Abstract
Partial Hemolysis, elevation of liver enzymes and low platelet count (HELLP) syndrome is a leading cause of maternal mortality. With the exceeding spread of COVID-19, leading to increasing number of COVID-19 infected cases there has been a emergence of an overlap of COVID-19 with HELLP Syndrome. Multiple factors are associated with the thrombocytopenia witnessed in COVID-19 somewhat similar to what is witnessed in preeclampsia and HELLP Syndrome. We Describe a case series of two ante natal cases who presented with a picture of HELLP syndrome and upon investigations turned out to be COVID-19 thus trying to establish an association between the two.
Keywords: COVID-19, HELLP syndrome, thrombocytopenia
Introduction
Severe Acute Respiratory Syndrome Coronavirus 2 (SARS Cov2) causes an acute respiratory as well as systemic illness. It can lead to complications such as respiratory distress, multiple organ dysfunction as well as intravascular coagulopathy. For optimized care of patients infected with COVID-19 active assessment is required in order to judge the severity of the disease.
On the other hand Pre-eclampsia is a leading cause of maternal mortality worldwide which leads to rapid deterioration without any prior warnings.[1] Proteinuria is essential for diagnosis of pre-eclampsia which is diagnosed as hypertension post 20 weeks of gestation along with proteinuria and/or acute kidney injury, neurological features, dysfunction of the liver, thrombocytopenia or hemolysis or growth restriction of the fetus. Pre-eclampsia may be diagnosed intrapartum or early postpartum.[2]
Hemolysis elevated liver enzymes along with low platelets (HELLP) syndrome also has a presentation with similar spectrum.
Primary care providers catering at the root level of the health care system are often the first line of defense against COVID-19 as well as in the combat against maternal mortality. During the ongoing pandemic providing care to pregnant patients becomes challenging with various complications of COVID-19 in ante natal period including the aspect of its postulated association or overlap with HELLP Syndrome.
We describe a case series with two cases that presented during their pregnancy with a lab picture of HELLP Syndrome and had ground glass opacities on HRCT Chest.
On investigating further, they turned out to be positive for COVID-19.
We support the hypothesis that the synergism in the pathophysiology of COVID-19 and HELLP syndrome has proved to be a lethal one which has led to increasing number of maternal mortalities.
Case Series
Case 1
A 32-year-old primigravida with 34 weeks presented with the chief complaint of myalgia, yellowish discoloration of skin, darkening of urine along with mild discomfort in the right upper abdomen since four days. There was no prior history of hypertension, diabetes mellitus or any other chronic medical conditions. The patient had no history of fever or flu like symptoms, no history of breathlessness or chest pain.
Obstetric history revealed duration of marriage 3 years, primi, two tetanus injections received. Menstrual history revealed last menstrual period 36 weeks prior to her admission.
On examination the patient was afebrile, respiratory rate was 24 breaths per minute, pulse was 82/min, regular in rhythm and blood pressure was 116/82 mm hg in right arm supine position. On systemic examination uterus was 32 weeks in size, relaxed, cephalic, Fetal heart sound were absent, On per vaginum examination os was 2 cm dilated, 25 percent effaced and station was -2, memneranes present, presenting part vertex, show present, pelvis seemed to be adequate. Heart sounds were normal, Patient was conscious and oriented and chest was bilateral clear. Laboratory investigations are mentioned in Table 1
Table 1.
