Abstract
Study Design:
Systematic review.
Objectives:
Synthesize previous studies evaluating clinical utility of preoperative Hb/Hct and HbA1c in patients undergoing common spinal procedures: anterior cervical discectomy and fusion (ACDF), posterior cervical fusion (PCF), posterior lumbar fusion (PLF), and lumbar decompression (LD).
Methods:
We queried PubMed, Embase, Cochrane Library, and Web of Science for literature on preoperative Hb/Hct and HbA1c and post-operative outcomes in adult patients undergoing ACDF, PCF, PLF, or LD surgeries.
Results:
Total of 4,307 publications were assessed. Twenty-one articles met inclusion criteria.
PCF and ACDF:
Decreased preoperative Hb/Hct were significant predictors of increased postoperative morbidity, including return to operating room, pulmonary complications, transfusions, and increased length of stay (LOS). For increased HbA1c, there was significant increase in risk of postoperative infection and cost of hospital stay.
PLF:
Decreased Hb/Hct was reported to be associated with increased risk of postoperative cardiac events, blood transfusion, and increased LOS. Elevated HbA1c was associated with increased risk of infection as well as higher visual analogue scores (VAS) and Oswestry disability index (ODI) scores.
LD:
LOS and total episode of care cost were increased in patients with preoperative HbA1c elevation.
Conclusion:
In adult patients undergoing spine surgery, preoperative Hb/Hct are clinically useful predictors for postoperative complications, transfusion rates, and LOS, and HbA1c is predictive for postoperative infection and functional outcomes. Using Hct values <35-38% and HbA1c >6.5%-6.9% for identifying patients at higher risk of postoperative complications is most supported by the literature. We recommend obtaining these labs as part of routine pre-operative risk stratification.
Level of Evidence:
III
Keywords: systematic review, spine surgery post-operative complications, hemoglobin, hematocrit, hemoglobin A1c
Introduction
Preoperative optimization is an important aspect of successful postoperative recovery in adult patients undergoing spinal surgery.1,2 In addition to baseline patient comorbidities,3-5 there is increasing evidence that abnormal preoperative lab values such as hemoglobin (Hb), hematocrit (Hct), Hemoglobin A1c (HbA1c), and electrolyte abnormalities are risk factors for poor post-operative outcomes.4,6
Hb is a polymeric protein found in red blood cells (RBCs) and is the primary mechanism of oxygen delivery to tissues. Normal lab values range from 14-18 g/dL for males and 12-16 g/dL for females and reflects the concentration of this protein in whole blood. 7 Hct is the percentage of the volume of red blood cells over total blood volume and is an indirect measure of oxygen carrying capacity. Normal Hct values range from 40 to 54% for males and 36 to 48% for females. 7 Low values of either parameter indicates anemia, which can be secondary to many etiologies including iron deficiency, chronic disease or malignancy, and vitamin B12 deficiency. 8 HbA1c is a measure of the percentage of glycated Hb and is associated with diabetes mellitus (DM), with values greater than 6.5% being diagnostic for DM. 9 Elevated HbA1c is associated with long-term DM complications and is an independent risk factor for stroke and heart disease. 9
To our knowledge, there are no comprehensive systematic reviews on the use of Hb/Hct or HbA1c in preoperative risk stratification for spinal surgery that synthesize the literature and provide an overview of the consensus recommendations. Our aim was to perform a systematic review on the utility of preoperative Hb/Hct and HbA1c for adult patients undergoing 4 common spinal procedures: anterior cervical discectomy and fusion (ACDF), posterior cervical fusion (PCF), posterior lumbar fusion (PLF), and lumbar decompression (LD).
Methods
Protocol
Our systematic review of the literature was constructed in accordance with Preferred Reporting Items and Meta-Analyses (PRISMA) guidelines and protocol. 10
Eligibility Criteria and Information and Search Strategy
Inclusion and exclusion criteria are demonstrated in Supplementary Table 1. Level of evidence of studies was assessed utilizing Oxford Centre for Evidence Based Medicine (OCEBM). 11 In consensus with the PRISMA guidelines, we conducted a systematic search of electronic databases (PubMed, Embase, the Cochrane Library, Web of Science) in August 2020 for all articles since 1990. Controlled vocabulary, such as Medical Subject Headings and Emtree terms were used in combination with keywords. The first group of terms include: hemoglobin(s)/haemoglobin(s), hematocrit, glycated hemoglobin, hemoglobin A1c protein, HB, Hba1c, or 1IC. The second group included: orthopedic procedures, spine surgery, spinal fusion, discectomy, laminectomy, discectomy, percutaneous, laminotomy, ACDF, spinal arthrodesis, spine arthrodesis, spinal arthrodesis, spine arthrodeses, spine surgery, spinal surgery, spinal surgeries, back surgery, or back surgeries. Results from the 2 categorizes of search words were combined to identify pertinent articles.
Study Selection
Two independent reviewers (K.S and K.W.) performed the initial screening of all studies based on article titles and abstracts. A third reviewer (B.Z.) served as an arbitrator when there was disagreement between the 2 primary reviewers.
Data Extraction and Data Items
The following data was extracted from each study utilizing a standardized data extraction form: title, authors, study design, study cohorts, type of spinal surgery, number of levels operated on, sample size, patient demographics, primary outcome measures, post-operative transfusion rates, mean length of stay (LOS), functional outcomes measures following surgery (visual analog scale (VAS), Japanese Orthopedic Association (JOA) scores, Oswestry Disability Index (ODI)), fusion rate, postoperative complications, and follow-up duration. Reported statistical differences for primary outcomes, including odds ratios and relative risks, were recorded for each included study.
Assessing Risk of Bias and Data Synthesis
2 independent reviewers determined level of evidence, sample size, data source/outcome assessors, and follow-up for each study utilizing a standardized assessment form (Supplementary Table 2). Both reviewers independently applied the qualitative Grading of Recommendations Assessment, Development, and Evaluation (GRADE) methodology to rate quality of included studies, and a third reviewer served as an arbitrator when there was disagreement between primary reviewers. To determine the risk of bias within the GRADE system, the Newcastle-Ottawa Scale (NOS) was utilized. 12 Included articles were separated based on independent variable (preoperative Hb/Hct or HbA1c) studied and by type of surgery performed.
