Abstract
Study Design:
Scoping review.
Objectives:
To identify a practical and reproducible approach to organize Quality of Care Indicators (QoCI) in individuals with traumatic spinal cord injury (TSCI).
Methods:
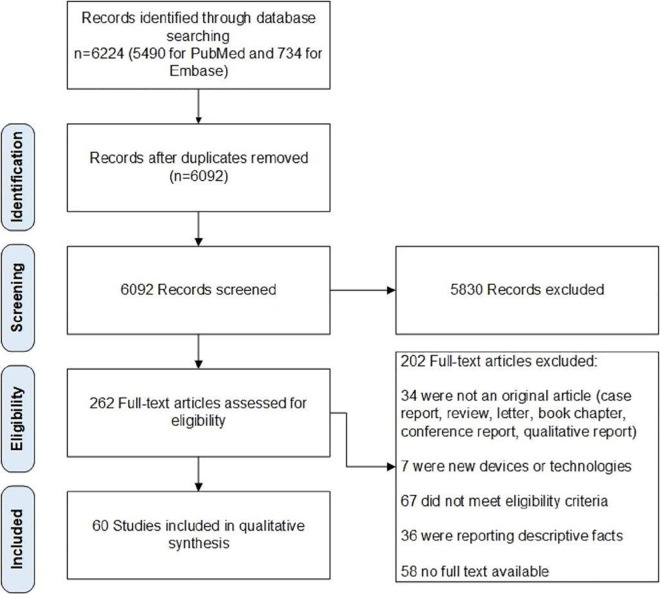
A comprehensive literature review was conducted in the Cochrane Central Register of Controlled Trials (CENTRAL) (Date: May 2018), MEDLINE (1946 to May 2018), and EMBASE (1974 to May 2018). Two independent reviewers screened 6092 records and included 262 full texts, among which 60 studies were included for qualitative analysis. We included studies, with no language restriction, containing at least 1 quality of care indicator for individuals with traumatic spinal cord injury. Each potential indicator was evaluated in an online, focused group discussion to define its categorization (healthcare system structure, medical process, and individuals with Traumatic Spinal Cord Injury related outcomes), definition, survey options, and scale.
Results:
A total of 87 indicators were identified from 60 studies screened using our eligibility criteria. We defined each indicator. Out of 87 indicators, 37 appraised the healthcare system structure, 30 evaluated medical processes, and 20 included individuals with TSCI related outcomes. The healthcare system structure included the impact of the cost of hospitalization and rehabilitation, as well as staff and patient perception of treatment. The medical processes included targeting physical activities for improvement of health-related outcomes and complications. Changes in motor score, functional independence, and readmission rates were reported as individuals with TSCI-related outcomes indicators.
Conclusion:
Indicators of quality of care in the management of individuals with TSCI are important for health policy strategists to standardize healthcare assessment, for clinicians to improve care, and for data collection efforts including registries.
Keywords: quality indicators, health care, spinal cord injuries, Iran, review, quality of health care, registries, health policy
Introduction
Traumatic spinal cord injury (TSCI) has an annual incidence of 40-80 per million people. About 90% of these cases in under-developed countries are caused by external factors such as motor vehicle accidents, falls, or sports-related activities. 1 An individual with TSCI can experience a variety of acute and chronic complications affecting their quality of life. To improve quality of care, healthcare systems have recently attempted to broaden access to care in addition to improving the care delivered. Studies identifying the quality of care for individuals with TSCI are rare and most of them are based on national registries.
To maximize outcomes following TSCI, timely access to a specialized, patient-centered, and evidence-based care is mandatory. A review of the World Health Organization 2 and other national and international databases demonstrate large differences across countries in the TSCI supply-demand relationship. 1 Interestingly, low- and middle-income countries tended to report less availability of all kinds of resources despite greater need. 3 To address this challenge, the WHO and the International Spinal Cord Society (ISCoS), in a collaborative effort to comprehensively map healthcare, social services, and policy requirements, developed evidence-based recommendations to address these needs based on income level. 4 However, we do not have evidence regarding the current adherence of different countries to these recommendations or improvement by different healthcare system interventions. The former is ongoing by the recent Learning Health System-International SCI Survey (LHS-InSCI) initiative, 5 but the latter requires a robust tool to monitor SCI care in different parts of the world.
Well-defined and validated Quality of Care Indicators (QoCI) can help improve TSCI care by establishing parameters that clinicians, healthcare managers and policymakers can monitor and report. These indicators must be based on evidence and experiences reflecting the standard of care. 6 In the present study, we reviewed the literature to summarize QoCI in individuals with TSCI into 3 groups: 1) healthcare system structure, 2) medical processes, and 3) individuals with traumatic spinal cord injury (TSCI)-related outcomes.
Method
Protocol and Registration
Our protocol included the Preferred Reporting Items for Systematic Reviews and Meta-Analysis protocol for scoping reviews.7,8 The PRISMA chart of this study is also available in Figure 1.
Figure 1.
Flowchart of studies excluded and included for this study.
Eligibility Criteria
We included studies with at least 1 QoC indicator to evaluate patients with TSCI without time and language limitations. We excluded case series with less than 10 cases, as well as animal studies. We excluded studies with new technologic instruments and devices (such as robotic-assistance devices or novel types of wheelchairs), as it was difficult to measure their impact and impractical for worldwide application.
Data Sources
To identify relevant studies, a search was done through the following databases: Cochrane Central Registry of Controlled Trials (CENTRAL) (Date: May 2018), MEDLINE (1946 to May 2018) and EMBASE (1974 to May 2018).
Selection of Sources of Evidence
In the first phase of screening, 2 authors independently screened related study titles and abstracts. After examining the discrepancies between the 2 teams, the second phase included full text screening of the included studies. The third stage resolved any potential discrepancy regarding the eligibility of studies through discussion and by the decision of a third review author. Then, based on the nature of indicators, we developed 3 categories: healthcare system structure, medical processes, and individuals with TSCI related outcomes. The same categorization was used in another national study. 9
Data Charting Process and Data Items
Four review authors independently proceeded with data extraction from included studies and entered the data in standardized data collection forms. Each potential indicator was evaluated in an online, focused group discussion to define its categorization (healthcare system structure, medical process, and individuals with Traumatic Spinal Cord Injury (TSCI) related outcomes), definition, survey options (e.g. types of questionnaire, data registries, etc.), and scale (e.g. percentage, day, hour, dollar, etc.), as well as reproducibility across various healthcare systems.
Results
The database search resulted in 6092 records. After screening relevant titles and abstracts, 262 records were included for further assessment. Full-text review resulted in 60 studies for evidence synthesis. Out of 60 studies, the main source of data collection of the 2 studies was national data registries. There were 21,574 cases from 60 studies. We identified 87 indicators from 60 studies, among which 37 indicators were associated with healthcare system structure (Table 1).
Table 1.
Healthcare System Structure Indicators.
