Sir,
The SARS-CoV-2 coronavirus outbreak has resulted in a severe acute respiratory distress syndrome (ARDS) with especially high morbidity and mortality, if not treated in time, results in subsequent interstitial lungs fibrosis.[1] Initial data revealed that manifestations in severe COVID-19 cases are a result of “cytokine storm” syndrome which includes ARDS, a macrophage activation syndrome with significantly raised inflammatory biomarkers including interleukin-6 (IL-6).[2] The Kallikrein system and raised bradykinin levels play key roles in COVID-19 clinical pathogenesis. Methylene blue (MB), a nitric oxide synthase inhibitor is known to neutralize effects of bradykinin.[3] Herein, we report seven cases of severe COVID-19 infection with ARDS who did not respond to antiviral (remedesivir, favipiravir), anti-inflammatory agents such as IL-6 antagonist (tocilizumab), steroids, heparin, and oxygen inhalation but subsequently responded to MB inhalation.
We studied seven (M5, F2) patients between the age group of 28 and 82 (mean - 56) years suffering from severe COVID-19 disease with ARDS, respiratory failure with bilateral extensive infiltration of lungs. Of these, four patients suffered from hypertension, diabetes, and ischemic heart disease. All the seven patients gave the history of febrile illness, myalgia, non-productive cough, weakness, recurrent headache, and loose motion for nearly 5 days preceding breathlessness. There was a loss of taste and smell sensation in four cases and only a loss of smell in two cases. All were admitted to a tertiary care hospital where appropriate investigations revealed them to be suffering from lymphopenia in 8--18% (normal 20--40%), eosinopenia, raised C-reactive protein 42--11.84 (mean 76.82) (n-<6) mg/dl.
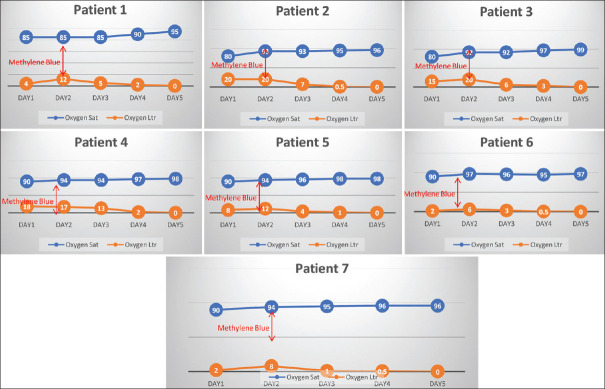
All of them were administered remedesivir, tocilizumab, steroids, vitamin D, vitamin-C, zinc, meropenem 1 gram 12 hourly, doxycycline 100 mg twice a day, aspirin 150 mg, low molecular weight heparin 60 mg twice a day, and non-invasive ventilation (NIV) in a prone position. Irrespective of administering oxygen varying between 2 and 20 (mean 11.57) litres per minute, the oxygen saturation continued to remain between 80 and 94 (mean 88%). All these cases were given MB in a 1:4 dilution by nebulisation every six hourly. There was a significant improvement in oxygen saturation with a reduction in oxygen requirement and a remarkable improvement in the lung lesions [Figures 1 and 2].
Figure 1.
Showing details of effects of methylene blue on oxygen saturation and oxygen nrequirement
Figure 2.
