Abstract
Purpose
Our analysis focuses explicitly on applying two sonographic and morphological indexes (sesamoid index and subsesamoid index) to better evaluate post-traumatic consequences to the sesamoids of the first finger.
Methods
In 2 years, we enrolled 75 patients, divided into two groups: 60 without any history of trauma and 15 reporting hyperextension trauma of the first finger. We performed clinical and instrumental examinations (sonography and X-ray) on patients with one or more symptoms compatible with sesamoiditis, while an MRI scan was performed only on patients with an acute onset and severe symptomatology. We measured both the short and long-axis diameter (in mm) for each sesamoid as well as the relation between the two parameters (sesamoid index, SI and subsesamoid index, SubI).
Results
All 15 patients showed sonographic alterations of the SI above the reference range, while the alterations of SubI varied according to the acuteness and gravity of trauma. In all cases, the X-ray did not show any relevant alterations. MRI scans in patients with acute symptoms confirmed the sonographic findings.
Conclusion
Sonography enabled diagnosis of micro-injuries which were invisible to X-Ray and allowed to detect possible damages to the sesamoid complex, providing a qualitative and quantitative evaluations of the post-traumatic alteration of the metacarpophalangeal joint of the 1st finger and is therefore valid, combined with clinical examination and hand X-ray, in the evaluation of sesamoiditis without the need to perform further examinations.
Keywords: Hand ultrasound, Pathological sesamoid bones, First finger hyperextension trauma, Sesamoid index, Subsesamoid index
Introduction
Sesamoid bones (or sesamoids) are located within certain joints or tendons; their function is to modify the direction of the tendon thereby modifying pressure and reducing friction.
Two typical sesamoid bones are located within the metacarpophalangeal joint of the 1st finger (MCP) on the hand's palmar surface; they are connected with the anterior border of the condyles of the metacarpal bone. The condylar head is concave in the ulnar area where the ulnar sesamoid is located, while it is convex in the radial area where the radial sesamoid is located. The flexor pollicis brevis tendon is inserted on the radial sesamoid, while the tendon of the adductor pollicis is inserted on the ulnar sesamoid.
Sesamoid bone pathology is barely known, undervalued, and often not diagnosed due to the extremely heterogeneous clinical presentation, characterized by pain, crepitus, reduced functionality, articular instability, and swelling. A non-infectious inflammatory process often causes sesamoiditis, mostly for the 1st finger due to many etiopathogenetic mechanisms, such as chronic and acute post-traumatic events.
We applied two sonographic indexes (sesamoid index, SI, and subsesamoid index, SubI) for a better evaluation of the sesamoid complex in post-traumatic alterations following a hyperextension trauma of the 1st finger, such as sesamoiditis, peritendinitis, and metacarpal sesamoid joint instability.
Materials and methods
A control group was created, which included 60 healthy people (30 men and 30 women, 25–34 years, mean age 29 years); exclusion criteria covered history of previous hand trauma and history of any rheumatological disease, potentially responsible for sesamoid bones alteration. Subsequently, we enrolled 15 patients (8 men and 7 women, mean age 28 years) admitted for a contusive-distortive trauma following thumb hyperextension; medical history was also collected, particularly the time elapsed from the trauma and the onset of symptoms (1–24 months, with an average of 5 months) and the kind of symptoms reported (acute pain 26%, chronic pain 46%, crepitation 46%, reduced functionality 60%, joint instability 46% and swelling 40%).
All patients underwent an X-ray of the hand as part of their diagnostic routine before the US examination; the radiologist who reported the X-rays and the one performing ultrasound did not exchange information. A written informed consent was obtained from all subjects; subsequently, both the control group and the patients underwent the US examination, which was performed with two Aplio XV scanners (Toshiba, Japan), both equipped with a multifrequency linear probe (7.5–15 MHz). The Color- and Power Doppler were set with technical parameters to detect both slow and low volume flows. The pulse repetition frequency used was 600–1000 Hz, whereas the bandpass filter was set at 50 Hz. The use of Color (CD) and Power Doppler (PD) techniques would help in detecting vascular alterations, compatible with increased vascularity or neovascularization phenomena.
