Abstract
We herein present the case of a 28-year-old male patient who presented with fever and bilateral upper eyelid edema without other upper airway symptoms and was diagnosed with acute dacryoadenitis due to Epstein-Barr virus (EBV) infection. The patient’s medical history was unremarkable. Laboratory tests revealed lymphocytosis with atypical lymphocytes and abnormal liver function tests. Physical examination and computed tomography revealed swelling in the lacrimal glands, and serological tests confirmed EBV infection. Although rare, ocular symptoms of primary EBV infection are important for diagnosis. Acute dacryoadenitis should be considered as a rare manifestation and an underdiagnosed complication of primary EBV infection.
Keywords: acute dacryoadenitis, Epstein-Barr virus, lacrimal gland, upper eye lid edema
Primary infection with Epstein-Barr virus (EBV), a prevalent pathogen, causes infectious mononucleosis (IM) in young individuals. Typical clinical symptoms of IM include fever, sore throat, anterior and posterior cervical lymphadenopathy, and hepatosplenomegaly [1, 2]. Complications of acute EBV infection include hepatitis, airway obstruction, and splenic rupture, whereas ocular involvement is rare [3]. However, conjunctivitis, dacryoadenitis, episcleritis, keratitis, and iritis have been reported in some cases [4–8].
As an important ocular finding in patients with IM, upper eyelid edema, also known as the Hoagland sign, was first reported by Hoagland et al., who noted its presence in 33.9% of young patients admitted for IM [9]. More recent studies suggest that the rate of upper eyelid edema varies with age, ranging from 11.5% to 41.0%, with higher frequency observed in children [10, 11]. Upper eyelid edema may appear as the initial symptom before the emergence of more common symptoms such as sore throat and is therefore an important finding that can facilitate diagnosis [12]. In 3.6%–6.6% of patients with IM, upper eyelid edema is the chief complaint at the initial visit [9, 13].
Acute dacryoadenitis is a rare ocular complication of EBV infection and can be challenging to differentiate from upper eyelid edema. Acute dacryoadenitis is caused by inflammation of the lacrimal gland, which is located lateral to the extraconal orbital fat [14]. While the prevalence of acute dacryoadenitis is unknown, it is commonly reported in children and young adults. Acute dacryoadenitis is usually associated with infectious diseases, and viruses are the more common causative pathogens compared with bacteria [14]. EBV is often overlooked as the causative pathogen in acute dacryoadenitis, although it is the most commonly reported etiology [4].
We herein report the case of a patient with acute dacryoadenitis and EBV infection who did not exhibit the typical symptoms of IM.
CASE REPORT
A 28-year-old man without medical history visited the emergency department with bilateral eyelid swelling for 1 week. The patient indicated that eyelid edema appeared soon after the onset of fever. The patient was an ex-smoker, with 10 cigarettes per day for 8 years, and was consuming ~1.8 units of alcohol per day. He had no history of food or medication allergies. He was an office worker and did not have contact with sick individuals.
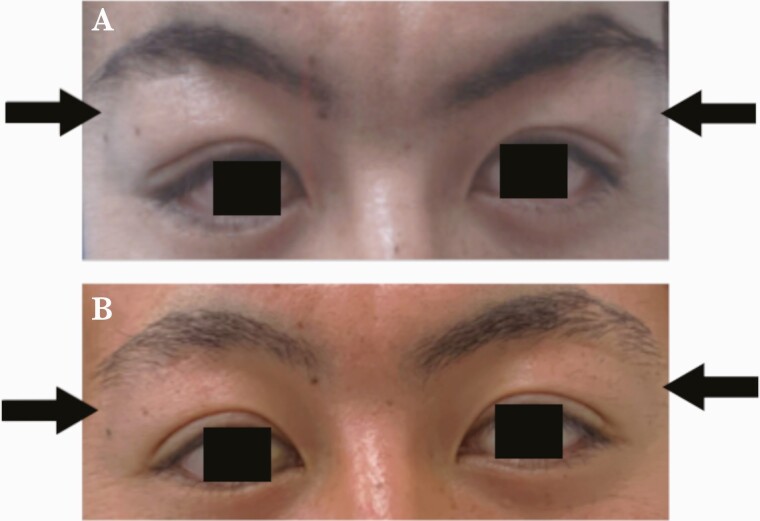
At presentation, the patient’s general appearance was good and afebrile (37.0°C). There were no other symptoms such as cough, sore throat, cervical pain, fatigue, and rash. On examination, ocular pain, diplopia, conjunctivitis, and discharge were absent; however, a mild pulling discomfort was observed during external ocular examination. Swelling on the lateral sides of both upper eyelids was noted, but redness and heat were absent (Figure 1A). Mild tenderness was observed only on the left upper eyelid. The thyroid gland and tonsils were normal, and leukoplakia, cervical lymphadenopathy, and hepatosplenomegaly were absent.
