Abstract
Background
The spread and emergence of antimicrobial resistance is the significant public health concerns over past decades. The major leading cause comes from irrational use of antibiotics.
Aim
To explore the characteristics of rational use of antibiotics and identify its predictive factors among public sector living in Nakhon Nayok Province, Thailand.
Methods
This project was conducted by using the data-source from Rational Use of Antibiotics (RUA) Survey Project at Nakhon Nayok Province. A cross-sectional community-based study method and face to face interviews were conducted. Two hundred fifty-four participants were selected by using Quota sampling method. Descriptive statistics were used to describe the sociodemographic and antibiotics use characteristics. Chi-square test were utilized to determine the association between explanatory variables and major outcome while multiple logistic regression was analysed to identify the predictors of antibiotics use behavior.
Results
The mean age of the participants was 42 years, those with aged between 35 and 56 had more rational use of antibiotics behavior than those with 13–34 years while older adults (57–78 years) were significantly associated with irrational use of antibiotics [AOR = 0.38; 95% CI (0.17–0.85)] than those with less than 34 years of age. Less than half (45.7%) and about one third of them (31.1%) showed adequate knowledge and appropriate attitude towards antibiotics use. An adequate knowledge [AOR = 3.37; 95% CI (1.92–5.90)], appropriate attitude [AOR = 2.90; 95% CI (1.54–5.43)], not using antibiotics within last 3 months [AOR = 1.89; 95% CI (1.04–3.43)], and not visiting drugstore when having three main diseases [AOR = 2.04; 95% CI (1.06–3.92)] were the significant predictors of rational antibiotics use (p-value <0.05).
Conclusion
Strategies development in terms of knowledge and attitude enhancement about antibiotics use particularly at the different ages together with RDU pharmacy encouragement and policy restriction of community drugstores antibiotics sales are the most effective method to promote rational antibiotics use behavior in the public sector.
Keywords: rational use of antibiotics, public sector, community-based survey, predictive factors, Thailand
Background
WHO defined “Rational Use of Medicine” as using correct medications that are relevant to clinical requirements of the patients, in exact doses according to the individual needs, for sufficient duration of time and at the lowest cost to them. A number of studies in different countries have hypothesized that behavior of rational antibiotic use was related to several factors such as age,1,2 gender,3 educational status,3,4 level of household income,1 health insurance1,5 and knowledge about antibiotic use3,4,6,7 of the participants.
Antibiotics are the most frequently used medications in majority of the developed and developing countries [especially when having 3 main diseases (Upper respiratory infection; URI, Acute Diarrhea; AD/ acute Gastroenteritis/ food poisoning and antibiotic prophylaxis in simple/ fresh wound; FW)]. Irrational use of medicines, especially antibiotics is one of the leading causes of AMR8 and was commonly seen in many developing countries with low level of Healthcare systems.9 WHO stated that the amount of antibiotics used in community areas was 80% of total antibiotics dispensed, of which 20–50% were used irrationally.10 Such irrational use of antibiotics can give rise to the development of resistance in certain microorganisms to effective antimicrobials, resulting in emergence and spread of antibiotic resistance at the community levels.11
The spread and emergence of antimicrobial resistance (AMR) is a global major public health challenge and concern that occurs across the world during recent years12 and it increases significantly in several countries which has Health and economic impacts on the life of people.13 Currently, more than 700,000 deaths happen around the world each year due to the higher prevalence of AMR infections and it was forecasted to project up to 10 million deaths by 2050 unless immediate and multidisciplinary actions were carried out in response to this critical situation.14,15 Asia region alone is considered as the most vulnerable area which over 4.7 million deaths due to AMR are predicted in 2050.16 Moreover, the World Health Organisation (WHO) also mentioned that South East Asia region is at the highest risk of AMR consequences where its problems on the issue of huge burden on health system and well-being of people are often neglected.17,18
In Thailand, the prevalence of bacterial infections, caused by AMR pathogens rose from less than 10% to over 40% between 2000 and 2011 and these kinds of infections, required 3.24 million days of hospitalization and about 38,000 deaths in 2010.19,20 Apart from the significant threats to many lives, AMR infections could lead to a remarkable economic burden of each country by resulting in a total cost of US$ 202 millions to the infections according to a recent study on AMR.19,21 According to the 2017 national household survey in Thailand, around 30% of adults misused the antibiotics and half of them had no idea about the after effect of antibiotics overuse. On top of these, only 17% of the whole population had received the correct information about rational use of antibiotics.22
These findings concluded that AMR became a crucial public health problem that requires urgent and comprehensive actions from many stakeholders to avert the consequences at both community and national levels.19 The Ministry of Public Health aware of the protection of people to receive the medicine treatment which is efficient, safe and cost effective, for this reason, in 2013, the Ministry of Public Health specified health system service development policy for rational drug use as the “Service plan of Rational drug use in hospital” (RDU service plan) under the Office of the Permanent Secretary for Public Health. However, only the Promotion of Rational antibiotics use behavior among healthcare personnel in health care setting is not the root cause problem solving because it should also be implemented in the public sector.
