Abstract
Purpose
This study aimed to comprehensively evaluate Chinese coronary heart disease (CHD) patients’ health-related quality of life (HRQoL) using various measures and explore influencing factors associated with HRQoL.
Methods
A cross-sectional study was conducted from April to September 2019 in the General Hospital of Tianjin Medical University. A convenience sampling framework was used to successively recruit 316 inpatients with CHD. Two generic preference-based instruments (EQ-5D-5L and 15D), a disease-specific instrument (Seattle Angina Questionnaire, SAQ), and the WHO-5 well-being index (WHO-5) were administered. Tobit regression model and multiple linear regression were used for data analyses.
Results
A total of 305 patients (mean age was 62.9) with CHD participated in this study. The mean health state utility (HSU) scores of EQ-5D-5L and 15D were 0.85 (SD=0.14) and 0.89 (SD=0.07), respectively. For EQ-5D-5L, pain/discomfort was the most frequently reported, followed by anxiety/depression. As for 15D, discomfort and symptoms was the most severely impaired dimension. For SAQ, more limitations were found in the domains of angina stability and disease perception. For WHO-5, the mean score was 16.93. Marital status, disease state and comorbidity were influencing factors associated with HRQoL, patient’s subjective well-being had a positive impact on HRQoL.
Conclusion
To improve the HRQoL of CHD patients in China, more attention needs to be paid to unmarried and relapsed patients, especially those with comorbidity of hypertension. Additionally, more social support and psychological counseling should be provided to patients.
Keywords: coronary heart disease, health-related quality of life, subjective well-being, EQ-5D-5L, 15D, SAQ
Introduction
Coronary heart disease (CHD) is characterized by cholesterol-containing deposits in major heart blood vessels, which can result in angina, shortness of breath, fatigue and myocardial infarction.1 It is a major public health problem worldwide because it is one of the most common diseases. Together with stroke, it is responsible for the largest number of premature cardiovascular diseases (CVDs) deaths.2 Although the CHD mortality rate has declined over the past two decades, the number of life years lost to premature CHD deaths has increased in low- and middle-income countries.3,4 In China, it is estimated that over 11 million people are living with CHD, and the figure is expected to increase steadily in the next few decades.5 The mortality rate of CHD was 121.59 per 10 thousand people in urban areas and 130.14 per 10 thousand people in rural areas of China in 20196 and continues to rise.7
Lower health-related quality of life (HRQoL) is often experienced post-cardiac events.8 Given the improvements in treatment and preventive measures, patients have to contend with CHD symptoms such as chest pain and breathlessness, as well as complex treatment regimens, which will give a far-reaching effect on their health related quality of life (HRQoL).9 HRQoL is a multidimensional concept, which refers to people’s capacity to perform daily activities (ie functioning) in addition to their life perspective (ie well-being) and subjective management of their health condition.10 It has gained attention as an important patient-reported outcome measure in recent years to inform patient-centered care, clinical decision-making, and health policy or reimbursement decisions.11 In addition, HRQoL is also important in predicting long-term prognosis, mortality, and coronary event recurrence.12 Furthermore, it has been proposed that subjective well-being (SWB) which refers to a broad category of phenomena that includes emotional responses, domain satisfactions, and global judgements of life satisfaction should be considered in quantifying people’s wellbeing.13 In view of these, SWB could be another important index to the HRQoL for CHD patients.14
There were a large variety of generic and disease-specific instruments with proven validity and reliability have been developed to assess HRQoL of CHD patients.15 Generic preference-based instruments can be used to measure health state utility (HSU) scores which are applied to calculate quality-adjusted life years (QALYs) for cost-utility analyses.16 Disease-specific instruments focus on problems associated with individual disease states, patient groups or areas of function.17 For example, the Seattle Angina Questionnaire (SAQ) is one of the most widely used disease-specific instruments which is designed to explicitly quantify HRQoL associated with CHD.18,19
There have been several investigations of HRQoL in patients with CHD.20–22 However, only a few studies used multiple HRQoL instruments to comprehensively measure the CHD patients’ HRQoL and subjective well-being.23,24 Moreover, most studies did not report health state utility scores of CHD patients at different clinical characteristics, which play an important role in the cost-utility analysis. At present, some studies have assessed factors affecting CHD in China, including age, education, alcohol consumption, diet and physical activity.25,26 Previous studies have highlighted the severity of CHD was related to HRQoL,27 however, most of the population was from rural areas, and little is known about hospitalized patients. Therefore, this study aimed to comprehensively evaluate the HRQoL and subjective well-being of CHD inpatients at different characteristics and to explore influencing factors associated with poor HRQoL.
Materials and Methods
Study Design and Population
A cross-sectional survey was conducted in the General Hospital of Tianjin Medical University, China, from April to September 2019. A convenience sampling framework was used to recruit all newly admitted patients with CHD in the cardiology department. Patients who were diagnosed by medical examination with CHD and were more than 18 years old were eligible to participate in this study. Exclusion criteria were those who were unable to understand the questionnaires, with serious comorbidities (such as a malignant tumor), with a history of mental illness, or those who have hearing or vision impairment and cannot answer questions. Written consent was obtained from all participants prior to entry into this study. Ethical approval was obtained from the Ethics Review Board of the School of Health Care Management, Shandong University (Reference No. ECSHCMSDU20191002), and the research adhered to the tenets of the Declaration of Helsinki.
The study sample size was powered based on the health state utility of uncertainty around the estimates. The highest standard deviation (σ) was assumed to be 0.17 in this study. The margin of error (ω) can be estimated with half of the 95% confidence interval (CI), the previous systematic review reported health utility value of cardiovascular disease patients was 0.77 (95% CI = 0.75–0.79).28 Using Equation (1) with σ=0.17 and ω=0.02 gives an estimated sample size for the survey of n=277 CHD patients.29 Furthermore, considering the rate of loss (10%), the total required theoretical sample size was 308 participants.
 |
(1) |
The patients were assured that even if they agreed to participate and signed informed consent, they still have the right to withdraw from the study at any time and their privacy will be assured. After giving informed consent, the trained investigators administered the survey via face-to-face interviews in a separate room.
The questionnaire consisted of three sections. The first section included questions on demographics and socioeconomics status (gender, age, residence, educational level, occupation, marital status, and monthly income). The clinical information included disease type, disease duration and comorbidities, which was filled by the patient’s attending doctor. The third section was the measurement of HRQoL, including two generic preference-based instruments (EQ-5D-5L and 15D), the disease-specific instrument (Seattle Angina Questionnaire, SAQ), and the WHO-5 Well-Being Index (WHO-5).
HRQoL and Wellbeing Measurement
EQ-5D-5L is a generic, preference-based instrument for measuring HRQoL with five dimensions: mobility (MO), self-care (SC), usual activities (UA), pain/discomfort (PD) and anxiety/depression (AD). Each dimension has five levels of response (no problems, slight problems, moderate problems, severe problems and extreme problems), which generate 3125 health states. The Chinese version of EQ-5D-5L and the Chinese-specific scoring algorithm of EQ-5D-5L were used in this study.30,31 The theoretical index score ranges from −0.391 to 1 (1= full health, 0= being dead), and a score less than 0 represents a health status worse than death.