Figure 1.
Bilateral lacrimal gland swelling on day 1 (A, arrow) and after 3 weeks (B, arrow).
The laboratory test results were as follows: leucocyte count, 12 170/μL (reference, 3300–8600/μL); absolute lymphocyte count, 7423/μL (reference, 990–3870/μL); absolute neutrophil count, 3833/μL (reference, 1551–5246/μL); atypical lymphocytes, 3.5% (425/μL); platelet count, 165 × 109/L (reference, 158–348 × 109/L); aspartate aminotransferase, 270 U/L (reference, 13–30 U/L); alanine aminotransferase, 354 U/L (reference, 10–42 U/L); serum lactate dehydrogenase, 642 U/L (reference, 124–222 U/L); and C-reactive protein level, 0.18 mg/dL (reference, 0–0.14 mg/dL). The patient was negative for antinuclear, anti-Ro, and anti-La antibodies, but positive for IgM and immunoglobulin G (IgG) antibodies against EBV viral capsid antigens (VCAs). The patient was negative for EBV nuclear antigen (EBNA) IgG based on enzyme-linked immunosorbent assay.
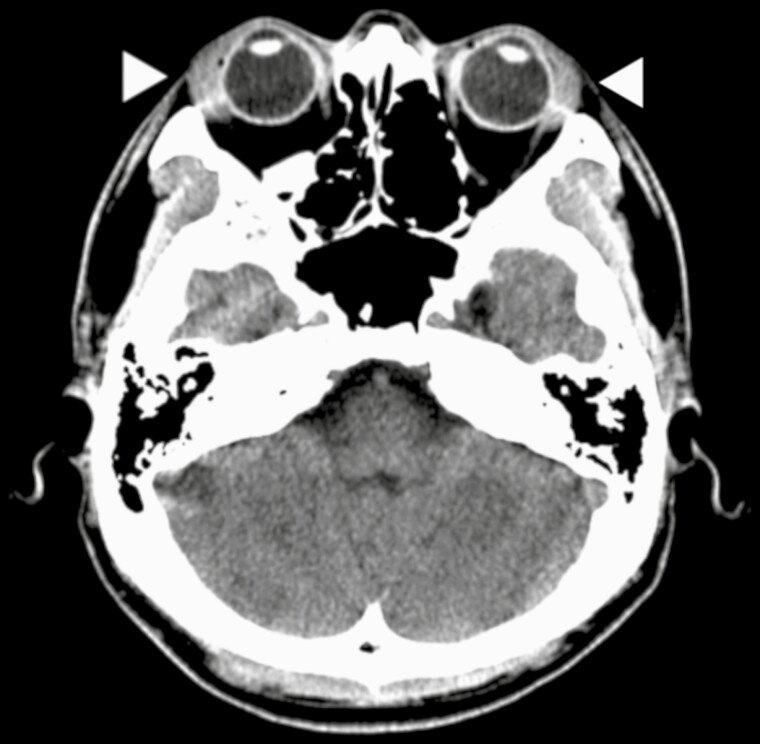
Head computed tomography revealed bilateral swelling of the lacrimal glands (Figure 2), and abdominal ultrasonography revealed mild splenomegaly. There were no abnormalities in visual acuity, intraocular pressure, eye movement, or visual field.
Figure 2.
Head computed tomography scan revealed bilateral lacrimal gland swelling (arrowhead).
In addition to the presence of acute lacrimal gland swelling, findings suggestive of viral infection, including an elevated lymphocyte/neutrophil ratio, atypical lymphocytes, elevated liver function tests and splenomegaly, and serology results supporting EBV infection, led to the definitive diagnosis of acute dacryoadenitis due to primary EBV infection.
Despite the persistence of bilateral lacrimal gland swelling, improvement was observed on the 10th day after visiting without treatment. At 3-week follow-up, the eyelid swelling had completely disappeared, and there was no recurrence or worsening (Figure 1B).