This paper highlights the reports on the research that explores the significant predictors of rational use of antibiotics behavior among community people. To our knowledge, very few studies have been conducted in Thailand. Since using antibiotics without necessity was detected in most of the hospitals, healthcare facilities, community, and drugstores, as well as in some cases, self-medication by the individuals.23 Identification of factors associated with rational antibiotic use behavior is crucial to generate effective interventional and policies including strategies for controlling unnecessary use of antibiotics in the communities which designed for changing behavior of the public sector towards better and more reasonable way of using antibiotics.
Materials and Methods
Study Area and Sampling
This research was conducted by using the data-source from “Rational Use of Antibiotics (RUA) Survey Project”24 which was performed with the cross-sectional method to survey community members at Nakhon Nayok Province, which is one of the central provinces that locates in northeast of Bangkok and the executive board of medical facilities and related organization give importance to Rational Drug Use (RDU) service plan national policy and need to publicize the implementation to the public sector.
Nakhon Nayok Province is divided into four main districts; Mueang Nakhon Nayok, Pak Phli, Ban Na and Ongkharak. Required sample size was calculated by using the formula as 20 numbers of subjects per one independent variable according to the rule of thumb.25 As from the literature, expert opinions and theoretical framework of 11 explanatory factors were contained in this study included gender, age, education, occupation, prevalence of antibiotics use, knowledge, attitude towards antibiotics use, pattern of antibiotics use and intention, antibiotics accessible sources, antibiotics usage information attainment channels and usage of herbal medicines, 220 participants were required. However, in order to reduce incomplete information by insufficient data and subjects’ withdrawal during the data collection process, sample size was further increased by 15%. Therefore, 254 samples were recruited which were the people living in Nakhon Nayok Province who were not mentally ill, agreed to participate in the study and used to take antibiotics with the aged between 13 and 78 years that were chosen by applying Quota sampling method from the proportion of general population in each setting which covered all four districts of Nakhon Nayok Province. This proportion was taken from proportional comparison with 10% of total patients who went to OPD per week in each of the three government hospitals (Banna Hospital, Ongkharak Hospital and Pak Phli Hospital) and it also included patients from Health Promoting Hospitals, Primary and Secondary school teachers, community members and those who worked in government or private establishments.
Research Instruments
Structured questionnaires were developed from RUA survey project by adapting standard structured questionnaires of the previous studies and literature reviews, moreover, to ensure the face validity of research instruments, before the pilot study were conducted, all questions were reviewed by the eminent persons which were the RDU/ RUA specialist physicians.
The knowledge part reliability coefficient of the questionnaires was calculated using Kuder-Richardson 21 formula (KR21) and the value was 0.73. As for the reliability of attitude towards antibiotics use section and self-care when having 3 main diseases, the internal consistency of related items was recorded using Cronbach’s Alpha coefficient of 0.81.
The questionnaires comprised 7 main sections: Sociodemographic characteristics of the respondents (Q1-Q7), Prevalence of antibiotic use (Q8-Q10), Knowledge (Q11-Q22), Attitude (Q23-Q39), Antibiotic accessibility sources/ Antibiotic usage information attainment channels/ Usage of herbal medicines (Q40-Q46), Pattern of antibiotic use intention (Q47-Q76) and Antibiotic use behavior (Q77-Q79). Questions related to the Knowledge were further divided into two categories that were “Knowledge about the causes of diseases (Q11-Q13) and “Knowledge about antibiotic use (Q14-Q22)”. Before the interview took place, the researcher showed respondents the pictures of some commonly used antibiotics and asked them “What type of the drugs in these pictures?” to ensure their understandings about the type of drug. After they answered the question, we replied them the correct answer and informed them to call those drugs as “Antibiotics or Disinfectants”, then the interview was started.
