Abstract
Background
Femoral head osteonecrosis (FHON) is a worldwide challenging clinical topic. Steroid use is one of the main etiologies of FHON. There are several genetic variants associated with FHON. Therefore, the purpose of this umbrella review was to provide a comprehensive summary of a meta-analysis and systematic review of genetic variations associated with nonsteroidal and steroid-induced FHON.
Methods
The eligible studies were selected from the PubMed and MEDLINE databases for the collection of diverse systematic meta-analyses and reviews. The genetic main effect score was assigned using the Human Genome Epidemiology Network’s Venice criteria to assess the cumulative evidence on the effects of a single nucleotide polymorphism (SNP) on FHON.
Results
Eight articles reported the meta-analysis of candidate SNP-based studies covering eight genes and 13 genetic variants. In the nonsteroid-induced FHON genetic variants including rs2012390 and rs11225394 in MMP8, rs1800629 and rs361525 in tumor necrosis factor (TNF)-α, VNTR in intron 4, rs1799983 and rs2070744 in endothelial nitric oxide synthase (eNOS), rs2010963 in vascular endothelial growth factor (VEGF), and rs6025 in factor V showed significance in each reference. The steroid-induced FHON genetic variants including rs693 and rs1042031 in apolipoprotein (Apo)B, rs1045642 in ABCB1, and rs1799889 in PAI-1 showed significance in each reference.
Conclusion
Based on the systematic review conducted in this study, we organized the genomes associated with FHON and looked at each contribution. Our results could give an integrative approach for understanding the mechanism of FHON etiology. It is expected that these results could contribute to the strategy of prediagnosis, evaluating the individual risk of nonsteroid-induced and steroid-induced FHON.
Level of Evidence: Level I.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13018-022-03079-4.
Keywords: Femoral head osteonecrosis, Umbrella review, Steroid, Polymorphism, Genetic variant
Introduction
Femoral head osteonecrosis (FHON) is a worldwide challenging clinical topic. FHON was described as hip trauma with late complications by Jean Cruveilhier, a French anatomist and pathologist [1]. Since then, many studies have identified the etiology of FHON [1–4]. According to studies that conducted pathology of FHON, classification of pathogenesis included the following. First, obstructed circulation to a specific area due to compromised blood flow was reported as the final pathway of FHON. Second, steroid-induced FHON has different pathogenesis, which is a kind of intraosseous compartment syndrome. Third, FHON has a complicated etiology including genetic factors and exposure to risk factors. This means that genetic factors can be the cause of disease emergence and are closely related to other pathogenesis factors [5–8]. The risk of FHOM increases in the presence of these genetic predisposing factors [9].
Steroid use is one of the main etiologies of FHON. Steroids are dose-dependent etiologic agents of FHON [10]. Long-term steroid use could lead to the collapse of the femoral head, structural alteration, and dysfunctional hip joint [11]. There are several pathogenesis theories of steroid-induced FHON, including (1) the lipid metabolism disorder theory that steroids cause fat embolism within the microvessels by increasing subcutaneous fat mobilization [12]; (2) the insufficient blood supply theory that some steroids disturb the blood supply to the femoral head with intravascular thrombosis [13, 14]; and (3) adipogenesis of the bone marrow stromal cells (BMSCs), which is the principal mechanism involved in the onset and progression of steroid-induced FHON [15, 16]. Although many theories are considered the etiology of steroid-induced FHON, the exact pathologic process is still not clear.
So far, several genetic factors associated with FHON have been reported including apolipoprotein (Apo)A, which is involved in lipid metabolism and the coagulation system [17, 18]; VEGF in the Korean population [19]; mutations in factor V Leiden (FVL) [20]; and plasminogen activator inhibitor type 1 polymorphism [21, 22]. In addition, genetic factors associated with steroid-induced FHON have also been reported including genes related to lipid transportation like ABCB1and CYP3A [23, 24]; and genetic polymorphisms involved in vascular occlusion and coagulopathy such as PAI and MTHFR [25–27]. These genetic factors are very useful tools for understanding FHON. Identifying the specific genetic differences between those with and without FHON will provide clues to FHON.
Therefore, the purpose of this umbrella review was to provide a comprehensive summary of a meta-analysis and systematic review of genetic variations associated with nonsteroidal and steroid-induced FHON.
Methods
Search strategy and eligible study selection criteria
The eligible studies were selected from the PubMed and MEDLINE databases for the collection of diverse systematic meta-analyses and reviews in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines [28]. The search strategy included the keywords "osteonecrosis"[MeSH Terms] OR "osteonecrosis"[All Fields] OR "avascular"[All Fields] AND "necrosis"[All Fields] OR "avascular necrosis"[All Fields]) AND "genes"[MeSH Terms] OR "genes"[All Fields] OR "gene"[All Fields] AND "meta"[Journal] OR "meta"[All Fields]. The retrieved publications were independently screened by two authors. Discrepancies were resolved according to a consensus. A third investigator was included if a final decision could not be reached. After the title and abstract were screened, the full texts of the publications were selected for determining the final eligibility.
The eligible studies included meta-analyses of four types: (i) SNP-based systematic reviews and gene meta-analyses related to femoral neck head necrosis, (ii) studies providing definite information on the statistical processes and results, and (iii) studies written in English and published after January 1, 2012. Only studies in adult populations were included, and gender differences were not considered because general SNP-based meta-analyses associated with FHON were performed regardless of sex. The following types of studies were excluded: (i) systematic meta-analyses without a quantitative synthesis of the evidence, (ii) non-human studies, (iii) having huge errors or poor quality, and (iv) studies with no specific statistical results including heterogeneity tests, the examined risk factors, and the overall p values.
Data extraction
Two independent authors were included in the data extraction stage. One author extracted the data and then it was checked by a second author. For selecting the eligible articles, the following information was included: (i) the first author’s name; (ii) year of publication; (iii) the genetic variants of each study and effect size (ES); (iv) the number of studies included in each article; and (v) sample size, p values, and heterogeneity estimates.
Methodological quality
Methodological quality was rated by the Assessment of Multiple Systematic Reviews (AMSTAR) instrument [2]. This version comprises 16 items evaluating the methodological quality of articles. This assessment is rated on a scale from high quality to very low quality.
