Abstract
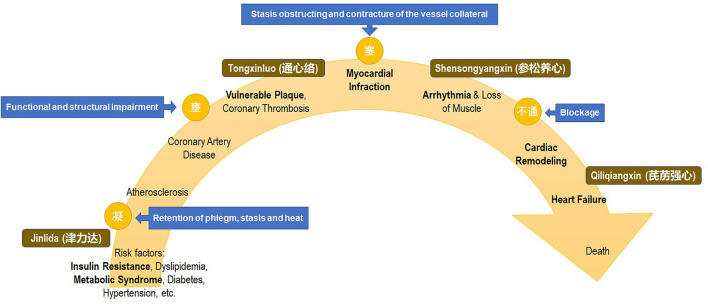
Cardiovascular disease has become a major public health problem. The concept of “cardiovascular continuum” refers to the continuous process from the risk factors that lead to arteriosclerosis, vulnerable plaque rupture, myocardial infarction, arrhythmia, heart failure, and death. These characteristics of etiology and progressive development coincide with the idea of “preventing disease” in traditional Chinese medicine (TCM), which corresponds to the process of systemic intervention. With the update of the understanding via translational medicine, this article reviews the current evidence of the TCM collateral disease theory set prescriptions in both mechanical and clinical aspects, which could lead to the development of new therapeutic strategies for prevention and treatment.
Keywords: cardiovascular disease, cardiovascular continuum, translational medicine, traditional Chinese medicine, set prescriptions
Background
The cardiovascular continuum refers to a chain of events that begins from a host of cardiovascular risk factors and continues as a progressive pathogenic process leading to late complications, such as heart failure and myocardial infarction (Dzau and Braunwald, 1991). Despite the recent advancement in cardiovascular disease (CVD) management, population aging and social development continue to contribute to the growing economic and social burden (Glovaci et al., 2019).
Traditional Chinese medicine (TCM) has years of accumulated experience in disease management. TCM was often considered as a complementary and alternative approach to the primary and secondary prevention of CVDs (Xu et al., 2013). Although the efficacy and safety of TCM remain to be explored (Hao et al., 2017), the emerging evidence has shown their unique pharmacological effects of various active ingredients on the cardiovascular system and potential mechanisms on improving outcomes in patients with CVDs. Also, the generalization of the TCM has been restricted to the Chinese community due to the language limitations, the regionality of the origin, and the incomprehensible abstract theory. TCM needs to be further confirmed by modern medical theory and translates in the modern and uniform linguistic system in order to be widely recognized internationally.
The collateral disease theory is one of the major theoretical systems of the TCM (Ma Y. et al., 2016; Hao et al., 2017). While the main channel system has been emphasized in the past, collateral disease theory has been inexplicably neglected. The collateral disease theory has been emerging along with the development of TCM. In the aspect of collateral disease, diseases are caused by the blockage of meridian qi and blood, which is interestingly in line with the modern “cardiovascular continuum” fundamental mechanism (Wu, 2009).
Herein, the aim of this review was to introduce the research regarding these TCM set prescriptions in recent years, and to integrate the past evidence address of their possible therapeutic mechanism toward cardiovascular diseases.
Prescriptions of Collateral Disease Theory in the Cardiovascular Continuum
Regarding these overlapped key nodes of the cardiovascular continuum, there are TCM set prescriptions based on collateral disease that could offer intervention targets at various continuum stages (Figure 1). For example, Jinlida granules (JLDG) for metabolic syndrome, Tongxinluo (TXL) for atherosclerotic plaque and myocardial protection, Shensongyangxin (SSYX) capsules for anti-arrhythmias via metabolic reconstruction, and Qiliqiangxin (QLQX) capsules for cardiac remodeling and heart failure have been recognized under the guidance of translational medicine (Table 1) (Bai et al., 2013; Wang et al., 2014; Zaki et al., 2014; Luan et al., 2015; Wang et al., 2015; Zhang et al., 2016; Fan et al., 2017; Shen et al., 2017; Zhao et al., 2017; Chen H. et al., 2018; Chen Y. et al., 2018; Gao et al., 2018; Wang et al., 2018; Zhang et al., 2018; Lyu et al., 2019; Tung et al., 2019; Zhou et al., 2019; Cheng W. et al., 2020; Li et al., 2020; Yang et al., 2020; Zhao et al., 2020; Jiang et al., 2021; Hao et al., 2022). These set prescriptions have been approved for by the Chinese National Medical Products Administration (NMPA), and broadly used in clinical practice in the Chinese community. However, the exact mechanism of these medicines on the modern evidence-based aspects was lacking in evidence-based translation to the modern medicine in the past.
FIGURE 1.
Cardiovascular continuum and intervention with traditional Chinese medicine set prescription of collateral disease theory.
TABLE 1.
Components of the set prescriptions.
| Set prescription | Species | Number of components | Representative herbs | Bioactive ingredients | Potential related mechanisms |
|---|---|---|---|---|---|
| Jinlida granules (JLDG) | Panax ginseng C.A. Meyer, Polygonatum kingianum Coll. et Hemsl, Atractylodes lancea (Thunb.) DC, Sophora flavescens Ait, Ophiopogon japonicas (L.f) Ker-Gawl, Rehmanniag lutinosa Libosch, Polygonum multiflorum Thunb, Cornus officinalis Sieb.et Zucc, Poriacocos (Schw.) Wolf, Eupatorium fortune Turcz, Coptis chinensis Franch., Anemarrhena asphodgfoides Bge, Epimedium brevicornu Maxim, Salvia miltiorrhiza Bge., Lycium chinense Mill., Pueraria lobata (Willd.) Ohwi, Litchi chinensis Sonn | 17 | Panax ginseng, Sophorae flavescentis Radix, Polygonati Rhizoma, Atractylodis Rhizoma | Ginsenosides (Rb1, Rc, Rb2), salvianic acid epimedin (B, C), Atractylodin, icariin | Metabolic regulation Wang et al. (2015); Wang et al. (2018); improve mitochondrial biogenesis Zhou et al. (2019); systemic anti-inflammation Lyu et al. (2019); Hao et al. (2022) |
| Tongxinluo (TXL) capsules | Panax ginseng C.A. Meyer, Paeonia lactiflora Pall., Ziziphus jujuba Mill. Var. spinosa (Bunge) Hu ex H.F.Chou, Santalum album L., Dalbergia odorifera T.C.Chen, Steleophaga plancyi (Boleny), Scolopendra subspinipes mutilans L. Koch, Hirudo nipponica Whitman, Cryptotympana pustulata Fabricius, Buthus martensii Karsch, Boswellia carteri, Borneolum syntheticum | 12 | Panax ginseng, Dalbergia odorifera, Boswellia carteri, Hirudo | Ginsenosides, Frankincense, Hirudinoidines | Inhibit ox-LDL-induced macrophage apoptosis Yifei Chen et al. (2018); alleviate ischemic/reperfusion-injury via activating PPAR-α and PI3K/Akt/eNOS/NO pathway Wang et al. (2014); Fan et al. (2017); anti-fibrosis and antioxidant effect Bai et al. (2013); Zaki et al. (2014) |
| Shensongyangxin (SSYX) capsules | Panax ginseng C.A. Meyer, Salvia miltiorrhiza Bge, Nardostachys jatamansi Dc., Cornus officinalis Sieb.et Zucc., Taxillus chinensis (DC.) Danser, Paeonia lactiflora Pall., Schisandra sphenanthera Rehd.et, Coptis chinensis Franch., Ophiopogon japonicas (Thunb.) Ker-Gawl., Polypodiodes chinensis, Eupolyphaga sinensis Walker, Ziziphus jujuba Mill. var. spinosa (Bunge) Hu ex H. F. Chou | 12 | Panax ginseng, Nardostachys jatamansi, Paeonia lactiflora , Coptis chinensis, Ophiopogon japonicus | Ginsenosides, Salvianolic acid B, Paeoniflorin, Berberine, Polysaccharide | Ion channel regulation effect Yang et al. (2020); Zhao et al. (2020); regulation of autonomic nerve ctivity Zhao et al. (2017); promoted angiogenesis Li et al. (2020); Jiang et al. (2021); anti-inflammation and remodeling Zhang et al. (2016); Hengwen Chen et al. (2018) |
| Qiliqiangxin (QLQX) capsules | Astragalus membranaceus (Fisch) Bge., Var. mongholicus (Bge.) Hsiao., Panax ginseng C. A. Mey., Aconitum carmichaeli Debx., Salvia miltiorrhiza Bge., Lepidium apetalum Willd., Alisma orientalis (Sam.) Juzep., Polygonatum odoratum (Mill.) Druce, Carthamus tinctorius L., Periploca sepium Bge., Cinnamomum cassia Presl, Citrus reticulata Blanco | 11 | Astragalus membranaceus, Aconitum carmichaeli, Salvia miltiorrhiza., Carthamus tinctorius, Cinnamomum cassia, Citri reticulatae Pericarpium | Astragalus polysaccharide, Diterpenoid Alkaloids, Salvianolic acid B, Hydroxysafflor yellow A, Cinnamomi ramulus, Nobiletin | Upregulation of PPARγ and PGC1α Shen et al. (2017); Gao et al. (2018); attenuate anoxia-induced injuries via NRG-1/ErbB-PI3K/Akt/mTOR pathway Regulating Energy Metabolism via HIF-1α and TNF-α/PGC-1α Zhang et al. (2016); Luan et al. (2015); Cheng W. et al. (2020); inhibit apoptotic response through IGF-I pathway Tung et al. (2019) |
Therefore, researchers have made substantial efforts by clarifying the important scientific issues in the past decade. To identify the characteristics and targeted pathway by the modern scientific protocol, their mechanism and clinical effects have been partially translated to achieve a cross-integration of cardiovascular management (Tang and Huang, 2013; Hao et al., 2015). Although there are further questions that remained to be clarified, we believe that integrating the useful elements of TCM could expand the research field of CVDs and could also benefit the effective prevention and precise treatment.
