Abstract
Background and Aims:
The efficacy of bilateral nasociliary and maxillary nerve blocks combined with general anaesthesia on intraoperative opioids consumption, emergence and recovery outcomes in adult patients is not well established. We conducted this study to test the hypothesis that the above blocks, combined with general anaesthesia, decrease the intraoperative opioid consumption following nasal surgery.
Methods:
In this prospective, double-blinded, randomised controlled study, 51 adult patients undergoing elective nasal surgery under general anaesthesia were randomised into one of two groups. Group A (n = 26) received bilateral nasociliary and maxillary nerve blocks with 12 mL of equal volumes of 0.5% bupivacaine and 2% lignocaine after induction of general anaesthesia. Group B (n = 25) did not receive any block (control group). The primary endpoint was the total intraoperative dose of fentanyl consumed. The secondary endpoints were the grade of cough, emergence agitation, the grade of post-operative nausea and vomiting, time to the first analgesia and time to post-anaesthesia care unit discharge.
Results:
The mean total intraoperative fentanyl dose (μg) was significantly lower in group A than in group B (2.31 ± 11.76 vs. 41.20 ± 31.00, P = 0.00). The incidence of emergence agitation was lower in group A than group B (11.5% vs. 88%, P = 0.00). The time to the first analgesia was significantly longer in group A than group B (543.27 vs. 199.84 min, P = 0.017).
Conclusion:
The pre-emptive administration of bilateral nasociliary and maxillary nerve block for nasal surgery is an effective technique for reducing the intraoperative dose of fentanyl and emergence agitation.
Keywords: Anaesthesia, maxillary, nasal surgery, nasociliary, nerve blocks, pre-emptive
INTRODUCTION
Nasal surgeries done under general anaesthesia can usually produce mild to moderate post-operative pain, but there can be unexpectedly high levels of post-operative pain in some instances.[1,2] This warrants appropriate pain management strategies as it can lead to emergence agitation, which may lead to self-extubation causing severe complications such as bleeding, aspiration, hypoxia or reoperation.[3,4] In this setting, the use of high doses of narcotics, to combat pain may produce decreased alertness, respiratory depression, hypoxia, nausea and vomiting. However, these side effects can be avoided when regional nerve block techniques are added with general anaesthesia. Pre-emptive analgesia is a pain management strategy initiated before surgery to prevent central sensitisation invoked by the incisional and inflammatory injuries occurring during surgery, and this technique is known to produce effective post-operative analgesia.[5] Facial nerve blocks are described for outpatient nasal surgeries, but their use for nasal procedures of prolonged duration and with risk of bleeding is limited.[6] Among these described nerve blocks, nasociliary and maxillary nerves form the primary nerve supply of the nose, nasal mucosa, septum and nasal cavity.[7] However, the importance of these nerve blocks when combined with general anaesthesia on intraoperative opioids consumption, emergence and recovery measures has not been previously estimated. We, therefore, conducted this study with the primary aim of determining the effect of pre-emptive bilateral maxillary and nasociliary nerve blocks on the dose of intraoperative fentanyl in nasal surgery under general anaesthesia. The secondary outcome measures were the effect of such nerve blocks on the emergence and recovery characteristics in terms of grade of cough, emergence agitation, post-operative nausea and vomiting (PONV), time to first analgesia and post-anaesthesia care unit (PACU) discharge.
METHODS
This double-blinded, prospective, randomised controlled study was certified by the Institutional Research and Human Ethics Committee and registered with the Clinical Trial Registry, India (CTRI/2019/11/022114). The study was conducted from November 2019 to August 2020 at a tertiary academic hospital. Patients aged between 18 to 60 years, having American Society of Anesthesiologists (ASA) physical status I and II, and undergoing elective nasal surgeries were included in the study. Patients with allergy to local anaesthetic solution, bleeding disorder, pregnancy or unable to comprehend the study protocol were excluded. After obtaining written informed consent, 51 patients were randomised using computer-generated random numbers and allocated into one of the two groups (group A or group B) [Figure 1]. Patients in group A (n = 26) received bilateral nasociliary and maxillary nerve block with 12 mL of the local anaesthetic mixture (equal volume of 0.5% bupivacaine and 2% lignocaine) after administration of general anaesthesia. Group B (n = 25) patients did not receive any nerve block (control group). For blinding, a regional anaesthesia trolley was kept open with the drugs, and syringes and plasters were applied on both sides of injection sites in patients in both groups. The nerve block was performed by the primary investigator involved in the study. The patient and the second investigator collecting data were blinded.
