Abstract
Objective
To determine the benefits of aquatic physical therapy as a rehabilitation strategy for knee osteoarthritis patients.
Methods
Electronic databases systematically searched up to July 2021.
Results
580 RCTs were selected. A total of thirteen studies comprising 883 participants were included in the study. For pain, meta-analyses showed that aquatic physical therapy is associated with a significant change in Western Ontario and McMaster University Osteoarthritis Index (WOMAC) pain (SMD = − 1.09, 95%CI − 1.97, − 0.21, p = 0.02) and visual analog scale (VAS) (SMD = − 0.55, 95%CI − 0.98, − 0.12, p = 0.01). In addition, for physical function, meta-analyses showed that aquatic physical therapy effectively improved WOMAC physical function (SMD = − 0.57, 95%CI − 1.14, − 0.01, p = 0.05). However, our findings showed no significant improvements in symptoms of joints, quality of life (QOL), flexibility, and body composition with knee osteoarthritis. For muscle strength, we found that aquatic physical therapy can only improve knee extension muscle strength (MD = 2.11, 95%CI 0.02, 4.20, p = 0.05). Additionally, for walking ability, we observed that aquatic physical therapy effectively reduced Timed-Up-and-Go Test (TUGT) in a large degree (MD = − 0.89, 95%CI − 1.25, − 0.53, p < 0.05).
Conclusions
According to the findings reported in the studies analyzed in the review, aquatic physical therapy had a positive effect on the pain, physical function, knee extension muscle strength, and walking ability among people with knee osteoarthritis.
Keywords: Knee osteoarthritis, Aquatic physical therapy, Meta-analysis
Introduction
Osteoarthritis (OA) is the most prevalent form of arthritis and the main cause of disability in the older adults, and the knee is its most frequently affected weight-bearing joint [1]. This chronic and disabling condition not only reduces individual quality of life (QOL), but also exhausts a lot of health care resources and socioeconomic costs [1, 2]. Additionally, with the combined effects of aging, increasing obesity in the global population, and increasing numbers of joint injuries, the burden of osteoarthritis is becoming more common. According to global estimates, 250 million people are currently affected [3]. Therefore, there is an urgent need to explore methods of slowing down the progression of the disease.
The guidelines have strongly recommended that exercise is an effective non-pharmacological intervention for OA patients, which can relieve pain and enhance physical function [4]. Although both land and aquatic exercises can alleviate pain and improve the physical function of patients with OA [5], patients experience pain, stiffness, and muscle weakness during land exercises [6, 7], which limits their physical activity levels and leads them to a sedentary lifestyle [8, 9]. Correspondingly, lack of exercise will aggravate the progression of the disease.
In light of this, aquatic physical therapy would be an ideal form of physical activity for patients with OA. Because the buoyancy of water reduces the weight that joints, bones and muscles must bear [10], the warmth and pressure of water can also promote blood circulation and reduce joint pain and stiffness [11]. In addition, compared with other forms of treatments, aquatic physical therapy does not worsen joint condition [12] and leads to a higher level of treatment compliance [11]. And it is widely used as part of rehabilitation interventions for many diseases [13], such as rheumatic disease, fibromyalgia, stroke, and Parkinson disease [14–16].
There has been a meta-analysis of 11 trials for knee and hip OA patients and showed the positive effects of aquatic exercise on pain, stiffness, physical function, and QOL [17]. And another Cochrane review of 13 clinical trials also reached a similar conclusion [11]. However, a recent meta-analysis explored whether aquatic exercise is superior to land-based exercise in knee OA patients that showed comparable effects on the above outcomes [18]. Therefore, a consistent conclusion for the effect of aquatic physical therapy on knee OA alone could not be drawn [11]. Further, lack of sufficient evidence for the benefits of aquatic physical therapy, which limits recommendation on knee OA.
Although pain is the most prominent symptom of knee OA, it is often associated with other functional impairments, such as muscle weakness, reduced joint range of motion (ROM) and joint instability [12]. So the purposes of exercise in knee OA are not only to reduce pain and stiffness and restore impaired physical function and functional status, but also to improve ROM and maintain joint function and integrity. Additionally, Bliddal and Christensen reported that a 10% reduction in body weight could reduce OA symptoms by 28% [19], and it is necessary to investigate the effectiveness of aquatic physical therapy on body fat. Therefore, in addition to including pain, symptoms of joints, physical function, and QOL, we also included outcome measures of flexibility, muscle strength, walking ability, and body composition would provide a more comprehensive picture of the therapeutic value associated with aquatic physical therapy. For this purpose, we performed a systematic review and meta-analysis of randomized controlled trials (RCTs) to evaluate overall treatment effects of aquatic physical therapy in knee OA.
Materials and methods
This is a meta-analysis of randomized trials involving the overall treatment effect of aquatic physical therapy in knee OA. The systematic review and meta-analysis were reported in accordance with the recommendations of the Preferred Reporting Items for Systematic Review and Meta-Analyses: The PRISMA Statement and Cochrane Handbook for Systematic Reviews of Interventions [20, 21]. The selected search strategy and methods of analysis were registered at the PROSPERO database (ref: CRD42021267364).
Search strategy
We searched the following databases including Medline/PubMed, Web of Science, Embase, Cochrane Library and Chinese databases of the CNKI Scholar, VIP and WanFang. The relevant studies were searched from the inception of each database to July 2021. The search terms and strategy used were as follows: (hydrotherapy OR aquatic exercise OR water-based exercise) AND (osteoarthrosis OR arthritis degenerative OR arthritis) AND (randomized controlled trial OR RCT). Additionally, to search all relevant studies, the reference lists were also manually reviewed.