Translation in Modern Medicine
Jinlida Granules in Regulating Metabolism
Systemic risk factors such as obesity, diabetes, and dyslipidemia often exist in the pathophysiological process of atherosclerotic cardiovascular disease (ASCVD), which could lead to adverse outcomes. A large number of clinical and experimental studies have confirmed that energy imbalance caused by excessive energy intake and reduced consumption is the main cause of obesity and glucose and lipid metabolism disorders. Furthermore, inflammation is associated with increased oxidative stress, platelet activation, vascular endothelial dysfunction, and other metabolic CVD which are closely related to these pathophysiological changes (Kolwicz et al., 2013; Schmidt, 2019; Wang et al., 2019; Glatz et al., 2020).
Treatment targeting metabolic aspects (such as SGLT-2 inhibitors) may significantly reduce the risk of atherosclerotic cardiovascular and cerebrovascular diseases (Ren et al., 2010; Hou et al., 2020). The balance of intake and consumption of energy substances is the basis for maintaining the normal physiological functions of the body. Insulin resistance as the core mechanism of metabolic syndrome is often associated with abnormal blood glucose regulation (Rochlani et al., 2017). Previous studies showed that Jinlida granules (JLDG) might be beneficial via their metabolic regulation effects by protecting islet β-cell (Shi et al., 2013), and play a role in various pathways in anti-metabolic disorders. JLDG could reduce insulin resistance by regulating the lipid metabolism (Wang et al., 2015), promoting skeletal muscle gene and protein expression (Zang et al., 2015). JLDG also improves metabolic disorders associated with the activation of brown adipose tissue (BAT) thermogenesis via enhancement of mitochondrial biogenesis and fatty acid oxidation metabolism (Zhang H. et al., 2019).
Furthermore, JLDG demonstrated the effect of anti-oxidative stress (Liu et al., 2015) and regulating hormones related to blood glucose (Pang et al., 2014). Systemic anti-inflammatory protective effect of JLDG also reflected in improving NAFLD by antagonizing hepatocyte pyroptosis in the high-fat-diet-induced liver injury mice model (Hao et al., 2022).
Clinical trials have also shown the efficacy of JLDG in diabetes treatment (Lian et al., 2015; Shi et al., 2016; Tian et al., 2018; Pan et al., 2021). Furthermore, a meta-analysis (Lian et al., 2019) that included clinical studies in the past decade showed the treatment with JLDG provided clinically and statistically significant reductions in fasting plasma glucose, 2-h postprandial plasma glucose, and the glycated hemoglobin (HbA1c) level in patients with type 2 diabetes mellitus.
These results suggest that JLDG might be a complementary therapeutic agent or even treatment regimen for metabolic syndrome and diabetes. The exploration in the mechanism of the ingredients and active monomers would contribute to recognizing the metabolic properties and its therapeutic effects in CVD.
Tongxinluo in Atherosclerosis
Atherosclerosis is associated with chronic and progressive inflammation (Zhu et al., 2018). Inflammation damage to endothelial cells plays an important role in the initiation and progression of atherosclerotic plaque. Factors such as cells and cytokines are involved in this process, namely, macrophages, lymphocytes, dendritic cells, endothelial cells, vascular smooth muscle cells, interleukin, adhesion molecules, and tumor necrosis factor (TNF-α) are involved in the process. At the same time, pathological changes including abnormal lipid metabolism, hemorheological changes, oxidative stress, intimal hyperplasia, and adventitia nourish angiogenesis interrelatedly promote atherosclerosis (Gimbrone and García-Cardeña, 2016; Poznyak et al., 2020).
As a TCM set prescription, studies have found that Tongxinluo (TXL) can regulate the lipid metabolism and anti-atherosclerosis, and improve atherosclerotic plaque stability through various pathophysiological pathways. One major pathway includes the alleviation of plaque inflammation by inhibiting inflammation-induced neovascularization in the plaque via inhibition of the NLRP3 pathway to stabilize the atherosclerotic plaque (Ma et al., 2015; Wang et al., 2021). TXL could regulate the lipid metabolism (Ma L. et al., 2016; Zhou et al., 2016; Chen et al., 2021) which strongly correlate to the composition of the intestinal flora and intestinal metabolites associated with the stability of plaque by promoting the adenosine triphosphate-binding cassette transporter A1 (ABCA1) (Li Y. et al., 2021; Huang et al., 2021). Furthermore, TXL protected the endothelial barrier integrity in reperfused diabetic rats’ hearts via peroxisome proliferator-activated receptors—alpha (PPARα) pathway independent of the blood glucose level (Bai et al., 2013). TXL has effects. The comprehensive mechanisms of TXL on inhibiting atherosclerosis development and stabilizing plaque might also involve cell physical function, hormone secretion, protein binding, and immune response process (Ma et al., 2019). In a clinical observation study (CAPITAL study), in addition to conventional treatments in patients with subclinical AS, treatment with the TXL group showed a significant delay in the progress of average IMT, plaque area, and carotid vascular remodeling without additional adverse drug safety outcomes (Zhang M. et al., 2019).
On the other hand, myocardial no-reflow is associated with microvascular endothelial damage, microthrombosis, microvascular spasm and injury, myocardial ischemia/reperfusion (I/R) injury, and microvessel dysfunction. In addition, these pathological changes of inflammation, oxidative stress, calcium overload, and mitochondrial dysfunction were shown to be persistent after reperfusion and suggested that the recovery is a continuous dynamic process (Kang et al., 2010).
Studies have shown that pre-administration of TXL could reduce the myocardial no-reflow area and myocardial infarction area in animal models (Li et al., 2006; Qian et al., 2007; Cheng et al., 2009). The specific mechanism may be related to the downregulation of miR-128-3p and promotion of p70s6k1 protein expression (Chen et al., 2017), the activation of the PKA-eNOS pathway (Li et al., 2010), and the activation of the MEK/ERK pathway, vascular endothelial growth factor (VEGF), angioprotein-like protein-4, granulocyte colony-stimulating factor (G-CSF) (Li X. L. et al., 2013), AMP-activated protein kinase (AMPK) (Li et al., 2017), etc. Also, TXL treatment significantly inhibited macrophage apoptosis by enhancing macrophage autophagy by increasing Beclin-1 expression and improving Bcl-2–Beclin-1 complex dissociation (Chen Y. et al., 2018). Recent studies have further demonstrated TXL could reduce myocardial/endothelial cell apoptosis and necrosis due to both hypoxia and reperfusion via upregulating the expression level of lincROR, downregulating miRNA145-5p, activating the p70s6k1/eNOS signaling pathway (Chen et al., 2020), and downregulating the expression of MMP family proteins in macrophages (Ma et al., 2019).
In a clinical aspect, the ENLEAT study (Zhang et al., 2010) also showed that TXL can promote myocardial reperfusion, significantly reduce the incidence of coronary no-reflow after reperfusion, reduce the area of myocardial infarction, and improve the cardiac systolic function for STEMI patients in addition to conventional medicine therapy. An ongoing randomized control trial CTS-AMI study regarding the efficacy and safety of TXL will provide more comprehensive evidence for the patients with coronary artery disease (Xu et al., 2020).
