Abstract
Study Design:
A systematic review and meta-analysis.
Objectives:
To evaluate clinical and radiographic outcomes, and perioperative complications of oblique lateral interbody fusion (OLIF) for adult spinal deformity (ASD).
Methods:
We performed a systematic review and meta-analysis of related studies reporting outcomes of OLIF for ASD. The clinical outcomes were assessed by visual analogue scale (VAS) and Oswestry Disability Index (ODI). The radiographic parameters were evaluated by sagittal vertical axis (SVA), pelvic tilt (PT), sacral slope (SS), thoracic kyphosis (TK), lumbar lordosis (LL), pelvic incidence-lumbar lordosis (PI-LL), Cobb angle and fusion rate. A random effects model and 95% confidence intervals (CI) were performed to investigate the results.
Results:
A total of 16 studies involving 519 patients were included in the present study. The mean difference of VAS-back score, VAS-leg score and ODI score before and after surgery was 5.1, 5.0 and 32.3 respectively. The mean correction of LL was 20.6°, with an average of 6.9° per level and the mean correction of Cobb was 16.4°, with an average of 4.7° per level. The mean correction of SVA, PT, SS, TK and PI-LL was 59.3 mm, 11.7°, 6.9°, 9.4° and 20.6° respectively. The mean fusion rate was 94.1%. The incidence of intraoperative and postoperative complications was 4.9% and 29.6% respectively.
Conclusions:
OLIF is an effective and safe surgery method in the treatment of mild or moderate ASD and it has advantages in less intraoperative blood loss and lower perioperative complications.
Keywords: oblique lateral interbody fusion, adult spinal deformity, systematic review, meta-analysis
Introduction
Adult spinal deformity (ASD) is a common cause of chronic low back pain and disability. The primary goals of ASD treatment are to obtain coronal and sagittal balance, relieve pain and achieve solid fusion. 1 For years, traditional open osteotomies, such as Smith-Petersen osteotomy (SPO), pedicle subtraction osteotomy (PSO), and vertebral column resection (VCR) have been used as powerful surgical methods for ASD and have gained excellent clinical outcome.2,3 However, these traditional methods are associated with various complications including excessive blood loss, pseudarthrosis, proximal junctional kyphosis (PJK), neurological deficit, rod breakage, dural tear, deep wound infection or hematoma.2-8 Therefore, minimally invasive surgery (MIS) has been increasingly used in ASD treatment to reduce intraoperative blood loss and perioperative complications in recent years.9,10 As a mini-open anterior retroperitoneal approach, oblique lateral interbody fusion (OLIF) was firstly introduced to treat lumbar degenerative diseases via a physiological corridor between the aorta and psoas in 2012. 11 The mechanism of oblique lateral approach is to achieve indirect neural decompression and lumbar lordosis correction by placing a larger cage into the disc space. 12
So far, a few studies have reported the results of OLIF used in ASD.13-15 However, these studies were limited by the number of patients, so the effectiveness and safety of OLIF in ASD treatment are still controversial and have not been systematically confirmed. Thus, the purpose of this systematic review and meta-analysis was to study whether OLIF is effective and safe in the treatment of ASD and provide scientific evidence for spine surgeons.
Methods
Literature Search
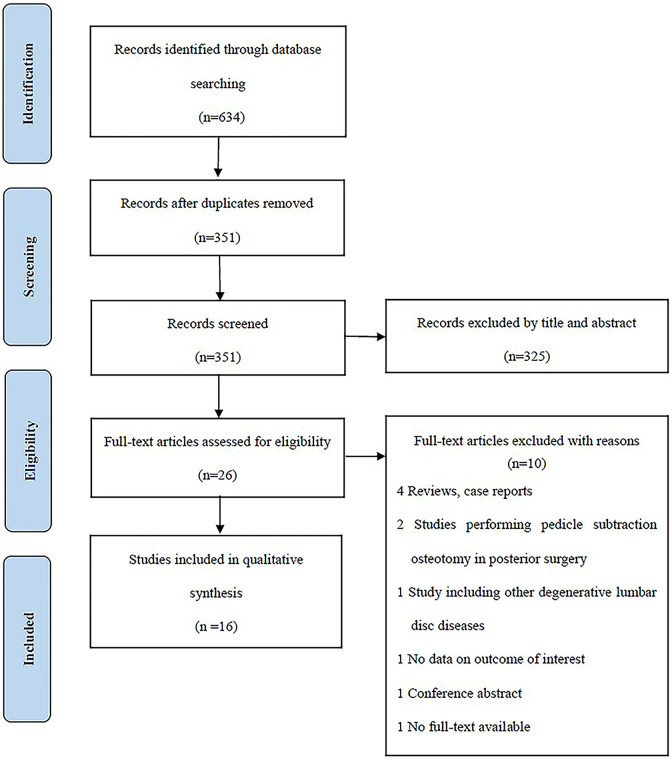
The systematic review was performed according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. 16 Literature was searched with no language restrictions. Since OLIF was firstly reported in 2012, we searched for articles published between January 2012 and August 2020 in PubMed, Embase, Cochrane Library, WANFANG, and CNKI databases. The terms used for the search were as follows: “oblique lateral interbody fusion” OR “oblique lumbar interbody fusion” OR “oblique lateral lumbar interbody fusion” OR “retroperitoneal lumbar interbody fusion” OR “pre-psoas lateral interbody fusion” OR “anterior to psoas lumbar interbody fusion” OR “anterolateral approach to lumbar” OR “OLIF” OR “OLLIF.” Articles from the same authors or institutions were examined, and duplicate data sets were excluded. The number of articles included and excluded was shown in a flow chart (Figure 1).
Figure 1.
Flow chart.
Selection Criteria
Articles included in the systematic review fulfilled the following criteria: 1) patients aged >18 years; 2) a diagnosis of idiopathic or degenerative lumbar kyphosis or scoliosis; 3) spinal deformity treated by OLIF combined with posterior or lateral fixation with or without posterior column osteotomy (PCO); 4) more than 3 months’ follow-up. Studies including less than 10 patients, involving other lumbar degenerative diseases without spinal deformity, or reporting OLIF combined with osteotomy of the vertebral body (such as PSO and VCR) were excluded.