Statistical analysis
The genetic main effect score was assigned using the Human Genome Epidemiology Network’s Venice criteria to assess the cumulative evidence of SNP effects on FHON [29]. Briefly, these guidelines provide criteria for assessing cumulative evidence in genetic epidemiology. The amount of evidence, the extent of replication, and protection from bias were indexes in these guidelines. The three levels of evidence were strong, moderate, or weak. According to these criteria, a large amount of evidence and large sample sizes ensure adequate power for detecting an association. By the genome-wide testing of thousands of polymorphisms, we evaluated the evidence for the main genetic effect score class with p values of at least < 0.005 to be considered for strong candidacy. A specific description of the application of the guidelines is provided in Table 1.
Table 1.
Description of the extension of the Human Genome Epidemiology Network’s Venice criteria to assess genetic main effect
| Criteria of consideration | Category | Proposed operationalization |
|---|---|---|
| Amount of evidence | A | Sample size over 1000 |
| B | Sample size 100–1000 | |
| C | Sample size under 100 | |
| Replication | A | I2 < 50% |
| B | 25% < I2 < 50% | |
| C | I2 > 50% | |
| Protection from bias | A | Consideration biases such as bias in genotyping, population stratification, and Selective reporting biases |
| B | Bias in genotype definition = Not reported what was done/No quality control checks/Appropriate quality control checks | |
| C |
Population stratification = Not reported what was done/Nothing done/Same descent group/Adjustment for reported descent/Family-based design/Genomic control, PCA or similar method Selective reporting biases = Meta-analysis of published data/Retrospective efforts to include unpublished data/Meta-analysis within consortium |
Evidence is classified as strong, moderate, and weak. When scored A in every criteria, evidence is categorized as strong. When scored no C in every criteria but no AAA, evidence is categorized as moderate. Weak evidence is recorded with C in one out of three criteria
Results
Number of articles and type identified
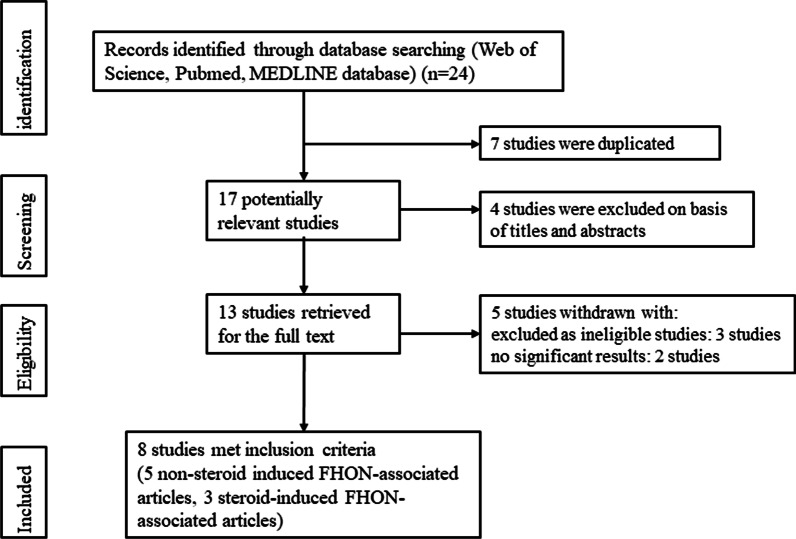
For the systematic reviews, 24 unique references were identified from the databases. After excluding the duplicates and articles that were not on the main topics, 13 articles remained. Three additional articles were excluded as ineligible studies because they provided inadequate data. Two other articles with no significant results were excluded. Finally, eight eligible publications [30–37] were selected for references as they included convincing data, appropriate qualitative evaluations, significant results, human studies, and topics fitting with our purpose (Fig. 1). In the eight included references, there were five nonsteroid-induced FHON-associated articles including nine genetic variants and three steroid-induced FHON-associated articles including four genetic variants. All references were retrospective studies to identify FHON-associated genetic variants. And all studies included in the references used blood samples for subject-specific genotyping. The publications that excluded with various reasons were provided in Additional file 1: Table S1.
Fig. 1.
Flowchart of study selection process
Main findings of the meta-analyses of SNP-based studies
Eight articles reported the meta-analyses of candidate SNP-based studies covering eight genes and 13 genetic variants.
In nonsteroid-induced FHON, MMP-8 displayed meaningful results in rs2012390 and rs11225394. Rs11225394 was very significant, with a p value of under 0.00001 for the genetic main effect. The rs11225394 SNP showed a strong evidence class according to the Venice criteria. Peng et al. [31] demonstrated that rs1800629 and rs361525, which are SNPs of TNF-α, showed a low odds ratio with the G allele. In rs361525, the odds ratio was under 0.3 and the p value was under 0.001 in the allele genetic model and recessive genetic model, respectively. This result of rs361525 showed extremely significant and strong evidence with a score of AAB in the Venice criteria. Song and Lee et al. [32] reported that the variable number of tandem repeats (VNTRs) in intron 4 of the eNOS gene showed high significance with a p value of under 0.001 in the allele genetic model and the dominant genetic model. The evidence class was moderate. Rs1799983 and rs2070744 also showed barely significant results and excessive heterogeneity with I2 values of 80.20% and 90%, respectively. Rs2010963 of the VEGF gene in Asians also showed significant results in the homozygote model and the dominant model with strong evidence [33]. A p value of < 0.001 with strong evidence was recorded in rs6025, which is a genetic variant of factor. Shang et al. demonstrated that rs6025 in a mixed ethnicity population showed a high possibility of disease occurrence with an odds ratio of 4.55 (Table 2).
Table 2.