Inclusion and exclusion criteria
The study inclusion criteria were as follows: (1) participants have a clinical diagnosis of knee OA; (2) participants aged ≥ 40 years; (3) participants have no medical conditions that prevent increased physical activities; (4) participants have not participated in an organized exercise program in the past 3 months; (5) during the intervention period, participants can actively participate in the treatment; (6) at least one group of intervention methods was aquatic physical therapy; (7) the study was reported at least one of the outcomes: pain, symptoms of joints, physical function, QOL, flexibility, muscle strength, walking ability, and body composition; (8) the type of study design was the RCT. Studies were excluded if (1) the type of article was conference abstracts, case reports, comments, letters to editor, review articles, or family-based studies; (2) the full text of the study was not available; (3) studies without available data; (4) the type of study design was not the RCT.
Data extraction and quality assessment
Two independent researchers screened all abstracts identified in the initial search, excluded studies that violated the inclusion criteria, and removed all the duplicated references. If it was unclear whether the study met the selection criteria, advice could be sought from a third researcher and a consensus of opinion was made.
Information on first author and publication year, country, sample size, exercise type of experimental group and control group, intervention time, follow-up time and outcomes measures were extracted from the original reports. The quality of the trials included was assessed by the two independent researchers according to the Cochrane Collaboration Handbook recommendations and items such as: randomization, allocation concealment, blinding, incomplete outcome data and selective reporting [21].
It means low risk if the thesis clearly described, high risk if not described and unclear if described indeterminate in the text. Researchers achieved consensus by discussion, and if researchers didn't achieve, a third reviewer was consulted.
Outcome measures
The main outcomes that were examined included: pain, symptoms of joints, physical function, QOL, flexibility, muscle strength, and walking ability and body composition. Across the studies, Western Ontario and McMaster University Osteoarthritis Index (WOMAC) pain, visual analog scale (VAS) score, and Knee Injury and Osteoarthritis Outcome Score (KOOS) pain were used to measure pain. Symptoms of joints were measured by the WOMAC stiffness and KOOS for symptoms. Physical function was measured by using the KOOS for activities of daily living (ADL), KOOS for sport/recreation, WOMAC physical function, and the medical outcomes study short form-36 (SF-36) physical function. QOL was measured by using the KOOS for QOL. Flexibility was measured by tests of joint range of motion (ROM) of knee extension and knee flexion. Knee extension and flexion and hip abduction muscle strength were used to measure muscle strength. Walking ability was quantified by the 6-min walk test (6MWT), walking speed, step test, or the Timed-Up-and-Go Test (TUGT). Body composition was evaluated by the body mass index (BMI) or the fat mass.
Statistical analysis and risk of bias assessment
The data were analyzed by RevMan software (version 5.4.1). A meta-analysis intended to carry out RCTs, if the same outcomes had been assessed in at least two studies in a similar way, and at least one group received aquatic physical therapy. The mean difference (MD) and 95% confidence interval (CI) were calculated for continuous data to assess the change. For continuous outcomes with different scoring units, the standardized mean difference (SMD) with 95% confidence intervals (CI) was used to pool each outcome measure for estimating the effect size. The heterogeneity among studies was assessed by I2; if I2 < 50%, it could be considered that there was homogeneity among the trials, and the fixed-effects model was used; otherwise, a random-effects model was used (I2 ≥ 50%). A z test was adopted to test the combined effect and statistical significance was set at p < 0.05 [22]. In addition, subgroup analyses were used to compare the hip abduction muscle strength (left and right), and evaluation instruments (body composition: BMI and fat mass).
Results
Study selection and characteristics
A total of 580 studies were obtained by searching electrical databases, and thirteen trials [12, 23–34] were finally included (Fig. 1). There were 883 patients in total and involved for meta-analysis (357 aquatic physical therapy and 526 no aquatic physical therapy). A summary of characteristics of the included studies is shown in Table 1. All of the studies were published in English. Published in 2003–2019, the studies come from 10 different countries and regions. The duration of the interventional programs ranged from 6 to 18 weeks.
Fig. 1.
Flow diagram based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement
Table 1.
