Abstract
Study Design:
Retrospective case series.
Objective:
To report our experience with corpectomy of the thoracolumbar (TL) spine through a minimally invasive lateral retropleural or retroperitoneal approach.
Methods:
This is a retrospective case series of 20 consecutive patients who underwent minimally invasive TL corpectomy and spinal reconstruction. Electronic medical records were reviewed for demographic, operative, and clinical outcome data.
Results:
Between 2015 and 2019, 20 consecutive cases of minimally invasive TL corpectomy were performed, comprising 12 men (60%) and 8 women (40%) with a mean age of 54.3 years. Indications for surgery were infection (n = 6, 30%), metastatic disease (n = 2, 10%), fracture (n = 6, 30%), and calcified disc herniation (n = 6, 30%). Partial and complete corpectomy was performed in 5 patients (25%) and 15 patients (75%), respectively. Mean operative time and estimated blood loss was 276.2 minutes and 558.4 mL, respectively. Mean length of stay from admission and surgery were 14.6 and 11.4 days, respectively. Mean length of stay from surgery for elective cases was 4.2 days. Mean follow-up time was 330.4 days. Visual analogue scale score improved from 7.7 to 4.5 (P < .01). There were a total of 3 postoperative complications in 2 patients, including 1 mortality for urosepsis. One patient had revision spinal surgery for adjacent segment disease.
Conclusions:
Corpectomy and reconstruction of the TL spine is feasible and safe using a minimally invasive lateral retropleural or retroperitoneal approach. Since this is a relatively new technique, more studies are needed to compare the short- and long-term radiographic and clinical outcomes between minimally invasive versus open corpectomy of the TL spine.
Keywords: minimally invasive surgery (MIS), thoracolumbar spine, thoracolumbar corpectomy, retropleural approach, retroperitoneal approach
Introduction
Surgical pathologies affecting the anterior or middle column of the thoracolumbar (TL) spine (eg, tumors, infections, fractures, cord-level calcified discs) are traditionally managed using open surgical approaches. 1 The thoracotomy and thoracoabdominal approaches often require access surgeons for exposure and are associated with high rates of short- and long-term complications.2-4
More recently, the development of minimally invasive surgery (MIS) techniques has allowed for safe access of the TL junction through a mini-open lateral retropleuralor retroperitoneal approach.5,6 Consistent with prior published literature, a TL corpectomy is considered MIS if the surgery utilizes specially designed retractors to access and directly visualize the spine with minimal soft tissue disruption.6,7 The incision for MIS TL corpectomy is typically 5 to 6 cm long, which is considerably shorter than the incisions for conventional open anterolateral transthoracic and thoracoabdominal approaches.6,8 Cadaveric studies have demonstrated MIS TL corpectomy and anterior column reconstruction is safe and feasible. 7 Because this technique is relatively new and has only been utilized regularly over the past decade, additional studies are needed to document clinical results and validate efficacy. In this study, we review our case series of 20 consecutive patients who had MIS TL corpectomy for various spinal pathologies.
Methods
This study was approved by our institutional review board. We retrospectively reviewed consecutive patients who underwent MIS TL corpectomy and anterior spinal reconstruction by a single surgeon (YJ) at a single academic institution between 2015 and 2019. The electronic medical charts were evaluated for demographics (age, sex, body mass index [BMI], primary diagnosis, American Society of Anesthesiologists [ASA] physical status, case type), operative data (corpectomy level, rib autograft harvest level, anterior spinal reconstruction construct, fixation method, bone morphogenetic protein [BMP] use, operative time, estimated blood loss [EBL], intraoperative transfusion), visual analogue scale (VAS), postoperative disposition, postoperative complications, reoperation, length of stay (LOS) from admission, and LOS from surgery. For cases in which the posterior spinal stabilization was performed on the same day, only the operative time for the MIS TL corpectomy was reported. Furthermore, EBL was only calculated for the MIS TL corpectomy portion of the case. Corpectomy involving <50% of the vertebral body was defined as partial, while corpectomy involving ≥50% of the vertebral body was defined as complete. A literature search was subsequently performed to compare the results of our case series with other published studies on MIS TL corpectomy.
