Abstract
There is a growing body of evidence highlighting the significant role of gut microbiota in various pathologies. We performed a systematic review to review the different microbiota involved in neuropsychiatric diseases. 50 studies (23 studies for autism spectrum disorders, 18 for major depression, and 9 for schizophrenia), representing 2,137 patients and 2,844 controls. Concerning the microbiota, the genera Prevotella, Clostridium, Bacteroides, Bifidobacterium, Ruminococcus, Megamonas, and Faecalbacterium were the ones detected with the most frequent variation of their relatives abundance. We also assess the overlap between the different pathologies. This study provides new insights into the complex relationship between the brain and the gut and the implications in neuropsychiatric pathologies. The identification of unique signatures in neuropsychiatric diseases suggests new possibilities in targeted anti or probiotic treatment.
Keywords: gut microbiota, psychiatric diseases, autism spectrum disorders, depression, schizophrenia
Introduction
The past decade has seen increasing interest in the microbiota-gut-brain axis, the bidirectional communication between the brain and the gut (Stilling et al., 2014). The microbiota-gut-brain interaction may play a role in the pathogenesis of various central nervous disorders (Wang and Kasper, 2014) and is, probably, one of the most promising new areas of research (Heiss and Olofsson, 2019; Sasmita, 2019; Seguella et al., 2019) from an epidemiologic and clinical perspective. Recent developments in high throughput DNA sequencing have made it possible to study the microbiota cost-effectively. Changes in the diversity and composition of the gut microbiota have been reported for a wide range of brain disorders and different potential mechanisms of action have been reviewed. For long, the gut microbiota has been linked to the hypothalamic-pituitary-adrenal axis and mood disorders such as bipolar disorders and major depression disorders (MDD) (Cheung et al., 2019; Kelly et al., 2019; Peirce and Alviña, 2019). Also, Autism Spectrum Disease (ASD) is one the diseases that have been studied in depth (Saurman et al., 2020) and there is increasing interest in the gut-brain axis in schizophrenia research (Golofast and Vales, 2020). There is increasing interest in the role of the gut microbiota in major depression, the most common psychiatric disorder. Overactivity of the hypothalamic-pituitary-adrenal (HPA) axis in major depression, a link between HPA axis activity and cognitive performance, and a possible involvement of HPA axis genetic variation in cognition have all been discovered in neuroendocrine investigations (Keller et al., 2017). Changes in gut microbiota composition could increase gut barrier permeability, activate systemic inflammation and immune responses, regulate monoamine neurotransmitter release and efficacy, change the activity and function of the HPA axis, and change the abundance of brain-derived neurotrophic factor, all of which could lead to depression (Du et al., 2020).
Despite the growing body of evidence, there is a lack of quantitative evidence about the different microbiota involved in psychiatric diseases. However, many questions remain to be answered. Are gut microbiota are implicated consistently to a specific disorder across studies? Are the associations unique to the disease or are the associations also seen in other psychiatric diseases? To answer these questions we have reviewed the direction of the relationship between microbiota and disease across various neurologic and neuropsychiatric diseases.
Methods
Search Strategy
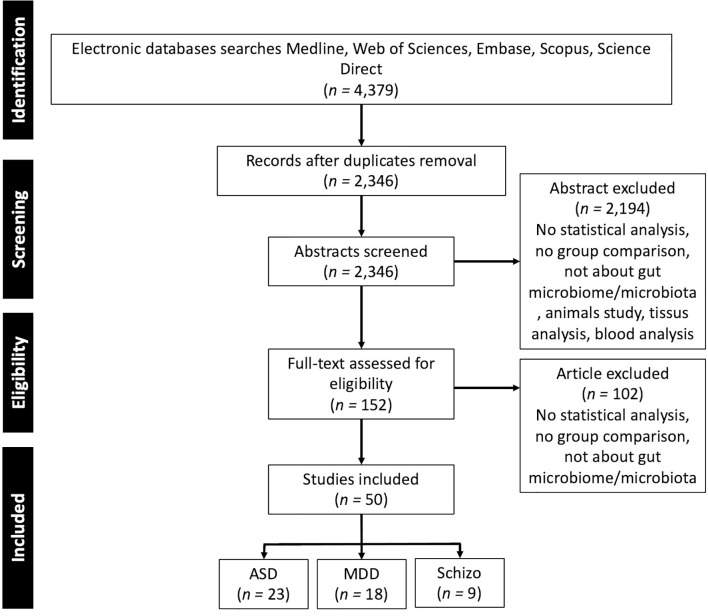
To identify the microbiota associated with neurological and neuropsychiatric disorders in the human population we performed a literature review that included articles published prior to 1st January 2021 with a combination of term “gut”, “microbiota”, “microbiome”, “stool”, “fecal” and the different pathologies “Depression”, “MDD”, “Autism”, “Autism spectrum disorders”, “Schizophrenia”. Additional relevant articles were sought through a manual bibliography search. Inclusion criteria were: human research, focus on depression, ASD, schizophrenia that makes a comparison between patients and healthy controls, focus on gut microbiota quantified from stool samples, articles published in English in peer-reviewed journals. A flow diagram of study selection is presented in Figure 1 .
Figure 1.
PRISMA flow diagram of the studies selection. ASD, Autism Spectrum Disorder; MDD, Major Depressive Disorder; Schizo., Schizophrenia.
Data Extraction
From the included studies the following parameters were extracted: the country where the experiments have been carried out, general characteristics of the patients and control (e.g., age, BMI, sex ratio), microbiota analysis method. We then listed the different taxon of which relative abundance has been found statistically significantly different between patients and healthy controls and indicated the direction: relative abundance increased or decreased in the various pathologies.
Statistical Analysis
We determined whether findings were consistent across studies of a single disorder based on statistical significance and the direction of association for the studies that showed significant results. If two studies were found to show the same direction of the relationship (e.g., microbiota Taxus was found more often in patients in both studies), findings were classified as consistent. As most studies were small, one expects heterogeneity across studies due to random fluctuation. We therefore also considered findings for which the consistency between was more than 50% as consistent. We present the phylogenetic trees of the microbiota that have been successfully found in the literature for the different pathologies using the GraPhIAn package in Python (Asnicar et al., 2015). General information about the included studies and baseline data on patients were summarized in graphics. To compare the different microbiota involved in the studies’ pathologies we used Venn diagrams using the VennDiagram package in R (Chen and Boutros, 2011).
Results
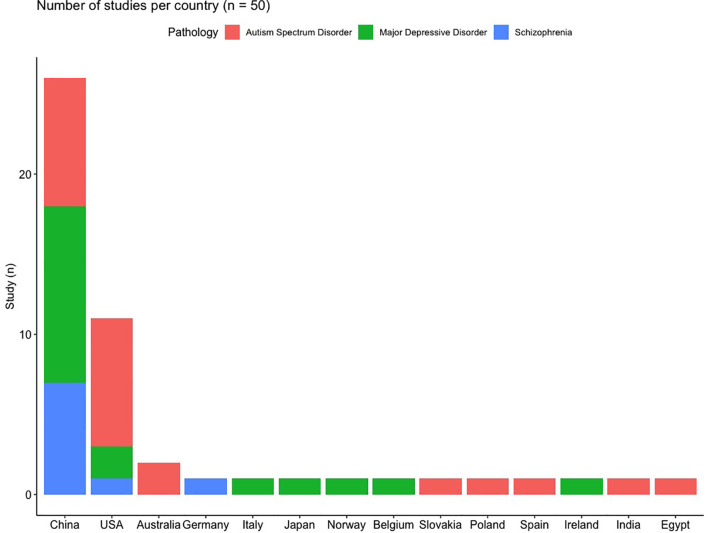
In total, 50 studies were included in this review, representing 2,137 patients and 2,844 controls, the repartition of the patients within the different pathologies is presented in Supplementary Figure 1 . ASD is the most frequently studied disorder ( Figure 1 and Supplementary Figure 1 ), comprising 46% of all patients and 44% of all studies. As the gut microbiota is known to depend on the environment (Anwar et al., 2021) and diet (Zmora et al., 2019), which differ across societies and cultures and thus across studies, the distribution of the studies per country is presented in Figure 2 . It is of note that most of the studies were conducted in China (n = 26, 52%) and in the USA (n = 11, 22%), only 8 (16%) of the included studies were done in Europe.
Figure 2.
Distribution of the included studies according to the countries and studied pathologies.
The characteristics for patients with ASD are presented in Supplementary Table 1 , for depression in Supplementary Table 2 , and for schizophrenia in Supplementary Table 3 .
