Abstract
This paper estimates the extent to which childhood circumstances contribute to health inequality in old age and evaluates the importance of major domains of childhood circumstances to health inequalities in the USA and China. We link two waves of the China Health and Retirement Longitudinal Study in 2013 and 2015 with the newly released 2014 Life History Survey, and two waves of the Health and Retirement Study in 2014 and 2016 with the newly released 2015 Life History Mail Survey in the USA, to quantify health inequality due to childhood circumstances for which they have little control. Using the Shapley value decomposition approach, we show that childhood circumstances may explain 7–16 and 14–30% of health inequality in old age in China and the USA, respectively. Specifically, the contribution of childhood circumstances to health inequality is larger in the USA than in China for self-rated health, mental health, and physical health. Examining domains of childhood circumstance, regional and rural/urban status contribute more to health inequality in China, while family socioeconomic status contributes more to health inequality in the USA. Our findings support the value of a life course approach in identifying the key determinants of health in old age. Distinguishing sources of health inequality and rectifying inequality due to early childhood circumstances should be the basis of policy promoting health equity.
Keywords: Life course approach, Inequality of opportunity, Self-rated health, Mental health, Frailty, Childhood circumstances
1. Introduction
One of the most significant advances in the measurement of inequality of human well-being has been the transition from a single-dimensioned focus to multiple key dimensions. Meanwhile, the economics literature often focuses on the trend of money metric inequality, such as inequalities of income, wealth, or consumption expenditures; less attention has been paid to how health inequality has evolved. As economic inequality worsens globally (Milanovic 2014), it is also important to understand how economic circumstances may shape health inequality, especially in the long term (Tang et al. 2008).
Population aging has been global and accelerating.1 Health condition of the elderly not only determines their own welfare, but affects health care spending for the whole society. As cumulative evidence suggests that aging begins in early stage of life during which individual circumstances play important roles (Zeng et al. 2007; Zhang et al. 2008; Mazumder et al. 2010; Stowasser et al. 2014; Sayer and Gill 2016; Ko and Yeung 2019; Liu et al. 2019), it is important to understand the lasting impact of early life circumstances on old-age health. Effective interventions can be most successful if applied early in the life course,2 prior to the onset of disease and disability, to slow the diverging aging process and benefit population health (Moffitt et al. 2017).
Meanwhile, existing studies on sources of health inequality focus on childhood circumstances as they are largely beyond the realm of individuals’ choices. An important principle emphasized in the framework of health inequality due to childhood circumstances (i.e. Inequality of Opportunity in health,3 a.k.a. IOP in health) is that childhood circumstances are often sources of health inequality that deserve prioritized policy interventions (Roemer and Trannoy 2016; Andreoli et al. 2019). Policies should be implemented to eliminate or compensate for health inequality resulting from childhood circumstances (Rosa-Dias and Jones 2007; Lefranc et al. 2008; Fleurbaey and Schokkaert 2009; Trannoy et al. 2010), rather than addressing health inequality originated from individual efforts (Marmot et al. 2008). Misallocations of resources from addressing gaps in childhood circumstances to gaps in efforts may distort health behaviors and lifestyle choices with large social costs.
Individuals are heterogeneous in their childhood circumstances and therefore trajectories of aging, which directly influence susceptibility to morbidity and mortality events (Almond et al. 2018). A growing body of economics and epidemiology studies conclude that a series of childhood circumstances may affect later life, such as rural/urban status (Strauss et al. 2018), family socioeconomic status (SES) (Dahl and Birkelund 1997; Moody-Ayers et al. 2007; Zhang et al. 2008; Katikireddi 2016; Gale et al. 2016; Adhvaryu et al. 2019), nutritional condition (Palloni et al. 2005; McEniry et al. 2008; Almond and Mazumder 2011), health conditions (Sayer et al. 2004; Kuh et al. 2006; Dodds et al. 2012; Venkataramani 2012), natural environments (Isen et al. 2017), parenting skills (Andersson and Stevens 1993; Krause 1998), parental educational attainment (Ramos 2007; Carrieri and Jones 2018; Leopold 2018), parental health behavior (Simon 2016; Nilsson 2017), service capacity in the community (Shen 2014), social mobility (Venkataramani et al. 2016), and maternal bereavement (Black et al. 2016; Persson and Rossin-Slater 2018). As a complement to this strand of literature on each circumstance contributing to health inequality, we assemble a comprehensive set of circumstances to understand how various childhood circumstances may coalesce and in turn domains of such circumstances manifest as health inequality.
While it is difficult to define the exact set of childhood circumstances that may contribute to health inequality, especially for multi-country comparisons, we follow the growing literature of IOP in health and income (see an excellent review by Hufe et al. 2017) to classify comprehensive childhood circumstances into seven domains. Specifically, childhood circumstances include major crisis, regional and urban/rural status, family SES, parental health status and health behaviors, health and nutritional status, relationship with parents, and friendship. Though all these domains influence health and aging to some extent, their relative contributions to aging and disease risk are uncertain. The multitude of factors defining an individual’s specific circumstances poses challenges for modeling their individual and cumulative effects.
Based on a wide range of comparable childhood circumstances and comprehensive health dimensions assembled from two nationally representative samples of older adults in the USA and China, our objective of this study is to quantify the overall contribution of childhood circumstances to health inequality in old age as well as the role played by domain of childhood circumstances in each health dimension. People normally have little control over childhood circumstances, which therefore should be the priority of public policies that aim to alleviate health inequality. We provide the first comparative evidence on IOP in health between the USA and China. While there are differences in childhood circumstances within a country, relatively small within-country heterogeneity calls for cross-country comparisons of the role of childhood circumstances, which may offer further insights into circumstances that vary more across countries.
In this regard, a comparative study between two large countries—China and the USA—can be representative of the range of vastly different economic development, health systems, institutions, lifestyles, culture and norms, etc. Their largest aging populations and economies in the world may have important global implications. Both countries have experienced high and fast rising social inequality. Specifcially, the USA has one of the highest economic inequality in the developed countries (Bratberg et al. 2017; Chetty et al. 2017; Hufe et al. 2017; landerso and Heckman 2017), while China has experienced fast increase in economic inequality, not only surpassing that of the USA by a large margin but ranking among the highest in the world (Yang 1999; Yang and Eriksson 2010; Xie and Zhou 2014). Both countries have also been aging fast. Specifically, the number of older persons aged 60 years or over has increased substantially, from 45.8 million (or 16.2% of the population) in 2000 to 66.5 billion (or 20.7% of the population) in 2015 in the USA, and from 125.2 million (or 9.9% of the population) in 2000 to 209.2 million (or 15.2% of the population) in 2015 in China. This growth is projected to accelerate in the coming decades, to reach almost 92.9 million (or 26.1% of the population) by 2030 and nearly 108.3 billion (or 27.9% of the population) by 2050 in the USA, and to reach almost 358.1 million (or 25.3% of the population) by 2030 and nearly 491.5 billion (or 36.5% of the population) by 2050 in China (United Nations 2015).
We may contribute to the literature in three main aspects. First, we advance the literature on life course epidemiology that has mostly been limited to shorter time periods, such as a decade in Simmonds et al. (2015); in contrast, our study links individuals’ health status at least 50 years since childhood. Second, we use a very comprehensive set of childhood circumstances and rich health measures. The rich childhood circumstances address the concern that insufficient information on circumstances may undervalue IOP and therefore mislead policymakers into a false sense of complacency that health inequality is largely fair (Kanbur and Wagstaff 2016). Third, we advance the literature that has often lacked comparability across studies and country contexts due to the use of different sets of childhood circumstances. In addition to the baseline results that make use of similar and one of the most comprehensive domains of childhood circumstances as in Hufe et al. (2017), we restrict the analysis to a subset of circumstances that we have information for both the USA and China to ensure closest comparisons between the two.
Our study of IOP in health is attributable to childhood circumstances at least five decades ago. While rising economic inequality in recent decades may enlarge gaps in health from mid-life to old age, it does not directly affect the age cohorts under this study via influencing their childhood circumstances. However, the perceptions of rising economic inequality may spark more concern about the rising IOP (McCall et al. 2017). Countries with greater economic inequality also tend to be countries with IOP, i.e. a greater fraction of economic advantage and disadvantage being passed on between parents and their children (Lefranc et al. 2008; Corak 2013). Further studies should keep monitoring IOP for younger age cohorts due to greater economic inequality affecting their childhood.
Reducing IOP in health has the potential to be a policy objective. Policymakers can be more averse to, or less tolerant of, IOP in health than economic inequality. This is not only because IOP in health is beyond the realm of individuals’ control and therefore is unethical, but because health has both intrinsic value (that directly affects individual well-being) and instrumental value. Economic inequality, on the other hand, has only instrumental value.
The remainder of the paper is organized as follows. Section 2 introduces our conceptual framework and empirical strategy. Section 3 describes the data and measurements. Section 4 presents findings and robustness tests. Section 5 discusses and concludes.
2. Conceptual Framework and Methodology
2.1. Conceptual Framework
While classical welfarism assumed that social welfare should be predicted only on the levels and equality of individuals’ outcomes, critics argue that it is ethically inappropriate to measure solely based on equality of outcomes. Rawls (1958, 1971) incorporated personal responsibility into discussions on the kind of equality that was ethically desirable. Since then, Sen (1980), Dworkin (1981a, b), Arneson (1989), and Cohen (1989), among others, have contributed to the development of egalitarian theory that attempted to replace equality of outcomes with equality of opportunities (Roemer and Trannoy 2016). Roemer (1993, 1998) designed an algorithm to evaluate policies that would equalize opportunities to achieve a given outcome.
On the other hand, inequality of opportunity in health (IOP in health) means health inequality attributable to circumstances, which are often beyond one’s own control, based on the framework of Roemer (2002). Childhood circumstances are main factors beyond individual control, since individuals cannot be held responsible for their birth lottery. In contrast, health inequality owing to factors that are freely chosen by individuals, namely their efforts, is not considered IOP in health.
There are two approaches to conceptualize inequality of opportunity: First, the ex ante approach focuses on the injustice of “unequal rewards to unequal circumstances” and calls for equalizing opportunity sets; Second, the ex post approach emphasizes the injustice of “unequal rewards to equal efforts” and calls for compensating outcomes (Roemer and Trannoy 2016). This study adopts the ex ante approach as our HRS-sister surveys provide us very rich information on childhood circumstances to measure share of unequal health rewards in later life associated with unequal childhood circumstances.
2.2. Methodology
Our main outcome of interest are health measures in old age y. To understand the extent to which childhood circumstances contribute to health inequality in old age, we measure the overall health inequality and the part of health inequality due to childhood circumstances using mean logarithmic deviation (MLD). MLD has been popular in measuring inequality of well-being in multiple dimensions (Haughton and Khandker 2009; Ferreira and Gignoux 2011, 2013; Hufe et al. 2017; Björklund et al. 2012).
Using MLD, health inequality is defined as the mean deviation of ln yi from ln . In other words, it measures the average difference between ln and ln yi.
where N is the number of individuals, yi is health status of individual i. is the mean of yi. is the mean of ln yi.
The MLD derives from the generalized entropy, a well-accepted family of inequality measures. The MLD form has several good features. Among the most relevant to us: (1) it considers aversion to higher health inequality. Given the average health outcome , more unequal health status corresponds to a higher MLD4; (2) it enables us to mitigate the possible overinfluence of outlier values.
The next step is to disentangle health inequality due to childhood circumstances from the overall inequality. Adopting the parametric Shapley Value Decomposition approach (The Shapley approach hereafter), suppose we have partitioned the population into types of individuals, each type corresponds to the set of individuals with the same value of childhood circumstances. Each type is characterized by its own health distribution. Let the type distributions be {Ft(y), tϵT} where T is the set of types, and let type t have frequency ft in the population and mean health outcome μt, summarized by the vectors f = f1, … , fT and .μ = μ1, … , μT. We can construct a hypothetical distribution, denoted by Ф(μ,f), in which all members of each type t have the mean health outcome μt of that type.5 If Ф(μ,f) were the true health distribution, then all health inequality is due to childhood circumstances and none to efforts. The MLD of health distribution F, i.e. MLD(F), is decomposable as follows:
| (1) |
MLD can be fully decomposed into inequality due to childhood circumstances MLD(Ф) and efforts (Shorrocks 1980, 2013; Jusot et al. 2013; Wendelspiess 2014). Therefore, the ratio r measures the extent to which health inequality is due to childhood circumstances.
2.3. Empirical Strategy
Our conceptual model partitions the population into types according to the value of their childhood circumstances and takes as data the type distributions and the aggregate distribution of the outcome of interest. This non-parametric Shapley approach requires either a very large data set, or a small set of types, to ensure meaningful distribution of health outcomes by type. However, a richer set of childhood circumstances in our study requires us to replace the partition of the population into a typology by regression analysis. Our regression-based Shapley approach enables us to estimate the impact of numerous childhood circumstances even in the presence of small sample and cell sizes. Following procedures in Ferreira and Gignoux (2011), Niehues and Peichl (2014), and Roemer and Trannoy (2016), we specify the empirical model
| (2) |
where C is a vector of circumstances (excluding age and gender) beyond the control of the individual, Y is a vector of health outcomes in old age, and i represents individual i. The reduced form parameter can be estimated by OLS to derive the fraction of variance in Y that is explained by childhood circumstances Ci.