Genetic variants derived from eligible meta-analyses of nonsteroid-induced FHON
| Genetic variant | Gene (or near gene) | Reference (year of data collection) | Ethnicity | Sample size (case/control) | Included studies | Minor allele & Reference allele | Genetic model | Type of model | Reported OR (95% CI) | p value for genetic main effect | Heterogeneity (%) | Venice criteria | Evidence class |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| rs2012390 | MMP-8 | Jiang et al. [30] | Asian | 884/1012 | 3 | A & G | Allele model | Fixed effect | 1.34 [1.00–1.79] | 0.005 | 0 | NA | NA |
| Heterozygote model | Fixed effect | 1.40 [1.14–1.73] | 0.002 | 0 | NA | NA | |||||||
| Dominant model | Fixed effect | 1.39 [1.13–1.71] | 0.002 | 0 | NA | NA | |||||||
| rs11225394 | MMP-8 | Jiang et al. [30] | Asian | 1184/1211 | 3 | C & T | Heterozygote model | Fixed effect | 0.63 [0.51–0.77] | < 0.00001 | 21 | AAB (equivalent to AAA) | Strong |
| rs1800629 | TNF-α | Peng et al. [31] | Caucasian/Asian | 432/760 | 7 | G & A | Allele model | Fixed effect | 0.73 [0.57–0.93] | 0.012 | 17.50 | NA | NA |
| Homozygote model | Fixed effect | 0.52 [0.26–1.05] | 0.069 | 10.00 | NA | NA | |||||||
| Heterozygote model | Fixed effect | 0.68 | 0.324 | 6.60 | NA | NA | |||||||
| Dominant model | Fixed effect | 0.54 [0.27–1.09] | 0.085 | 10.40 | NA | NA | |||||||
| Recessive model | Fixed effect | 0.73 [0.54–0.97] | 0.029 | 0 | NA | NA | |||||||
| rs361525 | TNF-α | Peng et al. [31] | Caucasian/Asian | 432/760 | 3 | G & A | Allele model | Fixed effect | 0.27 [0.15–0.49] | < 0.001 | 0 | AAB (equivalent to AAA) | Strong |
| Recessive model | Fixed effect | 0.25 [0.14–0.47] | < 0.001 | 0 | AAB (equivalent to AAA) | Strong | |||||||
| VNTR in intron 4 | eNOS | Song and Lee [32] | Caucasian/Asian | 296/329 | 3 | 4a & 4b | Allele model | Fixed effect | 3.24 [2.04–5.15] | < 0.001 | 0 | BAB | Moderate |
| Dominant model | Fixed effect | 3.50 [2.12–5.78] | < 0.001 | 0 | BAB | Moderate | |||||||
| 193/226 | 2 | 4a & 4b | Recessive model | Fixed effect | 4.76 [0.77–59.61] | 0.094 | 0 | NA | NA | ||||
| rs1799983 | eNOS | Song and Lee [32] | Asian | 403/661 | 3 | T & G | Allele model | Random effect | 1.72 [0.80–3.70] | 0.006 | 80.20 | ABB | Moderate |
| rs2070744 | eNOS | Song and Lee [32] | Asian/NA | 145/378 | 2 | C & T | Allele model | Random effect | 1.03 [0.19–5.96] | 0.001 | 90 | ABB | Moderate |
| rs2010963 | VEGF | Hong et al. [33] | Asian | 697/877 | 3 | C & G | Homozygote model | Fixed effect | 0.82 [0.72–0.93] | 0.002 | 0 | AAB (equivalent to AAA) | Strong |
| Dominant model | Fixed effect | 0.79 [0.67–0.92] | 0.003 | 0 | AAB (equivalent to AAA) | Strong | |||||||
| Recessive model | Fixed effect | 1.29 [1.06–1.59] | 0.015 | 0 | NA | NA | |||||||
| rs6025 | Factor V | Shang et al. [34] | Mixed | 481/867 | 7 | A & G | Homozygote model | Fixed effect | 4.55 [2.75–7.52] | < 0.001 | 0 | AAB (equivalent to AAA) | Strong |
The signature of bold represents OR, p value, and heterogeneity of genetic variances with a p value < 0.05
Evidence is classified as strong, moderate, and weak. When scored A in every criteria, evidence is categorized as strong. When scored no C in every criteria but no AAA, evidence is categorized as moderate. Weak evidence is recorded with C in one out of three criteria
In steroid-induced FHON, ApoB has genetic variants rs693 and rs1042031 with significant p values for the main effect [35]. Particularly, rs1042031 showed a very significant result in the dominant genetic model with an odds ratio of 2.90 in various ethnicities and an odds ratio of 4.81 in Asians. In the articles by Zhou et al. [36], the ABCB1 rs1045642 genetic variant also showed significant results in Asians. The PAI-1 rs1799889 genetic variant showed an exceedingly significant p value of under 0.0005 in the homozygote model and dominant model, with a moderate evidence class in the study by Gong et al. [37].
The 16 excluded publications and the reasons are shown in Table 3.
Table 3.
Genetic variants derived from eligible meta-analyses of steroid-induced FHON
| Genetic variant | Gene (or near gene) | Reference (year of data collection) | Ethnicity | Sample size (case/control) | Included studies | Minor allele & major allele | Genetic model | Type of model | Reported OR (95% CI) | p value for genetic main effect | Heterogeneity (%) | Venice criteria | Evidence class |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| rs693 | ApoB | Chen et al. [35] | Mixed | 570 (total) | 4 | C & T | Allelic model | NA | 2.63 [0.92–7.53] | 0.072 | 58.00 | NA | NA |
| Heterozygous model | NA | 2.46 [1.27–4.77] | 0.008 | 54.50 | NA | NA | |||||||
| Homozygous model | NA | 7.70 [1.23–48.18] | 0.029 | 24.40 | NA | NA | |||||||
| Recessive model | NA | 7.16 [1.19–43.05] | 0.031 | 32.10 | NA | NA | |||||||
