Abstract
Background:
COVID-19 pandemic led to increased self-medication of antimicrobials, vitamins, and immune boosters among the common people and consuming without prescription can lead to adverse consequences including antimicrobial resistance.
Methods:
A cross-sectional study was conducted on community pharmacies in Jodhpur, India. They were inquired regarding the prescription and increased sales (<25%, 25—50%, 50--75%, or 75--100%) of various medicines (Hydroxychloroquine, Azithromycin, Ivermectin, and Vitamin C) during the COVID-19 pandemic. Logistic regression analysis was conducted to assess the relationship between requests for certain COVID-19 medications and an increase in their sale.
Results:
A total of 204 pharmacies took part, and 88.23% reported patients to approach them without prescriptions. Most of the pharmacies revealed that <25% of patients came without prescription. The majority came for azithromycin (68%) and vitamin C (92%). Increased sales of the four targeted medications were seen by 85.92% of pharmacies compared to last year. A majority (51.5%) reported <25% increased sales of azithromycin, but no change in the sale of hydroxychloroquine and ivermectin. However, 39.6% reported >75% increase in vitamin C sales.
Conclusion:
There was an increase in the demand for COVID-19 medications without prescription. This study was unable to detect a significant increase in sales of antimicrobials, which is encouraging.
Keywords: Antimicrobial, azithromycin, community pharmacy, COVID-19, hydroxychloroquine, India, vitamin C
Introduction
The Coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2), has emerged as a global pandemic and has been cited as public health emergency of national and international concern.[1,2] SARS-CoV-2 is from the family coronaviridae, and the present pandemic is the third incidence of its emergence in the last two decades, the first being severe acute respiratory syndrome (SARS) in 2003, followed by Middle East respiratory syndrome (MERS CoV) in 2012.[3,4] Globally, COVID-19 has been an appreciable concern as this disease has an increased transmission rate, leading to an appreciable increase in infection rates, morbidity, and mortality among the population, including health care workers.[5,6] Initially, COVID-19 appeared as pneumonia of unidentified etiology in Wuhan (China) and presented with greater severity among the older population, especially in patients with comorbidities.[7]
The clinical presentation of patients admitted to hospitals was diverse and mostly resembled bacterial pneumonia with symptoms including fever and coughing with lung infiltrates which were caused due to inflammation and cytokine storm.[8,9] The seriousness of the disease and the additional possibility of bacterial superinfection led to an enhanced prescribing of antimicrobials despite limited data of co-infections.[10,11] In view of no approved therapy, various antivirals, antimicrobials, antiprotozoals, multivitamins, minerals, nutraceuticals, and complementary and alternative medicine therapies were tried to find a relative cure or answer to this condition.[12,13,14,15,16,17] This led to the unconstrained prescribing of antimicrobials and enhanced the risk of antimicrobial resistance (AMR).[18] Reduced visits to hospitals due to lockdown and other measures, coupled with early published studies showing the benefits of medicines such as hydroxychloroquine with antibiotics, and difficulties with diagnosing COVID-19 from other acute respiratory infections have resulted in increased purchasing of antimicrobials without a prescription, causing concern because of potentially increasing AMR.[14,19,20] The pandemic not only badly affected the healthcare system but also impaired professional and medical education which has further increased the challenges.[21,22]
There is a grave concern because of rising AMR rates worldwide with an associated impact on morbidity, mortality, and costs across countries.[23,24] There has been reports of an increased incidence of infections by multidrug-resistant bacteria reported from the countries with a high COVID-19 infection rates has added up to these concerns.[11,25,26] Despite many recommendations to constrict the liberal use of broad-spectrum antimicrobials in these situations, the processing of the microbiological samples in overburdened emergency labs, the lack of evidence-based treatment protocols, and the lack of antimicrobial stewardship groups, might have left the practitioners in some countries with little option other than prescribing broad-spectrum antimicrobials in the face of patient pressure.[27,28]
The liberal use of unprescribed antimicrobials has become a significant public health concern in recent years, accounting for an appreciable proportion of overall antibiotic use in ambulatory care.[29] Overall, 32.5--81.5% of the population worldwide have been estimated to be taking antibiotics purchased from the local pharmacist, enhancing AMR and compromising life expectancy.[29,30,31] The highest prevalence of self-purchasing of antibiotics is seen among developing countries where healthcare directives are less enforced, community pharmacies are opened for longer hours and patients do not have to pay physician fees.[29,32,33,34] Overall, pain killers, antipyretics, cough medications, antidiarrheals, calcium and vitamin supplements, anabolic steroids, sleep medications, antimicrobials, and several herbal and homeopathic remedies were frequently self-prescribed medications depending on the country and circumstances.[35,36,37,38,39] Uncomplicated urinary tract infections and watery diarrhea were the commonest conditions where antimicrobials were used in Eritrea, making ciprofloxacin (47.8%) and co-trimoxazole (37.5%) among the most commonly used antimicrobials, followed by amoxicillin, doxycycline, tinidazole, and metronidazole in the country.[40] This high prevalence of consumption of antimicrobial by the public is an important issue and community pharmacies can play a crucial role in minimizing the problem by curtailing the sale of antimicrobials only with valid prescriptions.