Figure 1.
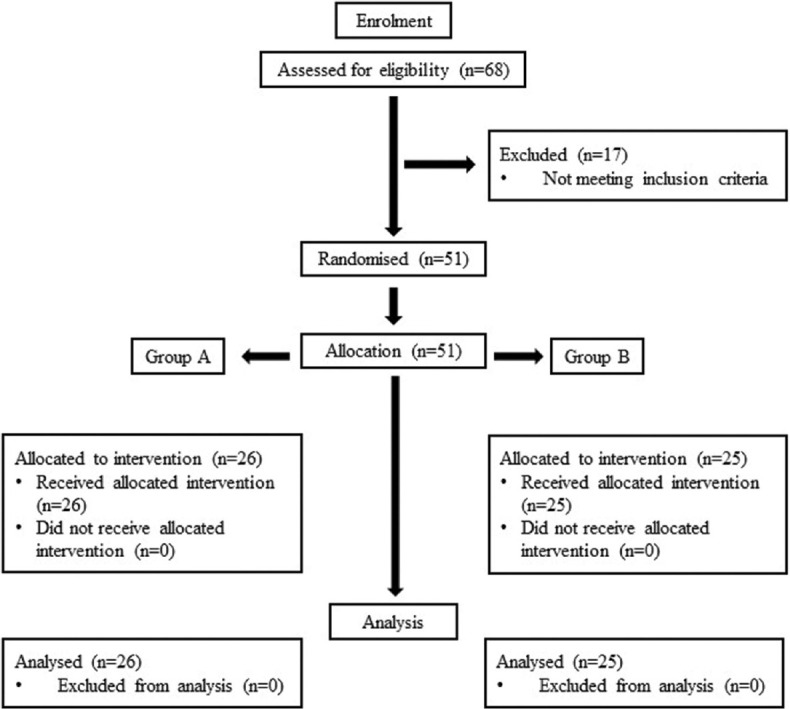
The Consolidated Standards of Reporting Trials (CONSORT) flow diagram
The patients enroled were advised a fasting period of at least 6 h before surgery. They received oral premedication with tablet alprazolam 0.5 mg per oral (PO) on the night before surgery and tablet ranitidine 150 mg PO on the day of surgery. In the preoperative holding room, intravenous access was secured and adrenaline packing (without local anaesthetic) was done as part of routine care. On arrival in the operating room, standard monitors including electrocardiography, non-invasive blood pressure and pulse oximetry were applied and baseline values were recorded. All patients were given 1 mg of intravenous midazolam before the induction of anaesthesia. General anaesthesia was induced following 3 min of preoxygenation with fentanyl 2 μg/kg and propofol given in successive 30 mg doses every 10 s until response to verbal commands was lost. Vecuronium bromide 0.1 mg/kg was provided intravenously to assist tracheal intubation. Following induction of general anaesthesia, the pre-emptive nerve block was administered depending on group allocation.
