Abstract
Background
The COVID-19 pandemic necessitated the adoption of telemental health (TMH). Pre-pandemic, clinicians had voiced many TMH concerns, but these had not been investigated with respect to autism spectrum disorder (ASD) even with it being known that there are distinct ASD-associated challenges for in-person mental health interventions.
Method
A convenience sample of (n = 55) clinicians completed an online survey regarding their perspectives of adopting TMH interventions in ASD, with closed- and open-answered questions. Quantitative and qualitative data were analysed descriptively/inferentially and via Content Analysis, respectively.
Results
Multiple clinicians endorsed each TMH challenges/barrier previously identified as concerns in the non-ASD literature. However, overall levels of concern over challenges/barriers were low, and challenges were more likely to be predicted than experienced and considered to be case/presentation specific. Challenges that were considered ASD-specific included the exacerbation of those associated with in-person delivery in ASD, alongside difficulties with trust and appropriate remote social behaviour. On average, clinicians indicated a preference for 50% TMH interventions post-pandemic. Clinicians’ perceived technological competence and extent of professional experience with ASD were not significantly associated with levels of concern, nor number of experienced challenges, with TMH interventions in ASD.
Conclusion
In support of the existing TMH literature, challenges/barriers were more likely to be predicted than experienced and were considered to be case/presentation-specific, though this may be more variable in ASD owing to the well-established marked heterogeneity in this population. Remote provision of interventions exacerbated in-person ASD-associated challenges, as predicted, but clinician-level factors appeared not to impact TMH perceptions.
Keywords: Telepsychiatry, ASD, Telehealth, Mental health interventions
1. . Introduction
Autism spectrum disorder (ASD) is a lifelong neurodevelopmental disorder. It is characterised by impairments in social interaction and communication, and the presence of repetitive and restricted behaviours/interests (American Psychiatric Association APA, 2013). Prevalence rates of mental health disorders in ASD are disproportionality high (70–80%, Lever & Geurts, 2016; Simonoff et al., 2008) and there are ASD-specific challenges in their treatment. These principally include effectively adapting treatment for autistic individuals (e.g. using visual-concrete materials), along with frequent misconceptions and stigmatisation surrounding autism and mental health problems amongst clinicians (e.g. Crane, Adams, Harper, Welch, & Pellicano, 2019; Lipinski, Boegl, Blanke, Suenkel, & Dziobek, 2021; National Institute for Health & Care Excellence NICE, 2013).
Ensuring mental health interventions and service provision are effective for autistic individuals thus ought to be a research priority, as voiced by the autistic community (Cusack & Sterry, 2016). Adapted versions of mental health interventions and service models for autistic individuals do show promise, though further work is required (e.g. see review by Dickson et al., 2021). Recently, mental health services have been delivered remotely to help control the spread of COVID-19 (Kuzman et al., 2021), which may have impacted the effectiveness of interventions, and will likely persist. The remote provision of health services is referred to as telemedicine or telehealth and involves delivering services at-a-distance, rather than in-person, using telecommunication technologies such as videoconferencing (World Health Organisation, 2009). This paper uses the term ‘telemental health’ (TMH) when referring to the remote provision of mental health services in particular (Di Carlo et al., 2021). The effectiveness and implementation of TMH interventions have been a well-documented concern amongst clinicians that has persisted through the pandemic, especially (though not exclusively) for certain clinical presentations that include ASD (e.g. see reviews by Appleton et al., 2021; Cowan, Mckean, Gentry, & Hilty, 2019; Siegel, Zuo, Moghaddamcharkari, McIntyre, & Rosenblat, 2021). A review of pandemic studies on clinicians’ views of TMH service delivery identified universal implementation barriers that included technological difficulties; issues surrounding safety, privacy and confidentiality; therapeutic delivery; and working alliance (Siegel et al., 2021).
Pre-pandemic, TMH concerns amongst clinicians and service-providers were vast and were considered as barriers to routine implementation (Chakrabarti, 2015, Cliffe et al., 2020, Cowan et al., 2019). Meta-analyses of numerous pre-pandemic intervention studies have however indicated that TMH interventions are non-inferior to in-person interventions(Batastini, Paprzycki, Jones, & MacLean, 2021; Drago, Winding, & Antypa, 2016; Kummervold, Johnsen, Skrøvseth, & Wynn, 2012; Norwood, Moghaddam, Malins, & Sabin‐Farrell, 2018, pp. 2315), though not consistently for working alliance. This research area had been comparatively neglected in the autism field pre-pandemic; TMH concerns had not been investigated with reference to autistic individuals, and particularly few studies had investigated direct (i.e. as opposed to solely parental/supporter or parent-mediated) TMH (or telemedicine) interventions for autistic individuals. It is herein that the focus of the present paper resides. Because this study commenced early during the pandemic (i.e. preceding the existence of related pandemic publications), we set out to specifically investigate whether TMH concerns already identified from surveying the pre-pandemic literature (e.g. surrounding effective communication, engagement, and rapport, Cowan et al., 2019) apply to the delivery of TMH interventions directly to autistic individuals, according to clinicians. Clinicians were further asked open-ended questions about their experiences because it was predicted that some TMH challenges and considerations may be ASD-specific, since this is true for conventional (i.e. in-person) mental health interventions, as aforementioned.
Existing intervention studies of direct TMH (and telemedicine) interventions for autistic individuals do provide preliminary indication of efficacy, feasibility, and acceptability, but results are not readily transferable to clinical practice owing to key limitations (see reviews by Adams, Valmaggia, & Simonoff, 2021; Ellison, Guidry, Picou, Adenuga, & Davis, 2021; Knutsen et al., 2016; Sutherland, Trembath, & Roberts, 2018). These limitations include the samples lacking representativeness due to strict exclusion criteria (e.g. severe cases) and the risk of self-selection bias, coupled with the interventions not having been transdiagnostic nor implemented into routine care. Additionally, only two of these studies (i.e. Hepburn, Blakeley-Smith, Wolff, & Reaven, 2016; McCrae et al., 2021) used the most popular TMH tool in current clinical practice – videoconferencing - but the only challenges reported were mostly specific to family exposure sessions and had not been methodically investigated. Autism studies that have investigated the remote delivery (via videoconferencing) of direct psychological interventions not targeting mental health, but rather solely targeting functional skills, have likewise shown promise (e.g. Cihon et al., 2021; Ferguson et al., 2020; Ford, Wang, Koegel, Koegel, & Fedders, 2020; Nohelty, Bradford, Hirschfeld, Miyake, & Novack, 2021; Pollard, LeBlanc, Griffin, & Baker, 2021). These were conducted before and since the pandemic started, and the only challenges reported surrounded technological issues, at-home distractions, instructional control, and the need for parental support for some individuals.
Methodical investigation of clinicians’ experiences and opinions of routine service delivery of direct TMH interventions to autistic individuals is therefore important. Whilst not a central focus, two online surveys did investigate this during the pandemic in health and social care professionals (i.e. study by Spain et al., 2021) and in graduate-trained therapists in social work, psychology, or behaviour analysis (i.e. study by Southey & Stoddart, 2021). The challenges identified largely overlapped with those in the existing TMH literature, although they were fewer in number and included additional challenges that are likely to be associated with ASD (e.g. using tactile resources) and the impact of COVID-19 circumstances.
Both ASD studies (i.e. Southey & Stoddart, 2021; Spain et al., 2021) obtained telemedicine views more broadly and only via one or three questions that were embedded in a longer questionnaire which instead focused on the mental health impact of the pandemic. In addition, the questions were open-ended and so relied upon the participants’ ability to recollect challenges/benefits, and some participants in Spain et al.’s (2021) study were researchers rather than clinicians within routine services. For these reasons, TMH intervention challenges/benefits for autistic individuals may not have been fully identified.
Lastly, to best ensure methods are directly capturing the usefulness of TMH interventions for autistic individuals, individual and contextual factors ought to be considered. It has previously been demonstrated that clinicians’ knowledge and attitudes towards technology can facilitate or hinder its use (Greenhalgh et al., 2017, Hollis et al., 2017). Further, evidence indicates that reduced sense of efficacy as a clinician, clinical competencies, and technological competencies can reduce clinicians’ satisfaction with telemedicine (Cowan et al., 2019, Donovan et al., 2015). To-date, no ASD studies have investigated this.