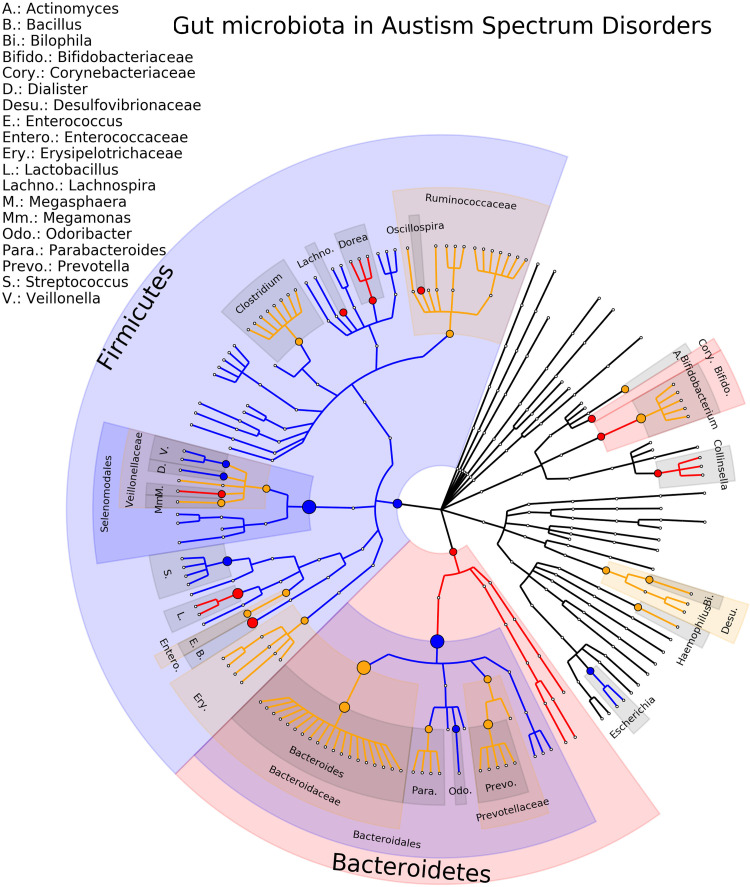
The most studied neuropsychiatric disorder is ASD with twenty-three studies included in the review, involving a total of 932 patients and 792 healthy controls (Adams et al., 2011; Wang et al., 2011; Gondalia et al., 2012; Kang et al., 2013; Son et al., 2015; Tomova et al., 2015; Luna et al., 2016; Strati et al., 2017; Iovene et al., 2017; Kushak et al., 2017; Kang et al., 2018; Pulikkan et al., 2018; Zhang et al., 2018; Rose et al., 2018; Liu et al., 2019; Zhai et al., 2019; Ma et al., 2019; Plaza-Díaz et al., 2019; Sun et al., 2019; Chen et al., 2020; Ding et al., 2020; Zou et al., 2020; Ahmed et al., 2020). At the genus level, there are 64 gut microbiota-disease associations reported. Of these, 12 (19%) associations are consistent (Bacillus, Collinsella, Dialister, Dorea, Escherichia/Shigella, Lachnospira, Lactobacillus, Megaspharea, Odoribacter, Oscillospira, Streptococcus, Veillonella) and for 4 there are multiple studies in the same direction (Escherichia/Shigella, Lachnospira, Lactobacillus, Streptococcus). For 14 (25%) gut microbiota, an opposite direction of association is reported (Actinomyces, Akkermansia, Bacteroides, Bifidobacterium, Bilophila, Clostridium, Erysipelatoclostridium, Faecalbacterium, Haemophilus, Lachnoclostridium, Megamonas, Parabacteroides, Prevotella, Ruminococcus). The phylogenetic tree representing the results are presented in Figure 3 , the complete results of the individual studies are presented in Supplementary Table 4 . Of note is that some studies did not find any statistical differences between ASD patients and controls (Gondalia et al., 2012; Son et al., 2015).
Figure 3.
Phylogenetic distributions of the microbiota involved in Autism Spectrum Disorder. Orange indicates inconsistent results, blue for a decrease in relative abundance and red increased in relative abundance.
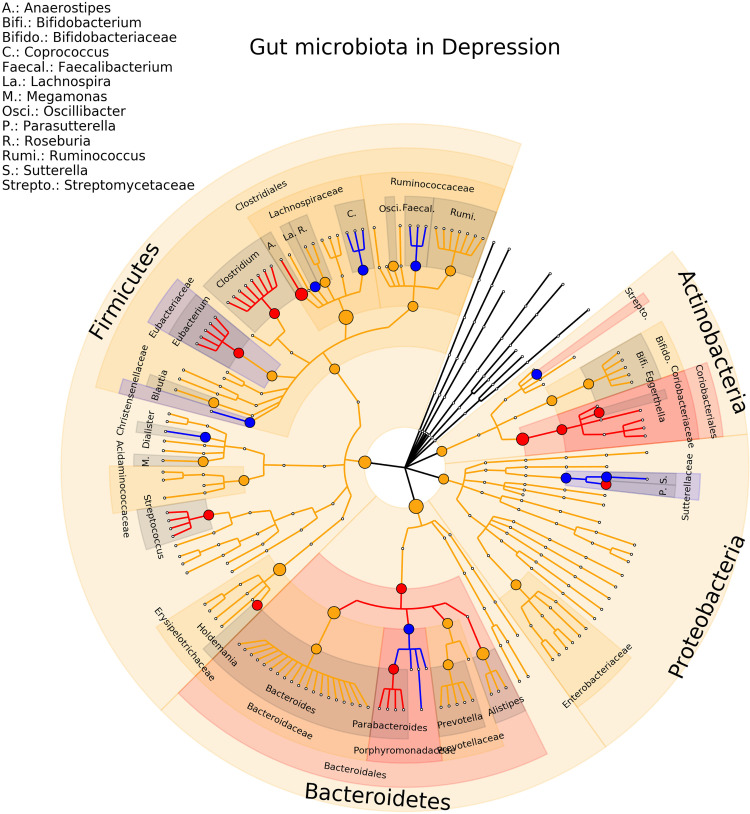
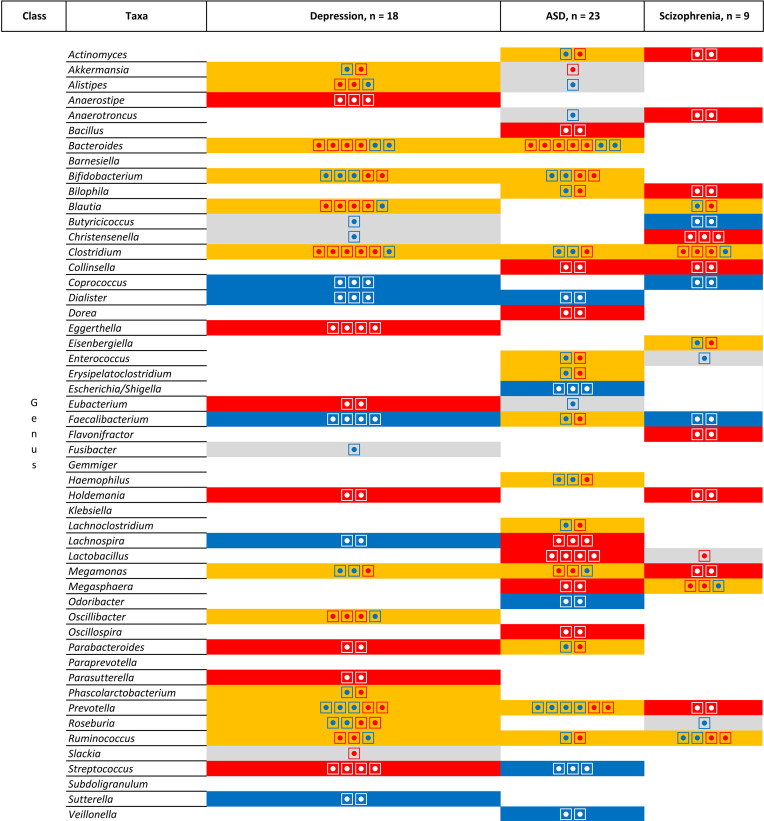
Eighteen studies on MDD were included in the review, involving a total of 801 depressed patients and 1,634 healthy controls (Naseribafrouei et al., 2014; Jiang et al., 2015; Aizawa et al., 2016; Zheng et al., 2016; Kelly et al., 2016; Liu et al., 2016; Lin et al., 2017; Chen et al., 2018; Chen et al., 2018; Valles-Colomer et al., 2019; Lai et al., 2019; Chung et al., 2019; Rong et al., 2019; Mason et al., 2020; Fontana et al., 2020; Zheng et al., 2020; Liu et al., 2020; Chen et al., 2020). At the genus levels, 21 associations were detected in only one study, 12 (27%) association were consistent in term of direction and significance (Anaerostipes, Coprococcus, Dialister, Eggerthella, Eubacterium, Faecalbacterium, Holdemania, Lachnospira, Parabacteroides, Parasutterella, Streptococcus, Sutterella). For the other associations, Bacteroides concentration was found increased in four studies and decreased in two studies, Blautia concentration was found increased in 4 studies while the relative abundance was found decreased in two studies, for Clostridium 5 studies found an increase of the relative abundance and only one study found a decreased concentration, for Oscillibacter 3 studies found an increase and only one a decrease of the relative abundance, for Bifidobacterium and Prevotella 3 studies found a decrease and 2 and increase of the relative abundance finally three associations (Alistipes, Megamonas, Ruminococcus) are found in the same direction in 2 studies and on the opposite direction in 1 study. The phylogenetic tree representing the results are presented in Figure 4 . Complete results of the included studies are presented in Supplementary Table 5 .
Figure 4.
Phylogenetic distributions of the microbiota involved in Major Depressive Disorder. Orange indicates inconsistent results, blue for a decrease in relative abundance and red increased in relative abundance.