Based on this estimation, we construct a parametric estimate of the smoothed distribution Ф defined earlier by replacing Y with their predictions:
| (3) |
Let Ф be the distribution of estimated Y. In this counterfactual, all individuals with the same childhood circumstances have the same Y. Thus, IOP, denoted by r can be rewritten as:
Similarly, we estimate the relative importance of domains of childhood circumstances. “Appendix 2” describes the process.
We present point estimates and bootstrap standard errors with 50 replications. To obtain population-based estimates, we incorporated survey weights in this analysis. Because variations in health may not be all accounted for due to unobserved circumstances (Tomasetti et al. 2017), which may bias the estimated total contribution to IOP in health, we interpret these estimates as measuring relative importance of circumstances. As we will show in sensitivity analyses, the relative importance of these domains of childhood circumstances are insensitive to a subset of more comparable circumstances between China and the USA.
There are substantial advantages to our methods compared with other decomposition methods, such as being order independent, meaning that the order of circumstances for decomposition does not affect the results, and being able to add up components to the total value. Though the decomposition should not be seen as causal, it offers an idea of the relative importance of circumstances (Ferreira and Gignoux 2013). The parametric Shapley approach has a built-in toolkit in popular statistical packages, such as STATA and R, which helps to standardize the analysis.
3. Data
3.1. HRS-Sister Studies
The databases we used are Health and Retirement Study (HRS) for the USA and China Health and Retirement Longitudinal Study (CHARLS) for China.
We match the 2013, 2015 waves of the CHARLS, a HRS-sister survey, to its 2014 Life History Survey (LHS). The merged dataset enables us to link rich information on individuals’ health status in old age with early childhood circumstances in a representative sample of older adults in China. The CHARLS national baseline survey in 2011 represented people aged 45 years or older with their spouses totaling 17,708 individuals (living in 10,287 households, 450 villages/urban communities, 150 county-level units in 28 of China’s 34 provinces).6 The 2013 follow-up survey successfully tracked 15,770 individuals from the baseline survey, while 431 individuals died in between the two surveys. The 2013 wave also added 2834 new respondents into the survey, reaching 18,604 individuals. The 2014 LHS recruited living respondents from both the 2011 baseline survey and the 2013 follow-up survey (Hong et al. 2017). The third wave of CHARLS was administered from mid-2015 to early 2016 and covered 12,450 households with 21,057 respondents (Strauss et al. 2018). Our analytic sample includes over 8000 elderly Chinese above age 60.
The HRS is a nationally representative, biennial survey of older Americans (aged above 51) beginning in 1992.7 HRS is funded by the National Institute on Aging and carried out by the University of Michigan. In this study, we assembled a large array of variables from two main data sources, including the core survey with two waves in 2014 and 2016, the newly released 2015 Life History Mail Survey (LHMS). The 2015 LHMS was conducted from December 2015 to August 2016 in a subsample of HRS participants (n = 11,256) though mails. It aimed to collect information on residential history, education history, and other important childhood and family events. The target subsample included all living HRS participants who completed their most recent HRS core survey interview in English (rather than Spanish). Finally, 6481 participants were enrolled in the LHMS with a response rate of 58%. We assembled health outcomes and some childhood circumstances from HRS core surveys, and most childhood circumstances from the 2015 LHMS. Our analytic sample includes around 3000 US persons aged 60 or over.
3.2. Measures
Health outcomes are presented in Table 1. Three dimensions of health status were assessed, including frailty, self-rated health, and mental health. They were chosen for two main reasons: First, they represent three key aspects of health ranging from more subjective measures to more objective measures, including general health, physical health and mental health. Specifically, self-rated health is reliable in assessing overall health (Lundberg and Manderbacka 1996), and has been commonly used in a wide range of disciplines (Bombak 2013). Frailty is considered highly prevalent in old age and indicates high risk of falls, disability, hospitalization, and mortality (Fried et al. 2001). CES-D scale offers a useful measure of mental illness (Radloff 1977). Depressive symptoms among older adults are associated with an increased risk of cardiac diseases and death from illnesses. Second, these indicators are widely available in social surveys, including in HRS and CHARLS, and they can be more comparable across countries. The longitudinal feature of our data mitigates measurement errors by averaging health status between two consecutive waves of survey (2014 and 2016 for HRS; 2013 and 2015 for CHARLS) before merging at the individual level with the corresponding life history surveys (HRS 2015 and CHARLS 2014).
Table 1.
Summary statistics of health outcomes (US vs. China, age 60 +)
| Variable | Country | Obs | Mean | SD | Min | Max | Variable description | CV |
|---|---|---|---|---|---|---|---|---|
| Self-rated health | US | 3014 | 2.788 | 0.924 | 1 | 5 | The average value of self-rated health between 2014 and 2016 (Would you say your health is excellent, very good, good, fair, or poor? 1. excellent, 2. very good, 3. good, 4. fair, 5. poor) | 0.33 |
| CHN | 8255 | 3.924 | 0.792 | 1 | 5 | The average value of self-rated health between 2013 and 2015 (Would you say your health is excellent, very good, good, fair, or poor? 1. excellent, 2. very good, 3. good, 4. fair, 5. poor) | 0.20 | |
| Mental health (CES-D score) | US | 3014 | 1.205 | 1.588 | 0 | 8 | The average value of mental2014 and mental2016; The Center for Epidemiological Studies Depression Scale (CES-D) 8-item version; each item score is 0 and 1, the total mental health score is from 0 to 8 | 1.32 |
| CHN | 7667 | 8.470 | 5.814 | 0 | 30 | The average value of mental2013 and mental2015; The Center for Epidemiological Studies Depression Scale (CES-D) 10-item version; each item scores from 0 to 3; the total mental health score is from 0 to 30 | 0.69 | |
| Mental health (depressive symptoms) | US | 3014 | 0.153 | 0.360 | 0 | 1 | The cutoff value for 8-item CES-D is 3 (1: yes; 0: no) | 2.353 |
| CHN | 7667 | 0.342 | 0.474 | 0 | 1 | The cutoff value for 10-item CES-D is 10 (1: yes; 0: no) | 1.386 | |
| Frailty | US | 2266 | 1.030 | 1.000 | 0 | 5 | The sum of low walking speed, low grip strength, exhaustion, low physical activity, and weight loss; age 65 + | 0.97 |
| CHN | 4647 | 2.088 | 1.009 | 0 | 5 | The sum of low walking speed, low grip strength, exhaustion, low physical activity, and weight loss; age 65 + | 0.50 |
We measure self-rated health with the same question in HRS and CHARLS, i.e. “Would you say your health is excellent, very good, good, fair, or poor?”. The five options are excellent, very good, good, fair, and poor. Unlike more objective measures, self-rated health can be subject to various biases in different contexts. Hence, special caution should be exercised in interpreting these results. It is, however, reassuring that the overall health and its distribution between China and the USA are consistent, whether subjective or objective measures of health are used.
Frailty score assesses vulnerability to an array of adverse outcomes. We follow Fried et al. (2001) to evaluate five components of frailty in both countries, i.e. weight loss, exhaustion, low physical activity, low grip strength, and low walking speed. Since only people over age 65 are eligible to test walking speed in HRS, we measure frailty among those over age 65. Only half of the survey subjects tested frailty in each wave of the HRS. Therefore, we use data from consecutive waves 2010 and 2012 to generate a frailty score for the full sample and consecutive waves 2014 and 2016 to generate another such frailty score. The average value between the two scores is our measure of physical frailty.
Mental health is measured using an 8-item Center for Epidemiological Studies Depression Scale (CES-D) (Radloff 1977) in the HRS, and a 10-item CES-D in the CHARLS. While of different scales, both these shorter forms of CES-D are comparable with the 20-item full version of CES-D (Kohout et al. 1993). Meanwhile, we derive another measure of mental health—depressive symptoms—using well-recognized cut-offs for shorter versions of CES-D.8
Table 1 compares health outcomes between the USA and China. Overall, the US respondents are in better health than their Chinese counterparts as measured by all three dimensions of health outcomes. The average self-rated health for older persons in the USA is between very good and good, while it is only fair for older persons in China. To compare the subjective measure more carefully, we plot the distributions of self-rated health between the USA and China in Fig. 5 in “Appendix 1”. The distributions of self-rated health are very robust—they changed very little for both the USA and China across two waves. The proportions of participants in excellent health, very good health or good health are all higher in the USA than in China, while the proportions of participants in fair or poor health were all lower in the USA than in China. Therefore, the US respondents demonstrate better self-rated health than their Chinese counterparts. This pattern is consistent with the objective health measures. The average value of frailty index is 1.030 in the USA and 2.088 in China, suggesting much worse physical functioning among the Chinese. The rates of depressive symptoms are 15.3% in the USA and 34.2% in China, again suggesting better mental health status among Americans.
While American older adults fared better than their Chinese counterparts on the three health measures, they also demonstrate larger variations as measured by Coefficient of Variance (CV). In Table 1, CVs of all four health outcomes in China are only half of those in the USA, meaning that the US elderly have more dispersed health distributions in all these health dimensions.
Measures of childhood circumstances are presented in Table 2. They are categorized into seven domains: (1) war or economic crisis at birth; (2) regional and urban/rural status at birth9; (3) family SES in childhood; (4) parental health status and health behaviors in childhood; (5) health and nutritional status in childhood; (6) relationship with parents in childhood; (7) friendship in childhood. Overall, domains 4 and 5 are directly health-related, while others are only indirectly health-related. We also highlight in Table 2 the more comparable circumstances between the USA and China, which will be used in a sensitivity analysis.10 While this subset of circumstances are generally more comparable, some domains and individual circumstance variables are more comparable than others. Some of these circumstances may still measure different things due to gaps in, for example, culture and norms between the two countries.
Table 2.