Data Management and Analysis
Statistical Package for Social Science (SPSS) version 26 was used for data coding, management and analysis. Descriptive statistics was performed to compute mean, median, standard deviation, inter quartile range, frequency and percentage which were used to describe sociodemographic characteristics, responses to knowledge, attitude questions and distribution of rational antibiotic use. Responses to knowledge items were divided into two groups: “Yes” and “No” and final result was determined by using the mean of total correct score as a cut point for organizing into two groups: “Inadequate knowledge (score of 0–5)” and “Adequate knowledge (score of 6–12)”. For the attitude section, five-point Likert scale was used to classify the responses into 5 groups: “Totally disagree”, “Disagree”, “Not sure”, “Agree” and “Totally agree”. “Criterion reference at 70” was used to measure the attitude of respondents as follows: those scoring higher than 70% of total score were had “Appropriate attitude (score of 60–85)” and those scoring lower than 70% were had “Inappropriate attitude (score of 0–59)”. Behavior of antibiotic use was assessed by 3 questions and for this research, respondents who had 2–3 correct answers were identified as “Rational behavior” and those who had no or one correct answers were identified as “Irrational behavior”.
Chi-square test was performed to examine the association between explanatory factors and rational behavior of antibiotic use of the respondents. Finally, Multiple Logistic Regression (MLR) was applied to identify the predictors of rational behavior of antibiotic use by adjusting the confounding factors.
Rational Use of Antibiotics (RUA) survey was approved by the Ethical Review Committee for Research in Human Subject, Nakhon Nayok Provincial Public Health Office with certificate number NPHO 2019–0010. In case of the participants were under the legal age of majority in Thailand, they were approved by the ethics committees to give information by providing informed consent on behalf of their own or obtained from their parents. And this research was also conducted under the approval of Ethical Committee of Mahidol University with certificate number 2020/027.1910.
Results
Characteristics of Respondents
Study population consisted of 254 respondents, of which nearly three quarters (72.4%) were female and about half of them were married. The mean age was 41.94 years (SD =15.78). Young (13–34years) and middle aged individuals (35–56years) were the majority of the respondents (80.3%). Most of them had educational level under or completed the secondary school (40.2%), followed by those achieving higher education such as completed Bachelor or Master’s degree (33.4%). Nearly one-third of them (31.5%) were recorded as private employees. The respondents who had household income less than 20,000 Baht were 72.8%. Regarding types of health insurance schemes, nearly half of them had enrolled into Universal Coverage Scheme (UCS) as shown in Table 1.
Table 1.
Socio-Economic Characteristics of Respondents
| Sociodemographic Characteristics | Frequency (n) | Percent (%) |
|---|---|---|
| Gender | ||
| Female | 184 | 72.4 |
| Male | 70 | 27.6 |
| Age | ||
| 13–34 years | 108 | 42.5 |
| 35–56 years | 96 | 37.8 |
| 57–78 years | 50 | 19.7 |
| Mean (SD) = 41.94 (15.78), Min = 13, Max = 78 | ||
| Marital Status | ||
| Single | 92 | 36.2 |
| Married | 128 | 50.4 |
| Widow/ Divorced/ Separated | 34 | 13.4 |
| Educational Status | ||
| Under and completed Secondary School | 102 | 40.2 |
| Moderate Level (Vocational Certificate, Diploma) | 67 | 26.4 |
| Completed Bachelor or Master Degree or higher | 85 | 33.4 |
| Occupation | ||
| Private Employee | 80 | 31.5 |
| Civil Servant/ Government Employee | 72 | 28.3 |
| Other (Farmer, Merchant/ Self Employed and others) | 102 | 40.2 |
| Monthly Household Income | ||
| 300–8000 Baht | 80 | 31.5 |
| 8001–20,000 Baht | 105 | 41.3 |
| 20,001–100,000 Baht | 69 | 27.2 |
| Median (IQR) = 15,000 (9516, 20,000), Min = 300, Max = 100,000 |
Prevalence of Antibiotic Use Among the Respondents
The individuals who used any types of antibiotics during the last 3 months and the last 3–6 months were 30.7% and 31.5% respectively. Most of them (59.8%) reported that they were already took antibiotics within the last one year (Table 2).
Table 2.
Prevalence of Antibiotic Use
| Prevalence of ATB Use | Number | Percent (%) |
|---|---|---|
| ATB use within last 3 months | ||
| Not use | 176 | 69.3 |
| Used | 78 | 30.7 |
| ATB use within last 3–6 months | ||
| Not use | 174 | 68.5 |
| Used | 80 | 31.5 |
| ATB use within last 1 year | ||
| Not use | 102 | 40.2 |
| Used | 152 | 59.8 |
Knowledge, Attitude, Behavior in Respect to Antibiotic Use
Over half of the respondents (54.3%) had inadequate knowledge about antibiotic use and causes of the main diseases. Likewise, most of them (68.9%) had inappropriate attitude related to antibiotic use and self-care when they had three main diseases. However, about half of them (51.2%) showed rational behavior towards antibiotic use in this research.