15D is a generic and multidimensional questionnaire for measuring HRQoL. It was originally developed in Finland and contains 15 dimensions: mobility, vision, hearing, breathing, sleeping, eating, speech, excretion, usual activities, mental function, discomfort and symptoms, depression, distress, vitality, and sexual activity. Each dimension is divided into five ordinal levels, by which more or less the attribute is distinguished. The single index score (15D score), which represents the overall HRQoL, is calculated by applying a set of population-based utility values to responses. The score ranges from 0 to 1, where 1 represents full health, 0 represents death, and higher scores indicate better functioning and HRQoL. The Chinese version of the 15D was used in this study and was scored using the Finnish tariff because the Chinese tariff has not yet been available.32
SAQ is a commonly used disease-specific instrument for assessing symptoms and their impact on daily life with CHD. It has 19 items which can be grouped into five domains: physical limitation (PL), angina stability (AS), angina frequency (AF), treatment satisfaction (TS) and disease perception (DP). The SAQ is scored by assigning each response an ordinal value, beginning with 1 for the response that implies the lowest level of functioning, and summing across items within each of the five scales. Scale scores are then transformed to a 0–100 range by subtracting the lowest possible score, dividing the range of the scale and multiplying by 100.33 A higher score on SAQ indicates a higher level of functioning and better HRQoL.
WHO-5 is one of the most widely used generic questionnaires assessing subjective psychological well-being. It consists of five positively items, which are related to positive mood, vitality and general interests. Each item is scored from 5 (all of the time) to 0 (none of the time), and the raw scores theoretically range from 0 (absence of well-being) to 25 (maximal well-being). The respondent is asked to rate to what extent each of the 5 statements can apply to him or her when considering the past two weeks. A total score of less than 13 indicates that the participant may be depressed.34
Statistical Analysis
Descriptive statistics were performed on participants’ characteristics and the distribution of HRQoL and wellbeing scores. Frequencies and percentages were used for categorical variables, while means and standard deviations (SD) were reported for continuous variables. Kolmogorov–Smirnov test was used to test the normality of the variable’s distribution. When testing the differences in participants’ health-related quality of life and subject well-being among various sub-groups, Student’s t-test or analysis of variance (ANOVA) was chosen when variables conformed to an approximately normal distribution; otherwise, the Mann–Whitney U-test or Kruskal–Wallis test was used. In the study, the floor or ceiling effect was considered to be present if more than 15% of respondents achieved the lowest or the highest possible score, respectively.35
When studying the factors associated with HRQoL, we chose EQ-5D-5L HSU scores (Chinese tariff of 15D has not yet been available) and SAQ scores as dependent variables. As the HSU scores of EQ-5D-5L were left-skewed with a large proportion of respondents in full health, the Tobit regression model was used, whilst for SAQ scores, a multiple linear regression was used to identify the significant independent predictors, respectively.
Independent variables consist of socio-demographic and clinical characteristics of the participants, including gender (male, female), age (30–54, 55–64, ≥65 years), residence (rural, urban), educational level (illiteracy or primary school, secondary school, high school or technical secondary school, university degree and above), occupation (employed, retired), marital status (married, unmarried), monthly income (<2000, 2000–4000, >4000), duration of CHD (≤0.5, 0.51–1, >1 month), disease state (first episode, relapse), comorbidity (hypertension, diabetes, hyperlipidemia), and whether participants could have depression according to the WHO-5 scores (<13, ≥13). Data were entered into Epidata 3.1 and analyzed using SPSS 20.0 and STATA 15.0. A two-tailed P<0.05 was considered statistically significant.
Results
Participants’ Characteristics
A total of 316 participants were invited to participate in the study and among them, five participants refused to participate. A further six participants who initially agreed to participate withdrew from the survey after completing socio-demographic information. The characteristics of 305 participants who completed the survey were presented in Table 1. The mean ± standard deviation (SD) age of participants was 62.9 ± 9.9 years, males and females were equally divided. Of the participants, 88.2% completed secondary school and above education, most of them (88.9%) lived in the urban area, 94.4% were married, 70.5% were retired, and more than half of them had more than 4000 RMB (around US$620) monthly income. Two-thirds (67.9%) of participants had unstable angina, the mean duration of CHD is 1.8±2.3 months, and 57.0% of participants were in the first episode. Many participants had comorbidities: hypertension, diabetes, and hyperlipidemia accounted for 63.9%, 31.8%, and 31.5%, respectively. There were 13.4% of participants who had a WHO-5 score of less than 13, indicating that they may have depression.
Table 1.
Participants’ Characteristics (n=305)
| Characteristics | N (%) |
|---|---|
| Socio-demographic | |
| Gender | |
| Male | 154 (50.5) |
| Female | 151 (49.5) |
| Age years (Mean ± SD) | 62.9 ± 9.9 |
| 30–54 | 47 (15.4) |
| 55–64 | 121 (39.7) |
| ≥65 | 137 (44.9) |
| Residence | |
| Rural area | 34 (11.1) |
| Urban area | 271 (88.9) |
| Educational level | |
| Illiteracy or primary school | 36 (11.8) |
| Secondary school | 120 (39.3) |
| High school or technical secondary school | 92 (30.2) |
| University degree and above | 57 (18.7) |
| Occupation | |
| Employeda | 90 (29.5) |
| Retired | 215 (70.5) |
| Marital status | |
| Married | 288 (94.4) |
| Unmarriedb | 17 (5.6) |
| Monthly income (RMB) | |
| <2000 | 25 (8.2) |
| 2000–4000 | 113 (37.0) |
| >4000 | 167 (54.8) |
| Clinical characteristics | |
| CHD type | |
| Stable angina | 76 (24.9) |
| Unstable angina | 207 (67.9) |
| Remote myocardial infarction | 6 (2.0) |
| Acute myocardial infarction | 16 (5.2) |
| Duration of CHD (Mean ± SD) | 1.8 ± 2.3 |
| ≤0.5 months | 117 (38.4) |
| 0.51–1 months | 82 (26.9) |
| >1 months | 106 (34.8) |
| Disease state | |
| First episode | 174 (57.0) |
| Relapse | 131 (43.0) |
| Prevalence of comorbidities | |
| Hypertension | 195 (63.9) |
| Diabetes | 97 (31.8) |
| Hyperlipidemia | 96 (31.5) |
| Subjective well-being | |
| WHO-5 scores <13 | 41 (13.4) |
| WHO-5 scores≥13 | 264 (86.6) |
Notes: aEmployed includes working in public institutions and companies, civil servants and freelancers. bUnmarried includes single, divorced, widowed and separate.
Participants’ HRQoL and Subject Well-Being
The descriptive statistics of EQ-5D-5L, 15D, SAQ and WHO-5 scores for CHD patients were shown in Table 2. Between the two generic, preference-based instruments, the mean HSU score of EQ-5D-5L was 0.85 (SD=0.14), while the HSU score of 15D was 0.89 (SD=0.07). It can be seen that substantial ceiling effects in the EQ-5D-5L with 18.4% respondents reported having full health. The SAQ had a mean score of 55.49 and no respondents reported having a full health state. The WHO-5 well-being index had a mean score of 16.93 and only one participant reported the highest wellbeing.
Table 2.