| No. | INDICATOR | Definition | Survey Option | Scale | Ref |
|---|---|---|---|---|---|
| Cost | |||||
| 1 | Median Cost of healthcare services in the year following SCI | Direct medical cost of SCI in the year following SCI | Questionnaire (Patients, Physician, & Caregiver) | Dollar | 10 |
| 2 | Acute hospital charges | Direct medical cost from hospital admission to discharge | Health system records | Dollar | 11 |
| 3 | Rehabilitation care costs | Direct rehabilitation cost in the year following SCI | Questionnaire (Patients, Physician, & Caregiver) | Dollar | 12 |
| 4 | Monitoring and addressing financial issues related to SCI | General financial status of SCI patients based on residence status or ability to quickly obtain up to 1200 US dollars | Swedish Annual Level-of-Living survey | General financial statusA | 13 |
| Infrastructure | |||||
| 5 | Rate of treatment outside health region of residence | Whether the patient who is treated outside of their residential area is treated in a spine/trauma center or a non-trauma center B | Questionnaire (Patients, Caregiver, & Health system record) | Percentage | 1,14 |
| 6 | Number of specialized rehabilitation centers | Regional number of private and non-private centers specializing in SCI | Health system records | Private or non-private center | 15 |
| 7 | TSCI surgery volume of the hospital | Hospitals were classified by the number of annual TSCI admissions and TSCI-related surgical procedures | Health system records | Number of admissions | 16 |
| 8 | Frequency of patient with access to domestic adaptations and outdoor transportation amenities | Measure of availability of domestic adaptationsC | Social system records | PercentageD | 17 |
| Education | |||||
| 9 | The number of training courses for SCI nurses in managing interpersonal interactions | Weekly meetings with rehabilitation staff to discuss problematic patient interaction | Questionnaire (nurse) | Hours/month | 18 |
| 10 | Number of patient education programs | Discharge appointments with a trained nurse | Questionnaire (patient) | Hours/month | 14 |
| 11 | Number of emergency care providers’ education toward patients’ quality of life after spinal cord injury (SCI) | Hours of training for paramedics for SCI patient care in emergency cases | Questionnaire (physicians) | Hours/month | 19 |
| 12 | Usage of Coping Inventory of Stressful Situations/patient/year | Response to difficult, stressful, or upsetting situation | Questionnaire (patient) | Five-point Likert-type rating scale | 20 |
| Time | |||||
| 13 | Length of hospital stay | Number of days the patient initially was hospitalized after first injury | Health system records | Day | 1,14,15,21-23 |
| 14 | Inpatient rehabilitation length of stay | Number of days stable and unstable patient spent in rehabilitation | Health system records | Day | 12,21 |
| 15 | Median Hours of direct care per patient (for nursing and all health care therapists) | Hours of direct care/per patient for nursing and other health care therapists combined | Health system records | Minute/week | 12 |
| 16 | Mean stay in the ICU | Number of days patient spent in Intensive Care Unit (ICU) | Health system records | Day | 1,24 |
| 17 | Mean stay in the IRCU | Length of stay for patients in the IRCU (Intermediate Respiratory Care Unit) | Health system records | Day | 24 |
| 18 | Median time to visit and treatment | Time SCI patients spent in a clinic waiting for their appointment for a visit or a pre-scheduled procedure | Health system records | Hours/day | 10 |
| 19 | Median Time: injury to surgery | Time from initial injury to the time patient enter the operation room | Health system records | Hours | 21,25-27 |
| 20 | Median time in the trauma emergency department | Time spent to stabilization in the emergency department | Health system records | Minutes | 21,28 |
| 21 | Pre-hospital time (transfer time) | Time spent from scene of trauma to hospital | Health system records | Minutes | 28 |
| 22 | Median time in secondary care center before transfer to a spine center | Time spent in a secondary care center before being transferred to a spine center for treatment | Health system records | Minutes | 26,28 |
| 23 | Median time between onset of SCI and rehabilitation | Median time from initial injury to rehabilitation | Health system records | Days | 10,22,29 |
| Patient satisfaction | |||||
| 24 | Patient satisfaction with follow-up care | Items involved quality, continuity, and coordination of care | Questionnaire (patient) | PercentageE | 30 |
| 25 | Satisfaction with availability of SCI-related medical care according to region | Patient satisfaction with the availability of SCI-related medical care services within and outside of the region in which they reside | Questionnaire (patient) | Likert scale | 10 |
| 26 | Satisfaction of SCI-related therapy according to region | Satisfaction with care provided by general practitioners, home care professionals available in the region | Questionnaire(patient) | Likert scale | 10 |
| 27 | Satisfaction with care for SCI-related health conditions according to region | Satisfaction with the availability of SCI-related therapy in the region in which individuals reside. | Questionnaire (patient) | Percentage satisfied | 10 |
| 28 | Patient satisfaction with care | Patient experience of hospital stay, rehabilitation, and new life situation | Patient interview | Patient access | 31 |
| 29 | Patient satisfaction with primary care and rehabilitation | Health Care Questionnaire (HCQ): a compilation of 2 published measures: The Primary Care Questionnaire and patient satisfaction with the Health Care Provider Scale (PSHCPS) | Patient interview | Percent | 32 |
| Others | |||||
| 30 | Median health care utilization post-discharge | 1. Unscheduled emergency department visits within 1 year; 2. Unscheduled hospital readmissions within 1 year are considered as utilization | Health system records | Number of visits | 1 |
| 31 | Number of promotional programs for physical activity/patient/year | Number of promotional programs targeted for encouraging individual with SCI to start a form of physical activity F | Questionnaire (patient) | Min./week | 33 |
| 32 | Number of social work and case management services that an individual with traumatic SCI receives during acute inpatient rehabilitation | Social work /case management services for each patient during the acute phase of rehabilitation G | Health system records | Hours/week | 34 |
| 33 | Spinal cord injury rehabilitation staff perceptions of individuals with SCI spinal cord -related problems | Study-specific questionnaire containing 45 Spinal Cord Lesion 35 related problems covering 6 problem areas: somatic symptoms, functional limitations, role problems, family-related problems, psychosocial problems, and emotional problems. H | Questionnaire (patients &rehabilitation staff) | The response scale had 6 grades, ranging from “not at all” to “very much.” Higher scores indicate a higher degree of perceived problems. | 36 |
| 34 | Spinal cord injury rehabilitation staff perceptions of individuals with spinal cord injury coping efforts | Coping activities were assessed by a self-report 47-item questionnaire covering 8 aspects of coping: self-trust, problem focusing, acceptance, fatalism, resignation, protest, minimization, and social trust. | Questionnaire patients & rehabilitation staff | 6-step response scale | 36 |
| 35 | Spinal cord Injury rehabilitation staff perceptions of SCI patients’ physical and mental well-being | The staff is asked to define their perception of mental and physical well-being and the answers were compared to each other | Questionnaire patients &rehabilitation staff | 6-step scale | 36 |
| 36 | Screening and addressing specific prescription misuse | Screening misuse in patients prescribed drugs by checking pharmacy database and adapting it to prescription | Health system records | Yes/No | 37 |
| 37 | Assessment of the health-related quality of life in caregivers (relatives of the patient) | Measuring the quality of life in SCI patients’ caregivers | Questionnaire (caregiver) | 0-100 | 38 |
Notes:
A: Residence: condominium vs house, Residence: rent vs own, Financial problems, inability to raise 1200 USD in a short period of time.
B: This refers to the inability of the patient to obtain adequate care within their local geographic region, and is therefore required to visit a specialized SCI center for treatment.
C: Domestic adaptions include (1) ramp to front door; removed thresholds; widening of doors; elevator to upper floor; adapted kitchen, toilet, and bathroom; and an annex to the house; (2) wheelchairs (manual, electrical, or other wheelchairs; and (3) external transport, such as an adapted car.
D: Patients were divided into complete and incomplete tetraplegia and paraplegia, and measured by percent who have access to a ramp to the front door; lowered thresholds; doors; an elevator; an adapted kitchen, toilet, and bathroom; and an annex to the house.
E: Items in this questionnaire were judged as “open for improvement.” Patients who believed items could be improved upon were reported as a percentage in each field, and compared between transmural and traditional follow-up plan.
F: How many hours per week a social worker has spent on a specific problem a patient presented during his acute phase of hospital stay.
G: Staff in a SCI center was asked to answer what challenges a SCI patient face after his injury, the patient was asked the same thing, and the compatibility of the answers is compared.
H: Like case E, the same thing was done this time about coping not the challenges.
Healthcare system structure indicators assessed 6 main domains including:
- Cost: which evaluates 2 classes:
- Medical care cost, including healthcare service, acute hospitalization charge, and rehabilitation care cost.
- Financial ramifications for the patient related to SCI, e.g. loss of income, etc.
Infrastructure: which evaluates infrastructure specialized for SCI care, such as number of SCI rehabilitation centers, availability and access to domestic adaptations and outdoor transportation amenities, etc.
Education: which evaluates educational programs for physicians, patients, and caregivers.
- Time: which evaluates 2 main classes including:
- Length of stay in the hospital, ICU, IRCU, rehabilitation unit.
- Time cost for different processes: pre-hospital transfer time, Emergency Department (ED) arrival to first visit, injury to surgery, etc.