| rs693 | ApoB | Chen et al. [35] | Mixed | 725 (total) | 5 | C & T | Dominant model | NA | 2.99 [1.71–5.22] | < 0.001 | 31.30 | BBB | Moderate |
| rs1042031 | ApoB | Chen et al. [35] | Mixed | 572 (total) | 4 | G & A/C | Dominant model | NA | 2.90 [1.49–5.65] | 0.002 | 50.30 | BCB | Weak |
| rs1042031 | ApoB | Chen et al. [35] | China | 415 (total) | 3 | G & A/C | Dominant model | NA | 4.81 [2.05–11.30] | < 0.001 | 0 | BAB | Moderate |
| rs1801133 | MTHFR | Chen et al. [35] | Mixed | 251 (total) | 3 | C & T | Allelic | NA | 0.92 [0.59–1.44] | 0.710 | 12.90 | NA | NA |
| Heterozygous model | NA | 0.62 [0.33–1.17] | 0.144 | 22.10 | NA | NA | |||||||
| Homozygous model | NA | 1.24 [0.48–3.21] | 0.653 | 0 | NA | NA | |||||||
| Recessive model | NA | 1.54 [0.63–3.76] | 0.339 | 0 | NA | NA | |||||||
| 507 (total) | 4 | C & T | Dominant model | NA | 0.94 [0.61–1.45] | 0.775 | 23.40 | NA | NA | ||||
| rs1045642 | ABCB1 | Zhou et al. [36] | Asian/mixed | 336/712 | 7 | T & C | Allelic | Fixed effect | 0.68 [0.54–0.84] | 0.295 | 18.30 | NA | NA |
| Heterozygous model | Fixed effect | 0.73 [0.53–1.00] | 0.722 | 0 | NA | NA | |||||||
| Homozygote model | Random effect | 0.43 [0.26–0.69] | 0.049 | 58.10 | NA | NA | |||||||
| Recessive model | Random effect | 0.52 [0.34–0.81] | 0.009 | 70.30 | NA | NA | |||||||
| Dominant model | Fixed effect | 0.64 [0.48–0.87] | 0.830 | 0 | NA | NA | |||||||
| rs2032582 | ABCB1 | Zhou et al. [36] | Mixed | 275/574 | 5 | T/A &G | Allelic | Fixed effect | 0.73 [0.58–0.90] | 0.587 | 0 | NA | NA |
| Heterozygous model | Fixed effect | 0.66 [0.45–0.96] | 0.985 | 0 | NA | NA | |||||||
| Homozygote model | Fixed effect | 0.52 [0.34–0.82] | 0.560 | 0 | NA | NA | |||||||
| Recessive model | Fixed effect | 0.71 [0.49–1.01] | 0.385 | 3.9 | NA | NA | |||||||
| Dominant model | Fixed effect | 0.61 [0.43–0.87] | 0.959 | 0 | NA | NA | |||||||
| rs1799889 | PAI-1 | Gong et al. [37] | Mixed | 108/917 | 4 | 4G/5G | Allele model | NA | 1.93 [1.15–3.26] | 0.014 | 0.0004 (P) | NA | NA |
| Homozygote model | NA | 3.22 [1.67–6.21] | < 0.0005 | 0.00111 (P) | ACB | Moderate | |||||||
| Dominant model | NA | 2.31 [1.53–3.49] | < 0.0005 | 0.06 (P) | ACB | Moderate | |||||||
| Recessive model | NA | 2.30 [1.24–4.30] | 0.009 | 0.162 (P) | NA | NA |
The signature of bold represents OR, p value, and heterogeneity of genetic variances with a p value < 0.05
Evidence is classified as strong, moderate, and weak. When scored A in every criteria, evidence is categorized as strong. When scored no C in every criteria but no AAA, evidence is categorized as moderate. Weak evidence is recorded with C in one out of three criteria
Qualitative methodological appraisal of eligible meta-analyses
The qualitative methodological appraisal was conducted using the AMSTAR tool as described in Table 4. Song et al. showed the lowest score of 7, whereas Yu Zhang et al. showed the highest score of 10.5.
Table 4.
Qualitative methodological appraisal of eligible meta-analyses using AMSTAR tool
| References | Checklist | Total | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | ||
| Chen et al. [35] | 1 | 0.5 | 1 | 0.5 | 1 | 1 | 0 | 0.5 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 9.5 |
| Jiang et al. [30] | 1 | 0.5 | 1 | 0.5 | 1 | 1 | 0 | 0.5 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 8.5 |
| Peng et al. [31] | 1 | 0.5 | 1 | 0.5 | 1 | 1 | 0 | 0.5 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 9.5 |
| Song et al., [32] | 1 | 0.5 | 1 | 0 | 0 | 0 | 0 | 0.5 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 7 |
| Hong et al. [33] | 1 | 0.5 | 1 | 0.5 | 1 | 1 | 0 | 0.5 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 9.5 |
| Zhou et al. [36] | 1 | 0.5 | 1 | 0 | 1 | 1 | 0 | 0.5 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 9 |
| Shang et al. [34] | 1 | 0.5 | 1 | 0.5 | 1 | 1 | 0 | 0.5 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 7.5 |
| Gong et al. [37] | 1 | 0.5 | 1 | 0.5 | 1 | 1 | 0 | 0.5 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 8.5 |
Abbreviations: 0, No; 1, Yes; 1.5, Partial Yes; AMSTAR, A Measurement Tool to Assess Systematic Reviews
Discussions
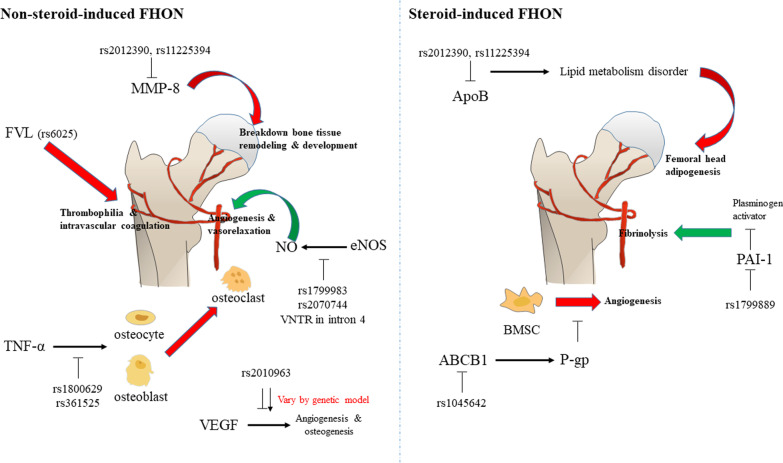
In the present study, the genes with variants in nonsteroid-induced FHON were MMP-8 (rs2012390 and rs11225394), TNF-α (rs1800629 and rs361525), eNOS (VNTR in intron 4, rs1799983, and rs2070744), VEGF (rs2010963), and factor V (rs6025). Among them, the variants in MMP8, TNF-α, eNOS, and factor V showed high significance, and particularly the variants in TNF-α (rs361525) and eNOS (VNTR in intron 4) had more than two types of model significance. Meanwhile, the genes with genetic variants in steroid-induced FHON were ApoB (rs693 and rs1042031), ABCB1 (rs1045642), and PAI-1 (rs1799889). Among them, the variants included in ApoB and PAI-1 showed high significance and particularly the variant in PAI-1 (rs1799889) had more than two types of model significance.