Descriptive Statistics of the Different Instruments
| Instruments | Theoretical Range | Observed Range | Mean (SD) | Ceiling Effect (%) | Floor Effect (%) |
|---|---|---|---|---|---|
| EQ-5D-5L | −0.39, 1 | 0.17, 1 | 0.85 (0.14) | 56 (18.4) | 0 (0) |
| 15D | 0, 1 | 0.60, 1 | 0.89 (0.07) | 22 (7.2) | 0 (0) |
| SAQ | 0, 100 | 27.59, 78.16 | 55.49 (10.57) | 0 (0) | 0 (0) |
| WHO-5 | 0, 25 | 5, 23 | 16.93 (3.51) | 0 (0) | 1 (0.3) |
The participants’ HRQoL scores and subject well-being by each characteristic were listed in Table 3. In the EQ-5D-5L, the average score of employed (0.87) was significantly higher than that of retired (0.84). Participants who had lower income, relapsed, comorbidities with hypertension scored lower compared to other groups (P<0.05). In the 15D, the average score of females (0.88) was significantly lower than males (0.90). Participants who were older, retired, relapsed, and comorbidities with hypertension scored lower compared to other groups in 15D and SAQ scores. The differences in WHO-5 scores between different levels of these characteristics were not statistically significant.
Table 3.
Participants’ Health-Related Quality of Life and Subject Well-Being
| Subject Characteristics | Health-Related Quality of Life | Subject Well-Being | ||||||
|---|---|---|---|---|---|---|---|---|
| EQ-5D-5L Mean (95% CI) | P-value | 15D Mean (95% CI) | P-value | SAQ Mean (95% CI) | P-value | WHO-5 Mean (95% CI) | P-value | |
| All | 0.85 (0.83,0.86) | 0.89 (0.88,0.90) | 55.49 (54.30,56.68) | 16.93 (16.53,17.32) | ||||
| Gender | 0.084a | 0.041a | 0.558c | 0.079c | ||||
| Male | 0.86 (0.84,0.88) | 0.90 (0.89,0.91) | 55.95 (55.27,57.63) | 17.31 (16.80,17.83) | ||||
| Female | 0.84 (0.81,0.86) | 0.88 (0.87,0.89) | 55.02 (53.31,56.73) | 16.54 (15.94,17.14) | ||||
| Age (years) | 0.213b | <0.001b | 0.049d | 0.958d | ||||
| 30–54 | 0.87 (0.84,0.90) | 0.92 (0.90,0.94) | 58.18 (55.03,61.33) | 16.87 (15.81,17.93) | ||||
| 55–64 | 0.86 (0.83,0.88) | 0.89 (0.88,0.91) | 56.01 (54.21,57.81) | 16.82 (16.15,17.48) | ||||
| ≥65 | 0.83 (0.80,0.86) | 0.87 (0.86,0.88) | 54.11 (52.27,55.94) | 17.04 (16.48,17.61) | ||||
| Residence | 0.214a | 0.513a | 0.389c | 0.375c | ||||
| Rural area | 0.86 (0.80,0.92) | 0.88 (0.85,0.91) | 56.69 (52.40,60.98) | 17.18 (15.86,18.49) | ||||
| Urban area | 0.85 (0.83,0.86) | 0.89 (0.88,0.90) | 55.34 (54.10,56.58) | 16.90 (16.48,17.31) | ||||
| Educational level | 0.943b | 0.897b | 0.983d | 0.991d | ||||
| Illiteracy or primary school | 0.84 (0.79,0.90) | 0.88 (0.86,0.91) | 56.00 (52.14,59.86) | 17.11 (15.95,18.27) | ||||
| Secondary school | 0.84 (0.82,0.87) | 0.89 (0.87,0.90) | 55.22 (53.30,57.14) | 16.99 (16.36,17.63) | ||||
| High school or technical secondary school | 0.85 (0.83,0.88) | 0.89 (0.87,0.90) | 55.82 (53.57.58.07) | 16.70 (15.94,17.45) | ||||
| University degree and above | 0.85 (0.82,0.89) | 0.89 (0.87,0.91) | 55.19 (52.63,57.76) | 17.05 (16.16,17.95) | ||||
| Occupation | 0.018a | 0.013a | 0.013c | 0.107c | ||||
| Employed | 0.87 (0.84,0.90) | 0.90 (0.89,0.92) | 57.51 (55.22,59.80) | 17.32 (16.59,18.05) | ||||
| Retired | 0.84 (0.82,0.86) | 0.88 (0.87,0.89) | 54.64 (53.26,56.03) | 16.76 (16.29,17.24) | ||||
| Marital status | 0.078a | 0.180a | 0.087c | 0.502c | ||||
| Married | 0.85 (0.84,0.87) | 0.89 (0.88,0.90) | 55.75 (54.52,56.97) | 16.96 (16.56,17.37) | ||||
| Unmarried | 0.77 (0.68,0.87) | 0.87 (0.83,0.90) | 51.12 (46.04,56.19) | 16.35 (14.42,18.28) | ||||
| Monthly income (RMB) | 0.046b | 0.101b | 0.317d | 0.326d | ||||
| <2000 | 0.81 (0.74,0.88) | 0.87 (0.84,0.90) | 54.21 (48.89,59.53) | 16.36 (14.53,18.19) | ||||
| 2000–4000 | 0.82 (0.80,0.85) | 0.88 (0.87,0.90) | 54.49 (52.57,56.41) | 16.47 (15.76,17.18) | ||||
| >4000 | 0.87 (0.85,0.89) | 0.89 (0.88,0.91) | 56.36 (54.77,57.94) | 17.32 (16.85,17.80) | ||||
| CHD type | 0.085b | 0.420b | 0.213d | 0.091d | ||||
| Stable angina | 0.85 (0.81,0.89) | 0.90 (0.88,0.91) | 56.79 (54.25,59.33) | 16.82 (16.04,17.60) | ||||
| Unstable angina | 0.85 (0.83,0.86) | 0.88 (0.87,0.89) | 54.76 (53.34,56.18) | 16.86 (16.37,17.34) | ||||
| Remote myocardial infarction | 0.96 (0.90,1.00) | 0.91 (0.83,1.00) | 61.11 (52.77,69.45) | 19.67 (16.96,22.38) | ||||
| Acute myocardial infarction | 0.82 (0.74,0.90) | 0.89 (0.85,0.92) | 56.61 (50.62,62.60) | 17.38 (15.54,19.21) | ||||
| Duration of CHD | 0.772b | 0.161b | 0.191d | 0.697d | ||||
| ≤0.5 months | 0.85 (0.83,0.88) | 0.90 (0.88,0.91) | 56.73 (54.63,58.84) | 16.92 (16.30,17.55) | ||||
| 0.51–1 months | 0.85 (0.82,0.88) | 0.89 (0.87,0.91) | 55.44 (53.31,57.57) | 16.68 (15.86,17.51) | ||||
| >1 months | 0.84 (0.81,0.87) | 0.88 (0.87,0.89) | 54.15 (52.22,56.09) | 17.12 (16.46,17.78) | ||||
| Disease state | 0.006a | 0.007a | 0.046c | 0.377c | ||||
| First episode | 0.87 (0.85,0.89) | 0.90 (0.89,0.91) | 56.53 (55.05,58.02) | 16.92 (16.36,17.48) | ||||
| Relapse | 0.82 (0.80,0.85) | 0.88 (0.86,0.89) | 54.10 (52.15,56.05) | 16.94 (16.38,17.50) | ||||
| Comorbidities with Hypertension | 0.018a | 0.026a | 0.048c | 0.127c | ||||
| Yes | 0.83 (0.81,0.85) | 0.88 (0.87,0.89) | 54.54 (53.03,56.04) | 16.71 (16.20,17.23) | ||||
| No | 0.88 (0.86,0.90) | 0.90 (0.89,0.92) | 57.18 (55.25,59.11) | 17.31 (16.69,17.93) | ||||
| Comorbidities with Diabetes | 0.903a | 0.215a | 0.383c | 0.139c | ||||
| Yes | 0.84 (0.80,0.87) | 0.88 (0.86,0.90) | 54.92 (52.60,57.24) | 16.55 (15.80,17.29) | ||||
| No | 0.85 (0.83,0.87) | 0.89 (0.88,0.90) | 55.75 (54.37,57.14) | 17.11 (16.64,17.57) | ||||
| Comorbidities with Hyperlipidemia | 0.234a | 0.453a | 0.673c | 0.443c | ||||
| Yes | 0.84 (0.81,0.87) | 0.88 (0.87,0.90) | 55.30 (53.26,57.34) | 16.78 (16.07,17.49) | ||||
| No | 0.85 (0.83,0.87) | 0.89 (0.88,0.90) | 55.57 (54.10,57.05) | 17.00 (16.52,17.48) | ||||
Notes: aMann–Whitney U-test, the statistic is Z. bKruskal–Wallis test, the statistic is x2. cStudent’s t-test, the statistic is t. dAnalysis of variance (ANOVA), the statistic is F. Bold p-values represent significant differences among subgroups.
