Highlights
-
•
First detailed analysis of overseas development aid (ODA) for the health of IDPs.
-
•
Reports low and declining health ODA for IDPs.
-
•
Indicates major inequity in health ODA for IDPs compared to refugees.
-
•
Negligible ODA for IDPs was for non-communicable diseases and mental health.
-
•
Health ODA for IDPs did not appear to be related to IDP health needs.
Keywords: Internally displaced persons, Refugees, Aid, Official development assistance
Abbreviations: CRS, creditor reporting system; DAC, development assistance committee; GAVI, global alliance for vaccines and immunization; IDP, internally displaced person; LMIC, low- and middle-income country; NCD, non-communicable diseases; ODA, official development assistance; OCED, organisation of economic cooperation and development; STD, sexually transmitted disease; UN, United Nations; USD, US dollar
Abstract
Background
There are an estimated 55 million internally displaced persons (IDPs) globally. IDPs commonly have worse health outcomes than host populations and other forcibly displaced populations such as refugees. Official development assistance (ODA) is a major source of the global financial response for health in low- and middle-income countries (LMICs), including for populations affected by armed conflict and forced displacement. Analysis of ODA supports efforts to improve donor accountability, transparency and the equitable use of ODA. The aim of this study is to examine international donor support and responsiveness to IDP health needs through analysis of ODA disbursements to LMICs between 2010 and 2019.
Methods
ODA disbursement data to LMICs from 2010 to 2019 were extracted from the Creditor Reporting System (CRS) database and analysed with Stata software using a combination of: (i) text searching for IDP and refugee related terms; and (ii) relevant health and humanitarian CRS purpose codes. Descriptive analysis was used to examine patterns of ODA disbursement, and nonlinear least squared regression analysis was used to examine responsiveness of ODA disbursement to recipient country IDP population size and health system capacity and health characteristics.
Findings
The study highlighted declining per IDP capita health ODA from USD 5.34 in 2010 to USD 3.72 in 2019 (with annual average decline of -38% from the 2010 baseline). In contrast, health ODA for refugees in LMICs increased from USD 18.55 in 2010 to USD 23.31 in 2019 (with an annual average increase of +14%). Certain health topics for IDPs received very low ODA, with only 0.44% of IDP health ODA disbursed for non-communicable diseases (including mental health). There was also weak evidence of IDP health ODA being related to recipient country IDP population size, and health system capacity and health characteristics. The paper highlights the need for increased investment by donors in IDP health ODA and to ensure that it is responsive to their health needs.
Introduction
There are estimated to be 55 million internally displaced persons (IDPs) globally (IDMC, 2022). These include 48 million people displaced by armed conflict and violence (in 59 countries and territories) and 7 million people displaced by disasters (in 103 countries and territories). Virtually all (99.5%) conflict/violence-driven IDPs are based in low- and middle-income countries (LMICs) (IDMC, 2021; UNHCR, 2021). Compared with resident populations and other forcibly displaced populations such as refugees, these IDPs typically experience higher rates of mortality, communicable diseases, non-communicable diseases (NCDs) and mental disorders (Greene-Cramer et al., 2020; Heudtlass et al., 2016; Lam et al., 2015; Porter and Haslam, 2005; Villamizar-Pena et al., 2021). Explanations for these worse health outcomes include exposure to higher levels of violence, poverty, worse living conditions, and reduced access to health services (World Bank, 2017; Cantor and Apollo, 2020; Cantor and Wooley, 2020; Cantor et al., 2021; Ekezie et al., 2020). One factor underpinning these differentials is that, unlike refugees, IDPs do not generally benefit from an agreed international legal status and nor do they have an international agency dedicated specifically to protecting and assisting them (Hakamies et al., 2008; Rae, 2011) (although there are now some regional treaties on IDP protection and assistance and diffuse responsibilities for different aspects of the IDP response are allocated through the humanitarian ‘cluster’ system (Cantor, 2018)). IDPs therefore depend principally on the government of their own country, which may have contributed to their forced displacement. In addition, IDPs are often in countries with low GDP and lower proportion of GDP spent on health. It is also argued that the international community is less interested in IDP than refugee situations, resulting in less assistance to IDPs (Cantor et al., 2021).
Official development assistance (ODA) is a major source of global financial assistance for health in LMICs, including for populations affected by armed conflict and forced displacement. ODA is defined as flows of official financing administered with the promotion of the economic development and welfare of developing countries as the main objective, (OECD, 2022) and it is inclusive of humanitarian assistance. ODA includes disbursements by all major bilateral government donors and multilateral agencies, global health initiatives (e.g. the Global Alliance for Vaccines and Immunization (GAVI)) and key philanthropic institutions (e.g. The Bill and Melinda Gates Foundation and the Wellcome Trust) (OECD, 2022). These ODA disbursements may be to recipient country governments, regional initiatives, non-governmental organisations and UN agencies. Analysis of ODA provides insight into levels of commitment by international development funders (including humanitarian funding) for specific topics (e.g., health topics) or populations (e.g., IDPs). It is also useful in understanding how equitable and responsive development and humanitarian assistance is to population needs, and for efforts to improve donor accountability and transparency (Esser and Bench, 2011; Kharas, 2011). The need to strengthen health financing for internal displacement was raised by the United Nations (UN) Secretary-General's High-Level Panel on Internal Displacement1 and subsequent draft ‘Action Agenda on Internal Displacement’ by the UN Secretary-General (UN, 2021; United Nations Secretary-General's High-Level Panel on Internal Displacement, 2021). To the best of our knowledge, there has been no analysis of patterns of health-related ODA explicitly for IDPs.
The aim of this study is to examine donor support and responsiveness to IDP health needs through analysis of ODA disbursements to LMICs between 2010 and 2019. The specific objectives are to: (i) describe the patterns of disbursement of health ODA explicitly to IDPs, including comparisons with refugees; (ii) describe the key health topics receiving health ODA to IDPs; and (iii) examine responsiveness of health ODA to IDPs in relation to host country health system capacity and health characteristics. It is hoped that such information can help strengthen appropriate and equitable investment of ODA for the health of IDPs.
Materials and methods
Data source
ODA data were used from the open access Creditor Reporting System (CRS) database, available at http://stats.oecd.org/Index.aspx?datasetcode=CRS1. CRS is maintained by the Development Assistance Committee (DAC) of the Organisation of Economic Cooperation and Development (OECD). CRS data were determined to be the most comprehensive source of information on ODA for health. CRS data have been widely used for research on tracking financial assistance across different health sectors to LMICs, including those affected by conflict, forced displacement and humanitarian crises (Patel et al., 2011; Patel et al., 2009; Pitt et al., 2010). The number of donors reporting to the CRS increasing greatly from the 15 rich-country bilateral members and five development banks of the OECD's DAC reporting in 1973 to over 50 bilateral, 35 multilateral, and private donors reporting by 2017 (Pitt et al., 2018). The reporting by OECD/DAC members is mandatory and it uses standardised methods to avoid double-counting and data are validated by a peer-review process. (OECD, 2022) Data included in alternative humanitarian aid databases such as OCHA's Financial Tracking System database are also included in CRS, but these alternative aid databases are less comprehensive than CRS and so were not included in our analysis (Grepin et al., 2012; OECD, 2022; Patel et al., 2011).