The nasociliary nerve block was given using a 24-gauge needle, inserted 1 cm above the inner canthus and directed medially and backward, keeping in contact with bone at the anterior ethmoidal foramen with 1 mL of the study drug on either side [Figure 2a]. The maxillary nerve block was performed using a lateral extraoral approach.[8] The 21-gauge needle was inserted perpendicular to the skin at a point below the midpoint of the zygomatic arch overlying the coronoid arch of the mandible into the infratemporal fossa until it contacted the lateral wall of the lateral pterygoid plate. Then the needle was advanced superiorly and anteriorly, for about half a centimetre, to reach the pterygopalatine fossa. After negative aspiration, 5 mL of the study drug was administered on either side [Figure 2b]. Anaesthesia was maintained with sevoflurane in oxygen and 66% nitrous oxide to achieve an end-tidal concentration equivalent to 1 minimum alveolar concentration. Positive pressure ventilation was initiated with a tidal volume of 8 mL/kg with an adjusted respiratory rate to maintain end-tidal carbon dioxide between 35 and 40 mmHg. The surgery was commenced 10 min later to allow for the full effect of the block. For any 20% increase in mean arterial pressure or heart rate intraoperatively, a rescue bolus of intravenous fentanyl 1 μg/kg was given and the total intraoperative dose of fentanyl (μg/kg) (the primary outcome measure) was recorded. Intraoperative adrenaline packing was minimised and no significant haemodynamic changes were noted. When the surgeon began nasal packing at the end of the surgery, sevoflurane administration was discontinued and the fresh gas flow rate was increased to 6 L/min of oxygen. At the beginning of spontaneous breathing by the patient, the reversal of neuromuscular blockade was done with a standard dose of neostigmine and glycopyrrolate. The trachea was extubated when the patient spontaneously breathed with tidal volume 5–8 mL/kg and could respond to a verbal request. During this time, the degree of agitation was measured using the Riker sedation-agitation scale and the maximum agitation score during this period was noted. Emergence agitation is defined as any score on the sedation-agitation scale ≥5.[9] Besides, the grade of cough during this period was assessed using a four-point scale [0 = no cough; 1 = single cough; 2 = persistent cough lasting 5 s and 3 = persistent cough lasting ≥5 s or bucking]. If the score was ≥2, then inj. lignocaine (xylocard) 1 mg/kg was given intravenously. Desaturation, laryngospasm and other respiratory complications were recorded during extubation, and the same was managed as per the attending anaesthesiologist. In the PACU, the quality of recovery was assessed using modified Aldrete scoring on arrival and then every 15 min until 60 min. On the same schedule, pain intensity was assessed using the pain Visual Analogue Scale (VAS), and the time taken for the first request of analgesia was noted (period from the PACU arrival to the first request made by the patient for rescue analgesics). Patients were allowed to receive intravenous fentanyl 0.5 μg/kg as rescue analgesia if VAS >3. PONV was assessed using four-point nausea and vomiting scale. [0 = no nausea; 1 = mild nausea; 2 = severe nausea requiring anti-emetics and 3 = retching, vomiting or both]. Patients with PONV (score ≥2) were treated with intravenous ondansetron 4 mg. Patients were discharged from PACU when their modified Aldrete score was ≥9 and the time to PACU discharge was recorded.
Figure 2.

Shows point of needle placement landmark for (a) nasociliary nerve block (b) maxillary nerve block
The target sample size was calculated from the study done by Boselli et al.[10] In this study, the total perioperative morphine dose in the control group was 9.5 ± 3 mg (mean ± standard deviation), where no nerve block was given, and the total morphine dose is converted to equianalgesic fentanyl dose (95 μg). Assuming a power of 80%, a level of significance of 0.05, 20 subjects were required in each group to detect a 30% reduction in total fentanyl consumption. Our sample size was taken as 25 in each group considering possible dropouts. The statistical analysis was done using Statistical Package for Social Sciences version 16 (International Business Machines Corp, Armonk, New York, United States of America). Categorical variables were presented as a percentage, and continuous variables were presented as mean ± standard deviation with a 95% confidence interval. Continuous variables were analysed using Student's t-test, and categorical variables were analysed using Fisher's exact test or Chi-square test as required. P value < 0.05 was considered statistically significant.
RESULTS
This study included 51 patients by the consecutive sampling method [Figure 1].
Patient characteristics and surgical procedures were similar between the groups [Table 1]. The mean total intraoperative fentanyl dose (μg) was significantly lower in group A than in group B (2.31 ± 11.76 vs. 41.20 ± 31.00, P = 0.00) [Table 2]. One patient out of 26 (3.8%) required a fentanyl repeat dose intraoperatively in group A, whereas 17 patients out of 25 (68%) required a fentanyl repeat dose in group B. Analysis of emergence characteristics outcomes revealed a reduction in the incidence of emergence agitation (11.5% vs. 88%, P = 0.00) and lower grade of cough requiring nil intervention during emergence (92.3% vs. 56%, P = 0.001). Only two patients in group A had a persistent cough (grade 3) when compared with eleven patients in group B (P = 0.00) [Table 2].