Abbreviation: CI, confidence interval.
Distribution of Self-Reported Health Problems of Participants
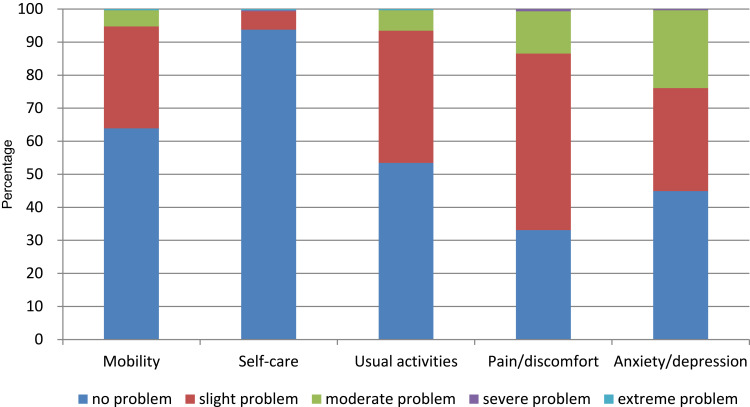
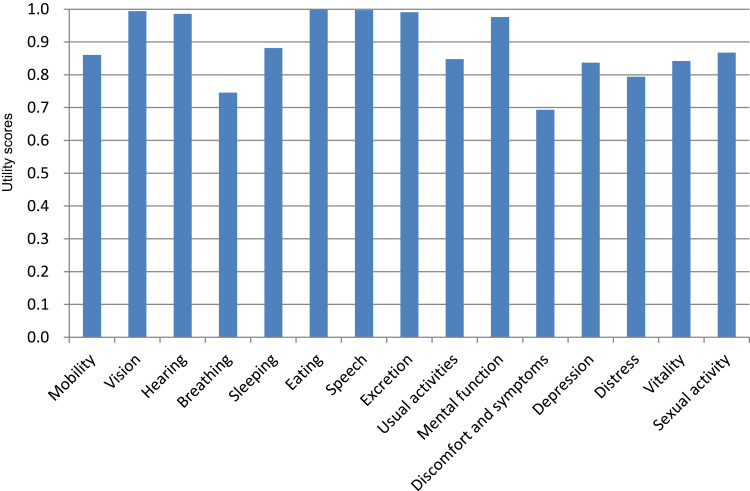
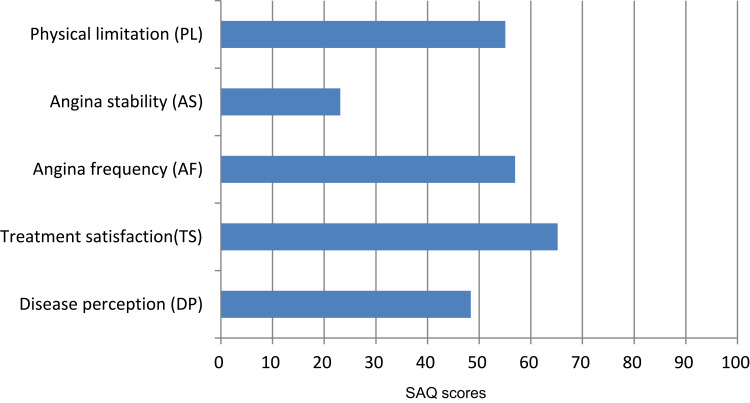
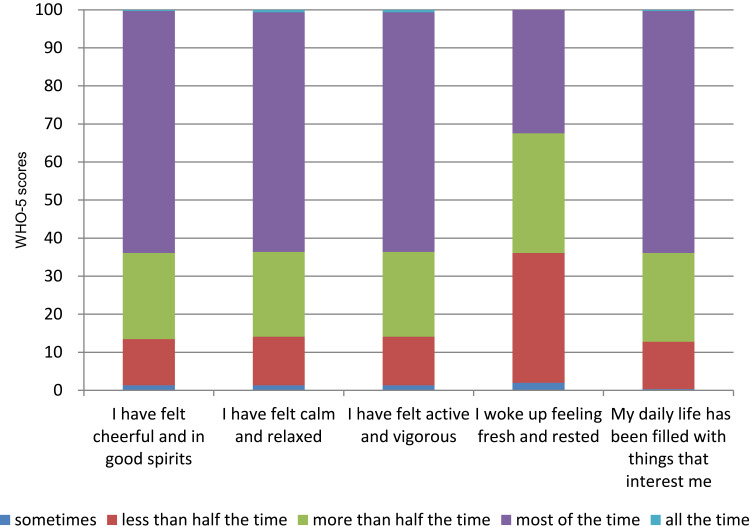
Self-reported health problems and HRQoL scores of participants were shown in Figures 1–4. For EQ-5D-5L (Figure 1), pain/discomfort was the most frequently reported, followed by anxiety/depression. As for 15D (Figure 2), discomfort and symptoms was the most impaired dimension among participants, followed by breathing. For SAQ (Figure 3), more limitations were found in the domains of angina stability and disease perception. For WHO-5, 36.1% of participants stated that they felt fresh and rested after waking up less than half of the time, which was the worst dimension (Figure 4).
Figure 1.
Health problems reported by participants in each dimension of EQ-5D-5L.
Figure 2.
The mean health state utility scores of 15D in different dimensions.
Figure 3.
The scores of different domains in SAQ.
Figure 4.
Distribution of responses of the WHO-5 well-being index.