Results
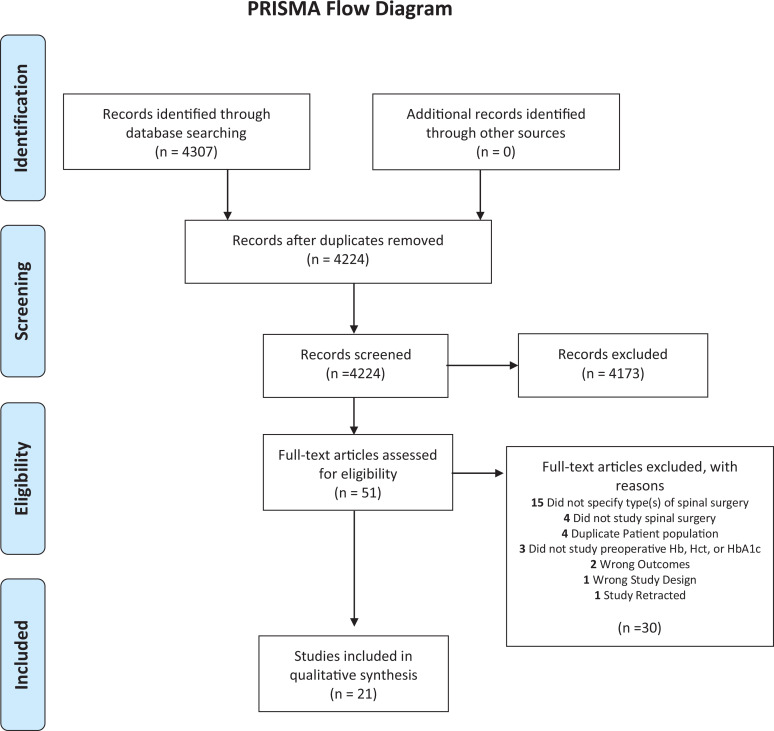
Of the 4307 articles originally identified, we identified 51 for full-text review. Ultimately, 21 articles were included in the systematic review ( Figure 1 ). Fifteen articles reported on the utility of preoperative Hb/Hct ( Table 1 ) and 6 articles reported on preoperative HbA1c as a predictor for postoperative outcomes in spine surgery ( Table 2 ). We did not identify any randomized controlled trials (RCTs), and all included articles were observational studies with level of evidence greater than 3. Twenty articles were retrospective cohort in design, and one was conducted prospectively.
Figure 1.
Literature search was performed using PubMed, Embase, the Cochrane library, and web of science databases in July 2020. The purpose was to determine the clinical utility of preoperative hemoglobin/hematocrit and HbA1c in patients undergoing ACDF, PCF, PLF, or LD.
Table 1.
Included Studies Evaluating Preoperative Hemoglobin or Hematocrit Levels and Postoperative Risk Following Spinal Surgery.
| First author, year | Design | OCEBM level of evidence | Sample size | Age | Surgery type | Levels of surgery |
|---|---|---|---|---|---|---|
| Cervical Procedures | ||||||
| Zreik 2020 | Retrospective | 3 | 47 111 | Median age: 54 | ACDF | One, Two, and Three levels |
| Phan 2017 | Retrospective | 3 | 3500 | NR | ACDF | Multi-level |
| Steinberger 2015 | Retrospective | 3 | 524 | NR | PCF | Multi-level |
| Phan 2017 | Retrospective | 3 | 473 | NR | PCF | Multi-level |
| Lumbar Procedures | ||||||
| Fosco 2012 | Retrospective | 3 | 40 | Mean: 53.6 | PLF LL |
Multi-level |
| Sanoufa 2015 | Retrospective | 3 | 317 | Mean: Anemic: 61.5 Non-anemic: 57.5 |
PLF | Multi-level |
| Basques 2015 | Retrospective | 3 | 4223 | Mean: 60.4 | PLF | Multi-level |
| Yew 2015 | Retrospective | 3 | 490 | Mean: 53.8 | PLF | Multi-level |
| Leu 2016 | Retrospective | 3 | 132 | Mean: 68.5 | PLF | Multi-level |
| Kaye 2018 | Retrospective | 3 | 50 495 | Mean: Cardiac risk: 66.75 Non-cardiac risk: 59.26 |
PLF | One-level |
| Ristagno 2018 | Retrospective | 3 | 6711 | Median age 66 | PLF | NR |
| Lakomkin 2018 | Retrospective | 3 | 6507 | Mean: 60 | PLF | One-level and Two-level |
| Basques 2014 | Retrospective | 3 | 2358 | Mean: 66.4 | LL | NR |
| Smith 2016 | Retrospective | 3 | 1033 | Mean: 50.6 | MIS-LF | Multi-level |
| Sachdeva 2020 | Retrospective | 3 | 81 | Mean: 62.8 | MIS-LF | Multi-level |
Abbreviations: ACDF, Anterior Cervical Discectomy and Fusion; PCF, Posterior cervical fusion; PLF, Posterior lumbar fusion; MIS-LF, Minimally invasive lumbar fusion; LL, Lumbar Laminectomy; NR, Not reported.
Table 2.
Included Studies Evaluating Preoperative Hemoglobin A1c Levels and Postoperative Risk Following Spinal Surgery.
| First author, year | Design | OCEBM level of evidence | Sample size | Mean age | Surgery | Levels of surgery |
|---|---|---|---|---|---|---|
| Cancienne, 2017 | Retrospective | 3 | 3,341 | NR | ACDF | NR |
| Walid, 2010 | Retrospective | 3 | 217 | No DM: 52, HbA1c: 58, DM: 60 | ACDF | NR |
| 118 | No DM: 60, HbA1c: 59, DM: 69 | LMD | NR | |||
| 107 | No DM: 55, HbA1c: 54, DM: 59 | LDF | NR | |||
| Cancienne, 2017 | Retrospective | 3 | 5,195 | NR | LD | One-level |
| Takahashi, 2013 | Retrospective | 3 | 165 | HbA1c<6.5% 68.6, >6.5% 70.9 | PLF | NR |
| Moazzeni, 2018 | Prospective | 2 | 96 | HbA1c<6.5% 56.1, >6.5% 59.5 | PLF | One-level |
| Hwang, 2019 | Retrospective | 3 | 92 | SSI group: 70 No SSI: 66.7 | PLF | One-level |
Abbreviations: ACDF, Anterior Cervical Discectomy and Fusion; PLF, Posterior lumbar fusion; LMD, Lumbar Microdiscectomy; LDF, Lumbar Decompression and Fusion; NR, Not reported.