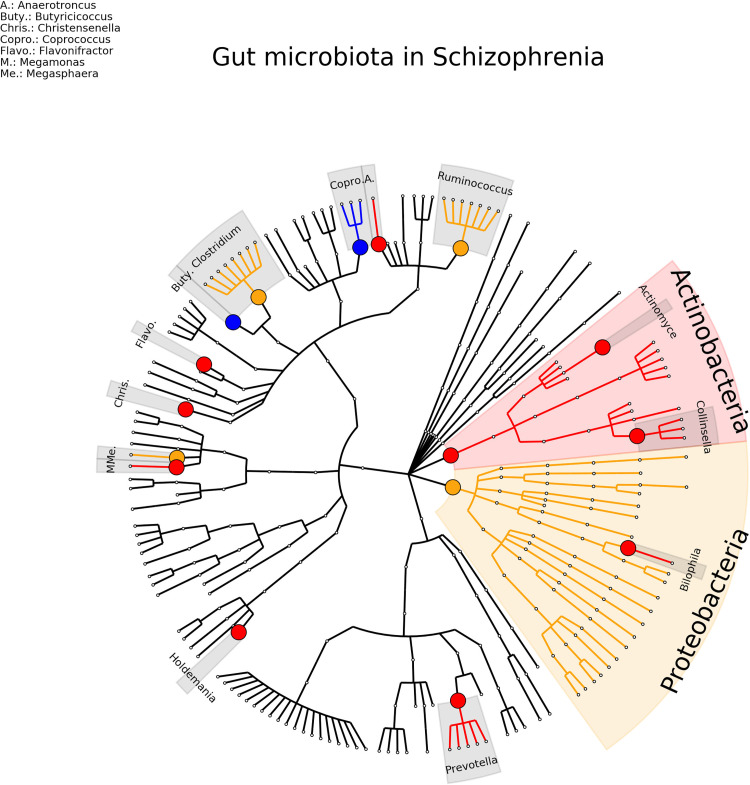
For schizophrenia, nine studies were included, involving a total of 404 patients and 418 healthy controls (Schwarz et al., 2018; Shen et al., 2018; Nguyen et al., 2019; Xu et al., 2019; Li et al., 2020; Ma et al., 2020; Pan et al., 2020; Xu et al., 2020; Zhang et al., 2020). 11 (16%) genera were found consistent in term of direction and significance (Actinomyces, Anaerococcus, Bilophila, Butyricicoccus, Christensenella, Collinsella, Coprococcus, Faecalbacterium, Flavonifractor, Holdemania, Prevotella) and 5 (7%) were inconsistent in term of direction (Blautia, Clostridium, Eisenbergiella, Megasphaera, Ruminococcus) (see Figure 5 and Supplementary Table 6 ).
Figure 5.
Phylogenetic distributions of the microbiota involved in Schizophrenia. Orange indicates inconsistent results, blue for a decrease in relative abundance and red increased in relative abundance.
The picture emerging is that for ASD association of 6 genera is replicated in 3 studies or more. For depression 12 associations were consistent but for 10 findings were in opposite direction. Finally, for schizophrenia, only 1 association was found consistent in 3 studies and 11 in two studies.
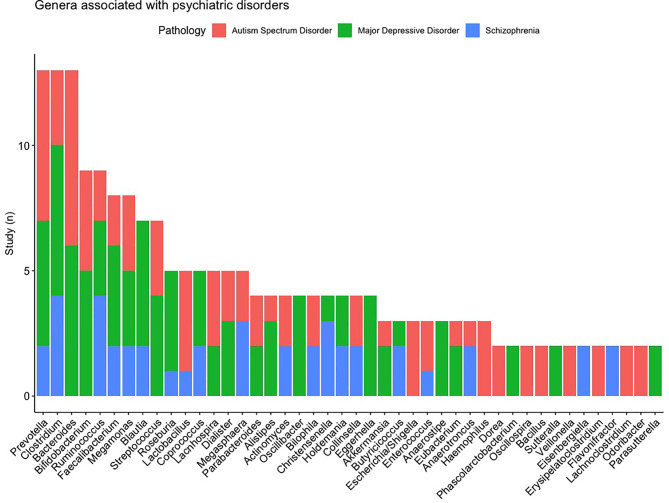
First, we started from the microbiota and determined whether the association was reported to different pathologies. Figure 6 shows the microbiota which are associated with multiple disorders and the number of studies that found the association of the genus to a disease. Prevotella and Clostridium are associated with multiple psychiatric disorders (the 3 studied disorders), the genus of Bacteroides is associated to MDD and ASD. It is interesting to note that the directions are inconsistent across the pathologies and studies.
Figure 6.
List of the microbiota the most frequently found and their distributions according to pathologies.
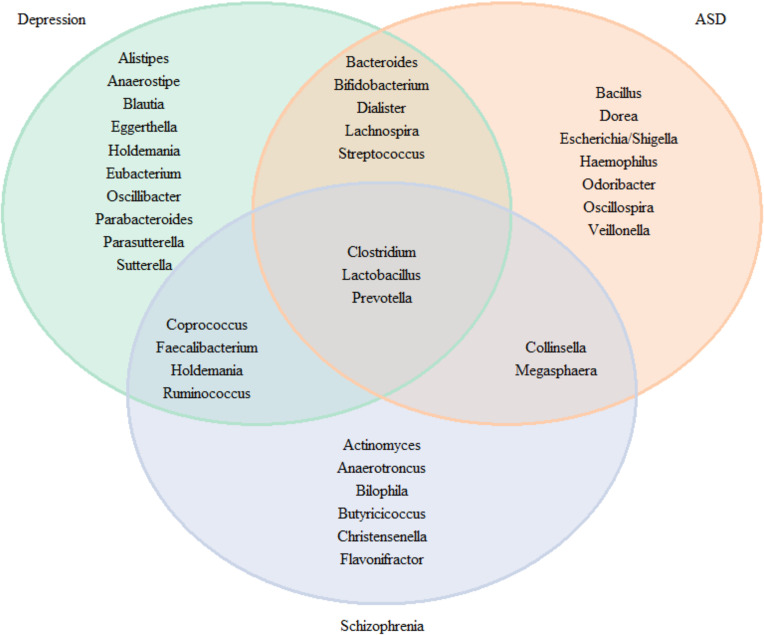
For research where inconsistency was discovered across trials, we define consistency as more than 50% of studies consistently finding an association in the same direction. In Figure 7 , we plotted Venn diagrams summarizing association to the neuropsychiatric disorders and check for overlap microbiota associated. We observed an overlap of the three pathologies for the Clostridium, Lactobacillus and Prevotella. Five genera were found in MDD and ASD (Bacteroides, Bifidobacterium, Dialister, Lachnospira and Steptococcus), 4 between MDD and schizophrenia (Coprococcus, Faecalbacterium, Holdemania, and Ruminococcus) and 2 between ASD and schizophrenia (Collinsella and Megasphaera).
Figure 7.
Venn diagram for the genus consistently found in the literature for neuropsychiatric diseases.
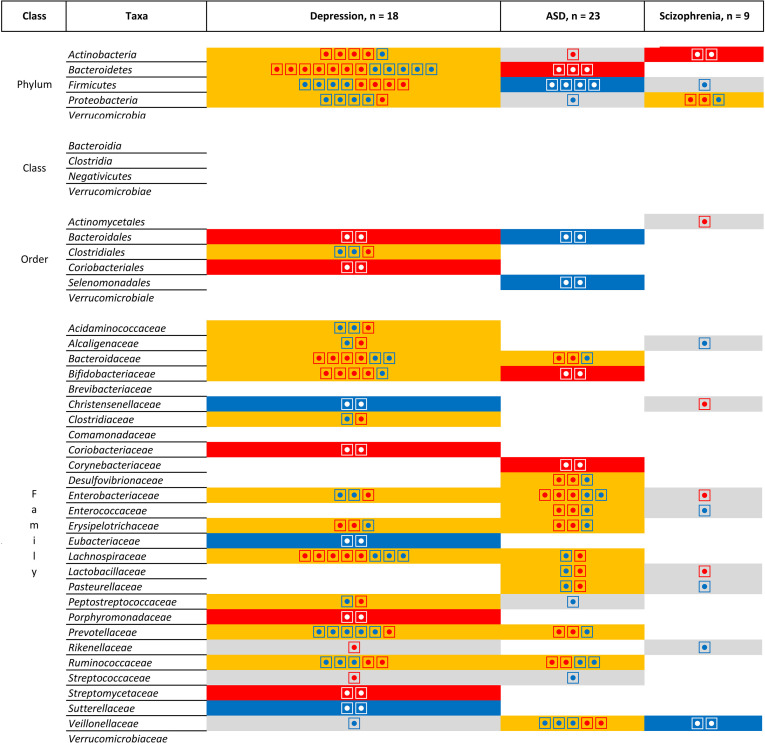
However, Figure 7 does not take into account the direction of association. When comparing the direction of the association [ Figure 8 (phylum, classer, order and family levels) and Figure 9 (genus level)], for MDD and ASD we found an increase in the relative abundance of Bacteroides and a decrease in the abundance of Dialister and Prevotella; opposite direction are found for Clostridium (increase in depression), Lachnospira (decrease in depression), Lactobacillus (decrease in depression), and Streptococcus (increase in depression). When comparing ASD and schizophrenia Collinsella, Megamonas, Megasphaera are found in the same direction (increase of relative abundance), while Clostridium and Prevotella are found in the opposite direction (decrease in ASD). Finally for depression and schizophrenia Clostridium, Collinsella, Holdemania are increased, Coprococcus and Faecalbacterium are decreased and opposite direction is found for Megamonas (decrease in depression) and Prevotella (decrease in depression).
Figure 8.
List of the microbiota that have been identified in at least two studies for the same pathologies at the Phylum, Class, Order and Family levels. Grey is use for one study, orange indicates inconsistent results, blue for a decrease in relative abundance and red increased in relative abundance. Each individual circle indicates a study that identify the microbiota.
Figure 9.
List of the microbiota that have been identified in at least two studies for the same pathologies at the genus level. Grey colour is used for one study, orange colour indicates inconsistent results, blue colour for consistent results showing a decrease in relative abundance in patients compared to patients and red colour for consistent results showing an increased in relative abundance in patients compared to patients. Each individual circle indicates a study that identify the microbiota.