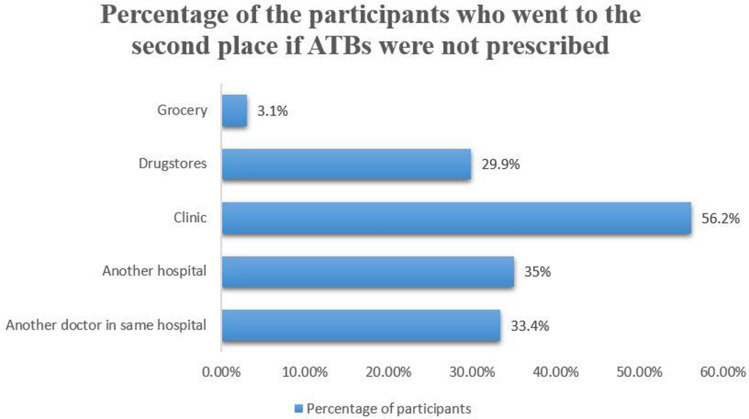
Antibiotic Access Sources/Antibiotic Usage Information Attainment Channels
Most respondents reported that their main sources of antibiotic (52.4%) attainment were hospitals and health promoting hospitals (HPH), followed by drugstore and grocery (35.4%). The majority (55.5%) firstly went to the hospitals and HPH when they felt sick and wanted to take antibiotics. Almost all of them (98.0%) replied that they would search for antibiotics when they were not prescribed antibiotics at the first place they visited and 56.2% chose ‘clinics’ as the second place to get antibiotics as depicted in Figure 1. Over 80% of the respondents searched for related information about antibiotic use from different channels, the majority (63.4%) searched for information from the physician or healthcare professionals at the hospitals.
Figure 1.
Percentage of the participants who went to the second place if ATBs were not prescribed at the first place.
Pattern of Antibiotics Use Intention
Table 3 presents the pattern of antibiotics use intention. About three-quarters of the respondents admitted that they went to the hospital or HPH and drugstore when they had three main diseases. While less than half of them (41.4%) intended to take antibiotics when they visited drugstore, only few proportion were willing to use antibiotics when they visited the hospital or HPH (16.4%) and clinic (13.0%). In terms of antibiotic prescription, most respondents reported they was prescribed or dispensed antibiotics when they visited clinics (76.7%) and drugstores (70.7%).
Table 3.
Pattern of Antibiotic Use Intention
| Pattern of Antibiotic Use Intention | Frequency (n) | Percent (%) |
|---|---|---|
| Participants who visited Hospital/ HPH | ||
| Not intended to use ATBs | 158 | 83.6 |
| Intended to use ATBs | 31 | 16.4 |
| Participants who visited Clinic | ||
| Not intended to use ATBs | 127 | 87.0 |
| Intended to use ATBs | 19 | 13.0 |
| Participants who visited Drugstore | ||
| Not intended to use ATBs | 110 | 58.6 |
| Intended to use ATBs | 78 | 41.4 |
| ATB prescription by Hospital/ HPH | ||
| Not prescribed | 88 | 46.6 |
| Prescribed | 101 | 53.4 |
| ATB prescription by Clinic | ||
| Not prescribed | 34 | 23.3 |
| Prescribed | 112 | 76.7 |
| ATB dispensing by Drugstore | ||
| Not dispensed | 55 | 29.3 |
| Dispensed | 133 | 70.7 |
Factors Related to Rational Behavior of Antibiotic Use
When performing MLR analysis, Enter method was firstly used for independent factors like Knowledge and Attitude because they are important variables that used to determine antibiotic use behavior. Forward Likelihood (LR) method was then performed as the best fit model for other variables to identify the predictors of rational behavior of antibiotic use. In MLR analysis by adjusting confounding factors, “Knowledge” and “Attitude” were significantly associated with antibiotic use behaviour, with the suggestion that respondents with sufficient knowledge and appropriate attitude were more likely to practice rational behavior. Both “Prevalence of antibiotic use within last 3 months” and “Visiting drugstore” were also found to be significant factors, with the respondents who did not use any kinds of antibiotics during last 3 months and visit drugstore if they had 3 main diseases, tended to show better practices than their counterparts. On the issue of age groups, the respondents between the ages of 35–56 had more rational use of antibiotics behavior than those with aged between 13 and 34 while older adults (57–78 years) were significantly associated with irrational behavior of antibiotics use comparing with the participants who were less than 34 years of age. For these results, age groups was related to rational drug use as concluded in Table 4.
Table 4.