MIS TL Corpectomy Technique
The technique has been previously described in detail by Javidan and Hurley. 6 The approach is performed by the senior author (YJ) without an access surgeon (Figure 1). For corpectomy of L2 and L3, we prefer a prepsoas, retroperitoneal approach using the standard direct lateral incision. For corpectomy of L1 and above, we prefer a retropleural, retrodiaphragmatic approach. The patient is positioned in the right lateral decubitus position (ie, left side up). A radiopaque crosshair tool is used under fluoroscopy to identify the appropriate level. A 6-cm oblique incision is made in line with the rib overlying the vertebra of interest. The latissimus dorsi, external oblique, internal oblique, and transverse abdominus muscles are sequentially split in line with the incision. At the level of the intercostal muscles, approximately 6 cm of the overlying rib is exposed and harvested for autograft. The retropleural plane is carefully developed with blunt dissection until the lateral vertebral body is encountered. Once the level is reconfirmed with fluoroscopy, expendable retractors are inserted to facilitate access and direct visualization. Discectomy, corpectomy, and anterior column reconstruction are then performed through this corridor.
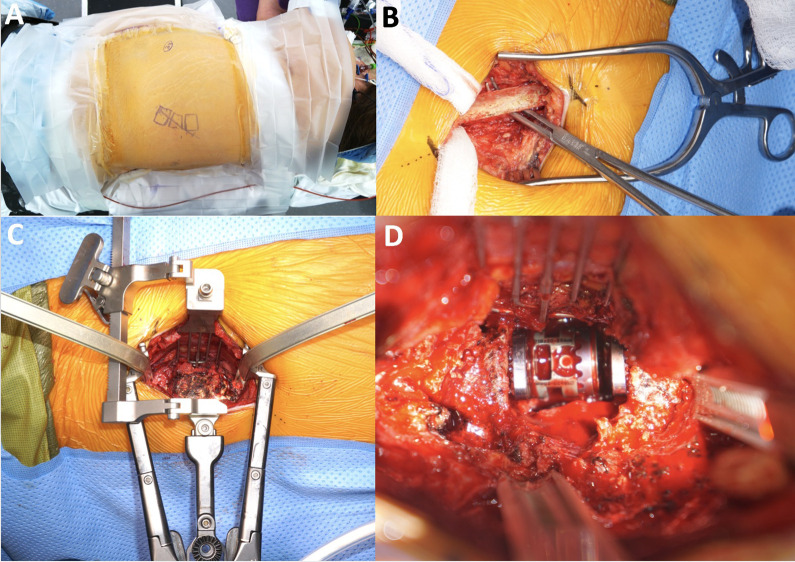
Figure 1.
(A) Patient is positioned in right lateral decubitus position (ie, left side up). A 6-cm oblique incision is made in line with the rib overlying vertebra of interest. (B) At the level of intercostal muscles, approximately 6 cm of overlying rib is exposed and harvested for autograft. (C) Retropleural plane is carefully developed with blunt dissection until lateral vertebral body and discs are encountered. Expendable retractors are subsequently inserted to facilitate access and direct visualization. (D) Discectomy, corpectomy, and anterior column reconstruction are performed through this corridor.
Results
Between 2015 and 2019, 20 consecutive cases of MIS TL corpectomy were performed by the principal investigator (YJ), comprising 12 men (60%) and 8 women (40%) with a mean age of 54.3 years (SD = 16.9) (Table 1). The mean BMI was 29.1 kg/m2 (SD = 8.5). The indications for surgery were infection (n = 6, 30%), metastatic disease (n = 2, 10%), fracture (n = 6, 30%), and calcified disc herniation (n = 6, 30%) (Table 2). Five cases (25%) were elective, while the remaining 15 were on-call cases (75%). The majority of patients were ASA 3 (n = 16, 80%).
Table 1.