Factors Associated with EQ-5D-5L HSU Scores and SAQ Scores
The results of multivariate analyses of the factors associated with HRQoL were shown in Table 4. For the EQ-5D-5L HSU scores, married patients had a significantly higher mean EQ-5D score than those of unmarried, while for SAQ scores, there was no significant statistical difference in marital status. Regarding clinical characteristics, patients who experienced a relapse of CHD had significant lower HSU scores and SAQ scores (P<0.001 and P=0.006). Comorbidities had a negative influence on HRQoL, where patients comorbidities with hypertension had lower HSU scores than those without comorbidities (P=0.030). Potential depression status (indicated by WHO-5 scores) was significantly associated with EQ-5D-5L HSU and SAQ scores (P<0.001 and P<0.001). On the other hand, gender, age, educational level, occupation, monthly income and duration of CHD were not significantly associated with EQ-5D-5L HSU scores and SAQ scores.
Table 4.
Tobit Regression Analysis and Multiple Linear Regression on the EQ-5D-5L HSU Scores and SAQ Scores
| Factors | EQ-5D-5L | SAQ | ||||
|---|---|---|---|---|---|---|
| Coefficient | SE | P-value | Coefficient | SE | P-value | |
| Gender (ref.: male) | ||||||
| Female | −0.017 | 0.017 | 0.313 | −0.150 | 1.143 | 0.896 |
| Age (years) (ref.: 30–54) | ||||||
| 55–64 | 0.016 | 0.030 | 0.602 | −0.766 | 2.024 | 0.705 |
| ≥65 | −0.001 | 0.033 | 0.982 | −1.950 | 2.206 | 0.377 |
| Educational level (ref.: illiteracy or primary school) | ||||||
| Secondary school | −0.023 | 0.034 | 0.488 | −1.444 | 2.243 | 0.520 |
| High school or technical secondary school | −0.017 | 0.035 | 0.623 | −0.770 | 2.338 | 0.742 |
| University degree and above | −0.024 | 0.037 | 0.519 | −1.619 | 2.454 | 0.510 |
| Occupation (ref.: employed) | ||||||
| Retired | −0.033 | 0.026 | 0.201 | −1.228 | 1.722 | 0.476 |
| Marital status (ref.: married) | ||||||
| Unmarried | −0.085 | 0.040 | 0.034 | −2.829 | 2.612 | 0.280 |
| Monthly income (ref.: <2000) | ||||||
| 2000–4000 | 0.037 | 0.035 | 0.294 | 2.570 | 2.461 | 0.297 |
| >4000 | 0.066 | 0.035 | 0.063 | 2.827 | 2.460 | 0.252 |
| Duration of CHD (ref.: ≤0.5 month) | ||||||
| 0.51–1 | 0.006 | 0.022 | 0.781 | −0.140 | 1.456 | 0.923 |
| >1 | −0.032 | 0.021 | 0.127 | −3.209 | 1.359 | 0.019 |
| Disease state (ref.: First episode) | ||||||
| Relapse | −0.067 | 0.018 | <0.001 | −3.331 | 1.192 | 0.006 |
| Comorbidities with Hypertension (ref.: Yes) | ||||||
| No | 0.041 | 0.019 | 0.030 | 1.896 | 1.248 | 0.130 |
| Comorbidities with Diabetes (ref.: Yes) | ||||||
| No | −0.009 | 0.020 | 0.637 | −0.266 | 1.295 | 0.838 |
| Comorbidities with Hyperlipidemia (ref.: Yes) | ||||||
| No | −0.005 | 0.019 | 0.782 | −0.796 | 1.266 | 0.530 |
| Subjective well-being (ref.: WHO-5 <13) | ||||||
| WHO-5 ≥13 | 0.158 | 0.025 | <0.001 | 11.480 | 1.715 | <0.001 |
Notes: Bold p-values represent significant relationship between the independent variable and dependent variable.
Abbreviation: SE, standard error.
Discussion
To our knowledge, this is the first comprehensive study evaluating the HRQoL of Chinese CHD inpatients using generic preference-based, disease-specific, and subjective well-being instruments. The result indicated that among Chinese CHD patients, pain/discomfort (EQ-5D-5L), discomfort and symptoms (15D) and angina stability (SAQ) were the most frequently reported problems. The study also identified that marital status, disease state, comorbidity, and being potentially depressive (according to WHO-S scores) were influencing factors that were significantly associated with HRQoL.
The mean EQ-5D-5L score was 0.85 (SD=0.14), with a range of 0.17 to 1.00, which was slightly lower than those of the general Chinese population.36 For CHD patients in China, previously reported health utility scores range from 0.75 to 0.914.25,37 A rural cohort study of Henan province in China reported a mean health utility score for CHD patients as 0.914, which was the highest HSU score of CHD patients in China at present.25 In an earlier cross-sectional study of stable angina patients recruited from 4 hospitals showed that the mean health utility score was 0.75.37 When comparing with relevant studies from other Asian countries, the mean EQ-5D index score was reported to be 0.82 among Vietnamese patients with cardiovascular disease,40 which was similar to our findings. Outside Asia, a Danish study compared utility values among different cardiovascular diseases and found that heart transplant patients had the highest value (0.82), while arrhythmia patients had the lowest value (0.70).38 The study by Jrab et al reported a much lower mean EQ-5D utility score of 0.392 in patients with angina in Jordan.39 There are a couple of notable reasons to explain the difference between our study and the literature, in addition to the differences in participants’ characteristics (eg our participants were hospitalized patients and most of them were older adults and with comorbidities). Previous Chinese studies using EQ-5D-5L for CHD in Chinese populations were based on value sets from other countries and this potentially introduces bias due to cultural and population discrepancies. For previous literature using the EQ-5D-3L, their results could be less sensitive than the new EQ-5D-5L instrument we adopted in this study.
Consistent with what has been well documented that CHD has the primary impact on the physical function of patients, our results also demonstrate that pain/discomfort was the most frequently reported problem in EQ-5D-5L (66.9%) whilst in 15D, discomfort and symptoms was the most impaired dimension with a score of 0.69. SAQ scores showed that patients experienced impaired disease-specific health status, especially in angina stability (23.11). Our findings highlight the fact that angina is a common symptom in patients with CHD, along with chest pain, chest tightness, fatigue or lowered mood. As reported in previous studies, discomfort in the chest due to CHD can significantly impact HRQoL.41 Recent evidence suggested coronary microvascular endothelial dysfunction is associated with cardiovascular events and can be an important mechanism for persistent chest pain in these patients.42 Furthermore, previous studies showed that treatment of angina is associated with improvement in physical, mental and social domains of HRQoL.43 It is therefore important to diagnose chest pain and other angina symptoms as well as to treat microvascular endothelial dysfunction timely to improve HRQoL of CHD patients.