Data extraction
All ODA from 2010 to 2019 were downloaded from CRS into Stata (at the time of submission the 2021 CRS data were not available, and the 2020 CRS data were very incomplete and so were excluded). The ODA dataset consisted of 2,442,571 ODA entries. For identifying ODA entries for the populations of interest to the study, the CRS variable ‘long description’ was searched for any ODA entries for words related to IDPs and refugees. ODA searchers were made in English, French, Spanish and Italian. All other donors report their ODA submissions to CRS in English. The Stata search function of ‘regexm’ was used to search CRS entries for the following terms: IDP; internally displaced; Internally Displaced; personne déplacée; Personne Déplacée; desplazado interno; Desplazado Interno; sfollato interno; Sfollato Intern. For comparisons with refugees, we also searched entries for: refugee; Refugee; réfugié; Réfugié; refugiado; Refugiado; profugo; Profugo. We did not include the CRS ‘purpose code’ for ‘refugees and asylum seekers in donor countries’ as the focus of our study was ODA and population displacement in LMICs given that 99% of conflict/violence-driven IDPs live in LMICs (as do over 86% of refugees and asylum seekers (UNHCR, 2021)) and so including this purpose code would have inflated the ODA disbursed for refugees overall.
For identifying health-related ODA (disbursed USD in constant USD), relevant CRS ‘purpose codes’ for health were selected. We also added a percentage of ODA reported under relevant CRS humanitarian purpose codes to our estimates as some of the humanitarian ODA is applied to health issues. This percentage allocated for health was assumed to be 8%, based on previous studies (Patel et al., 2011; Patel et al., 2009; Patel et al., 2016). We included this proportion of humanitarian ODA as without doing so would have risked under-estimating the amount of ODA allocated for IDP health. The purpose codes used for our analysis are shown in Box 1 (and a fuller description of the purpose codes is given in Online Appendix A).
Box 1.
Description of CRS purpose codes used for analysis.
| CRS Purpose code | Purpose code description |
|---|---|
| Health ODA | |
| Health, General: | |
| 12110 | Health policy and administrative management |
| 12181 | Medical education/training |
| 12182 | Medical research |
| 12191 | Medical services |
| Basic Health: | |
| 12220 | Basic health care |
| 12230 | Basic health infrastructure |
| 12240 | Basic nutrition |
| 12250 | Infectious disease control |
| 12261 | Health education |
| 12262 | Malaria control |
| 12263 | Tuberculosis control |
| 12281 | Health personnel development |
| Non-communicable diseases (NCDs): | |
| 12310 | NCDs control, general |
| 12320 | Tobacco use control |
| 12330 | Control of harmful use of alcohol and drugs |
| 12340 | Promotion of mental health and well-being |
| 12350 | Other prevention and treatment of NCDs |
| 12382 | Research for prevention and control of NCDs |
| Population Policies/Programmes & Reproductive Health: | |
| 13010 | Population policy and administrative management |
| 13020 | Reproductive health care |
| 13030 | Family planning |
| 13040 | STD control including HIV/AIDS |
| 13081 | Personnel development for population and reproductive health |
| Humanitarian ODA (8% allocated to health): | |
| 72010 | Material relief assistance and services |
| 72050 | Relief co-ordination and support services |
| 73010 | Immediate post-emergency reconstruction and rehabilitation |
| Budget support (sensitivity analysis only) | |
| 51010 | General budget support-related aid |
Note: See Online Appendix A for detailed descriptions of purpose codes.
Data analysis
The analysis was conducted in Stata v.16. It combined the searches for IDPs (and separately refugees) with the health-related and humanitarian ODA purpose codes to examine the disbursement of relevant health ODA explicitly to IDPs (and to refugees). Data are presented as either total average annual ODA (USD millions) over the study period of 2010–2019 or average annual per capita ODA for IDPs over the study period. Data used to support the descriptive analysis included number of IDPs (conflict-affected IDPs and also disaster displacement IDPs) Al-Mahaidi, 2021, number of refugees (UNHCR, 2021), and total country populations (World Bank 2022e).
For the investigation into the responsiveness of IDP health ODA to recipient country needs, we hypothesised that higher disbursement of health ODA for IDPs would be associated with higher numbers of IDPs in recipient countries. We also hypothesised that higher disbursement of health ODA for IDPs would be associated with weaker national health system capacity (e.g., financial capacity) and/or worse national health characteristics (e.g., health outcomes) in recipient countries. To test this, we conducted a regression analysis with the top 25 IDP generating countries (which account for 95% of all IDPs globally). The dependent variable was total health ODA for IDPs (USD millions). The independent variables were total IDPs per country UNHCR, 2021, national per capita GDP (World Bank, 2022d), national government domestic health expenditure (World Bank 2022e), national universal health coverage index score (Hogan et al., 2018; WHO, 2022), national-level life expectancy (World Bank 2022c), national-level maternal mortality ratio (World Bank, 2022b), and the national-level infant mortality rate (World Bank 2022a). These were all averaged over the ten year study period for each of the 25 countries (the country data can be found in Online Appendix B). These independent variables were chosen as they are commonly used indicators of health systems capacity and health needs. ore More direct indicators related to IDP health (e.g., IDP mortality rates, health expenditure on IDPs) would have been preferable but they were not available for IDP populations in all the study countries throughout the study period. The associations were examined through nonlinear least squared regression analysis as there were nonlinear relationships between IDP health ODA disbursements and the selected independent variables.
A separate sensitivity analysis was also conducted to include a proportion of all health ODA disbursed to the top 25 IDP generating countries as going towards IDPs (i.e., without being described as specifically for IDPs by the donor in CRS). The sensitivity analysis was done separately to the main analysis as the additional ODA does not reflect explicit donor funding for IDPs but may indicate the broader range of health ODA that could theoretically benefit IDPs. For this sensitivity analysis, we added two categories of funding. First, a proportion of all health ODA (i.e., that did not mention IDPs) as going to IDPs, based on the percentage of IDPs within each country population (see Online Appendix B). Second, we calculated 8% of the ODA in the CRS ‘general budget support’ purpose code as being used for health (as done with previous studies (Patel et al., 2011,2009,2016)), and then of this 8%, we allocated a proportion based on the percentage of IDPs within that country population (see Online Appendix B).. The amounts from the two categories were then combined and added to the IDP-explicit ODA reported in the main study.
No ethics approval was required as all data used are in the public domain.