For each sesamoid, two standard scans were performed: a transverse scan, to evaluate short-axis diameter (mm), and a longitudinal scan, to evaluate long-axis diameter (mm). We used the measured parameters of each sesamoid to calculate two indexes: the traditional sesamoid index (SI), radiographically measured and applied at present in the study of metabolic and rheumatological diseases, and the subsesamoid index (SubI), introduced in this study and defined as the space between the sesamoid facet joint and the corresponding metacarpal condylar head.
In 7 patients with a recent acute trauma (< 3 months from the traumatic event), with more than one clinical symptoms (swelling, severe pain, crepitations, reduced functionality, and joint instability) we performed MRI as confirmation of our sonographic findings (MRI with low field magnet, T1-weighted, T2-weighted, and GE-STIR on axial coronal and sagittal planes).
Results
In all 15 cases, according to the reporting radiologist, the X-ray did not show relevant alteration.
All 15 patients showed sonographic alterations of the sesamoid index above the reference values (18 ± 5.1 mm for the radial sesamoid and 15.7 ± 5 mm for the ulnar sesamoid): the abnormal values observed were 35.8 mm for the radial sesamoid and 32 mm for the ulnar sesamoid, with a statistical significance (p < 0.05). Four patients showed abnormal sesamoid index values for one sesamoid only: 3 patients in the radial one (31 < SI < 63 mm) and 1 patient for the ulnar one (SI = 34.5 mm). In 6 cases out of 15, the affected hand was the dominant one.
Nine patients out of 15 (60%) showed an alteration of the SubI: 3 patients with chronic symptoms (between 18–24 months from the event) showed a value almost equal to 0 mm (below the reference values, which were 1.6 mm for the radial side and 1.8 mm for the ulnar side); 6 patients with the most recent onset and more severe symptoms, showed values above the norm between (3.8 and 9.1 mm) (Table1).
Table 1.
Normal and abnormal values of SI and SubI for each sesamoid bone, in control group, acute and chronic post-traumatic patients
| Radial long axis (mm) | Radial short axis(mm) | Ulnar long axis (mm) | Ulnar short axis (mm) | Radial sesamoid index (mm) | Ulnar sesamoid Index (mm) | Radial subsesamoid index (mm) | Ulnar subsesamoid index (mm) | |
|---|---|---|---|---|---|---|---|---|
| Normal values |
M: 5.1 ± 0.5 F: 5.1 ± 0.5 |
M 3.8 ± 0.8 F 3.8 ± 0,8 |
M: 4.6 ± 0.6 F: 4.4 ± 0.9 |
M: 3.6 ± 0.8 F: 3.5 ± 0.8 |
M: 18.5 ± 4.9 F: 18.5 ± 5.3 |
M: 16.2 ± 4.8 F: 15.2 ± 5.2 |
M: 1.8 ± 0.2 F: 2.6 ± 0.8 |
M: 2.5 ± 0.7 F: 2.8 ± 0.9 |
| Acute patients values (n = 7) |
M: 6.7 ± 0.6 F: 6.7 ± 0.6 |
M:5.8 ± 0.7 F: 5.8 ± 0.7 |
M: 6.2 ± 0.5 F: 6.4 ± 0.5 |
M: 5.6 ± 0.7 F: 5.5 ± 0.6 |
M: 35 ± 0.2 F: 34 ± 0.4 |
M: 27 ± 0.7 F: 26 ± 0.6 |
M: 2.6 ± 0.5 F: 3.7 ± 0.3 |
M:3.6 ± 0.4 F: 4.1 ± 0.4 |
| Chronic patients values (n = 8) |
M: 6.1 ± 0.2 F: 6.3 ± 0.3 |
M:5.5 ± 0.2 F: 5.6 ± 0.4 |
M: 6.3 ± 0.6 F: 6.5 ± 0.4 |
M: 5.4 ± 0.3 F: 5.2 ± 0.5 |
M: 35 ± 0.2 F: 34 ± 0.4 |
M: 25 ± 0.5 F: 23 ± 0.2 |
M: 1.5 ± 0.8 F: 1.7 ± 0.9 |
M: 1.4 ± 0.9 F: 1.5 ± 0.9 |
All those patients who showed morphological and morphometric alterations revealed related signs: 8 patients (53%) showed osteophytosis; 2 patients (13%) had alterations compatible with tendon injuries; 5 patients (33%) had sesamoid complex inflammatory alterations (due to the abundant amount of peri-sesamoid hypoechoic tissue, intensely vascularized at CD/PD exams); 10 patients (66%) showed alterations compatible with a palmar plate fracture; 3 patients (20%) showed micro-fracture of the bone plate; 8 patients (53%) showed sesamoid dislocation compared to its normal site.