The present study thus aimed to achieve the following objectives. (1) Identify the proportion of mental health interventions delivered remotely versus in-person to autistic adolescents/adults and the technologies used before and during the pandemic. (2) Understand clinicians’ attitudes, perceptions and experiences of delivering direct TMH interventions to autistic adolescents/adults, identifying any perceived and experienced barriers, facilitators and benefits including whether participants would endorse those already identified in the (pre-pandemic) TMH literature. (3) Test whether reduced levels of perceived technological competence and reduced extent of professional experience with autistic service-users predict an increase in the number of barriers experienced and level of concern regarding TMH interventions in this patient group.
2. Methods
The methodology was mixed, preregistered (Adams, Adamo, Hollocks, Valmaggia, & Simonoff, 2020), and is further detailed and justified in Supplementary File 1. Methods and results are reported using the Checklist for Reporting Results of Internet E-surveys (CHERRIES, Eysenbach, 2004, in Supplementary File 2) and a Checklist of Good Practice in the Conduct and Reporting of Survey Research (Kelley, Clark, Brown, & Sitzia, 2003, in Supplementary File 3). The study received ethical clearance from King’s College London (KCL; Minimal Risk Registration Number: MRSP-19/20–20653) and underwent KCL’s Data Protection Registration.
2.1. Participants
2.1.1. Recruitment and eligibility criteria
A convenience sample of 55 clinicians participated in the online ‘open’ survey - recruited using snowball sampling. All authors distributed recruitment messages via social and professional networks. The recruitment period was from August 2020 to April 2021. The eligibility criteria were provided on the information sheet on the first page of the online survey. Participants were required to be a qualified clinician or a clinician-in-training with experience of delivering mental health interventions directly, remotely or otherwise, to adolescents/adults with an ASD diagnosis within UK-based mental health services. Applicable mental health interventions included psychological, psychosocial, and pharmacological interventions, but pharmacological interventions needed to have involved regular contact directly with the patient to review the medication which must have been used to target mental health. Participants were not required to have delivered mental health interventions during the COVID-19 pandemic to be eligible.
2.1.2. Response rates
Of the 229 individuals that viewed the information sheet (i.e. the view rate), 106 (46.3%) consented to participate (i.e. the participation/recruitment rate), and 55 (52.0% of consenting participants, i.e. completion rate) completed the study. Of the completers, five (9.1%) were excluded from the quantitative analysis (i.e. ratings were excluded but valid demographic and qualitative responses were retained) due to failing an attention check. The formulae used to compute these rates are provided in Supplementary File 2. The attention check consisted of a mid-questionnaire item asking participants to “Please rate agree here” with a 5-point Likert scale identical to that used for surrounding items (“Strongly disagree, Disagree, Neither Agree nor Disagree, Agree, Strongly Agree”) - participants failed if they did not select ‘Agree’. This item was forced choice, and if left unanswered the participant could not proceed with remaining items and consequently could not submit the questionnaire. The sample’s demographic and professional information is provided in Table 1.
Table 1.
Clinicians’ demographic and professional characteristics (n = 55).
| Information | Categories | Sub-categories present | Number of participants per sub-category | Percentage (%) of participants per sub-category |
|---|---|---|---|---|
| Demographics | Age | 18–24 years | 1 | 1.8 |
| 25–39 years | 36 | 65.5 | ||
| 40–60 years | 12 | 21.8 | ||
| 60 + years | 2 | 3.6 | ||
| Gender | Female | 40 | 72.7 | |
| Male | 11 | 20.0 | ||
| Primary role service | Sector | Public | 43 | 78.2 |
| Private | 5 | 9.1 | ||
| Both sectors | 1 | 1.8 | ||
| Third sector | 1 | 1.8 | ||
| Age group worked with | Children/adolescents | 36 | 65.5 | |
| Adults of a working age | 26 | 47.3 | ||
| Older adults | 10 | 18.2 | ||
| Multiple | 16 | 29.1 | ||
| Primary Service type | Specialist* | 19 | 34.5 | |
| Non-specialist | 31 | 56.4 | ||
| Role | Voluntary | No | 51 | 92.7 |
| Profession | Clinical psychologist*A | 19 | 35.0 | |
| Trainee Clinical Psychologist | 14 | 25.5 | ||
| Psychiatrist | 4 | 7.3 | ||
| Trainee Psychiatrist | 2 | 3.6 | ||
| Assistant Psychologist | 2 | 3.6 | ||
| CBT therapist | 2 | 3.6 | ||
| Graduate practitioner*B | 2 | 3.6 | ||
| Mental health nurse*C | 2 | 3.6 | ||
| Other*D | 4 | 7.3 | ||
| When present role started | 5 + years ago | 17 | 30.9 | |
| Less than 5 years | 20 | 36.4 | ||
| Less than a year ago | 8 | 14.5 | ||
| Since lockdown started | 6 | 10.9 | ||
| Duration per week in role | 2–34 h (i.e. part-time) | 19 | 35.0 | |
| 35 + hours (i.e. full time) | 30 | 55.0 | ||
| Mental health intervention(s) delivered | Type of intervention delivered | Psychological | 41 | 74.5 |
| Pharmacological | 6 | 10.9 | ||
| Psychosocial | 3 | 5.5 | ||
| Psychoeducational | 1 | 1.8 | ||
| Precise intervention delivered | CBT (including adapted) | 25 | 45.5 | |
| Systemic | 8 | 14.5 | ||
| Other (e.g. counselling, eye movement desensitisation therapy, and schema therapy). | 7 | 13.0 | ||
| Psychoeducation | 5 | 9.1 | ||
| Acceptance and Commitment therapy | 5 | 9.1 | ||
| Compassion-Focused therapy | 5 | 9.1 | ||
| Medication review | 4 | 7.3 | ||
| Behavioural interventions (e.g. Positive Behaviour Support) | 4 | 7.3 | ||
| Dialectical behavioural therapy | 3 | 5.5 | ||
| Narrative | 2 | 3.6 | ||
| Multiple types | 22 | 40.0 | ||
| Target of interventions | Anxiety (including social anxiety, generalised anxiety disorder, obsessive compulsive disorder, health anxiety, post-traumatic stress disorder, and vomit phobia) | 21 | 38.2 | |
| Depression or low mood | 12 | 21.8 | ||
| Other*E | 12 | 21.8 | ||
| Transdiagnostic | 9 | 16.4 | ||
| Emotional regulation or literacy | 9 | 16.4 | ||
| Multiple targets specified | 21 | 38.2 | ||
| ASD-specific clinical experience | Specialist ASD service | Yes | 28 | 50.9 |
| No | 22 | 40.0 | ||
| Years working with autistic service-users | Less than a year | 7 | 12.7 | |
| 1–9 years | 26 | 47.3 | ||
| 10–19 years | 11 | 20.0 | ||
| 20 + years | 8 | 15.0 | ||
| Number of autistic service-users worked with | 2–10 | 7 | 12.7 | |
| 11–20 | 3 | 5.5 | ||
| 21–49 | 10 | 18.2 | ||
| 50 + | 30 | 54.5 | ||
| General clinical experience | Years working in mental health services | Less than a year | 0 | 0 |
| 1–9 years | 33 | 60.0 | ||
| 10–19 years | 9 | 16.4 | ||
| 20 + years | 9 | 16.4 | ||
| Number of non-autistic service-users worked with | 1 | 1 | 1.8 | |
| 2–10 | 18 | 32.7 | ||
| 11–20 | 8 | 14.5 | ||
| 21–49 | 7 | 12.7 | ||
| 50 + | 20 | 36.4 |
Notes. The proportions presented are those of completers only, and non-responses per category varied between 1.8% and 10.9% (i.e. 1–6 participants) due to either skipping the questionnaire or skipping the questions (all items except those in the inferential statistics optional to reduce participant burden). Intervention sub-categories are not mutually exclusive. Percentages rounded to 1d.p. *Provided inSupplementary File 5. *A. 1 x clinical neuropsychologist. *B. mental health practitioner and psychological wellbeing practitioner. *C. 1 x mental health nurse was also a trainee CBT therapist. *D. Counselling Psychologist, Educational Psychologist, Occupational therapist, and Speech and language therapist. *E i.e. agitation/anger, adjustment, behavioural management and activation, assertiveness, psychoeducation, integrative, mood, perfectionism.