- Patient Satisfaction: which evaluates patient-centered point of view in the SCI care process.
- Others: not classified into other categories.
The number of indicators for the medical process and individuals with TSCI related outcomes were 30 and 20, respectively. The healthcare system structure indicators included: the effects of cost of the acute phase hospitalization and rehabilitation, facility costs (including MRI, CT scan, and staff- and patient-perception of treatment). The medical process indicators included physical activity and rehabilitation, complication rates, and overall treatment including every healthcare professional involved in the patient treatment. Furthermore, telemedicine was identified as a new form of care and a potential indicator (Table 2).
Table 2.
Medical Process Indicators.
| No. | Indicator | Definition | Survey Option | Scale | Ref. |
|---|---|---|---|---|---|
| Adherence to standard SCI care guideline | |||||
| 1 | CIC(Clean Intermittent Catheterization) education rate) | Caregivers CIC were approached when attending the pediatric urology outpatient clinic of hospital | Questionnaire (patient) | Time of education reported in minutes | 39 |
| 2 | Use of MRI in the diagnostic plan | MRI as an imaging modality in the diagnostic plan for the patients. | Health system records | [+,-] | 40 |
| 3 | Rate of out-of-hospital immobilization of the patients | Practice of spinal immobilization in prehospital and early hospital care for reducing secondary neurological damage to the spinal cord | Health system records/Questionnaire (patient) | [+,-] | 26 |
| 4 | Rate of administration of methylprednisolone | Early administration of methylprednisolone for isolated traumatic spinal cord injury by hospital data | Health system records | [+,-] | 26 |
| 5 | Consultation rate by orthopedic surgeon or neurosurgeon | Patients in trauma centers consulted by an orthopedic surgeon or a neurosurgeon in the early stages of treatment | Health system records | Hospitalized in a trauma center compared to a non-trauma center | 1 |
| 6 | Implementation rate of physical activity guideline (PAG) | Whether a PAG is followed during patient physical fitness training sessions | Questionnaire (physicians) | Adherence was calculated based on the percentage of a maximum of 32 sessions (2x per week for 16 weeks). | 41 |
| 7 | Adherence rate of physical activity guideline | Rate of adherence to a PAG for physical fitness of individual with TSCI | Questionnaire (patient) | Total number of sessions completed | 41 |
| 8 | The implementation rate of early VTE prophylaxis | Mechanical and chemical modalities for adult venous thromboembolism prophylaxis | Questionnaire (physicians) | Patients are given 5000 units heparin subcutaneously 3 times daily | 11 |
| 9 | Prescription rate of suitable self-care equipment by therapist before discharge | Prescription rate of self-care equipment before discharge and whether it is double-checked(by reviewing clinician progress notes and orders) before patient discharge | Health system records | Yes/No | 42 |
| Screening of adverse events | |||||
| 10 | Screenings of prescription compliance/patient/year | Screening of patients for medication consumption to find potential adverse reactions affecting hospital stay length. | Questionnaire (patient) | [+,-] | 43 |
| 11 | Pressure ulcer prevention rate | Providing structured and individualized patient education for pressure ulcer prevention; as part of the pan-Canadian SCI Knowledge Mobilization Network | Questionnaire (physicians) | Staff competency, organizational support, and leadership | 44 |
| 12 | Secondary complication rate (after discharge) | Secondary complication rate after discharge from hospital, measured by a questionnaire | Questionnaire (patient) | 26 secondary complication (in the article)a | 45 |
| Patient medical assessment frequency | |||||
| 13 | Prevalence of pressure sore infections | The number and duration of re-admissions to the hospital and rehabilitation center due to pressure sores | Questionnaire (patient) | The prevalence of pressure sores [4-15] | 30 |
| 14 | Number of physical activity assessments/patient/year | Physical activity of patients are self-reported and measured by Leisure Time Physical Activity Questionnaire for People with Spinal Cord Injury (LTPAQ-SCI) in the past 7 days | Questionnaire (patient) | Minutes/week | 33 |
| Number of assessments for Spinal Cord Independence Measure III (SCIM III) score (self-care, respiration and sphincter management, mobility) | Questionnaire (patient) | Score: Self-care subtotal (0-20), Respiration and Sphincter management subtotal (0-40), Mobility subtotal (0-40) | 40 | ||
| Physical activity of patients who use manual wheelchairs, as measured by Physical Activity Recall Assessment for People with SCI (PARA-SCI) semi-structured interview. | Questionnaire (patient) | Three categories of physical activity: leisure-time physical activity, lifestyle activity, and cumulative activity | 46 | ||
| 15 | Number of UTI screenings/patient/year | Infection in any parts of urinary tract | Questionnaire (patient) | Number/year | 39 |
| 16 | Number of UTI microorganism susceptibility/patient/year | Urine samples were collected for urine analysis and urine culture performance right after initial interview | Questionnaire (physicians) | Urine culture, colony count, type of organisms and antibiograms | 47 |
| 17 | Number of Screening of modifiable comorbidities/patient/ year | Screening of medical comorbidities | Questionnaire (patient) | [+,-] | 43 |
| 18 | Number of Screening of modifiable hazardous behavior/patient/year | Screening of modifiable hazardous behavior/patient/year: Substance use/withdrawal (Alcohol, drug, withdrawal) This assessed behavior that was gained after TSCI. | Questionnaire (patient) | [+,-] | 43 |
| 19 | Number of Screening of Psychiatric conditions/patient/year | Screening of psychiatric conditions (post injury)/patient/year by the medical record, questionnaire, interview | Questionnaire (patient) | [+,-] | 43 |
| 20 | Number of screening for depression/patient/year | Screening incidence of depression among SCI patients by Patient Health Questionnaire-9 (PHQ-9) in each yearB | Questionnaire (patient) | A cutoff of 11 yields optimal sensitivity (1.0) and specificity (.84) for identifying Major Depressive Disorders (MDDs) | 48 |
| 21 | Barthel Index (functional score) on admission | Calculating Barthel Index score during hospitalization (The Barthel Index for Activities of Daily Living (ADL) assesses functional independence). | Health system records | Feeding, bathing, grooming, dressing, bowels, bladder, toilet use, transfers (bed to chair & back), mobility (on level surfaces), stairs | 22 |
| 22 | Median time spent on bowel care per week | Median time in a week spent on bowel care (time documented before and after stoma) | Questionnaire (patient) | Hours | 49 |
| 23 | Number of pain assessments/patient/year | The Numeric Pain Rating Scale (NPRS) used to assess degree of back pain for each patient | Questionnaire (patient) | [0-10] | 50 |
| 24 | Number of fatigue assessments/patient/year | The Profile of Mood States-Brief Form (POMS-Brief) [26] was used to assess affective mood states. | Questionnaire (patient) | [0-120] | 50 |
| 25 | Monitoring program for psychometric performance | WHO Quality of Life-BREF (WHOQOL-BREF) used for monitoring psychometric performance | Questionnaire (patient) | A questionnaire with 100 items | 51 |
| 26 | Number of Psychological assessments/patient/year | Mood and psychopathology were measured by the PAI (Personality Assessment Inventory) during a 2-6 year period. | Questionnaire (Patient) | A 344-item self-reported instrument | 52 |
| SF-36 Mental Health scale (SF-36 MH) used for psychological assessment of patient during 2-6 year period. | Questionnaire (Patient) | The SF-36 consists of eight scaled scores, which are the weighted sums of the questions in their section | |||
| Positive Affect and Negative Affect Scale53 | Questionnaire (Patient) | Likert scale | 54 | ||
| 26 | Number of Psychological assessments/patient/year | Mood and psychopathology were measured by the PAI (Personality Assessment Inventory) during a 2-6 year period. | Questionnaire (patient) | A 344-item self-reported instrument | 52 |
| SF-36 Mental Health scale (SF-36 MH) used for psychological assessment of patient during 2-6 year period. | Questionnaire (patient) | The SF-36 consists of eight scaled scores, which are the weighted sums of the questions in their section | 52 | ||
| Positive Affect and Negative Affect Scale 53 | Questionnaire (patient) | Likert scale | 54 | ||
| Swedish Annual Level-of-Living Survey used for monitoring psychometric performance of the patients. | Questionnaire (patient) | Swedish Annual Level-of-Living Survey | 13 | ||
| Others | |||||
| 27 | Telemedicine usage rate in patients with SCI pre hospital clinical assessment rate of SCI and spine fracture by Emergency Medical Services (EMS) | Using telemedicine to report prehospital clinical data | Questionnaire (physicians & patients) | Patients signs and symptoms collected by EMS providers | 55 |
| Upon arrival at the trauma scene, EMS providers assessed for neck pain/tenderness, altered mental status, history of loss of consciousness, drug/alcohol use, neurologic deficit, and other painful/distracting injury. The results were reported using telemedicine. | Questionnaire (physicians & patients) | Yes/no | 56 | ||
| 28 | Telemedicine usage rate in patients with SCI | Using telemedicine to assess functional status (measured by Functional Independence Measure (FIM) and Spinal Cord Independence Measure II (SCIM II)) 10 days before discharge and 6 months after discharge | Questionnaire (physicians and patients) | Self-care/respiration and sphincter management/mobility (room and toilet)/mobility (indoors and outdoors) | 57 |
| Using telemedicine to find and report complications 6 and12 months post discharge | Questionnaire (physicians and patients) | Included pressure ulcers, urinary tract infections, problems associated with urinary catheters, pulmonary infections, fever, pain, autonomic dysreflexia, and deep vein thrombosis. | 57 | ||
| Annual rate of using telemedicine to report patients satisfaction with the care they received 57 | Questionnaire (patients) | Questions were rated on an ordinal scale (0-10) | 57 | ||
| 29 | Implementation rate of locomotor training program | Patients received standardized locomotor training sessions, as established by Neuro Recovery Network (NRN) protocol, and were evaluated monthly for progress | Questionnaire (physicians) | Model Fit | 58 |
| 30 | Person-Centered Care (PCC) in the rehabilitation program | PCC implementation measured by 4 instruments: the Patient Activation Measure (PAM), the Patient Assessment of Chronic Illness Care (PACIC), the Global Practice Experience measure, and 5 Press-Ganey questions | Questionnaire (patient) | [+,-] | 59 |
NOTE:
a: Supplementary information regarding row 20 of this table is here.