MRI scans performed in the 7 patients with a more recent trauma and severe symptomatology (< 3 months, more than one symptoms), showed alterations in T2* and STIR-sequences compatible with the US findings.
Discussion
Sesamoiditis can be both a chronic and acute inflammatory process, which often affects the radial and ulnar sesamoid of the 1st finger [1–3]. Pathogenesis is heterogeneous but frequently has a traumatic or degenerative origin. When it appears with an acute symptomatology, it is characterized by fast pain onset, local swelling, reduced functionality of the involved joint, but it may appear with a chronic symptomatology, characterized by local pain and associated with joint instability [1, 4, 5].
So far, this condition is diagnosed with clinical findings supported by traditional X-ray [6, 7]. However, in many cases, sesamoiditis is misdiagnosed because of aspecific symptoms and signs that lead general practitioners (GP) and orthopaedists to misdiagnose it with more frequent conditions (tenosynovitis and peritendinitis both of the flexor brevis muscle and adductor longus muscle); moreover, X-Ray exams are often negative or inconclusive.
In our group of cases, the GP assumed a provisional diagnosis of a sesamoid disease for only 1 patient out of 15 (6%). In most cases (66%), tendons and peritendons pathology (inflammatory or traumatic) were misdiagnosed.
Due to the low sensitivity of traditional X-ray exams, in case of clinical suspicion of sesamoiditis, we have considered the possibility of introducing ultrasound to diagnose the sesamoid pathology related to contusive-distortive trauma in hyperextension of the 1st finger (e.g., falling with hands in a position of defense).
We calculated the SI with ultrasound, only measured thus far with X-ray and previously applied in the evaluation of metabolic and rheumatological bone disease, such as psoriatic arthritis and acromegaly. Since we believe that the SI does not evaluate the joint space between the sesamoid inferior portion and the corresponding metacarpal head, which should be affected by traumatic and inflammatory disease of the sesamoid complex, we introduced the SubI, intended as a parameter which should reflect more precisely the damage to the joint space; we hypothesized that the SubI could be increased in acute disease, reflecting the typical swelling of the joint space, whereas it could be decreased in chronic conditions, as a consequence of damage to the joint cartilage [8]. In our opinion, these two morphostructural sonographic indexes combined can detect specific pathological patterns related to acute and chronic inflammatory processes (Fig. 1), even detecting micro-fractures and subluxations (Fig. 2).
Fig. 1.

Patient n° 3 Acute ulnar sesamoid: increase of the sub-sesamoid index (9.1 mm) due to the abundant amount of inflammatory hypoechoic tissue, sometimes profusely vascularized. The bone profile results smooth, regular, naturally convex.
Fig. 2.
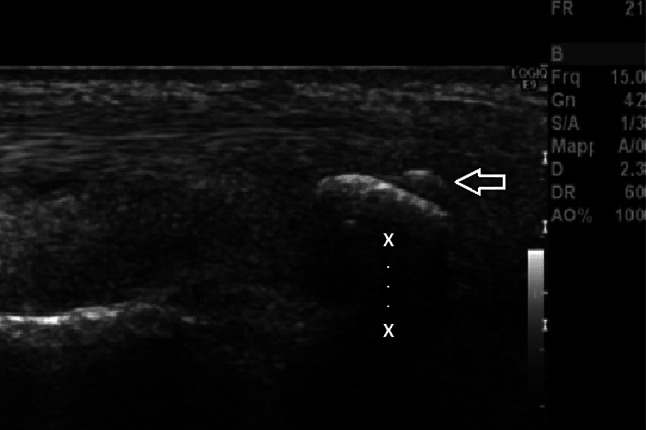
Patient n° 12 with micro injury of the ulnar sesamoid (empty arrow). Increase of the ulnar sub-sesamoid index (4 mm) caused by a bone micro fragment within the tendon of the flexor pollicis longus muscle and the superior sesamoid profile (fracture invisible to X-ray)
The values we measured with sonography in our control group agree with what has been highlighted in other similar studies available in literature [9–12].
