Abstract
Background:
Some studies reported the association between fibroids with uterine inflammation. By considering this hypothesis, the formation and recurrence of uterine fibroids can be prevented by diagnosis and treatment of inflammation, and complications and costs can be reduced. This study aimed to evaluate the association between chronic endometritis and uterine fibroids in non-menopausal women.
Materials and Methods:
This prospective case-control study was performed on non-menopausal women referred to Al-Zahra Hospital in Rasht during April 2019-April 2020. Non- menopausal women of reproductive age (20-55 years old) with abnormal uterine bleeding who were candidates for hysteroscopy based on medical history and ultrasound reports were included in this study. The case group with fibroids were divided into two groups of intramural and subserosal myoma group and submucosal group based on the location of fibroids. The control group was patients with abnormal uterine bleeding complaints and no uterine fibroid. Endometrial specimens were examined by a pathologist for histological and immunochemistry assessments. In interpreting the results of endometrial biopsy, a positive result was indicated by the presence of one or more plasma cells per 10 high power field. Data were gathered by a form including age, parity, history of recurrent miscarriage, patient’s complaint (abnormal uterine bleeding), hysteroscopic results (submucosal myoma-polyp-normal), uterine histology (polyp, endometritis, and hyperplasia) and prevalence of chronic endometritis based on plasma cell in the biopsy. Data were analyzed by SPSS software version 21. Data were reported by descriptive statistics including number, percent, mean and standard deviation. The normality of quantitative data was assessed by the Kolmogorov- Smirnov test. Mann-Whitney U test, Chi-square and Fisher exact tests were used to compare groups and logistic regression was used to control the effect of confounders.
Results:
The incidence of chronic endometritis was 39% (38 out of 97) and a higher incidence of chronic endometritis was noted in the case group than the control group (46% vs. 31%), No significant difference was observed between the two groups (P > 0.05). However, the incidence of chronic endometritis in women with submucosal myoma was higher than the intramural and subserosal groups (64% vs. 37%) (P = 0.04). To control the effect of age on the rate of chronic endometritis in both groups, no significant effect was observed in logistic regression.
Conclusions:
The results showed the overall incidence of chronic endometritis was higher than previous studies and also the incidence was higher and more significant in women with submucosal myoma than in the intramural and subserosal group. As in this study, authors assessed the association between chronic endometritis and uterine fibroids, further studies assessing the cause and effect relationships are recommended.
Keywords: Chronic endometritis, uterine fibroids, women
Introduction
Uterine fibroids are the most prevalent benign tumors of the uterine.[1] Their prevalence is 30-70% among women of reproductive age.[1] Uterine fibroids can cause menstrual irregularities, heavy menstrual bleeding, and anemia.[2] Furthermore, it seems that uterine fibroids associate with infertility and adverse obstetric outcomes.[3,4]
Despite, its high prevalence, no specific etiology has been proven so far. Some of these risk factors are age, race, body mass index, genetic, reproductive factors, sex hormones, obesity, lifestyle (diet, caffeine, alcohol use, physical activity, and stress), environmental factors and underlying diseases (hypertension and infection).[1,5,6]
To identify the pathogenesis of uterine fibroids, some studies have reported the association between fibroids with uterus infection and chronic inflammation[7] and it has been stated that with different mechanisms such as Extracellular matrix (ECM) protein increase, cytokine expression, etc., inflammatory conditions in both general and local endometrium can be effective in causing uterine fibroids.[8,9,10,11]
Ciebiera et al.,[12] reported that TNF-a is one of the most important cytokines that are related to the biology, complaints, and symptoms of uterine fibroids. It has been estimated that there is higher concentration of TNF-a and the existence of inflammation status in women with uterine fibroids.