In the study, married patients reported better HRQoL, which is consistent with other research that conclude being married is a protective factor for HRQoL in CHD patients.26,44 The available evidence indicates that the marital relationship holds the greatest significance for health.45 There were several possible reasons. First, the marital relationship becomes more salient to individuals later in life and that affects individual well-being.46,47 Second, poor marital status was a key source of stress for individuals, which can undermine immune function48 and declines with age over time, thus having stronger adverse effects on health.49 Third, marital stress would serve to activate and sustain cardiovascular reactivity (eg, high blood pressure, elevated heart rate), and those persons with CHD may be more vulnerable to this source of stress.50
The results indicate that CHD patients with a recurrence and long disease duration had impaired HRQoL. Disease recurrence was extremely common as 40% of acute coronary syndrome survivors were readmitted to a hospital within 30 days of discharge51 and 20% experienced a repeat cardiac event within the first year.52 Previous studies confirmed that prolonged disease duration increases the risk of cardiac arrest and aortic dissection in patients.53 In addition, patients who live with heart failure or survive an acute coronary event may live for an extended period of time but often may be incapacitated,54 and relapsed patients may suffer from physical and social dysfunctions such as slurred speech and reduced sensory sensitivity, which can make the patient’s HRQoL worse. Therefore, cardiac rehabilitation (CR) which aims to improve multiple aspects of a patient’s life and includes several interventions is needed. Exercise-based CR is the most widely recognised CR strategy,55 and a recent systematic review conducted that exercise-based CR could achieve clinically meaningful improvements in physical performance, general health, and physical functioning in the short and long term in contemporary acute coronary syndrome patients.56 To improve patients’ physical functioning, reduce physical limitations, and regain previous abilities, the Chinese government has implemented national guidelines since 2020 to promote the use of cardiac rehabilitation in primary hospitals.57
Comorbidity plays an important role in the variation of HRQoL. The findings of this study reveal that CHD patients had a high prevalence of comorbid hypertension (63.9%), and patients with hypertension had lower HRQoL than those without comorbidities, which is congruent with other studies in China.58 Hypertension is the leading modifiable risk factor for cardiovascular disease, which represents the top cause of death in China.59 A nationwide survey shows that 23.2% (≈244.5 million individuals) of the Chinese adult population ≥18 years of age had hypertension.60 Previous studies have found that for every 10 mmHg increase in blood pressure, the incidence of CHD will increase by about 30%. Hypertension can promote the formation of coronary atherosclerosis and increase the oxygen consumption of the myocardium, causing symptoms of angina.61 Many CHD patients do not pay much attention to hypertension in China due to the lack of obvious signs and symptoms. Therefore, healthcare workers should be aware of the additional influence of comorbidities on CHD patients’ HRQoL to design the treatment plan accordingly.
Better subjective well-being (ie when WHO-5≥13) was found to be positively associated with patients’ HRQoL. There was growing evidence that subjective well-being and health are closely related, and positive psychological factors are associated with a lower risk of CHD mortality.62–64 It was reported that positive subjective well-being may influence health by buffering against the effects of stress and adjusting behaviour through the process of engagement and disengagement.65 Other studies demonstrated that positive subjective well-being may indirectly affect heart disease via health behaviours such as improved diet and increased physical activity66 or directly affect heart disease through alterations in the neuroendocrine, cardiovascular, and inflammatory systems.67 These findings implicated that measuring and monitoring the SWB of CHD patients is very important to improve their SWB and HRQoL.
This study has several limitations. First, participants were recruited at one tertiary hospital in Tianjin city, the results were somewhat skewed because of the residence distribution of participants, which may not represent CHD patients in mainland China as a whole. Second, this was a cross-sectional study, which can only suggest factors affecting the HRQoL of patients with CHD and cannot provide evidence of causality. The multi-center longitudinal study is needed to further explore the HRQoL of CHD patients in the future.
Conclusion
The study simultaneously applies generic and disease-specific HRQoL instruments to measure CHD patients’ HRQoL in China. It showed that HRQoL in CHD patients was lower than that of the general population in China and was significantly associated with patients’ marital status, disease state, comorbidity and subjective well-being. To improve the HRQoL of CHD patients in China, more attention needs to be paid to unmarried and relapsed patients, especially those with comorbidity of hypertension. Additionally, more social support and psychological counseling should be provided to patients.
Acknowledgments
The authors gratefully thank the investigators of the Department of Cardiovascular surgery, General Hospital of Tianjin Medical University for helping to collect the questionnaires. Thanks to all the participants for the contribution to this study.
Funding Statement
The study was supported by NHC Key Lab of Health Economics and Policy Research (Shandong University) (No.NHC-HEPR2018003); National Natural Science Foundation of China (71403056).
Abbreviations
CHD, coronary heart disease; CVD, cardiovascular disease; HRQoL, health-related quality of life; SWB, subjective well-being; QALYs, quality-adjusted life years; SAQ, Seattle Angina Questionnaire; WHO-5, WHO-5 well-being index; HSU, health state utility; CR, cardiac rehabilitation.
Data Sharing Statement
The supporting data can be obtained by contacting the corresponding author by email.
Ethics Approval and Informed Consent
The study was approved by the Ethics Review Board of the School of Health Care Management, Shandong University (Reference No.ECSHCMSDU20191002), and the research adhered to tenets of the Declaration of Helsinki.
Consent for Publication
All the authors agreed to publish.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics–2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322. doi: 10.1161/CIR.0000000000000152 [DOI] [PubMed] [Google Scholar]
- 2.Cooper R, Cutler J, Desvigne-Nickens P, et al. Trends and disparities in coronary heart disease, stroke, and other cardiovascular diseases in the United States: findings of the national conference on cardiovascular disease prevention. Circulation. 2000;102(25):3137–3147. doi: 10.1161/01.CIR.102.25.3137 [DOI] [PubMed] [Google Scholar]
- 3.Global Burden of Disease Study. 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;2015(386):743–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roth GA, Huffman MD, Moran AE, et al. Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation. 2015;132(17):1667–1678. doi: 10.1161/CIRCULATIONAHA.114.008720 [DOI] [PubMed] [Google Scholar]