Secondary condition includes: 1. Bladder regulation 2. Bowel regulation 3. Pain 4. Spasms 5. Sexuality 6. Pressure scores 7. Dependency 8. Edema 9. Handicap management 10. Increased weight 11. Facilities, equipment, and housing 12. Coping with handicap 13. Daily living activities 14. Excessive sweating 15. Functioning in non-adapted environments 16. Asking for help, being assertive 17. Contractures 18. Breathing/respirator 19. Relationships 20. Household activities 21. Work 22. Leisure-time activities 23. Heterotrophic ossification 24. Low blood pressure 25. Communication 26. Thrombosis.
B: Patient Health Questionnaire (PHQ-9): Consists of 9 questions: 1. Little interest or pleasure in doing things 2. Feeling down, depressed, or helpless 3. Trouble falling or staying asleep, or sleeping too much 4. Feeling tired or having little energy 5. Poor appetite or over eating 6. Feeling bad about yourself—or that you are a failure or have let yourself or your family down 7. Trouble concentrating on things, such as reading the newspaper or watching television 8. Moving or speaking so slowly that other people could have noticed. Or the opposite—being so fidgety or restless that you have been moving around a lot more than usual 9.Thoughts that you would be better off dead, or of hurting yourself.
Medical process indicators assessed 4 main domains, which are:
Adherence to standard SCI care guideline: Venous Thromboembolism (VTE) prophylaxis, prehospital immobilization, use of MRI, use of steroid, CIC training, etc.
-
Screening of adverse events: which evaluates 2 main classes:
ˆ Medical process complications, such as prescription complications
ˆ SCI complications, such as bed sores
Patient medical assessment frequency: including physical activity, urinary tract infection (UTI) screening, etc.
Others: not classified into other categories.
The third table reports the indicators of individuals with TSCI-related outcomes. Measuring tools such as American Spinal Injury Association (ASIA) score, functional independence Measure (FIM), Oswestry disability index (ODI), Spinal Cord Independence Measure II (SCIM II), Self-efficacy improvement rate by Moorong Self-Efficacy Scale (MSES), Canadian Occupational Performance Measure (COPM), and Barthel Index were used to report functional independence outcomes. Discharge efficiency and readmission rate are also part of outcome measuring tools for individuals with TSCI (Table 3).
Table 3.
Individuals With TSCI-Related Outcomes.
| No. | Indicator | Definition ± tools for measure | Survey Option | Scale | Ref. |
|---|---|---|---|---|---|
| Medical Improvement | |||||
| 1 | Total change in motor score | Motor score measured with ASIA score employing neurological examinations at administration and discharge rehabilitation. Total change from each step is reported. | Patient physical examination | Scored on a 5-point ordinal scale from A (complete injury) to E (Normal sensory and motor function) | 21 |
| 2 | Functional Independence Measure (FIM) after discharge or during rehabilitation | FIM after discharge or during rehabilitation a | Questionnaire (patient) | 18-item of physical, psychological, and social function. Each domain is scored on a Likert-type scale | 15,12,60-62 |
| Oswestry Disability Index for Low Back Pain (ODI) Version 2.0 was reported for each patient after discharge.(ODI Version 2.0 consists of pain Intensity, personal care, lifting, walking, sitting, standing, sleeping, sex life, social life, and traveling) | Questionnaire (patient) | ODI scale | 50 | ||
| Spinal Cord Independence Measure II (SCIM II) during a 1-year follow-up examination after SCI | Questionnaire (patient) | SCIM II scale | 63 | ||
| Self-efficacy improvement rate using Moorong Self-Efficacy Scale (MSES) during rehabilitation | Questionnaire (patient) | Seven-point Likert scale for each subscale b | 20 | ||
| Canadian Occupational Performance Measure (COPM) and FIM during rehabilitation | Questionnaire (patient) | COPM: scale of 1-10 and FIM: Likert scale (1-7) | 64 | ||
| Barthel Index (functional score) used for measuring functional independence after discharge. | Health system records | Feeding, bathing, grooming, dressing, bowels, bladder, toilet use, transfers (bed to chair and back), mobility (on level surfaces), stairs scoring 0-100 | 22 | ||
| 3 | Functional Recovery Rate | SCIM II used to measure functional recovery rate | Physical exam | SCIM II | 63 |
| 4 | Motor and sensory recovery rate (before and after surgery) | Motor and sensory function is measured on a scale of A to E before and after surgery. The difference between these 2 scores represent the recovery rate of the patient. | Patient physical examination | Scored on a 5-point ordinal scale from A (complete injury) to E (Normal sensory and motor function) | 65 |
| 5 | Urinary function improvement after surgery | Urinary function of patients based on urinary sensation and frequency of using catheterization. | Questionnaire (patient) | A scale from no urinary sensation, intermittently dependent on catheterization, and completely dependent on catheterization. | 65 |
| 6 | Stoma formationh | Colostomy formation in patients with bowel management problems | Health system records | Number of patients | 49 |
| Complication Monitoring | |||||
| 7 | Re-admission rate for complications | Number and duration of re-admissions to hospital and rehabilitation center in the first year after discharge. | Questionnaire (patient) | Number of re-admissions and inpatient days | 30 |
| 8 | Discharge efficiency | Number of readmissions in 1 month/number of discharges | Health system records | Readmission/discharge | 14 |
| 9 | Mortality rate | Number of deaths after spine surgery due to related complications. | Health system records | Number | 11 |
| 10 | Adverse events rate | Spine Adverse Events Severity System (SAVES)d used for collecting adverse events reported post-operation such as instrumentation failure, nonunion, and infection. | Questionnaire (physicians) | Yes/No | 23 |
| 11 | Rate of in-hospital adverse events | Spine adverse events severity system (SAVES) used for reporting adverse events in the hospital setting such as pulmonary thromboembolism and DVT. | Health system records | Adverse events rate | 23 |
| Quality of life improvement | |||||
| 12 | Health-related quality of life assessment | SF-36 measures both mental and physical health related quality of life | Questionnaire (patient) | SF-36 Mental and Physical Health sub-scores | 20,23,38,66 |
| World Health Organization Quality of Life-BREF (WHOQOL-BREF) used to measure health related quality of life. | Questionnaire (patient) | 100-item questionnaire | 67 | ||
| SF12v2 consisting of 2 summary outcomes for physical health and mental health.e | Questionnaire (patient) | Summary of eight SF-36 sections | 50 | ||
| 13 | Quality of life improvement rate after rehabilitation | WHOQOL-BREF used to measure the improvement in quality of life after rehabilitation. | Questionnaire (patient) | 100-item questionnaire | 68 |
| Others | |||||
| 14 | Knowing postoperative complication rate | Explaining post-operative complications based on International Classification of Diseases, Ninth Revision (ICD-9)c to patients before surgery. | Questionnaire (patient) | Incidence (0-100) | 1,11 |
| Psychological Improvement | |||||
| 15 | Social participation after TSCI | Craig Handicap and Assessment-Reporting Technique 69 fused for reporting social participation after TSCI. | Questionnaire (patient) | Score [0-100] | 60 |
| 16 | Frequency of behavioral incident per month | Behavioral or “critical” incidents | clinicians | Number of incidents | 12 |
| 17 | Social integration rate after hospital discharge | The Community Integration Questionnaire 70 used for reporting social integration of patients after their discharge from the hospital. | Questionnaire (patient) | 13-item measure of the lack of handicap | 52 |
| Monitoring and addressing social participation and autonomy by Impact on Participation and Autonomy (IPA) | Questionnaire (patient) | 32 item questionnaire | 20 | ||