2.2. Procedure
After providing informed e-consent, participants were provided with a computer-generated pseudonym (for the opportunity to later withdraw data), and then proceeded with the questionnaire. To group participants for questionnaire branching (described in Table 2), participants were first asked “Have you delivered mental health interventions remotely (i.e. at a distance, including over-the-phone) to autistic service-users?” with four mutually exclusive response options: “Yes (before [the first] lockdown started)”, “Yes (since [the first] lockdown started)”, “Yes (before and since [the first] lockdown started)”, and “No”, and then “Which version of the questionnaire would you like to complete?” with two mutually-exclusive response options “Brief (5 min)” and “Full (10–20 min)”. The content in square brackets was added during the second national lockdown. The remaining items are in Supplementary File 1. The brief version of the questionnaire omitted open-ended questions and questions referring to content denoted ‘Full’ in the results section.
Table 2.
Participant per Questionnaire Branch, including the Number of Participants who had Delivered Interventions Remotely to Autistic Individuals at each Specified Timepoint.
| Questionnaire version |
||||
|---|---|---|---|---|
| Brief | Full | Total | ||
| All participants: | 29 | 21 | 50 | |
| Delivery group | Timepoint relative to pandemic | |||
| Remote | Before only | 1 | 2 | 3 |
| Since only | 20 | 15 | 35 | |
| Before and since | 5 | 3 | 8 | |
| Total Remote: | 26 | 20 | 46 | |
| Never remote | 3 | 1 | 4 | |
Notes. Summing the corresponding cells above: 11 participants had delivered interventions remotely before the pandemic (5 of which filled out the full questionnaire), and 43 participants since (18 of which filled out the full questionnaire). This table excludes those 5 participants that failed the attention check, 1 of whom reported never having delivered interventions remotely.
2.3. Measures
The survey was built by the first author using a software platform (www.gorilla.sc). All participants accessed the survey via an anonymous link.
2.3.1. Questionnaire development
The first author developed the questionnaire. It was informed by related studies outside of ASD as equivalent ASD studies on TMH concerns did not exist at this timepoint in the pandemic (Cliffe et al., 2020, Glueckauf et al., 2018, Tonn et al., 2017, see Supplementary File 1) and piloted with the research team who suggested revisions. Items included telemedicine concerns and barriers, for TMH interventions in particular, identified by the first author from existing research (e.g. Cliffe et al., 2020; Cowan et al., 2019; Kruse et al., 2018; Stoll, Müller, & Trachsel, 2020) that broadly encapsulated the few challenges identified in the only ASD study that had tested direct TMH interventions at the time (Hepburn et al., 2016). Participants who had delivered mental health interventions remotely to autistic individuals were asked to indicate if they had experienced any of these challenges; all participants were asked to rate their level of concern against each challenge. In the full version, if a participant indicated they were concerned about a specified challenge, they were asked if the challenge can be addressed and, if so, how so. Using a tick-box approach, these participants were also asked to identify whether they needed any further training or guidance to address any of the challenges. Further, participants in the full questionnaire were asked to outline any ASD-specific challenges for TMH intervention delivery, describe any perceived impact of COVID-19 on TMH intervention views, and leave any comments. All participants were asked to provide key demographic and professional information (questions are provided in Supplementary File 4).
2. .4. Design
The study uses a cross-sectional design. Confirmatory hypotheses are shown in Table 3 alongside how variables were operationalised.
Table 3.
Main Hypotheses and Variables.
| Hypothesis | Predictor variables | Outcome variable |
|---|---|---|
| 1. 'Technological Competence' and 'Professional Experience' will be negatively associated with 'Concern with direct TMH interventions in ASD'. | 'Technological competence' (Likert scale: 0 = novice; 10 = expert), ordinal and self-rated | 'Concern with direct TMH interventions in ASD' is a composite score. It has been computed by summing the self-reported ratings on the 5-point Likert scale (0 = not at all concerned; 5 extremely concerned) by each intervention aspect the participant indicates is a potential challenge. The total concern score can range from 0 (i.e. no concern) to 140 (i.e. very concerned about all possible challenges). |
| Professional experience, self-estimated number of autistic service users the participant reported having offered mental health interventions to in their career(s) (5 levels: 1; 2–10; 11–20; 21–49; Over 50). | ||
| 2. Levels of 'Technological Competence' and 'Professional Experience' will be negatively associated with the 'Number of Experienced Barriers' | As above | 'Number of experienced barriers' consists of challenges that participants (who have been delivering interventions remotely) indicate they have experienced (using a tick-box approach), summed with the number of intervention aspects (e.g. patient rapport) rated as ‘worse’ or ‘much worse’ due to remote delivery. |
2.5. Content analysis
Content analysis of responses to open-ended questions was preregistered a priori, and details about the analytical strategy and purpose are provided there (Adams et al., 2020). Example questions are provided as follows (note, the wording was altered based on previous answers, including those in Table 2, see Supplementary File 1), and all referred to direct TMH intervention delivery to autistic individuals. “Outline any patient characteristics you believe reduced or increased the usefulness of remote mental health interventions”, and “Outline any ASD-specific challenges you have experienced or might expect remotely delivering mental health interventions”. The type of content analysis was conventional and qualitative (Hsieh & Shannon, 2005) with a manifest and inductive approach. This means coding categories were derived directly from the textual data and focused on ‘what has been said’ rather than what was ‘intended to be said’ (Bengtsson, 2016). It followed the procedures outlined in Bengtsson (2016) and Hsieh and Shannon (2005). A blind independent coder (author 5) analysed a randomly selected 10% of responses per qualitative question using the coding frame, and percentage agreement (i.e. an inter-coder reliability metric) was 92% with one discrepancy agreed as a basic oversight.
3. Results
As shown in Table 2, 92% (n = 46) of clinicians had delivered mental interventions remotely (and directly) to autistic individuals, and the majority (70%; n = 35) of clinicians had been delivering these interventions remotely only since the pandemic started. Pre-pandemic, delivery was thus predominately in-person or via phone call (see Table 4). Since the pandemic started, delivery was mostly via videocall with (on average) only a small proportion of in-person sessions. The same pattern was found for delivery not directly to autistic individuals (e.g. parental-mediated therapy or to neurotypical individuals). On average, clinicians showed preference for delivering approximately 50% of sessions in-person to autistic individuals post-pandemic.
Table 4.
Average Self-Reported Percentages (with Ranges) of each Delivery Mode used Before the Pandemic, Since the Pandemic Started, and preferred, directly for the Specified Client Groups.
 |
Notes. To participate, participants needed to have delivered a mental health intervention (directly) to at least 1 autistic individual. 1. Full = participants who completed the full version of the questionnaire (i.e. only this version included these questions, more details in Table 2). Rounding error likely as drop-down percentages were in intervals of 10. Higher numbers are in darker shades.
As shown in Table 5, the most commonly and frequently used TMH intervention tools (for direct delivery in ASD) used before lockdown were phone technologies. Apps and ‘other’ tools had not been used pre-pandemic. All telemedicine tools had been used since the pandemic, with the most common and frequent being videoconferencing. The tool with the most marked uptake due to the onset of the pandemic was videoconferencing. Mean helpfulness ratings for tools tended to be higher than before lockdown ratings. Tools rated as most helpful were videoconferencing and email.
Table 5.
Percentage of participants that reported using each tool before and after the pandemic, per usage frequency*, for delivering mental health interventions directly to autistic individuals (n = 21, Full1).
 |
Notes. ‘Every 6 months’ was not included as an option for since lockdown as data collection started too close to lockdown, participants had the option to comment here. Frequencies for never used include the 1 participant who had never delivered interventions remotely and filled out the full questionnaire. No participants used the telemedicine tool ‘Chat room or instant messaging’ at any timepoint. Other tools specified only included paper. Higher numbers are in darker shades. 1. Full = participants who completed the full version of the questionnaire (i.e. only this version included these questions; more details in Table 2).
As can be seen in Table 6, most clinicians felt comfortable and confident delivering TMH interventions directly to autistic individuals and that they had organisational support, but not access to delivery resources, in particular prompt technological support. All clinicians agreed that hybrid delivery can be effective for autistic service-users, but views were mixed regarding the effectiveness of exclusive remote delivery and the necessity of live contacts. Most clinicians felt they understood the potential challenges of telemedicine, and some knowledge of the research but less so in ASD. TMH intervention satisfaction ratings tended to be higher since lockdown, with approximately half of clinicians satisfied and most clinicians indicated that COVID-19 may have impacted their satisfaction ratings.
Table 6.
The proportion of participants that rated each level of comfort, confidence, understanding, support, and knowledge for TMH interventions (n = 20 *, Full1).
 |
Notes. *1 full questionnaire participant with missing data for these (optional) items. For perceived effectiveness ratings only, an administrative error led to an extra Likert scale point, so categories had to be merged and the mid-point may thus be inflated. Higher numbers are in darker shades. *A ‘satisfied nor dissatisfied’. 1. Full = these are the participants that completed the full version, of which only one did not have experience of TMH.