Lab investigations of all the cases
| Lab Paramteter | Case 1 Age-32 Years |
Case 2 Age-29 Years |
Case 3 Age-26 Years |
|---|---|---|---|
| CBC | Hb-9.3 gm/dl MCV-86 fl Platelet count-86000/dl WBC Count-4900/dl |
Hb8.6 gm/dl, MCV: 82 fl, Platelet count 81000/dl, WBC Count 5800/dl |
Hb-10.1 gm/dl MCV-90 fl Platelet count-90000/dl, WBC Count 6000/dl |
| LFT | Total Protein-5.4 gm/dl, Albumin 2.1 gm/dl, Globulin 3.3 gm/dl, aspartate aminotransferase 626 units/l, alanine aminotransferase 228 units/l, Alkanline Phophatase 122 IU/l, Total Bilirubin :8.8 mg/dl Unconjugated -6.6 mg/dl |
Total Protein-5.8 gm/dl, Albumin 2.2 gm/dl, Globulin3.6 gm/dl, aspartate aminotransferase 524 units/l, alanine aminotransferase 230 units/l, Alkanline Phophatase 128 IU/l, Total Bilirubin :9.9 mg/dl Unconjugated -7.2 mg/dl |
Total protein -5.8 gm/dl Albumin-2.4 gm/dl, globulin-3.4 gm/dl, aspartate aminotransferase-589 units/l, alanine aminotransferase-300 units/l, alkaline phosphatase 134 IU/l, Total Bilirubin-9.4 mg/dl, Unconjugated -6.9 mg/dl |
| KFT | Creatinine: 1.4 mg/dl, Urea 30 mg/dl, Sodium 134 mmol/l, Potassium - 3.6 mmol/l |
Creatinine: 1.0 mg/dl, Urea 39 mg/dl, Sodium 137 mmol/l, Potassium - 3.89 mmol/l |
Creatinine-0.9 mg/dl Urea-33 mg/dl Sodium 139 mmol/l Potassium 0 4.49 mmol/l |
| CRP | 60.0 mg/dl | 91.7 mg/dl | 78.5 mg/dl |
| D-Dimer | 5.53 | 6.62 | 6.23 |
| Serum Ferritin | 650 ng/ml | 890 ng/ml | 734 ng/dl |
| LDH | 2500 | 2700 | 3100 |
| HRCT Score | 15/25 | 18/25 | 16/26 |
| CORAD | 5 | 6 | 6 |
Oxytocin 2.5 units was given and titration of oxytocin was done and in view of non-progression of labor, emergency caesarian section was done. Baby was declared still born.
On day 3 of admission, patient went into respiratory distress and spo2 reduced to 90 percent on room air. An urgent HRCT was done which was suggestive of ground glass opacities with HRCT Score of 15/25 with CORAD 5 as shown in Figure 1. A nasopharyngeal swab was sent which was positive for COVID-19. Patient was given oxygen support along with remdesavir, antibiotics and other supportive measures. Oxygen was titrated during the hospital stay and patient recovered by 14 day of admission and was discharged in stable condition.
Figure 1.
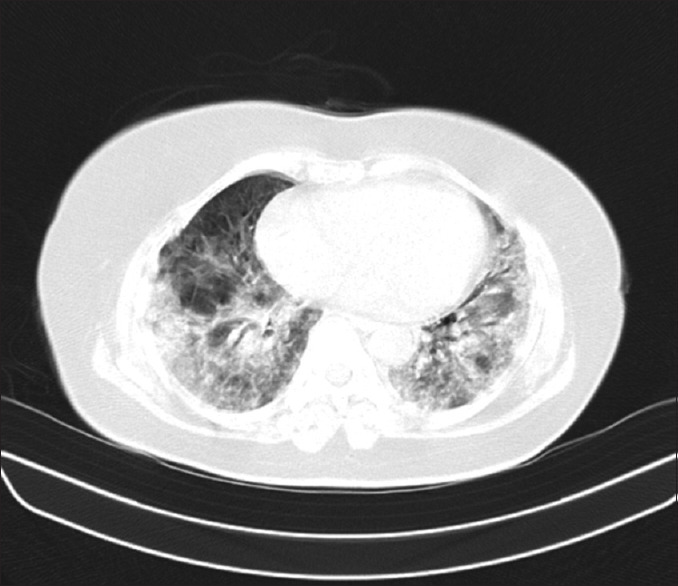
Showing HRCT of case 1 with ground glass opacity
Case 2
A 29-year-old G3P2L1D1 with 37 weeks presented with the chief complaint of fever and bilateral pedal edema.
There was no prior history of hypertension, diabetes mellitus or any other chronic medical conditions.