Utility of Preoperative Hemoglobin or Hematocrit in Spinal Surgery
The cut-off value for low Hb/Hct was slightly different for each study and can be found in Table 3 .
Table 3.
Definitions of Anemia or Patient Hemoglobin/Hematocrit Criteria.
| First author, year (procedure) | Hb level | Hct level |
|---|---|---|
| Fosco 2012 (PLF, LL) | Only associations reported All patients included had Hb >11 |
NR |
| Basques 2014 (LL) | NR | Anemia defined as <36 |
| Sanoufa 2015 (PLF) | Low Hb defined as <13.5 | NR |
| Basques 2015 (PLF) | NR | Anemia is <36 |
| Steinberger 2015 (PCF) | NR | Only associations reported |
| Yew 2015 (PLF) | NR | Anemia defined as <35 |
| Leu 2016 (PLF) | Patient Hb divided into 4 groups: >14.85, 14.0-14.85, 13.0-14.0, <12.9 | NR |
| Smith 2016 (MIS-LF) | Only associations reported | NR |
| Phan 2017 (ACDF) | NR | Anemia defined as <39 male, <36 female |
| Phan 2017 (PCF) | NR | Anemia defined as <39 male, <36 female |
| Kaye 2018 (PLF) | NR | Absolute difference in Hct per point from 45 |
| Ristagno 2018 (PLF) | Only associations reported | Only associations reported |
| Lakomkin 2018 (PLF) | NR | Normal defined as 38-54 |
| Sachdeva 2020 (MIS-LF) | Low Hb defined as <12 | NR |
| Zreik 2020 (ACDF) | NR | Abnormal defined as <38 |
Abbreviations: Hb = Hemoglobin, Hct = Hematocrit, NR = Not reported in study, ACDF =Anterior Cervical Discectomy and Fusion, PLF =Posterior lumbar fusion, LL = Lumbar laminectomy, MIS-LF = Minimally invasive lumbar fusion.
ACDF
Two studies reported on association of preoperative Hct and adverse outcomes in multi-level ACDF procedures.4,13 Low preoperative Hct was associated with significantly increased risk of any complication (Table 4). Phan et al reported that reduced preoperative Hct was associated with increased rate of pulmonary complications and return to the operating room. Both studies reported on readmission rates within 30 days, although only Zreik et al found a significant increase in readmission following ACDF. Finally, Phan et al reported increased risk of LOS greater than 5 days in patients with reduced Hct prior to multi-level ACDF ( Table 5 ).
Table 4.
Included Studies Evaluating Preoperative Hemoglobin or Hematocrit Levels and Postoperative Risk of Complications or Transfusion Following Spinal Surgery.
| First author, year (procedure) | Complications | Transfusion |
|---|---|---|
| Cervical Procedures | ||
| Zreik 2020 (ACDF) | Any comp: 1.45,[1.26,1.67], p < .001* | NR |
| Serious comp: OR = 1.49,[1.28,1.74], p < .001* | NR | |
| Phan 2017 (ACDF) | Any comp: OR = 1.8, [1.1-2.8], p = .018* | OR = 5.9, [2,17], p = .001* |
| Pulm: OR = 3.3, [1.7-6.1], p = .0002* | NR | |
| Return OR: OR = 2.7, [1.6,4.7], p = .0004* | NR | |
| Steinberger 2015 (PCF) | NR | NR |
| Phan 2017 (PCF) | Any comp: OR = 3.14, p = .0008* | OR = 3.063, [1.502, 6.245], p = .0021* |
| Mortality: p = .9092 | NR | |
| Pulm: 9.75 [2.551,37.227], p = .0009* | NR | |
| ROR: OR = 2.87, [1.305,6.311], p = .0087* | NR | |
| Lumbar Procedures | ||
| Fosco 2012 (PLF, LL) | NR | Transfused: Hb 13.1 Not transfused: Hb 14.1, p = 0.023* |
| Sanoufa 2015 (PLF) | NR | NR |
| Basques 2015 (PLF) | NR | Relative Risk 2.0, p < .001* |
| Yew 2015 (PLF) | NR | OR = 4.37, p = .008* |
| Leu 2016 (PLF) | NR | NR |
| Kaye 2018 (PLF) | Cardiac risk: OR = 1.07,[1.04,1.1], p < .001* | NR |
| Ristagno 2018 (PLF) | NR | OR = 2.838,[2.108,3.820], p < .01* |
| Lakomkin 2018 (PLF) | Any comp: OR = 1.57,[1.26,1.95] | NR |
| Major comp: OR = 1.34, [1 -1.81] | ||
| Minor comp OR = 1.84, [1.41-2.41] | ||
| Basques 2014 (LL) | NR | NR |
| Smith 2016 (MIS-LF) | NR | NR |
| Sachdeva 2020 (MIS-LF) | NR | NR |
Abbreviations: ACDF: Anterior Cervical Discectomy and Fusion, PCF: Posterior cervical fusion, PLF: Posterior lumbar fusion, MIS-LF: Minimally invasive lumbar fusion, LL: Lumbar Laminectomy, NR: Not reported, OR: Odds Ratio, ROR: Return to Operating Room, Pulm: Pulmonary, Comp: complication. Bold*= Demonstrated statistical significance.
Definition for any complication for Zriek et al: Any complications included superficial SSI, ventilation for >48 hours, and stroke/cerebrovascular accident (CVA) in addition to serious complications.
Definition for serious complication for Zriek et al: Serious complications included cardiac arrest, myocardial infarction, pneumonia, progressive renal insufficiency, acute renal failure, pulmonary embolism, deep vein thrombosis, deep incisional surgical site infection (SSI), organ space SSI, systemic sepsis, unplanned intubation, urinary tract infection, and wound disruption.
Definition for any complication for Phan et al: Wound complication (superficial or deep surgical site infection, organ space infection, or wound dehiscence), pulmonary complication (pneumonia, unplanned reintubation, or duration of ventilator-assisted respiration ≥48 hours), renal complication (progressive renal insufficiency or acute renal failure), urinary tract infection, peripheral nerve injury, cardiac complication (cardiac arrest requiring cardiopulmonary resuscitation, or myocardial infarction), intra-/postoperative transfusion, sepsis, CNS complication (cerebrovascular accident or coma),
Definition for Lakomkin et al:
Major: postoperative deep wound infection, organ space infection, myocardial infarction, deep vein thrombosis, pulmonary embolism, sepsis, septic shock, CVA, peripheral nerve injury, coma, and death.