It has also been reported that the chance of developing uterine fibroids may be increased 3.7 times after three occurrences of pelvic inflammatory disease (PID), 3.2 times after chlamydial infection, and 5.3 times after using an IUD.[13] Another study found that macrophage infiltration in submucosal fibroids was higher than intramural and subserosal fibroids.[14,15]
Chronic endometritis is defined as resistant inflammation in the uterine endometrium. The diagnosis of chronic endometritis in histology is the detection of the presence of plasma cells in the endometrial stroma. Plasma cell identification is performed using hematoxylin-eosin staining on paraffin-impregnated wax-embedded endometrial specimens, which is the gold standard method for the diagnosis of chronic endometritis.[16,17,18,19] Song reported that the prevalence of chronic endometritis in non- menopausal women was 24% and higher prevalence was noted in cases of recurrent implantation failure, abnormal uterine bleeding (AUB), endometrial hyperplasia and submucosal fibroids.[20]
In a previous study by the authors of the current article, it was found that in women with metabolic syndrome, submucosal fibroids were significantly lower than the non-metabolic syndrome group. On this basis, researchers hypothesized that inflammation and infection may play a possible role in the higher prevalence of submucosal fibroids in patients without metabolic syndrome.[21]
The relationship between chronic endometritis and reproductive outcomes such as recurrent miscarriage and recurrent implantation failure has been evaluated in previous studies, and some studies have been performed for use of antibiotic treatment.[22,23,24,25,26] However, there are limited studies about the relationship between chronic endometritis and uterine fibroids. As in this study authors assessed the association between chronic endometritis and uterine fibroids, further studies assessing the cause and effect relationships are recommended, so that if chronic endometritis is associated with uterine fibroids, medical treatment of chronic endometritis may reduce the rates of myomectomy and hysterectomy surgeries.
Material and Methods
This case-control prospective study was performed on all non-menopausal women referred to Al-Zahra Hospital in Rasht who were candidates for hysteroscopy due to abnormal uterine bleeding (AUB) during April 2019-April 2020. Non- menopausal women of reproductive age (20-55 years old) with abnormal uterine bleeding who were candidates for hysteroscopy based on medical history and ultrasound reports were included in this study. Exclusion criteria were noted as suspected gynecological infection, having an intrauterine device (IUD), a history of endometrial carcinoma, pregnancy or pregnancy-related complications, hysteroscopy surgery during the last 3 months and polyps with hyperemic and hypervascular hysteroscopy view.
The case group was all non-menopausal women with AUB who reported uterine fibroids according to the ultrasound report (by GE voluson (E6) Device-China). The control group included non- menopausal women of reproductive age (20-55 years old) who had polyps and no other gynecologic disorders and were candidates for hysteroscopy based on medical history and ultrasound reports. Both groups were matched based on <35 and >35 years of age.
Based on the ultrasound report of the fibroid site, the case group (patients with fibroids) were identified as submucosal and intramural and subserosal fibroids. For all eligible patients, height by tape meter and in barefoot and weight in light clothing with standardized scale were measured. Waist circumference measured by a tape meter placed on the upper surface of the iliac crest just below the navel.
Hysteroscopy
Hysteroscopy was performed by infertility fellowship on hospitalized patients under anesthesia in the follicular phase.
Before the operation, a dilator drug was not used to prepare the cervix, and during the operation, mechanical dilatation was used by a cervical dilator. The uterine expansion was performed by a 30-degree, 4-milimeter storze (Germany) hysteroscope, and using saline media. After complete observation of the entire uterine cavity and cervix and assessing the presence of anatomical lesions inside the cavity such as polyps, submucosal myomas, adhesions and evaluating endometrium for manifestations such as hyperemia and hypervascularity or irregular endometrium, the biopsy was obtained from all parts of the uterine cavity and a sample was sent in formalin for pathology. Polyp was removed with hysteroscopic scissors and submucosal myoma with a 12-degree bipolar resectoscope.
Histological and immunochemistry analysis
Endometrial specimens were fixed with formalin and placed in paraffin and sent to the laboratory of Al-Zahra Hospital in Rasht and histological and immunochemistry assessments were performed by a pathologist. In interpreting the results of endometrial biopsy, if there was less than one plasma cell per 10 high power fields, it was indicated as a negative result. The diagnosis of chronic endometritis was indicated when one or more plasma cell was seen per 10 high power field.[27]
Variables included age, parity, history of abortion, history of recurrent miscarriage, patient complaint (pattern of abnormal uterine bleeding), hysteroscopic results (submucosal-polyp-normal-intrauterine adhesion-uterine anomaly), uterine histology (normal-hyperplasia-polyp-fibroid), and the prevalence of chronic endometritis.