| 18 | Identifying well-being g | The Community Reintegration Outpatient (CROP) Service used to determine patient well-being | Questionnaire (patient) | Patient self-reporting | 20 |
| Outcome Assessment Frequency | |||||
| 19 | Number of rehabilitations visits per year | Frequency of contact with caregivers in the last 12 months after discharge to present unmet care. | Health system records | Not at all/1-3 times a year/4-11 times a year/1-3 times a month/1-6 times a week/Daily | 45 |
| 20 | Number of walking ability assessments/patient/year | Lower extremity motor score assessment within the first month and at 3, 6 and 12 months after discharge | Questionnaire (patient) | 0 to 5 for motor grading for each neurological area | 71 |
| The Walking Index for Spinal Cord Injury (WISCI II) assessment within the first month and at 3, 6 and 12 months after discharge | Questionnaire (patient) | Level of most severe impairment (0) to least severe impairment (20) | 72 | ||
| 6 Minute Walking Test (6MWT) assessment within the first month and at 3, 6 and 12 months after discharge | Questionnaire (patient) | The distance a patient walks in 6 minutes | 72 | ||
| Ten-Meter Walking Test (10MWT) assessment within the first month and at 3, 6 and 12 months after discharge | Questionnaire (patient) | The distance a patient walks in 10 minutes | 72 | ||
| Standardized locomotor training sessions with monthly evaluation for progress | Questionnaire (patient) | Number of screenings for walking ability/patient/year | 58 | ||
Note:
a: A self-administered scale to examine the level of independence in activities of daily living, The Functional Independence Measure (FIM) is an 18-item of physical, psychological and social function. The tool is implemented to evaluate patient level of disability and changed inpatient condition after rehabilitation or medical intervention.
b: The total scale score is obtained by adding the individual item responses. For the factor or subscale scores; “Daily Activities / Instrumental Self-efficacy” (7 items: good health, work, accomplishing things, personal hygiene, persistence in learning things, fulfilling lifestyle, and household participation), “Social Functioning / Interpersonal Self-efficacy.”(8 items: maintaining contact, friends, family, relationships, unexpected problems, fulfilling lifestyle, leisure, accomplishing things, household participation).
c: Deep vein thrombosis/pulmonary embolism, pneumonia, pressure ulcer, urinary tract infection, autonomic dysreflexia, bowel complications, renal complications.
d: The SAVES consists of 14 intraoperative and 22 pre- or postoperative adverse events that are common in patients who undergo spinal procedures with an option to record “other” events not already specified.
e: The SF-12 Health Survey (SF-12) is a 12-item questionnaire used to assess generic health outcomes. It contains 12 subsets from SF-36 while covering the same eight domains that SF-36 covers which are physical functioning, role-physical, bodily pain, general health, vitality functioning, social functioning, role-emotional, and mental health.
f: Scale measuring physical independence, cognitive independence, social integration, mobility, occupation, and economic self-sufficiency.
h: The third part of this services identifies and develops a visual roadmap for improving coping, well-being, and overall self-management skills while reintegrating back into the community.
h: Weekly average time of bowel care decreased from 10.3 hours (range 3.5-45) before stoma formation to 1.9 hours (range 0.5-7.75) afterward (P = 0.0001, paired t-test). At any point, 18 patients reported a stoma gave them more independence and quality of life. 25 patients reported improvement. The effect of colostomy formation is also reported.
Indicators involving individuals with TSCI-related outcomes evaluated 6 main domains:
Medical Improvement: Functional Independence Measure, motor improvement, etc.
Complication Monitoring, e.g. mortality, readmission rate, and discharge efficiency.
Quality of Life Improvement, e.g. health-related quality of life assessment and quality of life improvement rate after rehabilitation.
Psychological Improvement, e.g. social participation after TSCI
Outcome Assessment Frequency: number of rehabilitation visits/year and number of walking ability assessments/patient/year.
Other
Discussion
In the present study, we summarized important QoCI indicators in individuals with TSCI. In the current literature, the main focus has been on developing QoCI by finding gaps in care in different phases of the care continuum and designing solutions for the healthcare system, whereas this study focuses on factors affecting the patients care across the TSCI continuum (i.e. from the time of injury through to the community). Examining care in 3 stages is a unique way to report indicators that to our knowledge has not been previously used. We assessed QoCI in terms of access to care and quality of care.
TSCI QoC indicators must cover the TSCI continuum to assist healthcare policymakers, clinicians, and health managers monitor and enhance care. Our study categorized QoC indicators into 3 groups to assist healthcare policymakers with understanding their relevance to care delivery. These groups were healthcare system structure indicators, medical process indicators, and indicators involving individuals with TSCI-related outcomes. Not only were these indicators important for finding gaps in current knowledge, but they also assisted in data collection and designing data registries.1,73 This study is a scoping review; therefore, the main focus was to identify key concepts of care for individuals with TSCI and provide evidence to inform clinicians, healthcare managers, and policymakers.
Healthcare System Structure
Cost of care as a healthcare system structure is a challenging indicator to assess accurately. Cost of care has been mentioned as an indicator for QoC, however hospital care is directly affected by hospital length of stay. 12 If cost of in-hospital care is solely considered as a QoC indicator, many inconsistencies may therefore arise. For instance, certain medications prescribed in the setting of TSCI can be costly compared to other alternatives. In these cases, the incremental cost-effectiveness ratio 74 should be used in cost-effectiveness analysis. This ratio can measure how effective a costly intervention can be in certain patient-specific situations.
The cost of care in this review identified 3 types: acute care costs, cost in the first year following TSCI, and cost of rehabilitation. The effect of costs on the quality of care is not straightforward and there is a need for further research as highlighted by this review. Length of stay is acquainted with better care, including better emotional and social support and also more improvement in FIM, in patients who have suffered from TSCI.15,22 Shortening the length of stay in acute phase could have positive impact on patient outcome while longer stay in a center specialized for TSCI rehabilitation have been shown to improve FIM of individuals to a greater degree.12,22 In other words, the patient benefit the most when staying less in the acute phase of hospitalization and spending more time in a center specialized for TSCI rehabilitation. SCI centers have facilities and specialized services for patients who have sustained a TSCI. In the post-traumatic setting, these rehabilitation centers are equipped to manage the patient from arrival to the emergency room until discharge. Education of patients and staff regarding the challenges and concerns of individuals with TSCI is also an indicator that can often be taken for granted. Patient satisfaction with their care is also an indicator measured at multiple phases and has different measures. These QoC measures help us assess the current situation of healthcare systems in responding adequately to TSCI and provide avenues for future improvements in patient outcomes.