Predictive Factors Associated with Rational Use of Antibiotics Using Multiple Logistic Regression (n=254)
| Variables | AORa | 95% CI | p-valueb |
|---|---|---|---|
| Age Groups | |||
| 13–34 years | 1 | ||
| 35–56 years | 1.62 | (0.88–2.98) | 0.124 |
| 57–78 years | 0.38 | (0.17–0.85) | 0.018* |
| ATB use (last 3 months) | |||
| Used | 1 | ||
| Not used | 1.89 | (1.04–3.43) | 0.037* |
| Knowledge of participants | |||
| Inadequate | 1 | ||
| Adequate | 3.37 | (1.92–5.90) | 0.0001*** |
| Attitude of participants | |||
| Inappropriate | 1 | ||
| Appropriate | 2.90 | (1.54–5.43) | 0.001** |
| Visiting Drugstore | |||
| Visited | 1 | ||
| Not Visit | 2.04 | (1.06–3.92) | 0.033* |
| Intention to use ATBs when visiting Hospital/ HPH | |||
| Intended | 1 | ||
| Not Intended | 2.412 | (0.978–5.947) | 0.056 |
Notes: aAdjusted for all variables in the table, b*p-value<0.05, **p-value<0.01, ***p-value<0.001.
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval.
Discussion
This was one of the few studies in Thailand that were conducted to explore the characteristics of rational use of antibiotics and to identify factors associated with rational behavior among community members.
In our research, the prevalence of respondents having rational behavior of antibiotics use was 51.2%, a significantly lower percentage than these of studies in United Kingdom (90%),26 Namibia (80%),27 Hong Kong (78.5%) and Sydney (76.2%).4 Relatively similar percentage was detected in one of previous studies with 55% of respondents in Spain showing appropriate behavior of such use.26 However, our finding was slightly higher than that of previous study in Taiwan where 47.2% of respondents expressed responsible behavior towards using antibiotics.28 Various results could be explained by the differences in levels of health literacy of general population in regard to antibiotics use and self-care, cultural norms in terms of views and trust to healthcare providers, and standard criteria to define rational antibiotics use.
Among socio-economic characteristics, only age and education level of respondents were found to be significantly associated with behavior of antibiotics use. Respondents with higher educational status were more likely to have better practices towards antibiotics use, a finding that supported previous studies in Nepal, Sydney and Hong Kong3,4 but contrasting with French study that postulated appropriate behavior of using antibiotics were more frequently observed in subjects with low educational level.2 We recorded younger age groups to practice more rational antibiotics use than old individuals, a similar observation to that of Egyptian study,1 Serbia study and contrary result to those found in studies of France, Sydney, Norway and Hong Kong where older respondents showed better practices.2,4 Moreover, one study from Turkey stated that young respondents with higher education are more likely to be irrational about using the antibiotics.29 In respect of extent of antibiotics use, we found about 60% of respondents reported to have used antibiotics within one year prior to surveying. This figure was lower than those of other comparative studies27,30–32 but quite higher than the results of studies in Bahir Dar, Lithuania9,33 and in Taiwan which showed 55% of patients who visited emergency department were on regular use of antibiotics.34 Socio-demographic factors like age, educational status, income level together with individuals’ knowledge and attitude about the aspect of antibiotics use, antibiotics prescribing patterns of responsible doctors, and degree to which one’s national policies can optimize antibiotics usage, can contribute to such wide variation in magnitude of antibiotics usage.
We observed that over half of respondents (54.3%) had insufficient level of knowledge about antibiotics use, a significant higher percentage than that of comparable Serbian study6 and Malaysian studies, in which half of the respondents lacked for the knowledge of antibiotics appropriate usage.35 Base on our study, knowledge was the most significant predictor for antibiotics use behavior, with the suggestion that respondents with adequate knowledge were more likely to show rational behavior, similar findings were found out in many previous studies.3,4,6,7,36 Apart from knowledge, attitude was recorded to be another reliable independent factor of antibiotics use behavior. Respondents with appropriate attitude tended to express more rational behavior than those having inappropriate attitude, the studies against this observation were found in Malaysia, Sydney and Hong Kong.4,35
One interesting finding stated that respondents who had sufficient knowledge were able to have more likelihood of showing positive attitude towards antibiotics use which was harmonious with other previous researches.7,36,37 Generally, having proper knowledge about health related topics can lead to positive attitude towards health seeking behavior which will produce better practice of health behavior.