Sample size determination
The sample size was estimated based on the frequency of intramural and submucosal fibroids with chronic endometritis was 59.1% and in normal patients was 26.4% in the study by Song et al.[20] Considering 95% confidence interval, 95% test power, at least 43 samples were needed in each group. Sampling was performed by the convenient method.
Ethical consideration
Ethical approval was obtained from the ethics committee of the Vice-Chancellor of Research at Guilan University of Medical Sciences (Code: IR.GUMS.REC.1398.187, Date: 2019.07.17). Informed consent letters were taken from all participants.
Statistical analysis
Data were reported by descriptive statistics including number, percent, mean and standard deviation. The normality of quantitative data was assessed by the Kolmogorov- Smirnov test. A non-parametric Mann-Whitney U test was used to compare non-normally distributed variables. Chi-square and Fisher exact tests were used to compare qualitative variables. Due to the matching of the groups in terms of age (< and > 35), logistic regression was used to control the age as a confounding factor (by SPSS software version 21). The significance level in this study was considered less than 0.05. In the present study, 97 women were studied, of which 48 were in the group without fibroids (control group) and 49 in the group of uterine fibroids (case group) [Figure 1].
Figure 1.
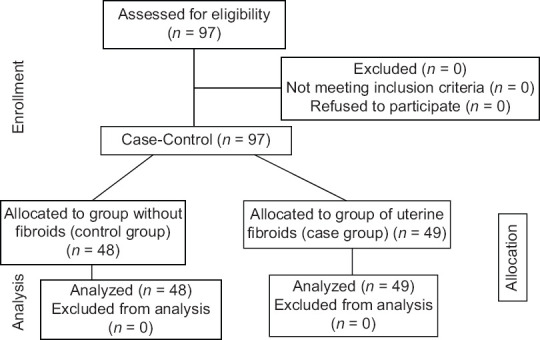
Study by Consort flowchart
Results
In the present study, 97 women were studied, of which 48 were in the group without fibroids (control group) and 49 in the group of uterine fibroids (case group). Of the case group with uterine, 32 had intramural and subserosal fibroids and 17 had submucosal fibroids. The frequency of demographic characteristics and obstetric variables between the two groups is shown in Table 1.
Table 1.
Frequency of demographic characteristics and obstetric variables between case and control groups
| Case group (n=49) | Control group (n=48) | P | |
|---|---|---|---|
| Age (years) | 43.41±5.12 | 39.87±7.21 | 0.01* |
| BMI | 30.20±1.12 | 28.12±5.1 | 0.14* |
| Waist circumference | 96.50±12.42 | 92.39±11.63 | 0.18* |
| Menarche age | 12.72±1.32 | 12.81±1.34 | 0.32* |
| Parity | 0.25*** | ||
| Nullipar | 6 (12.2%) | 10 (20.8%) | |
| Multipar | 43 (87.8%) | 38 (79.2%) | |
| Cesarean section | 0.15*** | ||
| Yes | 25 (54.2%) | 20 (39.6%) | |
| No | 22 (45.8%) | 29 (60.4%) | |
| Number of cesarean section | 0.60*** | ||
| 1 | 17 (68%) | 8 (40%) | |
| ≥2 | 8 (32%) | 12 (60%) | |
| Chief complaint | 0.68*** | ||
| Menorrhagia | 9 (18.4%) | 6 (12.5%) | |
| Menometrorrhagia | 29 (59.2%) | 29 (60.4%) | |
| Others | 11 (22.4%) | 13 (27.1%) | |
| History of infertility | 0.79*** | ||