Medical Processes
Medical process indicators mainly focused on screening common postoperative complications such as urinary tract infection, VTE, pressure injuries, and depression. Previous studies reported that urinary tract infections are the most common postoperative complication in patients with TSCI. Clean intermittent catheterization has been proven to reduce the incidence of UTIs and its further complications, such as sepsis in individuals with TSCI. 39 Physical activity and rehabilitation are also considered an essential part of a patient’s care. The use of telemedicine for managing complications and subsequent consultation is also reported to have an impact on a patient care. Patient functional score and psychomotor performance have been measured using a variety of different scales and performance scores.16,34,51,52 VTE prophylaxis at an early stage is an important indicator as well. Evidence-based medicine argues aggressive, early prophylaxis leads to reduced rates of VTE and pulmonary thromboembolism without an increased risk of an epidural hematoma. 11 Early consultation with a neurosurgeon and orthopedic surgeon for spinal cord decompression and spine stabilization was also suggested to increase the quality of care. 1
Individuals With TSCI-Related Outcomes
For measuring individuals with TSCI-related outcomes, the indicators mainly focused on the changes in motor score and functional recovery from initial visit to discharge. Characterizing patient well-being was captured through questionnaires and surveys. 20 An interesting indicator is the number of physician visits per year after discharge to evaluate outcome. Readmission after discharge, reoperation rates, and discharge efficiency (measured as the number of visits in the following month after discharge) were also considered as independent indicators.23,30,45
Future Directions
The identification of QoCI in patients with TSCI will help identify pitfalls in clinical data collection and data inclusion in SCI registries. Some of these indicators require resources to monitor over the long term, but the utility in improving future health care delivery outweighs these costs. Globally, developed and developing countries have healthcare systems that significantly differ from one another. Identifying QoCI could help standardize healthcare assessments for each country. Furthermore, these indicators could provide baseline elements for comprehensive QoC questionnaires to compare healthcare systems across the world. In areas where indicators measure similar concepts, a consensus process such as the Delphi method would help establish standards that can be used by all SCI centers.
Conclusion
This scoping review maps current literature and provides key concepts in the care of individuals with TSCI. These indicators are helpful in improving QoL of individuals with TSCI by providing improved care and enhanced clinical practice. The classification used in this study (healthcare system structure, medical process, and individuals with TSCI related outcomes) models the SCI continuum of care, and may be useful in further data collection efforts.
Supplemental Material
Supplemental Material, sj-docx-1-gsj-10.1177_2192568220981988 for Indicators of Quality of Care in Individuals With Traumatic Spinal Cord Injury: A Scoping Review by Sepehr Khosravi, Amirmahdi Khayyamfar, Milad Shemshadi, Masoud Pourghahramani Koltapeh, Mohsen Sadeghi-Naini, Zahra Ghodsi, Farhad Shokraneh, Mohadeseh Sarbaz Bardsiri, Pegah Derakhshan, Khalil Komlakh, Alex R. Vaccaro, Michael G. Fehlings, James D. Guest, Vanessa Noonan and Vafa Rahimi-Movaghar in Global Spine Journal
Footnotes
Competing Interest: None declared except Alex R Vaccaro (file attached).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval Number Is 97-02-38-323.: Scoping reviews do not directly access patient data, nor do they intervene in medical treatment course, but rather reviews other studies performed in this field. Hence, the ethical consideration is in the minimal risk category.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded and supported by Sina Trauma and Surgery Research Center, Tehran University of Medical Science (TUMS); Grant no. 97-02-38-39121 and approved by National Institute for Medical Research Development (NIMAD).
ORCID iD: Sepehr Khosravi, MS (Medical Student)  https://orcid.org/0000-0002-5372-0787
https://orcid.org/0000-0002-5372-0787
Amirmahdi Khayyamfar, MS (Medical Student)  https://orcid.org/0000-0001-9117-8207
https://orcid.org/0000-0001-9117-8207
Masoud Pourghahramani Koltapeh, MS (Medical Student)  https://orcid.org/0000-0001-8066-5739
https://orcid.org/0000-0001-8066-5739
Alex R. Vaccaro, MD, PhD, MBA  https://orcid.org/0000-0002-8073-0796
https://orcid.org/0000-0002-8073-0796
Michael G. Fehlings, MD, PhD, FRCSC, FACS  https://orcid.org/0000-0002-5722-6364
https://orcid.org/0000-0002-5722-6364
Vafa Rahimi-Movaghar, MD  https://orcid.org/0000-0001-7347-8767
https://orcid.org/0000-0001-7347-8767
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Guilcher SJ, Parsons D, Craven BC, Jaglal SB, Verrier M.Developing quality of care indicators for patients with traumatic and non-traumatic spinal cord injury (SCI): A feasibility study using administrative health data. J Spin Cord Med. 2015;38(6):765–776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wholey MH, Pugh DG, Bickel WH. Localized destructive lesions in rheumatoid spondylitis. Radiology. 1960;74:54–56. [DOI] [PubMed] [Google Scholar]
- 3.Gupta N, Castillo-Laborde C, Landry MD. Health-related rehabilitation services: assessing the global supply of and need for human resources. BMC Health Serv Res. 2011;11(1):276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bickenbach J, Officer A, Shakespeare T, von Groote P. World Health O, the International Spinal Cord S. International Perspectives on Spinal Cord Injury/Edited by Jerome Bickenbach…[et al]. Geneva: World Health Organization; 2013. [Google Scholar]
- 5.Stucki G, Bickenbach J. The international spinal cord injury survey and the learning health system for spinal cord injury. Am J Phys Med Rehabil. 2017;96(2 Suppl 1):S2–S4. [DOI] [PubMed] [Google Scholar]
- 6.Spinal Cord Injury Facts and Figures at a Glance. J Spin Cord Med. 2014;37(3):355–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Int Med. 2018;169(7):467–473. [DOI] [PubMed] [Google Scholar]
- 8.Craven BC, Alavinia SM. Methods for development of structure, process and outcome indicators for prioritized spinal cord injury rehabilitation domains: SCI-High Project. Spin J. 2019;42(sup1):51–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Craven BC, Alavinia SM, Wiest MJ, et al. Methods for development of structure, process and outcome indicators for prioritized spinal cord injury rehabilitation domains: SCI-High Project. J Spin Cord Med. 2019;42(sup1):51–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ronca E, Scheel-Sailer A, Koch HG, et al. Satisfaction with access and quality of healthcare services for people with spinal cord injury living in the community. J Spin Cord Med. 2018:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cox JB, Weaver KJ, Neal DW, Jacob RP, Hoh DJ. Decreased incidence of venous thromboembolism after spine surgery with early multimodal prophylaxis: clinical article. J Neurosurg Spine. 2014;21(4):677–684. [DOI] [PubMed] [Google Scholar]
- 12.Bradbury CL, Wodchis WP, Mikulis DJ, et al. Traumatic brain injury in patients with traumatic spinal cord injury: clinical and economic consequences. Arch Phys Med Rehabil. 2008;89(12 Suppl): S77–S84. [DOI] [PubMed] [Google Scholar]