Characteristics of studies included in the meta-analysis
| First author (year) | Country of study |
ne1/nc1 ne2/nc2 |
Experimental group (type of exercise) | Control group (type of exercise) | Intervention time | Outcomes measures |
|---|---|---|---|---|---|---|
| Dias [28] | Brazil | 33/32 | Aquatic exercise and an educational protocol | An educational protocol | Six weeks |
WOMAC muscle strength Power and resistance |
| Silva [9] | Brazil | 32/32 | Aquatic physical therapy | Land-based exercise | 18 weeks |
Lequesne Index Scores WOMAC, VAS, 50FWT |
| Kars Fertelli [24] | Turkey | 60/60 | Aquatic physical therapy | Not receive any intervention | 8 weeks |
WOMAC, ASS Muscle strength |
| Hale [33] | New Zealand | 23/16 | Aquatic physical therapy | Computer skills training | 12 weeks |
Falls risk ratio Step test, TUGT, ABC Scale AIMS2-SF 26, WOMAC |
| Hinman [31] | Australia | 36/35 | Aquatic physical therapy | Usual care | 6 weeks |
VAS, WOMAC, AQOL, PASE Muscle strength step test, TUGT, 6MWT |
| Lim [32] | Korea |
24/22 24/22 |
Aquatic physical therapy |
Land-based exercise Home-based exercise |
8 weeks |
Body weight, BMI, lean body mass, body fat mass, body fat proportion, abdominal fat, BPI WOMAC SF-36 Peak torque, knee extensor and flexor |
| Lund [12] | Denmark |
27/25 27/27 |
Aquatic physical therapy |
Land-based exercise Not receive any intervention |
8 weeks |
VAS KOOS |
| Rantalainen [26] | Finland | 42/42 | Aquatic physical therapy | Usual care | 16 weeks |
T2 relaxation time, DGEMRIC index Cardiorespiratory fitness, force KOOS |
| Suomi [25] | WI |
10/10 10/10 |
Aquatic physical therapy |
Land-based exercise Not receive any intervention |
8 weeks |
Flexibility, hand–eye coordination Right arm curls, Left arm curls RSHab isometric, LSHab isometric, LHab isometric Functional capacity evaluation |
| Taglietti [34] | Brazil | 31/29 | Aquatic physical therapy | Educational program | 8 weeks |
VAS, WOMAC, SF-36 Depression, TUGT |
| Waller [27] | Finland | 43/44 | Aquatic physical therapy | Usual care | 4 months |
Walking speed, body mass, BMI, lean mass, fat mass KOOS |
| Wang [30] | USA | 20/18 | Aquatic physical therapy | Usual care | 12 weeks |
Flexibility, muscle strength 6MWT, MDHAQ, VAS |
| Wang [23] | Taiwan |
26/26 26/26 |
Aquatic physical therapy |
Land-based exercise Not receive any intervention |
12 weeks | KOOS, ROM, 6MWT |
WOMAC, Western Ontario and McMaster University Osteoarthritis Index; VAS, Visual Analog Scale; 50FWT, 50-foot (15.24-m) Walk Test; ASS, Arthritis Self-Efficacy Scale; TUGT, Timed-Up-and-Go Test; ABC, activity-specific balance confidence; AIMS2-SF, Arthritis Impact Measurement Scales 2-Short Form; AQoL, Assessment of Quality of Life Scale; PASE, Physical Activity Scale for the Elderly; 6MWT, 6-Min walk test; BMI, body mass index; BPI, brief pain inventory; SF-36, medical outcomes study short form-36; KOOS, Knee Injury and Osteoarthritis Outcome Score; T2, transverse relaxation time; DGEMRIC, delayed gadolinium-enhanced magnetic resonance imaging of cartilage; RSHab, right shoulder abduction; LSHab, left shoulder abduction; LHab, left hip abduction; MDHAQ, multidimensional Health Assessment Questionnaire; ROM, range of motion
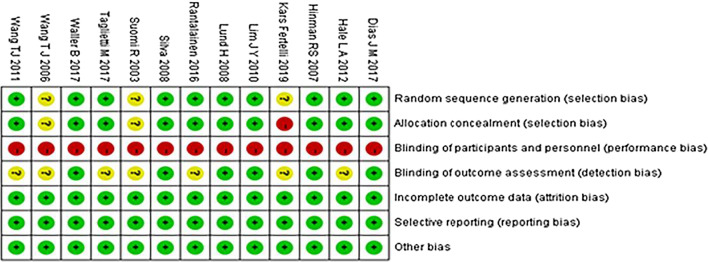
Critical appraisal
The results of quality assessment of the included studies by Cochrane Collaboration Handbook are shown in Figs. 2 and 3. Ten had random sequence generation, ten had allocation concealment, no trials had blinding of participants and personnel, six had blinding of outcome assessment, no trials were assessed to have incomplete outcome data, and risk of selective reporting and other bias in all trials were low.
Fig. 2.
Risk of bias graph
Fig. 3.
Risk of bias summary
Effect of intervention
Pain
Eleven studies were included in the meta-analysis with outcome assessed pain. WOMAC pain [24, 28, 31, 33, 34], VAS score [12, 29–31, 34], and KOOS pain [12, 23, 26, 27] were used to measure pain. Studies which used WOMAC pain and VAS showed high heterogeneity (WOMAC pain: p < 0.1, I2 = 93%, VAS: p < 0.1, I2 = 73%), whereas KOOS pain showed low heterogeneity (p = 0.85, I2 = 0%). There were statistically significant differences in WOMAC pain (SMD = − 1.09, 95%CI − 1.97, − 0.21, p = 0.02), and VAS (SMD = − 0.55, 95%CI − 0.98, − 0.12, p = 0.01) in the aquatic physical therapy group compared to the no aquatic physical therapy group, but no significant difference in KOOS pain (MD = 0.31, 95%CI − 2.12, 2.75, p = 0.80) (Fig. 4).
Fig. 4.
Forest plot of aquatic physical therapy versus no aquatic physical therapy interventions in pain
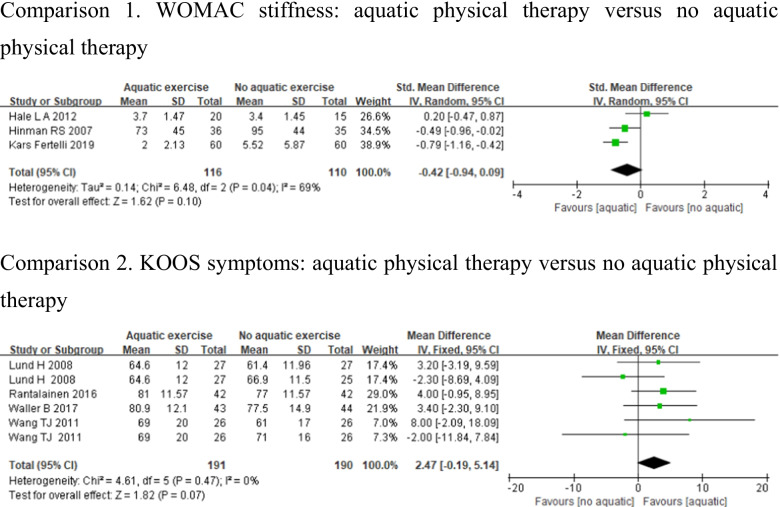
Symptoms of joints
Seven studies assessed symptoms of joints using WOMAC stiffness [24, 31, 33] and KOOS symptoms [12, 23, 26, 27]. Studies which used WOMAC stiffness showed substantial heterogeneity (p < 0.1, I2 = 69%), whereas KOOS symptoms showed low heterogeneity (p > 0.1, I2 = 0%). There were no significant differences in WOMAC stiffness (SMD = − 0.42, 95%CI − 0.94, 0.09, p = 0.1), and KOOS symptoms (MD = 2.47, 95%CI − 0.19, 5.14, p = 0.07) between aquatic physical therapy and no aquatic physical therapy (Fig. 5).