Table 1.
Patient characteristics and details of surgical procedures
| Group A (n=26) | Group B (n=25) | P | |
|---|---|---|---|
| Age (years) | 36.73 (8.92) | 35.08 (11.243) | 0.87 |
| Gender (M:F) | 21:5 | 15:10 | 0.11 |
| BMI (kg/m2) | 24.712 (2.50) | 23.22 (2.18) | 0.522 |
| ASA (I/II) | 18/8 | 17/8 | 0.92 |
| Surgery | |||
| FESS | 6 | 7 | 0.58 |
| Septoplasty | 14 | 14 | |
| FESS + Polypectomy | 6 | 4 | |
| Duration of surgery in minutes | 80.69 (28.426) | 86.32 (24.534) | 0.161 |
BMI, Body mass index; ASA, American Society of Anesthesiologists; FESS, Functional endoscopic sinus surgery. Values are represented as means (± standard deviation) or number; group A: nerve block group; group B: control group
Table 2.
Intraoperative fentanyl requirement, emergence and recovery characteristics of the patient
| Group A (n=26) | Group B (n=25) | P | |
|---|---|---|---|
| Intraoperative fentanyl requirement (µg) | 2.31 (11.77) | 41.2 (31) | 0.00 |
|
| |||
| Emergence Characteristics | |||
|
| |||
| Grade of Cough during Emergence | |||
| Not requiring intervention | 24 (92.3) | 14 (56) | 0.001 |
| Requiring intervention | 2 (7) | 11 (44) | 0.00 |
| Emergence agitation | 3 (11.5) | 22 (88) | 0.00 |
|
| |||
| Recovery characteristics | |||
|
| |||
| Grade of PONV requiring anti-emetics | 1 (3.8) | 4 (16) | 0.07 |
| Time to first analgesia (minutes) | 543.27 (156.5) | 199.84 (206) | 0.02 |
| Time to PACU discharge (minutes) | 25.73 (6.4) | 32.44 (7.8) | 0.20 |
PONV, post-operative nausea and vomiting; PACU, post-anaesthesia care unit. Values are represented as mean (±standard deviation) or number (percentage) Group A: nerve block group; group B: control group
Analysis of recovery characteristics outcomes demonstrated a significantly longer mean time to first analgesia in group A than group B (543.27 vs. 199.84 min, P = 0.017). No differences between the groups in the grade of PONV and time to PACU discharge were noted. The mean time to achieve discharge eligibility (Aldrete score ≥9) from PACU was similar in both the groups (25.73 vs. 32.44 min, P = 0.202) [Table 2].
DISCUSSION
The beneficial effect of bilateral nasociliary and maxillary nerve block, when combined with general anaesthesia for nasal surgery, is demonstrated in the present study.