Discussion
By far the most studied pathologies is ASD as well as the highest level of consistency as highlighted by the phylogenetic trees ( Figure 3 ). Several studies (Luna et al., 2016; Finegold et al., 2017) compared patients with functional gastrointestinal disorders (FGID) and controls without FGID making the comparison of gut microbiota difficult to interpret since the two factors play a role in the composition of microbiota. Only one study compared ASD children with and without FGID with controls with and without FGID (Rose et al., 2018). Authors found differences at the Family level: Bacteroidaceae, Lachnospiraceae, Prevotellaceae and Ruminocaccaceae were more abundant in ASD with FGID compared to control with FGID, interestingly the same differences were not detected between patients and controls without FGID (Rose et al., 2018). For major depressive disorders although the number of included studies is high (n = 18) we did not find such consistency between the studies as for ASD ( Figures 3 , 4 ). However the field is growing and the evidences starting to emerge. Interestingly it has been demonstrated that women with post-partum depression also presented significant modifications of the microbiota (Zhou et al., 2020), which seems to indicate that the changes are occurring quite quick and are not associated to the chronicity of the MDD. The age of the patients also influences the modification seen in depression (Chen et al., 2020). Finally a study of twins with depression shows that the affected twins had a lower diversity and an absence of a specific operational taxonomical unit in comparison with healthy control (Vinberg et al., 2019). This leads us to question the impact and the interactions between the gene and the environment on the observed modifications.
There are several possible explanations about the mechanisms of action driving the relationship between gut microbiota and the different diseases. A recent review underlines the relationship among inflammation, pain, microbiota and the different lipids, focusing on the possible involvement of N-acylethanolamine family and short-chain fatty acids in the gut-brain axis and their role in the central nervous system diseases (Russo et al., 2018). The lymphatic system could be the mediator of this communication between the gut microbiota and the brain (Tsunoda, 2017).
In this review, we summarized the current evidence of the modification of the gut microbiota in various pathologies. We limited our analysis to the main neuropsychiatric diseases but gut microbiota composition is also modified in other neurological disorders such as Rett syndrome (Strati et al., 2016) and in neurocritically ill patients (Xu et al., 2019). However, their roles are not limited to neurological or neuropsychiatric diseases, they are also involved in hypertension (Li et al., 2017; Yan et al., 2017), cirrhosis (Bajaj et al., 2012; Bajaj et al., 2014) or primary hepatocellular carcinoma (Ni et al., 2019), diabetes (Chen et al., 2019), autoimmune diseases (Chen et al., 2017), Systemic Lupus Erythematosus (Luo et al., 2018), systemic immunity in allergic disease (Ipci et al., 2017), Behcet’s disease (Ye et al., 2018), systemic sclerosis (Patrone et al., 2017), rheumatoid arthritis (Liu et al., 2013) and could also potentially influence vitamin D production (Zuo et al., 2019) and there are correlation between some gut microbiota and personality in adults (Kim et al., 2018).
An essential part of the research in this field is the development of treatments to modify the microbiota. For example, intermittent fasting led to increased gut bacteria richness, enrichment of the Lactobacillaceae, Bacteroidaceae, and Prevotellaceae families and enhanced antioxidative microbial metabolic pathways (Cignarella et al., 2018). Changes in microbiota composition and clinical improvement have also been observed after specific diet (Libbey et al., 2018; Rice et al., 2019). Other promising results and modification of the gut microbiota have been obtained with fecal transplantation in animals and human studies (Evrensel and Ceylan, 2016; Sun et al., 2018). So far the most promising results of clinical improvement after modification of the gut microbiota have been obtained in patients with epilepsy after ketogenic diet (Zhang et al., 2018; Fan et al., 2019; Lindefeldt et al., 2019). The researchers showed that there was an overall decrease in the mean species diversity after treatment and importantly, a difference between the variation of species between responders and non-responders. Further analysis of species composition before and after treatment showed a significant increase in Bacteroides and a decrease in Firmicutes and Actinobacteria. When comparing responders and non-responders, Clostridiales, Clostridia, Ruminococcaeceae, Lachnospiraceaea, Alistipes and Tikenellacase were significantly increased in non-responders (Spinelli and Blackford, 2018).
Another main field of research is to determine if modification of the gut microbiota can decrease the risk of developing disease or improve the health of the patients: in Alzheimer’s disease (Mancuso and Santangelo, 2018), Parkinson’s disease (Sun and Shen, 2018), multiple sclerosis (Mirza and Mao-Draayer, 2017), amyotrophic lateral sclerosis (Zhang et al., 2017), and epilepsy (De Caro et al., 2019).
There are a few limitations in this review. The first one concerns the methodology used in the different studies: all studies used 16sRNA analysis but in some studies, corrections were applied for medication or constipation, two factors known to modify the composition of gut microbiota, while in most of the other studies these factors were not taken into consideration. Another technical point is that some authors applied corrections for multiple testing, some not and the techniques used are also different [e.g. Bonferroni’s correction for multiple testing or false discovery rate (Brenner et al., 2018)]; the results are different adjusting or not for multiple analyses [see for example study of Kang et al. presenting both results (Kang et al., 2018)]. Other studies used linear discriminant analysis (LDA) (usually LDA > 2.0) to differentiate patients and control (Liu et al., 2019). For all of the above limitations, we were not able to perform a meta-analysis which could provide a clearer vision of the direction and intensity of the modifications observed in the different diseases.
Because of a lack of existing data, we were not able to assess sex difference while it seems that, at least for some pathologies, there are differences between male and female (Chen et al., 2018; Holingue et al., 2020; Jaggar et al., 2020), as well as the ethnicities (Ventura et al., 2019). We also limit our analysis to genetic analysis of gut microbiota composition. Recent research also evaluate immune-inflammation (Carissimi et al., 2019) and gut glutamate metabolism (Wang et al., 2019) to differentiate patients and healthy controls.
The main limitation of the current studies are the populations investigated. We have seen that a majority of the studies have been done in China and in USA. This high homogeneity made the generalization and the translation of the results for these pathologies more limited since it has been shown that genetics (Simões et al., 2013; Matsuki et al., 2016), socioeconomic status (Bowyer et al., 2019), host and environmental factors (Anwar et al., 2021) and diet influence the composition of the microbiota serve a significant role in shaping the gut microbiota population (Bibbò et al., 2016; Chassaing et al., 2017; Proctor et al., 2017; Sandhu et al., 2017).
Of note is that we limited our analysis to binary responses between patients and controls but it is interesting to analyse the microbiota concentration as continuous variables since the severity of some diseases is correlated with the relative abundance of various microbiota. It has, for example, been shown that a greater severity of depressive symptoms was correlated with a greater abundance of genus Bacteroides (r = 0.70; p = 0.0002), while increased negative symptoms were associated with decreased abundance of family Ruminococcaceae (r = −0.74; p = 0.0002). Overall self-reported mental well-being was positively correlated with phylum Verrumicrobia (r = 0.63; p = 0.002) (Nguyen et al., 2019).
Another limitation is that we only included results of the studies using DNA sequencing of the fecal stool while it may also be interesting to study the composition of microbiota from different samples (Park et al., 2017). Depending on the diseases, other biota can be analysed and be a good indicator of the severity of the diseases, such as mouth microbiota in schizophrenia (Castro-Nallar et al., 2015; Yolken et al., 2015). Although the analysis of other microbiota may be challenging from the point of view of tissue collection, it has been showed that brain (Branton et al., 2016) – blood (Olde Loohuis et al., 2018) or direct microbiota analysis from the intestinal tissue (Cosorich et al., 2017) in patients multiple sclerosis could provide different type of information.
In the future analysing the changes in microbiota from nose to gut could also be an essential source of knowledge’s to get a better insight into the diseases (Bell et al., 2019). Finally, we limited our analysis at the genus level using 16S sequencing while it is possible to investigate the bacterial species in depth by sequencing the full genome, but only a few studies are currently performing this kind of analysis requiring deep sequencing methods.
Conclusion
The gut microbiota plays an important role in the development of neuropsychiatric diseases. We summarized the current pieces of evidence about the quantified modifications of the gut microbiota compositions in patients compared to healthy controls. The most remarkable microbiota signature was observed in ASD. For future clinical applications, baseline value and standard reporting template have just been developed that should ease and spread the analysis of gut microbiota in daily practice for the clinicians (King et al., 2019). The analysis of the gut microbiota could therefore be used to refine diagnostic or to assess the severity of MDD (Averina et al., 2020). There is currently an urgent need for standardization of the analysis and report of studies related to gut microbiota modification in order to move this field forward.