Summary of Demographic Data, Operative Data, and Clinical Outcomes of All 20 Cases.
| Characteristic | Value | |
|---|---|---|
| Cases, n | 20 | |
| Age, years | 54.3 | |
| Sex, n (%) | ||
| Male | 12 (60) | |
| Female | 8 (40) | |
| BMI, kg/m2 | 29.1 | |
| ASA physical status, n (%) | ||
| ASA 2 | 2 (10) | |
| ASA 3 | 16 (80) | |
| ASA 4 | 2 (10) | |
| Case type, n (%) | Elective: 5 (25%) On-call: 15 (75%) |
|
| Elective | 5 (25) | |
| On-call | 15 (75) | |
| Operative time, minutes | 351.8 | |
| EBL, mL | 558.4 | |
| Intraoperative transfusion, n (%) | ||
| No | 12 (60) | |
| Yes | 8 (40) | |
| Postoperative disposition, n (%) | ||
| Floor | 12 (60) | |
| ICU | 8 (40) | |
| LOS from admission, days | 14.6 | |
| LOS from surgery, days | 11.4 | |
| VAS score | ||
| Preoperative | 7.7 | P < .01 |
| Postoperative | 4.5 | |
| Follow-up | 330.4 days | |
Abbreviations: BMI, body mass index; ASA, American Society of Anesthesiologists; EBL, estimated blood loss; ICU, intensive care unit; LOS, length of stay; VAS, visual analogue scale.
Table 2.
Clinical and Demographic Characteristics of Each Patient.
| Case | Age, years | Sex | Diagnosis | Corpectomy level | Rib harvested | Reconstruction | Lateral plating | Posterior fixationa | Complications | Reoperation |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 47 | M | Pott disease | T11, T12 | 10 | Cage | Y | T9-L2; open; staged | ||
| 2 | 68 | M | Osteomyelitis | T12, L1 | 10 | Cage | T10-L3; open; same day | |||
| 3 | 51 | F | Burst | L1 | 11 | Cage | T11-L2; percutaneous; same day | |||
| 4 | 43 | F | Burst | L1 | 10 | Cage | Ye | |||
| 5 | 37 | M | Burst | L2 | 11 | Cage | T12-L3; open; staged | |||
| 6 | 64 | F | Burst | T12, L1 | 10 | Cage | T11-L1; open; same day | |||
| 7 | 20 | M | Burst | T12 | 12 | Cage | Y | |||
| 8 | 68 | M | Osteomyelitis | T12, L1 | 10 | Cage | T10-L3; open; staged | Revision T10-L4 for ASD | ||
| 9 | 60 | F | Burst | T11, T12 | 9 | Cage | T8-L2; open; same day | Pleural violation; death | ||
| 10 | 52 | M | Calcified thoracic disc | T12, L1 | 10 | Cage | Y | |||
| 11 | 72 | M | Osteomyelitis | T11, T12 | 10 | Cage | T9-pelvis; open; staged | |||
| 12 | 50 | M | Osteomyelitis | T12 | 10 | Cage | Y | |||
| 13 | 75 | F | Calcified thoracic disc | bT10, T11 | 10 | Interbody graft | Y | |||
| 14 | 69 | M | Metastatic prostate cancer | T10 | 10 | Cage | T7-L1; open; same day | |||
| 15 | 86 | F | Osteomyelitis | L2, L3 | 12 | Cage | Y | L1-4; open; same day | Fascial dehiscence, I&D | |
| 16 | 52 | F | Calcified lumbar disc | bL1, L2 | 11 | Interbody graft | Y | |||
| 17 | 63 | M | Metastatic prostate cancer | T10 | 10 | Cage | Y | |||
| 18 | 27 | F | Calcified thoracic disc | bT9, T10 | 8 | Interbody graft | Y | |||
| 19 | 55 | M | Calcified thoracic disc | bT9, T10 | 9 | Interbody graft | Y | |||
| 20 | 27 | M | Calcified lumbar disc | bL1, L2 | 10 | Interbody graft | Y |
Abbreviations: ASD, adjacent segment disease; I&D, irrigation and debridement; F, female; M, male.
a Posterior stabilization was performed either open or percutaneous, and either same day or staged.
b Partial corpectomy (hemicorpectomy).
