLICATIONS
In our analysis of a diverse, low-income population enrolled in the District of Columbia WIC program over a 13-year period, African Americans experienced the lowest BFI rates, whereas Black immigrants demonstrated significantly higher rates. Combining African American and Black immigrant subgroups masks important differences and overestimates rates among African Americans. This in turn overestimates the impact of interventions, particularly among African Americans, and may lead to missed opportunities for targeting interventions and policies to improve breastfeeding.
ACKNOWLEDGMENTS
N. Ume was supported by a fellowship from the Clara Schiffer Project on Women’s Health.
The authors wish to thank the staff at the District of Columbia (DC) Department of Health, DC Women Infant Child State Agency, Washington, DC, for their assistance and support throughout the analysis.
Note. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the District of Columbia Department of Health.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare.
HUMAN PARTICIPANT PROTECTION
We conducted a secondary analysis of de-identified data collected as part of routine Special Supplemental Nutrition Program for Women, Infants and Children (WIC) program activities in the District of Columbia WIC program; thus the District of Columbia WIC institutional review board did not consider this study human participant research.
REFERENCES
- 1.Eidelman AI, Schanler RJ, Johnston M, et al. Breastfeeding and the use of human milk. Pediatrics. 2012;129(3):e827–e841. doi: 10.1542/peds.2011-3552. [DOI] [PubMed] [Google Scholar]
- 2.Office of Disease Prevention and Health Promotion. 2021. https://www.healthypeople.gov/2020
- 3.Centers for Disease Control and Prevention. 2021. https://www.cdc.gov/breastfeeding/data/nis_data/rates-any-exclusive-bf-sociodem-2017.html
- 4.Griffith DM, Johnson JL, Zhang R, Neighbors HW, Jackson JS. Ethnicity, nativity, and the health of American Blacks. J Health Care Poor Underserved. 2011;22(1):142–156. doi: 10.1353/hpu.2011.0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Odeniyi AO, Embleton N, Ngongalah L, Akor W, Rankin J. Breastfeeding beliefs and experiences of African immigrant mothers in high-income countries: a systematic review. Matern Child Nutr. 2020;16(3):e12970. doi: 10.1111/mcn.12970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Griswold MK, Crawford SL, Perry DJ, et al. Experiences of racism and breastfeeding initiation and duration among first-time mothers of the Black Women’s Health Study. J Racial Ethn Health Disparities. 2018;5(6):1180–1191. doi: 10.1007/s40615-018-0465-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hawkins SS, Gillman MW, Shafer EF, Cohen BB. Acculturation and maternal health behaviors: findings from the Massachusetts birth certificate. Am J Prev Med. 2014;47(2):150–159. doi: 10.1016/j.amepre.2014.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh GK, Kogan MD, Dee DL. Nativity/immigrant status, race/ethnicity, and socioeconomic determinants of breastfeeding initiation and duration in the United States, 2003. Pediatrics. 2007;119(suppl 1):S38–S46. doi: 10.1542/peds.2006-2089G. [DOI] [PubMed] [Google Scholar]
- 9.Whaley SE, Koleilat M, Jiang L. WIC infant food package issuance data are a valid measure of infant feeding practices. J Hum Lact. 2012;28(2):134–138. doi: 10.1177/0890334412436720. [DOI] [PubMed] [Google Scholar]
- 10.Fox M, Thayer Z, Wadhwa PD. Assessment of acculturation in minority health research. Soc Sci Med. 2017;176:123–132. doi: 10.1016/j.socscimed.2017.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hendi AS, Mehta NK, Elo IT. Health among Black children by maternal and child nativity. Am J Public Health. 2015;105(4):703–710. doi: 10.2105/AJPH.2014.302343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.López N. Killing two birds with one stone? Why we need two separate questions on race and ethnicity in the 2020 census and beyond. Lat Stud. 2013;11(3):428–438. doi: 10.1057/lst.2013.25. [DOI] [Google Scholar]