Author Contributions
The study was conceived by BB and CD. NA and CD verified the analytical methods. BB, NA, and CD did the data interpretation. CD supervised the findings of this work. All authors discussed the results and contributed to the final manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcimb.2022.831666/full#supplementary-material
References
- Adams J. B., Johansen L. J., Powell L. D., Quig D., Rubin R. A. (2011). Gastrointestinal Flora and Gastrointestinal Status in Children With Autism–Comparisons to Typical Children and Correlation With Autism Severity. BMC Gastroenterol. 11, 22. doi: 10.1186/1471-230X-11-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed S. A., Elhefnawy A. M., Azouz H. G., Roshdy Y. S., Ashry M. H., Ibrahim A. E., et al. (2020). Study of the Gut Microbiome Profile in Children With Autism Spectrum Disorder: A Single Tertiary Hospital Experience. J. Mol. Neurosci. MN 70, 887–896. doi: 10.1007/s12031-020-01500-3 [DOI] [PubMed] [Google Scholar]
- Aizawa E., Tsuji H., Asahara T., Takahashi T., Teraishi T., Yoshida S., et al. (2016). Possible Association of Bifidobacterium and Lactobacillus in the Gut Microbiota of Patients With Major Depressive Disorder. J. Affect. Disord. 202, 254–257. doi: 10.1016/j.jad.2016.05.038 [DOI] [PubMed] [Google Scholar]
- Anwar H., Iftikhar A., Muzaffar H., Almatroudi A., Allemailem K. S., Navaid S., et al. (2021). Biodiversity of Gut Microbiota: Impact of Various Host and Environmental Factors. BioMed. Res. Int. 2021, 5575245. doi: 10.1155/2021/5575245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asnicar F., Weingart G., Tickle T. L., Huttenhower C., Segata N. (2015). Compact Graphical Representation of Phylogenetic Data and Metadata With GraPhlAn. PeerJ 3, e1029. doi: 10.7717/peerj.1029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Averina O. V., Zorkina Y. A., Yunes R. A., Kovtun A. S., Ushakova V. M., Morozova A. Y., et al. (2020). Bacterial Metabolites of Human Gut Microbiota Correlating With Depression. Int. J. Mol. Sci. 21, E9234. doi: 10.3390/ijms21239234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bajaj J. S., Heuman D. M., Hylemon P. B., Sanyal A. J., White M. B., Monteith P., et al. (2014). Altered Profile of Human Gut Microbiome Is Associated With Cirrhosis and Its Complications. J. Hepatol. 60, 940–947. doi: 10.1016/j.jhep.2013.12.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bajaj J. S., Hylemon P. B., Ridlon J. M., Heuman D. M., Daita K., White M. B., et al. (2012). Colonic Mucosal Microbiome Differs From Stool Microbiome in Cirrhosis and Hepatic Encephalopathy and Is Linked to Cognition and Inflammation. Am. J. Physiol. - Gastrointest Liver Physiol. 303, G675–G685. doi: 10.1152/ajpgi.00152.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell J. S., Spencer J. I., Yates R. L., Yee S. A., Jacobs B. M., DeLuca G. C. (2019). Invited Review: From Nose to Gut - The Role of the Microbiome in Neurological Disease. Neuropathol. Appl. Neurobiol. 45, 195–215. doi: 10.1111/nan.12520 [DOI] [PubMed] [Google Scholar]
- Bibbò S., Ianiro G., Giorgio V., Scaldaferri F., Masucci L., Gasbarrini A., et al. (2016). The Role of Diet on Gut Microbiota Composition. Eur. Rev. Med. Pharmacol. Sci. 20, 4742–4749. [PubMed] [Google Scholar]
- Bowyer R. C. E., Jackson M. A., Le Roy C. I., Ni Lochlainn M., Spector T. D., Dowd J. B., et al. (2019). Socioeconomic Status and the Gut Microbiome: A TwinsUK Cohort Study. Microorganisms 7 (1), 37. doi: 10.3390/microorganisms7010017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branton W. G., Lu J. Q., Surette M. G., Holt R. A., Lind J., Laman J. D., et al. (2016). Brain Microbiota Disruption Within Inflammatory Demyelinating Lesions in Multiple Sclerosis. Sci. Rep. 6, 37344. doi: 10.1038/srep37344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenner D., Hiergeist A., Adis C., Mayer B., Gessner A., Ludolph A. C., et al. (2018). The Fecal Microbiome of ALS Patients. Neurobiol. Aging 61, 132–137. doi: 10.1016/j.neurobiolaging.2017.09.023 [DOI] [PubMed] [Google Scholar]
- Carissimi C., Laudadio I., Palone F., Fulci V., Cesi V., Cardona F., et al. (2019). Functional Analysis of Gut Microbiota and Immunoinflammation in Children With Autism Spectrum Disorders. Dig Liver Dis. Off J. Ital Soc. Gastroenterol. Ital Assoc. Study Liver 51, 1366–1374. doi: 10.1016/j.dld.2019.06.006 [DOI] [PubMed] [Google Scholar]
- Castro-Nallar E., Bendall M. L., Pérez-Losada M., Sabuncyan S., Severance E. G., Dickerson F. B., et al. (2015). Composition, Taxonomy and Functional Diversity of the Oropharynx Microbiome in Individuals With Schizophrenia and Controls. PeerJ 3, e1140. doi: 10.7717/peerj.1140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chassaing B., Vijay-Kumar M., Gewirtz A. T. (2017). How Diet Can Impact Gut Microbiota to Promote or Endanger Health. Curr. Opin. Gastroenterol. 33, 417–421. doi: 10.1097/MOG.0000000000000401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H., Boutros P. C. (2011). VennDiagram: A Package for the Generation of Highly-Customizable Venn and Euler Diagrams in R. BMC Bioinf. 12, 35. doi: 10.1186/1471-2105-12-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen P.-C., Chien Y.-W., Yang S.-C. (2019). The Alteration of Gut Microbiota in Newly Diagnosed Type 2 Diabetic Patients. Nutr. Burbank Los Angel Cty Calif. 63–64, 51–56. doi: 10.1016/j.nut.2018.11.019 [DOI] [PubMed] [Google Scholar]
- Chen Y., Fang H., Li C., Wu G., Xu T., Yang X., et al. (2020). Gut Bacteria Shared by Children and Their Mothers Associate With Developmental Level and Social Deficits in Autism Spectrum Disorder. mSphere 5 (6), e01044–20. doi: 10.1128/mSphere.01044-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J.-J., He S., Fang L., Wang B., Bai S.-J., Xie J., et al. (2020). Age-Specific Differential Changes on Gut Microbiota Composition in Patients With Major Depressive Disorder. Aging 12, 2764–2776. doi: 10.18632/aging.102775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Z., Li J., Gui S., Zhou C., Chen J., Yang C., et al. (2018). Comparative Metaproteomics Analysis Shows Altered Fecal Microbiota Signatures in Patients With Major Depressive Disorder. Neuroreport 29, 417–425. doi: 10.1097/WNR.0000000000000985 [DOI] [PubMed] [Google Scholar]
- Chen B., Sun L., Zhang X. (2017). Integration of Microbiome and Epigenome to Decipher the Pathogenesis of Autoimmune Diseases. J. Autoimmun 83, 31–42. doi: 10.1016/j.jaut.2017.03.009 [DOI] [PubMed] [Google Scholar]
- Chen J.-J., Zheng P., Liu Y.-Y., Zhong X.-G., Wang H.-Y., Guo Y.-J., et al. (2018). Sex Differences in Gut Microbiota in Patients With Major Depressive Disorder. Neuropsychiatr. Dis. Treat 14, 647–655. doi: 10.2147/NDT.S159322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung S. G., Goldenthal A. R., Uhlemann A.-C., Mann J. J., Miller J. M., Sublette M. E. (2019). Systematic Review of Gut Microbiota and Major Depression. Front. Psychiatry 10, 34. doi: 10.3389/fpsyt.2019.00034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung Y.-C. E., Chen H.-C., Chou H.-C. L., Chen I.-M., Lee M.-S., Chuang L.-C., et al. (2019). Exploration of Microbiota Targets for Major Depressive Disorder and Mood Related Traits. J. Psychiatr. Res. 111, 74–82. doi: 10.1016/j.jpsychires.2019.01.016 [DOI] [PubMed] [Google Scholar]
- Cignarella F., Cantoni C., Ghezzi L., Salter A., Dorsett Y., Chen L., et al. (2018). Intermittent Fasting Confers Protection in CNS Autoimmunity by Altering the Gut Microbiota. Cell Metab. 27, 1222–1235.e6. doi: 10.1016/j.cmet.2018.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cosorich I., Dalla-Costa G., Sorini C., Ferrarese R., Messina M. J., Dolpady J., et al. (2017). High Frequency of Intestinal TH17 Cells Correlates With Microbiota Alterations and Disease Activity in Multiple Sclerosis. Sci. Adv. 3, e1700492. doi: 10.1126/sciadv.1700492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Caro C., Iannone L. F., Citraro R., Striano P., De Sarro G., Constanti A., et al. (2019). Can We ‘Seize’ the Gut Microbiota to Treat Epilepsy? Neurosci. Biobehav. Rev. 107, 750–764. doi: 10.1016/j.neubiorev.2019.10.002 [DOI] [PubMed] [Google Scholar]
- Ding X., Xu Y., Zhang X., Zhang L., Duan G., Song C., et al. (2020). Gut Microbiota Changes in Patients With Autism Spectrum Disorders. J. Psychiatr. Res. 129, 149–159. doi: 10.1016/j.jpsychires.2020.06.032 [DOI] [PubMed] [Google Scholar]