Partial and complete corpectomy was performed in 5 patients (25%) and 15 patients (75%), respectively. Of the 15 complete corpectomy cases, 7 patients (46.7%) had single-level corpectomy, compared to 8 patients (53.3%) with 2-level corpectomy. All 15 complete corpectomy cases (100%) were reconstructed using a static or expandable cage with a wide rectangular footprint. In this group, lateral plating alone was utilized in 5 cases (33.3%), while additional posterior spinal stabilization was performed in the remaining 10 cases (66.7%). In the partial corpectomy group, interbody grafting and lateral plating only was performed in all 5 cases (100%). The 10th rib was harvested in 12 of the 20 cases (60%). BMP was used in 10 cases (50%) to facilitate fusion. The mean operative time and EBL were 276.2 minutes (SD = 71.2) and 558.4 mL (SD = 557.9), respectively. Eight patients (40%) required intraoperative packed red blood cell (pRBC) transfusion. Eight patients (40%) were transferred to the intensive care unit (ICU) after surgery. The mean LOS from admission and surgery were 14.6 days (SD = 19.1) and 11.4 days (SD = 16.2), respectively. The mean LOS from surgery for elective cases was 4.2 days. The VAS score improved from 7.7 (SD = 1.8) to 4.5 (SD = 3.3) (P < .01).
There were a total of 3 postoperative complications in 2 patients. One patient had a pleural injury requiring intraoperative general surgery consultation and chest tube placement. This patient expired at postoperative day 33 due to urosepsis. Another patient underwent irrigation and debridement for posterior wound dehiscence at postoperative day 35. The mean follow-up time was 330.4 days (SD = 390.6). Over this period, one patient had revision spinal surgery for adjacent segment disease roughly 10 months after the index operation.
Discussion
Corpectomy of the TL spine is commonly performed for tumors, infections (Figure 2), traumas (Figure 3), and less commonly calcified disc herniations (Figure 4, Table 3). Similar to our study, Khan et al 9 reported on their series in which 24 of 25 MIS TL corpectomy cases (96%) were for tumors, infections, or burst fractures. Likewise, in a larger study by Baaj et al, 10 all 80 patients (100%) had MIS TL corpectomy for the abovementioned diagnoses. Given the nature of these pathologies, in our experience, most cases were performed on-call when the patients were admitted through the emergency department. In addition, the majority of patients were medically complex with high ASA scores, thus necessitating prolonged LOS from admission and surgery to receive appropriate medical care for their infections, tumors, or polytraumas. In the literature, the length of hospitalization after MIS TL corpectomy ranged between 4 and 18.4 days.5,11 In our study, the LOS from surgery for all cases was 11.4 days. However, the LOS from surgery for elective cases was only 4.2 days, which suggests that patients who had longer LOS after MIS TL corpectomy were for medical rather than surgical reasons. Previously published studies have favored MIS over open TL corpectomy in terms of LOS. Singh et al 12 found patients undergoing anterior-posterior MIS TL corpectomy had shorter hospitalization compared with patients undergoing anterior-posterior open TL corpectomy or posterior open TL corpectomy.
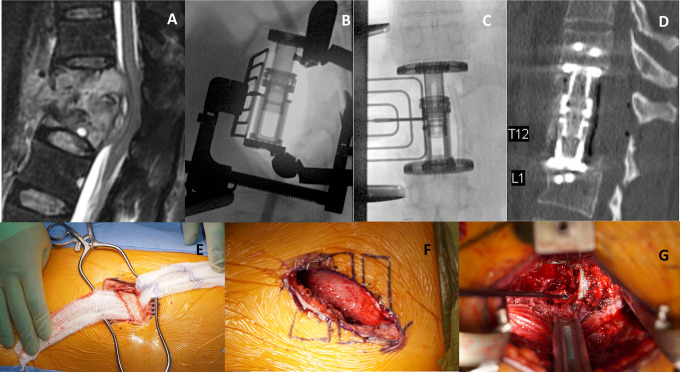
Figure 2.