We observed values of SubI in post-traumatic patients both above and below normal values. The above-average values observed for SubI (6/15 patients, those affected by acute trauma and more severe symptomatology), agree with the association of increased subsesamoid space due to micro-fractures, edemigenous and inflammatory phenomena, confirming the clinical suspicions of acute post-traumatic sesamoiditis. Nine patients out of 15 showed sub-average or average SubI values: we can assume that other acute/chronic alteration found in these patients on ultrasound examination (such as osteophytosis and dislocation), might have reduced the sub-sesamoid space bringing it closer to the normal range, despite the condition observed and the abnormal SI. As a matter of fact, in approximately 50% of cases, both sesamoids showed osteophytosis, another diagnostic element of chronic post-traumatic arthritis that is simple to detect with sonography (Fig. 3). Two cases showed a virtually absent SubI, and this helped us diagnose an overlapping syndrome caused by the entrapment of the sesamoid within the intercondylar space [13] (Fig. 4).
Fig. 3.

Post traumatic radial osteophytosis: sesamoid index within standard level (19.6 mm), post-traumatic chronic arthritis framework with a highly visible radial sesamoid bones osteophytosis (arrows)
Fig. 4.

Patient n° 12 with overlapping syndrome: aiming at studying the radial sesamoid we performed a longitudinal scan putting the 1st finger in passive hyperextension, since the radial sub-sesamoid index was equal to 0 (the metacarpus is not horizontal, empty arrow)
The integration between SI and SubI and the Color-Power Doppler was helpful, because we could detect vascularized perisesamoid hypoechoic tissue, compatible with a neoangiogenesis (Fig. 5). We performed MRI only in acute patients as a confirmation of our sonographic findings, assuming that it could be unnecessary considering that the combination of the morphological and functional sonographic parameters grants an accurate and readily available technique.
Fig. 5.
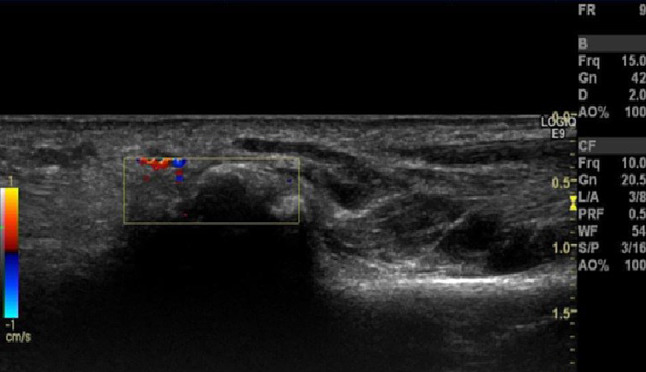
Patient n°11 with chronic radial sesamoiditis: within standard level sub-sesamoid index, presence of perisesamoid hypoechoic tissue nearby the radial sesamoid, with significant vascularization
Limitations of this study include the inability of ultrasound to provide a precise evaluation of the region underlying the bone, therefore measurement of SubI was difficult at times. Although it was conducted in a blind fashion, as the radiologist who reported the X-rays and the one performing ultrasound did not communicate with each other, the study is not randomized and involved only one experienced operator, which can be misleading because this particular application of sonography may provide unpredictable results in unexperienced hands. Finally, only a small number of patients was considered and studied, with MRI being performed only in patients with an acute onset of symptoms.
Conclusion
Sonography, with its affordability and its possibility to perform multi-planar scans, allows diagnosis of micro-injuries often invisible to X-ray as well as the detection of possible damages to the support system of the sesamoid (palmar plate) and nearby structures (e.g., the tendon of the flexor pollicis long muscle). New sonographic morphological indexes (SI and SubI), combined with a qualitative evaluation of the surrounding soft tissues (vascularization and neoangiogenesis), could enforce a clinical suspicion of inflammatory sesamoidal disease, possibly making it a first-line exam, without the need to perform further examinations.