Data Extraction
The extracted data is as follows. The general data was shown in Table 1 to 3 (author name, publication year, country, study design, gender, age, follow-up, hospital stay, diagnosis, type of surgery, OLIF levels, total fusion levels, fixation levels, posterior decompression, osteotomy, operative time, intraoperative blood loss and fusion materials). The clinical outcomes were shown in Figure 2 (VAS-back, VAS-leg, ODI). The radiographic parameters were shown in Figures 3 and 4 and Table 3 (SVA, PT, SS, TK, LL, PI-LL, Cobb and fusion rate) and complications were shown in Table 3. If all patients underwent OLIF standalone or OLIF combined with posterior or lateral fixation with or without posterior facetectomy and/or laminectomy in partial surgical segments in one study, type of surgery of this study was defined as OLIF stand-alone or OLIF combined with posterior or lateral fixation with or without selective posterior decompression and this study was included in OLIF group. If few patients underwent OLIF combined with PCO in partial surgical segments in one study, type of surgery of this study was defined as OLIF with selective PCO and this study was included in OLIF with selective PCO group. If all patients underwent OLIF combined with PCO in all surgical segments in one study, type of surgery of this study was defined as OLIF with PCO and this study was included in OLIF with PCO group. Data from articles was extracted independently by 2 reviewers and verified by the third reviewer when there was a disagreement.
Table 1.
General Data.
| Authors & year | Country | Study design | No of patients | Females, n (%) | Age, years, mean (range) | Follow-up, months, mean (range) | Hospital stay, days, mean (SD) | Diagnosis |
|---|---|---|---|---|---|---|---|---|
| Kim et al, 2017 18 | South Korea | Retrospective | 32 | 28 (87.5) | 68 (58-78) | 26.1 (>6) | Degenerative lumbar kyphosis or scoliosis | |
| Ohtori et al, 2015 15 | Japan | Prospective | 12 | 8 (66.7) | 64 (58-78) | 14.5 (12-24) | Degenerated lumbar kyphoscoliosis | |
| Zhao et al, 2017 20 | China | Retrospective | 17 | 13 (76.5) | 69.5 (46-80) | 18.2 (12-28) | Degenerative scoliosis | |
| He et al, 2020 19 | China | Retrospective | 56 | 35 (62.5) | 65.2 (48-81) | 9.3 (>6) | Degenerative lumbar scoliosis | |
| Anand et al, 2019 13 | USA | Prospective | 60 | 39 (65) | 66.8 (48-79) | 24 (3-60) | 8.9 (3.7) | Adult spinal deformity |
| Wang et al, 2019 22 | China | Retrospective | 11 | 10 (90.9) | 71.5 (56-86) | 9.7 (6-15) | 4.1 (1.6) | Degenerative scoliosis |
| Abbasi et al, 2017 23 | USA | Retrospective | 36 | 7 (19.4) | 69.6 | (>5) | 3 | Degenerative spinal deformity |
| Park et al, 2020 14 | Korea | Retrospective | 23 | 20 (87) | 69.4 (20-80) | 40.7 (>24) | Degenerative spinal deformity | |
| Lee et al, 2019 24 | Korea | Retrospective | 41 | 39 (95.1) | 72 (≥65) | 25.1 (>24) | Adult spinal deformity | |
| Mehren et al, 2020 25 | Germany | Retrospective | 15 | 12 (80) | 71 (34-84) | (>3) | Degenerative lumbar scoliosis or segmental kyphosis | |
| Lui et al, 2019 26 | UK | Prospective | 34 | 22 (64.7) | 62.9 (45-81) | (>24) | Adult spinal deformity | |
| Koike et al, 2020 27 | Japan | Retrospective | 74 | 65 (87.8) | 73.6 (52-84) | 22.4 (12-64) | Idiopathic or degenerative scoliosis | |
| Wu and Huang, 2019 28 | China | Retrospective | 38 | 26 (68.4) | 65 (48-82) | 18.5 (>12) | Degenerative scoliosis | |
| Fang et al, 2020 29 | China | Retrospective | 27 | 10 (37) | 54 (51-68) | 30 (6-52) | Degenerative scoliosis | |
| Xu et al, 2020 30 | China | Retrospective | 28 | (>18) | 24.2 (15-40) | 6 (2.4) | Degenerative lumbar scoliosis | |
| Patel et al, 2019 21 | South Korea | Prospective | 15 | 12 (80) | 67 (63-74) | 24 (21-30) | Degenerative lumbar scoliosis or kyphoscoliosis |
Table 2.
General Data.