The advent of COVID 19 and having no clarity of the etiology or potential effective treatments led to an increased practice of self-medication with antimicrobials upon advice from various sources exacerbated by early reports of the effectiveness of hydroxychloroquine with or without antibiotics.[41,42,43,44] In India, hydroxychloroquine and chloroquine were also used as self-medication.[41,42,43,44,45] Self-medication with antimicrobials including azithromycin (54.15%) and doxycycline (40.25%) were greater during the recent pandemic as compared to the pre-pandemic time where this was 21% and 25%, respectively, for azithromycin and doxycycline.[46,47] To date, among so many medications being used, dexamethasone has shown some promise in reducing morbidity and mortality in patients hospitalized with COVID-19.[48,49] The increased use of various medications without proven benefit can lead to raised risk of adverse drug reactions (ADRs) hence monitoring these and reporting them is crucial for rational drug use.[50,51] The vaccines have proven to improve immunity against the strains of COVID-19 and seem to be the only option at the current time to end this pandemic, however the safety of these newly developed vaccines needs to be monitored as done by various studies.[51,52,53,54]
Increase in the inappropriate use of antimicrobials has the potential to increase AMR along with its impact on morbidity, mortality, and costs. India is such a country where the majority of the population still approach community pharmacies for the treatment of minor ailments rather than visiting a physician and the burden of self-medication observed in several studies has ranged from high rates of 92.8% in urban Delhi and 81.5% in rural Maharashtra to lower rates of 23% in Tamil Nadu, 18.72% in Odisha, and 11.9% in Urban Puducherry.[55,56,57,58,59,60] Alongside this, a large online survey estimated that approximately 52% of Indians self-medicated themselves and one of the reasons was to avoid physician fees.[57,61] Due to financial constraints, patients often resort to self-medication as healthcare costs can exert a huge burden on them and their families.[62] Evidence shows that health insurance only covers about 15% of the population and hence out-of-pocket expenditure on treatment and healthcare is one of the leading expenditures among families and inflicts a tremendous burden on the financial status of the Indian population.[63,64,65,66]
Therefore, the current demand for various medications without a prescription for the treatment of COVID-19 needs to be assessed and also the increase in their costs in countries where self-medication is common due to high patient co-payments and issues of affordability. The assessment of the use and demand of these medications and perception of self-medication in the public can be a very crucial finding for the primary care physicians as this would give an idea regarding the burden of the problem, hence helping them to intervene and tackle the issue at a very early point by taking necessary steps.[67] The various activities by the Indian Government and other key stakeholder groups to try and prevent the spread of the virus during the early months have already been extensively described, and we would like to build on this.[68]
Materials and Methods
This was a cross-sectional study conducted among community pharmacies in Jodhpur, Rajasthan, which is situated in western India and is one of the largest districts of Rajasthan including a large population from the urban and rural areas. The study was conducted between November and December 2020, and the pharmacists were chosen by a convenient sampling method. All pharmacists were made aware of the study objectives and procedure and participation were entirely voluntary, with pharmacists only included in the study after obtaining free voluntary verbal consent.
The pharmacists were questioned about their sociodemographic details and various questions about the prescriptions and sales of multiple medicines and antimicrobials for COVID-19. The questions to be asked were designed on the basis of utilization of various medications for the treatment of COVID-19 similar to previous studies conducted across Africa and Asia.[25,44,68,69,70] The pharmacists were asked regarding four medications, namely azithromycin, hydroxychloroquine (HCQ), ivermectin, and Vitamin C, which were being repurposed in the treatment of COVID-19. The range of replies in the questionnaire (<25%, 25--50%, 50--75%, or 75--100%) were chosen based on the pilot study conducted and for easy classification of the data reported.
The following five questions were asked to build on our initial study among pharmacists across India:
In the last two months, did patients come to get medicines without prescriptions?
What proportion (<25%, 25--50%, 50--75%, or 75--100%) of total patients came for medicines without prescriptions?
For which of these medications (Azithromycin, Hydroxychloroquine, Ivermectin, and Vitamin C) did they come for without prescription?
Was there an increase in the sale of the above medicines in 2020 compared to the previous year (2019)? [Yes/No]
If yes, what percentage (<25%, 25--50%, 50--75%, or 75--100%) of sale of the above medicines (azithromycin, hydroxychloroquine, ivermectin, and vitamin C) was increased?
Ethical approval
The study was approved by the Institutional ethics committee, AIIMS, Jodhpur, with certificate reference number AIIMS/IEC/2020/3241.
Statistical analysis
The data were collected and entered Microsoft Excel v. 365. Descriptive analysis was used, and data were presented as frequencies and percentages. To explore the predictors of an increase in the sale of COVID-19 medicines requested by patients without a prescription in 2020 compared to 2019, logistic regression models were introduced. The explanatory variables were patient requests (yes or no) of certain medicines without a prescription in the last two months, including azithromycin, HCQ, ivermectin, and vitamin C. The response variable was an increase in the sale of these medicines. A multiple logistic regression model was utilized to identify the independent effects of explanatory variables. The level of significance was established as P ≤ 0.05, and 95% confidence intervals (CI) were used as OR estimates.
Results
The study was conducted among 212 pharmacies of which 204 pharmacies agreed to participate in the study (response rate = 96.22%). A total of 180 (88.23%) pharmacies revealed that in general, patients did come to get medicines without valid prescriptions, and 24 pharmacies (11.7%) reported no patients came without prescriptions to obtain their medicines. When asked about exactly what proportion of patients came without prescriptions, of the 180 pharmacies, 105 (58.33%) pharmacies reported that <25% of patients came without a prescription, 59 (32.77%) pharmacies reported 25--50% of patients, 14 (7.77%) pharmacies reported 50--75% of patients, and two pharmacies (1.1%) reported >75% of the patients.
Out of the 204 pharmacies, 188 pharmacies responded to the question regarding “for which drug did they came to get without prescription?”. Among the 188 pharmacies who responded, 68% of the pharmacies reported that patients came for purchasing azithromycin without a prescription. Additionally, 91.4% of the pharmacies reported that patients came for the over-the-counter medication Vitamin C and 17.5% each for HCQ and ivermectin [Figure 1].
Figure 1.
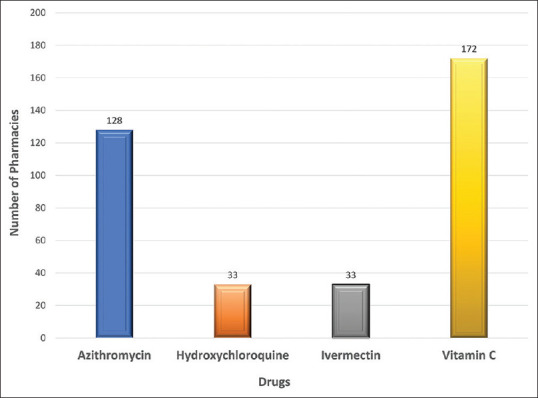
Prevalence of self-medication of various medications used in COVID-19 reported by community pharmacists
A total of 199 pharmacies responded to the query regarding the increase in sales during the pandemic with 171 (85.92%) reporting an increase compared to last year (2020 vs. 2019). Of the 204 pharmacies, 202 answered regarding the percentage increase in the sale of the four designated medications since two pharmacies were new and opened in 2020. The majority of the pharmacies (51.5%) reported that there was a < 25% increase in the sale of azithromycin. In comparison, most of the pharmacies reported that there was no change in the sale of HCQ (54%) or ivermectin (51.5%). 39.6% of pharmacies responding reported a >75% increase in vitamin C sales compared to the previous year [Table 1].