| Yes | 6 (13%) | 7 (14.9%) | |
| No | 40 (87%) | 40 (85.1%) | |
| History of vaginitis | 0.22** | ||
| Yes | 41 (83.7%) | 35 (72.9%) | |
| No | 8 (16.3%) | 13 (27.1%) | |
| History of PID | 0.11** | ||
| Yes | 0 | 3 (6.3%) | |
| No | 49 (100%) | 45 (93.8%) | |
| History of IUD use | 0.71** | ||
| Yes | 3 (6.1%) | 4 (8.3%) | |
| No | 46 (93.9%) | 44 (91.7%) | |
| History of oral contraceptive use | 0.97*** | ||
| Yes | 24 (49%) | 23 (47.9%) | |
| No | 25 (51%) | 25 (52.1%) | |
| Histology | 0.06** | ||
| Hyperplasia | 2 (4.1%) | 0 | |
| Polyp | 24 (49.6%) | 33 (68.8%) | |
| Endometritis | 23 (46.3%) | 15 (31.2%) |
*Mann Whitney u test **Fischer exact test ***Chi-square test
In the hysteroscopy report of the control group, it was observed that 15 patients (31.2%) were normal and 33 patients (68.8%) had polyps and in the case group, and in the case group, 17 patients (34.4%) had normal findings, 16 (32.7%) had polyps and 16 (32.7%) had uterine fibroids. The frequency of demographic characteristics and obstetric variables among patients with uterine fibroids in the intramural and subserosal group and the submucosal group are shown in Table 2.
Table 2.
Frequency of demographic characteristics and obstetric variables between submucosal, intramural and subserosal fibroids
| Submucosal fibroid (17 patient) | Intramural and subserousal fibroids (32 patients) | P | |
|---|---|---|---|
| Age (years) | 44.00±4.62 | 43.50±5.90 | 0.79* |
| BMI | 29.65±4.12 | 30.45±5.02 | 0.36* |
| Waist circumference | 93.62±10.05 | 97.43±13.69 | 0.52* |
| Menarche age | 12.52±1.54 | 12.68±1.67 | 0.71* |
| Parity | 1.000** | ||
| Nullipar | 2 (11.8%) | 4 (12.5%) | |
| Multipar | 15 (88.2%) | 28 (87.5%) | |
| Caesarean section | 0.68*** | ||
| Yes | 8 (50%) | 18 (56.3%) | |
| No | 8 (50%) | 14 (43.8%) | |
| Number of caesarean section | 0.025** | ||
| 1 | 3 (37.2%) | 14 (82.6%) | |
| ≥2 | 5 (62.8%) | 3 (17.4%) | |
| Chief complaint | 1.000** | ||
| Menorrhagia | 3 (17.6%) | 6 (18.8%) | |
| Menometrorrhagia | 10 (58.8%) | 19 (59.4%) | |
| Others | 4 (23.5%) | 7 (21.9%) | |
| History of infertility | 0.39** | ||
| Yes | 1 (5.9%) | 5 (17.2%) | |
| No | 16 (94.1%) | 24 (82.8%) | |
| History of vaginitis | 0.69** | ||
| Yes | 15 (88.2%) | 26 (81.2%) | |
| No | 2 (11.8%) | 6 (18.8%) | |
| History of oral contraceptive use | 0.42*** | ||
| Yes | 7 (41.2%) | 17 (53.1%) | |
| No | 10 (58.8%) | 15 (46.9%) | |
| Histology | |||
| Hyperplasia | 0 | 2 (6.3%) | 0.0001** |
| Polyp | 6 (35.3%) | 18 (56.3%) | |
| Endometritis | 11 (64.7%) | 12 (37.3%) |
*Mann Whitney U test. **Fischer exact test. ***Chi-square test
By backward stepwise (wald) logistic regression and controlling the effect of age in both groups in the third step (final step), no significant effect was observed.