Minor: superficial wound infection, pneumonia, urinary tract infection, and wound dehiscence.
Total: all Major and Minor complications.
Table 5.
Included Studies Evaluating Preoperative Hemoglobin or Hematocrit Levels and Postoperative Risk of Increased Length of Stay Readmission, and Discharge Location.
| First author, year (procedure) | Design | LOS | Readmission | Discharge location |
|---|---|---|---|---|
| Cervical Procedures | ||||
| Zreik 2020 (ACDF) | Retrospective | NR | OR = 1.36,[1.19,1.55], p =< 0.001* | NR |
| Phan 2017 (ACDF) | Retrospective | Risk of LOS >5, OR = 2.3,[1.6,3.2], p < 0.0001* | p = .219 | NR |
| Steinberger 2015 (PCF) | Retrospective |
LOS>5 days preop Hct: 38.48 vs LOS <5 days preop Hct: 40.99, p < 0.001* |
NR | NR |
| Phan 2017 (PCF) | Retrospective | Risk of LOS >5 days, OR 2.863, [1.758,4.662], p < 0.0001* | p = .0871 | NR |
| Lumbar Procedures | ||||
| Fosco 2012 (PLF, LL) | Retrospective | NR | NR | NR |
| Sanoufa 2015 (PLF) | Retrospective | Mean difference between Hb<13.5 and >13.5, 1.22 days, p < 0.001* |
NR | NR |
| Basques 2015 (PLF) | Retrospective | NR | NR | NR |
| Yew 2015 (PLF) | Retrospective | NR | NR | NR |
| Leu 2016 (PLF) | Retrospective | <12.9: 14.7+/-10.2, p = 0.002* | NR | NR |
| 13-14: 10.4+/-3.0, p = 0.014* | ||||
| 14-14.85: 11.3+/-5.2, p = 0.026* | ||||
| >14.85: 9.4+/-5.2, p = Reference | ||||
| Kaye 2018 (PLF) | Retrospective | NR | NR | NR |
| Ristagno 2018 (PLF) | Retrospective | NR | NR | NR |
| Lakomkin 2018 (PLF) | Retrospective | NR | NR | NR |
| Basques 2014 (LL) | Retrospective | Beta value +0.9, p < 0.001* (mean = 2.9+/-2.4) | p = .236 | NR |
| Smith 2016 (MIS-LF) | Retrospective | NR | NR | <24h Discharge Hb vs >24h Discharge Hb: 13.1 vs 13.8, p < 0.001* |
| Sachdeva 2020 (MIS-LF) | Retrospective | p = 0.15 | NR | NR |
Abbreviations: ACDF: Anterior Cervical Discectomy and Fusion, PCF: Posterior cervical fusion, PLF: Posterior lumbar fusion, MIS-LF: Minimally invasive lumbar fusion, LL: Lumbar Laminectomy, NR: Not reported, OR: Odds Ratio, ROR: Return to Operating Room, LOS: Length of Stay. Bold*= Demonstrated statistical significance.
PCF
Two studies reported on the association of preoperative anemia and postoperative outcomes following multi-level PCF.6,14 Steinberger et al reported that patients with increased LOS>5 days were more likely to have lower preoperative Hct (Hct: 38.48 vs 40.99, p < 0.001, Table 5 ). Phan et al reported that Hct <39% for males and <36% for females was associated with increased risk of any complication, rate of pulmonary complications, and return to the OR (Table 5). Similar to Steinberger et al, Phan et al reported associations between elevated risk of LOS greater than 5 days in patients with reduced preoperative Hct (OR 2.863, p < 0.0001, Table 5 ).
PLF
Eight studies demonstrated the association of preoperative anemia with postoperative outcomes following PLF.15-22 Four studies reported that low preoperative Hb/Hct was associated with increased risk of blood transfusion postoperatively( Table 4 ).15,17,18,20 Two studies reported that low preoperative Hb was associated with increased LOS ( Table 5 ).16,22 In single level PLF, increasing absolute difference in Hct from 45 was associated with significantly increased risk of adverse cardiac events (OR 1.07, p < 0.001) following PLF( Table 4 ). 19 Similarly, patients with Hct outside normal range, defined as 38%-54%, were at increased risk for minor, major, or any complications following 1 or 2 level PLF (Table 4). 21 In patients receiving outpatient minimally invasive lumbar fusion (MIS-LF), patients with delayed discharge (>24 hours) had significantly lower preoperative Hb (13.1 vs 13.8, p < 0.001) ( Table 5 ). 23 However, low preoperative Hb was not associated with increased LOS for MIS-LF patients ( Table 5 ). 24
LD
Two studies reported on the association of preoperative Hb/Hct and postoperative outcomes following lumbar laminectomy.15,25 Fosco and Di Fiore found that patients who received postoperative blood transfusion had significantly decreased preoperative (Hb: 13.1 vs 14.1, p = 0.023, Table 4 ). Basques et al reported that low preoperative Hct was associated with increased LOS (Beta value, +0.9, p < 0.001, Table 5 ).
Utility of Preoperative HbA1c in Spinal Surgery
The cut-off value for an elevated HbA1c was slightly different for each study and can be found in Table 6 .
Table 6.
Clinical Definition of Elevated HbA1c.
| First author, year (procedure) | Definition |
|---|---|
| Walid, 2010 (ACDF, LMD, LDF) | >6.1% |
| Takahashi, 2013 (PLF) | >6.5% |
| Cancienne, 2017 (ACDF) | >7.5% |
| Cancienne, 2017 (LD) | >7.5% |
| Moazzeni, 2018 (PLF) | >6.5% |
| Hwang (PLF) | >6.9% |
Abbreviations: HbA1c = Hemoglobin A1c Value, ACDF = Anterior Cervical Discectomy and Fusion, PLF = Posterior lumbar fusion, LMD:=Lumbar Microdiscectomy, LDF:=Lumbar Decompression and Fusion, LD: Lumbar Decompression.
ACDF
Two studies demonstrated the association of preoperative HbA1c and postoperative outcomes following ACDF.26,27 Cancienne et al reported that elevated HbA1c was associated with increased risk of postoperative surgical site infection (OR 1.84, p = 0.008, Table 7 ). Walid et al demonstrated that patients with an elevated HbA1c and history of DM had significantly increased total hospital cost compared to those without elevation ($36 748 vs $28 363, p < 0.05, Table 8 ).