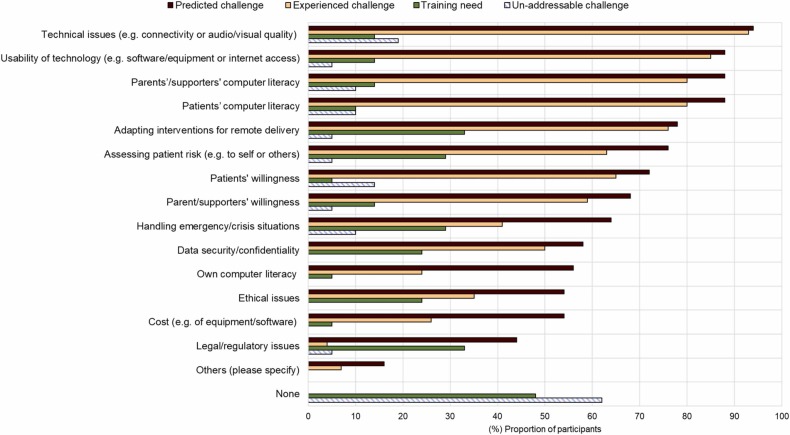
As can be seen in Fig. 1, the most commonly predicted and experienced TMH challenge, considered un-addressable by a minority of clinicians, was technical issues. This was followed by the usability of technology and computer literacy, but few clinicians considered these challenges un-addressable. Clinicians tended to consider all TMH challenges addressable, and to endorse very few challenges as training needs. All TMH challenges were more commonly endorsed as predicted than experienced, with this difference being most marked for legal/regulatory issues. No clinicians considered there to be no TMH challenges. On average, 10 of the 15 challenges were endorsed as predicted, eight as experienced, three as training needs, and one as un-addressable. Average concern ratings for challenges were low (in Supplementary File 5).
Fig. 1.
The proportion of participants (%) that endorsed each Telemental Health (TMH) challenge as predicted, experienced, a training need, or un-addressable. Notes. All participants were asked to endorse predicted challenges, only ‘remote’ participants were asked to endorse experienced challenges, and only the full (not brief) questionnaire asked if challenges were training needs or un-addressable (Table 2 shows participant groupings). Other challenges specified by 3 participants included disadvantaged families (resulting in reduced technological literacy and access), confidential spaces, and patient fatigue.
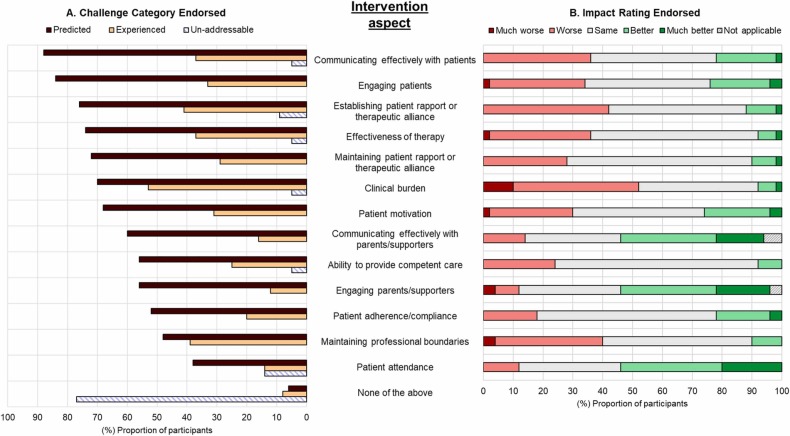
As before, most clinicians believed that the intervention aspects they considered potential challenges were addressable, and clinicians more commonly endorsed these as predicted than experienced (see Fig. 2). This difference was most marked for engaging and communicating with parents/supporters, though this will likely have been non-applicable to some clinicians (e.g. those supporting adults). On average, 8/13 intervention aspects were endorsed as predicted challenges, four as experienced challenges, and none as un-addressable challenges. Mean concern ratings for each aspect tended to be low. All aspects received both positive and negative ratings. Aspects were most commonly rated the same, aside from patient attendance, communicating effectively with patients, and clinical burden which also received the highest proportion of negative ratings. Aspects were more likely to be rated as ‘worse’ than ‘better’ but most rarely as 'much worse'. Aspects most commonly rated positively were engaging and communicating effectively with parents/supporters and patient attendance, though some clinicians rated these aspects negatively.
Fig. 2.
The proportion of participants (%) that endorsed each intervention aspect as a predicted, an experienced, or an un-addressable challenge (Chart A) and as ‘much worse’, ‘worse’, ‘same’, ‘better’ or ‘much better’ remotely (Chart B, i.e. impact ratings). Notes. All participants were asked to endorse predicted challenges and impact ratings, only ‘remote’ participants were asked to endorse experienced challenges, and only the full (not brief) questionnaire asked if challenges were un-addressable (Table 2 shows participant groupings). Training needs are captured in Figure 1.
3.1. Confirmatory quantitative analysis
Spearman’s rank order correlation was used to test all four hypotheses (see Table 2), and no statistically significant relationships were found at α = 0.05 (see Supplementary File 5).
3.2. Exploratory analysis: qualitative content analysis
The coding categories are italicised. According to clinicians, COVID-19 impacted their satisfaction with remote delivery owing to it having a perceived psychological impact on service-users (e.g. due to change in routine and increased health anxiety) and its altering of the session’s logistics, quality and environment. Equally, TMH intervention experiences were considered case/presentation specific. Spontaneously identified TMH intervention challenges included working alliance and content coverage (i.e. identified when asked about experiences in general). Equivalent, spontaneously identified benefits included perceptions that engagement was improved for some individuals (though worsened for others), atypical social interactions being more accepted online, a perceived reduction in social cues for some, and remote delivery fulfilling certain needs/preferences (e.g. use of structured and visual materials and being in a familiar environment). As such, some individuals were considered to prefer remote delivery. After endorsing potential challenges (see Fig. 1 and 2), clinicians offered some suggestions for addressing these, including pooling resources/tools/knowledge as a team, drawing on families/YPs’ experiences, and offering in-person or hybrid delivery. Experienced challenges that were considered to be ASD-specific/associated included intervention aspects (e.g. engaging clients), avoidance of social situations enforcing lack of social demand or practice of social skills, and socially inappropriate behaviour remotely. These overlapped with predicted challenges considered to be ASD-specific/associated that also included difficulties with video-calling and technology. Characteristics considered to have reduced the usefulness of remote delivery included diagnostic co-occurrences, hyperactivity and oppositionality, with those predicted to further including learning, communication and cognitive related abilities. Technological affinity and being a young person were identified as characteristics perceived to increase the usefulness of remote delivery, and some believed it was beneficial for those with social communication impairments and ADHD. Contrariwise, the cardinal symptoms of ADHD were considered by others to reduce the usefulness of remote delivery (e.g. hyperactivity causing someone not to stay on screen), although this was often mentioned with respect to severe and unmedicated ADHD. Generally, clinicians did not provide reasoning for their responses that might have allowed for seemingly conflicting views to be unified. Characteristics predicted to enhance remote delivery were much the same as those experienced, but also included engaged carers, familiarity with online education, and high intelligence. The full categorical framework is in Supplementary File 6.
4. Discussion
The is the first study to focus on clinicians’ views and experiences concerning the service delivery of (direct) TMH interventions to autistic individuals. It was carried out during the COVID-19 pandemic. Few clinicians in the sample were delivering mental health interventions remotely before the pandemic, whereas since the pandemic started in-person delivery was rare. This has been demonstrated outside of ASD (Kuzman et al., 2021) but not yet investigated in an ASD study. Of the tools used, email and videoconferencing were the only tools to receive the highest usefulness ratings for both before and since the pandemic.
This study also marks the first to establish the applicability of TMH intervention concerns identified from non-ASD research with reference to autistic individuals. The TMH concerns captured in questionnaire items had been identified by non-ASD clinicians (pre-pandemic due to the study's timepoint; e.g. Chiauzzi, Clayton, & Huh-Yoo, 2020; Cliffe et al., 2020; Cowan et al., 2019; Kruse et al., 2018; Stoll et al., 2020), aside from those relating to parental/supporter involvement which were included for being relevant in ASD (Perihan et al., 2020). All were endorsed as predicted and/or experienced by multiple participants in the present study. Clinicians in pandemic studies on the service delivery of TMH interventions commonly report the same concerns as in pre-pandemic studies. That is, concerns mostly surrounding technological difficulties; safety, privacy and confidentiality; therapeutic delivery; and working alliance (see review by Siegel et al., 2021). This was true of participants in the present study even though it was ASD-specific. However, concerns over communication appeared relatively more commonplace - possibly reflecting the social communication difficulties that characterise ASD (American Psychiatric Association APA, 2013). In line with this proposition, clinicians in pandemic studies have raised particular concerns about the suitability of TMH service delivery for autistic individuals (Appleton et al., 2021, Siegel et al., 2021). The perceived TMH intervention challenges, considerations, and benefits potentially associated with ASD, and those most frequently reported in the present study will now be discussed against existing literature, followed by a discussion of the implications of these findings.