| Authors & year | Type of surgery (cases) | OLIF levels, mean (range) | Total fusion levels, mean (range/SD) | Fixation levels, mean (range/SD) | Posterior decompression (cases) | Osteotomy (cases) | Operative time (min), mean (SD) | Intraoperative Blood Loss (ml) Mean (SD) |
|---|---|---|---|---|---|---|---|---|
| Kim et al, 2017 18 | OLIF with posterior pedicle screw | 3.8 (3-5, L3-S1) | 3.8 (3-5, L3-S1) | 7.3 (5-9, T10-S1) | Facetectomy and/or laminectomy | None | 94.7 | 98.4 |
| Ohtori et al, 2015 15 | OLIF with posterior open (4) or percutaneous (8) pedicle screw | 2.9 (2-4, L2-S1) | 7.3 (3-15, T4-S1) | (1) | None | 250 (35) | 350 (50) | |
| Zhao et al, 2017 20 | OLIF standalone (5) or OLIF with posterior open pedicle screw (12) and L5-S1 PLIF (4) | 2.6 (1-4, L1-L5) | 2.6 (1-4, L1-L5) | 5.5 (2-10, T10-S2) | Laminectomy (7) | None | 290 (107.4) | 405 (172.8) |
| He et al, 2020 19 | OLIF with posterior pedicle screw | 2.3 (2-3, L2-S1) | 2.3 (2-3, L2-S1) | None | None | 301 (87) | 407.2 (188.4) | |
| Anand et al, 2019 13 | OLIF with posterior percutaneous pedicle screw | 7 (4-9) | None | None | 493.5 | 642 | ||
| Wang et al, 2019 22 | OLIF with lateral screw fixation | 2.2 (1-3, L2-L5) | 2.2 (1-3, L2-L5) | None | None | 144 (50) | 94.5 (72.4) | |
| Abbasi et al, 2017 23 | OLIF with posterior percutaneous pedicle screw | 2.7 (1-6) | 2.7 (1-6) | None | None | 116.1 | 173.3 | |
| Park et al, 2020 14 | OLIF with posterior percutaneous pedicle screw and L5-S1 TLIF (10) | 4.4 (4-5, L1-S1) | 4.4 (4-5, L1-S1) | 6.7 (1.5) | Facetectomy and laminectomy (10) | None | 345 (50) | 331.3 (109.6) |
| Lee et al, 2019 24 | OLIF with PCO and pedicle screw fixation | 3 (T12-S1) | 8 (T10-S1) | Facetectomy | PCO | 379 (46) | 1736.6 (465.7) | |
| Mehren et al, 2020 25 | OLIF with posterior pedicle screw | 2.3 (1-4) | 2.3 (1-4) | None | None | |||
| Lui et al, 2019 26 | OLIF with posterior fusion and pedicle screw fixation | 9.4 (4.1) | (selective) | PCO (selective) |
398.5 (238.1) | 553.6 (354.9) | ||
| Koike etal., 2020 27 | OLIF with posterior percutaneous screw and lumbosacral open TLIF | 4.1 (L1-S1) | 4.7 | 7.7 (T3-S1) | Additional TLIF (selective) | PCO (selective) |
||
| Wu and Huang, 2019 28 | OLIF with posterior open pedicle screw | 2.6 (2-3) | 2.6 (2-3) | Laminectomy (selective) | None | |||
| Fang et al, 2020 29 | OLIF with posterior open pedicle screw and L5-S1 TLIF | 7.2 (2.3) | Facetectomy | SPO (selective) |
235 (33) | 433 (62) | ||
| Xu et al, 2020 30 | OLIF standalone | (1-3) | (1-3) | None | None | 87.6 (27.7) | 84.6 (33.6) | |
| Patel et al, 2019 21 | OLIF with posterior open pedicle screw | 3 (1-4) | 3 (1-4) | 6 (4-8) | Facetectomy (5) | SPO (3) | 420 (122.4) | 863 (296) |
Abbreviations: OLIF, oblique lateral interbody fusion; PLIF, posterior lumbar interbody fusion; TLIF, transforaminal lumbar interbody fusion; PCO, posterior column osteotomy; SPO, Smith-Petersen osteotomy.
Table 3.
Fusion Materials, Fusion Rate and Complications.
| Authors & year | Fusion materials | Fusion rate (no. of cage), evaluation method | Complications (cases) |
|---|---|---|---|
| Kim et al, 2017 18 | PEEK cage with autogenous and allogeneic bone grafts | 83.6% (102/122), X-rays/CT | Groin and medial thigh pains (3), peritoneal tear (2) |
| Ohtori et al, 2015 15 | Cage with autograft from the iliac bone | 88.6% (31/35), CT | Cage subsidence (1), thigh pain (1), thigh numbness (2), donor site pain (8) |
| Zhao et al, 2017 20 | Cage with allogeneic or autogenous iliac bone grafts | 100% (45/45), X-rays | Transient hip flexor weakness (5), anterolateral thigh pain (1), sympathetic chain injury (1) |
| He et al, 2020 19 | 97.7% (127/130), X-rays | Iliac vein or segmental artery injury (6), sympathetic chain injury (7), femoral nerve injury (2), cage subsidence (16) | |
| Anand et al, 2019 13 | PEEK cage with RhBMP-2 and Grafton putty | None | |
| Wang et al, 2019 22 | PEEK cage with allograft and hydroxyapatite | 100% (24 /24), CT | Cage subsidence (2) |
| Abbasi et al, 2017 23 | Cage with tricalcium phosphate soaked in autologous bone marrow aspirate | 100% (24 cases/24 cases) | Neuropraxia (1), nerve irritation with corresponding weakness (2) |
| Park et al, 2020 14 | PEEK cage with demineralized bone matrix or local bone chips from the lamina and facets | Proximal junctional kyphosis (7), psoas symptoms (8), ileus (13), leg dysesthesia (5) | |
| Lee et al, 2019 24 | PEEK cage with RhBMP-2 and allograft | Transient right L4 root palsy (1), hemothorax at L1–2 (1), superficial wound infection (1), PJK (9), pseudarthrosis (1) | |
| Mehren et al, 2020 25 | Cage with RhBMP-2 and allograft | None | |
| Lui et al, 2019 26 | Tantalum cage | ||
| Koike etal., 2020 27 | PEEK cage with allograft | ||
| Wu and Huang, 2019 28 | 100% (99/99) | Transient thigh pain and thigh numbness (2), transient hematuria (1), cage subsidence (1), sympathetic chain injury (1) | |
| Fang et al, 2020 29 | Cage with allograft | Psoas weakness (2), endplate injury and cage subsidence (3), fatty fluidization of incision (2), calf muscular venous thrombosis (3), PJK (3) | |
| Xu et al, 2020 30 | 100% (28 cases/28 cases) | Urinary tract infection (1), ileus (2), back pain (3), hip flexor pain (2), incision pain (1) | |
| Patel et al, 2019 21 | PEEK cage with demineralized bone matrix | 86.7% (13 cases/15 cases) | Transient hip flexion weakness (2), adjacent vertebrae (L2) fracture (1), wound infection (1) |
Abbreviations: PEEK, polyetheretherketone; RhBMP-2, recombinant human bone morphogenetic protein 2; CT, computed tomography; PJK, proximal junctional kyphosis.
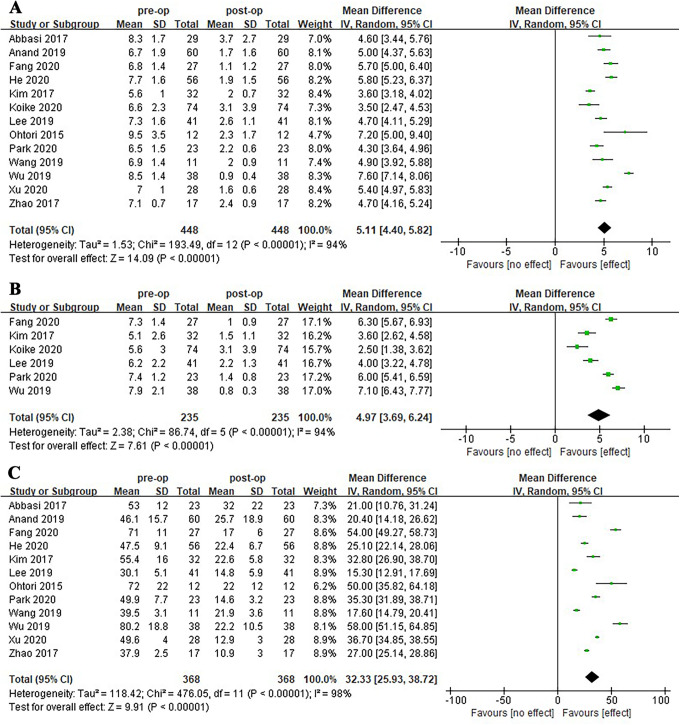
Figure 2.