Summary statistics of early life circumstances (the USA vs. China, age 60 +) (the most comparable subset of circumstances between the two countries are bold and italicized)
| Domain | Country | Obs | Mean | SD | Min | Max | Variable description |
|---|---|---|---|---|---|---|---|
| War or economic crisis | US (2) | 3015 | 0.099 | 0.298 | 0 | 1 | Born in the Great Recession (1929–1933) (1: yes; 0: no) |
| 3015 | 0.174 | 0.379 | 0 | 1 | Born in the World War II (1941–1945) (1: yes; 0: no) | ||
| CHN (2) | 8585 | 0.313 | 0.464 | 0 | 1 | Born in the Anti-Japan War (1937–1945) (1: yes; 0: no) | |
| 8585 | 0.241 | 0.428 | 0 | 1 | Born in the Civil War (1946–1949) (1: yes; 0: no) | ||
| Regional and urban/rural status | US (11) | 3014 | 0.051 | 0.220 | 0 | 1 | Northeast region: new England division (me, nh, vt, ma, ri, ct) (1: yes; 0: no) |
| 3014 | 0.147 | 0.354 | 0 | 1 | Northeast region: middle Atlantic division (ny, nj, pa) (1: yes; 0: no) | ||
| 3014 | 0.199 | 0.399 | 0 | 1 | Midwest region: east north central division (oh, in, il, mi, wi) (1: yes; 0: no) | ||
| 3014 | 0.115 | 0.319 | 0 | 1 | Midwest region: west north central division (mn, ia, mo, nd, sd, ne, ks) (1: yes; 0: no) | ||
| 3014 | 0.154 | 0.361 | 0 | 1 | South region: south Atlantic division (de, md, dc, va, wv, nc, sc, ga,fl) (1: yes; 0: no) | ||
| 3014 | 0.082 | 0.274 | 0 | 1 | South region: east south central division (ky, tn, al, ms) (1: yes; 0: no) | ||
| 3014 | 0.091 | 0.287 | 0 | 1 | South region: west south central division (ar, la, ok, tx) (1: yes; 0: no) | ||
| 3014 | 0.032 | 0.175 | 0 | 1 | West region: mountain division (mt, id, wy, co, nm, az, ut, nv) (1: yes; 0: no) | ||
| 3014 | 0.063 | 0.244 | 0 | 1 | West region: pacific division (wa, or, ca, ak, hi) (1: yes; 0: no) | ||
| 3014 | 0.008 | 0.091 | 0 | 1 | US, na division (in the US, but with no info on the census division) (1: yes; 0: no) | ||
| 3014 | 0.058 | 0.234 | 0 | 1 | Foreign country: not in a census division (includes U.S territories) (1: yes; 0: no) | ||
| CHN (7) | 8481 | 0.099 | 0.299 | 0 | 1 | Rural or urban status at birth (0: rural; 1: urban) | |
| 83,555 | 0.106 | 0.308 | 0 | 1 | Northern China (1: yes; 0: no) | ||
| 8355 | 0.074 | 0.262 | 0 | 1 | Northeastern China (1: yes; 0: no) | ||
| 8355 | 0.328 | 0.469 | 0 | 1 | Eastern China (1: yes; 0: no) | ||
| 8355 | 0.241 | 0.427 | 0 | 1 | South Central China (1: yes; 0: no) | ||
| 8355 | 0.181 | 0.385 | 0 | 1 | Southwestern China (1: yes; 0: no) | ||
| 8355 | 0.070 | 0.255 | 0 | 1 | Northwestern China (1: yes; 0: no) | ||
| Family socioeconomic status | US (20) | 2642 | 0.020 | 0.140 | 0 | 1 | Father: no schooling (1: yes; 0: no) |
| 2642 | 0.062 | 0.242 | 0 | 1 | Father: educated without completing primary school (1: yes; 0: no) | ||
| 2642 | 0.136 | 0.342 | 0 | 1 | Father: Graduated from primary school (1: yes; 0: no) | ||
| 2642 | 0.300 | 0.458 | 0 | 1 | Father: Graduated from junior high school (1: yes; 0: no) | ||
| 2642 | 0.325 | 0.468 | 0 | 1 | Father: Graduated from senior high school (1: yes; 0: no) | ||
| 2642 | 0.157 | 0.364 | 0 | 1 | Father: Graduated from college or above (1: yes; 0: no) | ||
| 2808 | 0.018 | 0.134 | 0 | 1 | Mother: no schooling (1: yes; 0: no) | ||
| 2808 | 0.035 | 0.183 | 0 | 1 | Mother: educated without completing primary school (1: yes; 0: no) | ||
| 2808 | 0.108 | 0.311 | 0 | 1 | Mother: Graduated from primary school (1: yes; 0: no) | ||
| 2808 | 0.271 | 0.445 | 0 | 1 | Mother: Graduated from junior high school (1: yes; 0: no) | ||
| 2808 | 0.430 | 0.495 | 0 | 1 | Mother: Graduated from senior high school (1: yes; 0: no) | ||
| 2808 | 0.138 | 0.345 | 0 | 1 | Mother: Graduated from college or above (1: yes; 0: no) | ||
| 2966 | 0.147 | 0.355 | 0 | 1 | Family received financial help (1: yes; 0: no) | ||
| 3015 | 0.195 | 0.397 | 0 | 1 | Before age 16, father had no job for several months or longer | ||
| 3015 | 0.007 | 0.083 | 0 | 1 | Dummy for father never worked/always disabled | ||
| 3015 | 0.077 | 0.266 | 0 | 1 | Dummy for never lived with father/father was not alive in childhood | ||
| 2954 | 0.875 | 0.330 | 0 | 1 | Type of residence at birth (1: single-family house;0: apartment/townhouse/condo/mobile home) | ||
| 2965 | 2.153 | 1.132 | 1 | 5 | When you were age 10, approximately how many books were in the place you lived? | ||
| 3001 | 0.940 | 0.238 | 0 | 1 | Was English the language that you usually spoke at home before you were age 18? | ||
| 2903 | 0.131 | 0.337 | 0 | 1 | Did you attend any organized pre-school program (1: yes; 0: no) | ||
| CHN (15) | 8585 | 0.069 | 0.24 | 0 | 1 | Parents’ political status (1: either father or mother is party member; 0: none of them are) | |
| 7795 | 0.654 | 0.476 | 0 | 1 | Father: no schooling (1: yes; 0: no) | ||
| 7795 | 0.212 | 0.409 | 0 | 1 | Father: educated without completing primary school (1: yes; 0: no) | ||
| 7795 | 0.082 | 0.276 | 0 | 1 | Father: Graduated from primary school (1: yes; 0: no) | ||
| 7795 | 0.027 | 0.163 | 0 | 1 | Father: Graduated from junior high school (1: yes; 0: no) | ||
| 7795 | 0.015 | 0.121 | 0 | 1 | Father: Graduated from senior high school (1: yes; 0: no) | ||
| 7795 | 0.009 | 0.095 | 0 | 1 | Father: Graduated from college or above (1: yes; 0: no) | ||
| 8156 | 0.945 | 0.228 | 0 | 1 | Mother: no schooling (1: yes; 0: no) | ||
| 8156 | 0.032 | 0.177 | 0 | 1 | Mother: educated without completing primary school (1: yes; 0: no) | ||
| 8156 | 0.015 | 0.123 | 0 | 1 | Mother: Graduated from primary school (1: yes; 0: no) | ||
| 8156 | 0.004 | 0.062 | 0 | 1 | Mother: Graduated from junior high school (1: yes; 0: no) | ||
| 8156 | 0.003 | 0.053 | 0 | 1 | Mother: Graduated from senior high school (1: yes; 0: no) | ||
| 8156 | 0.001 | 0.022 | 0 | 1 | Mother: Graduated from college or above (1: yes; 0: no) | ||
| 8484 | 3.559 | 0.996 | 1 | 5 | Family financial status (1: best; 5: worst) | ||
| 8552 | 2.168 | 0.621 | 1 | 3 | Type of residence at birth (1: concrete; 2 adobe; 3 wood or others) | ||
| Parents’ health status and health behaviors | US (8) | 3015 | 0.013 | 0.112 | 0 | 1 | Non-response of father (1: yes; 0: nos) |
| 3015 | 0.041 | 0.198 | 0 | 1 | Alive father (1: yes; 0: no) | ||
| 3015 | 0.435 | 0.496 | 0 | 1 | Father had shorter than the median level longevity (1: yes; 0: no) | ||
| 3015 | 0.511 | 0.500 | 0 | 1 | Father had longer than the median level longevity (1: yes; 0: no) | ||
| 3015 | 0.018 | 0.133 | 0 | 1 | Non-response of mother (1: yes; 0: nos) the four | ||
| 3015 | 0.117 | 0.322 | 0 | 1 | Alive mother (1: yes; 0: no) | ||
| 3015 | 0.359 | 0.480 | 0 | 1 | Mother had shorter than the median level longevity (1: yes; 0: no) | ||
| 3015 | 0.506 | 0.500 | 0 | 1 | Mother had longer than the median level longevity (1: yes; 0: no) | ||
| CHN (12) | 8585 | 0.171 | 0.376 | 0 | 1 | Parents’ health condition (1: anyone spent long time in bed; 0: none) | |
| 8585 | 0.058 | 0.232 | 0 | 1 | Father has drinking problem (1: alcoholism; 0: none) | ||
| 8585 | 0.099 | 0.299 | 0 | 1 | Mother smokes (1: yes; 0: none) | ||
| 8585 | 0.421 | 0.494 | 0 | 1 | Father smokes (1: yes; 0: none) | ||
| 8585 | 0.236 | 0.425 | 0 | 1 | Non-response of father (1: yes; 0: nos) | ||
| 8585 | 0.029 | 0.167 | 0 | 1 | Alive father (1: yes; 0: no) | ||
| 8585 | 0.360 | 0.480 | 0 | 1 | Father had shorter than the median level longevity (1: yes; 0: no) | ||
| 8585 | 0.375 | 0.484 | 0 | 1 | Father had longer than the median level longevity (1: yes; 0: no) | ||
| 8585 | 0.204 | 0.403 | 0 | 1 | Non-response of mother (1: yes; 0: no) | ||
| 8585 | 0.078 | 0.268 | 0 | 1 | Alive mother (1: yes; 0: no) | ||
| 8585 | 0.336 | 0.472 | 0 | 1 | Mother had shorter than the median level longevity (1: yes; 0: no) | ||
| 8585 | 0.382 | 0.486 | 0 | 1 | Mother had longer than the median level longevity (1: yes; 0: no) | ||
| Health and nutrition conditions in Childhood | US (5) | 3015 | 1.702 | 0.939 | 1 | 5 | Self-rated health before age 16 (1: excellent; 5: poor) |
| 3015 | 0.038 | 0.192 | 0 | 1 | Before age 16, were you ever disabled for six months or more because of a health problem? That is, were you unable to do the usual activities of classmates or other children your age? | ||
| 3015 | 0.102 | 0.302 | 0 | 1 | Before age 16, had a blow to the head, a head injury or head trauma severe enough to require medical attention, to cause loss of consciousness or memory loss for a period of time (Y/N) | ||
| 2930 | 2.583 | 0.895 | 1 | 5 | When you were 10 how well did you do in math compared to other children in your class (1: much better, 2: better, 3: about the same, 4: worse, 5: much worse) | ||
| 2929 | 2.400 | 0.928 | 1 | 5 | When you were 10 how well did you do in reading and writing compared to other children in your class? (1: much better, 2: better, 3: about the same, 4: worse, 5: much worse) | ||
| CHN (5) | 8469 | 2.684 | 0.995 | 1 | 5 | Self-rated health before age 15 (1: healthiest; 5: least healthy) | |
| 8348 | 1.071 | 0.733 | 0 | 2 | Did you ever experience hunger (0: no; 1: yes after age 5; 2: yes before age 5) | ||
| 8418 | 0.787 | 0.410 | 0 | 1 | Have you received any vaccinations before 15 years old?(1: yes; 0: no) | ||
| 8585 | 0.281 | 0.450 | 0 | 1 | The type of doctor you visited for the first time was in general hospital specialized hospital or township health clinics? (1: yes; 0: no) | ||
| 8585 | 0.258 | 0.438 | 0 | 1 | The type of doctor you visited for the first time was in community (or village) health centers or private clinics? (1: yes; 0: no) | ||
| Relationship with parents | US (4) | 3014 | 0.066 | 0.248 | 0 | 1 | Before you were 18 years old, were you ever physically abused by either of your parents? (1: often or somewhat; 0: rarely or never) |
| 2955 | 0.131 | 0.337 | 0 | 1 | Before age 16 did you ever separated from you mother for 6 months or longer? | ||
| 2956 | 0.239 | 0.427 | 0 | 1 | Before age 16 did you ever separated from you father for 6 months or longer? | ||
| 2963 | 0.072 | 0.258 | 0 | 1 | Were your grandparents ever your primary caregiver? | ||
| CHN (3) | 7883 | 2.435 | 1.164 | 1 | 5 | Relationship with parents (1: excellent; 2: very good; 3: good; 4: fair; 5: poor) | |
| 8585 | 0.135 | 0.342 | 0 | 1 | Did Male Dependents ever beat you (1: often or somewhat; 0: rarely or never) | ||
| 8585 | 0.207 | 0.405 | 0 | 1 | Did Female Dependents ever beat you (1: often or somewhat; 0: rarely or never) | ||
| Friendship in childhood | US (2) | 3014 | 0.150 | 0.357 | 0 | 1 | Before you were 18 years old, did you have to do a year of school over again? |
| 3014 | 0.052 | 0.222 | 0 | 1 | Before you were 18 years old, were you ever in trouble with the police? | ||
| CHN (1) | 8217 | 0.438 | 0.496 | 0 | 1 | Did you have a good friend (1: yes; 0: no) |
The Chinese and Americans born during the 1930th and the early 1950th may differ significantly. First, because China was a developing country with low rate of urbanization, the disparity between urban and rural areas was much larger. In our sample, the average values of self-rated health, frailty, and mental health are respectively 3.75 (3.94), 1.76 (1.97), and 6.40 (8.68) in urban (rural) China, meaning that older adults born in urban China tend to be healthier than those born in rural areas. Note that a significant proportion of the Chinese respondents, especially those born after 1940, were in childhood when China’s Hukou system (or household registration) was in place, which further strengthened the role played by rural/urban divide. Second, parents of this generation in the two countries have vastly different educational attainment. 65.4% of fathers and 94.5% of mothers received no education in China, while only 2% of fathers and 1.8% of mothers in the USA received no education. Other differences in childhood circumstances between the USA and China were evident in Table 2, such as type of residence at birth, self-rated heath in childhood, and so on. Third, Chinese and Americans born during these decades may have experienced very different historical events affecting their growth. Our decomposition model includes as circumstances key events that some of the Chinese or American birth cohorts experienced. Specifically, the domain—war or economic crisis at birth—contains binary variables for being born during the Great Recession (1929–1933) and the World War II (1941–1945) for Americans and the Anti-Japan War (1937–1945) and the Civil War (1946–1949) for Chinese, respectively. Future work is required to improve the measures of individuals’ exposure to these enormous historical events as they may demonstrate large heterogeneity.
4. Results
4.1. Main Results
Figure 1 shows the contribution of childhood circumstances to health inequality of older adults in the USA and China, respectively. Results show that childhood circumstances contribute to 14.0% of inequality in self-rated health, 18.3% of inequality in mental health, and 30.3% of inequality in frailty in the USA, saliently higher than those in China. These shares of contribution in both China and the USA are smaller in size than many European countries (Bricard et al. 2013). Three domains, i.e. family SES, health and nutrition condition, and parental health and health behaviors, contribute the most to overall health variations in the USA. In China, regional and urban/rural status, health and nutrition condition in childhood, and family SES are the three most important contributors to overall health variations. Notably, family SES in childhood and health and nutrition conditions in childhood contribute more to inequalities in all three health dimensions in the USA than in China, while regional and urban/rural status contribute more to inequalities in all three health dimensions in China than in the USA.
Fig. 1.