Shensongyangxing in Metabolic Reconstruction
However, metabolic syndrome (MS) is closely related to an increased morbidity of arrhythmia in various pathophysiological aspects (Kumar and Gehi, 2012; Gawałko et al., 2021; Joseph et al., 2021; Pool et al., 2021). A large cohort study showed that metabolic factors including obesity, hypertension, low LDL-C level, and impaired fasting blood glucose level are closely related to new-onset atrial fibrillation (AF) (Watanabe et al., 2008). Metabolic syndrome is an independent predictor of AF associated with the left atrial low voltage zone (Dinov et al., 2014). Furthermore, MS is also associated with the increased risk of ventricular arrhythmia (VA) (Fernández-Sada et al., 2017; Liptak et al., 2017) and was reported to contribute to a higher recurrence rate of outflow tract VA after catheter ablation (Sardu et al., 2014). However, the underlying role of MS in the occurrence and development of such arrhythmia remains unclear. Theories have been raised that it might be related to the oxidative stress, inflammation, myocardial fibrosis, and ferroportin pathway along with the process of cardiovascular continuum.
Shensongyangxing (SSYX) has an anti-arrhythmic effect. There is research interpreting its possible mechanism of the effectiveness. Studies have shown that SSYX can inhibit AMPK phosphorylation and PGC-1α activity, thereby improving myocardial energy metabolism and improving Ang-II-induced primary cardiomyocyte hypertrophy (Liu et al., 2018). Another study showed that SSYX reduces the occurrence of AF after myocardial infarction by inhibiting atrial fibrosis (Ma et al., 2018). At the same time, SSYX has shown to be a multichannel blocker with measurable modulation effects on various ion channels, such as L-type calcium channel and transient outward potassium (Ito), resulting in an overall prolongation of the action potential (Yang et al., 2020; Zhao et al., 2020). SSYX could inhibit IK1 and Ito currents by prolonging the duration of action potentials, reversing calcium overload, and inhibiting the occurrence of ventricular arrhythmias after ischemia (Zhao et al., 2016). In a metabolic aspect, animal research showed that SSYX can reverse and alleviate the metabolic and arrhythmic pathological changes such as impaired glucose tolerance, enlarged atria, atrial fibrosis, atrial inflammation, and oxidative stress; shortened effective refractory period; and prolonged action potential duration induced by metabolic syndrome (Zaki et al., 2014; Chen Y. et al., 2018; Yang et al., 2020).
Previous multicenter clinical studies showed that SSYX capsule has a significant effect on the treatment of heart failure (HF) complicated by ventricular arrhythmia (Liu et al., 2014; Wang X. et al., 2017; Cao et al., 2021). SSYX capsules have also been demonstrated to be effective in the treatment of paroxysmal AF (Jiang et al., 2022). In cohorts without HF, studies have demonstrated the effectiveness of SSYX for the concomitant treatment of frequent premature ventricular contractions and sinus bradycardia (SB), and alleviation of the related symptoms (Zou et al., 2011; Zhang F. et al., 2019).
Qiliqiangxin in Cardiac Remodeling
As an end stage in the development of various heart diseases, the morbidity and mortality of heart failure (HF) gradually increase due to population aging. Although some treatment progress has been made in the past decade, HF is still a major problem that seriously threatens human life and quality of life (Tomasoni et al., 2019). The basic mechanism of the occurrence and development in heart failure includes pathological cardiomyocyte hypertrophy with embryonic gene re-expression, cardiomyocyte apoptosis and necrosis, and excessive deposition or degradation of cardiomyocyte extracellular matrix (Gyöngyösi et al., 2017). The activation of peroxisome proliferator-activated receptors (gamma (PPARγ)) and its coactivator-1α (PGC-1α) play key roles in the amelioration of cardiac hypertrophy and dysfunction (Li et al., 2010). PPARγ also plays an important role in cardiac metabolism remodeling and the observed attenuation of cardiac fibrosis, inflammation, and ROS production (Wang et al., 2016; Penas et al., 2020).
Qiliqiangxin (QLQX) capsule is a compound preparation derived from TCM pathology which is in line with the modern prospective of neuroendocrine activation and ventricular remodeling in HF. QLQX can improve the heart function of HF rats and increase the excretion of water by reducing the expression of AQP2 in the kidneys (Cui et al., 2015). It can also reduce the expression of Ang II and periostin protein in HF rats after myocardial infarction (Zhou et al., 2015; Li F. et al., 2021), while the immunomodulatory effects of anti-inflammatory factors might be one of the immunopharmacological mechanisms of QLQX to improve the heart function of AMI rats. These previous cells and animal studies regarding the effect of QLQX in various models have shown the protective effects on inhibiting pathological cardiac remodeling, mechanistically via activation of PPARγ (He et al., 2013; Pan et al., 2014; Wang H. et al., 2017), and the protective effect of QLQX in the heart might also be attributed, but not limited, to the blood glucose reduction effect (Wu et al., 2021).
Further analysis of the QLQX component demonstrated that citri reticulatae Pericarpium (CRP) inhibits pathological cardiac hypertrophy (Cheng H. et al., 2020). CRP protected against pathological cardiac hypertrophy is induced by Ang II stimulation in neonatal rat cardiomyocytes (Ni et al., 2020), while the active monomer nobiletin isolated from CRP might be the major factor in attenuating the adverse cardiac remodeling via anti-inflammatory (Bunbupha et al., 2020) and antiapoptotic functions (Amarsanaa et al., 2021) similarly via activating PPARγ and PGC1α (Zhou et al., 2021). However, studies to explore the mechanism of QLQX for its protective effects on cardiac pathological hypertrophy, and the interaction of the component are still needed.
Regarding the clinical efficacy aspect, a multicenter randomized controlled clinical study (Li X. et al., 2013) showed that QLQX can significantly reduce the secondary endpoint of HF patients in addition to the standard HF treatment. The study assessing the prognosis on the hard endpoint-cardiovascular mortality and HF rehospitalization to further clarify the clinical efficacy and safety of QLQX is expected for further evidence-based confirmation (Yao et al., 2020).
Conclusion
Although the findings should be interpreted with caution because the studies might only represent a limited aspect of the set prescriptions, the exploration of these TCM set prescriptions on cardiac metabolism pathways and the relevance of this knowledge for current clinical practice may have utility for the future treatment of patients with cardiovascular diseases. To be noted, we should also acknowledge the potential reactions caused by drug/component interactions when combining traditional Chinese medicine and modern medicine. We believe integrating the evidence of TCM could provide sufficient elucidation of the mechanism to the clinical effect and complement the current management approaches.
Author Contributions
IC participated in drafting, conceptualization, and major writing of the manuscript. SL participated in the original draft and writing. QZ and GN performed the literature search and interpreted the results. CW, ZJ, and YW had validated and supervised the current works. XL participated in the original draft, had validation, and gave administration support of the current works. All the authors read and approved the final manuscript.
Funding
This study was supported by the National Key Research and Development Program of China (Nos 2017YFC1700500 and 2017YFC1700505).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ABCA1, adenosine triphosphate-binding cassette transporter A1; AMPK, AMP-activated protein kinase; ASCVD, atherosclerotic cardiovascular disease; AF, atrial fibrillation; BAT, brown adipose tissue; CVD, cardiovascular disease; CRP, citri reticulatae Pericarpium; HBA1c, glycated hemoglobin; G-CSF, granulocyte colony stimulating factor; HF, heart failure; I/R, ischemia/reperfusion; JLDG, Jinlida granules; NMPA, Chinese National Medical Products Administration; MS, metabolic syndrome; PPARγ, peroxisome proliferator-activated receptors gamma; PCG-1α, PPAR gamma coactivator-1α; QLQX, Qiliqiangxin; RXR, retinoic acid X receptor; SSYX, Shensongyangxin; SGLT-2, sodium-glucose cotransporter-2; TXL, Tongxinluo; TCM, traditional Chinese medicine; VEGF, vascular endothelial growth factor; VA, ventricular arrhythmia.