Nasal surgical procedures are associated with a high incidence of emergence agitation, leading to severe complications such as bleeding and increased hospital stay, thereby delaying recovery.[11] Although the cause of emergence agitation is not well established, pain in the immediate post-operative period is one of the significant risk factors for emergence agitation. Multiple analgesic interventions are applied to the patient before, during and after surgery for the above reasons. Among these interventions, the most utilised are combinations of narcotic and non-steroidal anti-inflammatory drugs. However, they are associated with gastrointestinal and neurological side effects, which cause discomfort to the patient and affect their recovery profile.[12,13] Therefore, the utility of combining regional nerve block with general anaesthesia has been popularised in clinical practice to provide improved perioperative analgesia, decreased narcotic consumption and enhanced emergence and recovery characteristics.[14,15,16]
Many studies have advocated the pre-emptive analgesic effect of different nerve blocks in nasal surgical procedures.[10,16,17,18] In one such study, bilateral infra-orbital and infra-trochlear nerve blocks with 0.25% levobupivacaine showed a significant reduction in the post-operative morphine requirement (2.5 ± 2.8 mg vs. 9.5 ± 3.5 mg, P < 0.001).[10] In a similar study conducted on 45 patients undergoing nasal surgery, the effect of infraorbital nerve block with 0.25% levobupivacaine showed a decrease in the total meperidine requirement in the PACU (17 ± 16 mg vs. 32 ± 13 mg, P = 0.01) when compared with a control.[17] The pre-emptive analgesic effect of sphenopalatine ganglion block with different local anaesthetics has been studied in patients undergoing functional endoscopic sinus surgery, which also demonstrated similar findings.[19,20] The use of nasociliary and infraorbital nerve blocks as the sole anaesthetic technique in outpatient nasal surgeries has shown encouraging results by providing good intraoperative conditions in 20 out of 24 patients.[6] However, the study reported a failure rate of 13% (4 out of 24 cases). These failures were only considered a partial loss as the surgery could proceed only with a single local anaesthetic infiltration. The possible explanation for the failure was attributed to the sparing of pterygopalatine nerves. For the above reasons, the maxillary nerve block was performed in the current study instead of the infraorbital nerve to prevent the incidence of block failure. Also, the usefulness of bilateral nasociliary and maxillary nerve block was apparent from successful anaesthetic management of bilateral nasal polypectomy in a patient with Kartagener's syndrome.[7] The efficacy of local anaesthetic infiltration technique combined with general anaesthesia during nasal surgery has also shown decreased post-operative pain and opioid consumption.[21,22] However, regional nerve blocks have an advantage over infiltration techniques due to various reasons, including reduced tissue distortion at the operative site and better pain control during handling of deeper tissues.[6]
The incidence of emergence agitation in adults is estimated to be more than 20% following general anaesthesia and 55.4% among patients undergoing ear, nose and throat surgery.[4,11] Several studies have demonstrated the use of pharmacological interventions like dexmedetomidine and propofol to reduce the incidence of emergence agitation in adults. However, they were associated with residual side effects such as sedation and haemodynamic changes, which prolonged the recovery period and hospital stay.[23,24] Recently, pain management through regional or peripheral nerve blocks is increasingly recommended to prevent emergence agitation. In the present study, the inclusion of pre-emptive nerve blocks has reduced the incidence of emergence agitation from 92% to 11.5%. These results are further corroborated by the similar reduction of emergence agitation from 62.5% to 20% in a study where bilateral infratrochlear and infraorbital nerve combined with general anaesthesia was given in patients undergoing nasal surgical procedures.[18] The aetiology for emergence agitation is still unclear, and various risk factors such as age, gender, presence of nasal packing, type of general anaesthesia and post-operative pain can be attributed to the development of emergence agitation. This study highlights only on the importance of effective pain management in reducing the incidence of emergence agitation.
In the present study, bilateral nasociliary and maxillary nerve block, when combined with general anaesthesia, did not decrease the time to PACU discharge following nasal surgical procedures despite having a useful effect on post-operative pain and emergence characteristics. Although the group receiving nerve block had a significantly longer mean time to first analgesia (minutes) (543.27 ± 156.48 vs. 199.84 ± 206.02, P = 0.017) when compared with the control group, the mean time to PACU discharge and the incidence of PONV was comparable between the groups and did not show early recovery. Several studies on recovery characteristics have shown that in addition to medical and surgical causes, other logistic non-medical reasons contribute to delayed recovery.[25,26] These probable non-medical causes can be speculated to be a delay in the availability of transportation, waiting for the surgeons to fill prescriptions and transfer orders.
The current study has the following limitations. Firstly, the sensory testing was not done before surgery as the bilateral nerve blocks were performed under general anaesthesia. Besides, post-operative sensory assessment of block was also hampered by the presence of surgical bruising and dressing. Both the blocks were performed by the extra-oral approach because of their ease of performance. Second, the haemodynamic measurements to corroborate haemodynamic stability were not made in this study.