Fig. 5.
Forest plot of aquatic physical therapy versus no aquatic physical therapy interventions in symptoms of joints
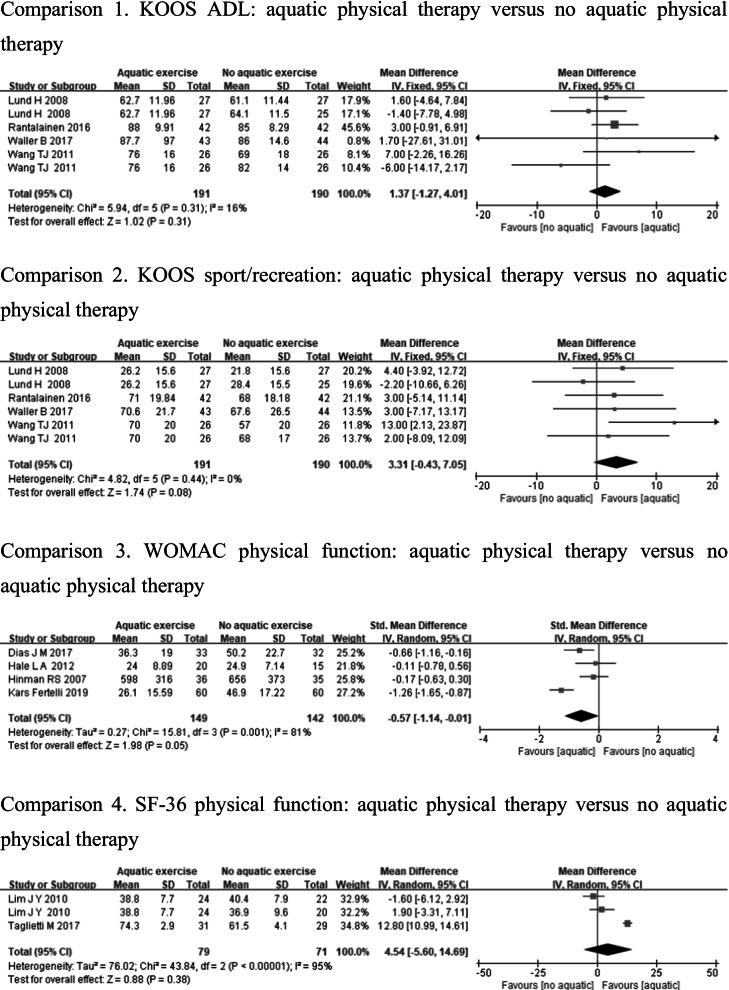
Physical function
Physical function was measured by using KOOS ADL [12, 23, 26, 27], KOOS sport/recreation [12, 23, 26, 27], WOMAC physical function [24, 28, 31, 33], and SF-36 physical function [32, 34]. Whereas KOOS ADL or KOOS sport/recreation showed low heterogeneity (KOOS ADL: p = 0.31, I2 = 16%, KOOS sport/recreation: p = 0.44, I2 = 0%), there were no significant differences in KOOS ADL (MD = 1.37, 95%CI − 1.27, 4.01, p = 0.31), and KOOS sport/recreation (MD = 3.31, 95%CI − 0.43, 7.05, p = 0.08) between aquatic physical therapy and no aquatic physical therapy. However, WOMAC physical function and SF-36 physical function demonstrated high heterogeneity (WOMAC physical function: p < 0.1, I2 = 81%, SF-36 physical function: p < 0.1, I2 = 95%), and there was statistically significant difference in WOMAC physical function (SMD = − 0.57, 95%CI − 1.14, − 0.01, p = 0.05) in the aquatic physical therapy group compared to the no aquatic physical therapy group, but no significant difference in SF-36 physical function (MD = 4.54, 95%CI − 5.60, 14.69, p = 0.38) (Fig. 6).
Fig. 6.
Forest plot of aquatic physical therapy versus no aquatic physical therapy interventions in physical function
Quality of life
Four studies assessed QOL using KOOS QOL [12, 23, 26, 27]. Heterogeneity was not observed in the analyses for QOL (p = 0.6, I2 = 0%), and the meta-analysis (MD = 0.07, 95%CI − 2.67, 2.81, p = 0.96) demonstrated that there was no significant difference in the improvement of QOL between the 2 groups (Fig. 7).
Fig. 7.
Forest plot of aquatic physical therapy versus no aquatic physical therapy interventions in quality of life
Flexibility
Flexibility was measured by tests of joint ROM of knee extension and knee flexion [23, 30]. Studies which used joint ROM of knee extension showed high heterogeneity (p = 0.05, I2 = 67%), whereas knee flexion showed low heterogeneity (p = 0.78, I2 = 0%). There were no significant differences in joint ROM of knee extension (MD = − 0.64, 95%CI − 1.86, 0.58, p = 0.30) and knee flexion (MD = − 1.97, 95%CI − 7.97, 4.03, p = 0.52) in the aquatic physical therapy group compared to the no aquatic physical therapy group (Fig. 8).