Forest plots of VAS-back pain (A), VAS-leg pain (B) and ODI (C). The vertical line indicates no change in the outcome after OLIF surgery. The position of the black diamond indicates whether there is any change and improvement or deterioration depends on whether it is on the effect side or the no effect side. The squares indicate the individual studies with their size proportional to the weightings given to each study.
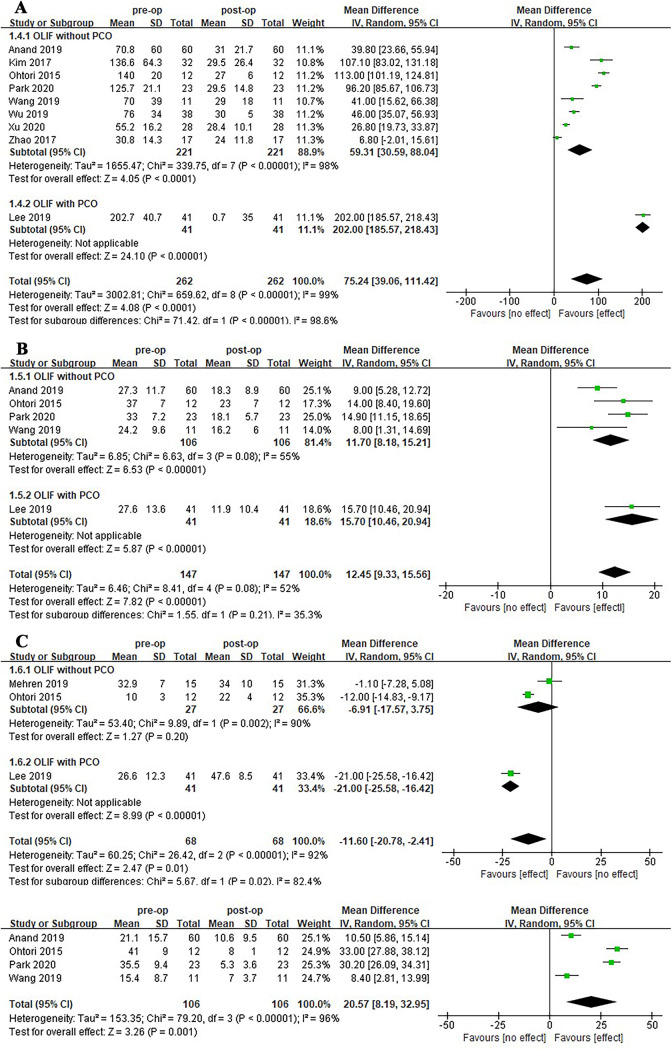
Figure 3.
Forest plots of sagittal parameters including SVA (A), PT (B), SS(C) and PI-LL (D).
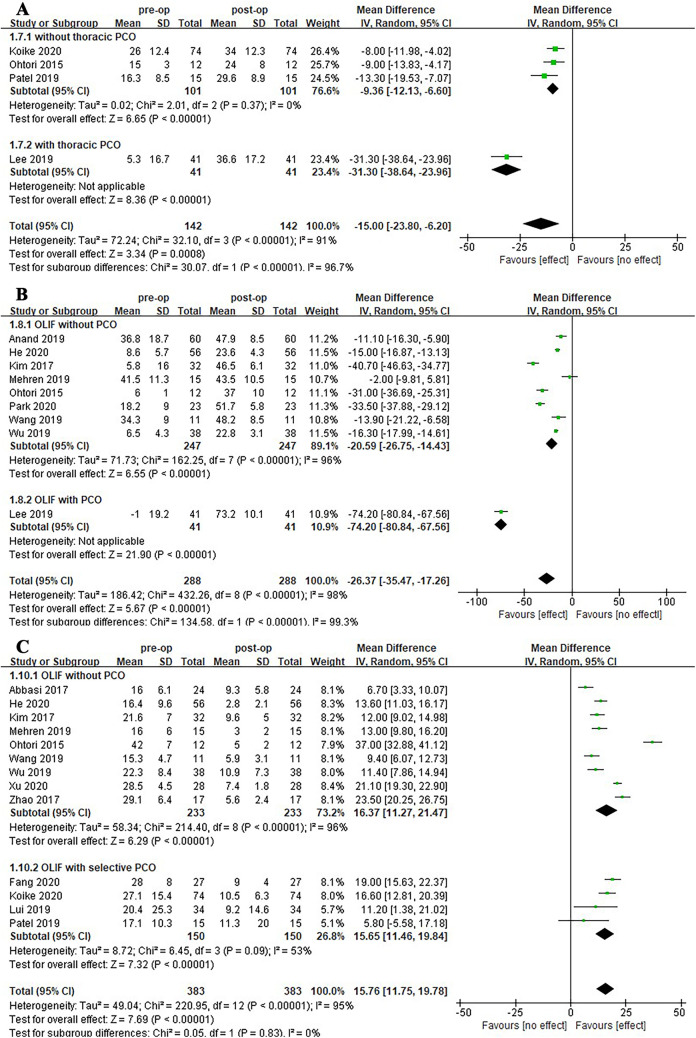
Figure 4.
Forest plots of TK (A), LL(B) and Cobb (C).
Quality Assessment
The methodological quality of each study included in the present meta-analysis was evaluated by the National Heart Lung and Blood Institute (NHLBI) quality assessment tool for case series studies (Table 4). 17 All studies were classified as either good, fair or poor.
Table 4.