The patient had no history of breathlessness or chest pain. Obstetric history revealed duration of marriage 6 years, two tetanus injections received.
Menstrual history revealed last menstrual period 39 weeks prior to her admission.
On examination the patient was febrile with temperature of 101 degree Fahrenheit, respiratory rate was 20 breaths per minute, pulse was 88/min, regular in rhythm and blood pressure was 144/98 mm hg in right arm supine position. On systemic examination uterus was 36 weeks in size, contractions present, Left occipito anterior position, cephalic, Fetal heart sound were present, regular, 150 beats per minute, head engaged, non-stress test was done indicative of more than 2 accelerations with beat to beat variability with no decelerations. On per vaginum examination cervix mid posterior and soft, os was 5 cm dilated, 75 percent effaced and station was 0, memneranes bulging, presenting part vertex, pelvis seemed to be adequate. Heart sounds were normal, Patient was conscious and oriented and chest was bilateral clear. Laboratory investigations are mentioned in Table 1.
Nasopharyngeal swab was done which came positive for COVID-19.
Baby was delivered and was declared to be normal with birth weight of 2.5 kg.
Patient developed generalized tonic clonic seizure post-delivery with a blood pressure of 180/110 mm Hg and was given magnesium sulfate along with labetalol.
Patient was stabilized and shifted to intensive care unit. Patient developed hematuria 4 hours post-delivery. Her spo2 dropped to 92 percent on room air, was given oxygen support and an HRCT chest was done which showed ground glass opacity with CT severity score of 18/25 and CORAD 6 as depicted in Figure 2. She was started on remdesavir, antibiotics and other supportive measures On day 3 of admission patient was taken in non-invasive ventilation as her condition deteriorated further. On day 6 of admission the patient was unable to maintain saturation and hence was taken on mechanical ventilator. Patient ultimately succumbed on day 8 of admission.
Figure 2.
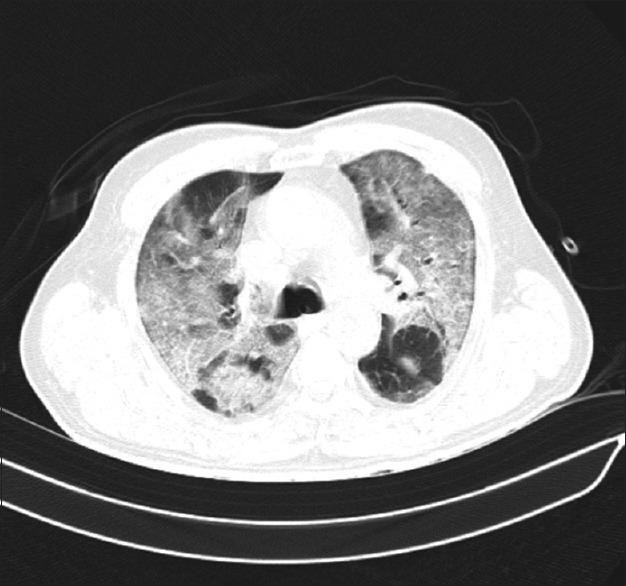
HRCT of case 2 with ground glass opacity
Case 3
A 26-year-old female primigravida presented at 39 weeks of gestation with the chief complaint of pain in the upper right quadrant of abdomen and headache since two days.
There was no history of hypertension, diabetes mellitus or thyroid disorder in the past however patient was diagnosed with gestational hypertension for the first time during her pregnancy and was on medication for the same.
Patient had tested positive for COVID-19 by RTPCR method two days back,
Obstetric History revealed duration of marriage to be one year and patient was primigravida
Two doses of tetanus toxoid were received.
Menstrual history revealed last menstrual cycle 40 weeks back
On general examination Pulse was 98 beats per minute, regular, blood pressure was 160/100 mm hg in right arm supine position and spo2 was 95 percent on room air.