Results
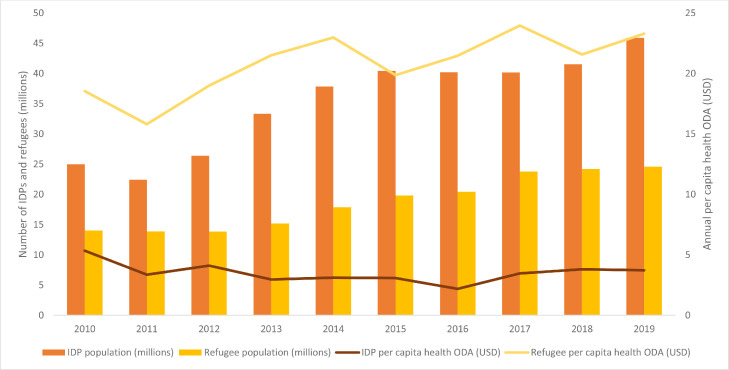
The total health ODA disbursed explicitly for all IDPs globally during 2010–2019 was USD 1213.1429 million (i.e., USD 1.2 billion). The average per capita ODA disbursed for all IDPs globally during 2010–2019 was USD 3.51 per IDP capita. This changed from USD 5.34 in 2010 to USD 3.72 in 2019, fluctuating from a low of USD 2.18 in 2016 to a high of USD 5.34 in 2010 (Fig. 1). The average annual percentage change during the study period compared with the 2010 baseline was -38%. In contrast, the average refugee health ODA disbursed for refugees during 2010 to 2019 was USD 21.20 per refugee capita. This increased from USD 18.55 in 2010 to USD 23.31 in 2019 (Fig. 1), with an average annual percentage change compared with the 2010 baseline of +14%. Further details are available in Online Appendix C.
Fig. 1.
Health ODA (USD per capita) explicitly for IDPs and refugees and their absolute numbers (millions), 2010–2019.
The main funders for health ODA specifically mentioning IDPs were the Global Fund (USD 382.0018 million – specifically for HIV/AIDS, malaria, and tuberculosis), Germany (USD 248.4816 million), the United States (USD 126.0215 million), Canada (USD 92.7318 million), and the European Union (USD 66.5148 million). The top ten health ODA funders for IDPs accounted for 92% of all disbursements (further details on their total ODA disbursements for IDPs are in Online Appendix D). The average amount disbursed (all funders) per ODA contribution specifically for IDPs was USD 0.1001 million. Some key donor agencies disbursing very low health ODA for IDPs included: GAVI (no entries reported), the Bill and Melinda Gates Foundation (USD 0.6985 million), the Central Emergency Response Fund (USD 1.2719 million), and the World Bank (USD 17.4977 million). Regional funds and development banks in Latin America, the Arab region, and Africa reported no health ODA disbursements for IDPs.
The disbursement of ODA for IDP health for different health topics is shown in Table 1. Most funds (50.44%) came from the 8% allocation that we assumed may be used towards health from the CRS humanitarian purpose codes (for entries which explicitly referred to IDPs). Of the explicit health purpose code allocations, most went to ‘basic health’ (26.05%) – particularly to malaria control (10.45%), general basic health care (6.39%) and tuberculosis control (4.77%). The purpose code for population and reproductive health programmes received 21.8% – the vast majority for HIV/AIDS and STD control (17.09%). In contrast, only 0.44% of ODA for health of IDPs was for NCDs (including mental health). There was considerable variation between IDPs and refugees in the pattern of disbursement to the different ODA health topics. Most notably, for refugees, a much greater amount (78.49%) came from the eight percent allocation of humanitarian ODA (which explicitly referred to refugees). IDPs also received a greater proportion related to HIV, malaria, and tuberculosis control (due to the funding from the Global Fund noted above).
Table 1.
Allocation of total health ODA (USD millions) explicitly for IDPs and refugees, by activity description, 2010–2019.
|
IDPs |
Refugees |
|||
|---|---|---|---|---|
| Millions (USD) | % | Millions (USD) | % | |
| Health ODA | ||||
| Health, General: | ||||
| Health policy and administrative management | 1.5734 | 0.13 | 76.7597 | 1.93 |
| Medical education/training | 0.7527 | 0.06 | 1.4870 | 0.04 |
| Medical research | 0.0547 | 0.00 | 2.7145 | 0.07 |
| Medical services | 12.9919 | 1.07 | 56.3923 | 1.40 |
| Basic Health: | ||||
| Basic health care | 77.5367 | 6.39 | 135.4366 | 3.34 |
| Basic health infrastructure | 33.8716 | 2.79 | 38.9521 | 0.96 |
| Basic nutrition | 12.5424 | 1.03 | 93.2303 | 2.31 |
| Infectious disease control | 4.7244 | 0.39 | 24.8169 | 0.63 |
| Health education | 1.3537 | 0.11 | 5.6132 | 0.14 |
| Malaria control | 126.7266 | 10.45 | 55.5041 | 1.40 |
| Tuberculosis control | 57.8133 | 4.77 | 71.2592 | 1.80 |
| Health personnel development | 1.4009 | 0.12 | 2.3619 | 0.06 |
| Non-communicable diseases (NCDs): | ||||
| NCDs control, general | 0.0000 | 0.00 | 0.0177 | 0.00 |
| Tobacco use control | 0.0000 | 0.00 | 0.0000 | 0.00 |
| Control of harmful use of alcohol and drugs | 4.8543 | 0.40 | 4.8543 | 0.12 |
| Promotion of mental health and well-being | 0.4582 | 0.04 | 1.3605 | 0.03 |
| Other prevention and treatment of NCDs | 0.0000 | 0.00 | 0.9424 | 0.02 |
| Research for prevention and control of NCDs | 0.0000 | 0.00 | 0.0000 | 0.00 |
| Population Policies/Programmes & Reproductive Health: | ||||
| Population policy and administrative management | 3.4478 | 0.28 | 47.6424 | 1.20 |
| Reproductive health care | 32.5882 | 2.69 | 37.6043 | 0.89 |
| Family planning | 21.1678 | 1.74 | 38.5063 | 0.97 |
| STD control including HIV/AIDS | 207.3249 | 17.09 | 159.5195 | 4.03 |
| Personnel development for population & reproductive health | 0.0031 | 0.00 | 0.5468 | 0.01 |
| Humanitarian ODA (8% allocated to health) | ||||
| Material relief assistance and services | 393.1720 | 32.41 | 2774.4330 | 69.92 |
| Relief co-ordination and support services | 150.7827 | 12.43 | 256.4505 | 6.45 |
| Immediate post-emergency reconstruction & rehabilitation | 68.0018 | 5.61 | 90.8920 | 2.29 |
| Total | 1213.1430 | 100.00 | 3977.2975 | 100.00 |
Note: See Online Appendix A for detailed descriptions of purpose codes.