4.1. ASD-associated challenges, considerations, and benefits
Unlike prior ASD studies that have likewise investigated the delivery of direct remote interventions in routine services via an online survey (conducted during the pandemic; i.e. Southey & Stoddart, 2021; Spain et al., 2021), the ability of clinicians to recall challenges in open-ended questions was not solely relied upon, which likely explains why more challenges were identified. Open-ended questions were included before the endorsement of challenges however, in order to identify those of salience. In support of these prior ASD studies, principal challenges encompassed working alliance (e.g. building relationships/rapport and engagement), content coverage (e.g. exposure work and avoidance of social situations), remote interaction fatigue, and clinical burden.
The present study is further distinguishable from these prior ASD studies (i.e. Southey & Stoddart, 2021; Spain et al., 2021) in that it focused on TMH (as opposed to telemedicine more broadly) and participants were asked to rate their level of concern over challenges and outline any considered to be ASD-specific. The latter included the exacerbation of those associated with in-person delivery in ASD (e.g. building rapport, supporting understanding, and the need for visual-tactile resources; Cooper, Loades, & Russell, 2018; National Institute for Health & Care Excellence NICE, 2013) alongside privacy concerns - challenges found by prior studies on direct TMH and telemedicine interventions in ASD (including intervention studies; i.e. Cihon et al., 2021; Hepburn et al., 2016; Kalvin et al., 2021; Loveland, 2020; McCrae et al., 2021; Southey & Stoddart, 2021; Spain et al., 2021), but also difficulties with trust and appropriate remote social behaviour. It must be mentioned, however, that typically fewer than half of clinicians reported having experienced these, though the majority endorsed them as possible, and levels of concern were low. This may be attributable to TMH intervention experiences being case/presentation specific, as noted by clinicians in the present study, with levels of complexity (e.g. diagnostic co-occurrences) and specific needs/difficulties impacting its usefulness. The possibility of such variability has only been a recognised concern of TMH interventions outside of ASD (e.g. Simms et al., 2011) but may be pronounced in ASD as clinical presentations are highly heterogenous in this population (Grzadzinski, Huerta, & Lord, 2013).
The perceived inter-individual variability in TMH intervention experiences potentially explains why impact ratings for remote delivery were consistently mixed across participants. It must be acknowledged here that this finding cannot be contrasted with either non-ASD or other ASD studies since neither have asked participants to rate whether aspects of interventions are better remotely (i.e. only worse) and have tended to omit concern ratings. Patterns in findings could be observed across the present sample, however. Participants were more likely to rate intervention aspects (e.g. effectiveness) as ‘worse’ than ‘better’ remotely, and typically reported experiencing multiple challenges. Still, challenges tended to be considered un-concerning and addressable, and intervention aspects (e.g. effectiveness) were most commonly rated the same as in-person with a general preference for offering hybrid delivery. Further, certain aspects were rated as ‘better’ or ‘much better’ by approximately half of participants: engaging and communicating with parents/supporters, and patient attendance. The latter has been recognised as a benefit of remote delivery outside of ASD (e.g. Sugarman, Horvitz, Greenfield, & Busch, 2021), and the former is of importance as involving parents/supporters can improve treatment effectiveness in ASD (Perihan et al., 2020) and has been reported in an autism study of practitioners’ and families’ experiences of telemedicine during the pandemic (Johnsson & Bulkeley, 2021).
The benefits spontaneously reported by clinicians have been identified in the TMH intervention literature (e.g. Thomas et al., 2021), aside from that of atypical social interactions considered more accepted online. However, only the perceived benefit of remote delivery fulfilling certain needs/preferences (e.g. being in a familiar environment) appears to have been identified in the ASD-specific TMH intervention literature (e.g. Kalvin et al., 2021). This is perhaps surprising given that the benefits mostly relate to the social communication impairments that characterise ASD, and that some have been recognised with respect to digitally mediated communication by autistic individuals themselves (e.g. preferring this mode of communication due to a reduction in social stimuli; Hassrick, Holmes, Sosnowy, Walton, & Carley, 2021).
4.2. Commonly experienced and predicted challenges
It would seem unlikely that clinicians’ views of TMH interventions that were reported in the present study are attributable to the sample’s levels of technological competence and professional experience. This is suggested because the TMH intervention views reported broadly reflect findings from a range of samples outside of ASD (e.g. Connolly, Miller, Lindsay, & Bauer, 2020; Li et al., 2021; Sugarman et al., 2021), and because levels of technological competence and professional experience were not significantly associated with levels of concern nor number of experienced challenges/barriers.
These non-significant associations would appear to contradict previous findings (Cowan et al., 2019, Donovan et al., 2015, Greenhalgh et al., 2017, Hollis et al., 2017). On the other hand, this apparent contradiction in findings may be ascribed to this being the first ASD study to explore such relationships, such that ASD-associated factors may be impactful (e.g. pronounced heterogeneity in ASD, as aforementioned) that are discussed in more detail later. The difference may equally be ascribed to the various methodological differences (e.g. in the concepts measured and their operationalisation), and the potential biases introduced by the use of self-report in all studies including the present one. The non-significance of associations ought to be interpreted with caution, however, as confidence intervals for these coefficients were wide. Additionally, levels of self-reported concern with remote delivery were low, and self-reported technological competence and professional experience in ASD were high, such that there may have been floor and ceiling effects, respectively. However, the number of experienced barriers and professional experience did vary in the sample.
Another potential explanation for why the present study was not able to replicate findings from previous (albeit non-ASD) studies showing technological competence to impact perceptions of TMH (see review by Cowan et al., 2019; Donovan et al., 2015) can be derived by considering the characteristics of the technological challenges reported, which simultaneously hold the potential to elucidate another key finding. Specifically, the finding that the most commonly experienced challenges were technological - as found within and outside of ASD (e.g. Cowan et al., 2019; Southey & Stoddart, 2021; Spain et al., 2021) - even with the sample reporting high levels of technological competence. This is because technological challenges were rarely considered training needs and ‘own computer literacy’ was an uncommon challenge, with technical issues such as connectivity, the usability of technology (e.g. internet access), and patients’ computer literacy being more frequently endorsed as technological challenges. Furthermore, half of participants reported not having access to prompt technological support - a barrier reported by other pandemic studies (Juan et al., 2021, Spain et al., 2021). These findings point towards another potential explanation for why the present study may have not been able to replicate past findings. That is, telemedicine tools (e.g. videoconferencing software) have become more user-friendly and used more frequently, especially during recruitment in this study due to the presence of COVID-19 related restrictions.
In a similar vein, it is perhaps the case that both professional experience and technological competence are of lesser importance than TMH experience and knowledge, particularly in ASD due to treatment complexities. The challenge most frequently identified as a training need and frequently as an experienced challenge was that of adapting interventions for remote delivery. As found by Kalvin et al. (2021) and Spain et al. (2021), participants reported that ASD-associated difficulties played a role here, such as verbal over-reliance and generalisation of coping skills. Since ensuring mental health interventions are effectively adapted for autistic individuals is a research priority (Cusack & Sterry, 2016), and only a few preliminary studies have tested direct TMH interventions in ASD (e.g. see reviews by Adams et al., 2021; Sutherland et al., 2018), further research is needed to develop ASD-specific TMH intervention training and resources (to accompany broader guidance, e.g. Kalvin et al., 2021; Katharine et al., 2020; Pears Foundation, 2021). It could then be observed whether improved TMH knowledge improves attitudes and effectiveness, as found outside of ASD (McClellan, Florell, Palmer, & Kidder, 2020).