Table 7.
Included Studies Evaluating Preoperative Hemoglobin A1c Levels and Postoperative Risk of Infection, Nonunion, and Bleeding.
| First author, year (procedure) | Infection | Fusion or nonunion rate | Bleeding |
|---|---|---|---|
| Cancienne, 2017 (ACDF) | A1c>7.5 vs A1c <7.5, OR = 1.84, [1.37,2.47], p = .008* |
NR | NR |
| Walid, 2010 (ACDF, LMD, LDF) | NR | NR | NR |
| Cancienne, 2017 (LD) | A1c>7.5 vs A1c <7.5, OR = 2.9; [1.8-4.9], p < .001* |
NR | NR |
| Takahashi, 2013 (PLF) | HbA1c>6.5, 0 case HbA1c <6.5, 1 case, p = NR |
Nonunion rate: HbA1c>6.5: 20% HbA1c<6.5: 3%, p = 0.095* |
NR |
| Moazzeni, 2018 (PLF) | NR | Fusion rate at 1 yr: HbA1c<6.5, 78% HbA1c>6.5, 53%, p = .002* |
HbA1c>6.5 vs <6.5, 556.2 ml vs 428.1 ml p = .006* |
| Hwang, 2019 (PLF) | A1c> 6.9 vs. A1c<6.9, OR = 4.5; [1.49-13.62), p = .008* |
NR | NR |
Abbreviations: ACDF: Anterior Cervical Discectomy and Fusion, PLF: Posterior lumbar fusion, LMD: Lumbar Microdiscectomy, LDF: Lumbar Decompression and Fusion, NR: Not reported, A1c: Hemoglobin A1c. Bold*= Demonstrated statistical significance.
Definition of Nonunion for Takahashi et al.: Nonunion after surgery anytime during follow-up period.
Table 8.
Included Studies Evaluating Preoperative Hemoglobin A1c Levels and Postoperative Functional Outcomes, Length of Stay, and Cost.
| First author, year | VAS | JOA | ODI | Fusion or nonunion rate | LOS | Cost |
|---|---|---|---|---|---|---|
| Cancienne, 2017 (ACDF) | NR | NR | NR | NR | NR | NR |
| Walid, 2010 (ACDF, LMD, LDF) | NR | NR | NR | NR | No DM: 1.42+/-1.984, HbA1c: 1.43 +/- 1.165, DM: 2.52 +/- 3.991 | No DM: 28 363 +/- 7673*, HbA1c: 29 420 +/- 6130, DM: 36 748 +/- 31 970* p < 0.05 between DM and No DM groups* |
| No DM: 2.75 +/- 4.318, HbA1c: 2.48 +/- 2.926, DM: 2.48 +/- 1.094 | No DM: 23 115 +/- 14 608, HbA1c: 22 306 +/- 7702, DM: 23 644 +/- 7068 | |||||
| No DM: 4.68 +/- 2.509*, HbA1c: 6.96 +/- 5.897*, DM: 5.55 +/- 3.615, p < 0.05 between no DM and HbA1c groups* |
No DM: 54 914 +/- 14 034*, HbA1c: 65 974 +/- 18 341*, DM: 61 536 +/- 14 527 p < 0.05 between no DM and HbA1c groups* |
|||||
| Cancienne, 2017 (LD) | NR | NR | NR | NR | NR | NR |
| Takahashi, 2013 (PLF) |
Low back pain: HbA1c >6.5: 29.3 vs HbA1c<6.5: 17.9, p = 0.013* Leg numbness: HbA1c >6.5: 37.9 vs HbA1c<6.5: 37.1 vs 27.9, p = 0.09 |
JOA Final FU: HbA1c>6.5, 24.4 vs HbA1c<6.5, 22.7, p = 0.137 | NR | Nonunion rate: HbA1c>6.5: 20% HbA1c<6.5: 3%, p = 0.095* |
NR | NR |
| Moazzeni, 2018 (PLF) | Preop: 7.8 vs 7.1, p < 0.001* | NR | Preop: 67.6 vs. 55.1, p < 0.001* | Fusion rate at 1 yr: HbA1c<6.5, 78% HbA1c>6.5, 53%, p = 0.002* |
NR | NR |
| 2wk: 5.4 vs 4.4, p = 0.003* | 2wk: 54.3 vs. 40.8, p < 0.001* | |||||
| 6mo: 4.2 vs. 3.6, p = 0.08 | 6mo: 45.5 vs 34.7, p < 0.001* | |||||
| 1yr: 3.5 vs. 2.9, p = 0.07 | 1yr: 40.7 vs 31.5, p = 0.002* | |||||
| Hwang, 2019 (PLF) | NR | NR | NR | NR | NR | NR |
Abbreviations: ACDF: Anterior Cervical Discectomy and Fusion, PLF: Posterior lumbar fusion, LMD: Lumbar Microdiscectomy, LDF: Lumbar Decompression and Fusion, LD: Lumbar Decompression, NR: Not reported, HbA1c: Hemoglobin A1c, VAS: Visual Analogue Scale, ODI: Oswestry Disability index, JOA: Japanese Orthopedic Association.
Bold*= Demonstrated statistical significance.
PCF
None of the studies explored the association between preoperative HbA1c and postoperative outcomes following PCF.
PLF
Four studies reported on the association between elevated HbA1c and adverse postoperative outcomes following PLF.27-30 Takashi et al reported that elevated HbA1c was associated with increased VAS scores for low back pain at final follow-up (29.3 vs 17.9, p < 0.013, Table 8 ). Moazzeni et al reported that VAS scores were significantly different between patients with elevated vs. normal HbA1c for the first 2 weeks postoperatively (5.4 vs 4.4, p = 0.003, Table 8 ) but reported that VAS scores were no longer significant after 6 months (4.2 vs 3.6, p = 0.08, Table 8 ). Elevated ODI scores were demonstrated up to one year postoperatively in patients with elevated HbA1c ( Table 8) . In addition, Walid et al reported an increased LOS (5.55 days vs 4.68 days, p < 0.05) and total cost (61 536 vs 54 914, p < 0.05) in patients with elevated HbA1c ( Table 8 ). Moreover, Takahashi et al reported that patients with an elevated HbA1c has a higher rate of non-unions ( Table 7 ). Similarly, Moazzeni et al reported a decreased fusion rate (53% vs 78%, p = 0.002) and increased postoperative bleeding (556.2 ml vs 428.1 ml, p = 0.006) in patients with elevated HbA1c ( Table 7 ).