(A) Sagittal T2-weighted magnetic resonance imaging (MRI) with contrast demonstrating T11 and T12 vertebral body erosion and collapse in the setting of tuberculosis infection. Bone erosion and phlegmon formation led to severe cord compression and cord signal changes. (B, C) Intraoperative lateral (B) and anteroposterior (C) fluoroscopic images showing an expandable cage spanning the T11 and T12 corpectomy defect with retractor in place. (D) Postoperative mid-sagittal computed tomography (CT) demonstrating adequate decompression and correction of the kyphotic deformity. An anteriorly placed expandable cage with anterior fixation points can be seen. (E) Intraoperative photograph illustrating subperiosteal dissection of the T10 rib prior to partial resection with the rib cutter. (F) Intraoperative photograph illustrating the retropleural space developed after blunt dissection and prior to placement of the lighted retractor system. (G) Intraoperative photograph with retractor in place illuminating the corpectomy defect. Adequate canal decompression can be seen.
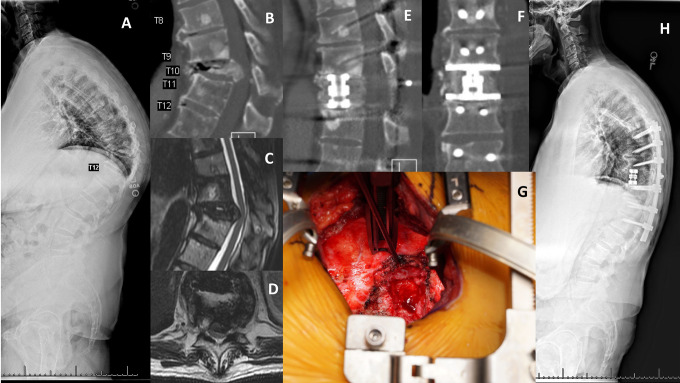
Figure 3.
(A) Standing full-length lateral spine radiograph demonstrating focal kyphotic collapse at T10 with compensatory pelvic retroversion and lumbar hyperlordosis. (B) Sagittal computed tomography (CT) of the thoracolumbar spine demonstrating T10 vertebral collapse and considerable retropulsion of the bony fragments, causing severe spinal canal compromise. (C, D) T2-weighted sagittal (C) and axial (D) magnetic resonance imaging (MRI) demonstrating severe thoracic cord compression. (E, F) Postoperative mid-sagittal (E) and coronal (F) CT reconstruction demonstrating adequate canal decompression and anterior column reconstruction using an expandable cage with wide rectangular footprint. Bone graft is demonstrated around the cage body. (G) Intraoperative photograph showing the corpectomy defect and dura with complete decompression of the spinal canal. (H) Postoperative standing full-length lateral spine radiograph demonstrating correction of the focal kyphosis with placement of an anterior cage and posterior instrumentation.
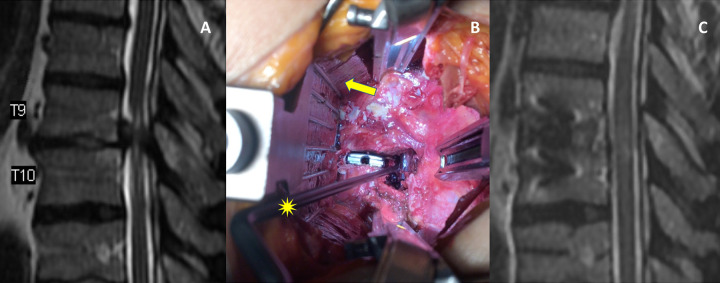
Figure 4.
(A) Sagittal T2-weighted magnetic resonance imaging (MRI) of the thoracolumbar spine demonstrating T9-10 disc-osteophyte complex causing severe cord compression with associated cord signal changes. (B) Intraoperative photograph showing an anteriorly placed interbody trial and triangular wedge osteotomy of the inferoposterior T9 and superoposterior T10 vertebral bodies. The yellow star delineates the MIS Penfield pointing to the well-decompressed canal and dura. The yellow arrow points to the pleura that has been mobilized anteriorly and held in place with the fan-blade retractor. (C) Postoperative sagittal T2-weighted MRI demonstrating adequate decompression of the T9-10 disc-osteophyte complex.
Table 3.