Quality Assessment Tool for Case Series Studies.
| Criteria | Yes/no/other (CD, NR, NA)* |
|---|---|
| 1. Was the study question or objective clearly stated? | |
| 2. Was the study population clearly and fully described, including a case definition? | |
| 3. Were the cases consecutive? | |
| 4. Were the subjects comparable? | |
| 5. Was the intervention clearly described? | |
| 6. Were the outcome measures clearly defined, valid, reliable, and implemented consistently across all study participants? | |
| 7. Was the length of follow-up adequate? | |
| 8. Were the statistical methods well-described? | |
| 9. Were the results well-described? | |
| Quality Rating (good, fair, or poor) | |
| Rater #1 initials: | |
| Rater #2 initials: | |
| Additional Comments (If POOR, please state why): |
Abbreviations: *CD, cannot determine; NA, not applicable; NR, not reported.
Statistical Analysis
Data is presented as n (%) for categorical variables and mean ± standard deviation (SD) for continuous variables. The SPSS v.17 was used to calculate the weighted mean value of general data (age, follow-up, hospital stay, OLIF levels, total fusion levels, fixation levels, operative time, intraoperative blood loss). The Review Manager v.5.3 software was used to merge the preoperative and postoperative clinical outcomes and radiographic parameters in each study and an overall estimate of the effect was shown in the form of forest plot.The treatment effect was expressed as mean difference and 95% CI. Mean difference was calculated by postoperative value minus preoperative value from each study. Heterogeneity of clinical outcomes and radiographic parameters between studies was assessed using the I2 value. A sensitivity analysis by eliminating one of all included studies at a time and subgroup analysis were performed to examine the source of the heterogeneity when heterogeneity existed (I2 > 50%). The random effects model was used if heterogeneity still existed. Otherwise, the fixed effects model was used (I2 < 50%).
Results
A total of 16 studies13-15,18-30 involving 519 patients underwent OLIF combined with posterior or lateral fixation with or without posterior decompression and PCO were included in the present meta-analysis. All included studies were assessed as good according to the NHLBI quality assessment tool.
General Data
Fifteen studies13-15,18-29 involving 491 patients reported gender (145 males and 346 females) and age (mean 67.6 years, 20-86). The mean follow-up of 434 patients in 13 studies13-15,18-22,24,27-30 was 22 months (3-64). The mean hospital stay of 135 patients in 4 studies13,22,23,30 was 6.3 days. The mean OLIF levels of 370 patients in 12 studies14,15,18-25,27,28 was 3.1 segments (1-6, T12-S1). The mean total fusion levels of 491 patients in 15 studies13-15,18-29 was 4.9 segments (1-15, T4-S1). The mean fixation levels of 146 patients in 4 studies14,18,20,27 was 7.2 segments (2-16, T3-S2). The mean operative time and intraoperative blood loss of 392 patients in 13 studies13-15,18-24,26,29,30 were 294.2 min (an average of 59 minutes per fusion level) and 529.3 ml (an average of 107.3 ml per fusion level) respectively. The mean operative time and intraoperative blood loss of 247 patients in 8 studies13-15,18,20-23 in OLIF group were 288 min (an average of 75.8 minutes per fusion level) and 366.2 ml (an average of 97.1 ml per fusion level) respectively.
Clinical Outcomes
Mean difference of all clinical outcomes was equal to the preoperative mean value of clinical outcomes minus the postoperative mean value of clinical outcomes. Thirteen studies13-15,18-20,22-24,27-30 involving 448 patients reported the VAS-back scores with a mean difference of 5.11 (95%CI, 4.40-5.82). Six studies14,18,24,27-29 involving 235 patients reported the VAS-leg scores with a mean difference of 4.97 (95%CI, 3.69-6.24). Twelve studies13-15,18-20,22-24,28-30 involving 368 patients reported the ODI scores with a mean difference of 32.33 (95%CI, 25.93-38.72).
Radiographic Parameters
In order to avoid the effect of selective PCO on the improvement of radiographic parameters, we only included studies in OLIF group and OLIF with PCO group in the analysis of most radiographic parameters. Due to the significant effect of muti-level PCO on the improvement of radiographic parameters, we separated the studies in OLIF group and the study in OLIF with PCO group. Mean difference of all radiographic parameters was equal to the preoperative mean value of radiographic parameters minus the postoperative mean value of radiographic parameters. Eight studies13-15,18,20,22,28,30 involving 221 patients in OLIF group showed that the average correction of SVA is 59.31 mm (95%CI, 30.59 to 88.04 mm). A study 24 in OLIF with PCO group showed that the average correction of SVA is 202.00 mm (95%CI, 185.57 to 218.43 mm). Four studies13-15,22 in OLIF group showed that the average correction of PT is 11.70° (95%CI, 8.18 to 15.21°). A study 24 in OLIF with PCO group showed that the average correction of PT is 15.70° (95%CI, 10.46 to 20.94°). Two studies15,25 in the OLIF group showed that the average correction of SS is -6.91° (95%CI, -17.57° to 3.75°). A study 24 in OLIF with PCO group showed that the average correction of SS is -21° (95%CI, -25.58° to -16.42°). Four studies14,20,23,26 involving 142 patients (one study was excluded because it was uncertain whether there was thoracic PCO) reported that the average correction of TK is -15° (95%CI, -23.80° to -6.20°).
To investigate the source of the heterogeneity, a subgroup analysis was performed according to whether there is thoracic PCO. The results of 3 studies15,21,27 which did not include thoracic PCO showed that the average correction of TK is -9.36° (95%CI, -12.13° to -6.60°). A study 24 involving thoracic PCO showed that the average correction of TK is -31.30° (95%CI, -38.64° to -23.96°). Eight studies13-15,18,21,22,25,28 in OLIF group showed that the average correction of LL is -20.59° (95%CI, -26.75° to -14.43°). An average correction of 6.9° per lumbar fusion level was found in 6 studies14,18,21,22,25,28 (2 studies were excluded for the absence of lumbar fusion level). A study 24 in OLIF with PCO group showed that the average correction of LL is -74.2° (95%CI, -80.84° to -67.56°). Four studies13-15,22 in OLIF group reported the PI-LL with a mean difference of 20.57° (95%CI, 8.19-32.95°). Thirteen studies15,18-23,25-30 involving 383 patients reported the Cobb with a mean difference of 15.76° (95%CI, 11.75-19.78°). A further subgroup analysis was performed according to whether there is selective PCO. Nine studies15,18,20-23,25,28,30 in OLIF group showed that the average correction of Cobb is 16.37° (95%CI, 11.27°-21.47°). An average correction of 4.7° per lumbar fusion level was found in 7 studies18,20-23,25,28 (2 studies were excluded for the absence of lumbar fusion level). Four studies21,26,27,29 in OLIF with selective PCO group showed that the average correction of Cobb is 15.76° (95%CI, 11.75° to 19.78°). Six studies15,18,20-22,28 involving 166 patients reported the fusion rate, with an average of 94.1% (3 studies were excluded for the absence of OLIF levels).