Discussion
In the present study, which aimed to evaluate the association between chronic endometritis with uterine fibroids in non-menopausal women, the overall incidence of chronic endometritis was 39% (38 out of 97) and it was observed that the incidence of chronic endometritis in patients with uterine fibroids was higher than the control group (46% vs. 31%, respectively), but no statistically significant difference was observed. Furthermore, the incidence of chronic endometritis in women with submucosal myoma was higher than the intramural and subserosal group (64% vs. 37%) and there was a significant difference between these two subgroups of fibroids (P = 0.0001). Whereas in the intramural and subserosal group, the presence of uterine polyps, and in the submucosal group, chronic endometritis was obvious in pathology. This finding was consistent with the Song study which examined chronic endometritis in patients with intramural and submucosal fibroids. Song reported the incidence of chronic endometritis in the 22 patients with submucosal myoma as 59.1%, which was statistically significant and different from the intramural and subserosal group. They noted that the overall prevalence of chronic endometritis was 24%.[20]
Despite the high prevalence of uterine fibroids and their impact on women’s health, its underlying pathogenesis is still unknown. Researchers have suggested that non-hormonal factors may be a risk factor for uterine fibroids.[11,13] Since inflammatory and infectious agents have a biological mechanism that can be controlled and modified, by confirming this hypothesis, a way can be found to prevent it.[14,15]
It has been stated that inflammatory conditions in both general and local endometrium can be effective in causing uterine fibroids with different mechanisms such as increased ECM protein, expression of cytokines, etc.[8–10] If the uterus had chronic inflammation by inflammatory factors such as injury, infection, menstruation inflammations, etc., it causes the imbalance of the immune system through increased T helper cytokines and decreased function of target cells (Tregs) and the inflammatory response of the immune system leads to fibrosis tissue formation and proliferation. Chronic inflammation increases estrogen and ultimately increases myoma growth.[28] A study in the Netherlands reported that serum levels of cytokine inflammatory factors like interleukin-1 alpha were higher in patients with uterine fibroids than in the control group.[29]
The relationship between chronic endometritis and reproductive outcomes such as recurrent miscarriage and recurrent implantation failure has been evaluated in previous studies, and some studies have been performed for use of antibiotic treatment. It has been found an improvement in chronic endometritis with reducing the number of plasma cells in endometrial biopsy specimens after antibiotic treatment.[22,23,24,25,26] However, there are limited studies about the relationship between chronic endometritis and uterine fibroids. To the best of our knowledge, no studies have been performed on treatment methods, but according to the evidence of other studies,[23,26] it seems that if the association of chronic endometritis in the development or recurrence of uterine fibroids be approved, antibiotic treatment may prevent the undesirable consequence of endometritis and invasive interventions.
Chronic endometritis is usually associated with AUB but most of the time it is asymptomatic or has mild symptoms. Therefore, its frequency is unknown in the general population. Adegboyega et al.,[30] mentioned 15.6% as the frequency of chronic endometritis stated that this frequency was much higher than previous studies (3-10%).[31]
In the present study, the same as Song et al.,[20] it was observed that the incidence of chronic endometritis in the submucosal group was higher than in the intramural group, but in the Miura study,[15] the inflammatory response and prostaglandin F2a level in the submucosal and intramural group were higher than in the subserosal and control groups.
In the study by Song et al.,[20] abortion, abnormal uterine bleeding, endometrial hyperplasia, and menstrual cycle phase were mentioned as risk factors for chronic endometritis, while in the present study, there was no difference between hyperplasia and abortion between case and control groups. The difference between these two studies may be due to differences in the characteristics of the study population. In the present study, the mean age in both groups with and without uterine fibroids was 43 to 44 years and the patients were mostly multiparous and without a history of infertility, and the most common reason for referral was AUB.
In the song study, the majority of the study population were nulliparous and infertile, and in the age range of 30 to 44 years. The majority of them had complaints of secondary infertility and a history of recurrent miscarriage.[20]
In the Miura study, it was reported that in women with intramural fibroids, even without deformity in the uterine cavity, there were fewer pregnancies and fetal replacements, which could be due to the influence of biological factors such as increased cumulative inflammatory cells between the fibroid and endometrial tissue.[15]
Despite age matching in the present study, the age of patients with uterine fibroids was higher than the control group and there was a statistically significant difference between groups in terms of mean age, which considers the increased chance of developing uterine myoma at older ages. Of course, this is one of the limitations of the present study.