Table 1.
Increase in sale of various drugs during COVID-19
| Drugs | What percentage of sales was increased as compared to the previous year? (n=202) | ||||
|---|---|---|---|---|---|
|
| |||||
| No increase | <25% increase | 25-50% increase | 50-75% increase | 75-100% increase | |
| Azithromycin | 31 | 104 | 44 | 18 | 5 |
| Hydroxychloroquine | 109 | 81 | 12 | 0 | 0 |
| Ivermectin | 104 | 55 | 22 | 10 | 11 |
| Vitamin C | 16 | 13 | 39 | 54 | 80 |
In a multiple logistic regression model (Chi2 = 25.14, P < 0.001), an increase in sale of COVID-19 medicines was significantly associated with patient requests for azithromycin [OR = 3.40 (1.13, 10.21), P = 0.029] and vitamin C [OR = 8.59 (2.54, 29.05), P = 0.001] in the last two months [Table 2]. This model could explain 22.0% of the variability.
Table 2.
Predictors of an increase in sale of COVID-19 drugs based on multivariate logistic regression analysis
| Patient requests of the following medicines | Crude | Adjusted | ||
|---|---|---|---|---|
|
|
|
|||
| OR (95% CI) | P | OR (95% CI) | P | |
| Azithromycin | 2.48 (1.10, 5.61) | 0.029 | 3.40 (1.13, 10.21) | 0.029 |
| HCQ | 0.46 (0.18, 1.17) | 0.102 | 0.25 (0.07, 0.87) | 0.029 |
| Ivermectin | 0.46 (0.18, 1.17) | 0.102 | 0.37 (0.12, 1.13) | 0.080 |
| Vitamin C | 7.60 (2.57, 22.50) | <0.001 | 8.59 (2.54, 29.05) | 0.001 |
Discussion
Overall, few studies have been conducted during the COVID-19 pandemic regarding the self-purchasing of medications without any prescription, particularly antimicrobials. The current study surveyed 212 pharmacies with a response rate of 96.2%, with most pharmacies reporting that patients, in general, do approach them without valid prescriptions. However, encouragingly the major proportion of patients without a valid prescription was less than 25% of the total patients approached. Among the four drugs enquired, the majority of patients approached the pharmacists for azithromycin and vitamin C. Overall though, increasing sales of azithromycin, HCQ, ivermectin, vitamin C were observed in 2020 as compared to the previous year, with the maximum increase seen with vitamin C.
Overall, 88% of pharmacists reported that in general, patients do come to them without valid prescriptions, but the proportion was low, and among them who approached without prescription, most of these were for azithromycin (68%) and vitamin C (91.4%). Self-medication has been an issue long before the current pandemic of COVID-19 and has been a crucial reason for the irrational use of drugs and associated complications. The prevalence of self-medication as reported by several studies ranges from 32.5 to 81.5% in various parts of the world.[31,59,71] Jorgji et al.,[72] in their research, reported that about 78.14% of the participants self-medicated themselves without prescriptions and the most common antimicrobial was amoxicillin (19.39%), followed by amoxicillin-clavulanic acid (15.24%).
This compares with Onchonga et al.[73] (2020), in their study on assessing the trend of several online searches regarding information of self-medication for health problems during the COVID-19 pandemic, reported a surge in the online searches. In another study, Onchonga et al.[74] (2020) found that the overall prevalence of self-medication increased to 60.4% as compared to 36.2% before the COVID-19 pandemic, with Sadio et al.[75] (2021) reporting that the gross prevalence of self-medication to prevent COVID-19 was 34.2%. This was greatest for vitamin C (27.6%) versus 1.2% for azithromycin and 2% for chloroquine/hydroxychloroquine.[75] These rates are considerably lower than those reported by Choudhary et al.[76] (2021) in their study who reported that 48% of patients during lockdown resorted to self-medication compared with 15% before lockdown. Antibiotics (16.67%) including amoxicillin-clavulanic acid and norfloxacin-tinidazole were among the most common medicines taken without prescription.[76] Chopra et al.[77] (2021) also reported that 24.2% of the participants had taken medication without a prescription, with 6% taking antimicrobials without a prescription and 1% specifically HCQ.
Most of the pharmacies in this study reported no increase (54%) in the sale of HCQ, with 40.1% reporting an increase but this was less than a 25% increase in sales. In addition, only 17.6% of patients approached the pharmacies without a valid prescription which was encouraging. This compares to an earlier study by Haque et al.[68] (2021) who found there was a 55% increase in demand for antimalarials among community pharmacies in India in the early stages of the pandemic. Chauhan et al.[45] also reported increased use of HCQ and chloroquine without a valid prescription for COVID-19. This compares with Chakraborty et al.[78] (2020) who reported that only 10.8% of the patients self-medicated with HCQ and Chopra et al.[77] (2021) who reported a low prevalence (1%) of the patients self-medicating with HCQ during this COVID-19 pandemic. This also compares with no change or decreased demand for antimalarials in Bangladesh (51.2%), Malaysia (83.3%), and Vietnam. In contrast, in Pakistan (88.9%), there was appreciably increased demand for HCQ.[69] A study conducted by Chauhan et al.[45] in India reported that there was an increased use of hydroxychloroquine and chloroquine without a valid prescription for COVID-19. We are not sure of the rationale behind the differences in findings between the various studies in India.[79,80,81] However, this may well reflect increasing concerns with HCQ in the COVID-19 patient management.