The PAI-1 gene is an important regulator of fibrinolysis because it plays a role as an inhibitor of plasminogen activators [38]. Rs1799889 is the most commonly studied polymorphism in the PAI-1 gene, which has a guanine deletion at the 675 nucleotide position. The PAI-1-675 4G allele shows higher transcriptional activity than the PAI-1-675 5G allele and the PAI-1-675 4G allele is related to higher PAI-1 levels in plasma [39]. In this study, the allele and recessive models of rs1799889 showed a highly significant association with steroid-induced FHON. That is, carriers of the 4G variant of PAI-1 had a higher risk of steroid-induced FHON than those with the 5G variant. It seems that the 4G allele is an important pathogenic factor with a fundamental function of disturbing PAI-1 gene expression. The low expression of the PAI-1 gene could be a cause of FHON with low fibrinolysis.
MMP-8, which is usually expressed in neutrophils but also in chondrocytes and synovial fibroblasts [40], is located on chromosome 11q22.3 [41]. The exact mechanism of the association between MMP-8 and FHON is unclear, but several studies suggested that it was the result of regulatory effects on the breakdown pathway of the extracellular matrix in bone tissue remodeling and development or that MMP-8 could affect femoral head impairment and inflammation [42, 43]. In this study, the heterozygote model of rs11225394 had a strong evidence class and high significance with a p value < 0.00001 and a mean OR of 0.63 in nonsteroid-induced FHON. It is supposed that MMP-8 has a protective effect in nonsteroid-induced FHON.
It is known that TNF-α promotor polymorphisms like TNF-α gene-308 or -238 affect transcriptional activity [44, 45]. Some studies demonstrated that the pathophysiology of nonsteroid-induced FHON was associated with the apoptosis of osteocytes and osteoblasts [31, 46]. In addition, TNF-α was reported to affect osteocytes and osteoblasts to release cytokines related to the proliferation and maturation of osteoclasts [47]. Therefore, polymorphisms in TNF-α could change the activation of osteoblasts and osteoclasts, which would result in the deterioration of nonsteroid-induced FHON. In this study, rs1045642, which is a polymorphism of TNF-α, showed high significance in the allele and recessive models. The mean OR was 0.27, 0.25 in the allele and recessive models, which could mean that the downregulation of TNF-α has a protective effect against nonsteroid-induced FHON.
The ABCB1 gene encodes the transport protein, p-glycoprotein (P-gp), which has crucial functions in pumping foreign substances out of cells [48]. In the study by Ning Han et al., the excessive adipogenesis of bone marrow-derived mesenchymal stem/stromal cells (BMSC) was found when P-gp was inhibited in steroid-induced FHON, indicating that bone formation in the femoral head was inhibited due to decreased BMSCs, which are precursors for osteoblast maturation [49]. In this study, rs1045642 in steroid-induced FHON decreased the risk of disease incidence with a minor T allele. It means that the ABCB1 gene might be an important gene in the regulation of steroid-induced FHON.
The eNOS gene which is located on chromosome 7q35-q36 is known to increase NO [32]. NO is known to mediate angiogenesis and vasorelaxation. However, its key role is in preventing thrombosis, which is the main pathophysiology of nonsteroid-induced FHON [50]. The 27-bp variable VNTR in intron 4 is a polymorphism of eNOS, which includes the wild 4b allele and the mutated 4a allele. This 4b/a polymorphism is related to reduced NO plasma concentrations [51]. In this study, 4b/a polymorphism in the eNOS gene showed high significance in nonsteroid-induced FHON. This might mean that the decreased expression of eNOS could lead to the incidence of nonsteroid-induced FHON. In addition, rs1799983 and rs2070744 polymorphisms in the eNOS gene also showed significance but their heterogeneity was too high (80.20% in rs1799983 and 90% in rs2070744).
VEGF is known to be highly expressed in the necrotic area of FHON. Its major role is in angiogenesis and osteogenesis [52]. The VEGF gene has also been reported to promote bone marrow cells and near endothelial cell proliferation [14, 53]. In this study, rs2010963, known as VEGF -634G/C polymorphisms, showed high significance. When all the genetic models were evaluated, the homozygote and dominant models showed a mean OR of under 1.00, while the recessive model showed a mean OR of over 1.00, suggesting that the genetic models of rs2010963 may have an important role in predicting the risk for FHON.
Factor V (FV) is well known as a component involved in the blood coagulation process [54]. The factor V Leiden (FVL) gene mutation is a typical polymorphism of FV causing thrombophilia and intravascular coagulation disorders [55]. Several studies suggested that thrombosis caused by FVL gene mutation could be the main etiology of nonsteroid-induced FHON [20, 56, 57]. In this study, rs6025, which is a polymorphism of the FVL gene, showed high significance in the homozygote model. The mean OR was 4.55. with strong evidence. This could mean that the downregulation of factor V could increase the risk of FHON occurrence.
APO is the main blood plasma protein mediating normal lipid metabolism by interacting with cellular receptors [58]. It has been reported that APOs are sensitive markers for evaluating lipid metabolic disorders in steroid-induced FHON [17, 59]. In a study by Karami et al., the C allele of rs693 had a high association with high familial cholesterol levels. In contrast, the presence of the T allele had protective effects [60]. Rs1042031 is also known as important for regulating the ApoB binding capacity to cholesterol receptors [35]. In this study, rs693 and rs1042031, which are polymorphisms of ApoB, each showed high significance in the dominant models. Their mean ORs were over 2.5, which means that if ApoB did not function well, the risk of FHON incidence could be increased. These results indicated that lipid metabolism disorders could lead to adipogenesis of the femoral head, which is one of the main causes of steroid-induced FHON [35].
In brief, the nonsteroid-induced associated genes were MMP-8, TNF-α, eNOS, VEGF, and factor V, and the steroid-induced associated genes were ApoB, ABCB1, and PAI-1. The overall gene mechanisms of FHON are presented in Fig. 2.
Fig. 2.