In the present study, to evaluate the inflammation and infection of the uterus, in addition to the chronic endometritis in the uterine endometrial biopsy specimen, risk factors such as the history of PID, history of vaginitis, history of IUD use were also asked and there was no significant difference. Between groups while in the study by Faerstein et al.,[13] results showed an increased chance of developing uterine fibroids in women with a history of 3 periods of PID, chlamydia, or IUD use. Also, in the study of Saadatnia et al.,[32] it was observed that by PCR diagnostic method, two common uterine infections including cytomegalovirus and chlamydia trachomatis were significantly associated with an increase in the number and size of uterine myomas.
Since the history of PID and vaginitis has been recorded based on the patient’s statement, it may not be reliable due to recall bias and is another limitation of the present study and it is suggested that based on the location of fibroids, clinicians consider various paraclinical assessments for PID and sexually transmitted diseases in women with uterine fibroids. Also, regarding the insignificant relation regarding the history of IUD use in two groups, this result may be obtained as a result of the low number of using IUDs in this population.
Also in the present study, no difference was observed between case and control groups in terms of BMI, waist size, menarche age, history of OCP use, parity, history of cesarean section, and history of infertility. Researchers tried to control these confounding factors as much as possible between groups. The results of the present study showed that the history of cesarean section was twice or more in the submucosal myoma group than in patients with intramural and subserosal myomas. This difference between the two groups was significant in terms of the number of cesarean sections, which could confirm the occurrence of uterine injury and the increased chance of uterine myoma. While multiparity has a protective role in the development of uterine fibroids, the number of cesarean sections is a controversial issue. Of course, due to the small sample size, further studies are needed. Regarding the effect of hormonal and anti-inflammatory factors on uterine fibroids, future studies assessing these factors are recommended. According to the evidence of other studies,[23,26] it seems that if the association of chronic endometritis in the development or recurrence of uterine fibroids be approved, antibiotic treatment may prevent the undesirable consequence of endometritis and invasive interventions. Also we suggest further studies on antibiotic treatment of endometritis.
Key message
It is recommended that the gynecologists in patients with uterine fibroids pay attention to the medical history, physical examination, and other findings indicating intrauterine infection to prevent recurrence of the lesion with appropriate treatment if necessary.
Key points
Some studies reported the association between fibroids with uterine inflammation.
In the present study, the overall incidence of chronic endometritis was higher than previous studies and also the incidence was higher and more significant in women with submucosal myoma than in the intramural and subserosal group.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published.
Financial support and sponsorship
This study was financially supported by the Vice-Chancellorship of Research and Technology, Guilan University of Medical Science.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We appreciate all participants in the research, the support and cooperation of chief and staff of hospitals in Guilan province.
References
- 1.Giuliani E, As-Sanie S, Marsh EE. Epidemiology and management of uterine fibroids. Int J Gynecol Obstet. 2020;149:3–9. doi: 10.1002/ijgo.13102. [DOI] [PubMed] [Google Scholar]