Encouragingly as well, an appreciable number of pharmacies reported no increase or less than a 25% increase in the sale of azithromycin (71.2%) and ivermectin (78.7%). This compares with Haque et al.[68] (2021) who reported a 42.3% increase in demand for antibiotics including azithromycin in India during the initial phase of the COVID-19 pandemic. Nasir et al.[47] (2020) in their study conducted in Bangladesh, reported that 54.15% of the participants self-medicated with azithromycin and 77.15% with ivermectin. Malik et al.[19] (2020) also reported that ivermectin is being sold over the counter in a few countries and patients were self-medicating with it for the treatment of COVID-19, which was a concern. Godman et al.[69] (2021) in their study reported that there was increased demand and use of antibiotics in Bangladesh (70.6%), India (42.3%), and Pakistan (100%) in the early phase of the pandemic contrasting with a minimal or no increase in demand in Malaysia and Vietnam.
Armitage et al.[82] in their study reported a significant increase in the number of antibiotic prescriptions during the current pandemic that was 6.71% higher than expected compared to the decrease in an absolute number of appointments. A study by Langford et al.[83] reported that about 71.8% of the COVID-19 patients consumed antimicrobial even when it was not clinically needed. Morgan et al.[84] systematically reviewed the non-prescription use of antimicrobial across the world and reported about 19–100% of antimicrobial use, which resulted in an associated rise in ADRs and masking of underlying infections. A study by Abelenda-Alonso et al.[27] reported a biphasic pattern of antimicrobial use. Amoxicillin/clavulanate use was increased during the first peak of COVID-19 till March 2020 but later showed a decline in its use.
Most of the pharmacies (92.1%) in the current study reported increased demand for over-the-counter medicine vitamin C. Similarly, most of the pharmacies (39.6%) reported that the sale increased up to 75--100% with vitamin C. Haque et al.[68] in their study, reported similar findings where there was an increase of 90.1% in utilization among immune boosters (multivitamins and Vitamin C) and an increase of 54.1% in the price.
Overall, even though the number of pharmacies reporting self-medication was high in our study, the proportion of patients who approached pharmacists for antimicrobials including azithromycin and HCQ without a valid prescription were low. The reason for the comparative low dispensing of antimicrobials from the pharmacies could be restrictions with prescription-only drugs including antimicrobials.
As community pharmacies are the stakeholder responsible for delivering medications to the patients, and in this time of pandemic due to the huge number of cases, most of the patients approached them for getting the medications hence they can serve as a checkpoint in order to restrict the inappropriate use of antimicrobials and other prescription-only drugs. Primary care physicians play the most crucial part in the treatment of the majority of the patients in the community as they are the ones who prescribe the medicines to the patients hence the findings of the study might help them to introspect and assess the burden of the self-medication in the society and assist them in planning strategies to curb the problem.
Overall, a number of activities can be undertaken to further lower the purchasing of antimicrobials without a prescription in India. Even though the proportion of patients consuming antimicrobials without prescription was comparatively low yet but the issue of irrational use or overuse of these agents without definite need poses a great threat as it is one of the leading reasons for antimicrobial resistance.[29,85,86] To tackle such a situation some steps that could be taken to minimize inappropriate drug use are enlisted below.
Strategic plans for the future to ensure rational use of drugs
The primary care physicians, nursing officers, and pharmacists should be updated with current knowledge and practices.
Healthcare workers and pharmacists should be regularly trained regarding the rational use of antimicrobials and the importance of antimicrobial stewardship.
The government should lay guidelines for the management of patients which should be evidence-based. This would enhance the confidence of the healthcare workers in managing the patients in the right direction.[87,88]
The sale of prescription drugs should be done only on the production of valid prescriptions by the patient, and it should be strictly followed by the pharmacists. To monitor the sale regular audit and inspections should be conducted.
The public should be educated regularly regarding the irrational use of drugs and their consequences in social media, channels and also should also be incorporated in the educational training of the students right from their schools which would sensitize them right from their primary education days.
Train and insist the healthcare workers make the patients understand the right usage of the prescription drugs and disagree with the compulsive need for antimicrobials even if the patient demands.
Limitations
Also, the study was conducted in a single city in India hence the findings of the study cannot be entirely generalized.
Key points
Irrational use of drugs has been a vexing issue for a long time and the pandemic of COVID-19 has further seemed to enhance it
Drug use without prescription can prove deleterious to both the patient and the healthcare system
Community pharmacies are a crucial point that can play an important part in curbing the issue of self-medication among the public
The current study showed a majority of the pharmacies reported that <25% of patients came without prescription which is a positive finding and the majority of them came for azithromycin and vitamin C
Increased sales of the four targeted medications were seen by 85.92% of pharmacies compared to last year and a maximum increase was observed for vitamin C sales.
There was an increase in the demand for COVID-19 medications, but no significant increased sales of antimicrobials were observed during the study period. However, we recommend conducting larger and multicenter studies to observe conclusive results
Conclusion
In the absence of definite therapy, combating COVID-19 with various therapeutic agents and vaccines has been a critical issue to date. Drugs and antimicrobials repurposing were the only option, and therefore there was an increase in the sale of antimicrobial and immune boosters even when they weren’t clinically required. Many pharmacies saw most patients came without prescriptions, which seems to be a critical issue; however, antimicrobials like hydroxychloroquine, azithromycin, and ivermectin dispensing were lesser. Increased demand for vitamin C was seen, which could be due to its believed benefit in respiratory diseases and flu.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Chatterjee P, Nagi N, Agarwal A, Das B, Banerjee S, Sarkar S, et al. The 2019 novel coronavirus disease (COVID-19) pandemic:A review of the current evidence. Indian J Med Res. 2020;151:147–59. doi: 10.4103/ijmr.IJMR_519_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. COVID-19 Public Health Emergency of International Concern (PHEIC) Global research and innovation forum 2020. [Last accessed on 2021 May 15]. Available from: https://www.who.int/publications/m/item/covid-19-public-health-emergency-of-international-concern-(pheic)-global-research-and-innovation-forum .