Relatedly, increased TMH usage and technological advances (e.g. in videoconferencing technologies), both of which were associated with pandemic-related restrictions, have been shown to be associated with fewer perceived barriers and concerns (Brooks et al., 2013, Connolly et al., 2020). This could explain why clinicians in the present study were more likely to endorse TMH intervention challenges as predicted than experienced, since this is likewise indicative of expectations regarding TMH being more negative than actual experiences. However, this difference was less marked for technology-related challenges which were commonly both experienced and predicted, and so the main reason clinicians were more likely to endorse TMH intervention challenges as predicted than experienced is perhaps because they are accounting for the aforementioned heterogeneity that is well-established in ASD. This reason could simultaneously account for why some (non-technological) challenges were rarely experienced. Indeed, as also aforementioned, participants did comment that TMH intervention experiences were case/presentation specific.
4.3. Limitations and future directions
The case/presentation-specific nature of TMH intervention experiences reported by clinicians in the present study ought to be the topic of future investigation, especially as it may be pronounced in ASD for reasons aforementioned. For now, it is difficult to determine which of the explanations for findings that have been proposed are most plausible without further research. Future studies might consider monitoring which autistic subpopulations most and least benefit from remote and/or hybrid delivery according to potentially impactful patient characteristics such as those identified by clinicians in the present study (e.g. levels of hyperactivity, oppositionality, intelligence, social communication impairment, and cognitive abilities), and according to ASD diagnostic status particularly as the non-ASD studies have not excluded on this basis - thus constraining comparisons with present findings. Indeed, a recent systematic review concluded that there is a need for more studies to explore the effectiveness of hybrid models for autistic individuals (Lamash, Little, & Hen-Herbst, 2022).
Further, autistic individuals’ views of direct TMH interventions ought to be obtained as service-users tend to view TMH more positively than clinicians (e.g. Hubley, Lynch, Schneck, Thomas, & Shore, 2016). A pandemic study (i.e. Johnsson & Bulkeley, 2021) on the adoption of telemedicine service delivery did find that both practitioners and autistic service-users generally reported high levels of satisfaction but - as in this study - found the experience to be challenging most owing to technical difficulties. However, views from service-users versus families/practitioners and for individual disciplines (across telemedicine) could not be easily ascertained from findings since they were combined. With respect to the importance of this latter caveat, a pandemic study (i.e. Ferguson, Jimenez-Muñoz, Feerst, & Vernon, 2021) on ASD specialist service delivery to families found that the magnitude of difference between caregivers’ satisfaction of in-person versus remote delivery varied across disciplines. Satisfaction ratings were significantly lower for the remote delivery of behavioural, speech/language, and occupational therapies compared to in-person, whereas this difference was non-significant for psychotherapy.
Future research in ASD and beyond may benefit from (1) testing technological and professional expertise (instead of self-report) in clinicians and the former in service-users, (2) using standardised methodologies, and (3) controlling for potential confounds such as individual characteristics of clinicians, patients, and families, intervention type and target, TMH experience and tools used. In the present study, these factors somewhat varied except interventions were mostly ‘adapted CBT’ delivered by psychologists for targeting anxiety, though this is a common intervention in ASD.
Inevitably, there is the confound of COVID-19 circumstances to consider as data was collected during the pandemic and only a handful of participants had delivered interventions remotely pre-pandemic, although such circumstances are set to continue and thus the applicability of present findings. Participants reported numerous respects in which COVID-19 influenced their experiences of TMH, including forced choice, changes to session equipment, and mental health impact. The latter of these has been investigated in other studies and may be marked in ASD (e.g. Spain et al., 2021). A limitation of this study is that it was cross-sectional and relied on retrospective self-report, and so future studies may consider longitudinal monitoring and manipulating key variables (as aforementioned) as well as directly testing efficacy. Lastly, owing to the limited albeit moderate sample size, inferential analyses were restricted and showed low precision. Nonetheless, this study provides a novel contribution to the literature and paves the way for future investigations of direct TMH interventions for autistic individuals which has received minimal research attention to-date.
4.4. Implications for practice
Findings have a number of implications for practice in the provision of mental health interventions for autistic individuals. Services might consider on an individual basis whether to continue offering remote delivery or a blend of in-person and remote delivery (i.e. hybrid delivery) to autistic individuals within and outside of COVID-19 circumstances, particularly via videoconferencing and email. This is for three main reasons: (1) clinicians tended to believe hybrid (though not solely remote) delivery could be effective in ASD, (2) clinicians showed a preference for offering hybrid delivery (including post-pandemic) for autistic individuals, and (3) levels of concern regarding remote delivery were low. Importantly, however, as highlighted by the clinicians, there are caveats and considerations. First and foremost, more TMH intervention research in ASD is needed (e.g. efficacy and effectiveness trials with representative samples, though preliminary studies show promise; Adams et al., 2021; Ellison et al., 2021). Secondly, experiences are likely to be case/presentation specific and so this ought to be factored in when considering service-users likelihood of benefitting from remote delivery. Thirdly, prompt technological support and more guidance and training for using telemedicine in ASD is required.
This third suggestion may help to address the TMH intervention challenges predicted and experienced, most of which were considered addressable and to require ongoing reflection and adjustment, with some also considered ASD-specific (e.g. engagement and building a relationship). Specific suggestions were provided by clinicians for addressing the TMH intervention challenges in ASD discussed. These included pooling TMH resources, tools and knowledge as a team, use of a therapy expectation guide for service-users, using interactive resources (e.g. instant messages with avatars, virtual games, and screen sharing), and allowing service-users to use the chat function and to turn their cameras off.
4.5. Conclusion
Overall, clinicians showed low levels of concern regarding delivering remote mental health interventions (i.e. TMH) directly to autistic individuals. The challenges experienced support the broader TMH literature, such as technical difficulties, and were more likely to be endorsed as predicted than experienced. TMH intervention experiences were considered case/presentation specific and may be more variable in ASD owing to the marked heterogeneity in clinical presentations within this population. Clinicians further identified challenges considered to be ASD-specific that included the exacerbation of ASD-associated challenges already seen in-person delivery, and appropriate remote social behaviour. Research and access to resources for TMH intervention delivery in ASD was an identified need that ought to be addressed in future work. These findings provide a novel contribution to the literature as they mark the first in-depth examination of remote mental health interventions in ASD.
CRediT authorship contribution statement
Lucy Adams: Conceptualisation, Methodology, Software, Formal analysis, Investigation, Data curation, Writing – original draft, Writing − review & editing, Visualization, Supervision, Project administration. Nicoletta Adamo: Conceptualisation, Methodology, Investigation, Writing − review & editing. Matthew Hollocks: Conceptualisation, Methodology, Investigation, Writing − review & editing. Lucia Valmaggia: Funding acquisition, Methodology, Investigation, Writing − review & editing. Aylana Brewster: Formal analysis, Investigation, Writing − review & editing. Jennifer Watson: Investigation, Data curation, Writing − review & editing. Maisie Krisson: Investigation, Writing − review & editing. Emily Simonoff: Funding acquisition, Methodology, Investigation, Writing − review & editing, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to acknowledge the clinicians who participated and helped to distribute the survey, members of the networks that helped to distribute the survey, and the funding bodies that provided financial support. Of the clinicians that helped, the authors would like to especially thank principal clinical psychologist Dr Kevin Tierney who also helped with conceptualisation and resources. LA was funded by a PhD studentship from the Psychiatry Research Trust (PRT, UK, Grant reference: 0c Valmaggia). ES, MH and LV acknowledge financial support from the National Institute for Health Research (NIHR) Biomedical Research Centre for Mental Health at South London and Maudsley NHS Foundation Trust and King’s College London (UK). The views expressed are those of the author(s) and not necessarily those of the PRT, NHS, the NIHR or the Department of Health. The authors can confirm that the funding bodies had no other role in the report.
Human and Animal Rights
The study received ethical approval from King’s College London (KCL; MRSP-19/20–20653) and underwent KCL’s Data Protection Registration to ensure compliance with the United Kingdom (UK) and European Union (EU) Data Protection laws including GDPR and the UK Data Protection Act 2018. Informed e-consent for participation and the publication of anonymous data was obtained from all included participants.
Research data is not available because this involved minimal risk ethical approval.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.rasd.2022.101956.
Appendix A. Supplementary material
Supplementary material
.
Supplementary material
.
Supplementary material
.
Supplementary material
.
Supplementary material
.
Supplementary material
.
Supplementary material
.
Supplementary material
.