LD
Two studies reported on the association between elevated HbA1c and adverse postoperative outcomes following lumbar microdiscectomy or lumbar decompression alone.27,31 Cancienne et al reported that elevated preoperative HbA1c was associated with a significant increase in surgical site infection following single level LD (OR 2.9, p < 0.001, Table 7 ). Walid et al demonstrated no significant association between elevated preoperative HbA1c and increased LOS or total hospitalization cost in patients undergoing lumbar microdiscectomy ( Table 8 ).
Risk of Bias and Quality of Evidence
Risk of bias was found to be not serious within all included studies. Quality of evidence was determined for all observational studies using the GRADE system. Across 19 included studies, there was low quality of evidence evaluating associations between preoperative Hemoglobin and HbA1c and postoperative outcomes demonstrates that lower preoperative hemoglobin and higher HbA1c values may have some utility in predicting adverse postoperative outcomes. The inconsistency portion of the GRADE system was unable to be evaluated for 2 studies, as primary outcomes in these articles were not evaluated in other included studies. As such, these studies were given a level lower in overall quality (Supplementary Table 3).
Discussion
We conducted a systematic review of the literature to determine the clinical utility of obtaining preoperative Hb/Hct and HbA1c in adult patients undergoing cervical and lumbar spinal surgeries. Specific procedures assessed included ACDF, PCF, PLF, and LD. Low preoperative Hb/Hct was found to be significantly associated with elevated risk for any postoperative complication and risk of postoperative transfusion, specifically for ACDF, PCF, and PLF. Decreased preoperative Hb/Hct was significantly associated with increased LOS for all procedures, except for MIS-LF. Preoperative HbA1c was reported to be predictive of postoperative infection following ACDF, LD, and PLF, and was found to be predictive of increased LOS and healthcare cost for PLFs.
Spinal operations carry varying risks of intraoperative and postoperative morbidity and appropriate perioperative planning requires preoperative risk stratification,32,33 and optimization of cardiovascular and pulmonary issues, and nutrition prior to surgery. 33 Risk factor evaluation commonly consists of screening labs, which include preoperative Hb/Hct. There is also some evidence supporting obtaining HbA1c in all patients, as prevalence of undiagnosed diabetes is fairly high with reported rates as high as 40.9%. 34
Our review indicates that regardless of exact Hb/Hct values utilized by studies, lower preoperative values are associated with adverse outcomes. Literature suggests that a Hct threshold of <35-38% may portend higher risk with spinal surgery. In our review, various thresholds for low preoperative Hb/Hct were reported ( Table 3 ). Hb cutoff values ranged from 11-13.5 g/dL, with studies reporting overall worse outcomes in patients with values below the reported threshold. Studies included in our review demonstrate that the use of Hb/Hct as a continuous variable is also valuable for postoperative risk assessment.19,22
For HbA1c, a threshold of 6.5-6.9% was associated with increased risk of complications in patients undergoing spine surgery. All 6 studies assessing preoperative HbA1c utilized threshold values ranging from 6.1 to 7.5%. Of these, 4 studies reported extensive postoperative follow-up of over 1 year; 3 of these studies utilized HbA1c threshold ranging from 6.5-6.9%, and indicated that elevated values above threshold were associated with poor long-term functional outcomes, increased nonunion rate, decreased fusion rate, and increased infection rate following PLF.28-30 The remaining study with 1 year follow-up reached similar conclusions but utilized a higher HbA1c threshold (7.5%). 31 Considering that HbA1c thresholds <7.5% still resulted in adverse postoperative outcomes, using lower values to gauge postoperative risk may be more recommended.
Because of strict inclusion and exclusion criteria to conduct the systematic review, we ended up excluding studies that did not directly examine the associations between postoperative outcomes after spinal surgery and preoperative Hb/Hct or HbA1c. A retrospective study performed by Perez et al was excluded because the authors only reported complications associated with decreased postoperative Hb. 35 Similarly, we excluded a retrospective study performed by Cai et al, in which the authors reported that decreased preoperative Hb was a significant predictor of reduced postoperative Hct; the authors did not investigate associations with decreased preoperative Hb/Hct. 36 For HbA1c, we excluded a retrospective study of over four-hundred thousand patients undergoing lumbar fusion as the authors identified diabetics patients using ICD-9 CM codes without examining actual preoperative HbA1c level. 37
The findings of our systematic review must be interpreted within its limitations. First, the heterogeneity of preoperative Hb/Hct and HbA1c thresholds, strict inclusion and exclusion criteria, and the possibility of missing studies may limit our review. Second, the absence of randomized controlled trials and variation in outcomes reported prevented us from performing a meta-analysis. Our review primarily consisted of only level III retrospective studies and one level II prospective study, perhaps because designing randomized controlled studies to evaluate association of preoperative hemoglobin or HbA1c on postoperative outcomes may be unfeasible. However, the lack of level I studies in our review limits our ability to make robust conclusions and provide more granular recommendations regarding preoperative management.
Conclusion
For ACDF, PCF, PLF, and LD procedures, preoperative Hb/Hct are clinically useful predictors for adverse postoperative outcomes, including complications, postoperative transfusion, and increased LOS. Based on this review, Hct values <35-38% and HbA1c>6.5-6.9% may be important thresholds for identifying patients who are higher risk of complications after undergoing spinal surgeries.
Supplemental Material
Supplemental Material, sj-docx-1-gsj-10.1177_2192568220979821 for Spine Surgery and Preoperative Hemoglobin, Hematocrit, and Hemoglobin A1c: A Systematic Review by Krishna V. Suresh, Kevin Wang, Ishaan Sethi, Bo Zhang, Adam Margalit, Varun Puvanesarajah and Amit Jain in Global Spine Journal
Supplemental Material, sj-docx-2-gsj-10.1177_2192568220979821 for Spine Surgery and Preoperative Hemoglobin, Hematocrit, and Hemoglobin A1c: A Systematic Review by Krishna V. Suresh, Kevin Wang, Ishaan Sethi, Bo Zhang, Adam Margalit, Varun Puvanesarajah and Amit Jain in Global Spine Journal
Supplemental Material, sj-docx-3-gsj-10.1177_2192568220979821 for Spine Surgery and Preoperative Hemoglobin, Hematocrit, and Hemoglobin A1c: A Systematic Review by Krishna V. Suresh, Kevin Wang, Ishaan Sethi, Bo Zhang, Adam Margalit, Varun Puvanesarajah and Amit Jain in Global Spine Journal
Acknowledgements
We thank Carrie L. Price, MLS, clinical informationist at the Johns Hopkins Welch Medical Library for her assistance in developing our search strategy.