The amount of health ODA explicitly for IDPs that was dispersed to the top 25 IDP generating countries is given in Table 2 (with country background data provided in Online Appendix B). The countries receiving the highest average annual per IDP capita health ODA disbursements were Central African Republic (6.07 USD), Iraq (6.05 USD), Georgia (USD 5.85), Somalia (USD 4.46), and Azerbaijan (USD 3.56). Those receiving the least were Afghanistan (zero), Guatemala (USD 0.14), Turkey (USD 0.16), Côte d'Ivoire (USD 0.34), Bangladesh (USD 0.56) and Colombia (USD 0.56). The top 25 IDP generating countries accounted for over 95% of all IDPs globally but received 60% of all the health ODA disbursed to IDPs. There were a number of countries with significantly lower numbers of IDPs during the study period but which received comparatively very high amounts of health ODA for IDPs, most notably: Uganda (USD 162.5335 million disbursed during study period, = USD 378.63 per IDP capita); Eritrea (USD 54.20801 million disbursed = USD 101.89 per IDP capita); Philippines (USD 41.5966 million disbursed = USD 24.53 per IDP capita); Angola (USD 29.5861 million disbursed = USD 68.92 per IDP capita); Cambodia (USD 27.2785 million disbursed = USD 36.94 per IDP capita), and Bosnia (USD 26.6874 million disbursed = USD 25.87 per IDP capita). The remaining IDP health ODA was disbursed either to regional IDP initiatives, ‘unspecified’ bilateral donations, or to other countries (i.e., outside of the top 25 IDP-generating countries).
Table 2.
Health ODA explicitly for IDPs and related data for the top-25 IDP generating countries, 2010–2019.
| Average number of IDPs | IDPs as % of national population | Total health ODA explicitly mentioning IDPs (USD millions) | Average annual per IDP capita health ODA explicitly mentioning IDPs (USD) | |
|---|---|---|---|---|
| Afghanistan | 1,353,200 | 4.01 | 0.0000 | 0.00 |
| Azerbaijan | 598,810 | 6.26 | 21.2898 | 3.56 |
| Bangladesh | 435,500 | 0.28 | 2.4437 | 0.56 |
| Cameroon | 224,500 | 0.97 | 4.4017 | 1.96 |
| Centr. African Repub. | 468,400 | 10.36 | 28.4097 | 6.07 |
| Colombia | 5,903,960 | 12.43 | 33.0489 | 0.56 |
| Côte d'Ivoire | 245,540 | 1.07 | 0.8302 | 0.34 |
| Dem. Rep. Congo | 2,880,200 | 3.83 | 37.6450 | 1.31 |
| Ethiopia | 744,000 | 0.75 | 19.4595 | 2.62 |
| Georgia | 257,700 | 6.90 | 15.0840 | 5.85 |
| Guatemala | 172,630 | 1.12 | 0.2494 | 0.14 |
| India | 743,300 | 0.06 | 12.0148 | 1.62 |
| Iraq | 2,536,630 | 7.30 | 153.3940 | 6.05 |
| Kenya | 245,240 | 0.52 | 7.6741 | 3.13 |
| Myanmar | 545,400 | 1.04 | 16.5109 | 3.03 |
| Nigeria | 1,507,500 | 0.84 | 21.8064 | 1.45 |
| Pakistan | 769,700 | 0.39 | 20.5336 | 2.67 |
| Palestine (West Bank and Gaza Strip) | 201,200 | 4.43 | 6.9042 | 3.43 |
| Somalia | 1,496,760 | 10.95 | 66.8008 | 4.46 |
| South Sudan | 1,184,800 | 11.30 | 38.4747 | 3.25 |
| Sudan | 2,855,900 | 7.41 | 23.7802 | 0.83 |
| Syria | 5,045,990 | 26.88 | 135.8468 | 2.69 |
| Turkey | 1,027,910 | 1.32 | 1.6260 | 0.16 |
| Ukraine | 630,900 | 1.40 | 24.9347 | 3.95 |
| Yemen | 1,417,240 | 5.42 | 39.4216 | 2.78 |
Notes: See Online Appendix B for full country demographic and economic data and data sources.
Using regression analysis, we examined whether the health ODA disbursed for IDPs to the top 25 IDP generating countries showed any association with recipient country IDP population size and health capacity and health characteristics. The findings (Table 3) from the ordinary least squared regression analysis showed mixed findings in relation to the hypothesis. There were significant (P < 0.05) associations between higher ODA disbursements for IDP health and higher IDP population size (Coef. 0.09), higher maternal mortality ratio (Coef. 0.11), and higher infant mortality rates (Coef. 0.11). Conversely, higher national per capita GDP (Coef. 0.10), higher national government health expenditure (Coef. 0.10), and a higher universal health coverage index score (Coef. 0.12) were associated with higher IDP health ODA (i.e., against the hypothesis). However, it should be noted that all the coefficients are small and the overall strength of the models was also very weak (with adjust. R2 ranging from 0.0222 to 0.0224).
Table 3.
Regression analysis on association of IDP population size and measures of national health system capacity and health characteristics with outcome of health ODA explicitly for IDPs disbursed to top 25 IDP generating countries, 2010–2019.
| Coef. | Std. Err. | [95% Conf. Interval] | P | Adj. R2 | ||
|---|---|---|---|---|---|---|
| IDP population size | 0.09 | 0.01 | [0.07; | 0.10] | <0.01 | 0.02 |
| National per capita GDP | 0.10 | 0.01 | [0.08; | 0.13] | <0.01 | 0.02 |
| National government health expenditure | 0.10 | 0.01 | [0.08; | 0.13] | <0.01 | 0.02 |
| Universal health coverage indicator | 0.12 | 0.03 | [0.05; | 0.18] | <0.01 | 0.02 |
| National life expectancy | 0.06 | 0.05 | [-0.03; | 0.15] | 0.19 | 0.02 |
| Maternal mortality ratio | 0.11 | 0.01 | [0.09; | 0.14] | <0.01 | 0.02 |
| Infant mortality ratio | 0.11 | 0.00 | [0.08; | 0.14] | <0.01 | 0.02 |
Notes: Nonlinear least squared regression analysis used due to nonlinear relationships. Dependent variable is total health ODA for IDPs (USD millions). See Online Appendix B for list of top 25 IDP generating countries and their associated data (with sources) for independent variables.
As noted above, we conducted a sensitivity analysis that included a proportion of all health ODA disbursed to the top 25 IDP generating countries as going towards IDPs (i.e., without being described as specifically for IDPs by the donor in CRS). The additional ODA included in the sensitivity analysis does not reflect donor funding explicitly for IDPs, but it may indicate the broader range of health ODA that could theoretically benefit IDPs. Without the additional ODA from the sensitivity analysis, the average annual health ODA per IDP capita to the top 25 IDP generating countries was USD 2.19. With the additional ODA in the sensitivity analysis, this increased to USD 7.46 per IDP capita. The detailed results are shown in Online Appendix E.