References
- Adams L., Valmaggia L., Simonoff E. Technology-based assessments and treatments of anxiety in autistic individuals: systematic review and narrative synthesis. Review Journal of Autism and Developmental Disorders. 2021:1–25. doi: 10.1007/S40489-021-00275-6. [DOI] [Google Scholar]
- Adams L., Adamo N., Hollocks M.J., Valmaggia L., Simonoff E. Investigating clinicians’ attitudes, perceptions and experiences of delivering mental health interventions to autistic individuals during Covid-19. Open Science Framework. 2020 doi: 10.17605/OSF.IO/RUXV6. [DOI] [Google Scholar]
- American Psychiatric Association (APA) Diagnostic and Statistical Manual of Mental Disorders. 5th ed.., Author; Washington, DC: 2013. [Google Scholar]
- Appleton R., Williams J., Juan N.V.S., Needle J.J., Schlief M., Jordan H.…Johnson S. Implementation, adoption, and perceptions of telemental health during the COVID-19 pandemic: systematic review. Journal of Medical Internet Research. 2021;23(12) doi: 10.2196/31746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batastini A.B., Paprzycki P., Jones A.C.T., MacLean N. Are videoconferenced mental and behavioral health services just as good as in-person? A meta-analysis of a fast-growing practice. Clinical Psychology Review. 2021;83 doi: 10.1016/J.CPR.2020.101944. [DOI] [PubMed] [Google Scholar]
- Bengtsson M. How to plan and perform a qualitative study using content analysis. NursingPlus Open. 2016;2:8–14. doi: 10.1016/J.NPLS.2016.01.001. [DOI] [Google Scholar]
- Brooks E., Turvey C., Augusterfer E.F. Provider barriers to telemental health: obstacles overcome, obstacles remaining. Telemedicine and E-Health. 2013;19(6):433–437. doi: 10.1089/tmj.2013.0068. [DOI] [PubMed] [Google Scholar]
- Chakrabarti S. Usefulness of telepsychiatry: A critical evaluation of videoconferencing-based approaches. World Journal of Psychiatry. 2015;5(3):286. doi: 10.5498/wjp.v5.i3.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiauzzi E., Clayton A., Huh-Yoo J. Videoconferencing-Based Telemental Health: Important Questions for the COVID-19 Era From Clinical and Patient-Centered Perspectives. JMIR Mental Health. 2020;7(12):e24021. doi: 10.2196/24021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cihon J.H., Ferguson J.L., Lee M., Leaf J.B., Leaf R., McEachin J. Evaluating the cool versus not cool procedure via telehealth. Behavior Analysis in Practice. 2021;15:260–268. doi: 10.1007/S40617-021-00553-Z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cliffe B., Croker A., Denne M., Stallard P. Clinicians’ use of and attitudes towards technology to provide and support interventions in child and adolescent mental health services. Child and Adolescent Mental Health. 2020;25(2):95–101. doi: 10.1111/camh.12362. [DOI] [PubMed] [Google Scholar]
- Connolly S.L., Miller C.J., Lindsay J.A., Bauer M.S. A systematic review of providers’ attitudes toward telemental health via videoconferencing. Clinical Psychology: Science and Practice. 2020;27(2):e12311. doi: 10.1111/cpsp.12311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper K., Loades M.E., Russell A. Adapting psychological therapies for autism. Research in Autism Spectrum Disorders. 2018;45:43–50. doi: 10.1016/j.rasd.2017.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowan K.E., Mckean A.J., Gentry M.T., Hilty D.M. Barriers to Use of Telepsychiatry: Clinicians as Gatekeepers. Mayo Clinic Proceedings. 2019;94(12):2510–2523. doi: 10.1016/j.mayocp.2019.04.018. [DOI] [PubMed] [Google Scholar]
- Crane L., Adams F., Harper G., Welch J., Pellicano E. ‘Something needs to change’: Mental health experiences of young autistic adults in England. Autism. 2019;23(2):477–493. doi: 10.1177/1362361318757048. [DOI] [PubMed] [Google Scholar]
- Cusack J., Sterry R. Autism Top 10 Your Priorities. Autistica; London: 2016. https://www.autistica.org.uk/our-research/our-research/your-research-priorities [Google Scholar]
- Di Carlo F., Sociali A., Picutti E., Pettorruso M., Vellante F., Verrastro V.…di Giannantonio M. Telepsychiatry and other cutting edge technologies in Covid‐19 pandemic: bridging the distance in mental health assistance. International Journal of Clinical Practice. 2021;75(1) doi: 10.1111/IJCP.13716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickson K.S., Lind T., Jobin A., Kinnear M., Lok H., Brookman-Frazee L. A systematic review of mental health interventions for ASD: characterizing interventions, intervention adaptations, and implementation outcomes. Administration and Policy in Mental Health. 2021;48(5):857–883. doi: 10.1007/S10488-021-01133-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan C.L., Poole C., Boyes N., Redgate J., March S. Australian mental health worker attitudes towards cCBT: What is the role of knowledge? Are there differences? Can we change them? Internet Interventions. 2015;2(4):372–381. doi: 10.1016/J.INVENT.2015.09.001. [DOI] [Google Scholar]
- Drago A., Winding T.N., Antypa N. Videoconferencing in psychiatry, a meta-analysis of assessment and treatment. European Psychiatry. 2016;36:29–37. doi: 10.1016/J.EURPSY.2016.03.007. [DOI] [PubMed] [Google Scholar]
- Ellison K.S., Guidry J., Picou P., Adenuga P., Davis T.E. Telehealth and Autism Prior to and in the Age of COVID-19: A Systematic and Critical Review of the Last Decade. Clinical Child and Family Psychology Review. 2021;24(3):599–630. doi: 10.1007/s10567-021-00358-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet e-surveys (CHERRIES) Journal of Medical Internet Research. 2004;6(3) doi: 10.2196/JMIR.6.3.E34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson E.F., Jimenez-Muñoz M., Feerst H., Vernon T.W. Predictors of satisfaction with autism treatment services during COVID-19. Journal of Autism and Developmental Disorders. 2021:1–12. doi: 10.1007/s10803-021-05232-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson J.L., Majeski M.J., McEachin J., Leaf R., Cihon J.H., Leaf J.B. Evaluating discrete trial teaching with instructive feedback delivered in a dyad arrangement via telehealth. Journal of Applied Behavior Analysis. 2020;53(4):1876–1888. doi: 10.1002/JABA.773. [DOI] [PubMed] [Google Scholar]
- Ford K., Wang M., Koegel L.K., Koegel R.L., Fedders A. Use of a Videoconferencing Intervention and Systematic Hierarchy to Teach Daily Living Skills to Young Adults With Autism Spectrum Disorder. Journal of Positive Behavior Interventions. 2020;23(2):81–92. doi: 10.1177/1098300720921214. [DOI] [Google Scholar]
- Glueckauf R.L., Maheu M.M., Drude K.P., Wells B.A., Wang Y., Gustafson D.J., Nelson E.L. Survey of psychologists’ telebehavioral health practices: Technology use, ethical issues, and training needs. Professional Psychology: Research and Practice. 2018;49(3):205–219. doi: 10.1037/pro0000188. [DOI] [Google Scholar]
- Greenhalgh T., Wherton J., Papoutsi C., Lynch J., Hughes G., A’Court C.…Shaw S. Beyond adoption: A new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. Journal of Medical Internet Research. 2017;19(11) doi: 10.2196/jmir.8775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grzadzinski R., Huerta M., Lord C. DSM-5 and autism spectrum disorders (ASDs): an opportunity for identifying ASD subtypes. Molecular Autism. 2013;4(1):12. doi: 10.1186/2040-2392-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassrick E.M., Holmes L.G., Sosnowy C., Walton J., Carley K. Benefits and risks: a systematic review of information and communication technology use by autistic people. Autism in Adulthood. 2021;3(1):72–84. doi: 10.1089/AUT.2020.0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hepburn S., Blakeley-Smith A., Wolff B., Reaven J. Telehealth delivery of cognitive-behavioral intervention to youth with autism spectrum disorder and anxiety: A pilot study. Autism. 2016;20(2):207–218. doi: 10.1177/1362361315575164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollis C., Falconer C.J., Martin J.L., Whittington C., Stockton S., Glazebrook C., Davies B.E. Annual Research Review: Digital health interventions for children and young people with mental health problems -A systematic and meta-review. Journal of Child Psychology and Psychiatry. 2017;58(4):474–503. doi: 10.1111/jc. [DOI] [PubMed] [Google Scholar]