The overall gene mechanisms related to femoral head osteonecrosis (FHON). Red arrow indicates risk factors of FHON, and green arrow indicates protective factors of FHON
Limitations
The present study had several limitations. First, our study excluded gender factors in the data collection. Second, classifications of ethnicity were not specified. Third, further validation of the study results was not conducted. Fourth, although this study included many SNP results from various papers, it was limited by the studies available at the time. Fifth, this study contains a significant amount of meta-analyses derived from various references. Therefore, results might lead to an over-estimation of one or the other genes’ actual significance. Finally, most genetic variations reported in meta-analyses only appear once when searching meta-analyses containing genetic variations to collect only reliable data related to steroid-induced FHON and nonsteroid-induced FHON. This result is thought to be because there were not many meta-analyses selected for the subject of this study, and the genetic variation that each study focuses on is different.
Conclusion
Based on a systematic review of published papers, we organized the genomes associated with FHON and examined each contribution. Our results could give an integrative approach for understanding the mechanism of FHON etiology. It is expected that these results could contribute to the strategy of prediagnosis and evaluating the individual risk of nonsteroid-induced and steroid-induced FHON.
Supplementary Information
Additional file 1. Table S1: Excluded publications with reasons.
Acknowledgements
Not applicable.
Author’s contributions
YJI and LSY contributed to concept, design, supervision, analysis and/or interpretation, literature search, writing manuscript, and critical review; YJI, KYJ, and LSY were involved in materials and data collection and/or processing. All authors read and approved the final manuscript.
Funding
This work was funded by the by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MEST) (No. NRF-2019R1F1A1059208). The National Research Foundation of Korea had no role in design or analysis of the project or the writing of this article.
Availability of data and materials
Not applicable.
Declarations
Consent for publication
Not applicable.
Competing interests
None declared by all authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dubois EL, Cozen L. Avascular (aseptic) bone necrosis associated with systemic lupus erythematosus. JAMA. 1960;174:966–971. doi: 10.1001/jama.1960.03030080028005. [DOI] [PubMed] [Google Scholar]
- 2.Pierre-Jacques H, Glueck CJ, Mont MA, Hungerford DS. Familial heterozygous protein-S deficiency in a patient who had multifocal osteonecrosis. A case report. J Bone Joint Surg Am. 1997;79(7):1079–1084. doi: 10.2106/00004623-199707000-00017. [DOI] [PubMed] [Google Scholar]
- 3.Shah KN, Racine J, Jones LC, Aaron RK. Pathophysiology and risk factors for osteonecrosis. Curr Rev Musculoskelet Med. 2015;8(3):201–209. doi: 10.1007/s12178-015-9277-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Drescher W, Pufe T, Smeets R, Eisenhart-Rothe RV, Jäger M, Tingart M. [Avascular necrosis of the hip—diagnosis and treatment]. Z Orthopadie Unfallchirurgie. 2011;149(2):231–240; quiz 241–242. 10.1055/s-0030-1270984. [DOI] [PubMed]
- 5.Mont MA, Hungerford DS. Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Am. 1995;77(3):459–474. doi: 10.2106/00004623-199503000-00018. [DOI] [PubMed] [Google Scholar]
- 6.Hauzeur JP, Perlmutter N, Appelboom T, Pasteels JL. Medullary impairment at early stage of non-traumatic osteonecrosis of the femoral head. Rheumatol Int. 1991;11(4–5):215–217. doi: 10.1007/BF00332565. [DOI] [PubMed] [Google Scholar]
- 7.Baig SA, Baig M. Osteonecrosis of the femoral head: etiology, investigations, and management. Cureus. 2020 doi: 10.7759/cureus.3171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mont MA, Jones LC, Hungerford DS. Nontraumatic osteonecrosis of the femoral head: ten years later. J Bone Joint Surg Am. 2006;88(5):1117–1132. doi: 10.2106/JBJS.E.01041. [DOI] [PubMed] [Google Scholar]
- 9.Chang C, Greenspan A, Beltran J, Gershwin ME. Osteonecrosis. Kelley Firesteins Textb Rheumatol. 2017 doi: 10.1016/B978-0-323-31696-5.00103-0. [DOI] [Google Scholar]
- 10.Zizic TM, Marcoux C, Hungerford DS, Dansereau JV, Stevens MB. Corticosteroid therapy associated with ischemic necrosis of bone in systemic lupus erythematosus. Am J Med. 1985;79(5):596–604. doi: 10.1016/0002-9343(85)90057-9. [DOI] [PubMed] [Google Scholar]
- 11.Wang A, Ren M, Wang J. The pathogenesis of steroid-induced osteonecrosis of the femoral head: a systematic review of the literature. Gene. 2018;671:103–109. doi: 10.1016/j.gene.2018.05.091. [DOI] [PubMed] [Google Scholar]
- 12.Motomura G, Yamamoto T, Miyanishi K, Yamashita A, Sueishi K, Iwamoto Y. Bone marrow fat-cell enlargement in early steroid-induced osteonecrosis—a histomorphometric study of autopsy cases. Pathol Res Pract. 2005;200(11):807–811. doi: 10.1016/j.prp.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 13.Fan L, Li J, Yu Z, Dang X, Wang K. Hypoxia-inducible factor prolyl hydroxylase inhibitor prevents steroid-associated osteonecrosis of the femoral head in rabbits by promoting angiogenesis and inhibiting apoptosis. PLoS ONE. 2014;9(9):e107774. doi: 10.1371/journal.pone.0107774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Varoga D, Drescher W, Pufe M, Groth G, Pufe T. Differential expression of vascular endothelial growth factor in glucocorticoid-related osteonecrosis of the femoral head. Clin Orthop Relat Res. 2009;467(12):3273–3282. doi: 10.1007/s11999-009-1076-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kerachian MA, Séguin C, Harvey EJ. Glucocorticoids in osteonecrosis of the femoral head: a new understanding of the mechanisms of action. J Steroid Biochem Mol Biol. 2009;114(3–5):121–128. doi: 10.1016/j.jsbmb.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yin L, Li Y, Wang YS. Dexamethasone-induced adipogenesis in primary marrow stromal cell cultures: mechanism of steroid-induced osteonecrosis. Chin Med. 2006;J119(7):581–588. doi: 10.1097/00029330-200604010-00012. [DOI] [PubMed] [Google Scholar]