- 2.Sparic R, Mirkovic L, Malvasi A, Tinelli A. Epidemiology of uterine myomas:A review. Int J Fertil Steril. 2016;9:424–35. doi: 10.22074/ijfs.2015.4599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee SJ, Hwang JY. Recent Advances in Uterine Myoma and Pregnancy. J Korean Soc Matern Child Heal. 2020;24:144–53. [Google Scholar]
- 4.Kesmodel US, Mogensen O, Humaidan P, Ravn P. Relationship between a uterine fibroid diagnosis and the risk of adverse obstetrical outcomes:A cohort study. BMJ Open. 2020;10:e032104. doi: 10.1136/bmjopen-2019-032104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen Y, Lin M, Guo P, Xiao J, Huang X, Xu L, et al. Uterine fibroids increase the risk of hypertensive disorders of pregnancy:A prospective cohort study. J Hypertens. 2021;39:1002–8. doi: 10.1097/HJH.0000000000002729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharami SH, Zahiri Z, Ghanaie M. Risk factors of uterine leiomyoma in women of reproductive ages. J Babol Univ Med Sci. 2009;11:54–61. [Google Scholar]
- 7.Gleason JL, Thoma ME, Zukerman Willinger N, Shenassa ED. Endometriosis and uterine fibroids and their associations with elevated C-reactive protein and leukocyte telomere length among a representative sample of US women:Data from the National Health and Nutrition Examination Survey, 1999–2002. J Womens Health (Larchmt) 2021 doi: 10.1089/jwh.2021.0044. doi:10.1089/jwh. 2021.0044. [DOI] [PubMed] [Google Scholar]
- 8.Armanini D, Sabbadin C, Donà G, Bordin L, Marin L, Andrisani A, et al. Uterine fibroids and risk of hypertension:Implication of inflammation and a possible role of the renin-angiotensin-aldosterone system. J Clin Hypertens. 2018;20:727–9. doi: 10.1111/jch.13262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Orciani M, Caffarini M, Biagini A, Lucarini G, Delli Carpini G, Berretta A, et al. Chronic inflammation may enhance leiomyoma development by the involvement of progenitor cells. Stem Cells Int. 2018;2018:1716246. doi: 10.1155/2018/1716246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Protic O, Toti P, Islam MS, Occhini R, Giannubilo SR, Catherino WH, et al. Possible involvement of inflammatory/reparative processes in the development of uterine fibroids. Cell Tissue Res. 2016;364:415–27. doi: 10.1007/s00441-015-2324-3. [DOI] [PubMed] [Google Scholar]
- 11.Cetin E, Al-Hendy A, Ciebiera M. Non-hormonal mediators of uterine fibroid growth. Curr Opin Obstet Gynecol. 2020;32:361–70. doi: 10.1097/GCO.0000000000000650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ciebiera M, Włodarczyk M, Zgliczyńska M, Łukaszuk K, Męczekalski B, Kobierzycki C, et al. The role of tumor necrosis factor a in the biology of uterine fibroids and the related symptoms. Int J Mol Sci. 2018;19:3869. doi: 10.3390/ijms19123869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Faerstein E, Szklo M, Rosenshein NB. Risk factors for uterine leiomyoma:A practice-based case-control study. II. Atherogenic risk factors and potential sources of uterine irritation. Am J Epidemiol. 2001;153:11–9. doi: 10.1093/aje/153.1.11. [DOI] [PubMed] [Google Scholar]
- 14.Zannotti A, Greco S, Pellegrino P, Giantomassi F, Delli Carpini G, Goteri G, et al. Macrophages and immune responses in uterine fibroids. Cells. 2021;10:982. doi: 10.3390/cells10050982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miura S, Khan KN, Kitajima M, Hiraki K, Moriyama S, Masuzaki H, et al. Differential infiltration of macrophages and prostaglandin production by different uterine leiomyomas. Hum Reprod. 2006;21:2545–54. doi: 10.1093/humrep/del205. [DOI] [PubMed] [Google Scholar]
- 16.Puente E, Alonso L, Laganà AS, Ghezzi F, Casarin J, Carugno J. Chronic endometritis:Old problem, novel insights and future challenges. Int J Fertil Steril. 2020;13:250–6. doi: 10.22074/ijfs.2020.5779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Greenwood SM, Moran JJ. Chronic endometritis:Morphologic and clinical observations. Obstet Gynecol. 1981;58:176–84. [PubMed] [Google Scholar]