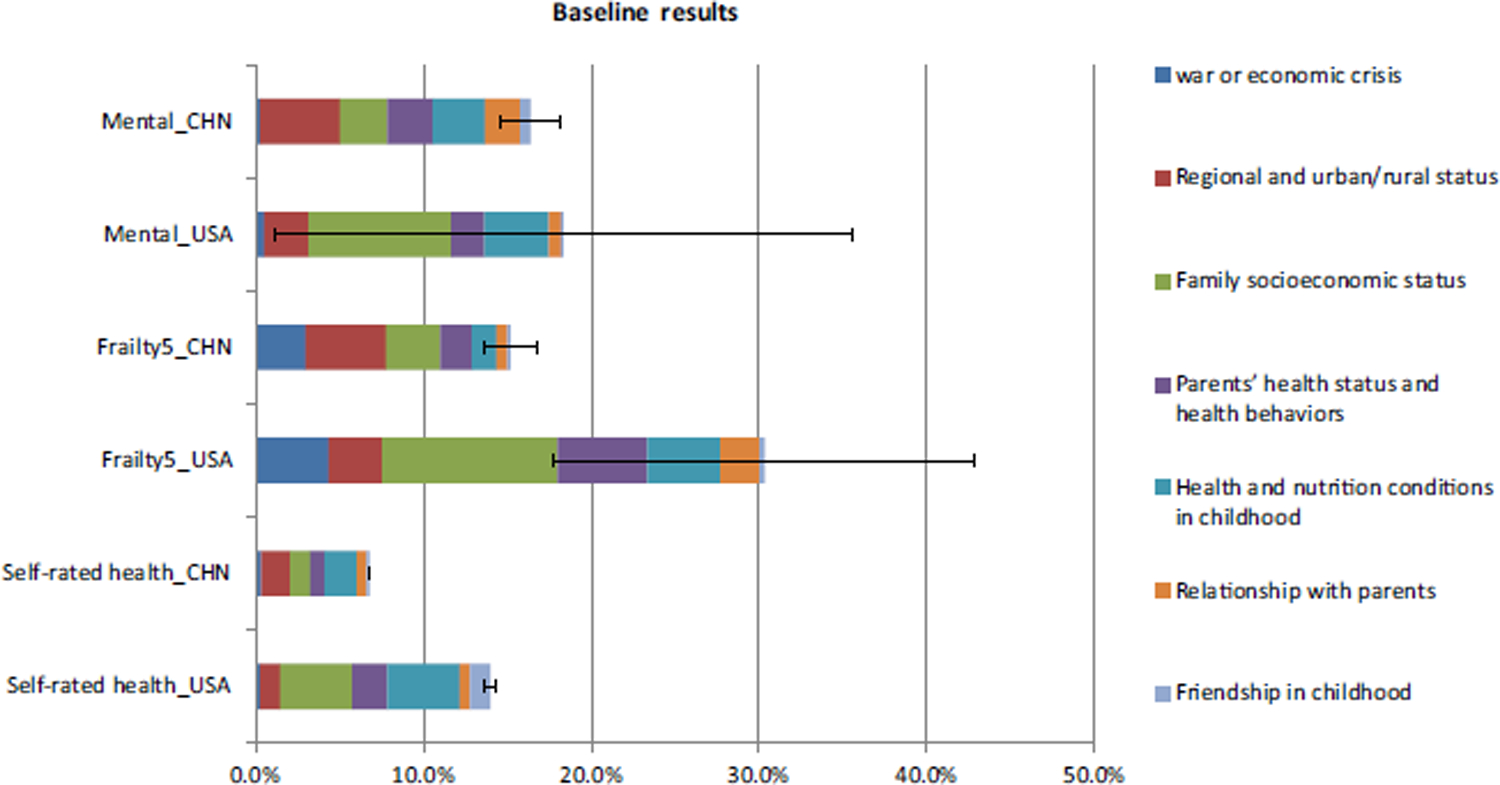
Share of health inequality in old age due to childhood circumstances (the USA vs. China, age 60 +)
Comparisons of the size and statistical significance of the contributions by domain of childhood circumstances may shed light on their different linkages with health inequality and the differences between the USA and China.
First, Fig. 2 shows IOP in self-rated health. Nearly all domains of circumstances contribute at 1% level of significance to self-rated health in the USA and China. Four domains of childhood circumstances, including family SES, parental health status and health behaviors, health and nutrition conditions, and friendship, contribute more to inequality of self-rated health in the USA than in China, while one domain—regional and urban/rural status—contributes more in China. Indirect health circumstances contribute slightly more (7.54% in the USA and 4.00% in China) than direct health circumstances (6.42% in the USA and 2.77% in China) to inequality of self-rated health. Inequality in self-rated health in the USA is generated more by micro or individual circumstances. In contrast, the greater regional and urban/rural disparities in China and their larger contributions to self-rated health inequality suggest important role of macro or institutional circumstances.
Fig. 2.
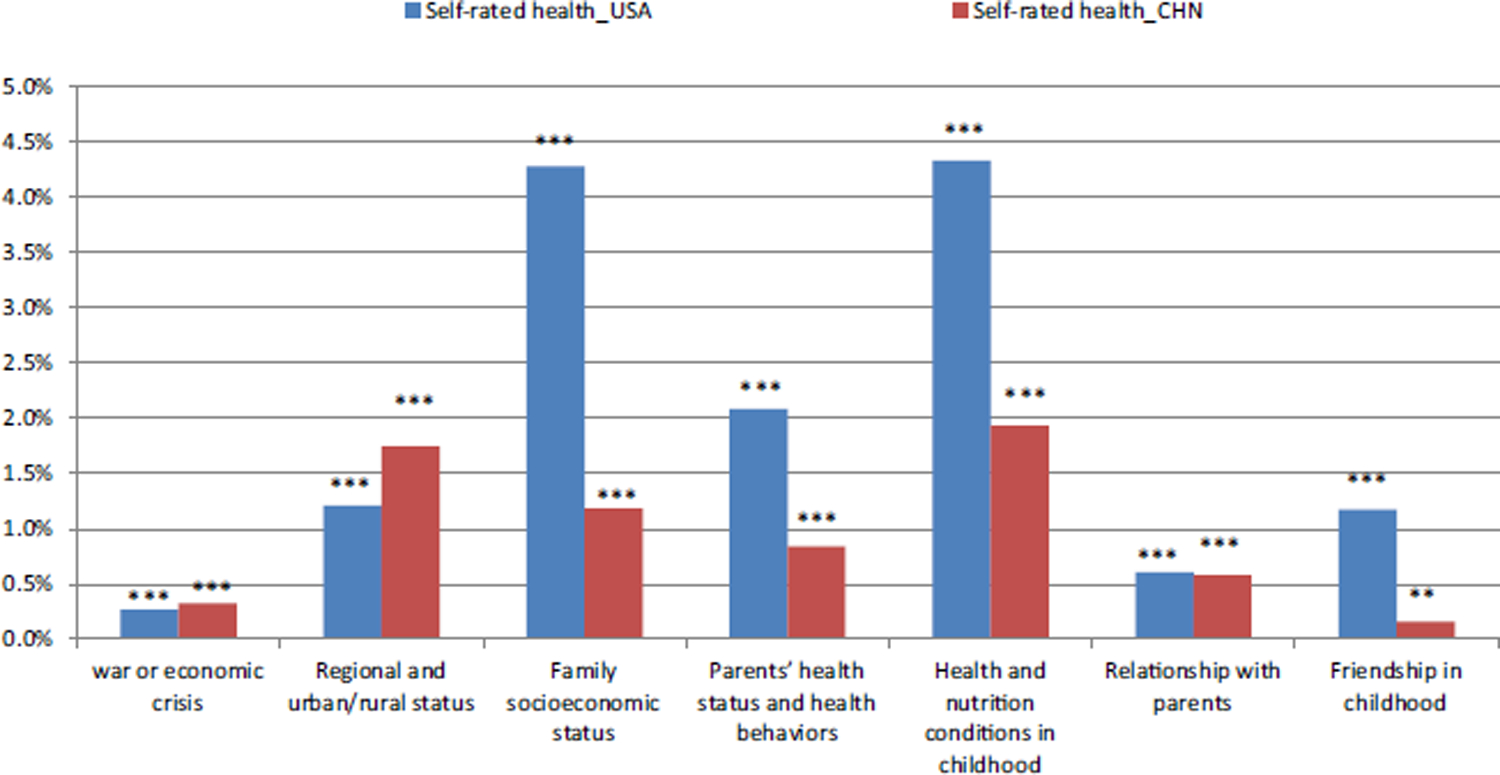
Contribution by domain of circumstances to inequality in self-rated health (the USA vs. China, age 60 +). Notes: **p < 0.05, ***p < 0.01
Figure 3 shows IOP in mental health. All seven domains of circumstances contribute at 1% level of significance to mental health inequality in the USA and China. Five domains of circumstances, i.e. war or economic crisis, family SES, parental health status and health behaviors, health and nutrition conditions in childhood, and relationship with parents, contribute more to inequality of mental health in the USA, while regional and urban/rural status contribute more in China. Indirect health circumstances contribute more (12.52% in the USA and 10.54% in China) than direct health circumstances (5.83% in the USA and 5.84% in China) to inequality of mental health.
Fig. 3.
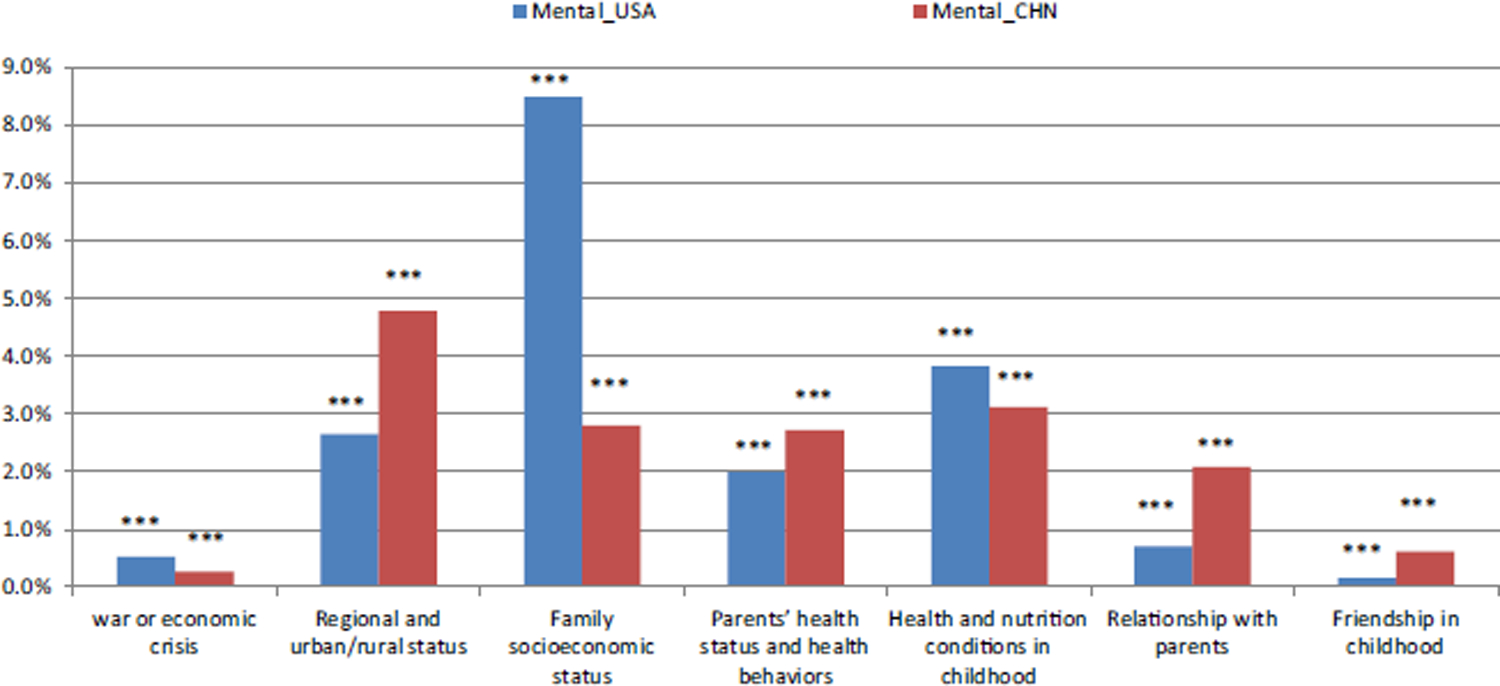
Contribution by domain of circumstances to inequality in mental health (the USA vs. China, age 60 +). Notes: ***p < 0.01
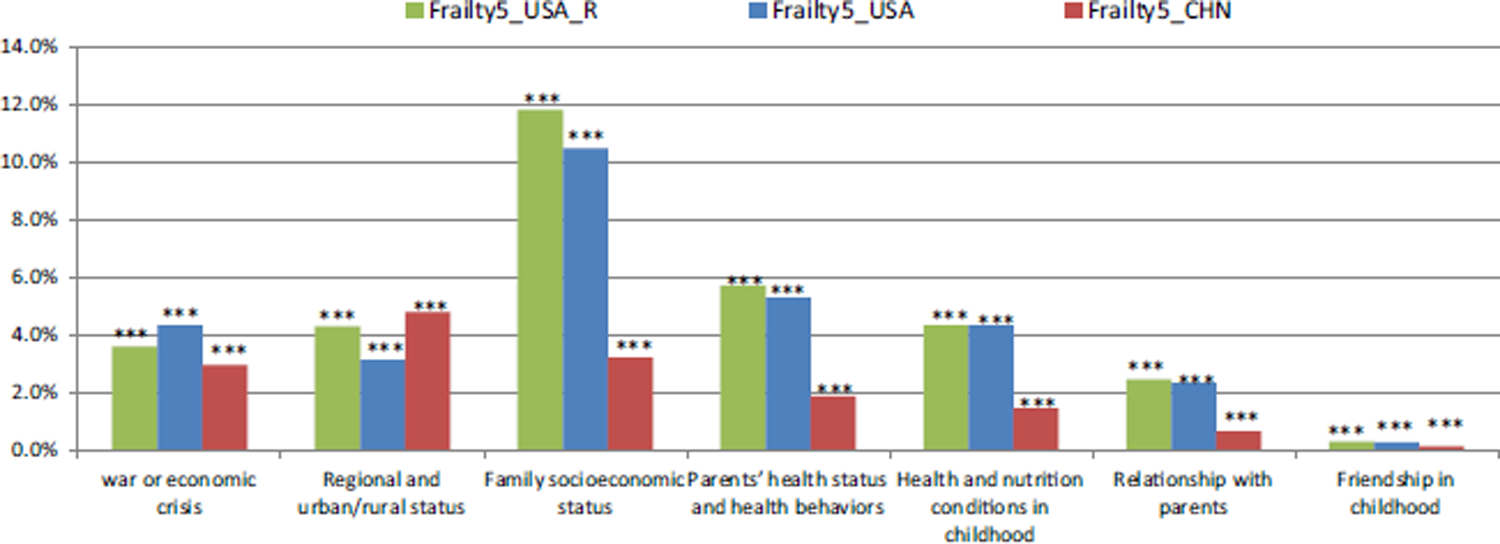
Figure 4 shows IOP in frailty. Nearly all domains of circumstances demonstrate impact at the 1% level of significance. Five domains of circumstances, i.e. war or economic crisis, family SES, health and nutrition conditions in childhood, parental health and health behaviors, and relationship with parents, contribute more to variations in frailty in the USA than in China, while regional and urban/rural status contributes more in China than in the USA. Indirect health circumstances contribute more (20.64% in the USA and 11.83% in China) than direct health circumstances (9.68% in the USA and 3.36% in China) to inequality of frailty.