- 5.China National Center for Cardiovascular Diseases. Report on Cardiovascular Diseases in China 2018. Encyclopedia of China: Publishing House; 2019. [Google Scholar]
- 6.National Health And Health Commission. 2020 China Health and Statistics Yearbook. Beijing: China Union Medical University Press; 2021. [Google Scholar]
- 7.Cheng J, Zhao D, Zeng Z, et al. The impact of demographic and risk factor changes on coronary heart disease deaths in Beijing, 1999–2010. BMC Public Health. 2009;9(1):30. doi: 10.1186/1471-2458-9-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Foxwell R, Morley C, Frizelle D. Illness perceptions, mood and quality of life: a systematic review of coronary heart disease patients. J Psychosom Res. 2013;75(3):211–222. doi: 10.1016/j.jpsychores.2013.05.003 [DOI] [PubMed] [Google Scholar]
- 9.Thomson P, Molloy GJ, Chung ML. The effects of perceived social support on quality of life in patients awaiting coronary artery bypass grafting and their partners: testing dyadic dynamics using the Actor-Partner Interdependence Model. Psychol Health Med. 2012;17:35–46. doi: 10.1080/13548506.2011.579988 [DOI] [PubMed] [Google Scholar]
- 10.Karimi M, Brazier J. Health, health-related quality of life, and quality of life: what is the difference? Pharmacoeconomics. 2016;34(7):645–649. doi: 10.1007/s40273-016-0389-9 [DOI] [PubMed] [Google Scholar]
- 11.Calvert M, Blazeby J, Altman DG, Revicki DA, Brundage MD. Reporting of patient-reported outcomes in randomized trials: the CONSORT PRO extension. JAMA J Am Med Assoc. 2013;309(8):814–822. doi: 10.1001/jama.2013.879 [DOI] [PubMed] [Google Scholar]
- 12.Hofer S, Benzer W, Oldridge N. Change in health-related quality of life in patients with coronary artery disease predicts 4-year mortality. Int J Cardiol. 2014;174(1):7–12. doi: 10.1016/j.ijcard.2014.03.144 [DOI] [PubMed] [Google Scholar]
- 13.Diener E, Suh EM, Lucas RE, Smith HL. Subjective well-being: three decades of progress. Psychol Bull. 1999;125(2):276–302. doi: 10.1037/0033-2909.125.2.276 [DOI] [Google Scholar]
- 14.Gao L, Moodie M, Chen G. Measuring subjective wellbeing in patients with heart disease: relationship and comparison between health-related quality of life instruments. Qual Life Res. 2019;28(4):1017–1028. doi: 10.1007/s11136-018-2094-y [DOI] [PubMed] [Google Scholar]
- 15.Le J, Dorstyn DS, Mpfou E, Prior E, Tully PJ. Health-related quality of life in coronary heart disease: a systematic review and meta-analysis mapped against the International Classification of Functioning, Disability and Health. Qual Life Res. 2018;27(10):2491–2503. [DOI] [PubMed] [Google Scholar]
- 16.Torrance GW. Measurement of health state utilities for economic appraisal. J Health Econ. 1986;5(1):1–30. doi: 10.1016/0167-6296(86)90020-2 [DOI] [PubMed] [Google Scholar]
- 17.Guyatt GH. Measurement of health-related quality of life in heart failure. J Am Coll Cardiol. 1993;22(4):185A–191A. doi: 10.1016/0735-1097(93)90488-M [DOI] [PubMed] [Google Scholar]
- 18.Kirtane AJ. The importance of listening to patients: the Seattle Angina Questionnaire. JAMA Cardiol. 2018;3(11):1037. doi: 10.1001/jamacardio.2018.2861 [DOI] [PubMed] [Google Scholar]
- 19.Spertus JA, Arnold SV. The evolution of patient-reported outcomes in clinical trials and management of patients with coronary artery disease: 20 years with the Seattle Angina questionnaire. JAMA Cardiol. 2018;3(11):1035–1036. doi: 10.1001/jamacardio.2018.2849 [DOI] [PubMed] [Google Scholar]
- 20.Wardoku R, Blair C, Demmer R, Prizment A. Association between physical inactivity and health-related quality of life in adults with coronary heart disease. Maturitas. 2019;128:36–42. doi: 10.1016/j.maturitas.2019.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barham A, Ibraheem R, Zyoud SH. Cardiac self-efficacy and quality of life in patients with coronary heart disease: a cross-sectional study from Palestine. BMC Cardiovasc Disor. 2019;19(1):290. doi: 10.1186/s12872-019-01281-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tang M, Wang SH, Li HL, Chen H, Ma SJ. Mental health status and quality of life in elderly patients with coronary heart disease. Peer J. 2021;9:e10903. doi: 10.7717/peerj.10903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Muhammad IMSO, He HG, Koh K, Thompson DR, Kowitlawakul Y, Wang W. Health-related quality of life and its predictors among outpatients with coronary heart disease in Singapore. Appl Nurs Res. 2014;27(3):175–180. doi: 10.1016/j.apnr.2013.11.008 [DOI] [PubMed] [Google Scholar]
- 24.Oreopoulos A, Padwal R, Mcalister FA. Association between obesity and health-related quality of life in patients with coronary artery disease. Int J Obesity. 2010;34(9):1434–1441. doi: 10.1038/ijo.2010.73 [DOI] [PubMed] [Google Scholar]
- 25.Mei YX, Wu H, Zhang HY, et al. Health-related quality of life and its related factors in coronary heart disease patients: results from the Henan Rural Cohort study. Sci Rep. 2021;11(1):5011. doi: 10.1038/s41598-021-84554-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang L, Yi-Qun W, Tang X. Profile and correlates of health-related quality of life in Chinese patients with coronary heart disease. Chin Med J Peking. 2015;128(14):1853. doi: 10.4103/0366-6999.160486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Muhammad I, He HG, Kowitlawakul Y, Wang W. Narrative review of health-related quality of life and its predictors among patients with coronary heart disease. Int J Nurs Pract. 2016;22(1):4–14. doi: 10.1111/ijn.12356 [DOI] [PubMed] [Google Scholar]
- 28.Zhou T, Guan H, Yao J, Xiong X, Ma A. The quality of life in Chinese population with chronic non-communicable diseases according to EQ-5D-3L: a systematic review. Qual Life Res. 2018;27(11):1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Walters SJ. Quality of Life Outcomes in Clinical Trials and Health-Care Evaluation: A Practical Guide to Analysis and Interpretation. John Wiley & Sons; 2009. [Google Scholar]
- 30.Luo N, Liu G, Li M, Guan H, Jin X, Rand-Hendriksen K. Estimating an EQ-5D-5L value set for China. Value Health. 2017;20(4):662–669. doi: 10.1016/j.jval.2016.11.016 [DOI] [PubMed] [Google Scholar]
- 31.Luo N, Li M, Liu GG, Lloyd A, de Charro F, Herdman M. Developing the Chinese version of the new 5-level EQ-5D descriptive system: the response scaling approach. Qual Life Res. 2013;22(4):885–890. doi: 10.1007/s11136-012-0200-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sintonen H. The 15-D measure of health related quality of life. II feasibility, reliability and validity of its valuation system. National Centre for Health Program Evaluation; 1995:42. [Google Scholar]
- 33.Spertus JA, Winder JA, Dewhurst TA, et al. Development and evaluation of the Seattle Angina questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25(2):333–341. doi: 10.1016/0735-1097(94)00397-9 [DOI] [PubMed] [Google Scholar]
- 34.Topp CW, Stergaard SD, Bech P, et al. The WHO-5 well-being index: a systematic review of the literature. Psychother Psychosom. 2015;84(3):167–176. doi: 10.1159/000376585 [DOI] [PubMed] [Google Scholar]
- 35.Terwee CB, Bot S, Boer M, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42. doi: 10.1016/j.jclinepi.2006.03.012 [DOI] [PubMed] [Google Scholar]