Fig. 8.
Forest plot of aquatic physical therapy versus no aquatic physical therapy interventions in flexibility
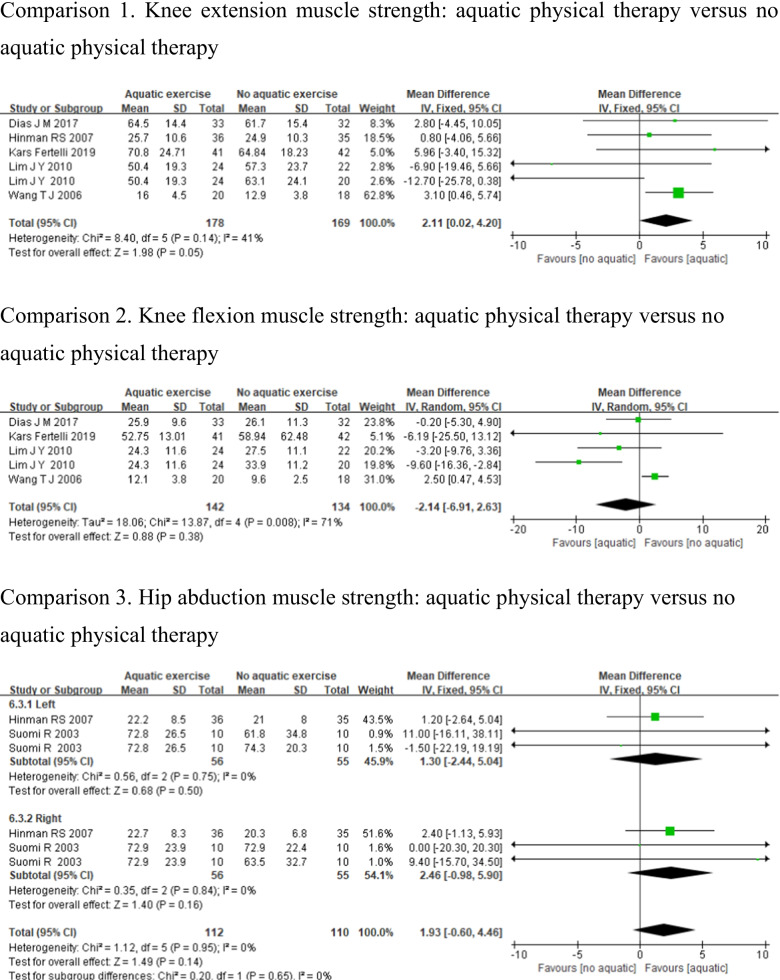
Muscle strength
Six studies were included in the meta-analysis with outcome measured muscle strength. Knee extension muscle strength [24, 28, 30–32], knee flexion muscle strength [24, 28, 30, 32], and hip abduction muscle strength [25, 31] were used to measure muscle strength. Due to the different muscle strength between the left and right sides in hip abduction studies, a subgroup analysis should be conducted for comparison. Heterogeneity was not apparent for knee extension (p = 0.14, I2 = 41%) and hip abduction muscle strength (left: p = 0.75, I2 = 0%, right: p = 0.84, I2 = 0%); however, knee flexion muscle strength demonstrated high heterogeneity (p < 0.01, I2 = 71%). And pooled analysis results demonstrate that aquatic physical therapy has no statistically significant differences than no aquatic physical therapy in improving knee flexion muscle strength (MD = − 2.14, 95%CI − 6.91, 2.63, p = 0.38), and hip abduction muscle strength (left: MD = 1.30, 95%CI − 2.44, 5.04, p = 0.50, right: MD = 2.46, 95%CI − 0.98, 5.90, p = 0.16). But there was a statistically significant difference in knee extension muscle strength between the 2 groups (MD = 2.11, 95%CI: 0.02, 4.20, p = 0.05) (Fig. 9).
Fig. 9.