References
- Amarsanaa K., Kim H. J., Ko E. A., Jo J., Jung S. C. (2021). Nobiletin Exhibits Neuroprotective Effects against Mitochondrial Complex I Inhibition via Regulating Apoptotic Signaling. Exp. Neurobiol. 30 (1), 73–86. PMID: 33424017; PMCID: PMC7926044. 10.5607/en20051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bai W. W., Xing Y. F., Wang B., Lu X. T., Wang Y. B., Sun Y. Y., et al. (2013). Tongxinluo Improves Cardiac Function and Ameliorates Ventricular Remodeling in Mice Model of Myocardial Infarction through Enhancing Angiogenesis. Evid. Based Complement. Alternat Med. 2013, 813247. Epub 2013 Aug 27. PMID: 24069057; PMCID: PMC3771470. 10.1155/2013/813247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunbupha S., Apaijit K., Maneesai P., Prasarttong P., Pakdeechote P. (2020). Nobiletin Ameliorates High-Fat Diet-Induced Vascular and Renal Changes by Reducing Inflammation with Modulating AdipoR1 and TGF-Β1 Expression in Rats. Life Sci. 260, 118398. Epub 2020 Sep 10. PMID: 32920004. 10.1016/j.lfs.2020.118398 [DOI] [PubMed] [Google Scholar]
- Cao X., Zhou M., Liu H., Chen X., Li X., Jia S. (2021). Clinical Efficacy and Safety of Shensong Yangxin Capsule-Amiodarone Combination on Heart Failure Complicated by Ventricular Arrhythmia: A Meta-Analysis of Randomized Controlled Trials. Front. Pharmacol. 12, 613922. PMID: 33692689; PMCID: PMC7937972. 10.3389/fphar.2021.613922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen G., Xu C., Gillette T. G., Huang T., Huang P., Li Q., et al. (2020). Cardiomyocyte-derived Small Extracellular Vesicles Can Signal eNOS Activation in Cardiac Microvascular Endothelial Cells to Protect against Ischemia/Reperfusion Injury. Theranostics 10 (25), 11754–11774. PMID: 33052245; PMCID: PMC7546010. 10.7150/thno.43163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen G. H., Xu C. S., Zhang J., Li Q., Cui H. H., Li X. D., et al. (2017). Inhibition of miR-128-3p by Tongxinluo Protects Human Cardiomyocytes from Ischemia/reperfusion Injury via Upregulation of P70s6k1/p-P70s6k1. Front. Pharmacol. 8, 775. PMID: 29163161; PMCID: PMC5670141. 10.3389/fphar.2017.00775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H., Dong Y., He X., Li J., Wang J. (2018). Paeoniflorin Improves Cardiac Function and Decreases Adverse Postinfarction Left Ventricular Remodeling in a Rat Model of Acute Myocardial Infarction. Drug Des. Devel Ther. 12, 823–836. Erratum in: Drug Des Devel Ther. 2020 Nov 18;14:5043. PMID: 29695894; PMCID: PMC5905848. 10.2147/DDDT.S163405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Li M., Zhang Y., Di M., Chen W., Liu X., et al. (2018). Traditional Chinese Medication Tongxinluo Attenuates Apoptosis in Ox-LDL-Stimulated Macrophages by Enhancing Beclin-1-Induced Autophagy. Biochem. Biophys. Res. Commun. 501 (2), 336–342. Epub 2018 May 11. PMID: 29550482. 10.1016/j.bbrc.2018.03.094 [DOI] [PubMed] [Google Scholar]
- Chen Y., Yu F., Zhang Y., Li M., Di M., Chen W., et al. (2021). Traditional Chinese Medication Tongxinluo Attenuates Lipidosis in Ox-LDL-Stimulated Macrophages by Enhancing Beclin-1-Induced Autophagy. Front. Pharmacol. 12, 673366. PMID: 34248627; PMCID: PMC8267176. 10.3389/fphar.2021.673366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng H., Wu X., Ni G., Wang S., Peng W., Zhang H., et al. (2020). Citri Reticulatae Pericarpium Protects against Isoproterenol-Induced Chronic Heart Failure via Activation of PPARγ. Ann. Transl Med. 8 (21), 1396. PMID: 33313141; PMCID: PMC7723657. 10.21037/atm-20-2200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng W., Wang L., Yang T., Wu A., Wang B., Li T., et al. (2020). Qiliqiangxin Capsules Optimize Cardiac Metabolism Flexibility in Rats with Heart Failure after Myocardial Infarction. Front. Physiol. 11, 805. PMID: 32848816; PMCID: PMC7396640. 10.3389/fphys.2020.00805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng Y. T., Yang Y. J., Zhang H. T., Qian H. Y., Zhao J. L., Meng X. M., et al. (2009). Pretreatment with Tongxinluo Protects Porcine Myocardium from Ischaemia/reperfusion Injury through a Nitric Oxide Related Mechanism. Chin. Med. J. (Engl) 122 (13), 1529–1538. PMID: 19719943. [PubMed] [Google Scholar]
- Cui X., Zhang J., Li Y., Sun Y., Cao J., Zhao M., et al. (2015). Effects of Qili Qiangxin Capsule on AQP2, V2R, and AT1R in Rats with Chronic Heart Failure. Evid. Based Complement. Alternat Med. 2015, 639450. Epub 2015 May 17. PMID: 26074997; PMCID: PMC4449905. 10.1155/2015/639450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinov B., Kosiuk J., Kircher S., Bollmann A., Acou W. J., Arya A., et al. (2014). Impact of Metabolic Syndrome on Left Atrial Electroanatomical Remodeling and Outcomes after Radiofrequency Ablation of Nonvalvular Atrial Fibrillation. Circ. Arrhythm Electrophysiol. 7 (3), 483–489. Epub 2014 May 15. PMID: 24833645. 10.1161/CIRCEP.113.001185 [DOI] [PubMed] [Google Scholar]
- Dzau V., Braunwald E. (1991). Resolved and Unresolved Issues in the Prevention and Treatment of Coronary Artery Disease: a Workshop Consensus Statement. Am. Heart J. 121 (4 Pt 1), 1244–1263. 10.1016/0002-8703(91)90694-d [DOI] [PubMed] [Google Scholar]
- Fan Z. M., Wang D. Y., Yang J. M., Lin Z. X., Lin Y. X., Yang A. L., et al. (2017). Dalbergia Odorifera Extract Promotes Angiogenesis through Upregulation of VEGFRs and PI3K/MAPK Signaling Pathways. J. Ethnopharmacol 204, 132–141. Epub 2017 Apr 12. PMID: 28412217. 10.1016/j.jep.2017.04.006 [DOI] [PubMed] [Google Scholar]
- Fernández-Sada E., Torres-Quintanilla A., Silva-Platas C., García N., Willis B. C., Rodríguez-Rodríguez C., et al. (2017). Proinflammatory Cytokines Are Soluble Mediators Linked with Ventricular Arrhythmias and Contractile Dysfunction in a Rat Model of Metabolic Syndrome. Oxidative Med. Cell Longevity 2017, 1–12. Epub 2017 Oct 19. PMID: 29201273; PMCID: PMC5671748. 10.1155/2017/7682569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao R. R., Wu X. D., Jiang H. M., Zhu Y. J., Zhou Y. L., Zhang H. F., et al. (2018). Traditional Chinese Medicine Qiliqiangxin Attenuates Phenylephrine-Induced Cardiac Hypertrophy via Upregulating PPARγ and PGC-1α. Ann. Transl Med. 6 (8), 153. PMID: 29862242; PMCID: PMC5952020. 10.21037/atm.2018.04.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gawałko M., Agbaedeng T. A., Saljic A., Müller D. N., Wilck N., Schnabel R., et al. (2021). Gut Microbiota, Dysbiosis and Atrial Fibrillation. Arrhythmogenic Mechanisms and Potential Clinical Implications. Cardiovasc. Res. cvab292. Epub ahead of print. PMID: 34550344. 10.1093/cvr/cvab292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gimbrone M. A., Jr, García-Cardeña G. (2016). Endothelial Cell Dysfunction and the Pathobiology of Atherosclerosis. Circ. Res. 118 (4), 620–636. PMID: 26892962; PMCID: PMC4762052. 10.1161/CIRCRESAHA.115.306301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glatz J. F. C., Zuurbier C. J., Larsen T. S. (2020). Targeting Metabolic Pathways to Treat Cardiovascular Diseases. Biochim. Biophys. Acta Mol. Basis Dis. 1866 (10), 165879. Epub 2020 Jun 18. PMID: 32562699. 10.1016/j.bbadis.2020.165879 [DOI] [PubMed] [Google Scholar]