Fig. 4.
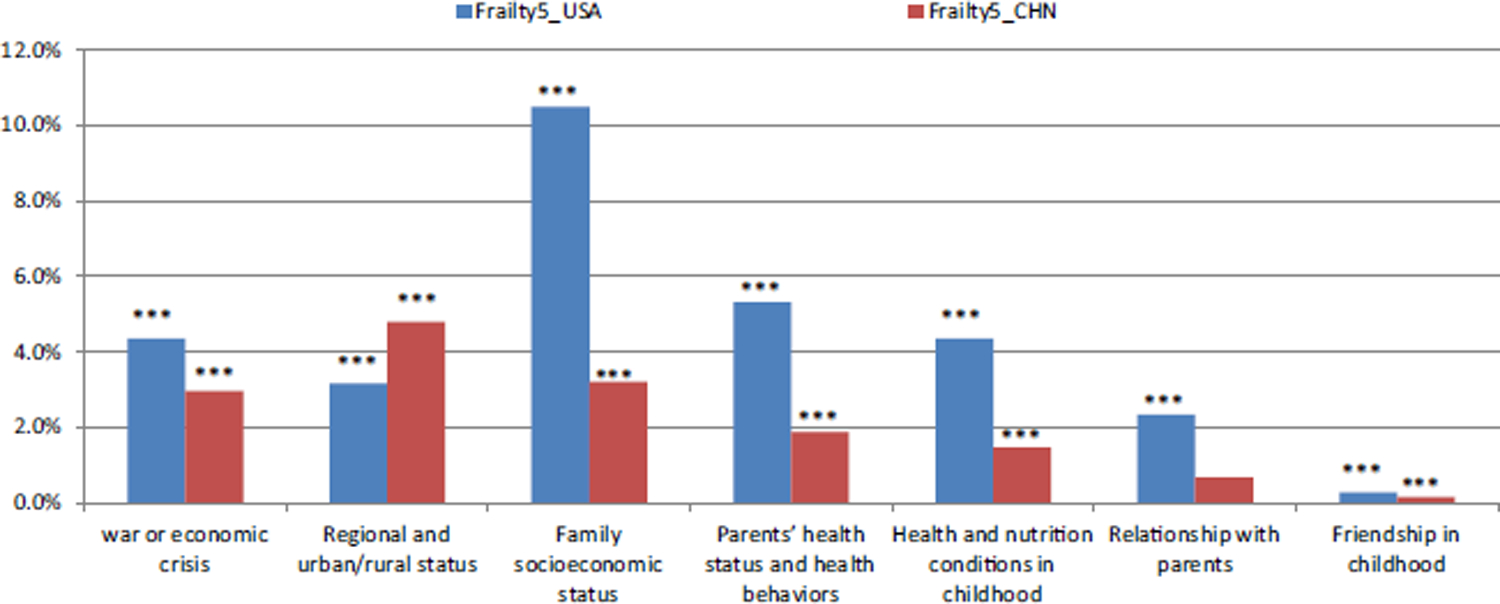
Contribution by domain of circumstances to inequality in physical health (the USA vs. China, age 60 +). Notes: ***p < 0.01
4.2. Other Findings and Robustness
As an important sensitivity analysis, Fig. 6 in “Appendix 1” further restricts our analysis to a subset of circumstances in each domain (highlighted in Table 2) most comparable between the USA and China. This more parsimonious set of childhood circumstances also mitigates the concern that overfitting the decomposition models may inflate the measures of IOP in health. All main findings in Fig. 6 in “Appendix 1” are robust to this test. First, the contributions of childhood circumstances to health inequality are higher in the USA than in China across health dimensions. Second, indirect health circumstances contribute larger than direct health circumstances to health inequality. Third, health inequality in the USA is especially more associated with micro or individual circumstances, while larger share of health inequality in China is attributable to macro or institutional circumstances.
A major concern of the life course approach is that each age cohort may have experienced very different childhood circumstances, making our findings only specific to the age cohort under study. Our main analysis has focused on persons older than 60 in both the China and the USA samples. Next, we extend our tests to IOP in health for other and younger age cohorts and examine potential differences in the contribution of childhood circumstances to old-age health by age cohort.
Since the youngest respondents in HRS-sister surveys were age 45 and age 50 in CHARLS and HRS respectively, we divided the sample and estimated using the CHARLS age cohorts 45–49 and 50–5911 (Fig. 7 in “Appendix 1”) and the HRS age cohort 50–64 (Fig. 8 in “Appendix 1”).12 Because frailty was only measured for those older than 65, and younger cohort did not experience the same historical events that may have affected their growth, Figs. 7 and 8 in “Appendix 1” exclude frailty and a domain of childhood circumstances, i.e. war or economic crisis.
First, we find once again that the contributions of childhood circumstances to health inequality for younger cohorts are higher in the USA than in China across health dimensions (Figs. 7, 8 in “Appendix 1”). Second, in both countries IOP in health is larger for younger age cohort. Specifically, in China IOP in health is the largest for age cohort 45–49 among those older than 45. In the USA it is the largest for age cohort 50–64 among those older than 50. Third, across younger and older age cohorts, our results once again show that childhood health is a commonly important contributor to health in old age across China and the USA. The dominating contributors in China and the USA, however, are regional and rural/urban status at birth (for Chinese) and family SES (for Americans). These childhood circumstances also have varying contributions to health variations over age. Specifically, the contributions of regional and urban/rural status to health variations decrease with age, indicating that the Hukou (registration) system can be more binding for younger cohorts. Family SES contributes more to health variations with age, suggesting a long-lasting effect of SES. The importance of health and nutrition conditions in childhood to health variations decline with age.
We provide further evidence in Fig. 9 in “Appendix 1” that our estimated contribution of childhood circumstances to variations in frailty for older Americans remain robust to alternative sample screening, so are the conclusions we drew from the comparison between the USA and China. In comparison to the main analysis that uses all individuals who participated in at least one of the two waves of frailty tests, in this robustness check only individuals who participated in both waves of HRS frailty tests over four years are included.
5. Conclusion and Discussions
This paper documents IOP in health in the United States and China. We link dimensions of older adults’ health outcomes with most comprehensive domains of their childhood circumstances at least 50 years earlier.
First, we find sizable IOP in health in both the USA and China, with greater contributions of childhood circumstances to self-rated health, mental health and physical frailty in the USA than in China. Specifically, childhood circumstances may respectively explain 7–16 and 14–30% of health inequality in old age in China and the USA, depending on the health measures. Given the larger variations of health status as well as larger shares of health inequality due to childhood circumstances in the USA than in China, this result suggests that the USA has larger room to address health inequality out of the realm of individual choices.
Second, we demonstrate that the most important observable childhood circumstances in China and the USA are geographic factors at birth and family SES, respectively. Regional and urban/rural status at birth (e.g. characterized by Hukou system) has played a substantially important role in determining health inequality in China (Zhang and Kanbur 2005; Strauss et al. 2018). While respondents in this study were all born before early 1950 s, i.e. prior to the onset of the stringent Hukou (urban/rural) system, its enforcement during their childhood still had consequence on health inequality in olde age. In the same era, the USA was already the world’s largest industrial nation with almost no restriction on population mobility. Therefore, larger gap in regional development at birth in China than in the USA could contribute to more health variations in the former. Family SES in childhood is a commonly important contributor to health inequality in both countries, with a greater contribution to the USA than to China. As expected, our finding suggests health and nutritional condition in childhood being an important circumstance in both countries.
Third, we show that in both countries IOP in health is larger for younger age cohort. There are at least two interpretations. One is that childhood circumstances may explain a declining portion of health variation in old age, assuming these age cohorts are homogeneous. In other words, while existing studies have shown that child health is a strong predictor of health in adulthood or old age (Case, Fertig and Paxson 2005; Smith 2009), IOP in health may converge over age. Another interpretation postulates that different age cohorts may have experienced very different childhood circumstances. For example, rising inequality in recent decades has affected younger cohort more than older cohort during childhood. Countries with greater economic inequality also tend to be countries with larger inequality of opportunity, as disadvantage can be more passed on from parents to children (Lefranc et al. 2008; Corak 2013).
Fourth, while both direct and indirect health circumstances contribute significantly to health inequality in old age, the latter tends to contribute more to all three health dimensions in both the USA and China. This is consistent with the notion that social determinants often play an important role beyond health care in promoting population health and health equity (Mcginnis et al. 2002). As many countries spend an increasingly large portion of resources on health care with no expected gain in population health (Bradley et al. 2016), our study suggests that more attention should be given to how and to what extent indirect health circumstances contribute to long-term health and health inequality. Both China, the largest developing country with among the highest growth rate and potential of health spending, and the United States, the largest developed country with the highest share of national income on the health sector, have recognized the need to focus health resources more heavily on population health. This is a key component of Healthy China 2030 and U.S. Healthy People 2020 (Chen 2018).
This study demonstrates the value of integrating a life course approach with a cross-country comparative perspective in identifying key determinants of health inequality among older adults. Distinguishing sources of health inequality and rectifying key childhood circumstances should be the basis of policy that promotes health equity. Adequate policy responses must be informed by the specific circumstances of the society among which IOP in health is generated. To improve the health of older persons, further studies are needed to develop and evaluate successful interventions to childhood circumstances.
The main strengths of this study include that we provide some of the first evidence of IOP in health using comprehensive dimensions of health outcomes and domains of childhood circumstances. Our comparative analyses are between two large countries with different lifestyles and health systems, and large gaps in economic development, rendering it potential to shed light on the role that specific institutions play in shaping individual lifetime outcomes in specific contexts.
This study has the following limitations. First, this observational study cannot draw casual inference. To uncovering causal mechanisms, future work will investigate potential channels through which the effect of childhood circumstances on late-life health may operate. Second, early-life circumstances correlate not only with lifetime health trajectories, but also with lifetime socio-economic trajectories, and the latter are bound to affect observed health outcomes independently of the former. Future studies should distinguish direct link between early-life circumstances and long-term health from the effects of lifetime circumstances stemming from early-life circumstances. Third, while this study incorporates richer set of childhood circumstances in the analysis, our partial observation of the full information determines what we obtained can be lower bounds of the actual contribution by childhood circumstances, after mitigating the concern over overfitting the models with such circumstances. Fourth, childhood conditions in the life history survey are based on recall, therefore may suffer from reporting errors. Fifth, our life course study focusses on a specific cohort (i.e. above age 60 at the time of survey). While we try best to model the specific circumstances during their childhood, such as wars or economic crisis, it leaves for further tests if our findings could be generalized to other age cohorts with distinctive childhood circumstances. Finally, future work should aim to explain why overall childhood circumstances account for more health inequality in the USA than in China, and may better explain why regional and rural/urban status are more important to health inequality in China than in the USA.