Forest plot of aquatic physical therapy versus no aquatic physical therapy interventions in muscle strength
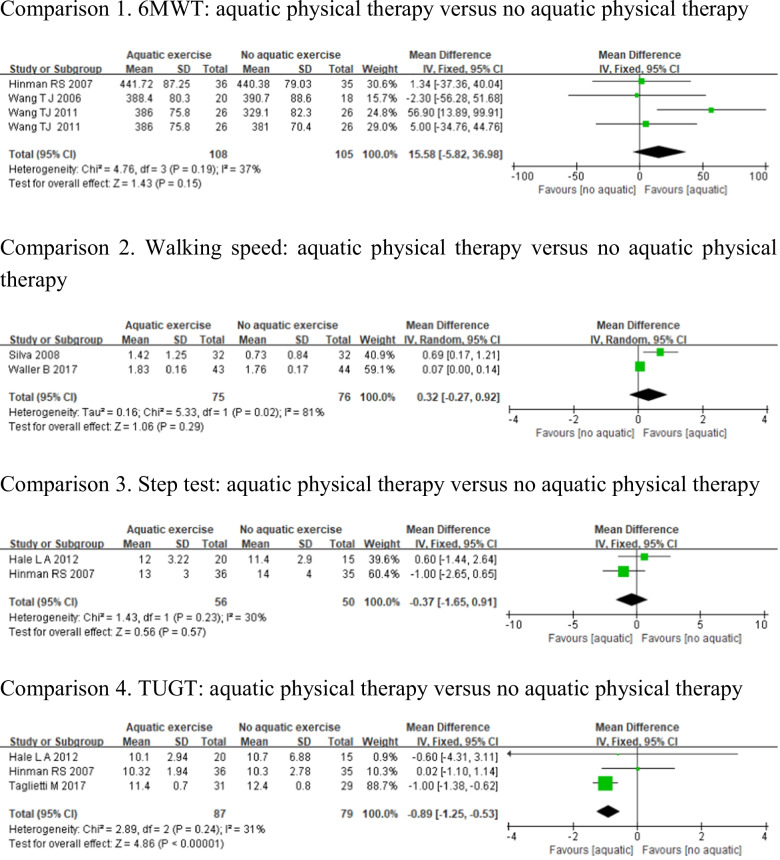
Walking ability
Walking ability was evaluated by 6-min walk test [23, 30, 31], walking speed [27, 29], step test [31, 33], and Timed-Up-and-Go Test [31, 33, 34]. Heterogeneity was not apparent for 6MWT (p = 0.19, I2 = 37%), step test (p = 0.23, I2 = 30%), and TUGT (p = 0.24, I2 = 31%); however, walking speed demonstrated high heterogeneity (p = 0.02, I2 = 81%). The aquatic physical therapy has no statistically significant difference in improving the scores of 6MWT (MD = 15.58, 95%CI − 5.82, 36.98, p = 0.15), walking speed (MD = 0.32, 95%CI − 0.27, 0.92, p = 0.29), and step test (MD = − 0.37, 95%CI − 1.65, 0.91, p = 0.57) compared to no aquatic physical therapy. But there was a statistically significant difference in TUGT between the 2 groups (MD = − 0.89, 95%CI − 1.25, − 0.53, p < 0.05) (Fig. 10).
Fig. 10.
Forest plot of aquatic physical therapy versus no aquatic physical therapy interventions in walking ability
Body composition
Two studies assessed body composition using BMI [27, 32] and fat mass [27, 32]. Because the evaluation methods are different among these studies, a subgroup analysis should be conducted for comparison. Whereas BMI or fat mass showed low heterogeneity (BMI: p = 0.47, I2 = 0%, fat mass: p = 0.38, I2 = 0%), there were no significant differences in BMI (MD = − 0.30, 95%CI − 0.98, 0.39, p = 0.39), and fat mass (MD = − 0.62, 95%CI − 2.20, 0.96, p = 0.44) between the 2 groups (Fig. 11).
Fig. 11.
Forest plot of aquatic physical therapy versus no aquatic physical therapy interventions in body composition
Discussion
This systematic review and meta-analysis aimed to determine the overall treatment effect of aquatic physical therapy in patients with knee OA. Based on the included RCTs (n = 13), for pain, we found that aquatic physical therapy is associated with a significant change in WOMAC pain and VAS but not KOOS pain in people with knee OA. For symptoms of joints, our meta-analysis showed that aquatic physical therapy did not significantly relieve WOMAC stiffness and KOOS symptoms. Compared with no aquatic physical therapy, aquatic physical therapy cannot improve three test scores of physical function (KOOS ADL, KOOS sport/recreation and SF-36 physical function), but it has significant statistical differences in WOMAC physical function, and the effect size was moderate (WOMAC: SMD = − 0.57, 95%CI − 1.14, − 0.01, p = 0.05). Our findings also showed no significant improvements in QOL, flexibility, and body composition with knee OA. For muscle strength, we found that aquatic physical therapy can only improve knee extension muscle strength. In addition, for walking ability, we observed that aquatic physical therapy effectively reduced TUGT in a large degree. However, we also found that aquatic physical therapy cannot improve scores of the other three tests in walking ability (6MWT, walking speed, and step test). This may be due to the training was not intense or long enough, which is not enough to produce a significant statistical difference. Therefore, we concluded that aquatic physical therapy can improve pain, physical function, knee extension muscle strength, and walking ability to a certain extent.
Joint pain and stiffness are the most common symptoms in patients with knee OA and are the primary barriers for performing activities of daily living in this patient population [8]. Aquatic physical therapy is based on the buoyancy and temperature of water, which may encourage muscle relaxation, enhance greater movement to reduce joint and soft-tissue stiffness and, therefore, improve pain and physical function [31, 35]. Our study demonstrated that aquatic physical therapy can have a small and significant effect on pain and physical function, thus strengthening previous meta-analysis [11, 17, 36]. In addition, contrary to the previous findings [11, 17], our meta-analysis revealed that aquatic physical therapy cannot improve joints stiffness and QOL among people with knee OA. These differences in results can stem from the differences in the characteristics of the included studies. Therefore, our results may not accurately represent the true changes in joints stiffness and QOL within this population.
Meanwhile, the above changes were accompanied by the improvements in muscle strength and flexibility, as well as reductions in body composition. Muscle strength is clinically important as strong muscles act as shock absorbers and joint stabilizers, assisting to protect diseased joints [37]. The previous review [17] did not find any effect on muscle strength, whereas our study is the first to show that aquatic physical therapy can have a small but significant effect on knee extension muscle strength. The gradually and consistently increase in strength of knee extensor was a promising outcome of the program for preventing OA-associated disabilities in later life. The aquatic physical therapy, on the other hand, showed no effect on other major muscle groups, possibly due to too insufficient intervention intensity or duration to cause physiological changes in muscle structure [12].
A great improvement in walking ability of this study is a reduction in the TUGT, reflecting better control of the knee joint during walking and standing. Although the other three tests (6MWT, walking speed, and step test) used to evaluate walking ability have not been improved, this indicates that TUGT has greater specificity to patients with OA compared to the other three tests and consequently better responsiveness.