Concerning sources of antibiotics accessibility among the respondents, most of them frequently visited healthcare facilities when they wanted to take antibiotics in case they got certain symptoms. The result was revealed that hospital and HPH were reported as the major sources if they have common medical illness, therefore, respondents in this study area were seemed to rely mostly on hospitals or HPH as their trusted health centres. Our finding revealed that almost all of the respondents were asked for antibiotics if they were not prescribed antibiotics at the first visit and most of them selected clinics as the second place for requesting antibiotics.
With respect to information channels for antibiotics usage, physicians or other healthcare providers were recorded as the most commonly information source for about 63% of respondents. Our observation was significantly higher than that of United Kingdom study which stated only 13% of subjects using this channels.26 However, the percentage of respondents in UK study acquiring information from the internet was found to be similar to our study. Such variation in different findings could be explained by cultural perspective of individuals towards certain health related behavior, which supported most Asian people are more likely to approach doctors or other healthcare professionals for finding out information about one’s health.
In this research, those respondents who visited local drugstores when they had symptoms of main diseases were less likely to show rational practices of antibiotics use than their counterparts. The suggestion of the possible reason is that those who were not visited drugstores might have better knowledge about self-limiting nature of these common diseases and better practice for taking care of their own health rather than using antibiotics. Although, most of them went to healthcare places such as hospitals, HPH and clinics when having main diseases, only small percentage had intention to request antibiotics, except for those who visited drugstores, indicating over one-third having such intention of antibiotics use. In accordance with this finding, local people showed certain degree of dependency on healthcare centres in spite of having self-limiting diseases for taking care of their own health rather than intention to use antibiotics.
In terms of antibiotics use in healthcare facilities, we observed that prescribing and dispensing antibiotics in clinics and drugstores were significantly higher than those of hospital or HPH. Several factors like non-compliance to antibiotics sales policy by suppliers, increased demand by the consumers in case of self-medication to treat some medical conditions and the lack of law enforcement regarding antibiotics use and sales might contribute to widespread antibiotics consumption at both clinics and community drugstores.
Conclusion
To our knowledge, it was one of very few studies in Thailand that were conducted to assess the extent of antibiotics use and to identify related factors of rational behavior of using antibiotics among general population. Since data source used in this research was collected in only one province as the provincial model, generalizability should be of concern when applying related findings to other areas. Further researches should be conducted by using a larger scale study to get more definitive findings. Based on the results of this study, it is important to encourage people to have the correct knowledge and appropriate attitudes about rational use of antibiotics. In addition, a nationwide study of the association between rational antibiotic use at different ages is recommended as a data base for policy interventions that promote antibiotic use at the different ages. Encouraging RDU in drugstore or RDU pharmacy, and public policy restriction with respect to antibiotics sales in drugstores is a challenge of optimise antibiotics consumption by the community people whenever they had common medical illnesses which helps to reduce irrational drug use in the community.
Acknowledgments
The authors would like to thank Health Systems Research Institute for promoting the research project. Moreover, the respondents who had been surveyed in RUA project as well as all health staffs from Nakhon Nayok Province are also acknowledged for supplying information of the survey.
Funding Statement
The Rational Use of Antibiotics (RUA) survey was funded by Health Systems Research Institute of Thailand. The funding source had no role in all processes of the study include study design, data collection, data analysis, data interpretation and manuscript writing. However, it plays key role in publication fee support.
Abbreviations
AD, Acute Diarrhea; AMR, Antimicrobial Resistance; AOR, Adjusted Odd Ratio; ATB, Antibiotics; FW, Fresh wound; HPH, Health Promoting Hospital; MLR, Multiple Logistic Regression; RDU, Rational Drug Use; RUA, Rational Use of Antibiotics; URI, Upper Respiratory Infection; WHO, World Health Organization.
Data Sharing Statement
The corresponding author can make the required data and material available whenever needed, upon reasonable request.
Ethics Approval and Inform Consent
Rational Use of Antibiotics (RUA) survey was approved by the Ethical Review Committee for Research in Human Subject, Nakhon Nayok Provincial Public Health Office with certificate of NPHO 2019-0010 and this research was also conducted under the approval of Ethical Committee of Mahidol University with certificate of 2020/027.1910. The Committee are in full compliance with International Guidelines of Human Research Protection such as Declaration of Helsinki, The Belmont Report, and CIOMS Guidelines and are independent of all the institutions involved and had no role in the design, conduct or reporting of the research. All the participants gave informed consent and verbal consent to the researchers before the interviews took place.