CONCLUSION
Pre-emptive bilateral nasociliary and maxillary nerve blocks are effective pain management strategies because of their beneficial effects in reducing perioperative pain, opioid requirements and emergence agitation in patients undergoing nasal surgery under general anaesthesia.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Gerbershagen HJ, Aduckathil S, van Wijck AJM, Peelen LM, Kalkman CJ, Meissner W. Pain intensity on the first day after surgery: A prospective cohort study comparing 179 surgical procedures. Anesthesiology. 2013;118:934–44. doi: 10.1097/ALN.0b013e31828866b3. [DOI] [PubMed] [Google Scholar]
- 2.Wittekindt D, Wittekindt C, Schneider G, Meissner W, Guntinas-Lichius O. Postoperative pain assessment after septorhinoplasty. Eur Arch Otorhinolaryngol. 2012;269:1613–21. doi: 10.1007/s00405-011-1854-x. [DOI] [PubMed] [Google Scholar]
- 3.Lepousé C, Lautner CA, Liu L, Gomis P, Leon A. Emergence delirium in adults in the post-anaesthesia care unit. Br J Anaesth. 2006;96:747–53. doi: 10.1093/bja/ael094. [DOI] [PubMed] [Google Scholar]
- 4.Yu D, Chai W, Sun X, Yao L. Emergence agitation in adults: Risk factors in 2,000 patients. Can J Anaesth. 2010;57:843–8. doi: 10.1007/s12630-010-9338-9. [DOI] [PubMed] [Google Scholar]
- 5.Kissin I. Preemptive analgesia. Anesthesiology. 2000;93:1138–43. doi: 10.1097/00000542-200010000-00040. [DOI] [PubMed] [Google Scholar]
- 6.Molliex S, Navez M, Baylot D, Prades JM, Elkhoury Z, Auboyer C. Regional anaesthesia for outpatient nasal surgery. Br J Anaesth. 1996;76:151–3. doi: 10.1093/bja/76.1.151. [DOI] [PubMed] [Google Scholar]
- 7.Parthasarathy S. Anaesthetic management of bilateral nasal polypectomy in a patient with Kartagener syndrome. Sri Lankan J Anaesthesiol. 2012;20:56. [Google Scholar]
- 8.Terrence M Murphy. Somatic blockade of head and neck. In: Michael CJ, Bridenbargh PO, editors. Neural Blockade in Clinical Anaesthesia and Management of Pain. 3rd ed. Philadelphia: Lippincott Ravel; 1998. pp. 501–2. [Google Scholar]
- 9.Riker RR, Picard JT, Fraser GL. Prospective evaluation of the Sedation-Agitation Scale for adult critically ill patients. Crit Care Med. 1999;27:1325–9. doi: 10.1097/00003246-199907000-00022. [DOI] [PubMed] [Google Scholar]
- 10.Boselli E, Bouvet L, Augris-Mathieu C, Bégou G, Diot-Junique N, Rahali N, et al. Infraorbital and infratrochlear nerve blocks combined with general anaesthesia for outpatient rhinoseptoplasty: A prospective randomised, double-blind, placebo-controlled study. Anaesth Crit Care Pain Med. 2016;35:31–6. doi: 10.1016/j.accpm.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 11.Kim H-J, Kim D-K, Kim H-Y, Kim J-K, Choi S-W. Risk factors of emergence agitation in adults undergoing general anesthesia for nasal surgery. Clin Exp Otorhinolaryngol. 2015;8:46–51. doi: 10.3342/ceo.2015.8.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gray ML, Fan CJ, Kappauf C, Kidwai S, Colley P, Iloreta AM, et al. Postoperative pain management after sinus surgery: A survey of the American Rhinologic Society. Int Forum Allergy Rhinol. 2018;8:1199–203. doi: 10.1002/alr.22181. [DOI] [PubMed] [Google Scholar]
- 13.Çelik EC, Kara D, Koc E, Yayik AM. The comparison of single-dose preemptive intravenous ibuprofen and paracetamol on postoperative pain scores and opioid consumption after open septorhinoplasty: A randomized controlled study. Eur Arch Oto-Rhino-Laryngol. 2018;275:2259–63. doi: 10.1007/s00405-018-5065-6. [DOI] [PubMed] [Google Scholar]