- Du Y., Gao X.-R., Peng L., Ge J.-F. (2020). Crosstalk Between the Microbiota-Gut-Brain Axis and Depression. Heliyon 6, e04097. doi: 10.1016/j.heliyon.2020.e04097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evrensel A., Ceylan M. E. (2016). Fecal Microbiota Transplantation and Its Usage in Neuropsychiatric Disorders. Clin. Psychopharmacol. Neurosci. Off Sci. J. Korean Coll. Neuropsychopharmacol. 14, 231–237. doi: 10.9758/cpn.2016.14.3.231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan Y., Wang H., Liu X., Zhang J., Liu G. (2019). Crosstalk Between the Ketogenic Diet and Epilepsy: From the Perspective of Gut Microbiota. Mediators Inflamm. 2019, 8373060. doi: 10.1155/2019/8373060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finegold S. M., Summanen P. H., Downes J., Corbett K., Komoriya T. (2017). Detection of Clostridium Perfringens Toxin Genes in the Gut Microbiota of Autistic Children. Anaerobe 45, 133–137. doi: 10.1016/j.anaerobe.2017.02.008 [DOI] [PubMed] [Google Scholar]
- Fontana A., Manchia M., Panebianco C., Paribello P., Arzedi C., Cossu E., et al. (2020). Exploring the Role of Gut Microbiota in Major Depressive Disorder and in Treatment Resistance to Antidepressants. Biomedicines 8 (9), 311. doi: 10.3390/biomedicines8090311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golofast B., Vales K. (2020). The Connection Between Microbiome and Schizophrenia. Neurosci. Biobehav. Rev. 108, 712–731. doi: 10.1016/j.neubiorev.2019.12.011 [DOI] [PubMed] [Google Scholar]
- Gondalia S. V., Palombo E. A., Knowles S. R., Cox S. B., Meyer D., Austin D. W. (2012). Molecular Characterisation of Gastrointestinal Microbiota of Children With Autism (With and Without Gastrointestinal Dysfunction) and Their Neurotypical Siblings. Autism Res. Off J. Int. Soc. Autism Res. 5, 419–427. doi: 10.1002/aur.1253 [DOI] [PubMed] [Google Scholar]
- Heiss C. N., Olofsson L. E. (2019). The Role of the Gut Microbiota in Development, Function and Disorders of the Central Nervous System and the Enteric Nervous System. J. Neuroendocrinol 31, e12684. doi: 10.1111/jne.12684 [DOI] [PubMed] [Google Scholar]
- Holingue C., Budavari A. C., Rodriguez K. M., Zisman C. R., Windheim G., Fallin M. D. (2020). Sex Differences in the Gut-Brain Axis: Implications for Mental Health. Curr. Psychiatry Rep. 22, 83. doi: 10.1007/s11920-020-01202-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iovene M. R., Bombace F., Maresca R., Sapone A., Iardino P., Picardi A., et al. (2017). Intestinal Dysbiosis and Yeast Isolation in Stool of Subjects With Autism Spectrum Disorders. Mycopathologia 182, 349–363. doi: 10.1007/s11046-016-0068-6 [DOI] [PubMed] [Google Scholar]
- Ipci K., Altıntoprak N., Muluk N. B., Senturk M., Cingi C. (2017). The Possible Mechanisms of the Human Microbiome in Allergic Diseases. Eur. Arch. Oto-Rhino-Laryngol Off J. Eur. Fed Oto-Rhino-Laryngol Soc. EUFOS Affil Ger Soc. Oto-Rhino-Laryngol - Head Neck Surg. 274, 617–626. doi: 10.1007/s00405-016-4058-6 [DOI] [PubMed] [Google Scholar]
- Jaggar M., Rea K., Spichak S., Dinan T. G., Cryan J. F. (2020). You’ve Got Male: Sex and the Microbiota-Gut-Brain Axis Across the Lifespan. Front. Neuroendocrinol 56, 100815. doi: 10.1016/j.yfrne.2019.100815 [DOI] [PubMed] [Google Scholar]
- Jiang H., Ling Z., Zhang Y., Mao H., Ma Z., Yin Y., et al. (2015). Altered Fecal Microbiota Composition in Patients With Major Depressive Disorder. Brain Behav. Immun. 48, 186–194. doi: 10.1016/j.bbi.2015.03.016 [DOI] [PubMed] [Google Scholar]
- Kang D.-W., Ilhan Z. E., Isern N. G., Hoyt D. W., Howsmon D. P., Shaffer M., et al. (2018). Differences in Fecal Microbial Metabolites and Microbiota of Children With Autism Spectrum Disorders. Anaerobe 49, 121–131. doi: 10.1016/j.anaerobe.2017.12.007 [DOI] [PubMed] [Google Scholar]
- Kang D.-W., Park J. G., Ilhan Z. E., Wallstrom G., Labaer J., Adams J. B., et al. (2013). Reduced Incidence of Prevotella and Other Fermenters in Intestinal Microflora of Autistic Children. PloS One 8, e68322. doi: 10.1371/journal.pone.0068322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller J., Gomez R., Williams G., Lembke A., Lazzeroni L., Murphy G. M., et al. (2017). HPA Axis in Major Depression: Cortisol, Clinical Symptomatology and Genetic Variation Predict Cognition. Mol. Psychiatry 22, 527–536. doi: 10.1038/mp.2016.120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly J. R., Borre Y., O’ Brien C., Patterson E., El Aidy S., Deane J., et al. (2016). Transferring the Blues: Depression-Associated Gut Microbiota Induces Neurobehavioural Changes in the Rat. J. Psychiatr. Res. 82, 109–118. doi: 10.1016/j.jpsychires.2016.07.019 [DOI] [PubMed] [Google Scholar]
- Kelly J. R., Keane V. O., Cryan J. F., Clarke G., Dinan T. G. (2019). Mood and Microbes: Gut to Brain Communication in Depression. Gastroenterol. Clin. North Am. 48, 389–405. doi: 10.1016/j.gtc.2019.04.006 [DOI] [PubMed] [Google Scholar]
- Kim H.-N., Yun Y., Ryu S., Chang Y., Kwon M.-J., Cho J., et al. (2018). Correlation Between Gut Microbiota and Personality in Adults: A Cross-Sectional Study. Brain Behav. Immun. 69, 374–385. doi: 10.1016/j.bbi.2017.12.012 [DOI] [PubMed] [Google Scholar]
- King C. H., Desai H., Sylvetsky A. C., LoTempio J., Ayanyan S., Carrie J., et al. (2019). Baseline Human Gut Microbiota Profile in Healthy People and Standard Reporting Template. PloS One 14, e0206484. doi: 10.1371/journal.pone.0206484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushak R. I., Winter H. S., Buie T. M., Cox S. B., Phillips C. D., Ward N. L. (2017). Analysis of the Duodenal Microbiome in Autistic Individuals: Association With Carbohydrate Digestion. J. Pediatr. Gastroenterol. Nutr. 64, e110–e116. doi: 10.1097/MPG.0000000000001458 [DOI] [PubMed] [Google Scholar]
- Lai W., Deng W., Xu S., Zhao J., Xu D., Liu Y., et al. (2019). Shotgun Metagenomics Reveals Both Taxonomic and Tryptophan Pathway Differences of Gut Microbiota in Major Depressive Disorder Patients. Psychol. Med. 51 (1), 1–12. doi: 10.1017/S0033291719003027 [DOI] [PubMed] [Google Scholar]
- Libbey J. E., Sanchez J. M., Doty D. J., Sim J. T., Cusick M. F., Cox J. E., et al. (2018). Variations in Diet Cause Alterations in Microbiota and Metabolites That Follow Changes in Disease Severity in a Multiple Sclerosis Model. Benef Microbes 9, 495–513. doi: 10.3920/BM2017.0116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindefeldt M., Eng A., Darban H., Bjerkner A., Zetterström C. K., Allander T., et al. (2019). The Ketogenic Diet Influences Taxonomic and Functional Composition of the Gut Microbiota in Children With Severe Epilepsy. NPJ Biofilms Microbiomes 5, 5. doi: 10.1038/s41522-018-0073-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin P., Ding B., Feng C., Yin S., Zhang T., Qi X., et al. (2017). Prevotella and Klebsiella Proportions in Fecal Microbial Communities Are Potential Characteristic Parameters for Patients With Major Depressive Disorder. J. Affect. Disord. 207, 300–304. doi: 10.1016/j.jad.2016.09.051 [DOI] [PubMed] [Google Scholar]
- Liu S., Li E., Sun Z., Fu D., Duan G., Jiang M., et al. (2019). Altered Gut Microbiota and Short Chain Fatty Acids in Chinese Children With Autism Spectrum Disorder. Sci. Rep. 9, 287. doi: 10.1038/s41598-018-36430-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu R. T., Rowan-Nash A. D., Sheehan A. E., Walsh R. F. L., Sanzari C. M., Korry B. J., et al. (2020). Reductions in Anti-Inflammatory Gut Bacteria Are Associated With Depression in a Sample of Young Adults. Brain Behav. Immun. 88, 308–324. doi: 10.1016/j.bbi.2020.03.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Zhang L., Wang X., Wang Z., Zhang J., Jiang R., et al. (2016). Similar Fecal Microbiota Signatures in Patients With Diarrhea-Predominant Irritable Bowel Syndrome and Patients With Depression. Clin. Gastroenterol. Hepatol. 14, 1602–1611.e5. doi: 10.1016/j.cgh.2016.05.033 [DOI] [PubMed] [Google Scholar]
- Liu X., Zou Q., Zeng B., Fang Y., Wei H. (2013). Analysis of Fecal Lactobacillus Community Structure in Patients With Early Rheumatoid Arthritis. Curr. Microbiol. 67, 170–176. doi: 10.1007/s00284-013-0338-1 [DOI] [PubMed] [Google Scholar]