Complications
A total of 14 studies13-15,18-25,28-30 involving 406 patients reported the incidence of intraoperative and postoperative complications is 4.9% and 29.6% respectively. The most common intraoperative complications were sympathetic chain (2.2%) and vascular (1.5%) injury. However, endplate injury (n = 3) and peritoneal tear (n = 2) were rare. The most common postoperative complications included transient thigh pain or numbness and hip flexor weakness or pain (9.4%), cage subsidence (5.7%), PJK (4.7%), ileus (3.7%) and donor site pain (2%). The rare complications included back pain (n = 3), calf muscular venous thrombosis (n = 3), wound infection (n = 2), fatty fluidization of incision (n = 2), incision pain (n = 1), pseudarthrosis (n = 1), adjacent vertebrae fracture (n = 1), transient hematuria (n = 1), urinary tract infection (n = 1), neuropraxia (n = 1) and hemothorax (n = 1).
Discussion
ASD is mainly caused by asymmetric degeneration of the intervertebral disc and facet joint, usually accompanied by coronal and sagittal imbalance, loss of lumbar lordosis, and spinal stenosis. 31 Various spinal osteotomies have been widely used to treat ASD for many years. Schwab et al 32 proposed classification system of spinal osteotomy based on 6 anatomic grades of resection corresponding to the extent of bone resection. The extent of PCO including SPO 2 (grade I) and Ponte osteotomy 33 (grade II) is small, which corrects spinal deformity by removing articular processes. PSO 2 (grade Ⅲ), SRS-Schwab osteotomy 34 (grade Ⅳ), VCR 3 (grade Ⅴ) and multiple VCRs (grade Ⅵ) belong to 3-column osteotomy. Among them, SPO, PSO and VCR are the most commonly used, and other osteotomies are improved on their basis. Although the above various spinal osteotomies have achieved excellent clinical outcomes in ASD treatment, there are still various problems such as excessive intraoperative blood loss and high perioperative complication rate.2-8
Surgical Trauma
In order to reduce intraoperative blood loss and perioperative complications, MIS is increasingly used to treat ASD and has achieved excellent clinical outcomes.9,10 The present study found that the average volume of intraoperative blood loss is merely 366.2 ml with an average of 97.1 ml per fusion level in OLIF group. Lee et al 24 reported that the average volume of intraoperative blood loss is 1736 ml in multi-level OLIF combined with multi-level PCO group and 2824 ml in PSO group respectively. Cho et al 2 reported that the average volume of intraoperative blood loss is 1398 ml in multi-level SPO group and 2617 ml in single-level PSO group respectively. Suk et al 35 reported that the average volume of intraoperative blood loss is 7034 ml in the posterior VCR for severe rigid scoliosis. These results found that intraoperative blood loss increased enormously as the extent of spinal osteotomy expanded. Besides, these results also demonstrated that multi-level OLIF combined with posterior or lateral fixation with or without selective posterior decompression significantly decrease intraoperative blood loss in the treatment of ASD compared with multi-level SPO. And multi-level OLIF combined with multi-level PCO also significantly decrease intraoperative blood loss compared with single-level PSO and VCR. This was mainly due to the application of the physiological corridor between the peritoneum and anterior edge of the psoas muscle, which avoided posterior multi-level facetectomy and laminectomy. In addition, the present study also found that the average length of hospital stay is only 6.3 days due to the application of the circumferential MIS, which was meaningful for patients’ early recovery after surgery.
Clinical Outcomes
The present meta-analysis also found that VAS-back score, VAS-leg score and ODI score in all included studies improved significantly postoperatively, which indicated that OLIF is effective in the treatment of ASD.
Radiographic Parameters
Correction of Sagittal Imbalance
Many previous studies36,37 have confirmed that sagittal imbalance is closely related to patient’s quality of life and thus restoring sagittal balance can better improve clinical outcomes. Schwab et al 38 proposed that the radiographic parameters for ideal sagittal balance after surgery should be SVA ≤ 40 mm, PT ≤ 20° and PI-LL ≤ 9°. Cho et al 2 reported that the average correction of SVA is 55 mm in multi-level SPO group and 112 mm in single-level PSO group respectively. The present meta-analysis found that SVA is decreased from 87.9 mm preoperatively to 28.6 mm postoperatively with a mean difference of 59.3 mm in OLIF group and 202.7 mm preoperatively to 0.7 mm postoperatively with a mean difference of 202 mm in OLIF with PCO group, respectively. These results demonstrated that OLIF is similar to multi-level SPO and OLIF combined with PCO is superior to single-level PSO in terms of SVA correction. Besides, this study found that PT is decreased from 30.6° preoperatively to 18.9° postoperatively with a mean difference of 11.7° in OLIF group and 27.6° preoperatively to 11.9° postoperatively with a mean difference of 15.7° in OLIF with PCO group, respectively. In addition, this study found that PI-LL is decreased from 28.3° preoperatively to 7.7° postoperatively with a mean difference of 20.6° in OLIF group.