- 3.Ramadan N, Shaib H. Middle East respiratory syndrome coronavirus (MERS-CoV):A review. Germs. 2019;9:35–42. doi: 10.18683/germs.2019.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhong NS, Zheng BJ, Li YM, Poon Xie ZH, Chan KH, et al. Epidemiology and cause of severe acute respiratory syndrome (SARS) in Guangdong, People's Republic of China, in February, 2003. Lancet. 2003;362:1353–8. doi: 10.1016/S0140-6736(03)14630-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bandyopadhyay S, Baticulon RE, Kadhum M, Alser M, Ojuka DK, Badereddin Y, et al. Infection and mortality of healthcare workers worldwide from COVID-19:A systematic review. BMJ Glob Health. 2020;5:e003097. doi: 10.1136/bmjgh-2020-003097. doi:10.1136/bmjgh-2020-003097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jan H, Faisal S, Khan A, Khan S, Usman H, Liaqat R, et al. COVID-19:Review of epidemiology and potential treatments against 2019 novel coronavirus. Discoveries (Craiova) 2020;8:e108. doi: 10.15190/d.2020.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Varghese GM, John R, Manesh A, Karthik R, Abraham OC. Clinical management of COVID-19. Indian J Med Res. 2020;151:401–10. doi: 10.4103/ijmr.IJMR_957_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rowaiye AB, Okpalefe OA, Adejoke OO, Ogidigo JO, Oladipo OH, Ogu AC, et al. Attenuating the effects of novel COVID-19 (SARS-CoV-2) infection-induced cytokine storm and the implications. J Inflamm Res. 2021;14:1487–510. doi: 10.2147/JIR.S301784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kumar T, Dutta S, Sahai R, Khasbage S, Kumar R, Banerjee S. Dermatological manifestations of COVID-19:A review based on existing reports. Int J Cur Res Rev. 2020;12:65–8. [Google Scholar]
- 10.Rawson TM, Moore LSP, Zhu N, Ranganathan N, Skolimowska K, Gilchrist M, et al. Bacterial and fungal coinfection in individuals with coronavirus:A rapid review to support COVID-19 antimicrobial prescribing. Clin Infect Dis. 2020;71:2459–68. doi: 10.1093/cid/ciaa530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rodríguez-Álvarez M, López-Vidal Y, Soto-Hernández JL, Miranda-Novales MG, Flores-Moreno K, Ponce de León-Rosales S. COVID-19:Clouds over the antimicrobial resistance landscape. Arch Med Res. 2021;52:123–6. doi: 10.1016/j.arcmed.2020.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Charan J, Bhardwaj P, Dutta S, Kaur R, Bist KS, Detha M, et al. Use of complementary and alternative medicine (CAM) and home remedies by COVID-19 patients:A telephonic survey. Indian J Clin Biochem. 2021;36:108–11. doi: 10.1007/s12291-020-00931-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Charan J, Dutta S, Kaur R, Bhardwaj P, Sharma P, Ambwani S, et al. Tocilizumab in COVID-19:A study of adverse drug events reported in the WHO database. Expert Opin Drug Saf. 2021;28:1–12. doi: 10.1080/14740338.2021.1946513. doi:10.1080/14740338.2021.1946513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dutta S, Kaur R, Bhardwaj P, Deora S, Singh K, Ambwani S, et al. Hydroxychloroquine as therapeutic option in COVID-19:Analysis of suspected cardiovascular adverse drug events reported in the VigiBase. Bangladesh J Med Sci. 2021;20:897–910. [Google Scholar]
- 15.Kaur RJ, Charan J, Dutta S, Sharma P, Bhardwaj P, Sharma P, et al. Favipiravir use in COVID-19:Analysis of suspected adverse drug events reported in the WHO database. Infect Drug Resist. 2020;13:4427–38. doi: 10.2147/IDR.S287934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Samad N, Dutta S, Sodunke TE, Fairuz A, Sapkota A, Miftah ZF, et al. Fat-soluble vitamins and the current global pandemic of COVID-19:Evidence-based efficacy from literature review. J Inflamm Res. 2021;14:2091–10. doi: 10.2147/JIR.S307333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Samad N, Sodunke TE, Abubakar AR, Jahan I, Sharma P, Islam S, et al. The implications of zinc therapy in combating the COVID-19 global pandemic. J Inflamm Res. 2021;14:527–50. doi: 10.2147/JIR.S295377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beović B, Doušak M, Ferreira-Coimbra J, Nadrah K, Rubulotta F, Belliato M, et al. Antibiotic use in patients with COVID-19:A 'snapshot'infectious diseases international research initiative (ID-IRI) survey. J Antimicrob Chemother. 2020;75:3386–90. doi: 10.1093/jac/dkaa326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Malik M, Tahir MJ, Jabbar R, Ahmed A, Hussain R. Self-medication during Covid-19 pandemic:Challenges and opportunities. Drugs Ther Perspect. 2020:1–3. doi: 10.1007/s40267-020-00785-z. doi:10.1007/s40267-020-00785-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dutta S, Kaur RJ, Bhardwaj P, Charan J, Bist SKS, Detha MD, et al. Household transmission of COVID-19:A cross-sectional study. Infect Drug Resist. 2020;13:4637–42. doi: 10.2147/IDR.S285446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dutta S, Ambwani S, Lal H, Ram K, Mishra G, Kumar T, et al. The satisfaction level of undergraduate medical and nursing students regarding distant preclinical and clinical teaching amidst COVID-19 across India. Adv Med Educ Pract. 2021;12:113–22. doi: 10.2147/AMEP.S290142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dutta S, Ambwani S, Lal H, Ram K, Mishra G, Kumar T, et al. A response to “the satisfaction level of undergraduate medical and nursing students regarding distant preclinical and clinical teaching amidst COVID-19 across India”[Response to Letter] Adv Med Educ Pract. 2021;12:349–50. doi: 10.2147/AMEP.S313975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Founou RC, Founou LL, Essack SY. Clinical and economic impact of antibiotic resistance in developing countries:A systematic review and meta-analysis. PLoS One. 2017;12:e0189621. doi: 10.1371/journal.pone.0189621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hofer U. The cost of antimicrobial resistance. Nat Rev Microbiol. 2019;17:3. doi: 10.1038/s41579-018-0125-x. [DOI] [PubMed] [Google Scholar]