DISCUSSION
Acute dacryoadenitis can be caused by bacterial or viral infections. Among the causative viral pathogens are EBV, mumps virus, adenovirus, herpes simplex virus, and herpes zoster virus, whereas the main bacterial pathogens that can cause acute dacryoadenitis are Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus influenzae, and Moraxella catarrhalis [14]. In contrast, chronic dacryoadenitis is often caused by autoimmune diseases such as Sjögren syndrome, sarcoidosis, and IgG4-related diseases [14]. EBV is an important causative microorganism for acute viral dacryoadenitis. Marcus et al. reported that EBV was serologically detected in approximately one-third of patients with confirmed acute dacryoadenitis [4]. Acute dacryoadenitis associated with EBV infection has been reported to occur in about 1 in every 300 patient with EBV infection, although the exact incidence is not well known [15].
During primary infection, EBV gains access via the epithelial cells in the oral cavity and infects B cells. After resolution of the initial infection, EBV resides in memory B cells and persists throughout life. EBV has been detected in salivary glands and saliva [1, 16]. As exocrine salivary tissues, lacrimal glands comprise mucosal-associated lymphoid tissue, and EBV has been demonstrated to infect lacrimal glands; EBV DNA was detected in biopsy specimens of lacrimal glands in 32% of healthy individuals [17]. Additionally, the EBV genome can be isolated in tear fluid [18]. Furthermore, EBV DNA can be detected other ocular tissues and fluids such as cornea, aqueous humor, vitreous humor, and iris [19]. Overall, these findings suggest that lacrimal glands are among the lymphoid tissues that can be infected by EBV and that EBV causes ocular symptoms by direct infection of ocular tissues. However, in primary EBV infection, EBV DNA exist in both peripheral blood and tissue. Most of the EBV DNA detected by PCR is an episomal or naked DNA rather than true virion [20]. Therefore, it is difficult to truly demonstrate the presence of EBV DNA in human tissues, including the lacrimal gland. On the other hand, a histopathological examination of lacrimal gland biopsy specimens from patients with dacryoadenitis revealed focal accumulation of lymphocytes in the lacrimal gland and EBV-specific capsid antigen positivity [5].
The present patient developed acute dacryoadenitis as the initial manifestation of late primary EBV infection. Typically, most people acquire EBV at an earlier age, with 92% in the 20s and 95% in the 40s [21]. Our patient presented with only upper eyelid swelling in the absence of erythema and had mild pain localized only to the left upper eyelid. Swelling of the lateral upper eyelid is a common clinical manifestation of acute dacryoadenitis. Acute dacryoadenitis can be painless, although most patients report mild pain on palpation of the upper eyelid [4, 6, 8, 19]. Erythema is often absent; however, secondary bacterial infection or dacryocystitis should be suspected in patients with severe erythema and pain with lacrimal scrotum swelling [22, 23].
Acute dacryoadenitis is usually observed early in the course of EBV infection and sometimes precedes the typical symptoms of IM [6]. Several studies reported that fever and lacrimal gland swelling were the only symptoms of primary EBV infection in patients with pharyngitis or other symptoms [4]. Similar to the current case, the lack of other typical symptoms of IM often hinders accurate diagnosis. In the current case, the initial complaint was eyelid symptoms, and physical examination and computed tomography revealed lacrimal gland swelling. In the absence of careful physical examination, distinguishing between eyelid edema and lacrimal gland swelling may be difficult. Therefore, acute dacryoadenitis may be underdiagnosed in patients with EBV infection and may not be accurately differentiated from upper eyelid edema in some cases.
In most cases, acute dacryoadenitis improves spontaneously, although some studies have reported that symptoms can persist for 3–6 weeks [4]. In the current case, the symptoms improved 14 days after onset without any treatment. The efficacy of corticosteroids, which are used in some cases, is unknown, and their routine use is not recommended [6]. In patients failing to exhibit improvement, additional investigation is necessary for other autoimmune diseases, including Sjögren syndrome, IgG4-related diseases, and sarcoidosis, as well as secondary bacterial infections [14]. In summary, acute dacryoadenitis is a rare ocular manifestation of primary EBV infection. Ocular symptoms may appear as an early manifestation of EBV infection and are important for initial diagnosis.
Acknowledgments
Financial support. None to declare.
Potential conflicts of interest. All authors: no reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Patient consent. An ethical committee approval was not applicable for this article type. Written consent for publication was obtained from the patient.
Author contributions. Satoshi Hayano: conceptualization, writing, original draft preparation; Naruhiko Nakada: writing, reviewing, editing; Masayuki Kashima: writing, reviewing, editing, supervising.