On systemic examination abdominal examination revealed uterus to be term size, relaxed, oblique lie, Fetal heat sound present, regular, 158 beats per minute
On per vaginum examination os closed, uneffaced, pelvis seemed to be borderline
Laboratory investigations were suggestive of a picture of HELLP Syndrome which are mentioned in Table 1. Emergency section was done in view of oblique lie and a healthy infant of male gender of 2.9 kg was delivered. An HRCT was done which was suggestive of bilateral ground glass opacities with CT severity score of 16/25 and CORAD 6 as shown in Figure 3. Patient was started on antibiotics, steroids and other supportive measures. During the course of hospital stay patient improved clinically, pain reduced and bilirubin and liver enzymes were showing reducing trend. Patient recovered completely and was discharged on 15th day of admission.
Figure 3.
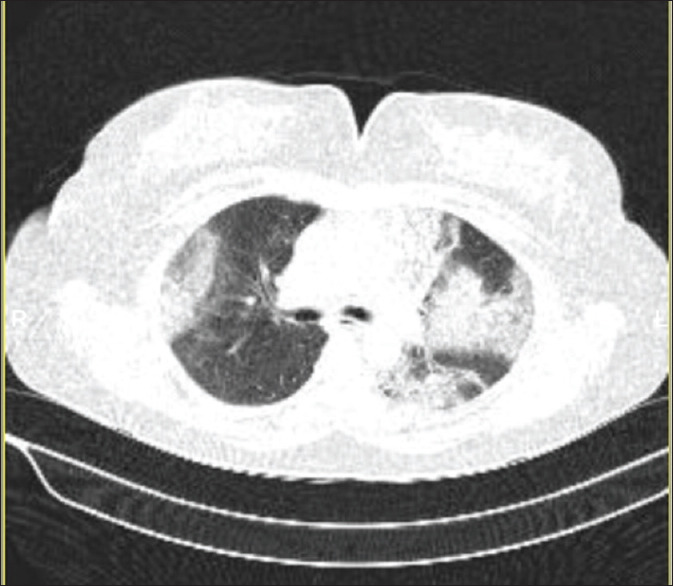
HRCT Chest of CASE 3 showing bilateral ground glass opacity
Discussion
Considering the clinical and laboratory parameters diagnosis of HELLP Syndrome seemed to be acceptable in all of our cases, decision making was done keeping in account the safety of the mother prior to the safety of the fetus and management was thus done.
It is important to note that the findings along with the COVID-19 positive status points towards COVID-19 being the etiology behind hemolysis and thrombocytopenia. Severe clinical deterioration which was rapid is observed and it might result in fatal outcomes.
Thrombocytopenia observed in COVID-19 has multiple causes including damage to the endothelium, activation and aggregation of the platelets, bone marrow suppression impairment of activity of the megakaryocytes.[3] Platelet defragmentation may also be caused due to the changes observed in morphology of the pulmonary capillary bed.
It is established that the endothelial damage, activation of the platelet and thrombus formation is somewhat similar to HELLP Syndrome as well as pre-eclampsia.[4,5]
Our cases presented with the classical presentations of HELLP Syndrome however upon further investigations HRCT Revealed ground glass opacity, a tell-tale sign of COVID-19.[6]
It was ultimately concluded to be a case of COVID-19 presenting as HELLP Syndrome.
Hemolysis with elevated liver enzymes, hemolysis and low platelet count (HELLP) syndrome is a dangerous obstetric disease which leads on to activation of the general inflammatory cascade progressing into extensive damage to the endothelium along with thrombocytopenia.[7] It is associated with increased maternal and fetal complications.[8]
Given the background of our case series it can be concluded that there is obvious synergism in COVID-19 and HELLP Syndrome thus adding upon each other leading to a profound response and greater maternal and fetal compromise.[9]
During the pandemic of COVID-19 patients with increased risk of compilations remain the ant natal cases and proper care should therefore be provided to prevent adverse effects of COVID-19 associated with HELLP Syndrome.[10]
The physicians at primary healthcare facilities tend to be encountering patients with HELLP Syndrome and therefore they need to be warned of an association of COVID-19. Physicians posted at primary healthcare should thus screen the patients with HELLP syndrome for COVID-19 as the association of both these entities can prove to be fatal such as in the cases we have presented.