- Glovaci D., Fan W., Wong N. D. (2019). Epidemiology of Diabetes Mellitus and Cardiovascular Disease. Curr. Cardiol. Rep. 21 (4), 21. 10.1007/s11886-019-1107-y [DOI] [PubMed] [Google Scholar]
- Gyöngyösi M., Winkler J., Ramos I., Do Q. T., Firat H., McDonald K., et al. (2017). Myocardial Fibrosis: Biomedical Research from Bench to Bedside. Eur. J. Heart Fail. 19 (2), 177–191. PMID: 28157267; PMCID: PMC5299507. 10.1002/ejhf.696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao P., Jiang F., Cheng J., Ma L., Zhang Y., Zhao Y. (2017). Traditional Chinese Medicine for Cardiovascular Disease: Evidence and Potential Mechanisms. J. Am. Coll. Cardiol. 69 (24), 2952–2966. PMID: 28619197. 10.1016/j.jacc.2017.04.041 [DOI] [PubMed] [Google Scholar]
- Hao P. P., Jiang F., Chen Y. G., Yang J., Zhang K., Zhang M. X., et al. (2015). Traditional Chinese Medication for Cardiovascular Disease. Nat. Rev. Cardiol. 12 (2), 115–122. Epub 2014 Nov 11. Erratum in: Nat Rev Cardiol. 2015 Jun;12(6):318. PMID: 25384847. 10.1038/nrcardio.2014.177 [DOI] [PubMed] [Google Scholar]
- Hao Y. Y., Cui W. W., Gao H. L., Wang M. Y., Liu Y., Li C. R., et al. (2022). Jinlida Granules Ameliorate the High-Fat-Diet Induced Liver Injury in Mice by Antagonising Hepatocytes Pyroptosis. Pharm. Biol. 60 (1), 274–281. PMID: 35138995; PMCID: PMC8843117. 10.1080/13880209.2022.2029501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He C., Zhu H., Li H., Zou M. H., Xie Z. (2013). Dissociation of Bcl-2-Beclin1 Complex by Activated AMPK Enhances Cardiac Autophagy and Protects against Cardiomyocyte Apoptosis in Diabetes. Diabetes 62 (4), 1270–1281. Epub 2012 Dec 7. PMID: 23223177; PMCID: PMC3609561. 10.2337/db12-0533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou Y. C., Zheng C. M., Yen T. H., Lu K. C. (2020). Molecular Mechanisms of SGLT2 Inhibitor on Cardiorenal Protection. Int. J. Mol. Sci. 21 (21), 7833. PMID: 33105763; PMCID: PMC7660105. 10.3390/ijms21217833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang K., Jo H., Echesabal-Chen J., Stamatikos A. (2021). Combined LXR and RXR Agonist Therapy Increases ABCA1 Protein Expression and Enhances ApoAI-Mediated Cholesterol Efflux in Cultured Endothelial Cells. Metabolites 11 (9), 640. PMID: 34564456; PMCID: PMC8466889. 10.3390/metabo11090640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang C., Wang X., Dang S., Wang X., Deng Q., Hu J., et al. (2021). Chinese Medicine Shensong Yangxin Capsule () Ameliorates Myocardial Microcirculation Dysfunction in Rabbits with Chronic Myocardial Infarction. Chin. J. Integr. Med. 27 (1), 24–30. Epub 2019 Jan 9. PMID: 30656600. 10.1007/s11655-018-2578-1 [DOI] [PubMed] [Google Scholar]
- Jiang X., Luo Y., Wang X., Chen Y., Wang T., He J., et al. (2022). Investigating the Efficiency and Tolerability of Traditional Chinese Formulas Combined with Antiarrhythmic Agents for Paroxysmal Atrial Fibrillation: A Systematic Review and Bayesian Network Meta-Analysis. Phytomedicine 94, 153832. Epub 2021 Oct 29. PMID: 34781230. 10.1016/j.phymed.2021.153832 [DOI] [PubMed] [Google Scholar]
- Joseph L. C., Reyes M. V., Homan E. A., Gowen B., Avula U. M. R., Goulbourne C. N., et al. (2021). The Mitochondrial Calcium Uniporter Promotes Arrhythmias Caused by High-Fat Diet. Sci. Rep. 11 (1), 17808. PMID: 34497331; PMCID: PMC8426388. 10.1038/s41598-021-97449-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang S., Yang Y. J., Wu Y. L., Chen Y. T., Li L., Tian Y. (2010). Myocardium and Microvessel Endothelium Apoptosis at Day 7 Following Reperfused Acute Myocardial Infarction. Microvasc. Res. 79 (1), 70–79. Epub 2009 Nov 11. PMID: 19913038. 10.1016/j.mvr.2009.11.003 [DOI] [PubMed] [Google Scholar]
- Kolwicz S. C., Jr, Purohit S., Tian R. (2013). Cardiac Metabolism and its Interactions with Contraction, Growth, and Survival of Cardiomyocytes. Circ. Res. 113 (5), 603–616. PMID: 23948585; PMCID: PMC3845521. 10.1161/CIRCRESAHA.113.302095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar P., Gehi A. K. (2012). Atrial Fibrillation and Metabolic Syndrome: Understanding the Connection. J. Atr Fibrillation 5 (3), 647. PMID: 28496775; PMCID: PMC5153215. 10.4022/jafib.647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C. L., Liu B., Wang Z. Y., Xie F., Qiao W., Cheng J., et al. (2020). Salvianolic Acid B Improves Myocardial Function in Diabetic Cardiomyopathy by Suppressing IGFBP3. J. Mol. Cel Cardiol 139, 98–112. Epub 2020 Jan 23. PMID: 31982427. 10.1016/j.yjmcc.2020.01.009 [DOI] [PubMed] [Google Scholar]
- Li F., Wang J., Song Y., Shen D., Zhao Y., Li C., et al. (2021). Qiliqiangxin Alleviates Ang II-Induced CMECs Apoptosis by Downregulating Autophagy via the ErbB2-AKT-FoxO3a axis. Life Sci. 273, 119239. Epub 2021 Feb 27. PMID: 33652033. 10.1016/j.lfs.2021.119239 [DOI] [PubMed] [Google Scholar]
- Li Q., Li N., Cui H. H., Tian X. Q., Jin C., Chen G. H., et al. (2017). Tongxinluo Exerts Protective Effects via Anti-apoptotic and Pro-autophagic Mechanisms by Activating AMPK Pathway in Infarcted Rat Hearts. Exp. Physiol. 102 (4), 422–435. Epub 2017 Mar 14. PMID: 28150462. 10.1113/EP086192 [DOI] [PubMed] [Google Scholar]
- Li X., Zhang J., Huang J., Ma A., Yang J., Li W., et al. (2013). A Multicenter, Randomized, Double-Blind, Parallel-Group, Placebo-Controlled Study of the Effects of Qili Qiangxin Capsules in Patients with Chronic Heart Failure. J. Am. Coll. Cardiol. 62 (12), 1065–1072. Epub 2013 Jun 7. PMID: 23747768. 10.1016/j.jacc.2013.05.035 [DOI] [PubMed] [Google Scholar]
- Li X. D., Yang Y. J., Cheng Y. T., Dou K. F., Tian Y., Meng X. M. (2013). Protein Kinase A-Mediated Cardioprotection of Tongxinluo Relates to the Inhibition of Myocardial Inflammation, Apoptosis, and Edema in Reperfused Swine Hearts. Chin. Med. J. (Engl) 126 (8), 1469–1479. PMID: 23595379. [PubMed] [Google Scholar]
- Li X. D., Yang Y. J., Geng Y. J., Jin C., Hu F. H., Zhao J. L., et al. (2010). Tongxinluo Reduces Myocardial No-Reflow and Ischemia-Reperfusion Injury by Stimulating the Phosphorylation of eNOS via the PKA Pathway. Am. J. Physiol. Heart Circ. Physiol. 299 (4), H1255–H1261. Epub 2010 Aug 6. PMID: 20693395. 10.1152/ajpheart.0045910.1152/ajpheart.00459.2010 [DOI] [PubMed] [Google Scholar]
- Li Y., Ji X., Wu H., Li X., Zhang H., Tang D. (2021). Mechanisms of Traditional Chinese Medicine in Modulating Gut Microbiota Metabolites-Mediated Lipid Metabolism. J. Ethnopharmacol 278, 114207. Epub 2021 May 14. PMID: 34000365. 10.1016/j.jep.2021.114207 [DOI] [PubMed] [Google Scholar]
- Li Z., Yang Y. J., Qin X. W., Ruan Y. M., Chen X., Meng L., et al. (2006). Effects of Tongxinluo and Simvastatin on the Stabilization of Vulnerable Atherosclerotic Plaques of Aorta in Aortic Atherosclerosis and Molecular Mechanism Thereof: a Comparative Study with Rabbits. Zhonghua Yi Xue Za Zhi 86 (44), 3146–3150. Chinese. PMID: 17313769. [PubMed] [Google Scholar]