References
- 1. Luzuriaga K, Sullivan JL.. Infectious mononucleosis. N Engl J Med 2010; 362:1993–2000. [DOI] [PubMed] [Google Scholar]
- 2. Lennon P, Crotty M, Fenton JE.. Infectious mononucleosis. BMJ 2015; 350:h1825. [DOI] [PubMed] [Google Scholar]
- 3. Fugl A, Andersen C.. Epstein-Barr virus and its association with disease - a review of relevance to general practice. BMC Fam Pract 2019; 20:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rhem MN, Wilhelmus KR, Jones DB.. Epstein-Barr virus dacryoadenitis. Am J Ophthalmol 2000; 129:372–5. [DOI] [PubMed] [Google Scholar]
- 5. Merayo-Lloves J, Baltatzis S, Foster CS.. Epstein-Barr virus dacryoadenitis resulting in keratoconjunctivitis sicca in a child. Am J Ophthalmol 2001; 132:922–3. [DOI] [PubMed] [Google Scholar]
- 6. Marchese-Ragona R, Marioni G, Staffieri A, de Filippis C.. Acute infectious mononucleosis presenting with dacryoadenitis and tonsillitis. Acta Ophthalmol Scand 2002; 80:345–6. [DOI] [PubMed] [Google Scholar]
- 7. Matoba AY. Ocular disease associated with Epstein-Barr virus infection. Surv Ophthalmol 1990; 35:145–50. [DOI] [PubMed] [Google Scholar]
- 8. Ghauri AJ, Keane PA, Scotcher SM, Clarke JL, Madge SN.. Acute dacryocystitis associated with Epstein-Barr virus infection. Orbit 2011; 30:245–8. [DOI] [PubMed] [Google Scholar]
- 9. Hoagland RJ. Infectious mononucleosis. Am J Med 1952; 13:158–71. [DOI] [PubMed] [Google Scholar]
- 10. Sasaki Y, Ishii T, Maeda T, et al. Sex difference in clinical presentation of patients with infectious mononucleosis caused by Epstein-Barr virus. J Infect Chemother 2020; 26:1181–5. [DOI] [PubMed] [Google Scholar]
- 11. Wu Y, Ma S, Zhang L, et al. Clinical manifestations and laboratory results of 61 children with infectious mononucleosis. J Int Med Res 2020; 48:030006052092455300060520924550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Demonchy E, Pulcini C.. Three cases of primary EBV infection in young adults manifested by periorbital and eyelid oedema. Infection 2013; 41:1029–30. [DOI] [PubMed] [Google Scholar]
- 13. Stevens JE, Bayrd ED, Heck FJ.. Infectious mononucleosis; a study of 210 sporadic cases. Am J Med 1951; 11:202–8. [DOI] [PubMed] [Google Scholar]
- 14. Patel R, Patel BC.. Dacryoadenitis. StatPearls; 2021. [Google Scholar]
- 15. Jones BR. Lacrimal disease associated with infectious mononucleosis. Trans Ophthalmol Soc UK 1955; 75:101–19. [PubMed] [Google Scholar]
- 16. Odumade OA, Hogquist KA, Balfour HH Jr. Progress and problems in understanding and managing primary Epstein-Barr virus infections. Clin Microbiol Rev 2011; 24:193–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Crouse CA, Pflugfelder SC, Cleary T, Demick SM, Atherton SS.. Detection of Epstein-Barr virus genomes in normal human lacrimal glands. J Clin Microbiol 1990; 28:1026–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pflugfelder SC, Crouse C, Pereira I, Atherton S.. Amplification of Epstein-Barr virus genomic sequences in blood cells, lacrimal glands, and tears from primary Sjögren’s syndrome patients. Ophtalmol 1990; 97:976–84. [DOI] [PubMed] [Google Scholar]
- 19. Aburn NS, Sullivan TJ.. Infectious mononucleosis presenting with dacryoadenitis. Ophtalmol 1996; 103:776–8. [DOI] [PubMed] [Google Scholar]
- 20. Kimura H, Ito Y, Suzuki R, Nishiyama Y.. Measuring Epstein-Barr virus (EBV) load: the significance and application for each EBV-associated disease. Rev Med Virol 2008; 18:305–19. [DOI] [PubMed] [Google Scholar]
- 21. Sharifipour S, Davoodi Rad K.. Seroprevalence of Epstein-Barr virus among children and adults in Tehran, Iran. New Microbes New Infect 2020; 34:100641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Steele RJ, Meyer DR.. Nasolacrimal duct obstruction and acute dacryocystitis associated with infectious mononucleosis (Epstein-Barr virus). Am J Ophthalmol 1993; 115:265–6. [DOI] [PubMed] [Google Scholar]
- 23. Marqués Fernández VE, Galindo Ferreiro A.. Acute dacryocystitis retention syndrome due to Epstein-Barr virus. Arch Soc Esp Oftalmol 2021; 96:321–5. [DOI] [PubMed] [Google Scholar]