Study limitations
However, some potential limitations of this study should be noted. First, more participants are needed to further study how aquatic physical therapy affects muscle strength of knee OA in a more systematic way. It may also be beneficial to follow the progress of participants to investigate the impact of aquatic physical therapy on knee OA patients over a longer period of time. Additionally, our review is unable to demonstrate the optimal intervention dose, type of exercise and training intensity for this population group.
Conclusion
In conclusions, this meta-analysis confirmed that aquatic physical therapy is an effective treatment option for persons with severe symptoms of knee OA and should be considered as an important initial treatment option for rehabilitation programs. Researchers planning an aquatic physical therapy study should ensure that all aspects of the disease are considered, not just pain and physical function, and they need to refer to current recommendations when measuring results to promote the effectiveness of treatment. Future studies should aim to improve program content by maximizing the hydrostatic and hydrodynamic properties of water, so as to maximize the potential benefits of aquatic physical therapy for patients with knee OA.
Acknowledgements
We would like to thank Dean Qin and Lijun Li for their assistance with this study.
Abbreviations
- ADL
Activities of daily living
- BMI
Body mass index
- KOOS
Knee Injury and Osteoarthritis Outcome Score
- 6MWT
6-Min walk test
- QOL
Quality of life
- ROM
Range of motion
- SF-36
Short form-36
- TUGT
Timed-Up-and-Go Test
- VAS
Visual analog scale
- WOMAC
Western Ontario and McMaster University Osteoarthritis Index
Author's contributions
All authors read and approved the final manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ji Ma, Email: Majisxty@163.com.
Xiaoyu Chen, Email: cxy136434@126.com.
Juan Xin, Email: 1561068754@qq.com.
Xin Niu, Email: nxkxsh0928@163.com.
Zhifang Liu, Email: lzf13546444276@163.com.
Qian Zhao, Email: zhaoqian_sara@126.com.
References
- 1.Hunter DJ, Schofield D, Callander E. The individual and socioeconomic impact of osteoarthritis. Nat Rev Rheumatol. 2014;10:437–441. doi: 10.1038/nrrheum.2014.44. [DOI] [PubMed] [Google Scholar]
- 2.Prieto-Alhambra D, Judge A, Javaid MK, et al. Incidence and risk factors for clinically diagnosed knee, hip and hand osteoarthritis: influences of age, gender and osteoarthritis affecting other joints. Ann Rheum Dis. 2014;73:1659–1664. doi: 10.1136/annrheumdis-2013-203355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019;393:1745–1759. doi: 10.1016/S0140-6736(19)30417-9. [DOI] [PubMed] [Google Scholar]
- 4.McAlindon TE, Bannuru RR, Sullivan MC, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage. 2014;22:363–388. doi: 10.1016/j.joca.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 5.Bartels EM, Lund H, Hagen KB, et al. Aquatic exercise for the treatment of knee and hip osteoarthritis. Cochrane Database Syst Rev. 2007;2007:CD005523. doi: 10.1002/14651858.CD005523.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Ball K, Crawford D, Owen N. Too fat to exercise? Obesity as a barrier to physical activity. Aust N Z J Public Health. 2000;24:331–333. doi: 10.1111/j.1467-842X.2000.tb01579.x. [DOI] [PubMed] [Google Scholar]
- 7.Lim K, Taylor L. Factors associated with physical activity among older people—a population-based study. Prev Med. 2005;40:33–40. doi: 10.1016/j.ypmed.2004.04.046. [DOI] [PubMed] [Google Scholar]
- 8.Pisters MF, Veenhof C, van Dijk GM, et al. The course of limitations in activities over 5 years in patients with knee and hip osteoarthritis with moderate functional limitations: risk factors for future functional decline. Osteoarthritis Cartilage. 2012;20:503–510. doi: 10.1016/j.joca.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 9.Theis KA, Murphy L, Hootman JM, et al. Prevalence and correlates of arthritis-attributable work limitation in the US population among persons ages 18–64: 2002 National Health Interview Survey Data. Arthritis Rheum. 2007;57:355–363. doi: 10.1002/art.22622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Biscarini A, Cerulli G. Modeling of the knee joint load in rehabilitative knee extension exercises under water. J Biomech. 2007;40:345–355. doi: 10.1016/j.jbiomech.2005.12.018. [DOI] [PubMed] [Google Scholar]
- 11.Bartels EM, Juhl CB, Christensen R, et al. Aquatic exercise for the treatment of knee and hip osteoarthritis. Cochrane Database Syst Rev. 2016;3:CD005523. doi: 10.1002/14651858.CD005523.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lund H, Weile U, Christensen R, et al. A randomized controlled trial of aquatic and land-based exercise in patients with knee osteoarthritis. J Rehabil Med. 2008;40:137–144. doi: 10.2340/16501977-0134. [DOI] [PubMed] [Google Scholar]
- 13.Eversden L, Maggs F, Nightingale P, et al. A pragmatic randomised controlled trial of hydrotherapy and land exercises on overall well being and quality of life in rheumatoid arthritis. BMC Musculoskelet Disord. 2007;8:23. doi: 10.1186/1471-2474-8-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bidonde J, Busch AJ, Webber SC, et al. Aquatic exercise training for fibromyalgia. Cochrane Database Syst Rev. 2014;2014:CD011336. doi: 10.1002/14651858.CD011336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Forestier R, et al. Health benefits of immersion and therapeutic aquatic exercise in swimming pools and spas in health care, with focus on rheumatologic, orthopaedic and neurological disorders. J Jpn Soc Balneol Climatol Phys Med. 2014;77:417–418. [Google Scholar]