Disclosure
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.El Sherbiny NA, Ibrahim EH, Masoud M. Assessment of knowledge, attitude and behavior towards antibiotic use in primary health care patients in Fayoum Governorate, Egypt. Alexandria J Med. 2018;54(4):535–540. doi: 10.1016/j.ajme.2018.06.001 [DOI] [Google Scholar]
- 2.Demoré B, Mangin L, Tebano G, et al. Public knowledge and behaviors concerning antibiotic use and resistance in France: a cross-sectional survey. Infection. 2017;45(4):513–520. doi: 10.1007/s15010-017-1015-2 [DOI] [PubMed] [Google Scholar]
- 3.Nepal A, Hendrie D, Robinson S, et al. Knowledge, attitudes and practices relating to antibiotic use among community members of the Rupandehi District in Nepal. BMC Public Health. 2019;19(1):1558. doi: 10.1186/S12889-019-7924-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee SS, Yau B, Huang JQ. Determinants of appropriate antibiotic use in the community - a survey in Sydney and Hong Kong. Br J Infect Contr. 2008;9(6):6–9. doi: 10.1177/1469044607097219 [DOI] [Google Scholar]
- 5.Hadi U, Duerink DO, Lestari ES, et al. Survey of antibiotic use of individuals visiting public healthcare facilities in Indonesia. Int J Infect Dis. 2008;12(6):622–629. doi: 10.1016/j.ijid.2008.01.002 [DOI] [PubMed] [Google Scholar]
- 6.Horvat OJ, Tomas AD, Paut Kusturica MM, et al. Is the level of knowledge a predictor of rational antibiotic use in Serbia? PLoS One. 2017;12(7):e0180799. doi: 10.1371/journal.pone.0180799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim SS, Moon S, Kim EJ. Public Knowledge and Attitudes Regarding Antibiotic Use in South Korea. J Korean Acad Nurs. 2011;41(6):742–749. doi: 10.4040/jkan.2011.41.6.742 [DOI] [PubMed] [Google Scholar]
- 8.National Institute of Health. Causes of Antimicrobial (Drug) Resistance: national Institute of Allergy and Infectious Diseases 2011. Available from: https://www.niaid.nih.gov/research/antimicrobial-resistance-causes. Accessed August 23, 2020.
- 9.Gebeyehu E, Bantie L, Azage M. Inappropriate Use of Antibiotics and Its Associated Factors among Urban and Rural Communities of Bahir Dar City Administration, Northwest Ethiopia. PLoS One. 2015;10(9):e0138179. doi: 10.1371/journal.pone.0138179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organisation. The World Health Report 2007: A Safer Future: Global Public Health Security in the 21st Century: Overview. Geneva: World Health Organization; 2007. [Google Scholar]
- 11.Goossens H, Ferech M, Vander Stichele R, et al. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet. 2005;365(9459):579–587. doi: 10.1016/S0140-6736(05)17907-0 [DOI] [PubMed] [Google Scholar]
- 12.World Health Organisation. Antimicrobial resistance; 2020. Available from: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance. Accessed August 22, 2020.
- 13.Prestinaci F, Pezzotti P, Pantosti A. Antimicrobial resistance: a global multifaceted phenomenon. Pathog Glob Health. 2015;109(7):309–318. doi: 10.1179/2047773215Y.0000000030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organisation. New report calls for urgent action to avert antimicrobial resistance crisis 2019. Available from: https://www.who.int/news-room/detail/29-04-2019-new-report-calls-for-urgent-action-to-avert-antimicrobial-resistance-crisis. Accessed August 22, 2020.
- 15.Friedman EA Behind The Headlines: 10 million deaths from antimicrobial resistance by 2050 (or not?) 2020. Available from: https://oneill.law.georgetown.edu/behind-the-headlines-10-million-antimicrobial-deaths-by-2050-or-not/. Accessed August 22, 2020.
- 16.O’Neill J Review on Antimicrobial Resistance. Antimicrobial Resistance: Tackling a Crisis for the Health and Wealth of Nations. 2014.