Overview of Clinical Studies Evaluating Outcomes of Mini-Open Thoracolumbar Corpectomy.
| Study | Case number | Pathology | Follow-up | Outcomes | Complications |
|---|---|---|---|---|---|
| Smith et al (2010), case seriesa | 52 | Trauma: 52 | 24 months | Operating time: 127.5 minutes EBL: 300 mL Hospital stay: 4 days Improvement in ASIA scores; no neurologic deterioration |
8 complications (15.4%) in 7 patients: 2 dural tear, 2 intercostal neuralgia, 2 DVT, 1 pleural effusion, 1 wound infection Cage subsidence in 7 patients (13.5%) No reoperations |
| Khan et al (2012), case series | 25 | Tumor: 10 Infection: 5 Trauma: 9 Disc herniation: 1 |
5.1 months | Operating time: 188.5 minutes EBL: 423 mL 9 transfusion (36%) 62% improvement in VAS |
No perioperative complications (within 30 days) 2 mortalities (8%) (>3 months from index operation) No implant subsidence |
| Baaj et al (2012), case series | 80 | Tumor: 21 Infection: 2 Trauma: 57 |
Not reported | Not reported | 10 complications (12.5%): 2 dural tear, 2 intercostal neuralgia, 2 DVT, 1 pleural effusion, 1 wound infection, 1 hardware failure, 1 hemothorax 2 reoperations (2.5%): hardware failure (cage collapse) and hemothorax |
| Doria et al (2012), case series | 26 | Trauma: 26 | Not reported | Reduction of kyphosis angle by 5° Improvement of vertebral height by 5.7 mm Improvement in VAS from 9 to 5 Improvement in ODI from 86% to 38% |
No intraoperative complications |
| Theologis et al (2016), case seriesb | 12 | Trauma: 12 | 38 months | Operating time: 288.7 minutes EBL: 988 mL 2 transfusion (16.7%) Hospital stay: 18.4 days Improvement in focal lordosis and lumbar lordosis |
3 pleural violation (25%) requiring chest tube placement 3 complications (25%): 1 MSSA deep wound infection requiring I&D, 1 PE, 1 revision for cage subsidence |
| Sulaiman et al (2017), retrospective case controlc | 23 | Tumor: 4 Infection: 7 Trauma: 12 |
Not reported | Operating time: 295 minutes EBL: 560 mL 241.9 mL blood transfusion Hospital stay: 7.2 days from admission, 5.8 days from surgery All patients (100%) improved or preserved ASIA Impairment Scale score |
4 chest tubes placed 1 medical and 2 surgical complications |
| Yu et al (2018), retrospective case controld | 20 | Trauma: 19 Infection: 1 |
14.1 months | Operating time: 382.2 minutes EBL: 687.5 mL Hospital stay: 8 days Reduction in VAS by 4.6 Improvement in kyphosis angle by 7.2° |
5 patients (25%) with postoperative anterior thigh numbness No reoperations |
Abbreviations: ASIA, American Spinal Injury Association; EBL, estimated blood loss; VAS, visual analogue scale; DVT, deep vein thrombosis; PE, pulmonary embolism; ODI, Oswestry Disability Index; I&D, irrigation and debridement; MSSA, methicillin-sensitive Staphylococcus aureus.
a Included cases involving midthoracic and lower lumbar spine, not just thoracolumbar spine.
b Lumbar pathologies only.
c Only minimally invasive surgery cases were included in this chart.
d Combined all cases together in this chart.