- 14.Mehrotra S. Postoperative anaesthetic concerns in children: Postoperative pain, emergence delirium and postoperative nausea and vomiting. Indian J Anaesth. 2019;63:763–70. doi: 10.4103/ija.IJA_391_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mariano ER, Watson D, Loland VJ, Chu LF, Cheng GS, Mehta SH, et al. Bilateral infraorbital nerve blocks decrease postoperative pain but do not reduce time to discharge following outpatient nasal surgery. Can J Anaesth. 2009;56:584–9. doi: 10.1007/s12630-009-9119-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ibrahim M, Elnabtity AM, Keera A. Efficacy of external nasal nerve block following nasal surgery: A randomized, controlled trial. Anaesthesist. 2018;67:188–97. doi: 10.1007/s00101-018-0410-0. [DOI] [PubMed] [Google Scholar]
- 17.Cekic B, Geze S, Erturk E, Akdogan A, Eroglu A. A comparison of levobupivacaine and levobupivacaine-tramadol combination in bilateral infraorbital nerve block for postoperative analgesia after nasal surgery. Ann Plast Surg. 2013;70:131–4. doi: 10.1097/SAP.0b013e318236baa8. [DOI] [PubMed] [Google Scholar]
- 18.Choi H, Jung SH, Hong JM, Joo YH, Kim Y, Hong SH. Effects of bilateral infraorbital and infratrochlear nerve block on emergence agitation after septorhinoplasty: A randomized controlled trial. J Clin Med. 2019;8:769. doi: 10.3390/jcm8060769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rezaeian A, Hashemi SM, Dokhanchi ZS. Effect of sphenopalatine ganglion block with bupivacaine on postoperative pain in patients undergoing endoscopic sinus surgery. Allergy Rhinol Provid RI. 2019;10:2152656718821282. doi: 10.1177/2152656718821282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Degirmenci N, Ozdem A, Uysal H, Sen P, Senturk E, Ozturan O, et al. The effect of sphenopalatine ganglion block on the postoperative pain in patients undergoing septorhinoplasty. Ann Otol Rhinol Laryngol. 2020;129:722–6. doi: 10.1177/0003489420909417. [DOI] [PubMed] [Google Scholar]
- 21.Bagatin T, Bagatin D, Šakić L, Šakić K. Impact of local infiltration anesthesia on postoperative pain management after rhinoplasty in day care surgery. Acta Clin Croat. 2019;58(Suppl 1):62–6. doi: 10.20471/acc.2019.58.s1.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tsai S-C, Lai M-T, Kao Y-L, Wu C-C. Effect of infiltrating nasal packing with local anesthetics in postoperative pain and anxiety following sinonasal surgeries: A systemic review and meta-analysis. Braz J Otorhinolaryngol. 2020;86:376–82. doi: 10.1016/j.bjorl.2019.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fang X-Z, Gao J, Ge Y-L, Zhou L-J, Zhang Y. Network meta-analysis on the efficacy of dexmedetomidine, midazolam, ketamine, propofol, and fentanyl for the prevention of sevoflurane-related emergence agitation in children. Am J Ther. 2016;23:e1032–42. doi: 10.1097/MJT.0000000000000321. [DOI] [PubMed] [Google Scholar]
- 24.Garg A, Kamal M, Mohammed S, Singariya G, Chouhan DS, Biyani G. Efficacy of dexmedetomidine for prevention of emergence agitation in patients posted for nasal surgery under desflurane anaesthesia: A prospective double-blinded randomised controlled trial. Indian J Anaesth. 2018;62:524–30. doi: 10.4103/ija.IJA_788_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shirakami G, Teratani Y, Namba T, Hirakata H, Tazuke-Nishimura M, Fukuda K. Delayed discharge and acceptability of ambulatory surgery in adult outpatients receiving general anesthesia. J Anesth. 2005;19:93–101. doi: 10.1007/s00540-004-0297-6. [DOI] [PubMed] [Google Scholar]
- 26.Seago JA, Weitz S, Walczak S. Factors influencing stay in the postanesthesia care unit: A prospective analysis. J Clin Anesth. 1998;10:579–87. doi: 10.1016/s0952-8180(98)00084-1. [DOI] [PubMed] [Google Scholar]