- 25.Haque M, Abubakar A, Ogunleye O, Sani IH, Sefah I, Kurdi A, et al. Changes in availability, utilization, and prices of medicines and protection equipment for COVID-19 in an Urban population of Northern Nigeria. J Res Pharm Pract. 2021;10:17–22. doi: 10.4103/jrpp.JRPP_20_92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hsu J. How covid-19 is accelerating the threat of antimicrobial resistance. BMJ (Clinical research ed) 2020;369:m1983. doi: 10.1136/bmj.m1983. doi:10.1136/bmj.m1983. [DOI] [PubMed] [Google Scholar]
- 27.Abelenda-Alonso G, Padullés A, Rombauts A, Gudiol C, Pujol M, Alvarez-Pouso C, et al. Antibiotic prescription during the COVID-19 pandemic:A biphasic pattern. Infect Control Hosp Epidemiol. 2020;41:1371–2. doi: 10.1017/ice.2020.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stevens MP, Patel PK, Nori P. Involving antimicrobial stewardship programs in COVID-19 response efforts:All hands on deck. Infect Control Hosp Epidemiol. 2020;41:744–5. doi: 10.1017/ice.2020.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Godman B, Haque M, McKimm J, Abu Bakar M, Sneddon J, Wale J, et al. Ongoing strategies to improve the management of upper respiratory tract infections and reduce inappropriate antibiotic use particularly among lower and middle-income countries:Findings and implications for the future. Curr Med Res Opin. 2020;36:301–27. doi: 10.1080/03007995.2019.1700947. [DOI] [PubMed] [Google Scholar]
- 30.Al Rasheed A, Yagoub U, Alkhashan H, Abdelhay O, Alawwad A, Al Aboud A, et al. Prevalence and predictors of self-medication with antibiotics in Al Wazarat Health Center, Riyadh City, KSA. Biomed Res Int. 2016;2016:3916874. doi: 10.1155/2016/3916874. doi:10.1155/2016/3916874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kassie AD, Bifftu BB, Mekonnen HS. Self-medication practice and associated factors among adult household members in Meket district, Northeast Ethiopia, 2017. BMC Pharmacol Toxicol. 2018;19:15. doi: 10.1186/s40360-018-0205-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chang J, Ye D, Lv B, Al Battal S. Sale of antibiotics without a prescription at community pharmacies in urban China:A multicentre cross-sectional survey. J Antimicrob Chemother. 2017;72:1235–42. doi: 10.1093/jac/dkw519. [DOI] [PubMed] [Google Scholar]
- 33.Goossens H, Ferech M, Vander Stichele R, Elseviers M ESAC Project Group. Outpatient antibiotic use in Europe and association with resistance:A cross-national database study. Lancet. 2005;365:579–87. doi: 10.1016/S0140-6736(05)17907-0. [DOI] [PubMed] [Google Scholar]
- 34.Horumpende PG, Sonda TB, van Zwetselaar M, Antony ML, Tenu FF, Mwanziva CE, et al. Prescription and non-prescription antibiotic dispensing practices in part I and part II pharmacies in Moshi Municipality, Kilimanjaro Region in Tanzania:A simulated clients approach. PLoS One. 2018;13:e0207465. doi: 10.1371/journal.pone.0207465. doi:10.1371/journal.pone.0207465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Afridi MI, Rasool G, Tabassum R, Shaheen M, Siddiqullah Shujauddin M. Prevalence and pattern of self-medication in Karachi:A community survey. Pak J Med Sci. 2015;31:1241–5. doi: 10.12669/pjms.315.8216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ateshim Y, Bereket B, Major F, Emun Y, Woldai B, Pasha I, et al. Prevalence of self-medication with antibiotics and associated factors in the community of Asmara, Eritrea:A descriptive cross sectional survey. BMC Public Health. 2019;19:726. doi: 10.1186/s12889-019-7020-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Domingues PH, Galvão TF, Andrade KR, Sá PT, Silva MT, Pereira MG. Prevalence of self-medication in the adult population of Brazil:A systematic review. Rev Saude Publica. 2015;49:36. doi: 10.1590/S0034-8910.2015049005709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Isameldin E ASA, Mousnad MA. Self-medication practice among patients living in Soba-Sudan. Health Prim Car. 2020;4:2–5. [Google Scholar]
- 39.Kamati M, Godman B, Kibuule D. Prevalence of self-medication for acute respiratory infections in young children in Namibia:Findings and implications. J Res Pharm Pract. 2019;8:220–4. doi: 10.4103/jrpp.JRPP_19_121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bahta M, Tesfamariam S, Weldemariam DG, Yemane H, Tesfamariam EH, Alem T, et al. Dispensing of antibiotics without prescription and associated factors in drug retail outlets of Eritrea:A simulated client method. PLoS One. 2020;15:e0228013. doi: 10.1371/journal.pone.0228013. doi:10.1371/journal.pone.0228013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Abena PM, Decloedt EH, Bottieau E, Suleman F, Adejumo P, Sam-Agudu NA, et al. Chloroquine and hydroxychloroquine for the prevention or treatment of COVID-19 in Africa:Caution for inappropriate off-label use in healthcare settings. Am J Trop Med Hyg. 2020;102:1184–8. doi: 10.4269/ajtmh.20-0290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Godman B. Combating COVID-19:Lessons learnt particularly among developing countries and the implications. Bangladesh J Med Sci. 2020;19:S103–8. [Google Scholar]