Our study supports MIS TL corpectomy is safe with low perioperative complications. Specifically, the complication rate in our study was 10% (2 of 20 patients). One patient developed superficial posterior wound dehiscence requiring return to the operating room (OR) for formal debridement and primary closure. There was no wound-related complication over the lateral incision in any of the cases. Similarly, Singh et al 12 reported 0% infection rate in patients undergoing anterior-posterior MIS TL corpectomy, compared with 13.3% and 20% infection rates in patients undergoing posterior open and anterior-posterior open TL corpectomy, respectively. With MIS techniques, the incision is smaller (average of 5-6 cm) with less soft tissue dissection and disruption, and therefore the reported rates of wound complication are low compared with traditional open approaches. Khan et al 9 reported no perioperative complications in 25 patients undergoing MIS TL corpectomy. Baaj et al 10 reported a complication rate and reoperation rate of 12.5% and 2.5%, respectively. In 1 comparative study, the reoperation rate was significantly lower in the MIS corpectomy cohort (0%) compared with the open cohort (40%). 12 The most common surgical complications include durotomy, pleurotomy, intercostal neuralgia, wound infection, and anterior thigh numbness.5,10-14 Care must be taken to not injure the pleura or peritoneum during the exposure. In circumstances when the pleura or peritoneum is violated, primary repair is usually feasible, and a chest tube can be placed for pleural injuries. In our review of the published literature, there was only 1 case of return to the OR for hemothorax. 10 The most common medical complications include deep vein thrombosis and pulmonary embolism.5,11 While cage subsidence is a leading cause for return to the OR,10,11 not all cases of radiographic subsidence is clinically symptomatic requiring revision surgery. 5 Despite the medical complexity of our patient population, the mortality rate remained low after MIS TL corpectomy. We had 1 mortality (5%) for urosepsis at a mean follow-up of 11 months, while Khan et al 9 reported 2 mortalities (8%) for metastatic disease progression at a mean follow-up of 5 months.
Our EBL and operative time were comparably higher than those reported by Smith et al 5 and Khan et al 9 . In our literature review, the EBL and operative time following MIS TL corpectomy varied significantly,5,9,11-14 suggesting a steep learning curve for this MIS technique. However, compared with open corpectomy, minimally invasive corpectomy of the TL spine results in lower EBL and operative time. 11 Singh et al 12 reported patients undergoing anterior-posterior MIS TL corpectomy had decreased operative time and blood loss when compared with anterior-posterior open TL corpectomy or posterior open TL corpectomy.
In our experience, lateral plating alone is sufficient for TL hemicorpectomy or single-level corpectomy, while same-day or staged posterior spinal stabilization is often necessary for 2-level corpectomy. Nonetheless, the decision for posterior spinal stabilization should be on a case by case basis based on the patient’s bone quality and/or the need for posterior decompression or deformity correction. Posterior instrumented fusion is performed open when posterior decompression is required; otherwise, it can be performed percutaneously. We always use the rib autograft for strut grafting, in addition to BMP in selective cases. When a cage is selected for anterior column reconstruction, we recommend using a wide footprint over a cylindrical cage as there is a lower reported rate of radiographic subsidence. 5
We have transitioned to performing TL corpectomy almost exclusively through a minimally invasive approach, regardless of etiology. Consequently, there is no open corpectomy cohort for direct comparison, which is one of the weaknesses of this study. In fact, most published studies on this topic are case series.5,9-11,15 As demonstrated in this study and other studies, there was noticeable improvement in VAS score postoperatively.9,14,15 Other studies have also documented improvement in neurological function,5,13 Oswestry Disability Index, 15 lumbar lordosis, 11 and kyphosis angle. 14 We identified only 1 comparative study between open and minimally invasive TL corpectomy. 13 In the mini-open group, the operative time, EBL, blood transfusion, and LOS from admission and surgery were significantly lower. The complication rates were similar between the two cohorts. 13