Discussion
To the best of our knowledge this is the first study examining the disbursement of health ODA for IDPs. It highlights how health ODA for IDPs has decreased between 2010 and 2019 on a per capita basis. This contrasts with refugees for whom health ODA has increased over the same period. In addition, refugees are receiving over six times more health ODA per capita than IDPs. This is despite commonly higher health needs among IDPs compared to refugees (Greene-Cramer et al., 2020; Heudtlass et al., 2016; Lam et al., 2015; Porter and Haslam, 2005; Villamizar-Pena et al., 2021).
It is unlikely that the difference in health ODA between IDPs and refugees could be attributable to refugees possibly being located in more ‘costly’ countries than IDPs and thus requiring more resources to sustain them at the same level, as our analysis focused only on LMICs and the regression analysis also indicated no meaningful association between ODA disbursements and national GDP. There are several other more likely explanations for the lower levels of health ODA for IDPs than refugees. The first is that IDPs are more likely than refugees to be implicitly included in health services funded through host country domestic financing as IDPs are citizens of that country and so automatically entitled to the benefits of citizenship of that country, including access to national health services (UN, 1998). However, it should be recognised that even where such implicit inclusion exists, in some countries IDPs have documentation restrictions which limits access to health, even when they are citizens of that country.
A second possible explanation for the lower levels of health ODA for IDPs as compared to refugees is that IDPs may also benefit more from ODA not explicitly named for them in CRS. For example, by donors shifting towards more generalised allocations to countries with large IDP populations rather than IDP-specific allocations, such as through pooled funding arrangements as used in Afghanistan, South Sudan, Democratic Republic of Congo, and Somalia (Ayeni et al., 2021; Newbrander et al., 2014; The Ministry of Health and Human Service at the Federal Government of Somalia, 2020; USAID, 2022). This would accord with the initiative to increasingly try to roll the IDP response into more general national development initiatives (although the same argument could also apply to some refugee responses). However, even after adjusting for this in the sensitivity analysis (where we assumed additional ODA unspecified for IDPs may still benefit IDPs), there was still a significant difference in per capita health ODA between IDPs and refugees. In addition, evidence that IDP health outcomes are typically worse than host and refugee communities supports arguments that highlight a lack of investment in IDP health (Cantor et al., 2021; Heudtlass et al., 2016). More in-depth research is particularly required at the national level to examine the disbursement of health ODA and domestic health financing for IDPs. Additionally, it should be noted that the results in this paper only represent disbursements by donors, rather than expenditure. An analysis of national health accounts, which would help track actual ODA expenditure at the country level to get a more comprehensive picture of how ODA is spent for IDPs, along with alternative non-ODA funding sources for IDP health (and what the contextual influences are on that expenditure over time) (Price et al., 2016).
An alternative explanation for the large difference in IDP and refugee health ODA is that IDPs are under-prioritized by national and international policy-makers and donors (Al-Mahaidi, 2021; Cantor et al., 2021). This reflects the historic relative neglect of IDPs in contrast to refugees who benefit from a well-established framework of international legal protection and the existence of a specific UN agency with a mandate for refugee protection (i.e. UNHCR) (Hakamies et al., 2008; Rae, 2011). While there have been improvements over the past two decades in the international recognition of IDPs, particularly through the formulation of the UN Guiding Principles on Internal Displacement and through regional mechanisms (Cantor and Apollo, 2020; UNHCR, 2020),and in efforts to better coordinate the IDP response through the humanitarian cluster system and New Way of Working (UN, 2022), our findings suggest there remain major gaps in proportional international financing to support the health of IDPs. Policy analysis is required at global, regional and national levels to help explain decision-making in relation to the patterns of health resource allocation for IDPs. It should be noted that overall ODA (i.e. ODA for all sectors and populations) has been trending downwards during the study period, (IDA, 2020) but this does not explain the increase in ODA for refugees. It could be speculated that the increase in refugee health ODA during the study period may have come at the expense of IDP health ODA which declined during the same period (Beytrison, 2018). For example, the large increase in ODA in response to the Syria refugee crisis may have reduced ODA for IDPs in Syria (and potentially elsewhere).
The study also reported on the disbursement of funding to different health topics. Three key findings emerged from this. Firstly, the proportionately large amount of ODA for HIV/AIDS and malaria (and to a lesser extent tuberculosis), which came almost entirely from the Global Fund. The increased funding and engagement by the Global Fund with IDPs is to be welcomed (Spiegel et al., 2010; The Global Fund, 2022). The second key finding was the extremely low amount of ODA disbursed for NCDs (including mental health) to IDPs (and also refugees). This is despite the high burden of mental disorders among conflict-affected populations (and particularly among IDPs) (Charlson et al., 2019; Porter and Haslam, 2005), and the increasing burden of NCDs such as diabetes and cardiovascular disease among conflict-affected populations (Kehlenbrink et al., 2019; Naja et al., 2019). It should be noted that ODA for NCDs and mental health may be covered through other CRS purpose codes (e.g. ‘basic health care’), but it nevertheless appears a major funding shortfall. The very limited ODA for NCDs among IDPs highlights belated donor recognition of the burden of NCDs among conflict-affected and forcibly displaced populations which may be partly attributable to insufficient epidemiological data, limited evidence on costs and models of NCD care, and concerns about costs and complexity of NCD care for forcibly displaced persons (Jaung et al., 2021; Jobanputra et al., 2016; Spiegel et al., 2014). The implications are that the treatment gap for mental health and psychosocial support will remain extremely large among IDPs (and refugees) (Roberts et al., 2019); and that IDPs (and refugees) will not be able to receive essential life-saving medicines and treatment for NCDs (Jobanputra et al., 2016; Kehlenbrink et al., 2019). The third main finding was that half of the ODA we recorded for IDPs came from the proportion (8%) from the CRS humanitarian purpose codes that we assumed a priori may be for health (i.e. it was not explicitly for health). This creates some uncertainty about the true amount disbursed for IDP health and detailed in-country examination is important to understand the degree to which ODA is being used to support IDP health. It also suggests more specific humanitarian-related CRS purpose codes would be valuable in strengthening understanding and transparency in ODA reporting for humanitarian activities.