Footnotes
Authors’ Note: This study used publicly available information and was not subject to evaluation by our Institutional Review Board.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Each author certifies that he or she has no commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements) that might pose a conflict of interest in connection with the submitted article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Krishna V. Suresh, BS  https://orcid.org/0000-0002-1785-8797
https://orcid.org/0000-0002-1785-8797
Amit Jain, MD  https://orcid.org/0000-0002-9983-3365
https://orcid.org/0000-0002-9983-3365
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Pellisé F, Serra-Burriel M, Smith JS, et al. Development and validation of risk stratification models for adult spinal deformity surgery. J Neurosurg Spine. 2019:1–13. doi:10.3171/2019.3.SPINE181452 [DOI] [PubMed] [Google Scholar]
- 2.Bohl DD, Idarraga AJ, Holmes GBJ, Hamid KS, Lin J, Lee S. Validated risk-stratification system for prediction of early adverse events following open reduction and internal fixation of closed ankle fractures. J Bone Joint Surg Am. 2019;101(19):1768–1774. doi:10.2106/JBJS.19.00203 [DOI] [PubMed] [Google Scholar]
- 3.Holm JP, Amar AOS, Hyldstrup L, Jensen JEB. Hyponatremia, a risk factor for osteoporosis and fractures in women. Osteoporos Int. 2016;27(3):989–1001. doi:10.1007/s00198-015-3370-0 [DOI] [PubMed] [Google Scholar]
- 4.Phan K, Wang N, Kim JS, et al. Effect of preoperative anemia on the outcomes of anterior cervical discectomy and fusion. Glob Spine J. 2017;7(5):441–447. doi:10.1177/2192568217699404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hennrikus E, Ou G, Kinney B, et al. Prevalence, timing, causes, and outcomes of hyponatremia in hospitalized orthopaedic surgery patients. J Bone Joint Surg Am. 2015;97(22):1824–1832. doi:10.2106/JBJS.O.00103 [DOI] [PubMed] [Google Scholar]
- 6.Phan K, Dunn AE, Kim JS, et al. Impact of preoperative anemia on outcomes in adults undergoing elective posterior cervical fusion. Glob Spine J. 2017;7(8):787–793. doi:10.1177/2192568217705654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Billett HH. Hemoglobin and hematocrit. In: Walker HK, Hall WD, Hurst JW, eds. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Boston: Butterworths; 1990. Chapter 151. PMID: 21250102. [PubMed] [Google Scholar]
- 8.Broadway-Duren JB, Klaassen H. Anemias. Crit Care Nurs Clin North Am. 2013;25(4):411–426. v. doi:10.1016/j.ccell.2013.09.004 [DOI] [PubMed] [Google Scholar]
- 9.Sherwani SI, Khan HA, Ekhzaimy A, Masood A, Sakharkar MK. Significance of HbA1c test in diagnosis and prognosis of diabetic patients. Biomark Insights. 2016;11:95–104. doi:10.4137/BMI.S38440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. doi:10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oxford Centre for Evidence-Based Medicine 2011 Levels of Evidence. Phys Rev E. Published 2011. Updated June 2014. Accessed August 1, 2020. http://ridum.umanizales.edu.co:8080/jspui/bitstream/6789/377/4/Muñoz_Zapata_Adriana_Patricia_Artículo_2011.pdf [Google Scholar]
- 12.Wells G, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. http//www.ohri.ca/programs/clinical_epidemiology/oxford.asp. 2012. doi:10.2307/632432
- 13.Zreik J, Goyal A, Alvi MA, Freedman BA, Bydon M.Utility of preoperative laboratory testing in assessing risk of adverse outcomes after anterior cervical discectomy and fusion: insights from national surgical registry. World Neurosurg. 2020;136:e398–e406. doi:10.1016/j.wneu.2020.01.023 [DOI] [PubMed] [Google Scholar]
- 14.Steinberger J, Kothari P, Lee NJ, et al. Influencing factors on length of stay in adults undergoing elective posterior cervical fusion: an analysis of the American College of Surgeons National Surgical Quality Improvement Program Database. Spine J. 2015;15(10):S231. doi:10.1016/j.spinee.2015.07.338 [Google Scholar]
- 15.Fosco M, Di Fiore M. Factors predicting blood transfusion in different surgical procedures for degenerative spine disease. Eur Rev Med Pharmacol Sci. 2012;16(13):1853–1858. [PubMed] [Google Scholar]
- 16.Sanoufa M, Smisson W, Floyd H, Robinson JS. The effect of anaemia on hospital length of stay in lumbar decompression and fusion procedures. J Perioper Pract. 2015;25(12):267–271. doi:10.1177/175045891502501204 [DOI] [PubMed] [Google Scholar]
- 17.Basques BA, Anandasivam NS, Webb ML, et al. Risk factors for blood transfusion with primary posterior lumbar fusion. Spine (Phila Pa 1976). 2015;40(22):1792–1797. doi:10.1097/BRS.0000000000001047 [DOI] [PubMed] [Google Scholar]
- 18.Yew AY, Hoffman H, Li C, McBride DQ, Holly LT, Lu DC. Quantitative data-driven utilization of hematologic labs following lumbar fusion. J Spinal Disord Tech. 2015;28(4): E231–E236. doi:10.1097/BSD.0000000000000194 [DOI] [PubMed] [Google Scholar]
- 19.Kaye ID, Wagner SC, Butler JS, Sebastian A, Morrissey PB, Kepler C. Risk factors for adverse cardiac events after lumbar spine fusion. Int J Spine Surg. 2018;12(5):638–643. doi:10.14444/5079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ristagno G, Beluffi S, Tanzi D, et al. Red blood cell transfusion need for elective primary posterior lumbar fusion in a high-volume center for spine surgery. J Clin Med. 2018;7(2):19. doi:10.3390/jcm7020019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lakomkin N, Goz V, Cheng JS, Brodke DS, Spiker WR. The utility of preoperative labs in predicting postoperative complications following posterior lumbar fusion. Spine J. 2016. doi:10.1016/j.spinee.2016.07.369 [DOI] [PubMed] [Google Scholar]