Compliance with ethical standards
Conflict of interest
Marianna Glorioso, Stefano Perri, Valentina Lombardo, Martina Di Brino and Francesco Giovagnorio declare that they have no conflict of interest.
Ethical approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions.
Informed consent
Informed consent was obtained from all the patients.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Marianna Glorioso, Email: mariannagl@libero.it.
Stefano Perri, Email: Stefano.perri@uniroma1.it.
Valentina Lombardo, Email: Cv.lombardo@libero.it.
Martina Di Brino, Email: martina.dibrino@gmail.com.
Francesco Giovagnorio, Email: Francesco.giovagnorio@uniroma1.it.
References
- 1.Mohler LR, Trumble TE. Disorders of the thumb sesamoids. Hand Clin. 2001;17:291–301. doi: 10.1016/S0749-0712(21)00249-3. [DOI] [PubMed] [Google Scholar]
- 2.Wood VE. The sesamoid bones of the hand and their pathology. J Hand Surg Br. 1984;9(3):261–264. doi: 10.1016/0266-7681(84)90038-X. [DOI] [PubMed] [Google Scholar]
- 3.Bruser P. Pathology of the sesamoid bones of the hand. Handchir Mikrochir Plast Chir. 1994;110:302–306. [PubMed] [Google Scholar]
- 4.Van der Voort JH, Kon M. Chronic Painful sesamoids of the thumb. Arch Orthop Trauma Surg. 1990;110:22–23. doi: 10.1007/BF00431360. [DOI] [PubMed] [Google Scholar]
- 5.Parks BJ, Hamlin C. Chronic sesamoiditis of the thumb: pathomecanics and treatment. J Hand Surg Am. 1985;10:94–110. doi: 10.1016/S0363-5023(85)80257-4. [DOI] [PubMed] [Google Scholar]
- 6.Trumble TE, Watson HK. Post traumatic sesamoid arthritis of the metacarpophalangeal joint of the thumb. J Hand Surg Am. 1985;10:94–110. doi: 10.1016/S0363-5023(85)80257-4. [DOI] [PubMed] [Google Scholar]
- 7.Mohler LR, Trumble TE. Disorders of the thumb sesamoids. Hand Clin. 2001;1:291–301. doi: 10.1016/S0749-0712(21)00249-3. [DOI] [PubMed] [Google Scholar]
- 8.Glorioso M, Miozzi F, Sartori A, et al. Morphometric evaluation of sesamoid bones of the first meta-carpophalangeal joint with ultrasound. Clin Ter. 2013;164(6):e449–e452. doi: 10.7417/CT.2013.1635. [DOI] [PubMed] [Google Scholar]
- 9.Whitehouse RW, Aslam R, Bukhari M, et al. The sesamoid index in psoriatic arthropathy. Skeletal Radiol. 2005;34(4):217–220. doi: 10.1007/s00256-004-0823-5. [DOI] [PubMed] [Google Scholar]
- 10.Sabet D, Stark AR. Sesamoid index of the foot in acromegaly. J Am Podiatr Med Assoc. 1981;71(11):625–627. doi: 10.7547/87507315-71-11-625. [DOI] [PubMed] [Google Scholar]
- 11.Duncan TR. Validity of the sesamoid index in the diagnosis of acromegaly. Radiology. 1975;115:617–619. doi: 10.1148/15.3.617. [DOI] [PubMed] [Google Scholar]
- 12.Balaji RA, Apoorva V, Katti V, et al. Morphological and topographic anatomy of sesamoid bones of human thumb. Muscles Ligaments Tendons J (MLTJ) 2020;10(1):138–143. doi: 10.32098/mltj.01.2020.19. [DOI] [Google Scholar]
- 13.Sze-Chung C, Chi-Hung Y, Wing-Cheung W, et al. Cadaveric study of locked thumb metacarpophalangeal joint caused by entrapment of radial sesamoid bone. J Orthop Trauma Rehabil. 2011;15:2–4. [Google Scholar]