- 36.Yang Z, Busschbach J, Liu G, et al. EQ-5D-5L norms for the urban Chinese population in China. Health Qual Life Outcomes. 2018;16(1). doi: 10.1186/s12955-018-1036-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jing W, Han Y, Xu J, et al. Chronic stable angina is associated with lower health-related quality of life: evidence from Chinese patients. PLoS One. 2014;9. doi: 10.1371/journal.pone.0095955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Berg SK, Rasmussen TB, Thrysoee L, et al. DenHeart: differences in physical and mental health across cardiac diagnoses at hospital discharge. J Psychosom Res. 2017;94:1–9. doi: 10.1016/j.jpsychores.2017.01.003 [DOI] [PubMed] [Google Scholar]
- 39.Jarab AS, Almousa A, Rababa’H AM, Mukattash TL, Farha RA. Health-related quality of life and its associated factors among patients with angina in Jordan. Qual Life Res. 2019;29. 1027–1035. [DOI] [PubMed] [Google Scholar]
- 40.Tran BX, Moir MP, Thai T, et al. Socioeconomic inequalities in health-related quality of life among patients with cardiovascular diseases in Vietnam. Biomed Res Int. 2018;2018:1–8. doi: 10.1155/2018/2643814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Morys JM, Bellwon J, Hofer S, Rynkiewicz A, Gruchala M. Quality of life in patients with coronary heart disease after myocardial infarction and with ischemic heart failure. Arch Med Sci. 2016;12:326–333. doi: 10.5114/aoms.2014.47881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Reriani M, Flammer AJ, Duhe J, et al. Coronary endothelial function testing may improve long-term quality of life in subjects with microvascular coronary endothelial dysfunction. Open Heart. 2019;6(1):e870. doi: 10.1136/openhrt-2018-000870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Buser MA, Buser PT, Kuster GM, Grize L, Pfisterer M. Improvements in physical and mental domains of quality of life by anti-ischaemic drug and revascularisation treatment in elderly men and women with chronic angina. Heart. 2008;94(11):1413–1418. doi: 10.1136/hrt.2007.127589 [DOI] [PubMed] [Google Scholar]
- 44.Christian AH, Cheema AF, Smith SC, Mosca L. Predictors of quality of life among women with coronary heart disease. Qual Life Res. 2007;16(3):363–373. doi: 10.1007/s11136-006-9135-7 [DOI] [PubMed] [Google Scholar]
- 45.Umberson D, Williams K, Powers DA, Liu H, Needham B. You make me sick: marital quality and health over the life course. J Health Soc Behav. 2006;47(1):1–16. doi: 10.1177/002214650604700101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Carstensen LL. Social and emotional patterns in adulthood: support for socioemotional selectivity theory. Psychol Aging. 1992;7(3):331–338. doi: 10.1037/0882-7974.7.3.331 [DOI] [PubMed] [Google Scholar]
- 47.Simon RW. The meanings individuals attach to role identities and their implications for mental health. J Health Soc Behav. 1997;38(3):256–274. doi: 10.2307/2955370 [DOI] [PubMed] [Google Scholar]
- 48.Burman B, Margolin G. Analysis of the association between marital relationships and health problems: an interactional perspective. Psychol Bull. 1992;112(1):39–63. doi: 10.1037/0033-2909.112.1.39 [DOI] [PubMed] [Google Scholar]
- 49.Kiecolt-Glaser JK, Glaser R. Stress and immunity: age enhances the risks. Curr Dir Psychol Sci. 2001;10(1):18–21. doi: 10.1111/1467-8721.00105 [DOI] [Google Scholar]
- 50.Schaie KW, Dan B, House JS. Aging, Health Behaviors, and Health Outcomes. Lawrence Erlbaum Associates; 1992. [Google Scholar]
- 51.Sangu PV, Ranasinghe I, Costa BA, et al. Trends and predictors of rehospitalisation following an acute coronary syndrome: report from the Australian and New Zealand population of the Global Registry of Acute Coronary Events (GRACE). Heart. 2012;98(23):1728. doi: 10.1136/heartjnl-2012-302532 [DOI] [PubMed] [Google Scholar]
- 52.Tomas J, Pål H, Martin H, Hans H, Marcus T, Magnus J. Cardiovascular risk in post-myocardial infarction patients: nationwide real world data demonstrate the importance of a long-term perspective. Eur Heart J. 2015;36(19):1163. doi: 10.1093/eurheartj/ehu505 [DOI] [PubMed] [Google Scholar]
- 53.Wang J. The Research of Hospitalized Patients Quality Evaluation and Influencing Factors with Chronic Disease in One City. Dalian Medical University; 2016. [Google Scholar]
- 54.Fayers P, De Haes JC. Quality of life and clinical trials. Lancet. 1995;346(1):346. doi: 10.1016/S0140-6736(05)64534-5 [DOI] [PubMed] [Google Scholar]
- 55.Abell B, Glasziou P, Briffa T, Hoffmann T. Exercise training characteristics in cardiac rehabilitation programmes: a cross-sectional survey of Australian practice. Open Heart. 2016;3(1):e000374. doi: 10.1136/openhrt-2015-000374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Candelaria D, Randall S, Ladak L, Gallagher R. Health-related quality of life and exercise-based cardiac rehabilitation in contemporary acute coronary syndrome patients: a systematic review and meta-analysis. Qual Life Res. 2020;29(3):579–592. [DOI] [PubMed] [Google Scholar]
- 57.Chinese Medical Association. Coronary heart disease cardiac rehabilitation basic guidelines (2020). Chin J Gen Pract. 2021;20:16. [Google Scholar]
- 58.Wang W, Thompson DR, Ski CF, Liu M. Health-related quality of life and its associated factors in Chinese myocardial infarction patients. Eur J Prev Cardiol. 2014;21(3):321–329. doi: 10.1177/2047487312454757 [DOI] [PubMed] [Google Scholar]
- 59.Global, regional, and national age-sex specific mortality for. 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1151–1210. doi: 10.1016/S0140-6736(17)32152-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wang Z, Chen Z, Zhang L, et al. Status of hypertension in China: results from the China hypertension survey, 2012–2015. Circulation. 2018;137(22):2344–2356. doi: 10.1161/CIRCULATIONAHA.117.032380 [DOI] [PubMed] [Google Scholar]
- 61.Zhou L. The effect of health education and nursing intervention on the quality of life of patients with coronary heart disease and hypertension. J Clin Rational Use. 2017;10(29):105–106. [Google Scholar]
- 62.Tanno K, Sakata K, Ohsawa M, et al. Associations of ikigai as a positive psychological factor with all-cause mortality and cause-specific mortality among middle-aged and elderly Japanese people: findings from the Japan Collaborative Cohort Study. J Psychosom Res. 2009;67(1):67–75. doi: 10.1016/j.jpsychores.2008.10.018 [DOI] [PubMed] [Google Scholar]
- 63.Tindle HA, Chang YF, Kuller LH, et al. Optimism, cynical hostility, and incident coronary heart disease and mortality in the women’s health initiative. Circulation. 2009;120:656–662. doi: 10.1161/CIRCULATIONAHA.108.827642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Steptoe A, Deaton A, Stone AA. Subjective wellbeing, health, and ageing. Lancet. 2015;385(9968):640–648. doi: 10.1016/S0140-6736(13)61489-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rozanski A, Kubzansky LD. Psychologic functioning and physical health: a paradigm of flexibility. Psychosom Med. 2005;67:S47–53. doi: 10.1097/01.psy.0000164253.69550.49 [DOI] [PubMed] [Google Scholar]
- 66.Giltay EJ, Geleijnse JM, Zitman FG, Buijsse B, Kromhout D. Lifestyle and dietary correlates of dispositional optimism in men: the Zutphen Elderly Study. J Psychosom Res. 2007;63(5):483–490. doi: 10.1016/j.jpsychores.2007.07.014 [DOI] [PubMed] [Google Scholar]
- 67.Steptoe A, Dockray S, Wardle J. Positive affect and psychobiological processes relevant to health. J Pers. 2009;77(6):1747–1776. doi: 10.1111/j.1467-6494.2009.00599.x [DOI] [PMC free article] [PubMed] [Google Scholar]