- Lian F., Jin D., Bao Q., Zhao Y., Tong X. (2019). Effectiveness of Traditional Chinese Medicine Jinlida Granules as an Add-On Therapy for Type 2 Diabetes: A System Review and Meta-Analysis of Randomized Controlled Trials. J. Diabetes 11 (7), 540–551. Epub 2018 Dec 25. PMID: 30430757. 10.1111/1753-0407.12877 [DOI] [PubMed] [Google Scholar]
- Lian F., Tian J., Chen X., Li Z., Piao C., Guo J., et al. (2015). The Efficacy and Safety of Chinese Herbal Medicine Jinlida as Add-On Medication in Type 2 Diabetes Patients Ineffectively Managed by Metformin Monotherapy: A Double-Blind, Randomized, Placebo-Controlled, Multicenter Trial. PLoS One 10 (6), e0130550. PMID: 26098833; PMCID: PMC4476735. 10.1371/journal.pone.0130550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liptak B., Knezl V., Gasparova Z. (2017). Metabolic Disturbances Induce Malignant Heart Arrhythmias in Rats. Bratisl Lek Listy 118 (9), 539–543. PMID: 29061061. 10.4149/BLL_2017_103 [DOI] [PubMed] [Google Scholar]
- Liu B. L., Cheng M., Hu S., Wang S., Wang L., Hu Z. Q., et al. (2018). Effect of the Shensong Yangxin Capsule on Energy Metabolism in Angiotensin II-Induced Cardiac Hypertrophy. Chin. Med. J. (Engl) 131 (19), 2287–2296. PMID: 30246714; PMCID: PMC6166447. 10.4103/0366-6999.241819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Li N., Jia Z., Lu F., Pu J. (2014). Chinese Medicine Shensongyangxin Is Effective for Patients with Bradycardia: Results of a Randomized, Double-Blind, Placebo-Controlled Multicenter Trial. Evid. Based Complement. Alternat Med. 2014, 605714. Epub 2014 Jan 16. PMID: 24527049; PMCID: PMC3914313. 10.1155/2014/605714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Song A., Zang S., Wang C., Song G., Li X., et al. (2015). Jinlida Reduces Insulin Resistance and Ameliorates Liver Oxidative Stress in High-Fat Fed Rats. J. Ethnopharmacol 162, 244–252. Epub 2015 Jan 9. PMID: 25577992. 10.1016/j.jep.2014.12.040 [DOI] [PubMed] [Google Scholar]
- Luan A., Tang F., Yang Y., Lu M., Wang H., Zhang Y. (2015). Astragalus Polysaccharide Attenuates Isoproterenol-Induced Cardiac Hypertrophy by Regulating TNF-Α/pgc-1α Signaling Mediated Energy Biosynthesis. Environ. Toxicol. Pharmacol. 39 (3), 1081–1090. Epub 2015 Mar 31. PMID: 25880160. 10.1016/j.etap.2015.03.014 [DOI] [PubMed] [Google Scholar]
- Lyu Z., Ji X., Chen G., An B. (2019). Atractylodin Ameliorates Lipopolysaccharide and D-Galactosamine-Induced Acute Liver Failure via the Suppression of Inflammation and Oxidative Stress. Int. Immunopharmacol 72, 348–357. Epub 2019 Apr 24. PMID: 31030090. 10.1016/j.intimp.2019.04.005 [DOI] [PubMed] [Google Scholar]
- Ma J., Qiao L., Meng L., Ma L., Zhao Y., Liu X., et al. (2019). Tongxinluo May Stabilize Atherosclerotic Plaque via Multiple Mechanisms Scanning by Genechip. Biomed. Pharmacother. 113, 108767. Epub 2019 Mar 11. PMID: 30870720. 10.1016/j.biopha.2019.108767 [DOI] [PubMed] [Google Scholar]
- Ma J., Yin C., Ma S., Qiu H., Zheng C., Chen Q., et al. (2018). Shensong Yangxin Capsule Reduces Atrial Fibrillation Susceptibility by Inhibiting Atrial Fibrosis in Rats with post-myocardial Infarction Heart Failure. Drug Des. Devel Ther. 12, 3407–3418. PMID: 30349194; PMCID: PMC6186904. 10.2147/DDDT.S182834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma L., Ni M., Hao P., Lu H., Yang X., Xu X., et al. (2016). Tongxinluo Mitigates Atherogenesis by Regulating Angiogenic Factors and Inhibiting Vasa Vasorum Neovascularization in Apolipoprotein E-Deficient Mice. Oncotarget 7 (13), 16194–16204. PMID: 26908443; PMCID: PMC4941307. 10.18632/oncotarget.7477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma L., Liu X., Lu H., Yang X., Wang Y., Zhang C., et al. (2015). Traditional Chinese Medication Tongxinluo Inhibits Inflammatory Angiogenesis via Bmx/NF- B/MAPK Pathways. Eur. Heart J. Supplements 17 (Suppl. B), B13–B22. 10.1093/eurheartj/suv020 [DOI] [Google Scholar]
- Ma Y., Zhou K., Fan J., Sun S. (2016). Traditional Chinese Medicine: Potential Approaches from Modern Dynamical Complexity Theories. Front. Med. 10 (1), 28–32. Epub 2016 Jan 25. PMID: 26809465. 10.1007/s11684-016-0434-2 [DOI] [PubMed] [Google Scholar]
- Ni G., Wang K., Zhou Y., Wu X., Wang J., Shang H., et al. (2020). Citri Reticulatae Pericarpium Attenuates Ang II-Induced Pathological Cardiac Hypertrophy via Upregulating Peroxisome Proliferator-Activated Receptors Gamma. Ann. Transl Med. 8 (17), 1064. PMID: 33145283; PMCID: PMC7575934. 10.21037/atm-20-2118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan J., Xu Y., Chen S., Tu Y., Mo Y., Gao F., et al. (2021). The Effectiveness of Traditional Chinese Medicine Jinlida Granules on Glycemic Variability in Newly Diagnosed Type 2 Diabetes: A Double-Blinded, Randomized Trial. J. Diabetes Res. 2021, 6303063. PMID: 34660811; PMCID: PMC8519714. 10.1155/2021/6303063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan Y., Wang Y., Zhao Y., Peng K., Li W., Wang Y., et al. (2014). Inhibition of JNK Phosphorylation by a Novel Curcumin Analog Prevents High Glucose-Induced Inflammation and Apoptosis in Cardiomyocytes and the Development of Diabetic Cardiomyopathy. Diabetes 63 (10), 3497–3511. Epub 2014 May 21. PMID: 24848068. 10.2337/db13-1577 [DOI] [PubMed] [Google Scholar]
- Pang J., Gao H. L., Wang H. T., Wei C., Wu Y. L. (2014). Study on the Intervention Effect of Jinlida on Blood Glucose Regulating Hormone and Islet Cell Function in Diabetic Rats. Chin. J. Basic Med. Tradit Chin. Med. 20, 605–648. Available online at: http://www.cnki.com.cn/Article/CJFDTotal-ZYJC201405019.htm . [Google Scholar]
- Penas F. N., Carta D., Cevey Á. C., Rada M. J., Pieralisi A. V., Ferlin M. G., et al. (2020). Pyridinecarboxylic Acid Derivative Stimulates Pro-angiogenic Mediators by PI3K/AKT/mTOR and Inhibits Reactive Nitrogen and Oxygen Species and NF-Κb Activation through a PPARγ-dependent Pathway in T. Cruzi-Infected Macrophages. Front. Immunol. 10, 2955. PMID: 31993046; PMCID: PMC6964702. 10.3389/fimmu.2019.02955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pool L., Wijdeveld L. F. J. M., de Groot N. M. S., Brundel B. J. J. M. (2021). The Role of Mitochondrial Dysfunction in Atrial Fibrillation: Translation to Druggable Target and Biomarker Discovery. Int. J. Mol. Sci. 22 (16), 8463. PMID: 34445167; PMCID: PMC8395135. 10.3390/ijms22168463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poznyak A., Grechko A. V., Poggio P., Myasoedova V. A., Alfieri V., Orekhov A. N. (2020). The Diabetes Mellitus-Atherosclerosis Connection: The Role of Lipid and Glucose Metabolism and Chronic Inflammation. Int. J. Mol. Sci. 21 (5), 1835. PMID: 32155866; PMCID: PMC7084712. 10.3390/ijms21051835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian H. Y., Yang Y. J., Huang J., Gao R. L., Dou K. F., Yang G. S., et al. (2007). Effects of Tongxinluo-Facilitated Cellular Cardiomyoplasty with Autologous Bone Marrow-Mesenchymal Stem Cells on Postinfarct Swine Hearts. Chin. Med. J. (Engl) 120 (16), 1416–1425. PMID: 17825171. 10.1097/00029330-200708020-00008 [DOI] [PubMed] [Google Scholar]