- 17.Hirata T, Fujioka M, Takahashi KA, et al. ApoB C7623T polymorphism predicts risk for steroid-induced osteonecrosis of the femoral head after renal transplantation. J Orthop Sci Off J Jpn Orthop Assoc. 2007;12(3):199–206. doi: 10.1007/s00776-007-1110-9. [DOI] [PubMed] [Google Scholar]
- 18.Wang XY, Niu XH, Chen WH, et al. Effects of apolipoprotein A1 and B gene polymorphism on avascular necrosis of the femoral head in Chinese population. Zhongguo Gu Shang China J Orthop Traumatol. 2008;21(2):99–102. [PubMed] [Google Scholar]
- 19.Kim TH, Hong JM, Lee JY, et al. Promoter polymorphisms of the vascular endothelial growth factor gene is associated with an osteonecrosis of the femoral head in the Korean population. Osteoarthr Cartil. 2008;16(3):287–291. doi: 10.1016/j.joca.2007.06.017. [DOI] [PubMed] [Google Scholar]
- 20.Björkman A, Svensson PJ, Hillarp A, Burtscher IM, Rünow A, Benoni G. Factor V leiden and prothrombin gene mutation: risk factors for osteonecrosis of the femoral head in adults. Clin Orthop. 2004;425:168–172. doi: 10.1097/00003086-200408000-00023. [DOI] [PubMed] [Google Scholar]
- 21.Sobhan MR, Mahdinezhad-Yazdi M, Moghimi M, et al. Plasminogen activator inhibitor-1 4G/5G polymorphism contributes to osteonecrosis of the femoral head susceptibility: evidence from a systematic review and meta-analysis. NUMBER. 2018;6(6):10. [PMC free article] [PubMed] [Google Scholar]
- 22.Glueck CJ, Fontaine RN, Gruppo R, et al. The plasminogen activator inhibitor-1 gene, hypofibrinolysis, and osteonecrosis. Clin Orthop. 1999;366:133–146. doi: 10.1097/00003086-199909000-00017. [DOI] [PubMed] [Google Scholar]
- 23.Wang B. ABCB1 gene polymorphisms and glucocorticoid-induced avascular necrosis of the femoral head susceptibility: a meta-analysis. Med Sci Monit. 2014;20:2811–2816. doi: 10.12659/MSM.891286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guo FQ, Deng M. Correlation between steroid-induced osteonecrosis of the femoral head and hepatic CYP3A activity: a systematic review and meta-analysis. J Invest Surg. 2019;32(2):118–126. doi: 10.1080/08941939.2017.1385663. [DOI] [PubMed] [Google Scholar]
- 25.Assouline-Dayan Y, Chang C, Greenspan A, Shoenfeld Y, Gershwin ME. Pathogenesis and natural history of osteonecrosis. Semin Arthritis Rheum. 2002;32(2):94–124. doi: 10.1053/sarh.2002.33724b. [DOI] [PubMed] [Google Scholar]
- 26.Jones JP. Intravascular coagulation and osteonecrosis. Clin Orthop. 1992;277:41–53. doi: 10.1097/00003086-199204000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Schroer WC. Current concepts on the pathogenesis of osteonecrosis of the femoral head. Orthop Rev. 1994;23(6):487–497. [PubMed] [Google Scholar]
- 28.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 29.Ioannidis JPA, Boffetta P, Little J, et al. Assessment of cumulative evidence on genetic associations: interim guidelines. Int J Epidemiol. 2008;37(1):120–132. doi: 10.1093/ije/dym159. [DOI] [PubMed] [Google Scholar]
- 30.Jiang L, Zhang C, Wei B. Association of MMP-8 rs2012390 and rs11225394 polymorphisms with osteonecrosis of the femoral head risks: Evidence from a meta-analysis. Medicine. 2018;97(41):e12753. doi: 10.1097/MD.0000000000012753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peng Y, Liu Y, Huang D, Huang W, Shao Z. Association of TNF-α-308(G/A) and -238(G/A) polymorphisms with non-traumatic osteonecrosis of the femoral head risks: a meta-analysis. Int Orthop. 2018;42(7):1711–1721. doi: 10.1007/s00264-018-3859-1. [DOI] [PubMed] [Google Scholar]
- 32.Song GG, Lee YH. Association of eNOS polymorphisms with susceptibility to osteonecrosis of the femur head: a meta-analysis. Z Für Rheumatol. 2017;76(3):267–273. doi: 10.1007/s00393-016-0093-3. [DOI] [PubMed] [Google Scholar]
- 33.Hong GJ, Lin N, Chen LL, Chen XB, He W. Association between vascular endothelial growth factor gene polymorphisms and the risk of osteonecrosis of the femoral head: systematic review. Biomed Rep. 2016;4(1):92–96. doi: 10.3892/br.2015.527. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 34.Shang X, Luo Z, Li X, Hu F, Zhao Q, Zhang W. Meta-analysis of factor V Leiden G1691A polymorphism and osteonecrosis of femoral head susceptibility. Biomed Rep. 2013;1(4):594–598. doi: 10.3892/br.2013.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen X, Zhang L, Liang D, Li J, Liu F, Ma H. Lipid transporter activity-related genetic polymorphisms are associated with steroid-induced osteonecrosis of the femoral head: an updated meta-analysis based on the GRADE guidelines. Front Physiol. 2018;9:1684. doi: 10.3389/fphys.2018.01684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhou Z, Hua Y, Liu J, et al. Association of ABCB1/MDR1 polymorphisms in patients with glucocorticoid-induced osteonecrosis of the femoral head: evidence for a meta-analysis. Gene. 2015;569(1):34–40. doi: 10.1016/j.gene.2015.03.023. [DOI] [PubMed] [Google Scholar]
- 37.Gong LL, Fang LH, Wang HY, et al. Genetic risk factors for glucocorticoid-induced osteonecrosis: a meta-analysis. Steroids. 2013;78(4):401–408. doi: 10.1016/j.steroids.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 38.Zhao L, Huang P. Plasminogen activator inhibitor-1 4G/5G polymorphism is associated with type 2 diabetes risk. Int J Clin Exp Med. 2013;6(8):632–640. [PMC free article] [PubMed] [Google Scholar]