Country IDP population sizes seemed to have limited bearing on the amounts of ODA disbursed. For example, was no health ODA being disbursed to Afghanistan despite it having an average of 1,353,200 IDPs during the study period. There has certainly been significant donor investment for health in Afghanistan (Bertone et al., 2019), and the lack of health ODA specifically for IDPs may be due to donors preferring to use pooled funding approaches in Afghanistan, including multi-donor trust funds, which are intended for the whole population rather than specific groups such as IDPs (Frost et al., 2016; Newbrander et al., 2014). Nevertheless this raises concern about how well the specific health needs of IDPs are identified and addressed in Afghanistan (Médecins sans Frontières, 2014) .Other countries to which very limited health ODA was disbursed for IDPs included Turkey and Colombia but this may be due to their greater levels of national wealth and capacity to provide health care to IDPs. However, studies indicate commonly worse health outcomes in Colombia among IDPs than resident populations (Castañeda-Hernández et al., 2018; Lagos-Gallego et al., 2017; Rodriguez-Morales et al., 2018), while evidence on the health of IDPs in Turkey appears very limited. Conversely, health ODA disbursed for IDPs was comparatively very high in several countries with relatively low numbers of IDPs during the study period (e.g., Uganda, Eritrea, Philippines, Angola, Cambodia, and Bosnia). This is potentially attributable to these ODA disbursements being used to support the health of former IDPs (given some of these countries had historically high numbers of IDPs). However, this does not necessarily explain disbursements to countries such as the Philippines and Eritrea which did not have historically high numbers of IDPs. The lack of responsiveness of ODA to IDP needs was suggested in the regression analysis, which indicated mixed and statistically weak associations between disbursements of health ODA for IDPs and numbers of IDPs and health system and health characteristics.
There is a need for more equitable health ODA for IDPs. Rather than re-distributing funds from refugees towards IDPs, there is a need to increase overall funding to help meet the substantial health needs of IDPs. The UN's 2021 High-level Panel on Internal Displacement report noted the need to harness international financing, including establishing a Global Fund for Solutions to Internal Displacement (United Nations Secretary-General's High-Level Panel on Internal Displacement, 2021). In addition to rights-based justifications, there are also economic arguments for greater attention paid to IDPs given that the global economic cost of internal displacement is estimated to amount to USD 20.5 billion (and this is still considered a significant underestimate), investment in IDPs, including their health, is likely to be economically advantageous (Heggenes and Bilak, 2021; United Nations Secretary-General's High-Level Panel on Internal Displacement, 2021). It is important that international donor agencies such as the World Bank (and regional development banks and funds) review their approach to IDPs as these entities have not contributed significantly to health ODA for IDPs. Notably, the World Bank has engaged more recently on the issue of internal displacement and greater investment in the health of IDPs would be timely (World Bank, 2021). Development actors have expressed interest in incorporating internal displacement into existing financing to ensure that IDPs benefit from general development assistance, rather than launching specific interventions for IDPs, but the UN High-level Panel on Internal Displacement has argued for specific, complementary measures for IDPs to avoid IDPs becoming “mainstreamed into oblivion” (United Nations Secretary-General's High-Level Panel on Internal Displacement, 2021).
ODA also needs to be more responsive to country IDP health needs, for which we require a better understanding of the severity and diversity of those health needs. Such responsiveness is one of the steps needed to address key international donor commitments such as the Paris Declaration on Aid Effectiveness and the High-Level Forums on Aid Effectiveness. ODA investment in IDP health should also be predictable and avoid aid fragmentation and the associated added burden to recipient national governments and humanitarian agencies. This includes addressing the dominance of smaller and short-term humanitarian ODA (particularly given the mean amount disbursed per ODA contribution specifically for health and IDPs was only USD 0.1001 million). This dominance of smaller ODA disbursements risks impeding national governments and other key actors in developing the long-term strategies and programmes required to respond to the needs of IDPs in a sustainable manner (Cantor et al., 2021; Heudtlass et al., 2016).
Finally, it is important to recognise that ODA is not a panacea – it is only one source of country-level funds and one that should complement, rather than substitute, host country investment for IDP health. It is critical that national governments dedicate resources to supporting solutions to internal displacement and avoid aid dependency (Farag et al., 2009; Kenny, 2006; United Nations Secretary-General's High-Level Panel on Internal Displacement, 2021). Innovative financing mechanisms for IDPs could also support such initiatives (UNHCR, 2020). This should be accompanied by strategies to support national IDP health policies to help ensure the strategic and effective use of IDP health financing (Al-Mahaidi, 2021). Such efforts to support adequate financing for IDP health are essential if global and national commitments to achieving universal health coverage are to be reached.
Strengths and limitations
The main strengths of this study are that, to the best of our knowledge, it provides the first in-depth, systematic analysis of ODA disbursements for the health of IDPs. Indeed, we are not aware of any equivalent analysis for IDPs for other sectors. It provides important empirical evidence of inequity in aid funding for IDPs generally, and specifically for certain health topics such as NCDs and mental health. It also suggests a lack of responsiveness in health ODA for IDPs in relation to country IDP population sizes and health system capacity and health characteristics. The findings can support advocacy and policy initiatives to strengthen more equitable and appropriate responses for IDP health.
The main limitation of this study is that the text searching of the CRS dataset may have excluded ODA entries which could have been for IDPs but did not explicitly use our search terms or refer to IDPs. This limitation risks under-estimating the true amount of health ODA for IDPs (although the same limitation could apply to refugees too). Conversely, using text searching of the CRS dataset risks capturing text entries coincidentally using the same terms but not actually related to IDPs. This would result in an over-reporting of health ODA for IDPs. We could not manually search all the relevant entries as they numbered in the thousands. However, we consider the likelihood of accidentally capturing such entries as very low. Another limitation was that we included an assumed proportion (8%) of the ODA reported in the relevant CRS humanitarian purpose codes (and which explicitly referred to IDPs) that could potentially have been used for health activities. Over half of the IDP ODA we recorded came from this source (i.e., rather than being explicitly for health) and this creates a degree of uncertainty about the true amount ultimately disbursed for health for IDPs. Another limitation was that we did not analyse national health accounts for disbursements of domestic revenues by national governments to IDPs in their countries. These domestic revenues likely represent a significant source of health financing that could benefit IDPs, as do other forms of support such as through donations from private philanthropic donors that do not report to CRS, donations from the public, the diaspora, and other actors such as religious groups. Another limitation was that we could not examine the in-country expenditure of ODA and the degree to which it benefits IDP populations, and in-depth country research is recommended for this (Price et al., 2016). Finally, when examining the relationship between disbursements of health ODA for IDPs and health needs, we could only use proxy measures rather than more direct measures such as mortality as such data were not sufficiently available. It is strongly recommended that more epidemiological data are collected with IDPs to support more appropriate, equitable and responsive funding for IDP health.
Conclusions
The study highlights declining per capita amounts of health ODA for IDPs between 2010 and 2019. It also reveals substantially lower amounts of health ODA for IDPs as compared to refugees, despite typically worse health outcomes among IDPs. There were also major IDP ODA shortfalls for certain health topics, particularly NCDs and mental health. Disbursement of health ODA was also poorly correlated with IDP population size in that country and other proxy measures of need. The paper highlights the need for increased investment by donors in health ODA for IDPs, and the need to ensure that it is both responsive to health needs and supports national governments and other key stakeholders in developing long-term support to sustain improvements in the health and wellbeing of IDPs.