- 43.Gautret P, Lagier JC, Parola P, Hoang VT, Meddeb L, Mailhe M, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19:Results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 2020;56:105949. doi: 10.1016/j.ijantimicag.2020.105949. doi:10.1016/j.ijantimicag. 2020.105949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sefah IA, Ogunleye OO, Essah DO, Opanga SA, Butt N, Wamaitha A, et al. Rapid assessment of the potential paucity and price increases for suggested medicines and protection equipment for COVID-19 across developing countries with a particular focus on africa and the implications. Front Pharmacol. 2021;11:588106. doi: 10.3389/fphar.2020.588106. doi:10.3389/fphar. 2020.588106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chauhan V, Galwankar S, Raina S, Krishnan V. Proctoring hydroxychloroquine consumption for health-care workers in India as per the revised national guidelines. J Emerg Trauma Shock. 2020;13:172–3. doi: 10.4103/JETS.JETS_75_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chouduri AU, Biswas M, Haque MU, Arman MSI, Uddin N, Kona N, et al. Cephalosporin-3G, highly prescribed antibiotic to outpatients in Rajshahi, Bangladesh:Prescription errors, carelessness, irrational uses are the triggering causes of antibiotic resistance. J App Pharm Sci. 2018;8:105–12. [Google Scholar]
- 47.Nasir M, Chowdhury ASMS, Zahan T. Self-medication during COVID-19 outbreak:A cross-sectional online survey in Dhaka city. COVID-19, self-medication, drug dispensing, rational use of drug. Int J Basic Clin Pharmacol. 2020;9:1325–30. [Google Scholar]
- 48.RECOVERY Collaborative Group. Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, et al. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021;384:693–704. doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Johnson RM, Vinetz JM. Dexamethasone in the management of covid -19. BMJ. 2020;370:m2648. doi: 10.1136/bmj.m2648. doi:10.1136/bmj.m2648. [DOI] [PubMed] [Google Scholar]
- 50.Dutta S. Pharmacovigilance in India:Evolution and change in scenario in India. Int J Sci Res. 2018;7:976–8. [Google Scholar]
- 51.Dutta S, Ambwani S, Mishra G, Lal HI, Ram K, Kumar T, et al. Pharmacovigilance in the era of Covid-19:A concise review of the current scenario, implications, and challenges. Int J App Pharm. 2021;13:1–4. doi:10.22159/ijap. 2021v13i3.41063. [Google Scholar]
- 52.Dutta S, Kaur RJ, Bhardwaj P, Sharma P, Ambwani S, Islam S, et al. Adverse events reported from the COVID-19 vaccines:A descriptive study based on the WHO database (VigiBase®) J Appl Pharm Sci. 2021;11:1–9. [Google Scholar]
- 53.Jeet Kaur R, Dutta S, Charan J, Bhardwaj P, Tandon A, Yadav D, et al. Cardiovascular adverse events reported from COVID-19 vaccines:A study based on WHO database. Int J Gen Med. 2021;14:3909–27. doi: 10.2147/IJGM.S324349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kaur RJ, Dutta S, Bhardwaj P, Charan J, Dhingra S, Mitra P, et al. Adverse events reported from COVID-19 vaccine trials:A systematic review. Indian J Clin Biochem. 2021;36:1–13. doi: 10.1007/s12291-021-00968-z. doi:10.1007/s12291-021-00968-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dutta R, Raja D, Anuradha R, Dcruze L, Jain T, Sivaprakasam P. Self-medication practices versus health of the community. Int J Community Med Public Health. 2017;4:2757–61. [Google Scholar]
- 56.Kumar V, Mangal A, Yadav G, Raut D, Singh S. Prevalence and pattern of self-medication practices in an urban area of Delhi, India. Med J DY Patil Univ. 2015;8:16–20. [Google Scholar]
- 57.Marathe PA, Kamat SK, Tripathi RK, Raut SB, Khatri NP. Over-the-counter medicines:Global perspective and Indian scenario. J Postgrad Med. 2020;66:28–34. doi: 10.4103/jpgm.JPGM_381_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Panda A, Pradhan S, Mohapatro G, Kshatri JS. Predictors of over-the-counter medication:A cross-sectional Indian study. Perspect Clin Res. 2017;8:79–84. doi: 10.4103/2229-3485.203043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Phalke V, Phalke D, Durgawale P. Self-medication practices in rural Maharashtra Indian J Community Med. 2006;31:34–5. [Google Scholar]
- 60.Selvaraj K, Kumar SG, Ramalingam A. Prevalence of self-medication practices and its associated factors in Urban Puducherry, India. Perspect Clin Res. 2014;5:32–6. doi: 10.4103/2229-3485.124569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jha DN. [Updated on 2015 Apr 08, 2015;Last accessed on 2021 May 16];52% Indians self-medicate The Times of India 2015. Available from: https://timesofindia.indiatimes.com/city/delhi/52-Indians-self-medicate/articleshow/46844097.cms . [Google Scholar]
- 62.Charan J, Saxena D, Chaudhari M, Dutta S, Kaur RJ, Bhardwaj P. Opinion of patients seeking primary care regarding prescription of generic drugs:A cross-sectional study. J Family Med Prim Care. 2020;9:5725–30. doi: 10.4103/jfmpc.jfmpc_1694_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Health in India:NSS 71 st Round (Jan –Jun 2014) Government of India. Ministry of Statistics and Programme Implementation:National Sample Survey Office, Government of India. 2016. [Updated on 2016 Apr;Last accessed on 2021 May 16]. Available from: http://mospi.nic.in/sites/default/files/publication_reports/nss_rep574.pdf .