- 13.Levi R, Hultling C, Seiger A. The Stockholm spinal cord injury study: 4. psychosocial and financial issues of the Swedish annual level-of-living survey in SCI subjects and controls. Paraplegia. 1996;34(3):152–157. [DOI] [PubMed] [Google Scholar]
- 14.Robertson FC, Logsdon JL, Dasenbrock HH, et al. Transitional care services: a quality and safety process improvement program in neurosurgery. J Neurosurg. 2018;128(5):1570–1577. [DOI] [PubMed] [Google Scholar]
- 15.New PW, Simmonds F, Stevermuer T. Comparison of patients managed in specialised spinal rehabilitation units with those managed in non-specialised rehabilitation units. Spinal Cord. 2011;49(8):909–916. [DOI] [PubMed] [Google Scholar]
- 16.Macias CA, Rosengart MR, Puyana JC, et al. The effects of trauma center care, admission volume, and surgical volume on paralysis after traumatic spinal cord injury. Ann Surg. 2009;249(1):10–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Post MW, van Asbeck FW, van Dijk AJ, Schrijvers AJ. Services for spinal cord injured: availability and satisfaction. Spinal Cord. 1997;35(2):109–115. [DOI] [PubMed] [Google Scholar]
- 18.Dunn M, Sommer N. Managing difficult staff interactions: effectiveness of assertiveness training for SCI nursing staff. Rehabil Nurs. 1997;22(2):82–87. [DOI] [PubMed] [Google Scholar]
- 19.Gerhart KA, Koziol-McLain J, Lowenstein SR, Whiteneck GG. Quality of life following spinal cord injury: knowledge and attitudes of emergency care providers. Ann Emerg Med. 1994;23(4):807–812. [DOI] [PubMed] [Google Scholar]
- 20.Zinman A, Digout N, Bain P, Haycock S, Hebert D, Hitzig SL. Evaluation of a community reintegration outpatient program service for community-dwelling persons with spinal cord injury. Rehabil Res Pract. 2014;2014:989025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paquet J, Rivers CS, Kurban D, et al. The impact of spine stability on cervical spinal cord injury with respect to demographics, management, and outcome: a prospective cohort from a national spinal cord injury registry. Spine J. 2018;18(1):88–98. [DOI] [PubMed] [Google Scholar]
- 22.Rinkaewkan P, Kuptniratsaikul V. The effectiveness of inpatients rehabilitation for spinal cord patients in Siriraj hospital. Spinal Cord. 2015;53(8):591–597. [DOI] [PubMed] [Google Scholar]
- 23.Street JT, Noonan VK, Cheung A, Fisher CG, Dvorak MF. Incidence of acute care adverse events and long-term health-related quality of life in patients with TSCI. Spine J. 2015;15(5):923–932. [DOI] [PubMed] [Google Scholar]
- 24.Romero-Ganuza J, Garcia-Forcada A, Vargas E, Gambarrutta C.An intermediate respiratory care unit for spinal cord-injured patients. A retrospective study. Spinal Cord. 2015;53(7):552–556. [DOI] [PubMed] [Google Scholar]
- 25.Battistuzzo CR, Armstrong A, Clark J, et al. Early decompression following cervical spinal cord injury: examining the process of care from accident scene to surgery. J Neurotrauma. 2016;33(12):1161–1169. [DOI] [PubMed] [Google Scholar]
- 26.Kreinest M, Ludes L, Turk A, Grutzner PA, Biglari B, Matschke S. Analysis of prehospital care and emergency room treatment of patients with acute traumatic spinal cord injury: a retrospective cohort study on the implementation of current guidelines. Spinal Cord. 2017;55(1):16–19. [DOI] [PubMed] [Google Scholar]
- 27.Bourassa-Moreau E, Mac-Thiong JM, Li A, et al. Do patients with complete spinal cord injury benefit from early surgical decompression? Analysis of neurological improvement in a prospective cohort study. J Neurotrauma. 2016;33(3):301–306. [DOI] [PubMed] [Google Scholar]
- 28.Furlan JC, Tung K, Fehlings MG. Process benchmarking appraisal of surgical decompression of spinal cord following traumatic cervical spinal cord injury: opportunities to reduce delays in surgical management. J Neurotrauma. 2013;30(6):487–491. [DOI] [PubMed] [Google Scholar]
- 29.Zhou Z, Zhang H, Guo C, Yu H, Wang L, Guo Q. Management of eosinophilic granuloma in pediatric patients: surgical intervention and surgery combined with postoperative radiotherapy and/or chemotherapy. Childs Nerv Syst. 2017;33(4):583–593. [DOI] [PubMed] [Google Scholar]
- 30.Bloemen-Vrencken JH, de Witte LP, Post MW, et al. Comparison of two Dutch follow-up care models for spinal cord-injured patients and their impact on health problems, re-admissions and quality of care. Clin Rehabil. 2007;21(11):997–1006. [DOI] [PubMed] [Google Scholar]
- 31.Sand A, Karlberg I, Kreuter M. Spinal cord injured persons’ conceptions of hospital care, rehabilitation, and a new life situation. Scand J Occup Ther. 2006;13(3):183–192. [DOI] [PubMed] [Google Scholar]
- 32.Donnelly C, McColl MA, Charlifue S, et al. Utilization, access and satisfaction with primary care among people with spinal cord injuries: a comparison of three countries. Spinal Cord. 2007;45(1):25–36. [DOI] [PubMed] [Google Scholar]
- 33.Rocchi M, Routhier F, Latimer-Cheung AE, Ginis KAM, Noreau L, Sweet SN. Are adults with spinal cord injury meeting the spinal cord injury-specific physical activity guidelines? A look at a sample from a Canadian province. Spinal Cord. 2017;55(5):454–459. [DOI] [PubMed] [Google Scholar]
- 34.Hammond FM, Gassaway J, Abeyta N, Freeman ES, Primack D. The SCIRehab project: social work and case management. Social work and case management treatment time during inpatient spinal cord injury rehabilitation. J Spinal Cord Med. 2011;34(2):216–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sclafani JA, Kim CW. Complications associated with the initial learning curve of minimally invasive spine surgery: a systematic review. Clin Orthop Relat Res. 2014;472(6):1711–1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Siosteen A, Kreuter M, Lampic C, Persson LO. Patient-staff agreement in the perception of spinal cord lesioned patients’ problems, emotional well-being, and coping pattern. Spinal Cord. 2005;43(3):179–186. [DOI] [PubMed] [Google Scholar]
- 37.Li C, DiPiro ND, Krause J. A latent structural equation model of risk behaviors and pressure ulcer outcomes among people with spinal cord injury. Spinal Cord. 2017;55(6):553–558. [DOI] [PubMed] [Google Scholar]
- 38.Lucke KT, Coccia H, Goode JS, Lucke JF. Quality of life in spinal cord injured individuals and their caregivers during the initial 6 months following rehabilitation. Qual Life Res. 2004;13(1):97–110. [DOI] [PubMed] [Google Scholar]
- 39.Alavinia SM, Omidvar M, Farahani F, Bayley M, Zee J, Craven BC. Enhancing quality practice for prevention and diagnosis of urinary tract infection during inpatient spinal cord rehabilitation. J Spin Cord Med. 2017;40(6):803–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kaminski L, Cordemans V, Cernat E, M’Bra KI, Mac-Thiong JM. Functional outcome prediction after traumatic spinal cord injury based on acute clinical factors. J Neurotrauma. 2017;34(12):2027–2033. [DOI] [PubMed] [Google Scholar]
- 41.Pelletier CA, Totosy de Zepetnek JO, MacDonald MJ, Hicks AL. A 16-week randomized controlled trial evaluating the physical activity guidelines for adults with spinal cord injury. Spinal Cord. 2015;53(5):363–367. [DOI] [PubMed] [Google Scholar]
- 42.Harvey LA, Chu J, Bowden JL, et al. How much equipment is prescribed for people with spinal cord injury in Australia, do they use it and are they satisfied 1 year later? Spinal Cord. 2012;50(9):676–681. [DOI] [PubMed] [Google Scholar]