Acknowledgements
Dr. Yan is supported by the Natural Science Foundation of China (71974097, 71503129) and the Fundamental Research Funds for the Central Universities (SKCX2019006), a project funded by the Priority Academic Program Development of Jiangsu Higher Education Institute (PAPD), a research grant by China Center for Food Security Studies at Nanjing Agricultural University, and Jiangsu Center of Agricultural Modernization. Dr. Gill is the recipient of an Academic Leadership Award (K07AG043587) from the National Institute on Aging. Drs. Gill and Chen are supported by the Yale Claude D. Pepper Older Americans Independence Center (P30AG21342). Dr. Chen acknowledges financial support from the James Tobin Research Fund at Yale Economics Department, NIH/NIA grants (R03AG048920; K01AG053408), and faculty research grant awarded by Yale Macmillan Center (2017-2019). We are grateful to Maya Mahin for research assistance. The authors declare that there is no conflict of interest regarding the preparation of this manuscript.
Appendix 1.
Fig. 5.
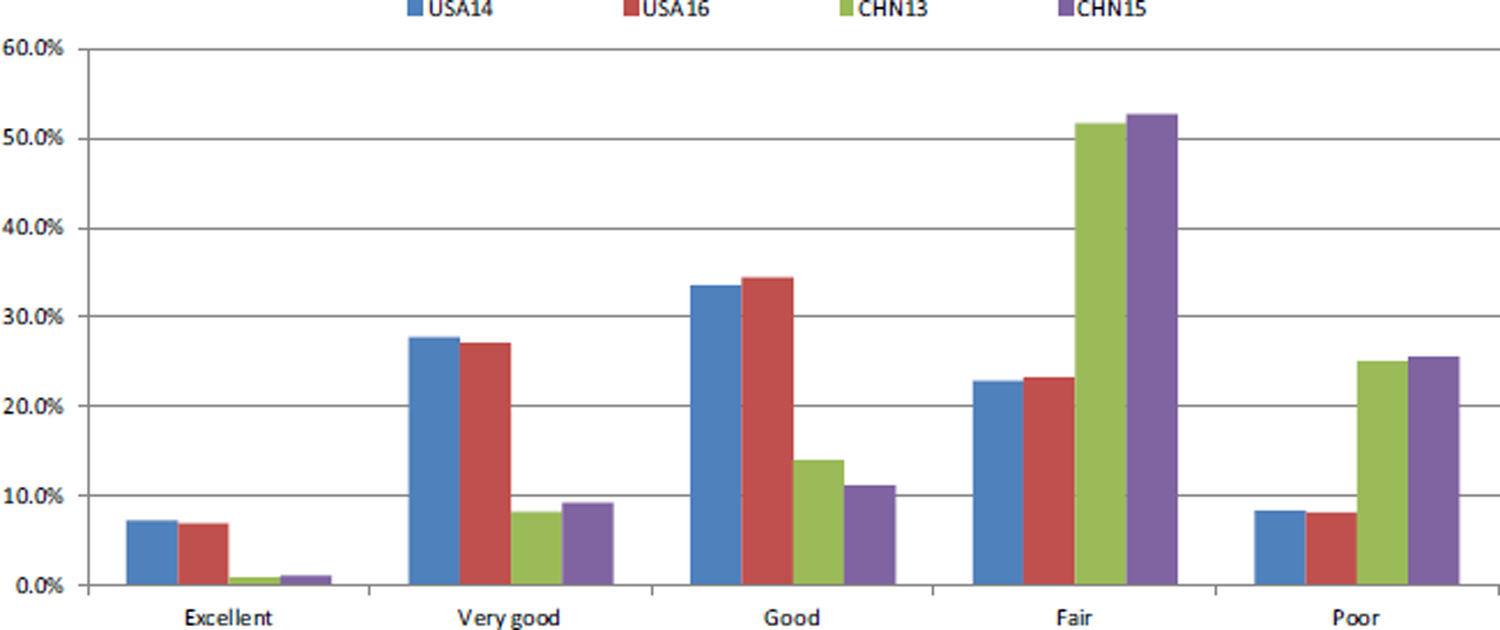
Distributions of self-rated health (the USA vs. China, age 60 +). Notes: USA14 and USA16 respectively represent self-rated health in 2014 and 2016 in the USA, CHN13 and CHN15 respectively represent self-rated health in 2013 and 2015 in China
Fig. 6.
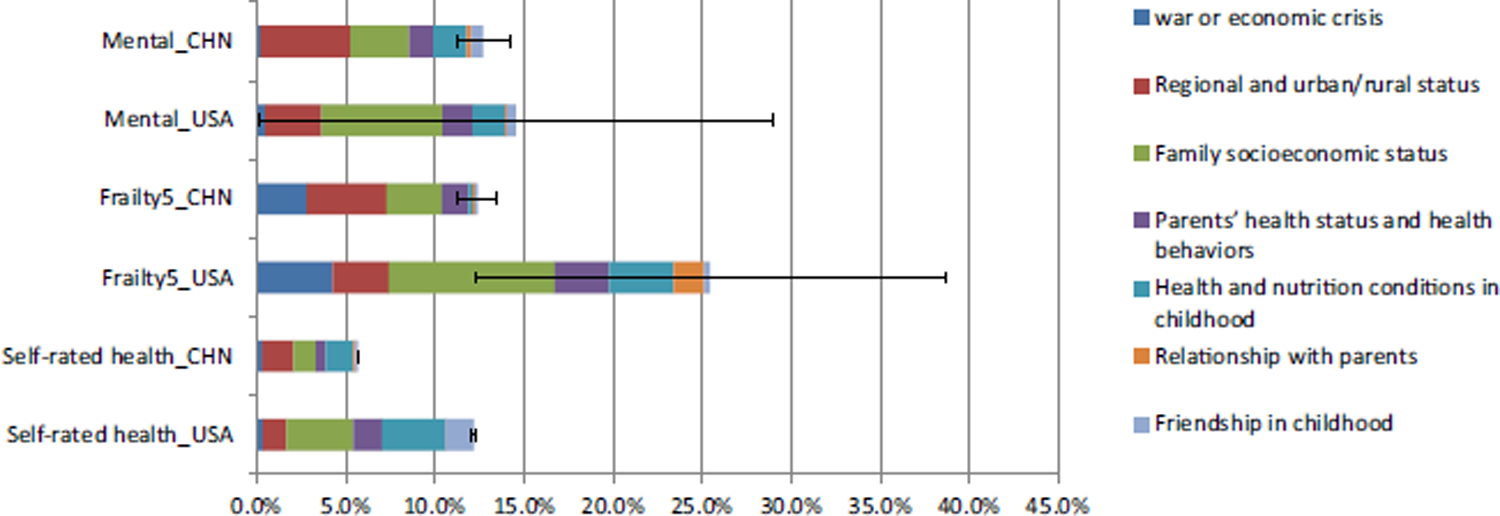
Sensitivity analysis of main findings in Fig. 1 (the USA vs. China, on Age Cohort 60 +, Restricting to More Comparable Childhood Circumstances Defined in Table 2). Notes: This set of results only consider childhood circumstances comparable between the USA and China. Specifically, the family SES domain only includes parents’ educational attainments, household type, family financial status; the domain of parents’ health status and health behaviors only includes parents’ longevity status; the domain of relationship with parents only includes physical abuse by parents; the domain of health and nutrition conditions in childhood only includes self-rated health
Fig. 7.
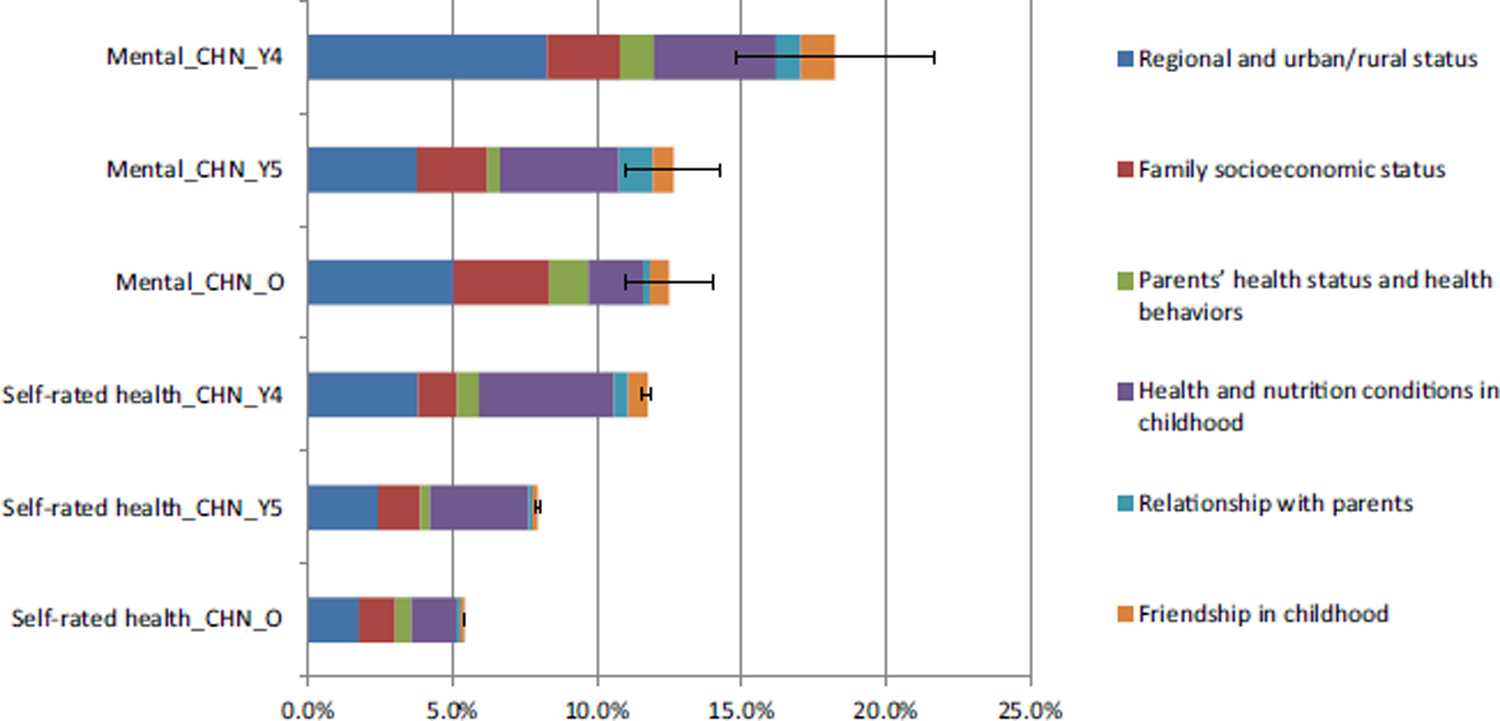
Robustness Checks Comparing Age Cohorts 45–49, 50–59, and 60 + using the Chinese Sample (Restricting to More Comparable Childhood Circumstances Defined in Table 2). Note: O represents age cohort 60 +, Y4 represents age cohort 45–49, Y5 denotes age cohort 50–59
Fig. 8.
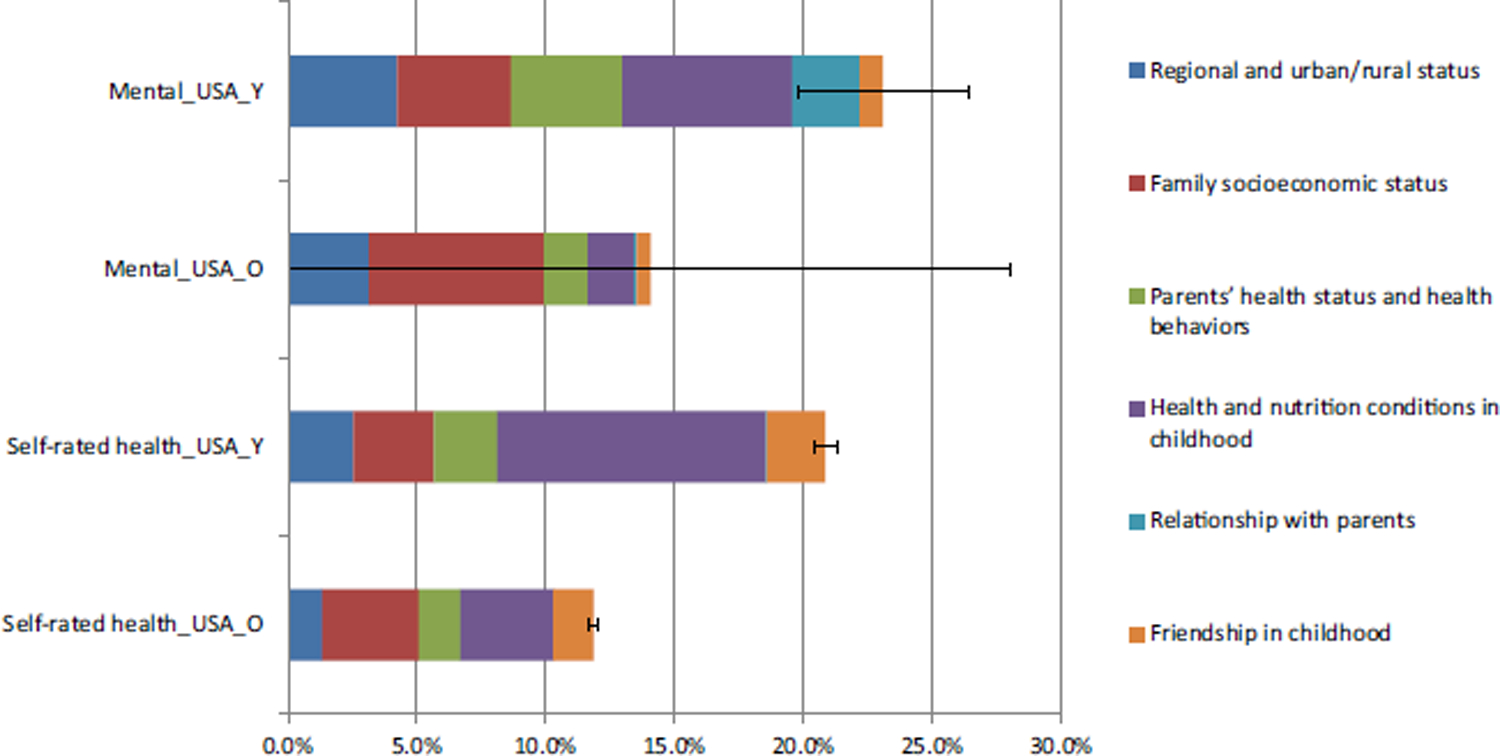
Robustness Checks Comparing Age Cohorts 50–64 and 65 + using the American Sample (Restricting to More Comparable Childhood Circumstances Defined in Table 2). Note: Y represents age cohort 50–64, O represents age cohort 65 +
Fig. 9.