- 64.Murphy A, Palafox B, Walli-Attaei M, Powell-Jackson T, Rangarajan S, Alhabib KF, et al. The household economic burden of non-communicable diseases in 18 countries. BMJ Global Health. 2020;5:e002040. doi: 10.1136/bmjgh-2019-002040. doi:10.1136/bmjgh-2019-002040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pandey A PG, Clarke L, Dandona L. Trends in catastrophic health expenditure in India:1993 to 2014. Bulletin of the World Health Organization:World Health Organization. 2017. [Updated on 2018;Last accessed on 2021 May 16]. Available from: https://www.who.int/bulletin/volumes/96/1/17-191759/en/#:~:text=Out%2Dof%2Dpocket%20payments%20remain,%20is%20covered%20by%20health%20insurance.&text=In%202014%2C%20such%20payments%20were,%20of%20US%24%2097.1%20 billion . [DOI] [PMC free article] [PubMed]
- 66.Selvaraj S, Farooqui HH, Karan A. Quantifying the financial burden of households'out-of-pocket payments on medicines in India:A repeated cross-sectional analysis of National Sample Survey data, 1994–2014. BMJ Open. 2018;8:e018020. doi: 10.1136/bmjopen-2017-018020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Charan J, Saxena D, Chaudhri M, Dutta S, Kaur RJ, Bhardwaj P. Opinion of primary care physicians regarding prescription of generic drugs:A cross-sectional study. J Family Med Prim Care. 2021;10:1390–8. doi: 10.4103/jfmpc.jfmpc_2157_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Haque M, Kumar S, Charan J, Bhatt R, Islam S, Dutta S, et al. Utilisation, availability and price changes of medicines and protection equipment for COVID-19 among selected regions in India:Findings and implications. Front Pharmacol. 2021;11:582154. doi: 10.3389/fphar.2020.582154. doi:10.3389/fphar. 2020.582154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Godman B, Haque M, Islam S, Iqbal S, Urmi UL, Kamal ZM, et al. Rapid assessment of price instability and paucity of medicines and protection for COVID-19 across Asia:Findings and public health implications for the future. Front Public Health. 2020;8:585832. doi: 10.3389/fpubh.2020.585832. doi:10.3389/fpubh. 2020.585832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kibuule D, Nambahu L, Sefah IA, Kurdi A, Phuong TNT, Kwon H-Y, Godman B. Activities in Namibia to limit the prevalence and mortality from COVID-19 including community pharmacy activities and the implications. Sch Acad J Pharm. 2021;10:82–92. [Google Scholar]
- 71.Lam CL, Catarivas MG, Munro C, Lauder IJ. Self-medication among Hong Kong Chinese. Soc Sci Med. 1994;39:1641–7. doi: 10.1016/0277-9536(94)90078-7. [DOI] [PubMed] [Google Scholar]
- 72.Jorgji K, Bebeci E, Apostoli P, Apostoli A. Evaluation of use of antibiotics without prescription among young adults in Albania case study:Tirana and Fier District. Hippokratia. 2014;18:217–20. [PMC free article] [PubMed] [Google Scholar]
- 73.Onchonga D. A Google trends study on the interest in self-medication during the 2019 novel coronavirus (COVID-19) disease pandemic. Saudi Pharm J. 2020;28:903–4. doi: 10.1016/j.jsps.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Onchonga D, Omwoyo J, Nyamamba D. Assessing the prevalence of self-medication among healthcare workers before and during the 2019 SARS-CoV-2 (COVID-19) pandemic in Kenya. Saudi Pharm J. 2020;28:1149–54. doi: 10.1016/j.jsps.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sadio AJ, Gbeasor-Komlanvi FA, Konu RY, Bakoubayi AW, Tchankoni MK, Bitty-Anderson AM, et al. Assessment of self-medication practices in the context of the COVID-19 outbreak in Togo. BMC Public Health. 2021;21:58. doi: 10.1186/s12889-020-10145-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Choudhary N, Lahiri K, Singh M. Increase and consequences of self-medication in dermatology during COVID-19 pandemic:An initial observation. Dermatol Ther. 2021;34:e14696. doi: 10.1111/dth.14696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chopra D, Bhandari B, Sidhu JK, Jakhar K, Jamil F, Gupta R. Prevalence of self-reported anxiety and self-medication among upper and middle socioeconomic strata amidst COVID-19 pandemic. J Edu Health Promot. 2021;10:73. doi: 10.4103/jehp.jehp_864_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chakraborty K, Chatterjee M. Psychological impact of COVID-19 pandemic on general population in West Bengal:A cross-sectional study [ACCELERATED RESEARCH] Indian J Psychiatry. 2020;62:266–72. doi: 10.4103/psychiatry.IndianJPsychiatry_276_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nina PB, Dash AP. Hydroxychloroquine as prophylaxis or treatment for COVID-19:What does the evidence say? Indian J Public Health. 2020;64(Suppl):S125–7. doi: 10.4103/ijph.IJPH_496_20. [DOI] [PubMed] [Google Scholar]
- 80.Saghir SAM, AlGabri NA, Alagawany MM, Attia YA, Alyileili SR, Elnesr SS, et al. Chloroquine and hydroxychloroquine for the prevention and treatment of COVID-19:A fiction, hope or hype?An updated review. Ther Clin Risk Manag. 2021;17:371–87. doi: 10.2147/TCRM.S301817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Tripathy JP. Does pandemic justify the use of hydroxychloroquine for treatment and prevention of COVID-19 in India? J Med Virol. 2020;92:1391–3. doi: 10.1002/jmv.25933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Armitage R, Nellums LB. Antibiotic prescribing in general practice during COVID-19. Lancet Infect Dis. 2021;21:e144. doi: 10.1016/S1473-3099(20)30917-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Langford BJ, So M, Raybardhan S, Leung V, Westwood D, MacFadden DR, et al. Bacterial co-infection and secondary infection in patients with COVID-19:A living rapid review and meta-analysis. Clin Microbiol Infect. 2020;26:1622–9. doi: 10.1016/j.cmi.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Morgan DJ, Okeke IN, Laxminarayan R, Perencevich EN, Weisenberg S. Non-prescription antimicrobial use worldwide:A systematic review. Lancet Infect Dis. 2011;11:692–701. doi: 10.1016/S1473-3099(11)70054-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Cassini A, Högberg LD, Plachouras D, Quattrocchi A, Hoxha A, Simonsen GS, et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015:A population-level modelling analysis. Lancet Infect Dis. 2019;19:56–66. doi: 10.1016/S1473-3099(18)30605-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Llor C, Bjerrum L. Antimicrobial resistance:Risk associated with antibiotic overuse and initiatives to reduce the problem. Ther Adv Drug Saf. 2014;5:229–41. doi: 10.1177/2042098614554919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Eriksen J, Gustafsson LL, Ateva K, Bastholm-Rahmner P, OvesjöML, Jirlow M, et al. High adherence to the 'Wise List'treatment recommendations in Stockholm:A 15-year retrospective review of a multifaceted approach promoting rational use of medicines. BMJ Open. 2017;7:e014345. doi: 10.1136/bmjopen-2016-014345. doi:10.1136/bmjopen-2016-014345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Gustafsson LL, Wettermark B, Godman B, Andersén-Karlsson E, Bergman U, Hasselström J, et al. The 'wise list'- a comprehensive concept to select, communicate and achieve adherence to recommendations of essential drugs in ambulatory care in Stockholm. Basic Clin Pharmacol Toxicol. 2011;108:224–33. doi: 10.1111/j.1742-7843.2011.00682.x. [DOI] [PubMed] [Google Scholar]