CRediT authorship contribution statement
Bayard Roberts: Visualization, Formal analysis, Writing – original draft. Winifred Ekezie: Writing – original draft. Kiran Jobanputra: Writing – original draft. James Smith: Writing – original draft. Sara Ellithy: Writing – original draft. David Cantor: Writing – original draft. Neha Singh: Writing – original draft. Preeti Patel: Visualization, Writing – original draft.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
This paper was supported by the RECAP project funded by the United Kingdom Research and Innovation as part of the Global Challenges Research Fund (ES/P010873/1).
Footnotes
The High-Level Panel on Internal Displacement was established by the UN Secretary-General in 2019 to identify concrete recommendations on how to better prevent, respond and achieve solutions to the global internal displacement crisis.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jmh.2022.100090.
Appendix. Supplementary materials
References
- Al-Mahaidi A. Financing opportunities for durable solutions to internal displacement: building on current thinking and practice. Refug. Surv. Q. 2021;39(4):481–493. [Google Scholar]
- Ayeni G.O., et al. Perception of basic package of health services’ impact on health service delivery and mortality among residents of Wulu County, South Sudan. J. Public Health. 2021;29(4):893–902. [Google Scholar]
- Bertone M.P., et al. Health financing in fragile and conflict-affected settings: what do we know, seven years on? Soc. Sci. Med. 2019;232:209–219. doi: 10.1016/j.socscimed.2019.04.019. [DOI] [PubMed] [Google Scholar]
- Beytrison, F. (2018).Funding for internally displaced persons, London: Christian Aid.
- Cantor D., et al. Understanding the health needs of internally displaced persons: a scoping review. J. Migr. Health. 2021;4 doi: 10.1016/j.jmh.2021.100071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantor D.J. The IDP in international law’? Developments, debates, prospects. Int. J. Refug. Law. 2018;30(2):191–217. [Google Scholar]
- Cantor D.J., Apollo J.O. Internal displacement, internal migration and refugee flows: connecting the dots. Refug. Surv. Q. 2020;39(4):647–664. [Google Scholar]
- Cantor, D.J., & Wooley, A. (2020).Internal displacement and responses at the global level: a review of the scholarship. Internal Displacement Research Programme Working Paper Series, 1: P. 1–2.
- Castañeda-Hernández D.M., et al. Comparative incidence of tuberculosis among internally displaced people of Colombia, 2009-2016. Int. J. Infect. Dis. 2018;73:345. [Google Scholar]
- Charlson F., et al. New WHO prevalence estimates of mental disorders in conflict settings: a systematic review and meta-analysis. Lancet. 2019;394(10194):240–248. doi: 10.1016/S0140-6736(19)30934-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekezie W., Adaji E.E., Murray R.L. Essential healthcare services provided to conflict-affected internally displaced populations in low and middle-income countries: a systematic review. Health Promot. Perspect. 2020;10(1):24–37. doi: 10.15171/hpp.2020.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esser D.E., Bench K.K. Does global health funding respond to recipients’ needs? Comparing public and private donors’ allocations in 2005–2007. World Dev. 2011;39(8):1271–1280. [Google Scholar]
- Farag M., et al. Does funding from donors displace government spending for health in developing countries? Health Aff. 2009;28(4):1045–1055. doi: 10.1377/hlthaff.28.4.1045. (Millwood) [DOI] [PubMed] [Google Scholar]
- Frost A., et al. An assessment of the barriers to accessing the basic package of health services (BPHS) in Afghanistan: was the BPHS a success? Glob. Health. 2016;12(1):71. doi: 10.1186/s12992-016-0212-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene-Cramer B., et al. Noncommunicable disease burden among conflict-affected adults in Ukraine: a cross-sectional study of prevalence, risk factors, and effect of conflict on severity of disease and access to care. PLoS One. 2020;15(4) doi: 10.1371/journal.pone.0231899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grepin K.A., et al. How to do (or not to do) ... tracking data on development assistance for health. Health Policy Plan. 2012;27(6):527–534. doi: 10.1093/heapol/czr076. [DOI] [PubMed] [Google Scholar]
- Hakamies N., Geissler P.W., Borchert M. Providing reproductive health care to internally displaced persons: Barriers experienced by humanitarian agencies. Reprod. Health Matters. 2008;16(31):33–43. doi: 10.1016/S0968-8080(08)31349-4. [DOI] [PubMed] [Google Scholar]
- Heggenes, P., & Bilak, A. (2021).Opinion: it's time for a global fund for displacement. 19 January 2022]; Available from: https://www.un.org/internal-displacement-panel/content/opinion-its-time-global-fund-displacement.
- Heudtlass P., Speybroeck N., Guha-Sapir D. Excess mortality in refugees, internally displaced persons and resident populations in complex humanitarian emergencies (1998-2012) - insights from operational data. Confl. Health. 2016;10:15. doi: 10.1186/s13031-016-0082-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogan D.R., et al. Monitoring universal health coverage within the sustainable development goals: development and baseline data for an index of essential health services. Lancet Glob. Health. 2018;6(2):e152–e168. doi: 10.1016/S2214-109X(17)30472-2. [DOI] [PubMed] [Google Scholar]
- IDA, Report from the executive directors of the international development association to the board of governors: IDA19: ten years to 2030: growth, people, resilience. (2020).,Washington D.C.: IDA.
- IDMC, Global report on internal displacement 2020. (2021). Geneva: Internal Displacement Monitoring Centre.
- IDMC. Global internal displacement database. (2022). Available from: https://www.internal-displacement.org/database/displacement-data.
- Jaung M.S., et al. Models of care for patients with hypertension and diabetes in humanitarian crises: a systematic review. Health Policy Plan. 2021;36(4):509–532. doi: 10.1093/heapol/czab007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jobanputra K., et al. Three steps to improve management of noncommunicable diseases in humanitarian crises. PLoS Med. 2016;13(11) doi: 10.1371/journal.pmed.1002180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kehlenbrink S., et al. The burden of diabetes and use of diabetes care in humanitarian crises in low-income and middle-income countries. Lancet Diabetes Endocrinol. 2019;7(8):638–647. doi: 10.1016/S2213-8587(19)30082-8. [DOI] [PubMed] [Google Scholar]
- Kenny C. World bank; Washington d.c: 2006. What is Effective Aid? How Would Donors Allocate it? [Google Scholar]
- Kharas H., Kharas H., Makino K., Jung W. Catalyzing Development. Brookings Institution Press; Washington, D.C: 2011. Transparency: changing the accountability engagement, and effectiveness of aid. [Google Scholar]
- Lagos-Gallego M., et al. Post-traumatic stress disorder in internally displaced people of Colombia: an ecological study. Travel Med. Infect. Dis. 2017;16:41–45. doi: 10.1016/j.tmaid.2017.02.008. [DOI] [PubMed] [Google Scholar]
- Lam E., McCarthy A., Brennan M. Vaccine-preventable diseases in humanitarian emergencies among refugee and internally-displaced populations. Hum. Vaccines Immunother. 2015;11(11):2627–2636. doi: 10.1080/21645515.2015.1096457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Médecins sans Frontières, Between rhetoric and reality: the ongoing struggle to access healthcare in Afghanistan. (2014)., MSF.