Robustness Checks Comparing Alternative Samples of the USA in physical health (the USA vs. China, age 65 +). Notes: ***p < 0.01. Frailty5_USA represents results using the sample in original submission with 2266 individuals who participated in at least one of the two waves of frailty tests. Frailty5_ USA_R represents results using the sample with 2075 individuals who participated in both waves of HRS frailty tests
Appendix 2: Measuring Relative Contribution of Each Domain of Childhood Circumstances
The overall contribution can be neatly decomposed into components for each category j in childhood circumstances C with the idea of the Shapley approach.
| (4) |
where j, k=1, 2, … are categories of childhood circumstances. αj and αk are coefficients of categories j and k. Equation (4) presents an example of a Shapley Value Decomposition. This approach provides an appropriate way to assign roles to sources in generating health inequality (Björklund et al. 2012; Ferreira and Gignoux 2013; Jusot et al. 2013; Shorrocks 2013; Roemer and Trannoy 2016).
A particular category j’s overall contribution to the variance in Y——corresponds to an average between two channels. Intuitively, childhood circumstances may not only directly impact health in old age, but exert their effects indirectly through shaping other childhood circumstances and adulthood efforts. Formally, all are held constant in the direct contribution of category j, i.e. . Regarding the indirect contribution, category j itself is held constant, and its indirect contribution, i.e. , is taken as the difference between the total variance and the ensuing variance.
To compute the Shapley value decomposition, we first estimate the inequality measure for all possible permutations of the circumstance variables. In a second step, the average marginal effect of each circumstance variable on the measure of IOP is computed (Juarez and Soloaga 2014). This procedure is very computationally intensive as 2 K (K= number of circumstances) must be computed.
Footnotes
The number of older persons—those aged 60 years or over—has increased substantially, from 0.61 billion (or 9.9% of the population) in 2000 to 0.90 billion (or 12.3% of the population) in 2015 in the world. This growth is projected to accelerate in the coming decades, to reach almost 1.40 billion (or 16.5% of the population) by 2030 and nearly 2.09 billion (or 21.5% of the population) by 2050 in the world (United Nations 2015).
A life course approach emphasizes a temporal and social perspective, looking back across an individual’s or a cohort’s life experiences or across generations for clues to current patterns of health and disease, while recognizing that both past and present experiences are shaped by the wider social, economic and cultural context (WHO 2000).
Inequality of Opportunity in health refers to health inequality due to circumstances that are beyond individual control (Roemer 2002). Childhood circumstances are the main factors beyond individual control, since individuals cannot be held responsible for their birth lottery. In contrast, efforts can be freely chosen by individuals according to their preferences and, hence, may contribute to health inequality.
Let us suppose there are two individuals with logarithmic values of health outcome lnx1 and lnx2, respectively. According to Jensen’s Inequality, MLD increases with inequality −(lnx1 + lnx2)/2 > − ln [(x1 + x2)/2]. The MLD is nonnegative, takes the value zero when everyone has the same health status, and takes larger positive values as health becomes more unequal.
Ф(μ,f) has a cumulative distribution function that is a step function, with as many steps as types. This is often called the ‘smoothed’ distribution of F associated with the typology (f , μ).
The 150 county-level units were randomly selected using probability proportional to size (PPS) and stratified by region, urban/rural and county-level gross domestic product (GDP). Within each county-level unit, three village-level units (villages in rural areas and urban communities in urban areas) were randomly selected using PPS as primary sampling units (PSUs). Within each PSU, 80 dwellings were randomly selected from a complete list of dwelling units generated from a mapping or listing operation, using augmented Google Earth maps (Google Inc) along with considerable ground checking. In scenarios with more than one age-eligible household in a dwelling unit, one was randomly selected. From this sample for each PSU, the proportion of households with age-eligible members was determined, as was the proportion of empty residences. From these proportions and an assumed response rate, we selected households from our original PSU frame to obtain a target number of 24 age-eligible households per PSU. Thus, the final household sample size in a PSU depended on the PSU age-eligibility and empty residence rates. In each household, one person aged 45 years or older was randomly chosen as the main respondent, and the individual’s spouse was automatically included. On the basis of this sampling procedure, 1 or 2 individuals in each household were interviewed depending on the marital status of the main respondent.
The HRS sample is selected under a multi-stage area probability sample design. The first stage involves PPS selection of U.S. Metropolitan Statistical Area(MSA) and non-MSA counties. The second stage involves sampling of area segments (SSUs) within sampled PSUs. The third stage includes a complete listing (enumeration) of all housing units (HUs) that are physically located within the bounds of the selected SSUs. The final stage includes the selection of the household financial unit within a sample HU (Heeringa and Connor 1995). More information about the sample design is provided in Sonnega et al. (2014).
Specifically, in terms of the choice of cutoff, Andresen et al. (1994) proposed a 10-item CES-D (total score ranges from 0 to 30) and suggested a cutoff of 10. HRS adopts 8-item CES-D as the measurement of mental health. The possible range for 8-item CES-D is 0–8, and a value of 3 is often used as the cutoff. At a cutoff point of 3 or higher for the 8-item CES-D, Turvey et al. (1999) found high levels of both sensitivity and specificity.
We follow the most adopted rule in existing studies to divide China into 6 regions and the USA into 11 regions to facilitate comparisons with the mainstream literature. While the set of regional and urban/rural status in the CHARLS is smaller than in the HRS, our findings are robust to alternative divisions of regions not reported here.
Overall, all seven domains of childhood circumstances are comparable between the USA and China. These domains range from macro-level regional circumstances to micro-level family circumstances. However, due to the differences in economic development, institutions and culture between the USA and China, some of the specific variables within the circumstances domains differ. For example, parents’ political affiliation (e.g. communist party membership) is an important indicator of family SES in China, but is less important and not provided in America’s HRS survey. The range of number of books at home in childhood is an important circumstances variable in the USA, but not surveyed in China’s CHARLS. Therefore, the subset of circumstances in the robustness check exclude all variables that could not be well matched between CHARLS (China) and HRS (USA), including being inconsistently measured or nonexistent in one country.
The sample sizes of age cohort 60 +, 50–59, and 45–49 are 8255, 6062 and 3219 in the CHARLS 2013/2015.
Since the age cohort 50–59 in HRS only includes about 700 respondents, we use the age cohort 50–64 with about 1400 persons to enlarge the sample size. The sample sizes of age cohort 60 + and 50–59 are 14,167 and 4542 in the HRS 2014/2016 without life history data, and 3014 and 713 in the HRS 2014/2016 with life history data. Therefore, there seems little sample bias between age cohort 60 + and 50–59.
References
- Adhvaryu A, Fenske J, & Nyshadham A (2019). Early life circumstance and adult mental health. Journal of Political Economy, 127(4), 1516–1549. [Google Scholar]
- Almond D, Currie J, & Duque V (2018). Childhood circumstances and adult outcomes: Act II. Journal of Economic Literature, 56(4), 1360–1446. [Google Scholar]
- Almond D, & Mazumder B (2011). Health capital and the prenatal environment: The effect of Ramadan observance during pregnancy. American Economic Journal: Applied Economics, 3(4), 1501–1533. [Google Scholar]
- Andersson L, & Stevens N (1993). Associations between early experiences with parents and well-being in old-age. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 48(3), 109–116. [DOI] [PubMed] [Google Scholar]
- Andreoli F, Havnes T, & Lefranc A (2019). Robust inequality of opportunity comparisons: Theory and application to early-childhood policy evaluation. Review of Economics and Statistics, 101(2), 355–369. 10.1162/rest_a_00747. [DOI] [Google Scholar]
- Andresen EM, Malmgren JA, Carter WB, & Patrick DL (1994). Screening for depression in well older adults: Evaluation of a short form of the CES-D. American Journal of Preventive Medicine, 10(2), 77–84. [PubMed] [Google Scholar]
- Arneson Richard J. (1989). Equality and equal opportunity for welfare. Philosophical Studies, 56(1), 77–93. [Google Scholar]
- Björklund A, Jäntti M, & Roemer JE (2012). Equality of opportunity and the distribution of long-run income in Sweden. Social Choice and Welfare, 39(2), 675–696. [Google Scholar]
- Black S, Devereux P, & Salvanes K (2016). Does grief transfer across generations? Bereavements during pregnancy and child outcomes. American Economic Journal: Applied Economics, 8(1), 193–223. [Google Scholar]
- Bombak A (2013). Self-rated health and public health: A critical perspective. Frontiers in Public Health, 1, 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley EH, Canavan M, Rogan E, Talbert-Slagle K, Ndumele C, Taylor L, et al. (2016). Variation in health outcomes: The role of spending on social services, public health, and health care, 2000–09. Health Affairs, 35(5), 760–768. [DOI] [PubMed] [Google Scholar]
- Bratberg E, Davis J, Mazumder B, Nybom M, & Schnitzlein D (2017). A Comparison of Intergenerational mobility curves in Germany, Norway, Sweden, and the USA. Scandinavian Journal of Economics, 119(1), 72–101. [Google Scholar]
- Bricard D, Jusot F, Trannoy A, & Tubeuf S (2013). Inequality of opportunity in health and the principle of natural reward: Evidence from European Countries. Research on Economic Inequality, 21, 335–370. [Google Scholar]
- Carrieri V, & Jones A (2018). Inequality of opportunity in health: A decomposition-based approach. Health Economics, 27(12), 1–15. [DOI] [PubMed] [Google Scholar]
- Case A, Fertig A, & Paxson C (2005). The lasting impact of childhood health and circumstance. Journal of Health Economics, 24(2), 365–389. [DOI] [PubMed] [Google Scholar]
- Chen X (2018). Promoting population health: Some U.S. lessons for China at the crossroads. The Journal of the American Chamber of Commerce in Shanghai. Insight, pp. 11–13. [Google Scholar]
- Chetty R, Grusky D, Hell M, Hendren N, Manduca R, & Narang J (2017). The fading American Dream: Trends in absolute income mobility since 1940. Science, 356(6336), 398–406. [DOI] [PubMed] [Google Scholar]
- Cohen GA (1989). On the currency of egalitarian justice. Ethics, 99(4), 906–944. [Google Scholar]
- Corak M (2013). Income inequality, equality of opportunity, and intergenerational mobility. Journal of Economic Perspectives, 27(3), 79–102. [Google Scholar]
- Dahl E, & Birkelund G (1997). Health inequalities in later life in a social democratic welfare state. Social Science and Medicine, 44, 871–881. [DOI] [PubMed] [Google Scholar]
- Dodds R, Denison HJ, Ntani G, et al. (2012). Growth in early life and muscle strength: A systematic review and meta-analysis. Journal of Nutrition, Health & Aging, 16, 609–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dworkin Ronald. (1981a). What is equality? Part 1: Equality of welfare. Philosophy & Public Affairs, 10(3), 185–246. [Google Scholar]
- Dworkin Ronald. (1981b). What is equality? Part 2: Equality of resources. Philosophy & Public Affairs, 10(4), 283–345. [Google Scholar]
- Ferreira F, & Gignoux J (2011). The measurement of inequality of opportunity: Theory and an application to Latin American. Review of Income Wealth, 57(4), 622–657. [Google Scholar]
- Ferreira F, & Gignoux J (2013). The measurement of educational inequality: Achievement and opportunity. World Bank Economic Review, 28, 210–246. [Google Scholar]
- Fleurbaey M, & Schokkaert E (2009). Unfair inequalities in health and health care. Journal of Health Economics, 28(1), 73–90. [DOI] [PubMed] [Google Scholar]