- 22.Leu S, Kamenova M, Mehrkens A, Mariani L, Schären S, Soleman J. Preoperative and postoperative factors and laboratory values predicting outcome in patients undergoing lumbar fusion surgery. World Neurosurg. 2016;92:323–338. doi:10.1016/j.wneu.2016.05.011 [DOI] [PubMed] [Google Scholar]
- 23.Smith WD, Wohns RNW, Christian G, Rodgers EJ, Rodgers WB. Outpatient minimally invasive lumbar interbody: fusion predictive factors and clinical results. Spine (Phila Pa 1976). 2016;41:S106–S122. 10.1097/BRS.0000000000001479 [DOI] [PubMed] [Google Scholar]
- 24.Sachdeva I, Carmouche JJ. Postoperative anemia predicts length of stay for geriatric patients undergoing minimally invasive lumbar spine fusion surgery. Geriatr Orthop Surg Rehabil. 2020;11. doi:10.1177/2151459320911874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Basques BA, Varthi AG, Golinvaux NS, Bohl DD, Grauer JN. Patient characteristics associated with increased postoperative length of stay and readmission after elective laminectomy for lumbar spinal stenosis. Spine (Phila Pa 1976). 2014;39(10):833–840. doi:10.1097/BRS.0000000000000276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cancienne JM, Werner BC, Hassanzadeh H, Singla A, Shen FH, Shimer AL. The association of perioperative glycemic control with deep postoperative infection after anterior cervical discectomy and fusion in patients with diabetes. World Neurosurg. 2017;102:13–17. doi:10.1016/j.wneu.2017.02.118 [DOI] [PubMed] [Google Scholar]
- 27.Walid MS, Newman BF, Yelverton JC, Nutter JP, Ajjan M, Robinson JS. Prevalence of previously unknown elevation of glycosylated hemoglobin in spine surgery patients and impact on length of stay and total cost. J Hosp Med. 2010;5(1):E10–14. doi:10.1002/jhm.541 [DOI] [PubMed] [Google Scholar]
- 28.Takahashi S, Suzuki A, Toyoda H, et al. Characteristics of diabetes associated with poor improvements in clinical outcomes after lumbar spine surgery. Spine (Phila Pa 1976). 2013;38(6):516–522. doi:10.1097/BRS.0b013e318273583a [DOI] [PubMed] [Google Scholar]
- 29.Moazzeni K, Kazemi KA, Khanmohammad R, Eslamian M, Rostami M, Faghih-Jouibari M. Comparison of surgical outcome between diabetic versus nondiabetic patients after lumbar fusion. Int J Spine Surg. 2018;12(4):528–532. doi:10.14444/5064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hwang JU, Son DW, Kang KT, et al. Importance of hemoglobin a1c levels for the detection of post-surgical infection following single-level lumbar posterior fusion in patients with diabetes. Korean J Neurotrauma. 2019;15(2):150–158. doi:10.13004/kjnt.2019.15.e36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cancienne JM, Werner BC, Chen DQ, Hassanzadeh H, Shimer AL. Perioperative hemoglobin A1c as a predictor of deep infection following single-level lumbar decompression in patients with diabetes. Spine J. 2017;17(8):1100–1105. doi:10.1016/j.spinee.2017.03.017 [DOI] [PubMed] [Google Scholar]
- 32.Street JT, Lenehan BJ, Dipaola CP, et al. Morbidity and mortality of major adult spinal surgery. a prospective cohort analysis of 942 consecutive patients. Spine J. 2012;12(1):22–34. doi:10.1016/j.spinee.2011.12.003 [DOI] [PubMed] [Google Scholar]
- 33.Casper DS, Rihn JA. Preoperative risk stratification: who needs medical consultation? Spine (Phila Pa 1976). 2020;45:860–861. 10.1097/BRS.0000000000003437 [DOI] [PubMed] [Google Scholar]
- 34.Shohat N, Goswami K, Tarabichi M, Sterbis E, Tan TL, Parvizi J. All patients should be screened for diabetes before total joint arthroplasty. J Arthroplasty. 2018;33(7):2057–2061. doi:10.1016/j.arth.2018.02.047 [DOI] [PubMed] [Google Scholar]
- 35.Perez JJ, Yanamadala V, Wright AK, Bohl MA, Leveque JCA, Sethi RK. Outcomes surrounding perioperative transfusion rates and hemoglobin nadir values following complex spine surgery. World Neurosurg. 2019;126:e1287–e1292. doi:10.1016/j.wneu.2019.03.079 [DOI] [PubMed] [Google Scholar]
- 36.Cai Q, Zeng S, Zhi L, Wu J, Ma W.Predictors of haematocrit in lumbar fusion for lumbar disc herniation: a surgical assessment. BMC Musculoskelet Disord. 2017;18(1):323. doi:10.1186/s12891-017-1655-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guzman JZ, Iatridis JC, Skovrlj B, et al. Outcomes and complications of diabetes mellitus on patients undergoing degenerative lumbar spine surgery. Spine (Phila Pa 1976). 2014;39(19):1596–1604. doi:10.1097/BRS.0000000000000482 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-docx-1-gsj-10.1177_2192568220979821 for Spine Surgery and Preoperative Hemoglobin, Hematocrit, and Hemoglobin A1c: A Systematic Review by Krishna V. Suresh, Kevin Wang, Ishaan Sethi, Bo Zhang, Adam Margalit, Varun Puvanesarajah and Amit Jain in Global Spine Journal
Supplemental Material, sj-docx-2-gsj-10.1177_2192568220979821 for Spine Surgery and Preoperative Hemoglobin, Hematocrit, and Hemoglobin A1c: A Systematic Review by Krishna V. Suresh, Kevin Wang, Ishaan Sethi, Bo Zhang, Adam Margalit, Varun Puvanesarajah and Amit Jain in Global Spine Journal
Supplemental Material, sj-docx-3-gsj-10.1177_2192568220979821 for Spine Surgery and Preoperative Hemoglobin, Hematocrit, and Hemoglobin A1c: A Systematic Review by Krishna V. Suresh, Kevin Wang, Ishaan Sethi, Bo Zhang, Adam Margalit, Varun Puvanesarajah and Amit Jain in Global Spine Journal