- 18.Crum CP, Egawa K, Fenoglio CM, Richart RM. Chronic endometritis:The role of immunohistochemistry in the detection of plasma cells. Am J Obstet Gynecol. 1983;147:812–5. doi: 10.1016/0002-9378(83)90045-5. [DOI] [PubMed] [Google Scholar]
- 19.McQueen DB, Maniar KP, Hutchinson A, Confino R, Bernardi L, Pavone ME. Redefining chronic endometritis:The importance of endometrial stromal changes. Fertil Steril. 2021;116:855–61. doi: 10.1016/j.fertnstert.2021.04.036. [DOI] [PubMed] [Google Scholar]
- 20.Song D, Feng X, Zhang Q, Xia E, Xiao Y, Xie W, et al. Prevalence and confounders of chronic endometritis in premenopausal women with abnormal bleeding or reproductive failure. Reprod Biomed Online. 2018;36:78–83. doi: 10.1016/j.rbmo.2017.09.008. [DOI] [PubMed] [Google Scholar]
- 21.Sharami S, Fakor F, Sani MK, Omidi S, Jahromi SK, Ghalandari M, et al. The characteristics of Uterine Leiomyoma and metabolic syndrome in the multiparous overweight women in northern Iran. Pakistan J Med Heal Sci. 2020;14:1137–42. [Google Scholar]
- 22.Cicinelli E, Matteo M, Tinelli R, Lepera A, Alfonso R, Indraccolo U, et al. Prevalence of chronic endometritis in repeated unexplained implantation failure and the IVF success rate after antibiotic therapy. Hum Reprod. 2015;30:323–30. doi: 10.1093/humrep/deu292. [DOI] [PubMed] [Google Scholar]
- 23.Cicinelli E, Resta L, Loizzi V, Pinto V, Santarsiero C, Cicinelli R, et al. Antibiotic therapy versus no treatment for chronic endometritis:A case-control study. Fertil Steril. 2021;115:1541–8. doi: 10.1016/j.fertnstert.2021.01.018. [DOI] [PubMed] [Google Scholar]
- 24.Kitaya K, Matsubayashi H, Takaya Y, Nishiyama R, Yamaguchi K, Takeuchi T, et al. Live birth rate following oral antibiotic treatment for chronic endometritis in infertile women with repeated implantation failure. Am J Reprod Immunol. 2017;78:e12719. doi: 10.1111/aji.12719. [DOI] [PubMed] [Google Scholar]
- 25.McQueen DB, Bernardi LA, Stephenson MD. Chronic endometritis in women with recurrent early pregnancy loss and/or fetal demise. Fertil Steril. 2014;101:1026–30. doi: 10.1016/j.fertnstert.2013.12.031. [DOI] [PubMed] [Google Scholar]
- 26.Song D, He Y, Wang Y, Liu Z, Xia E, Huang X, et al. Impact of antibiotic therapy on the rate of negative test results for chronic endometritis:A prospective randomized control trial. Fertil Steril. 2021;115:1549–56. doi: 10.1016/j.fertnstert.2020.12.019. [DOI] [PubMed] [Google Scholar]
- 27.Kannar V, Lingaiah HKM, Sunita V. Evaluation of endometrium for chronic endometritis by using syndecan-1 in abnormal uterine bleeding. J Lab Physicians. 2012;4:69–73. doi: 10.4103/0974-2727.105584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Modugno F, Ness RB, Chen C, Weiss NS. Inflammation and endometrial cancer:A hypothesis. Cancer Epidemiol Prev Biomarkers. 2005;14:2840–7. doi: 10.1158/1055-9965.EPI-05-0493. [DOI] [PubMed] [Google Scholar]
- 29.Sikorski R, Kapeć E, Zaleska W. Serum levels of proinflammatory cytokines in women with uterine myomas. Ginekol Pol. 2001;72:1485–8. [PubMed] [Google Scholar]
- 30.Adegboyega PA, Pei Y, McLarty J. Relationship between eosinophils and chronic endometritis. Hum Pathol. 2010;41:33–7. doi: 10.1016/j.humpath.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 31.Bayer-Garner IB, Nickell JA, Korourian S. Routine syndecan-1 immunohistochemistry aids in the diagnosis of chronic endometritis. Arch Pathol Lab Med. 2004;128:1000–3. doi: 10.5858/2004-128-1000-RSIAIT. [DOI] [PubMed] [Google Scholar]
- 32.Saadatnia G, Saremi S, Salehian B, Salehian P. Uterine leiomyoma and reproductive tract infections detected by polymerase chain reaction. Iran J Pathol. 2019;14:33–40. doi: 10.30699/IJP.14.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]