- 39.Liang XN, Xie L, Cheng JW, et al. Association between PAI-1 4G/5G Polymorphisms and osteonecrosis of femoral head: a Meta-analysis. Thromb Res. 2013;132(2):158–163. doi: 10.1016/j.thromres.2013.06.023. [DOI] [PubMed] [Google Scholar]
- 40.Cole AA, Chubinskaya S, Schumacher B, et al. Chondrocyte matrix Metalloproteinase-8: human articular chondrocytes express neutrophil collagenase (∗) J Biol Chem. 1996;271(18):11023–11026. doi: 10.1074/jbc.271.18.11023. [DOI] [PubMed] [Google Scholar]
- 41.Hanemaaijer R, Sorsa T, Konttinen YT, et al. Matrix metalloproteinase-8 is expressed in rheumatoid synovial fibroblasts and endothelial cells. Regulation by tumor necrosis factor-alpha and doxycycline. J Biol Chem. 1997;272(50):31504–31509. doi: 10.1074/jbc.272.50.31504. [DOI] [PubMed] [Google Scholar]
- 42.Du J, Jin T, Cao Y, et al. Association between genetic polymorphisms of MMP8 and the risk of steroid-induced osteonecrosis of the femoral head in the population of northern China. Medicine. 2016;95(37):e4794. doi: 10.1097/MD.0000000000004794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chen J, Liu W, Cao Y, et al. MMP-3 and MMP-8 single-nucleotide polymorphisms are related to alcohol-induced osteonecrosis of the femoral head in Chinese males. Oncotarget. 2017;8(15):25177–25188. doi: 10.18632/oncotarget.15587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pardo A, Selman M. Idiopathic pulmonary fibrosis: new insights in its pathogenesis. Int J Biochem Cell Biol. 2002;34(12):1534–1538. doi: 10.1016/s1357-2725(02)00091-2. [DOI] [PubMed] [Google Scholar]
- 45.Kroeger KM, Carville KS, Abraham LJ. The -308 tumor necrosis factor-alpha promoter polymorphism effects transcription. Mol Immunol. 1997;34(5):391–399. doi: 10.1016/s0161-5890(97)00052-7. [DOI] [PubMed] [Google Scholar]
- 46.Shibahara M, Nishida K, Asahara H, et al. Increased osteocyte apoptosis during the development of femoral head osteonecrosis in spontaneously hypertensive rats. Acta Med Okayama. 2000;54(2):67–74. doi: 10.18926/AMO/32287. [DOI] [PubMed] [Google Scholar]
- 47.Dai CY, Chuang WL, Lee LP, et al. Associations of tumour necrosis factor alpha promoter polymorphisms at position -308 and -238 with clinical characteristics of chronic hepatitis C. J Viral Hepat. 2006;13(11):770–774. doi: 10.1111/j.1365-2893.2006.00767.x. [DOI] [PubMed] [Google Scholar]
- 48.Gunes A, Spina E, Dahl ML, Scordo MG. ABCB1 polymorphisms influence steady-state plasma levels of 9-hydroxyrisperidone and risperidone active moiety. Ther Drug Monit. 2008;30(5):628–633. doi: 10.1097/FTD.0b013e3181858ca9. [DOI] [PubMed] [Google Scholar]
- 49.Han N, Yan Z, Guo C, et al. Effects of P-glycoprotein on steroid-induced osteonecrosis of the femoral head. Calcif Tissue Int. 2010;87(3):246–253. doi: 10.1007/s00223-010-9385-9. [DOI] [PubMed] [Google Scholar]
- 50.Tan XL, Xue YQ, Ma T, et al. Partial eNOS deficiency causes spontaneous thrombotic cerebral infarction, amyloid angiopathy and cognitive impairment. Mol Neurodegener. 2015 doi: 10.1186/s13024-015-0020-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tsukada T, Yokoyama K, Arai T, et al. Evidence of association of the ecNOS gene polymorphism with plasma NO metabolite levels in humans. Biochem Biophys Res Commun. 1998;245(1):190–193. doi: 10.1006/bbrc.1998.8267. [DOI] [PubMed] [Google Scholar]
- 52.Hoeben A, Landuyt B, Highley MS, Wildiers H, Oosterom ATV, Bruijn EAD. Vascular endothelial growth factor and angiogenesis. Pharmacol Rev. 2004;56(4):549–580. doi: 10.1124/pr.56.4.3. [DOI] [PubMed] [Google Scholar]
- 53.Suzuki O, Bishop AT, Sunagawa T, Katsube K, Friedrich PF. VEGF-promoted surgical angiogenesis in necrotic bone. Microsurgery. 2004;24(1):85–91. doi: 10.1002/micr.10190. [DOI] [PubMed] [Google Scholar]
- 54.Rosing J, Tans G. Coagulation factor V: an old star shines again. Thromb Haemost. 1997;78(1):427–433. doi: 10.1055/s-0038-1657564. [DOI] [PubMed] [Google Scholar]
- 55.Bertina RM, Koeleman BP, Koster T, et al. Mutation in blood coagulation factor V associated with resistance to activated protein C. Nature. 1994;369(6475):64–67. doi: 10.1038/369064a0. [DOI] [PubMed] [Google Scholar]
- 56.Ekmekci Y, Keven K, Akar N, et al. Thrombophilia and avascular necrosis of femoral head in kidney allograft recipients. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc Eur Ren Assoc. 2006;21(12):3555–3558. doi: 10.1093/ndt/gfl400. [DOI] [PubMed] [Google Scholar]
- 57.Celik A, Tekis D, Saglam F, et al. Association of corticosteroids and factor V, prothrombin, and MTHFR gene mutations with avascular osteonecrosis in renal allograft recipients. Transplant Proc. 2006;38(2):512–516. doi: 10.1016/j.transproceed.2005.12.062. [DOI] [PubMed] [Google Scholar]
- 58.Marcel YL, McPherson R, Hogue M, et al. Distribution and concentration of cholesteryl ester transfer protein in plasma of normolipemic subjects. J Clin Invest. 1990;85(1):10–17. doi: 10.1172/JCI114397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shuai B, Shen L, Yang YP, Xie J, Shou ZX, Wei B. Low plasma adiponectin as a potential biomarker for osteonecrosis of the femoral head. J Rheumatol. 2010;37(10):2151–2155. doi: 10.3899/jrheum.100342. [DOI] [PubMed] [Google Scholar]
- 60.Karami F, Salahshourifar I, Houshmand M. The study of rs693 and rs515135 in APOB in people with familial hypercholestrolemia. Cell J Yakhteh. 2019;21(1):86–91. doi: 10.22074/cellj.2019.5692. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Table S1: Excluded publications with reasons.
Data Availability Statement
Not applicable.