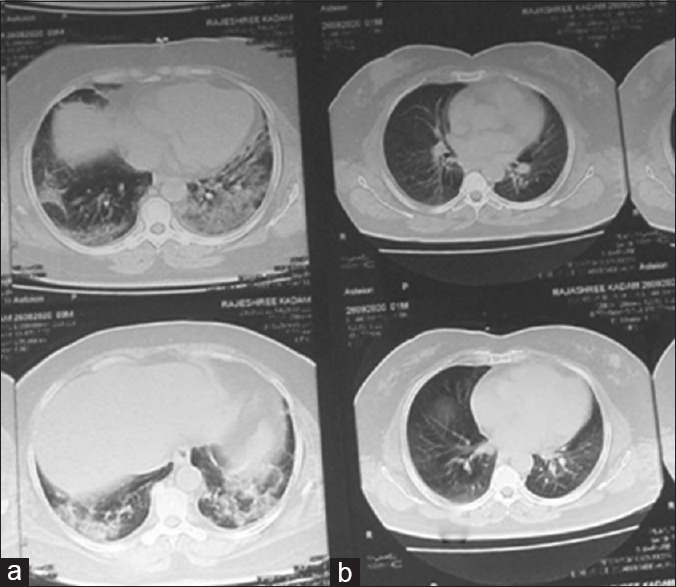
HRCT of 32 years cases of severe ARDS (a) and extensive fibrosis prevented (b) due to methylene blue bebulization
Up till now, it was believed that “cytokine storm” plays an important role in the pathogenesis of COVID-19. However, this was a hypothesis and till now it has not been proven that cytokine or autacoids act as igniters or are the main culprit for the storm. More recently, the role of kininogen system in SARS-CoV-2 has been studied in detail which reveals that there is derangement of ACE-2 receptors which subsequently leads to uninhibition of the kininogen- kallikrein system and as result of this there is an increase in bradykinin activity which is a key factor contributing towards COVID-19 clinical effects such as dry cough and coagulopathy. There are ameliorating effects of zinc supplements, and angiotensin receptor blockers have less detrimental effects with respect to ACE inhibitors and are in part even preventive against loss of taste, smell, and diarrhoea.[4,5]
Bradykinin plays important role in the pathogenesis of COVID-19 disease. Methylene blue a phenothiazine derivities inhibits the brdaykinin synthetase enzyme result in inhibition of synthesis of nitric oxide; in pulmonary capillaries and subsequently improves the acute respiratory distress syndrome and oxygenation. Previously known as endothelial-derived relaxation factors (EDRF). The soluble intracellular enzyme guanylate cyclase was activated to produce cyclic guanosine monophosphate (cGMP) which is under influence of several mediators including NO. MB acts by inhibiting cGMP and vascular smooth muscle relaxation. MB acts by converting red blood cell content of hemoglobin to leuko-methylene blue. MB is a reducing agent of oxidized hemoglobin converting the ferric ion back to its oxygen-carrying ferrous state. Non-steroid anti-inflammatory drug (NSAID) may block alternative pathways of bradykinin activity. These alternative pathways may be over-activated and continue the disease process. Recently, it has been observed that the addition of NSAID may benefit the role played by MB. MB improves the oxygen-carrying capacity and the alveolar-capillary perfusion and hypoxia.[6]
MB is a scientific bradykinin antagonist which is easily available, cheap, non-toxic and is easy to administer in rural settings. It is contraindicated in patients consuming antidepressant drugs such as SSRI, in cases of G-6-PD deficiency and in pregnancy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We are grateful to Pranav Ajmera, a senior resident in the Department of Radiology, Dr DY Patil Medical College, Pune for editing the manuscript. Dr R.S. Mohite treated cases under guidance of author HSB.
Post script - During second phase of COVID-19 disease more than 200 cases mild to severe COVID-19 were treated with methylene blue nebulization at hospital and then continued at home result in nil fatality and serendipitously enough victims followed in outpatient department no patient suffered of post COVID fibrosis and COPD
References
- 1.Wong AW, Fidler L, Marcoux V, Johannson KA, Assayag D, Fisher JH, et al. Practical considerations for the diagnosis and treatment of fibrotic interstitial lung disease during the coronavirus disease 2019 Pandemic. Chest. 2020;158:1069–78. doi: 10.1016/j.chest.2020.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult in patients with COVID-19 in wuhan, china:A retrospective cohort study. Lancet. 2020;395:1054–62. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ghahestani SM, Shahab ES, Karimi S, Madani MH. Methylene blue may have a role in the treatment of COVID—19. Med Hypotheses. 2020;144:110163. doi: 10.1016/j.mehy.2020.110163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Toluunian R, Vahed SZ, Ghiyasvand S, Tolouian A. Covid-19 interactions with angiotensin-coverting enzyme 2 (ACE2) and the kinin system;looking at a potential treatment. J Renal Inj Prev. 2020;9:e19–e21. [Google Scholar]
- 5.Van de Veerdonk FL, Netea MG, van Deuren M, van der Meer JW, de Mast Q, Brüggemann RJ, et al. Kallikrein-kinin blockade in patients with COVID-19 to prevent acute respiratory distress syndrome. Elife. 2020;9:e57555. doi: 10.7554/eLife.57555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ginimuge PR, Jyothi SD. Methylene blue:Revisited. J Anaesthesiol Clin Pharmacol. 2010;26:517–20. [PMC free article] [PubMed] [Google Scholar]