- Hsieh H.-F., Shannon S.E. Three approaches to qualitative content analysis. Qualitative Health Research. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- Hubley S., Lynch S.B., Schneck C., Thomas M., Shore J. Review of key telepsychiatry outcomes. World Journal of Psychiatry. 2016;6(2):269. doi: 10.5498/wjp.v6.i2.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnsson G., Bulkeley K. Practitioner and service user perspectives on the rapid shift to teletherapy for individuals on the autism spectrum as a result of COVID-19. International Journal of Environmental Research and Public Health. 2021;18(22):11812. doi: 10.3390/IJERPH182211812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juan N.V.S., Shah P., Schlief M., Appleton R., Nyikavaranda P., Birken M., Johnson S. Service user experiences and views regarding telemental health during the COVID-19 pandemic: a co-produced framework analysis. PLoS ONE. 2021;16(9):e0257270. doi: 10.1371/journal.pone.0257270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalvin C.B., Jordan R.P., Rowley S.N., Weis A., Wood K.S., Wood J.J., Sukhodolsky D.G. Conducting CBT for anxiety in children with autism spectrum disorder during COVID-19 pandemic. Journal of Autism and Developmental Disorders. 2021;51:4239–4247. doi: 10.1007/S10803-020-04845-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley K., Clark B., Brown V., Sitzia J. Good practice in the conduct and reporting of survey research. International Journal for Quality in Health Care. 2003;15(3):261–266. doi: 10.1093/INTQHC/MZG031. [DOI] [PubMed] [Google Scholar]
- Knutsen J., Wolfe A., Burke B.L., Hepburn S., Lindgren S., Coury D. A systematic review of telemedicine in autism spectrum disorders. Review Journal of Autism and Developmental Disorders. 2016;3(4):330–344. doi: 10.1007/s40489-016-0086-9. [DOI] [Google Scholar]
- Kruse C.S., Karem P., Shifflett K., Vegi L., Ravi K., Brooks M. Evaluating barriers to adopting telemedicine worldwide: A systematic review. Journal of Telemedicine and Telecare. 2018;24(1):4–12. doi: 10.1177/1357633X16674087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kummervold P.E., Johnsen J.A.K., Skrøvseth S.O., Wynn R. Using noninferiority tests to evaluate telemedicine and e-health services: systematic review. Journal of Medical Internet Research. 2012;14(5):e132. doi: 10.2196/JMIR.2169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuzman M.R., Vahip S., Fiorillo A., Beezhold J., Costa M.P., da, Skugarevsky O., Goorwod P. Mental health services during the first wave of the COVID-19 pandemic in Europe: Results from the EPA Ambassadors Survey and implications for clinical practice. European Psychiatry. 2021;64(1):E41. doi: 10.1192/J.EURPSY.2021.2215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamash L., Little L., Hen-Herbst L. Telehealth interventions to promote health and behavior-related outcomes in adolescents with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2022:1. doi: 10.1007/S10803-022-05440-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lever A.G., Geurts H.M. Psychiatric co-occurring symptoms and disorders in young, middle-aged, and older adults with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2016;46:1916–1930. doi: 10.1007/s10803-016-2722-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H., Glecia A., Kent-Wilkinson A., Leidl D., Kleib M., Risling T. Transition of mental health service delivery to telepsychiatry in response to COVID-19: a literature review. The Psychiatric Quarterly. 2021 doi: 10.1007/S11126-021-09926-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipinski S., Boegl K., Blanke E.S., Suenkel U., Dziobek I. A blind spot in mental healthcare? Psychotherapists lack education and expertise for the support of adults on the autism spectrum. Autism. 2021 doi: 10.1177/13623613211057973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loveland K.A. Research on Adults with ASD: Making Some Lemonade from the Lockdown Lemon. Autism Research. 2020;13(6):844–869. doi: 10.1002/aur.2329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClellan M.J., Florell D., Palmer J., Kidder C. Clinician telehealth attitudes in a rural community mental health center setting. Journal of Rural Mental Health. 2020;44(1):62–73. doi: 10.1037/rmh0000127. [DOI] [Google Scholar]
- McCrae C.S., Chan W.S., Curtis A.F., Nair N., Deroche C.B., Munoz M.…Mazurek M.O. Telehealth cognitive behavioral therapy for insomnia in children with autism spectrum disorder: A pilot examining feasibility, satisfaction, and preliminary findings. Autism. 2021;25(3):667–680. doi: 10.1177/1362361320949078. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence (NICE), 2013, Autism spectrum disorder in under 19s: support and management. Clinical guideline [CG170]. NICE. [PubMed]
- Nohelty K., Bradford C.B., Hirschfeld L., Miyake C., Novack M.N. Effectiveness of telehealth direct therapy for individuals with autism spectrum disorder. Behavior Analysis in Practice. 2021 doi: 10.1007/S40617-021-00603-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norwood C., Moghaddam N.G., Malins S., Sabin‐Farrell R. Working alliance and outcome effectiveness in videoconferencing psychotherapy: A systematic review and noninferiority meta‐analysis. Clinical Psychology & Psychotherapy. 2018;25(6):797–808. doi: 10.1002/c. [DOI] [PubMed] [Google Scholar]
- Pears Foundation New research and free guide: how to adapt mental health talking therapies for autistic children and adults. National Autistic Society. 2021 〈https://www.autism.org.uk/what-we-do/news/adapt-mental-health-talking-therapies〉 [Google Scholar]
- Perihan C., Burke M., Bowman-Perrott L., Bicer A., Gallup J., Thompson J., Sallese M. Effects of cognitive behavioral therapy for reducing anxiety in children with high functioning ASD: a systematic review and meta-analysis. Journal of Autism and Developmental Disorders. 2020;50:1958–1972. doi: 10.1007/s10803-019-03949-7. [DOI] [PubMed] [Google Scholar]
- Pollard J.S., LeBlanc L.A., Griffin C.A., Baker J.M. The effects of transition to technician‐delivered telehealth ABA treatment during the COVID‐19 crisis: A preliminary analysis. Journal of Applied Behavior Analysis. 2021;54(1):87. doi: 10.1002/JABA.803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel A., Zuo Y., Moghaddamcharkari N., McIntyre R.S., Rosenblat J.D. Barriers, benefits and interventions for improving the delivery of telemental health services during the coronavirus disease 2019 pandemic: a systematic review. Current Opinion in Psychiatry. 2021;34(4):434–443. doi: 10.1097/YCO.0000000000000714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonoff E., Pickles A., Charman T., Chandler S., Loucas T., Baird G. Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47(8):921–929. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- Southey S.J., Stoddart K.P. Clinical intervention with autistic adolescents and adults during the first Two months of the COVID-19 pandemic: Experiences of clinicians and their clients. Voices from Practice. 2021;64(5):777–782. doi: 10.1177/00208728211012462. [DOI] [Google Scholar]
- Spain D., Mason D., Capp S.J., Stoppelbein L., White S.W., Happé F. This may be a really good opportunity to make the world a more autism friendly place”: Professionals’ perspectives on the effects of COVID-19 on autistic individuals. Research in Autism Spectrum Disorders. 2021;83 doi: 10.1016/J.RASD.2021.101747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoll J., Müller J.A., Trachsel M. Ethical issues in online psychotherapy: a narrative review. Frontiers in Psychiatry. 2020;10(993) doi: 10.3389/fpsyt.2019.00993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugarman D.E., Horvitz L.E., Greenfield S.F., Busch A.B. Clinicians perceptions of rapid scale-up of telehealth services in outpatient mental health treatment. Telemedicine and E-Health. 2021;27(12):1399–1408. doi: 10.1089/tmj.2020.0481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutherland R., Trembath D., Roberts J. Telehealth and autism: A systematic search and review of the literature. International Journal of Speech-Language Pathology. 2018;20(3):324–336. doi: 10.1080/17549507.2018.1465123. [DOI] [PubMed] [Google Scholar]
- Thomas N., Mcdonald C., Deboer K., Brand R.M., Nedeljkovic M., Seabrook L. Review of the current empirical literature on using videoconferencing to deliver individual psychotherapies to adults with mental health problems. Psychology and Psychotherapy: Theory, Research and Practice. 2021;94(3):854–883. doi: 10.1111/papt.12332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonn P., Reuter S.C., Kuchler I., Reinke B., Hinkelmann L., Stöckigt S.…Schulze N. Development of a Questionnaire to Measure the Attitudes of Laypeople, Physicians, and Psychotherapists Toward Telemedicine in Mental Health. JMIR Mental Health. 2017;4(4) doi: 10.2196/mental.6802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organisation . World Health Organisation; Geneva: 2009. (Telemedicine: opportunities and developments in member states. Report on the second global survey on eHealth). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Supplementary material
Supplementary material
Supplementary material
Supplementary material
Supplementary material
Supplementary material
Supplementary material