Correction of LL and TK
Lafage et al 39 found that correction of LL is linearly related to the improvement of SVA and PT. Cho et al 2 reported that the average correction of LL is 33° with an average of 10.7° per level in multi-level SPO and 31.7° in single-level PSO respectively. This present study found that LL is increased from 19.1° preoperatively to 39.6° postoperatively with a mean difference of 20.6° in OLIF group and -1° preoperatively to 73.2° postoperatively with a mean difference of 74.2° in OLIF with PCO group, respectively. The average correction of LL per lumbar fusion level is 6.9° in OLIF group and 14.8° in OLIF with PCO group, respectively. Kim et al 18 reported that the average correction of LL is 40.7° with an average of 10.7° per level by releasing anterior longitudinal ligament (ALL) and using a lordotic cage in multi-level OLIF for ASD. These results indicated that releasing ALL and using a lordotic cage in multi-level OLIF for ASD could achieve similar LL correction compared to multi-level SPO. Besides, these results also indicated that OLIF combined with PCO could obtain adequate LL correction in the treatment of severe lumbar kyphosis, thereby avoiding huge surgical injury caused by traditional 3-column osteotomy. In addition, this study found that the average correction of TK is 9.4° in OLIF group and 31.30° in OLIF with PCO group, respectively, which indicated that OLIF combined with PCO is necessary to obtain adequate correction of sagittal imbalance for patients with marked thoracic kyphosis deformity.
Correction of Coronal Imbalance
This study found that the average correction of Cobb is 16.4°, with an average of 4.7° per level in OLIF group. Bekmez et al 40 reported that the average correction of Cobb is 56.1° with an average of 11.2° per level in multi-level SPO and 66.7° in single-level PSO respectively. These results showed that OLIF is effective for mild or moderate lumbar coronal deformity, but OLIF combined with multi-level SPO or PSO is also effective for severe coronal deformity.
Fusion Rate
The present study found that the average fusion rate is up to 94.1%, which may be related to the placement of larger cage in OLIF surgery.
In a word, OLIF can achieve satisfactory improvement of radiographic parameters in the treatment of mild and moderate ASD.
Complications
Many previous studies2-8,41 on various osteotomies for ASD reported that the overall complication rate ranges from 42% to 69.2% and the major complication rate ranges from 20% to 46%, including pseudarthrosis (10%-24%), PJK (7.7%-34%), neurological deficit (6.3%-18.1%), rod breakage (4.4%-14.7%), dural tear (3.3%-23.1%) and wound infection (6.5%). Besides, many studies2-5,7,8 found that the incidence of perioperative complications and major complications increased significantly as the extent of spinal osteotomy expanded. Furthermore, since ASD is more common in the elderly, the risk of surgery is higher. Daubs et al 41 found that the major complication rate of patients older than 69 years are 9 times that of patients younger than 69 years in osteotomies for spinal deformity. Therefore, the surgical treatment of ASD should be as minimally invasive as possible to reduce the incidence of perioperative complications. 10 The present meta-analysis showed that the overall complication rate of OLIF is 34.5% and the major complication rate is lower. The most complications are transient thigh pain or numbness and hip flexor weakness or pain (9.4%), cage subsidence (5.7%), proximal junctional kyphosis (4.7%), ileus (3.7%), sympathetic chain (2.2%) and vascular (1.5%) injury. The transient thigh pain/numbness and hip flexor weakness/pain may be related to the intraoperative pulling and stimulating of the psoas or postoperative hematoma.42 Since most of the patients in this study were female and elderly, osteoporosis was the main pathological basis for intraoperative endplate injury and postoperative cage subsidence. 42 PJK may be related to osteoporosis and fusion to pelvis. 27 The postoperative ileus may be related to stimulating of the intraoperative peritoneum. 42 The sympathetic chain injury mainly occurred during pulling psoas. 42 The vascular injury mainly included segmental vessels and iliac vessels injury, which was more common in patients with anatomical variation. 42 Most complications of OLIF surgery were transient and the major complication rate was lower. Thus, OLIF is an safe surgery method in the treatment of ASD.
Conclusions
OLIF combined with posterior or lateral fixation was effective and safe in the treatment of mild and moderate ASD. It has advantages in less intraoperative blood loss and lower perioperative complication rate. However, OLIF combined with PCO may be needed to obtain sufficient correction of coronal and sagittal deformity to reduce the need of 3-column osteotomy in ASD with severe coronal and sagittal imbalance.
Footnotes
Authors’ Note: Lei Zhu and Jun-Wu Wang contributed equally to this work.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by National Natural Science Foundation of China [81 401 830]; Jiangsu Provincial Medical Youth Talent [QNRC2016342]; Project on Maternal and Child Health Talents of Jiangsu Province [F201801]; and Six Talent Peaks Project in Jiangsu Province [LGY2019035].
ORCID iDs: Lei Zhu, MM  https://orcid.org/0000-0001-8556-2077
https://orcid.org/0000-0001-8556-2077
Liang Zhang, MD  https://orcid.org/0000-0002-1475-495X
https://orcid.org/0000-0002-1475-495X
Xin-Min Feng, MD  https://orcid.org/0000-0001-9287-858X
https://orcid.org/0000-0001-9287-858X
References
- 1.Heary RF, Kumar S, Bono CM. Decision making in adult deformity. Neurosurgery. 2008;63(3):69–77. [DOI] [PubMed] [Google Scholar]
- 2.Cho KJ, Bridwell KH, Lenke LG, Berra A, Baldus C. Comparison of Smith-Petersen versus pedicle subtraction osteotomy for the correction of fixed sagittal imbalance. Spine (Phila Pa 1976). 2005;30(18):2030–2037. [DOI] [PubMed] [Google Scholar]
- 3.Iyer S, Nemani VM, Kim HJ. A review of complications and outcomes following vertebral column resection in adults. Asian Spine J. 2016;10(3):601–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: prevalence and risk factor analysis of 144 cases. Spine (Phila Pa 1976). 2006;31(20):2329–2336. [DOI] [PubMed] [Google Scholar]
- 5.Buchowski JM, Bridwell KH, Lenke LG, et al. Neurologic complications of lumbar pedicle subtraction osteotomy: a 10-year assessment. Spine (Phila Pa 1976). 2007;32(20):2245–2252. [DOI] [PubMed] [Google Scholar]