- Fried L, Tangen C, Walston J, Newman A, Hirsch C, Gottdiener J, et al. (2001). Frailty in older adults: Evidence for a phenotype. Journal of Gerontology, Series A: Biological Sciences and Medical Sciences, 56(3), M146–M156. [DOI] [PubMed] [Google Scholar]
- Gale C, Booth T, Starr J, & Deary I (2016). Intelligence and socioeconomic position in childhood in relation to frailty and cumulative allostatic load in later life: The Lothian Birth Cohort 1936. Journal of Epidemiology and Community Health, 70, 576–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haughton J, & Khandker SR (2009). Handbook on poverty and inequality. Washington, DC: World Bank. [Google Scholar]
- Heeringa S, & Connor J (1995). Technical description of the health and retirement study sample design. Ann Arbor, Michigan: Institute for Social Research, University of Michigan. https://hrs.isr.umich.edu/publications/biblio/5310. [Google Scholar]
- Hong Y, Zhou Z, Fang Y, & Shi L (2017). The digital divide and health disparities in china: Evidence from a national survey and policy implications. Journal of Medical Internet Research, 19(9), e317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hufe P, Peichl A, Roemer J, & Ungerer M (2017). Inequality of income acquisition: The role of childhood circumstances. Social Choice Welfare, 49, 499–544. [Google Scholar]
- Isen A, Rossin-Slater M, & Walker R (2017). Every breath you take—every dollar you’ll make: The long-term consequences of the Clean Air Act of 1970. Journal of Political Economy, 125(3), 848–902. [Google Scholar]
- Juarez F, & Soloaga I (2014). IOP: Estimating ex-ante inequality of opportunity. Stata Journal, 14(4), 830–846. [Google Scholar]
- Jusot F, Tubeuf S, & Trannoy A (2013). Circumstances and efforts: How important is their correlation for the measurement of inequality of opportunity in health? Health Economics, 22(12), 1470–1495. [DOI] [PubMed] [Google Scholar]
- Kanbur R, & Wagstaff A (2016). How Useful Is Inequality of Opportunity as a Policy Construct? In Basu Kaushik & Stiglitz Joseph E. (Eds.), Inequality and growth: Patterns and policy. Volume 1: Concepts and analysis (pp. 131–148). London: Palgrave McMillan. [Google Scholar]
- Katikireddi S (2016). Economic opportunity: A determinant of health? Lancet Public Health, 1, E4–E5. [DOI] [PubMed] [Google Scholar]
- Ko P-C, & Yeung W-JJ (2019). Childhood conditions and productive aging in China. Social Science and Medicine, 229, 60–69. [DOI] [PubMed] [Google Scholar]
- Kohout F, Berkman L, Evans D, & Cornoni-Huntley J (1993). Two shorter forms of the CES-D depression symptoms index. Journal of Aging and Health, 5(2), 179–193. [DOI] [PubMed] [Google Scholar]
- Krause N (1998). Early parental loss, recent life events, and changes in health among older adults. Journal of Aging and Health, 10, 395–421. [DOI] [PubMed] [Google Scholar]
- Kuh D, Hardy R, Butterworth S, Okell L, et al. (2006). Developmental origins of midlife grip strength: Findings from a birth cohort cohort study. Journal of Gerontology, Series A: Biological Sciences and Medical Sciences, 61, 702–706. [DOI] [PubMed] [Google Scholar]
- Landerso R, & Heckman J (2017). The Scandinavian Fantasy: The sources of intergenerational mobility in Denmark and the U.S. Scandinavian Journal of Economics, 119(1), 178–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lefranc A, Pistolesi N, & Trannoy A (2008). Inequality of opportunities VS inequality of outcomes: Are western societies all alike? Review of Income and Wealth, 54, 513–546. [Google Scholar]
- Leopold L (2018). Education and Physical Health Trajectories in later life: A comparative study. Demography, 55(3), 901–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z, Chen X, Gill T, Ma C, Crimmins EM, & Levine ME (2019). Disentangling the contribution of childhood and adulthood circumstances and genetics to phenotypic aging: Prospective cohort study. forthcoming. PLoS Medicine. [Google Scholar]
- Lundberg O, & Manderbacka K (1996). Assessing reliability of a measure of self-rated health. Scandinavian Journal of Public Health, 24(3), 218–224. [DOI] [PubMed] [Google Scholar]
- Marmot M, Friel S, Bell R, Houweling T, & Taylor S (2008). Closing the gap in a generation: Health equity through action on the social determinants of health. The Lancet, 372, 1661–1669. [DOI] [PubMed] [Google Scholar]
- Mazumder B, Almond D, Park K, Crimmins EM, & Finch CE (2010). Lingering prenatal effects of the 1918 influenza pandemic on cardiovascular aging. Journal of Developmental Origins of Health and Disease, 1, 26–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCall L, Burk D, Laperriere M, & Richeson J (2017). Exposure to rising inequality shapes Americans’ opportunity beliefs and policy support. Proceedings of the National Academy of Sciences of the United States of America, 114(36), 9593–9598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEniry M, Palloni A, Davila A, & Gurucharri A (2008). Early life exposure to poor nutrition and infectious diseases and its effects on the health of older Puerto Rican adults. Journal of Gerontology, Series B: Psychological Sciences and Social Sciences, 63(6), S337–S348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcginnis J, Russo PW, & Knickman JR (2002). The case for more active policy attention to health promotion. Health Affairs, 21, 78–93. [DOI] [PubMed] [Google Scholar]
- Milanovic B, (2014). Inequality in the United States and China. Harvard Business Review, (1). https://hbr.org/2014/01/inequality-in-the-united-states-and-china. [Google Scholar]
- Moffitt TE, Belsky DW, Danese A, et al. (2017). The longitudinal study of aging in human young adults: Knowledge gaps and research agenda. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 72(2), 210–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moody-Ayers S, Lindquist K, Sen S, & Covinsky K (2007). Childhood social and economic well-being and health in older age. American Journal of Epidemiology, 166, 1059–1067. [DOI] [PubMed] [Google Scholar]
- Niehues J, & Peichl A (2014). Upper bounds of inequality of opportunity: Theory and evidence for Germany and the US. Social Choice and Welfare, 43(1), 73–99. [Google Scholar]
- Nilsson P (2017). Alcohol availability, prenatal conditions, and long-term economic outcomes. Journal of Political Economy, 125(4), 1149–1207. [Google Scholar]
- Palloni A, McEniry M, Davila A, & Gurucharri A (2005). The influence of early conditions on health status among elderly Puerto Ricans. Social Biology, 52(3–4), 132–163. [DOI] [PubMed] [Google Scholar]
- Persson P, & Rossin-Slater M (2018). Family ruptures, stress, and the mental health of the next generation. American Economic Review, 108(4–5), 1214–1252. [PubMed] [Google Scholar]
- Radloff L (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. [Google Scholar]
- Ramos M (2007). Impact of socioeconomic status on Brazilian elderly health. Revista de Saude Publica, 41, 616–624. [DOI] [PubMed] [Google Scholar]
- Rawls John. (1958). Justice as Fairness. Philosophical Review, 67(2), 164–194. [Google Scholar]
- Rawls John. (1971). A theory of justice. Cambridge: Harvard University Press. [Google Scholar]
- Roemer J (1993). A pragmatic theory of responsibility for the Egalitarian planner. Philosophy and Public Affairs, 22(2), 146–166. [Google Scholar]
- Roemer J (1998). Equality of opportunity, Cambridge, MA and London: Harvard University Press. [Google Scholar]
- Roemer J (2002). Equality of opportunity: A progress report. Social Choice and Welfare, 19, 455–471. [Google Scholar]
- Roemer J, & Trannoy A (2016). Equality of Opportunity: Theory and measurement. Journal of Economic Literature, 54, 1288–1332. [Google Scholar]
- Rosa-Dias R, & Jones A (2007). Giving equality of opportunity a fair innings. Health Economics, 16(2), 109–112. [DOI] [PubMed] [Google Scholar]
- Sayer AA, & Gill TM (2016). Commentary: Value of the life course approach to the health care of older people. International Journal of Epidemiology, 45(4), 1011–1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayer AA, Syddall HE, Gilbody HJ, Dennison EM, & Cooper C (2004). Does sarcopenia originate in early life? Findings from the Hertfordshire Cohort Study. Journal of Gerontology, Series A: Biological Sciences and Medical Sciences, 59, M930–M934. [DOI] [PubMed] [Google Scholar]
- Sen Amartya. (1980). Equality of What? In McMurrin SM (Ed.), The tanner lectures on human values (Vol. 1). Salt Lake City: University of Utah Press. [Google Scholar]
- Shen Y (2014). Community building and mental health in mid-life and older life: Evidence from China. Social Science and Medicine, 107, 209–216. [DOI] [PubMed] [Google Scholar]
- Shorrocks AF (1980). The class of additively decomposable inequality measures. Econometrica, 48(3), 613–625. [Google Scholar]
- Shorrocks A (2013). Decomposition procedures for distributional analysis: A unified framework based on the Shapley value. J Econ Inequal, 11(1), 99–126. [Google Scholar]
- Simmonds SJ, Syddall HE, Westbury LD, Dodds RM, Cooper C, & Sayer AA (2015). Grip strength among community-dwelling older people predicts hospital admission during the following decade. Age and Ageing, 44, 954–959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon D (2016). Does early life exposure to cigarette smoke permanently harm childhood welfare? Evidence from cigarette tax hikes. American Economic Journal: Applied Economics, 8(4), 128–159. [Google Scholar]
- Smith J (2009). Reconstructing childhood health histories. Demography, 46(2), 387–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonnega A, Faul J, Ofstedal M, Langa K, Phillips J, & Weir D (2014). Cohort profile: The health and retirement study (HRS). International Journal of Epidemiology, 43, 576–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stowasser T, Heiss F, McFadden D, & Winter J (2014). Understanding the SES gradient in health among the elderly: The role of childhood circumstances. In Wise DA (Ed.) NBER book discoveries in the economics of aging, pp. 187–219. [Google Scholar]
- Strauss J, Witoelar F, Meng Q, Chen X, Zhao Y, Sikoki B, et al. (2018). Cognition and SES relationships among the mid-aged and elderly: A comparison of China and Indonesia. National Bureau of Economic Research Working Paper 24583. [Google Scholar]
- Tang S, Meng Q, Chen L, Bekedam H, Evans T, & Whitehead M (2008). Tackling the challenges to health equity in China. The Lancet, 372(9648), 25–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomasetti C, Li L, & Vogelstein B (2017). Stem cell divisions, somatic mutations, cancer etiology, and cancer prevention. Science, 355, 1330–1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trannoy A, Tubeuf S, Jusot F, & Devaux M (2010). Inequality of opportunities in Health in France: A first pass. Health Economics, 19, 921–938. [DOI] [PubMed] [Google Scholar]
- Turvey CL, Wallace RB, & Herzog AR (1999). A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. International Psychogeriatrics, 11(2), 139–148. [DOI] [PubMed] [Google Scholar]
- United Nations Department of Economic and Social Affairs Population Division. (2015). World Population Ageing 2015 (ST/ESA/SER.A/390).
- Venkataramani A (2012). Early life exposure to Malaria and cognition in Adulthood: Evidence from Mexico. Journal of Health Economics, 31(5), 767–780. [DOI] [PubMed] [Google Scholar]
- Venkataramani A, Brigell R, O’Brien R, Chatterjee P, Kawachi I, & Tsai A (2016). Economic opportunity health behaviours and health outcomes in the USA: A population-based cross-sectional study. Lancet Public Health, pp. 18–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wendelspiess Chávez Juárez F, & Soloaga I (2014). Iop: Estimating ex-ante inequality of opportunity. Stata J, 14(4), 830–846. [Google Scholar]
- WHO. (2000). A life course approach to health. https://www.who.int/ageing/publications/lifecourse/alc_lifecourse_training_en.pdf.
- Xie Y, & Zhou X (2014). Income inequality in today’s China. Proceedings of the National Academy of Sciences of the United States of America, 111(19), 6928–6933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang D (1999). Urban-biased policies and rising income inequality in China. American Economic Review, 89(2), 306–310. [Google Scholar]
- Yang Y, & Eriksson T (2010). Inequality of opprtunity and income inequality in nine Chinese provinces, 1989–2006. China Economic Review, 21(4), 607–616. [Google Scholar]
- Zeng Y, Gu D, & Land KC (2007). The association of childhood socioeconomic conditions with healthy longevity at the oldest-old ages in China. Demography, 44, 497–518. [DOI] [PubMed] [Google Scholar]
- Zhang Z, Gu D, & Hayward M (2008). Early life influences on cognitive impairment among oldest old Chinese. Journal of Gerontology, Series B: Psychological Sciences and Social Sciences, 63(1), S25–S33. [DOI] [PubMed] [Google Scholar]
- Zhang X, & Kanbur R (2005). Spatial inequality in education and health care in China. China Economic Review, 16(1), 189–204. [Google Scholar]