- Ren J., Pulakat L., Whaley-Connell A., Sowers J. R. (2010). Mitochondrial Biogenesis in the Metabolic Syndrome and Cardiovascular Disease. J. Mol. Med. (Berl) 88 (10), 993–1001. Epub 2010 Aug 20. PMID: 20725711; PMCID: PMC4319704. 10.1007/s00109-010-0663-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rochlani Y., Pothineni N. V., Kovelamudi S., Mehta J. L. (2017). Metabolic Syndrome: Pathophysiology, Management, and Modulation by Natural Compounds. Ther. Adv. Cardiovasc. Dis. 11 (8), 215–225. Epub 2017 Jun 22. PMID: 28639538; PMCID: PMC5933580. 10.1177/1753944717711379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sardu C., Carreras G., Katsanos S., Kamperidis V., Pace M. C., Passavanti M. B., et al. (2014). Metabolic Syndrome Is Associated with a Poor Outcome in Patients Affected by Outflow Tract Premature Ventricular Contractions Treated by Catheter Ablation. BMC Cardiovasc. Disord. 14, 176. PMID: 25480761; PMCID: PMC4364311. 10.1186/1471-2261-14-176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt A. M. (2019). Diabetes Mellitus and Cardiovascular Disease. Arterioscler Thromb. Vasc. Biol. 39 (4), 558–568. PMID: 30786741; PMCID: PMC6532416. 10.1161/ATVBAHA.119.310961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen S., Jiang H., Bei Y., Zhang J., Zhang H., Zhu H., et al. (2017). Qiliqiangxin Attenuates Adverse Cardiac Remodeling after Myocardial Infarction in Ovariectomized Mice via Activation of PPARγ. Cell Physiol Biochem 42 (3), 876–888. Epub 2017 Jun 23. PMID: 28647730. 10.1159/000478641 [DOI] [PubMed] [Google Scholar]
- Shi J.-l., Wu Y., Song Y.-p., Han C., Liu Z.-m. (2013). Protective Effect of Jinlida Granules on Islet β Cells in Diabetes Mellitus Rats. Acad. J. Second Mil. Med. Univ. 32, 385–389. 10.3724/SP.J.1008.2012.00385 [DOI] [Google Scholar]
- Shi Y. L., Liu W. J., Zhang X. F., Su W. J., Chen N. N., Lu S. H., et al. (2016). Effect of Chinese Herbal Medicine Jinlida Granule in Treatment of Patients with Impaired Glucose Tolerance. Chin. Med. J. (Engl) 129 (19), 2281–2286. PMID: 27647185; PMCID: PMC5040012. 10.4103/0366-6999.190676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang W. H. W., Huang Y. (2013). Cardiotonic Modulation in Heart Failure: Insights from Traditional Chinese Medicine. J. Am. Coll. Cardiol. 62 (12), 1073–1074. Epub 2013 Jun 7. PMID: 23747774; PMCID: PMC4024708. 10.1016/j.jacc.2013.05.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian J., Lian F., Yang L., Tong X. (2018). Evaluation of the Chinese Herbal Medicine Jinlida in Type 2 Diabetes Patients Based on Stratification: Results of Subgroup Analysis from a 12-week Trial. J. Diabetes 10 (2), 112–120. Epub 2017 Jun 5. PMID: 28418191. 10.1111/1753-0407.12559 [DOI] [PubMed] [Google Scholar]
- Tomasoni D., Adamo M., Lombardi C. M., Metra M. (2019). Highlights in Heart Failure. ESC Heart Fail. 6 (6), 1105–1127. PMID: 31997538; PMCID: PMC6989277. 10.1002/ehf2.12555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tung C. L., Ju D. T., Velmurugan B. K., Ban B., Dung T. D., Hsieh D. J., et al. (2019). Carthamus tinctorius L. Extract Activates Insulin-like Growth Factor-I Receptor Signaling to Inhibit FAS-Death Receptor Pathway and Suppress Lipopolysaccharides-Induced H9c2 Cardiomyoblast Cell Apoptosis. Environ. Toxicol. 34 (12), 1320–1328. Epub 2019 Sep 4. PMID: 31486215. 10.1002/tox.22833 [DOI] [PubMed] [Google Scholar]
- Wang B., Lyu Z., Chan Y., Li Q., Zhang L., Liu K., et al. (2021). Tongxinluo Exerts Inhibitory Effects on Pyroptosis and Amyloid-β Peptide Accumulation after Cerebral Ischemia/Reperfusion in Rats. Evid. Based Complement. Alternat Med. 2021, 5788602. PMID: 34567216; PMCID: PMC8460392. 10.1155/2021/5788602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang B., Yang Q., Bai W. W., Xing Y. F., Lu X. T., Sun Y. Y., et al. (2014). Tongxinluo Protects against Pressure Overload-Induced Heart Failure in Mice Involving VEGF/Akt/eNOS Pathway Activation. PLoS One 9 (6), e98047. Erratum in: PLoS One. 2019;14(8):e0220845. PMID: 24887083; PMCID: PMC4041651. 10.1371/journal.pone.0098047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Dai X., Zhang D., Liu Z., Huang Q. (2018). Jinlida Granules Improve Dysfunction of Hypothalamic-Pituitary-Thyroid Axis in Diabetic Rats Induced by STZ. Biomed. Res. Int. 2018, 4764030. PMID: 29984235; PMCID: PMC6011157. 10.1155/2018/4764030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D., Tian M., Qi Y., Chen G., Xu L., Zou X., et al. (2015). Jinlida Granule Inhibits Palmitic Acid Induced-Intracellular Lipid Accumulation and Enhances Autophagy in NIT-1 Pancreatic β Cells through AMPK Activation. J. Ethnopharmacol 161, 99–107. Epub 2014 Dec 13. PMID: 25510732. 10.1016/j.jep.2014.12.005 [DOI] [PubMed] [Google Scholar]
- Wang H., Zhang X., Yu P., Zhou Q., Zhang J., Zhang H., et al. (2017). Traditional Chinese Medication Qiliqiangxin Protects against Cardiac Remodeling and Dysfunction in Spontaneously Hypertensive Rats. Int. J. Med. Sci. 14 (5), 506–514. PMID: 28539827; PMCID: PMC5441043. 10.7150/ijms.18142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S., Dougherty E. J., Danner R. L. (2016). PPARγ Signaling and Emerging Opportunities for Improved Therapeutics. Pharmacol. Res. 111, 76–85. Epub 2016 Jun 4. PMID: 27268145; PMCID: PMC5026568. 10.1016/j.phrs.2016.02.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X., Hu D., Dang S., Huang H., Huang C. X., Yuan M. J., et al. (2017). Effects of Traditional Chinese Medicine Shensong Yangxin Capsules on Heart Rhythm and Function in Congestive Heart Failure Patients with Frequent Ventricular Premature Complexes: A Randomized, Double-Blind, Multicenter Clinical Trial. Chin. Med. J. (Engl) 130 (14), 1639–1647. PMID: 28685712; PMCID: PMC5520549. 10.4103/0366-6999.209906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Xue H., Sun M., Zhu X., Zhao L., Yang Y. (2019). Prevention and Control of Obesity in China. Lancet Glob. Health 7 (9), e1166–e1167. PMID: 31401995. 10.1016/S2214-109X(19)30276-1 [DOI] [PubMed] [Google Scholar]
- Watanabe H., Tanabe N., Watanabe T., Darbar D., Roden D. M., Sasaki S., et al. (2008). Metabolic Syndrome and Risk of Development of Atrial Fibrillation: the Niigata Preventive Medicine Study. Circulation 117 (10), 1255–1260. Epub 2008 Feb 19. Erratum in: Circulation. 2010;122(7):e433. PMID: 18285562; PMCID: PMC2637133. 10.1161/CIRCULATIONAHA.107.744466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X., Zhang T., Lyu P., Chen M., Ni G., Cheng H., et al. (2021). Traditional Chinese Medication Qiliqiangxin Attenuates Diabetic Cardiomyopathy via Activating PPARγ. Front. Cardiovasc. Med. 8, 698056. PMID: 34336956; PMCID: PMC8322738. 10.3389/fcvm.2021.698056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y. (2009). Collateral Theory and Vascular Lesion Treatment. Am. J. Chin. Med. 37 (2), 241–252. PMID: 19507269. 10.1142/S0192415X09006801 [DOI] [PubMed] [Google Scholar]