- Naja F., et al. Burden of non-communicable diseases among Syrian refugees: a scoping review. BMC Public Health. 2019;19(1):637. doi: 10.1186/s12889-019-6977-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newbrander W., et al. Afghanistan's basic package of health services: its development and effects on rebuilding the health system. Glob. Public Health. 2014;9(Suppl 1):S6–28. doi: 10.1080/17441692.2014.916735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OECD. Technical guide to terms and data in the creditor reporting system (CRS) aid activities database. (2022). 5 December 2013]; Available from: http://www.oecd.org/dac/stats/crsguide.htm.
- Patel P., et al. Tracking official development assistance for reproductive health in conflict-affected countries. PLoS Med. 2009;6(6) doi: 10.1371/journal.pmed.1000090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel P., et al. A review of global mechanisms for tracking official development assistance for health in countries affected by armed conflict. Health Policy. 2011;100(2-3):116–124. doi: 10.1016/j.healthpol.2010.08.007. [DOI] [PubMed] [Google Scholar]
- Patel P., et al. Tracking official development assistance for reproductive health in conflict-affected countries: 2002-2011. BJOG. 2016;123(10):1693–1704. doi: 10.1111/1471-0528.13851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitt C., et al. Countdown to 2015: assessment of official development assistance to maternal, newborn, and child health, 2003-08. Lancet. 2010;376(9751):1485–1496. doi: 10.1016/S0140-6736(10)61302-5. [DOI] [PubMed] [Google Scholar]
- Pitt C., et al. Tracking aid for global health goals: a systematic comparison of four approaches applied to reproductive, maternal, newborn, and child health. Lancet Glob. Health. 2018;6(8):e859–e874. doi: 10.1016/S2214-109X(18)30276-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter M., Haslam N. Predisplacement and postdisplacement factors associated with mental health of refugees and internally displaced persons: a meta-analysis. JAMA. 2005;294(5):602–612. doi: 10.1001/jama.294.5.602. [DOI] [PubMed] [Google Scholar]
- Price J.A., et al. How to do (or not to do) ... translation of national health accounts data to evidence for policy making in a low resourced setting. Health Policy Plan. 2016;31(4):472–481. doi: 10.1093/heapol/czv089. [DOI] [PubMed] [Google Scholar]
- Rae F. Border-controlled health inequality: the international community's neglect of internally displaced persons. Med. Confl. Surviv. 2011;27(1):33–41. doi: 10.1080/13623699.2011.562396. [DOI] [PubMed] [Google Scholar]
- Roberts B., et al. Mental health care utilisation among internally displaced persons in Ukraine: results from a nation-wide survey. Epidemiol. Psychiatr. Sci. 2019;28(1):100–111. doi: 10.1017/S2045796017000385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Morales A.J., et al. Differences in the incidence of malaria between internally displaced people and general population of Colombia from 2007 to 2016. Int. J. Infect. Dis. 2018;73:319–320. [Google Scholar]
- Spiegel P., Khalifa A., Mateen F.J. Cancer in refugees in Jordan and Syria between 2009 and 2012: challenges and the way forward in humanitarian emergencies. Lancet Oncol. 2014;15(7):e290–e297. doi: 10.1016/S1470-2045(14)70067-1. [DOI] [PubMed] [Google Scholar]
- Spiegel P.B., et al. Conflict-affected displaced persons need to benefit more from HIV and malaria national strategic plans and global fund grants. Confl. Health. 2010;4:2. doi: 10.1186/1752-1505-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OECD, Reporting directives for the creditor reporting system, OECD. (2022). 1 March 2022. http://www.oecd.org/dac/stats/1948102.pdf.
- The Global Fund. The global fund: key populations. (2022). [cited 2022 9 February 2022]; Available from: https://www.theglobalfund.org/en/key-populations/.
- The Ministry of Health and Human Service at the Federal Government of Somalia, The essential package of health services (EPHS) Somalia, 2020. (2020). The Ministry of Health and Human Service, the Federal Government of Somalia: Mogadishu.
- UN, Guiding principles on internal displacement, UN, (Ed.). (1998). Geneva: UN.
- UN, The United Nations secretary-general's action agenda on internal displacement. (2021).,Geneva: UN.
- UN. The new way of working. (2022). Available from: https://www.un.org/jsc/content/new-way-working.
- UNHCR, A review of innovative financing mechanisms for internally displaced persons. (2020).,Geneva: UNHCR.
- UN. United Nations Secretary-General's High-Level Panel on Internal Displacement, Shining a light on internal displacement a vision for the future: report of the United Nations secretary-general's high-level panel on internal displacement. (2021).,Geneva: United Nations. p. 90.
- USAID. Essential health services: the democratic republic of the congo. (2022). 1 March 2022]; Available from: https://www.hfgproject.org/essential-package-of-health-services-country-snapshot-the-democratic-republic-of-the-congo/.
- UNHCR . Global trends in forced displacement in 2020. UNHCR; Geneva: UNHCR: 2021. [Google Scholar]
- Villamizar-Pena R., et al. Leishmaniasis among internally displaced people of Colombia, 2007-2018 - a comparative analysis with the general population. Travel Med. Infect. Dis. 2021;41 doi: 10.1016/j.tmaid.2021.102043. [DOI] [PubMed] [Google Scholar]
- WHO. UHC service coverage index. (2022). [cited 2022 1 March 2022]; Available from: https://www.who.int/data/gho/data/indicators.
- World Bank . World Bank; Washington D.C: 2017. Forcibly Displaced: Toward a Development Approach Supporting Refugees, the Internally Displaced, and their Hosts. [Google Scholar]
- World Bank . World Bank; Washington D.C: 2021. A Development Approach to Conflict-Induced Internal Displacement. [Google Scholar]
- World Bank. Infant mortality rate. (2022a). 1 March 2022]; Available from: https://data.worldbank.org/indicator/SP.DYN.IMRT.IN.
- World Bank. Maternal mortality ratio. (2022b). 1 March 2022]; Available from: https://data.worldbank.org/indicator/SH.STA.MMRT.
- World Bank. Life expectancy at birth, total (years). (2022c). 18 January 2022]; Available from: https://data.worldbank.org/indicator/SP.DYN.LE00.IN.
- World Bank. GDP per capita (current USD dollars). (2022d). 18 January 2022]; Available from: https://data.worldbank.org/indicator/NY.GDP.PCAP.CD.
- World Bank. Population, total. (2022e). 18 January 2022]; Available from: https://data.worldbank.org/indicator/SP.POP.TOTL.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.