- 16.Park J, Lee D, Lee S, et al. Comparison of the effects of exercise by chronic stroke patients in aquatic and land environments. J Phys Ther Sci. 2011;23:821–824. doi: 10.1589/jpts.23.821. [DOI] [Google Scholar]
- 17.Waller B, Ogonowska-Slodownik A, Vitor M, et al. Effect of therapeutic aquatic exercise on symptoms and function associated with lower limb osteoarthritis: systematic review with meta-analysis. Phys Ther. 2014;94:1383–1395. doi: 10.2522/ptj.20130417. [DOI] [PubMed] [Google Scholar]
- 18.Dong R, Wu Y, Xu S, et al. Is aquatic exercise more effective than land-based exercise for knee osteoarthritis? Medicine (Baltimore) 2018;97:e13823. doi: 10.1097/MD.0000000000013823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bliddal H, Christensen R. The management of osteoarthritis in the obese patient: practical considerations and guidelines for therapy. Obes Rev. 2006;7(4):323–331. doi: 10.1111/j.1467-789X.2006.00252.x. [DOI] [PubMed] [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cumpston M, Li T, Page MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev. 2019; 10: 000142. 10.1002/14651858.ED000142. [DOI] [PMC free article] [PubMed]
- 22.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 23.Wang T-J, Lee S-C, Liang S-Y, et al. Comparing the efficacy of aquatic exercises and land-based exercises for patients with knee osteoarthritis. J Clin Nurs. 2011;20:2609–2622. doi: 10.1111/j.1365-2702.2010.03675.x. [DOI] [PubMed] [Google Scholar]
- 24.Kars Fertelli T, Mollaoglu M, Sahin O. Aquatic exercise program for individuals with osteoarthritis: pain, stiffness, physical function self-efficacy. Rehabil Nurs. 2019;44:290–299. doi: 10.1097/rnj.0000000000000142. [DOI] [PubMed] [Google Scholar]
- 25.Suomi R, Collier D. Effects of arthritis exercise programs on functional fitness and perceived activities of daily living measures in older adults with arthritis. Arch Phys Med Rehabil. 2003;84:1589–1594. doi: 10.1053/S0003-9993(03)00278-8. [DOI] [PubMed] [Google Scholar]
- 26.Munukka M, Waller B, Rantalainen T, et al. Efficacy of progressive aquatic resistance training for tibiofemoral cartilage in postmenopausal women with mild knee osteoarthritis: a randomised controlled trial. Osteoarthritis Cartilage. 2016;24:1708–1717. doi: 10.1016/j.joca.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 27.Waller B, Munukka M, Rantalainen T, et al. Effects of high intensity resistance aquatic training on body composition and walking speed in women with mild knee osteoarthritis: a 4-month RCT with 12-month follow-up. Osteoarthritis Cartilage. 2017;25:1238–1246. doi: 10.1016/j.joca.2017.02.800. [DOI] [PubMed] [Google Scholar]
- 28.Dias JM, Cisneros L, Dias R, et al. Hydrotherapy improves pain and function in older women with knee osteoarthritis: a randomized controlled trial. Braz J Phys Ther. 2017;21:449–456. doi: 10.1016/j.bjpt.2017.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Silva LE, Valim V, Pessanha APC, et al. Hydrotherapy versus conventional land-based exercise for the management of patients with osteoarthritis of the knee: a randomized clinical trial. Phys Ther. 2008;88:12–21. doi: 10.2522/ptj.20060040. [DOI] [PubMed] [Google Scholar]
- 30.Wang T-J, Belza B, Elaine Thompson F, et al. Effects of aquatic exercise on flexibility, strength and aerobic fitness in adults with osteoarthritis of the hip or knee. J Adv Nurs. 2007;57:141–152. doi: 10.1111/j.1365-2648.2006.04102.x. [DOI] [PubMed] [Google Scholar]
- 31.Hinman RS, Heywood SE, Day AR. Aquatic physical therapy for hip and knee osteoarthritis: results of a single-blind randomized controlled trial. Phys Ther. 2007;87:32–43. doi: 10.2522/ptj.20060006. [DOI] [PubMed] [Google Scholar]
- 32.Lim J-Y, Tchai E, Jang S-N. Effectiveness of aquatic exercise for obese patients with knee osteoarthritis: a randomized controlled trial. PM R. 2010 doi: 10.1016/j.pmrj.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 33.Hale LA, Waters D, Herbison P. A randomized controlled trial to investigate the effects of water-based exercise to improve falls risk and physical function in older adults with lower-extremity osteoarthritis. Arch Phys Med Rehabil. 2012;93:27–34. doi: 10.1016/j.apmr.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 34.Taglietti M, Facci LM, Trelha CS, et al. Effectiveness of aquatic exercises compared to patient-education on health status in individuals with knee osteoarthritis: a randomized controlled trial. Clin Rehabil. 2018;32:766–776. doi: 10.1177/0269215517754240. [DOI] [PubMed] [Google Scholar]
- 35.Bender T, Karagülle Z, Bálint GP, et al. Hydrotherapy, balneotherapy, and spa treatment in pain management. Rheumatol Int. 2005;25:220–224. doi: 10.1007/s00296-004-0487-4. [DOI] [PubMed] [Google Scholar]
- 36.Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, part I: critical appraisal of existing treatment guidelines and systematic review of current research evidence. Osteoarthritis Cartilage. 2007;2007:15. doi: 10.1016/j.joca.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 37.Bennell KL, Wrigley TV, Hunt MA, et al. Update on the role of muscle in the genesis and management of knee osteoarthritis. Rheum Dis Clin N Am. 2013;39:145–176. doi: 10.1016/j.rdc.2012.11.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.