- 17.Chereau F, Opatowski L, Tourdjman M, et al. Risk assessment for antibiotic resistance in South East Asia. BMJ. 2017;358:j3393. doi: 10.1136/bmj.j3393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organisation. Antimicrobial Resistance: Global Report on Surveillance. Geneva: World Health Organization; 2014. [Google Scholar]
- 19.Thamlikitkul V, Rattanaumpawan P, Boonyasiri A, et al. Thailand Antimicrobial Resistance Containment and Prevention Program. J Glob Antimicrob Resist. 2015;3(4):290–294. doi: 10.1016/j.jgar.2015.09.003 [DOI] [PubMed] [Google Scholar]
- 20.Sumpradit N, Chongtrakul P, Anuwong K, et al. Antibiotics Smart Use: a workable model for promoting the rational use of medicines in Thailand. Bull World Health Organ. 2012;90:905–913. doi: 10.2471/BLT.12.105445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zellweger RM, Carrique-Mas J, Limmathurotsakul D, et al. A current perspective on antimicrobial resistance in Southeast Asia. J Antimicrob Chemother. 2017;72(11):2963–2972. doi: 10.1093/jac/dkx260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chanvatik S, Kosiyaporn H, Lekagul A, et al. Knowledge and use of antibiotics in Thailand: a 2017 national household survey. PLoS One. 2019;14(8):e0220990. doi: 10.1371/journal.pone.022099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Suttajit S, Wagner AK, Tantipidoke R, et al. Patterns, appropriateness, and predictors of antimicrobial prescribing for adults with upper respiratory infections in urban slum communities of Bangkok. Southeast Asian J Trop Med Public Health. 2005;36(2):489–497. [PubMed] [Google Scholar]
- 24.Jayasvasti I, Urwannachotima N, Teekasap P. System Dynamics Analysis of Factors Affect Rational Use of Antibiotics Behavior in Public Sector Provincial Level Model: A Case Study of Nakhon Nayok Province, Thailand (RUA Survey Project). Health System Research Institute; 2019. [Google Scholar]
- 25.Hair JF, Black WC, Babin BJ, et al. Multivariate Data Analysis. 6th. New Jersey: Pearson University Press;2006. [Google Scholar]
- 26.Pechère JC. Patients’ interviews and misuse of antibiotics. Clin Infect Dis. 2001;33(Suppl 3):S170–3. doi: 10.1086/321844 [DOI] [PubMed] [Google Scholar]
- 27.Pereko DD, Lubbe MS, Essack SY. Public knowledge, attitudes and behavior towards antibiotic usage in Windhoek, Namibia. S Afr J Infect Dis. 2015;30(4):134–137. doi: 10.1080/23120053.2015.1107290 [DOI] [Google Scholar]
- 28.Chen C, Chen YM, Hwang KL, et al. Behavior, attitudes and knowledge about antibiotic usage among residents of Changhua, Taiwan. J Microbiol Immunol Infect. 2005;38(1):53–59. [PubMed] [Google Scholar]
- 29.Tengilimoğlu D, Tekin PŞ, Zekioğlu A, et al. Consumer Awareness, Attitude, and Behavior Related to the Rational Use of Medicines in a Developing Country Context: the Case of Turkey. Open Access Maced J Med Sci. 2020;8(E):162–171. [Google Scholar]
- 30.Jifar A, Ayele Y. Assessment of Knowledge, Attitude, and Practice toward Antibiotic Use among Harar City and Its Surrounding Community, Eastern Ethiopia. Interdiscip Perspect Infect Dis. 2018;2018:8492740. doi: 10.1155/2018/8492740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Awad AI, Aboud EA. Knowledge, attitude and practice towards antibiotic use among the public in Kuwait. PLoS One. 2015;10(2):e0117910–e. doi: 10.1371/journal.pone.0117910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aljayyousi GF, Abdel-Rahman ME, El- Heneidy A, et al. Public practices on antibiotic use: a cross-sectional study among Qatar University students and their family members. PLoS One. 2019;14(11):e0225499. doi: 10.1371/journal.pone.0225499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pavydė E, Veikutis V, Mačiulienė A, et al. Public Knowledge, Beliefs and Behavior on Antibiotic Use and Self-Medication in Lithuania. Int J Environ Res Public Health. 2015;12(6):7002–7016. doi: 10.3390/ijerph120607002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu Y-C, Huang W-K, Huang T-S, et al. Extent of antibiotic use in Taiwan shown by antimicrobial activity in urine. Lancet. 1999;354(9187):1360. [DOI] [PubMed] [Google Scholar]
- 35.Shakeel S, Hayat F, Mehsud S, Khan AH, Iqbal MS, Khan J. Students’ knowledge and attitude towards rational use of antibiotics. Med Sci. 2020;24(106):4499–4509. [Google Scholar]
- 36.Anderson A. Online health information and public knowledge, attitudes, and behaviors regarding antibiotics in the UK: multiple regression analysis of Wellcome Monitor and Eurobarometer Data. PLoS One. 2018;13(10):e0204878. doi: 10.1371/journal.pone.0204878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vallin M, Polyzoi M, Marrone G. Knowledge and Attitudes towards Antibiotic Use and Resistance - A Latent Class Analysis of a Swedish Population-Based Sample. PLoS One. 2016;11(4):e0152160. doi: 10.1371/journal.pone.0152160 [DOI] [PMC free article] [PubMed] [Google Scholar]