- Li J., Zhao F., Wang Y., Chen J., Tao J., Tian G., et al. (2017). Gut Microbiota Dysbiosis Contributes to the Development of Hypertension. Microbiome 5, 14. doi: 10.1186/s40168-016-0222-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S., Zhuo M., Huang X., Huang Y., Zhou J., Xiong D., et al. (2020). Altered Gut Microbiota Associated With Symptom Severity in Schizophrenia. PeerJ 8, e9574. doi: 10.7717/peerj.9574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luna R. A., Oezguen N., Balderas M., Venkatachalam A., Runge J. K., Versalovic J., et al. (2016). Distinct Microbiome-Neuroimmune Signatures Correlate With Functional Abdominal Pain in Children With Autism Spectrum Disorder. Cell Mol. Gastroenterol. Hepatol. 3, 218–230. doi: 10.1016/j.jcmgh.2016.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo X. M., Edwards M. R., Mu Q., Yu Y., Vieson M. D., Reilly C. M., et al. (2018). Gut Microbiota in Human Systemic Lupus Erythematosus and a Mouse Model of Lupus. Appl. Environ. Microbiol. 84 (4), e02288–17. doi: 10.1128/AEM.02288-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma X., Asif H., Dai L., He Y., Zheng W., Wang D., et al. (2020). Alteration of the Gut Microbiome in First-Episode Drug-Naïve and Chronic Medicated Schizophrenia Correlate With Regional Brain Volumes. J. Psychiatr. Res. 123, 136–144. doi: 10.1016/j.jpsychires.2020.02.005 [DOI] [PubMed] [Google Scholar]
- Ma B., Liang J., Dai M., Wang J., Luo J., Zhang Z., et al. (2019). Altered Gut Microbiota in Chinese Children With Autism Spectrum Disorders. Front. Cell Infect. Microbiol. 9, 40. doi: 10.3389/fcimb.2019.00040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mancuso C., Santangelo R. (2018). Alzheimer’s Disease and Gut Microbiota Modifications: The Long Way Between Preclinical Studies and Clinical Evidence. Pharmacol. Res. 129, 329–336. doi: 10.1016/j.phrs.2017.12.009 [DOI] [PubMed] [Google Scholar]
- Mason B. L., Li Q., Minhajuddin A., Czysz A. H., Coughlin L. A., Hussain S. K., et al. (2020). Reduced Anti-Inflammatory Gut Microbiota Are Associated With Depression and Anhedonia. J. Affect. Disord. 266, 394–401. doi: 10.1016/j.jad.2020.01.137 [DOI] [PubMed] [Google Scholar]
- Matsuki T., Yahagi K., Mori H., Matsumoto H., Hara T., Tajima S., et al. (2016). A Key Genetic Factor for Fucosyllactose Utilization Affects Infant Gut Microbiota Development. Nat. Commun. 7, 11939. doi: 10.1038/ncomms11939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirza A., Mao-Draayer Y. (2017). The Gut Microbiome and Microbial Translocation in Multiple Sclerosis. Clin. Immunol. Orlando Fla 183, 213–224. doi: 10.1016/j.clim.2017.03.001 [DOI] [PubMed] [Google Scholar]
- Naseribafrouei A., Hestad K., Avershina E., Sekelja M., Linløkken A., Wilson R., et al. (2014). Correlation Between the Human Fecal Microbiota and Depression. Neurogastroenterol Motil. Off J. Eur. Gastrointest Motil. Soc. 26, 1155–1162. doi: 10.1111/nmo.12378 [DOI] [PubMed] [Google Scholar]
- Nguyen T. T., Kosciolek T., Maldonado Y., Daly R. E., Martin A. S., McDonald D., et al. (2019). Differences in Gut Microbiome Composition Between Persons With Chronic Schizophrenia and Healthy Comparison Subjects. Schizophr. Res. 204, 23–29. doi: 10.1016/j.schres.2018.09.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ni J., Huang R., Zhou H., Xu X., Li Y., Cao P., et al. (2019). Analysis of the Relationship Between the Degree of Dysbiosis in Gut Microbiota and Prognosis at Different Stages of Primary Hepatocellular Carcinoma. Front. Microbiol. 10, 1458. doi: 10.3389/fmicb.2019.01458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olde Loohuis L. M., Mangul S., Ori A. P. S., Jospin G., Koslicki D., Yang H. T., et al. (2018). Transcriptome Analysis in Whole Blood Reveals Increased Microbial Diversity in Schizophrenia. Transl. Psychiatry 8, 96. doi: 10.1038/s41398-018-0107-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan R., Zhang X., Gao J., Yi W., Wei Q., Su H. (2020). Analysis of the Diversity of Intestinal Microbiome and Its Potential Value as a Biomarker in Patients With Schizophrenia: A Cohort Study. Psychiatry Res. 291, 113260. doi: 10.1016/j.psychres.2020.113260 [DOI] [PubMed] [Google Scholar]
- Park A.-M., Omura S., Fujita M., Sato F., Tsunoda I. (2017). Helicobacter Pylori and Gut Microbiota in Multiple Sclerosis Versus Alzheimer’s Disease: 10 Pitfalls of Microbiome Studies. Clin. Exp. Neuroimmunol 8, 215–232. doi: 10.1111/cen3.12401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrone V., Puglisi E., Cardinali M., Schnitzler T. S., Svegliati S., Festa A., et al. (2017). Gut Microbiota Profile in Systemic Sclerosis Patients With and Without Clinical Evidence of Gastrointestinal Involvement. Sci. Rep. 7, 14874. doi: 10.1038/s41598-017-14889-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peirce J. M., Alviña K. (2019). The Role of Inflammation and the Gut Microbiome in Depression and Anxiety. J. Neurosci. Res. 97, 1223–1241. doi: 10.1002/jnr.24476 [DOI] [PubMed] [Google Scholar]
- Plaza-Díaz J., Gómez-Fernández A., Chueca N., de la Torre-Aguilar M. J., Gil Á, Perez-Navero J. L., et al. (2019). Autism Spectrum Disorder (ASD) With and Without Mental Regression Is Associated With Changes in the Fecal Microbiota. Nutrients 11(2), 337–349. doi: 10.3390/nu11020337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proctor C., Thiennimitr P., Chattipakorn N., Chattipakorn S. C. (2017). Diet, Gut Microbiota and Cognition. Metab. Brain Dis. 32, 1–17. doi: 10.1007/s11011-016-9917-8 [DOI] [PubMed] [Google Scholar]
- Pulikkan J., Maji A., Dhakan D. B., Saxena R., Mohan B., Anto M. M., et al. (2018). Gut Microbial Dysbiosis in Indian Children With Autism Spectrum Disorders. Microb. Ecol. 76, 1102–1114. doi: 10.1007/s00248-018-1176-2 [DOI] [PubMed] [Google Scholar]
- Rice M. W., Pandya J. D., Shear D. A. (2019). Gut Microbiota as a Therapeutic Target to Ameliorate the Biochemical, Neuroanatomical, and Behavioral Effects of Traumatic Brain Injuries. Front. Neurol. 10, 875. doi: 10.3389/fneur.2019.00875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rong H., Xie X., Zhao J., Lai W., Wang M., Xu D., et al. (2019). Similarly in Depression, Nuances of Gut Microbiota: Evidences From a Shotgun Metagenomics Sequencing Study on Major Depressive Disorder Versus Bipolar Disorder With Current Major Depressive Episode Patients. J. Psychiatr. Res. 113, 90–99. doi: 10.1016/j.jpsychires.2019.03.017 [DOI] [PubMed] [Google Scholar]
- Rose D. R., Yang H., Serena G., Sturgeon C., Ma B., Careaga M., et al. (2018). Differential Immune Responses and Microbiota Profiles in Children With Autism Spectrum Disorders and Co-Morbid Gastrointestinal Symptoms. Brain Behav. Immun. 70, 354–368. doi: 10.1016/j.bbi.2018.03.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russo R., Cristiano C., Avagliano C., De Caro C., La Rana G., Raso G. M., et al. (2018). Gut-Brain Axis: Role of Lipids in the Regulation of Inflammation, Pain and CNS Diseases. Curr. Med. Chem. 25, 3930–3952. doi: 10.2174/0929867324666170216113756 [DOI] [PubMed] [Google Scholar]
- Sandhu K. V., Sherwin E., Schellekens H., Stanton C., Dinan T. G., Cryan J. F. (2017). Feeding the Microbiota-Gut-Brain Axis: Diet, Microbiome, and Neuropsychiatry. Transl. Res. J. Lab. Clin. Med. 179, 223–244. doi: 10.1016/j.trsl.2016.10.002 [DOI] [PubMed] [Google Scholar]
- Sasmita A. O. (2019). Modification of the Gut Microbiome to Combat Neurodegeneration. Rev. Neurosci 30 (8), 795–805. doi: 10.1515/revneuro-2019-0005 [DOI] [PubMed] [Google Scholar]
- Saurman V., Margolis K. G., Luna R. A. (2020). Autism Spectrum Disorder as a Brain-Gut-Microbiome Axis Disorder. Dig Dis. Sci. 65, 818–828. doi: 10.1007/s10620-020-06133-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarz E., Maukonen J., Hyytiäinen T., Kieseppä T., Orešič M., Sabunciyan S., et al. (2018). Analysis of Microbiota in First Episode Psychosis Identifies Preliminary Associations With Symptom Severity and Treatment Response. Schizophr. Res. 192, 398–403. doi: 10.1016/j.schres.2017.04.017 [DOI] [PubMed] [Google Scholar]
- Seguella L., Capuano R., Sarnelli G., Esposito G. (2019). Play in Advance Against Neurodegeneration: Exploring Enteric Glial Cells in Gut-Brain Axis During Neurodegenerative Diseases. Expert Rev. Clin. Pharmacol. 12, 555–564. doi: 10.1080/17512433.2019.1612744 [DOI] [PubMed] [Google Scholar]
- Shen Y., Xu J., Li Z., Huang Y., Yuan Y., Wang J., et al. (2018). Analysis of Gut Microbiota Diversity and Auxiliary Diagnosis as a Biomarker in Patients With Schizophrenia: A Cross-Sectional Study. Schizophr. Res. 197, 470–477. doi: 10.1016/j.schres.2018.01.002 [DOI] [PubMed] [Google Scholar]
- Simões C. D., Maukonen J., Kaprio J., Rissanen A., Pietiläinen K. H., Saarela M. (2013). Habitual Dietary Intake Is Associated With Stool Microbiota Composition in Monozygotic Twins. J. Nutr. 143, 417–423. doi: 10.3945/jn.112.166322 [DOI] [PubMed] [Google Scholar]