- 43.Marion TE, Rivers CS, Kurban D, et al. Previously identified common post-injury adverse events in traumatic spinal cord injury-validation of existing literature and relation to selected potentially modifiable comorbidities: a prospective Canadian cohort study. J Neurotrauma. 2017;34(20):2883–2891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Scovil CY, Flett HM, McMillan LT, et al. The application of implementation science for pressure ulcer prevention best practices in an inpatient spinal cord injury rehabilitation program. J Spinal Cord Med. 2014;37(5):589–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.van Loo MA, Post MW, Bloemen JH, van Asbeck FW. Care needs of persons with long-term spinal cord injury living at home in the Netherlands. Spinal Cord. 2010;48(5):423–428. [DOI] [PubMed] [Google Scholar]
- 46.Tawashy AE, Eng JJ, Lin KH, Tang PF, Hung C. Physical activity is related to lower levels of pain, fatigue and depression in individuals with spinal-cord injury: a correlational study. Spinal Cord. 2009;47(4):301–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Martins CF, Bronzatto E, Neto JM, Magalhaes GS, D’Anconna CA, Cliquet A, Jr. Urinary tract infection analysis in a spinal cord injured population undergoing rehabilitation—how to treat? Spinal Cord. 2013;51(3):193–195. [DOI] [PubMed] [Google Scholar]
- 48.Wong AW, Heinemann AW, Wilson CS, et al. Predictors of participation enfranchisement after spinal cord injury: the mediating role of depression and moderating role of demographic and injury characteristics. Arch Phys Med Rehabil. 2014;95(6):1106–1113. [DOI] [PubMed] [Google Scholar]
- 49.Branagan G, Tromans A, Finnis D. Effect of stoma formation on bowel care and quality of life in patients with spinal cord injury. Spinal Cord. 2003;41(12):680–683. [DOI] [PubMed] [Google Scholar]
- 50.Saban KL, Penckofer SM, Androwich I, Bryant FB. Health-related quality of life of patients following selected types of lumbar spinal surgery: a pilot study. Health Qual Life Outcomes. 2007;5:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Backx APM, Spooren AIF, Bongers-Janssen HMH, Bouwsema H. Quality of life, burden and satisfaction with care in caregivers of patients with a spinal cord injury during and after rehabilitation. Spinal Cord. 2018;56(9):890–899. [DOI] [PubMed] [Google Scholar]
- 52.Jensen MP, Hoffman AJ, Cardenas DD. Chronic pain in individuals with spinal cord injury: a survey and longitudinal study. Spinal Cord. 2005;43(12):704–712. [DOI] [PubMed] [Google Scholar]
- 53.Savage P, Sharkey R, Kua T, et al. Malignant spinal cord compression: NICE guidance, improvements and challenges. QJM. 2014;107(4):277–282. [DOI] [PubMed] [Google Scholar]
- 54.Kortte KB, Gilbert M, Gorman P, Wegener ST. Positive psychological variables in the prediction of life satisfaction after spinal cord injury. Rehabil Psychol. 2010;55(1):40–47. [DOI] [PubMed] [Google Scholar]
- 55.Domeier RM, Evans RW, Swor RA, Rivera-Rivera EJ, Frederiksen SM. Prehospital clinical findings associated with spinal injury. Prehosp Emerg Care. 1997;1(1):11–15. [DOI] [PubMed] [Google Scholar]
- 56.Brown LH, Gough JE, Simonds WB. Can EMS providers adequately assess trauma patients for cervical spinal injury? Prehosp Emerg Care. 1998;2(1):33–36. [DOI] [PubMed] [Google Scholar]
- 57.Dallolio L, Menarini M, China S, et al. Functional and clinical outcomes of telemedicine in patients with spinal cord injury. Arch Phys Med Rehabil. 2008;89(12):2332–2341. [DOI] [PubMed] [Google Scholar]
- 58.Lorenz DJ, Datta S, Harkema SJ. Longitudinal patterns of functional recovery in patients with incomplete spinal cord injury receiving activity-based rehabilitation. Arch Phys Med Rehabil. 2012;93(9):1541–1552. [DOI] [PubMed] [Google Scholar]
- 59.Heinemann AW, LaVela SL, Etingen B, et al. Perceptions of person-centered care following spinal cord injury. Arch Phys Med Rehabil. 2016;97(8):1338–1344. [DOI] [PubMed] [Google Scholar]
- 60.Kennedy P, Smithson E, McClelland M, Short D, Royle J, Wilson C. Life satisfaction, appraisals and functional outcomes in spinal cord-injured people living in the community. Spinal Cord. 2010;48(2):144–148. [DOI] [PubMed] [Google Scholar]
- 61.Garcia RA, Gaebler-Spira D, Sisung C, Heinemann AW. Functional improvement after pediatric spinal cord injury. Am J Phys Med Rehabil. 2002;81(6):458–463. [DOI] [PubMed] [Google Scholar]
- 62.Johnston M, Nissim EN, Wood K, Hwang K, Tulsky D. Objective and subjective handicap following spinal cord injury: interrelationships and predictors. J Spinal Cord Med. 2002;25(1):11–22. [DOI] [PubMed] [Google Scholar]
- 63.Wirth B, van Hedel HJ, Kometer B, Dietz V, Curt A. Changes in activity after a complete spinal cord injury as measured by the Spinal Cord Independence Measure II (SCIM II). Neurorehabil Neural Repair. 2008;22(3):279–287. [PubMed] [Google Scholar]
- 64.Donnelly C, Eng JJ, Hall J, et al. Client-centred assessment and the identification of meaningful treatment goals for individuals with a spinal cord injury. Spinal Cord. 2004;42(5):302–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Motiei-Langroudi R, Sadeghian H. Traumatic spinal cord injury: long-term motor, sensory, and urinary outcomes. Asian Spine J. 2017;11(3):412–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lidal IB, Veenstra M, Hjeltnes N, Biering-Sorensen F. Health-related quality of life in persons with long-standing spinal cord injury. Spinal Cord. 2008;46(11):710–715. [DOI] [PubMed] [Google Scholar]
- 67.Chan SC, Chan AP. User satisfaction, community participation and quality of life among Chinese wheelchair users with spinal cord injury: a preliminary study. Occup Ther Int. 2007;14(3):123–143. [DOI] [PubMed] [Google Scholar]
- 68.Kullmann L, Toth K. Exploration of quality-of-life goals in individuals with spinal cord injury. Int J Rehabil Res. 2012;35(1):85–87. [DOI] [PubMed] [Google Scholar]
- 69.Campbell J, Velard M, Denys P, Chartier-Kastler E, Kowalski J, Sullivan S. Cost-effectiveness and financial impact of onabotulinumtoxina treatment for urinary incontinence due to neurogenic detrusor overactivity in spinal cord injury patients within the french healthcare system. Int Urogynecol J Pelvic Floor Dysfunct. 2011;2:S329. [Google Scholar]
- 70.de Andrade AF, Marino R, Ciquini O, Figueiredo EG, Machado AG. Guidelines for neurosurgical trauma in Brazil. World J Surg. 2001;25(9):1186–1201. [DOI] [PubMed] [Google Scholar]
- 71.Lin MR, Hwang HF, Chen CY, Chiu WT. Comparisons of the brief form of the world health organization quality of life and short form-36 for persons with spinal cord injuries. Am J Phys Med Rehabil. 2007;86(2):104–113. [DOI] [PubMed] [Google Scholar]
- 72.van Hedel HJ, Wirz M, Curt A. Improving walking assessment in subjects with an incomplete spinal cord injury: responsiveness. Spinal Cord. 2006;44(6):352–356. [DOI] [PubMed] [Google Scholar]
- 73.Dvorak MF, Cheng CL, Fallah N, et al. Spinal cord injury clinical registries: improving care across the SCI care continuum by identifying knowledge gaps. J Neurotrauma. 2017;34(20):2924–2933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Garrido-Castro JL, Escudero A, Medina-Carnicer R, et al. Validation of a new objective index to measure spinal mobility: the University of Cordoba Ankylosing Spondylitis Metrology Index (UCOASMI). Rheumatol Int. 2014;34(3):401–406. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-docx-1-gsj-10.1177_2192568220981988 for Indicators of Quality of Care in Individuals With Traumatic Spinal Cord Injury: A Scoping Review by Sepehr Khosravi, Amirmahdi Khayyamfar, Milad Shemshadi, Masoud Pourghahramani Koltapeh, Mohsen Sadeghi-Naini, Zahra Ghodsi, Farhad Shokraneh, Mohadeseh Sarbaz Bardsiri, Pegah Derakhshan, Khalil Komlakh, Alex R. Vaccaro, Michael G. Fehlings, James D. Guest, Vanessa Noonan and Vafa Rahimi-Movaghar in Global Spine Journal