Conclusion
Thus, through the means of this case series we conclude that there is a synergism in the pathophysiology of COVID-19 and HELLP Syndrome thus adding upon each other these two deadly conditions lead to a rare but difficult compromise of the fetus and the mother.
This can be a dangerous overlap or an association which should be kept in mind by the clinicians when they encounter a pregnant female with thrombocytopenia as that simple thrombocytopenia can be a warning sign of a lethal storm in the form of COVID-19 associated with HELLP Syndrome.
Key Points
There in an important overlap or association between HELLP Syndrome and COVID-19.
Clinicians treating COVID-19 on the frontline should be aware of the similarities of COVID-19 and HELLP Syndrome in pregnancy
COVID-19 contracted during pregnancy can result in significant morbidity or mortality and hence should be treated judiciously.
Take Home Message
Special care should be taken for ante natal cases during the ongoing pandemic of COVID-19 as they are at higher risk of getting deadly complications such as HELLP Syndrome which might be an association or an similar presentation with potentially lethal outcome resulting in maternal mortality.
Informed Consent
Written & Oral informed consent was obtained from all individual participants included in the study. Additional informed consent was obtained from all individual participants for whom identifying information is included in this manuscript.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kreutz R, Algharably EAE, Azizi M. Hypertension, the renin-angiotensin system, and the risk of lower respiratory tract infections and lung injury:implications for COVID-19. Cardiovasc Res. 2020;116:1688–99. doi: 10.1093/cvr/cvaa097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yoon SH, Lee KH, Kim JY. Chest radiographic and CT findings of the 2019 novel coronavirus disease (COVID- 19):Analysis of nine patients treated in Korea. Korean J Radiol. 2020;21:494–500. doi: 10.3348/kjr.2020.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haram K, Svendsen E, Abildgaard U. The HELLP syndrome:clinical issues and management. A Review. BMC Pregnancy Childbirth. 2009;9:8. doi: 10.1186/1471-2393-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schnettler WT, Al Ahwel Y, Suhag A. Severe acute respiratory distress syndrome in coronavirus disease 2019 -infected pregnancy:Obstetric and intensive care considerations. Am J Obstet Gynecol MFM. 2020;2:100120. doi: 10.1016/j.ajogmf.2020.100120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women:a retrospective review of medical records. Lancet. 2020;395:809–15. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mahajan O, Talwar D, Kumar S, Jaiswal A, Madaan S, Khanna S, et al. Fatal HELLP syndrome in pregnancy:A sequelae of Long COVID? Med Sci. 2021;25:1878–81. [Google Scholar]
- 7.Norooznezhad AH, Nurzadeh M, Darabi MH, Naemi M. Coronavirus disease 2019 (COVID-19) in a pregnant women with treatment resistance thrombocytopenic purpura with and suspicion to HELLP syndrome:A case report. BMC Pregnancy Childbirth. 2021;21:567. doi: 10.1186/s12884-021-04030-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martínez-Martínez C, Montes-García AE, Barrera-García AG, Marchan-Tovar TL, Adaya-Leythe EA, Mendoza-Hernández F, et al. COVID-19 and HELLP Syndrome, uncertain diagnosis:Case report. Ginecol Obstet Mex. 2021;89:247–54. [Google Scholar]
- 9.Ronnje L, Länsberg J-K, Vikhareva O, Hansson SR, Herbst A, Zaigham M. Complicated COVID-19 in pregnancy:A case report with severe liver and coagulation dysfunction promptly improved by delivery. BMC Pregnancy Childbirth. 2020;20:1–8. doi: 10.1186/s12884-020-03172-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Futterman I, Toaff M, Navi L, Clare CA. COVID-19 and HELLP:Overlapping clinical pictures in two gravid patients. Am J Perinatol Rep. 2020;10:e179–82. doi: 10.1055/s-0040-1712978. [DOI] [PMC free article] [PubMed] [Google Scholar]