- Xu Q., Bauer R., Hendry B. M., Fan T. P., Zhao Z., Duez P., et al. (2013). The Quest for Modernisation of Traditional Chinese Medicine. BMC Complement. Altern. Med. 13, 132. PMID: 23763836; PMCID: PMC3689083. 10.1186/1472-6882-13-132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Y., Li X., Zhang H., Wu Y., Zhang J., Li J., et al. (2020). China Tongxinluo Study for Myocardial protection in Patients with Acute Myocardial Infarction (CTS-AMI): Rationale and Design of a Randomized, Double-Blind, Placebo-Controlled, Multicenter Clinical Trial. Am. Heart J. 227, 47–55. Epub 2020 Jun 20. PMID: 32679281; PMCID: PMC7305744. 10.1016/j.ahj.2020.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang H. J., Kong B., Shuai W., Zhang J. J., Huang H. (2020). Shensong Yangxin Protects against Metabolic Syndrome-Induced Ventricular Arrhythmias by Inhibiting Electrical Remodeling. Front. Pharmacol. 11, 993. PMID: 32733242; PMCID: PMC7363804. 10.3389/fphar.2020.00993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao W., Cheang I., Liao S., Zhou Y., Zhou F., Xu D., et al. (2020). Study Protocol for a Randomized Controlled Trial: Qiliqiangxin in Heart failUre: assESsment of Reduction in morTality (QUEST). BMC Complement. Med. Ther. 20 (1), 38. PMID: 32024496; PMCID: PMC7076750. 10.1186/s12906-020-2821-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaki A. A., Hashish N. E., Amer M. A., Lahloub M. F. (2014). Cardioprotective and Antioxidant Effects of Oleogum Resin "Olibanum" from Bos Boswellia Carteri Birdw. (Bursearceae). Chin. J. Nat. Med. 12 (5), 345–350. PMID: 24856757. 10.1016/S1875-5364(14)60042-X [DOI] [PubMed] [Google Scholar]
- Zang S. S., Song A., Liu Y. X., Wang C., Song G. Y., Li X. L., et al. (2015). Chinese Medicine Jinlida (JLD) Ameliorates High-Fat-Diet Induced Insulin Resistance in Rats by Reducing Lipid Accumulation in Skeletal Muscle. Int. J. Clin. Exp. Med. 8 (3), 4620–4634. PMID: 26064395; PMCID: PMC4443229. [PMC free article] [PubMed] [Google Scholar]
- Zhang F., Zou J., Yu H., Li X., Kojodjojo P., Cai X., et al. (2019). Acute Efficacy of a Traditional Chinese Medicine for Treatment of Frequent Premature Ventricular Contractions in Patients with Concomitant Sinus Bradycardia: Results from a Double-Blind, Placebo-Controlled, Multicentre, Randomized Clinical Trial. Evid. Based Complement. Alternat Med. 2019, 3917282. PMID: 30949218; PMCID: PMC6425419. 10.1155/2019/3917282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H., Hao Y., Wei C., Yao B., Liu S., Zhou H., et al. (2019). Chinese Medicine Jinlida Granules Improve High-Fat-Diet Induced Metabolic Disorders via Activation of Brown Adipose Tissue in Mice. Biomed. Pharmacother. 114, 108781. Epub 2019 Mar 20. PMID: 30903919. 10.1016/j.biopha.2019.108781 [DOI] [PubMed] [Google Scholar]
- Zhang H. T., Jia Z. H., Zhang J., Ye Z. K., Yang W. X., Tian Y. Q., et al. (2010). No-reflow protection and Long-Term Efficacy for Acute Myocardial Infarction with Tongxinluo: a Randomized Double-Blind Placebo-Controlled Multicenter Clinical Trial (ENLEAT Trial). Chin. Med. J. (Engl) 123 (20), 2858–2864. PMID: 21034597. [PubMed] [Google Scholar]
- Zhang J., Fan S., Mao Y., Ji Y., Jin L., Lu J., et al. (2016). Cardiovascular Protective Effect of Polysaccharide from Ophiopogon Japonicus in Diabetic Rats. Int. J. Biol. Macromol 82, 505–513. Epub 2015 Oct 3. PMID: 26434529. 10.1016/j.ijbiomac.2015.09.069 [DOI] [PubMed] [Google Scholar]
- Zhang M., Liu Y., Xu M., Zhang L., Liu Y., Liu X., et al. (2019). Carotid Artery Plaque Intervention with Tongxinluo Capsule (CAPITAL): A Multicenter Randomized Double-Blind Parallel-Group Placebo-Controlled Study. Sci. Rep. 9 (1), 4545. PMID: 30872737; PMCID: PMC6418108. 10.1038/s41598-019-41118-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Q., Shao M., Zhang X., Wang Q., Guo D., Yang X., et al. (2018). The Effect of Chinese Medicine on Lipid and Glucose Metabolism in Acute Myocardial Infarction through PPARγ Pathway. Front. Pharmacol. 9, 1209. PMID: 30405421; PMCID: PMC6207917. 10.3389/fphar.2018.01209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao H. Y., Zhang S. D., Zhang K., Wang X., Zhao Q. Y., Zhang S. J., et al. (2017). Effect of Shensong Yangxin on the Progression of Paroxysmal Atrial Fibrillation Is Correlated with Regulation of Autonomic Nerve Activity. Chin. Med. J. (Engl) 130 (2), 171–178. PMID: 28091409; PMCID: PMC5282674. 10.4103/0366-6999.197997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J., Wang Y., Gao J., Jing Y., Xin W. (2020). Berberine Mediated Positive Inotropic Effects on Rat Hearts via a Ca2+-dependent Mechanism. Front. Pharmacol. 11, 821. PMID: 32581792; PMCID: PMC7289965. 10.3389/fphar.2020.00821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y., Gao F., Zhang Y., Wang H., Zhu J., Chang L., et al. (2016). Shensong Yangxin Capsules Prevent Ischemic Arrhythmias by Prolonging Action Potentials and Alleviating Ca2+ Overload. Mol. Med. Rep. 13 (6), 5185–5192. Epub 2016 Apr 28. PMID: 27122298. 10.3892/mmr.2016.5203 [DOI] [PubMed] [Google Scholar]
- Zhou J., Cao B., Ju W., Liu S., Song J., Liu L. (2016). Effects of Tongxinluo on Angiogenesis in the Carotid Adventitia of Hyperlipidemic Rabbits. Mol. Med. Rep. 14 (4), 3832–3840. Epub 2016 Aug 25. PMID: 27572484. 10.3892/mmr.2016.5675 [DOI] [PubMed] [Google Scholar]
- Zhou J., Jiang K., Ding X., Fu M., Wang S., Zhu L., et al. (2015). Qiliqiangxin Inhibits Angiotensin II-Induced Transdifferentiation of Rat Cardiac Fibroblasts through Suppressing Interleukin-6. J. Cel Mol Med 19 (5), 1114–1121. Epub 2015 Mar 6. PMID: 25752645; PMCID: PMC4420613. 10.1111/jcmm.12512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou P., Xie W., He S., Sun Y., Meng X., Sun G., et al. (2019). Ginsenoside Rb1 as an Anti-diabetic Agent and its Underlying Mechanism Analysis. Cells 8 (3), 204. PMID: 30823412; PMCID: PMC6468558. 10.3390/cells8030204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Y., Yin T., Shi M., Chen M., Wu X., Wang K., et al. (2021). Nobiletin Attenuates Pathological Cardiac Remodeling after Myocardial Infarction via Activating PPARγ and PGC1α. PPAR Res. 2021, 9947656. PMID: 34422028; PMCID: PMC8373512. 10.1155/2021/9947656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Xian X., Wang Z., Bi Y., Chen Q., Han X., et al. (2018). Research Progress on the Relationship between Atherosclerosis and Inflammation. Biomolecules 8 (3), 80. PMID: 30142970; PMCID: PMC6163673. 10.3390/biom8030080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou J. G., Zhang J., Jia Z. H., Cao K. J. (2011). Evaluation of the Traditional Chinese Medicine Shensongyangxin Capsule on Treating Premature Ventricular Contractions: a Randomized, Double-Blind, Controlled Multicenter Trial. Chin. Med. J. (Engl) 124 (1), 76–83. PMID: 21362312. [PubMed] [Google Scholar]