- Son J. S., Zheng L. J., Rowehl L. M., Tian X., Zhang Y., Zhu W., et al. (2015). Comparison of Fecal Microbiota in Children With Autism Spectrum Disorders and Neurotypical Siblings in the Simons Simplex Collection. PloS One 10, e0137725. doi: 10.1371/journal.pone.0137725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinelli E., Blackford R. Gut Microbiota, the Ketogenic Diet and Epilepsy. Pediatr. Neurol. Briefs (2018) 32, 10. doi: 10.15844/pedneurbriefs-32-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stilling R. M., Dinan T. G., Cryan J. F. (2014). Microbial Genes, Brain & Behaviour - Epigenetic Regulation of the Gut-Brain Axis. Genes Brain Behav. 13, 69–86. doi: 10.1111/gbb.12109 [DOI] [PubMed] [Google Scholar]
- Strati F., Cavalieri D., Albanese D., De Felice C., Donati C., Hayek J., et al. (2016). Altered Gut Microbiota in Rett Syndrome. Microbiome 4, 41. doi: 10.1186/s40168-016-0185-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strati F., Cavalieri D., Albanese D., De Felice C., Donati C., Hayek J., et al. (2017). New Evidences on the Altered Gut Microbiota in Autism Spectrum Disorders. Microbiome 5 (1), 24. doi: 10.1186/s40168-017-0242-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun M.-F., Shen Y.-Q. (2018). Dysbiosis of Gut Microbiota and Microbial Metabolites in Parkinson’s Disease. Ageing Res. Rev. 45, 53–61. doi: 10.1016/j.arr.2018.04.004 [DOI] [PubMed] [Google Scholar]
- Sun H., You Z., Jia L., Wang F. (2019). Autism Spectrum Disorder Is Associated With Gut Microbiota Disorder in Children. BMC Pediatr. 19, 516. doi: 10.1186/s12887-019-1896-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun M.-F., Zhu Y.-L., Zhou Z.-L., Jia X.-B., Xu Y.-D., Yang Q., et al. (2018). Neuroprotective Effects of Fecal Microbiota Transplantation on MPTP-Induced Parkinson’s Disease Mice: Gut Microbiota, Glial Reaction and TLR4/TNF-α Signaling Pathway. Brain Behav. Immun. 70, 48–60. doi: 10.1016/j.bbi.2018.02.005 [DOI] [PubMed] [Google Scholar]
- Tomova A., Husarova V., Lakatosova S., Bakos J., Vlkova B., Babinska K., et al. (2015). Gastrointestinal Microbiota in Children With Autism in Slovakia. Physiol. Behav. 138, 179–187. doi: 10.1016/j.physbeh.2014.10.033 [DOI] [PubMed] [Google Scholar]
- Tsunoda I. (2017). Lymphatic System and Gut Microbiota Affect Immunopathology of Neuroinflammatory Diseases, Including Multiple Sclerosis, Neuromyelitis Optica and Alzheimer’s Disease. Clin. Exp. Neuroimmunol 8, 177–179. doi: 10.1111/cen3.12405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valles-Colomer M., Falony G., Darzi Y., Tigchelaar E. F., Wang J., Tito R. Y., et al. (2019). The Neuroactive Potential of the Human Gut Microbiota in Quality of Life and Depression. Nat. Microbiol. 4, 623–632. doi: 10.1038/s41564-018-0337-x [DOI] [PubMed] [Google Scholar]
- Ventura R. E., Iizumi T., Battaglia T., Liu M., Perez-Perez G. I., Herbert J., et al. (2019). Gut Microbiome of Treatment-Naïve MS Patients of Different Ethnicities Early in Disease Course. Sci. Rep. 9, 16396. doi: 10.1038/s41598-019-52894-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinberg M., Ottesen N. M., Meluken I., Sørensen N., Pedersen O., Kessing L. V., et al. (2019). Remitted Affective Disorders and High Familial Risk of Affective Disorders Associate With Aberrant Intestinal Microbiota. Acta Psychiatr. Scand. 139, 174–184. doi: 10.1111/acps.12976 [DOI] [PubMed] [Google Scholar]
- Wang L., Christophersen C. T., Sorich M. J., Gerber J. P., Angley M. T., Conlon M. A. (2011). Low Relative Abundances of the Mucolytic Bacterium Akkermansia Muciniphila and Bifidobacterium Spp. In Feces of Children With Autism. Appl. Environ. Microbiol. 77, 6718–6721. doi: 10.1128/AEM.05212-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Kasper L. H. (2014). The Role of Microbiome in Central Nervous System Disorders. Brain Behav. Immun. 38, 1–12. doi: 10.1016/j.bbi.2013.12.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang M., Wan J., Rong H., He F., Wang H., Zhou J., et al. (2019). Alterations in Gut Glutamate Metabolism Associated With Changes in Gut Microbiota Composition in Children With Autism Spectrum Disorder. mSystems 4 (1), e00321–18. doi: 10.1128/mSystems.00321-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu R., Tan C., Zhu J., Zeng X., Gao X., Wu Q., et al. (2019). Dysbiosis of the Intestinal Microbiota in Neurocritically Ill Patients and the Risk for Death. Crit. Care Lond Engl. 23, 195. doi: 10.1186/s13054-019-2488-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu R., Wu B., Liang J., He F., Gu W., Li K., et al. (2019). Altered Gut Microbiota and Mucosal Immunity in Patients With Schizophrenia. Brain Behav. Immun 85, 120–7. doi: 10.1016/j.bbi.2019.06.039 [DOI] [PubMed] [Google Scholar]
- Xu R., Wu B., Liang J., He F., Gu W., Li K., et al. (2020). Altered Gut Microbiota and Mucosal Immunity in Patients With Schizophrenia. Brain Behav. Immun. 85, 120–127. doi: 10.1016/j.bbi.2019.06.039 [DOI] [PubMed] [Google Scholar]
- Yan Q., Gu Y., Li X., Yang W., Jia L., Chen C., et al. (2017). Alterations of the Gut Microbiome in Hypertension. Front. Cell Infect. Microbiol. 7, 381. doi: 10.3389/fcimb.2017.00381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye Z., Zhang N., Wu C., Zhang X., Wang Q., Huang X., et al. (2018). A Metagenomic Study of the Gut Microbiome in Behcet’s Disease. Microbiome 6, 135. doi: 10.1186/s40168-018-0520-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yolken R. H., Severance E. G., Sabunciyan S., Gressitt K. L., Chen O., Stallings C., et al. (2015). Metagenomic Sequencing Indicates That the Oropharyngeal Phageome of Individuals With Schizophrenia Differs From That of Controls. Schizophr. Bull. 41, 1153–1161. doi: 10.1093/schbul/sbu197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhai Q., Cen S., Jiang J., Zhao J., Zhang H., Chen W. (2019). Disturbance of Trace Element and Gut Microbiota Profiles as Indicators of Autism Spectrum Disorder: A Pilot Study of Chinese Children. Environ. Res. 171, 501–509. doi: 10.1016/j.envres.2019.01.060 [DOI] [PubMed] [Google Scholar]
- Zhang M., Ma W., Zhang J., He Y., Wang J. (2018). Analysis of Gut Microbiota Profiles and Microbe-Disease Associations in Children With Autism Spectrum Disorders in China. Sci. Rep. 8 (1), 13981. doi: 10.1038/s41598-018-32219-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X., Pan L.-Y., Zhang Z., Zhou Y.-Y., Jiang H.-Y., Ruan B. (2020). Analysis of Gut Mycobiota in First-Episode, Drug-Naïve Chinese Patients With Schizophrenia: A Pilot Study. Behav. Brain Res. 379, 112374. doi: 10.1016/j.bbr.2019.112374 [DOI] [PubMed] [Google Scholar]
- Zhang Y.-G., Wu S., Yi J., Xia Y., Jin D., Zhou J., et al. (2017). Target Intestinal Microbiota to Alleviate Disease Progression in Amyotrophic Lateral Sclerosis. Clin. Ther. 39, 322–336. doi: 10.1016/j.clinthera.2016.12.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Zhou S., Zhou Y., Yu L., Zhang L., Wang Y. (2018). Altered Gut Microbiome Composition in Children With Refractory Epilepsy After Ketogenic Diet. Epilepsy Res. 145, 163–168. doi: 10.1016/j.eplepsyres.2018.06.015 [DOI] [PubMed] [Google Scholar]
- Zheng P., Yang J., Li Y., Wu J., Liang W., Yin B., et al. (2020). Gut Microbial Signatures Can Discriminate Unipolar From Bipolar Depression. Adv. Sci. 7(7), 1902862. doi: 10.1002/advs.201902862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng P., Zeng B., Zhou C., Liu M., Fang Z., Xu X., et al. (2016). Gut Microbiome Remodeling Induces Depressive-Like Behaviors Through a Pathway Mediated by the Host’s Metabolism. Mol. Psychiatry 21, 786–796. doi: 10.1038/mp.2016.44 [DOI] [PubMed] [Google Scholar]
- Zhou Y., Chen C., Yu H., Yang Z. (2020). Fecal Microbiota Changes in Patients With Postpartum Depressive Disorder. Front. Cell Infect. Microbiol. 10, 567268. doi: 10.3389/fcimb.2020.567268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zmora N., Suez J., Elinav E. (2019). You Are What You Eat: Diet, Health and the Gut Microbiota. Nat. Rev. Gastroenterol. Hepatol. 16, 35–56. doi: 10.1038/s41575-018-0061-2 [DOI] [PubMed] [Google Scholar]
- Zou R., Xu F., Wang Y., Duan M., Guo M., Zhang Q., et al. (2020). Changes in the Gut Microbiota of Children With Autism Spectrum Disorder. Autism Res. 13, 1614–1625. doi: 10.1002/aur.2358 [DOI] [PubMed] [Google Scholar]
- Zuo K., Li J., Xu Q., Hu C., Gao Y., Chen M., et al. (2019). Dysbiotic Gut Microbes May Contribute to Hypertension by Limiting Vitamin D Production. Clin. Cardiol. 42, 710–719. doi: 10.1002/clc.23195 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.