Conclusions
Corpectomy and reconstruction of the TL spine for tumors, infections, traumas, or calcified disc herniations is feasible and safe using an MIS lateral retropleural or retroperitoneal approach. Similar to prior studies, we in general have seen a decrease in operative time, EBL, and perioperative complications compared with standard open corpectomy procedures. Additionally, no access surgeon was required for exposure. Since this is a relatively new technique, more studies are needed to compare the short- and long-term radiographic and clinical outcomes between minimally invasive versus open corpectomy of the TL spine.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Hai Le, MD  https://orcid.org/0000-0002-9111-9060
https://orcid.org/0000-0002-9111-9060
Eileen Phan, BA  https://orcid.org/0000-0002-3770-2626
https://orcid.org/0000-0002-3770-2626
References
- 1.D’Aliberti G, Talamonti G, Villa F, et al. Anterior approach to thoracic and lumbar spine lesions: results in 145 consecutive cases. J Neurosurg Spine. 2008;9:466–482. [DOI] [PubMed] [Google Scholar]
- 2.Landreneau RJ, Hazelrigg SR, Mack MJ, et al. Postoperative pain-related morbidity: video-assisted thoracic surgery versus thoracotomy. Ann Thorac Surg. 1993;56:1285–1289. [DOI] [PubMed] [Google Scholar]
- 3.Faciszewski T, Winter RB, Lonstein JE, Denis F, Johnson L.The surgical and medical perioperative complications of anterior spinal fusion surgery in the thoracic and lumbar spine in adults. A review of 1223 procedures. Spine (Phila Pa 1976). 1995;20:1592–1599. [DOI] [PubMed] [Google Scholar]
- 4.Kim YB, Lenke LG, Kim YJ, et al. The morbidity of an anterior thoracolumbar approach: adult spinal deformity patients with greater than five-year follow-up. Spine (Phila Pa 1976). 2009;34:822–826. [DOI] [PubMed] [Google Scholar]
- 5.Smith WD, Dakwar E, Le TV, Christian G, Serrano S, Uribe JS. Minimally invasive surgery for traumatic spinal pathologies: a mini-open, lateral approach in the thoracic and lumbar spine. Spine (Phila Pa 1976). 2010;35(26 suppl):S338–S346. [DOI] [PubMed] [Google Scholar]
- 6.Javidan Y, Hurley RK. Minimally invasive lateral approach to thoracic and lumbar spine: for discectomy and corpectomy for trauma, tumor, infection, and deformity. Oper Tech Orthop. 2019;29:1–14. [Google Scholar]
- 7.Uribe JS, Dakwar E, Cardona RF, Vale FL. Minimally invasive lateral retropleural thoracolumbar approach: cadaveric feasibility study and report of 4 clinical cases. Neurosurgery. 2011;68(1 suppl operative):32–39. [DOI] [PubMed] [Google Scholar]
- 8.Scheufler KM. Technique and clinical results of minimally invasive reconstruction and stabilization of the thoracic and thoracolumbar spine with expandable cages and ventrolateral plate fixation. Neurosurgery. 2007;61:798–809. [DOI] [PubMed] [Google Scholar]
- 9.Khan SN, Chat T, Hoskins JA, Pelton M, Singh K. Minimally invasive thoracolumbar corpectomy and reconstruction. Orthopaedics. 2012;35:e74–e79. [DOI] [PubMed] [Google Scholar]
- 10.Baaj AA, Dakwar E, Le TV, et al. Complications of the mini-open anterolateral approach to the thoracolumbar spine. J Clin Neurosci. 2012;19:1265–1267. [DOI] [PubMed] [Google Scholar]
- 11.Theologis AA, Tabaraee E, Toogood P, et al. Anterior corpectomy via the mini-open, extreme lateral, transpsoas approach combined with short-segment posterior fixation for single-level traumatic lumbar burst fractures: analysis of health-related quality of life outcomes and patient satisfaction. J Neurosurg Spine. 2016;24:60–68. [DOI] [PubMed] [Google Scholar]
- 12.Singh K, Tabaree E, Ahn J, et al. A comparison of surgical outcomes between minimally invasive and open thoracolumbar corpectomy: a minimum of two-year follow-up. Spine J. 2015;15:S260–S261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sulaiman OAR, Garces J, Mathkour M, et al. Mini-open thoracolumbar corpectomy: perioperative outcomes and hospital cost analysis compared with open corpectomy. World Neurosurg. 2017;99:295–301. [DOI] [PubMed] [Google Scholar]
- 14.Yu JYH, Fridley J, Gokaslan Z, Telfeian A, Oyelese AA. Minimally invasive thoracolumbar corpectomy and stabilization for unstable burst fractures using intraoperative computed tomography and computer-assisted spinal navigation. World Neurosurg. 2019;122:e1266–e1274. [DOI] [PubMed] [Google Scholar]
- 15.Doria C, Zachos A, Muresu F, Leali PT. The corpectomy using minimally invasive access in thoracolumbar fractures. Orthop Muscul Syst. 2012;1:1–3. [Google Scholar]