- 6.Abdul-Jabbar A, Takemoto S, Weber MH, et al. Surgical site infection in spinal surgery: description of surgical and patient-based risk factors for postoperative infection using administrative claims data. Spine (Phila Pa 1976). 2012;37(15):1340–1345. [DOI] [PubMed] [Google Scholar]
- 7.Bianco K, Norton R, Schwab F, et al. Complications and intercenter variability of three-column osteotomies for spinal deformity surgery: a retrospective review of 423 patients. Neurosurg Focus. 2014;36(5):E18. [DOI] [PubMed] [Google Scholar]
- 8.Kelly MP, Lenke LG, Shaffrey CI, et al. Evaluation of complications and neurological deficits with three-column spine reconstructions for complex spinal deformity: a retrospective Scoli-RISK-1 study. Neurosurg Focus. 2014;36(5):E17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Phillips FM, Isaacs RE, Rodgers WB, et al. Adult degenerative scoliosis treated with XLIF: clinical and radiographical results of a prospective multicenter study with 24-month follow-up. Spine (Phila Pa 1976). 2013;38(21):1853–1861. [DOI] [PubMed] [Google Scholar]
- 10.Mummaneni PV, Shaffrey CI, Lenke LG, et al. The minimally invasive spinal deformity surgery algorithm: a reproducible rational framework for decision making in minimally invasive spinal deformity surgery. Neurosurg Focus. 2014;36(5):E6. [DOI] [PubMed] [Google Scholar]
- 11.Silvestre C, Mac-Thiong JM, Hilmi R, Roussouly P. Complications and morbidities of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lumbar interbody fusion in 179 patients. Asian Spine J. 2012;6(2):89–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fujibayashi S, Hynes RA, Otsuki B, Kimura H, Takemoto M, Matsuda S. Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine (Phila Pa 1976). 2015;40(3):E175–182. [DOI] [PubMed] [Google Scholar]
- 13.Anand N, Alayan A, Agrawal A, Kahwaty S, Nomoto E, Khandehroo B. Analysis of spino-pelvic parameters and segmental lordosis with L5-S1 oblique lateral interbody fusion at the bottom of a long construct in circumferential minimally invasive surgical correction of adult spinal deformity. World Neurosurg. 2019;130:e1077–e1083. [DOI] [PubMed] [Google Scholar]
- 14.Park SW, Ko MJ, Kim YB, Le Huec JC. Correction of marked sagittal deformity with circumferential minimally invasive surgery using oblique lateral interbody fusion in adult spinal deformity. J Orthop Surg Res. 2020;15(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ohtori S, Mannoji C, Orita S, et al. Mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for degenerated lumbar spinal kyphoscoliosis. Asian Spine J. 2015;9(4):565–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–34. [DOI] [PubMed] [Google Scholar]
- 17.The National Heart Lung and Blood Institute. Quality assessment tool for case series studies. Accessed August 12, 2020. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
- 18.Kim KT, Jo DJ, Lee SH, Seo EM. Oblique retroperitoneal approach for lumbar interbody fusion from L1 to S1 in adult spinal deformity. Neurosurg Rev. 2018;41(1):355–363. [DOI] [PubMed] [Google Scholar]
- 19.He D, He W, Sun YQ, et al. A comparative study of the efficacy and complications of oblique lumbar interbody fusion and transforaminal lumbar interbody fusion in lumbar degenerative scoliosis [in Chinese]. Chin J Orthopaedics. 2020;40(8):515–525. [Google Scholar]
- 20.Zhao X, Fan SW, Fang XQ, et al. Clinical value of oblique lateral interbody fusion in the treatment of adult degenerative scoliosis [in Chinese]. Chin J Orthopaedics. 2017;37(16):989–996. [Google Scholar]
- 21.Patel RS, Suh SW, Kang SH, et al. The radiologic and clinical outcomes of oblique lateral interbody fusion for correction of adult degenerative lumbar deformity. Indian J Orthop. 2019;53(4):502–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang K, Zhang C, Cheng C, Jian F, Wu H. Radiographic and clinical outcomes following combined oblique lumbar interbody fusion and lateral instrumentation for the treatment of degenerative spine deformity: a preliminary retrospective study. Biomed Res Int. 2019;2019:5672162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abbasi H, Miller L, Abbasi A, Orandi V, Khaghany K. Minimally invasive scoliosis surgery with oblique lateral lumbar interbody fusion: single surgeon feasibility study. Cureus. 2017;9(6):e1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee KY, Lee JH, Kang KC, et al. Minimally invasive multilevel lateral lumbar interbody fusion with posterior column osteotomy compared with pedicle subtraction osteotomy for adult spinal deformity. Spine J. 2020;20(6):925–933. [DOI] [PubMed] [Google Scholar]
- 25.Mehren C, Wanke-Jellinek L, Krenauer A, Korge A. The mono- and multisegmental ventral minimally invasive approach to the lumbar spine (OLIF) in lumbar deformities [in German]. Oper Orthop Traumatol. 2020;32(3):200–208. [DOI] [PubMed] [Google Scholar]
- 26.Lui DF, Butler JS, Yu HM, et al. Neurologic injury in complex adult spinal deformity surgery: staged multilevel oblique lumbar interbody fusion (MOLIF) using hyperlordotic tantalum cages and posterior fusion versus pedicle subtraction osteotomy (PSO). Spine (Phila Pa 1976). 2019;44(16):E939–E949. [DOI] [PubMed] [Google Scholar]
- 27.Koike Y, Kotani Y, Terao H, Iwasaki N. Risk factor analysis of proximal junctional kyphosis after surgical treatment of adult spinal deformity with oblique lateral interbody fusion. Asian Spine J. 2020. 10.31616/asj.2019.0341 [DOI] [PMC free article] [PubMed]
- 28.Wu XL, Huang JJ. Lateral anterior retroperitoneal lumbar interbody fusion combined with posterior pedicle screw fixation via Wiltse approach for the treatment of 38 cases of degenerative scoliosis [in Chinese]. Shandong Med J. 2019;59(24):72–75. [Google Scholar]
- 29.Fang Z, Xu Y, Gao F, et al. Clinical and radiographic evaluation of oblique lumbar interbody fusion combined with posterior surgery via Wiltse approach for adult degenerative scoliosis [in Chinese]. Zhonghua Yi Xue Za Zhi. 2020;100(27):2132–2137. [DOI] [PubMed] [Google Scholar]
- 30.Xu ZJ, Hao YJ, Yu L, et al. Oblique lumbar interbody fusion for degenerative lumbar scoliosis [in Chinese]. Orthopedic Journal of China. 2020;28(13):1185–1190. [Google Scholar]
- 31.Pritchett JW, Bortel DT. Degenerative symptomatic lumbar scoliosis. Spine (Phila Pa 1976). 1993;18(6):700–703. [DOI] [PubMed] [Google Scholar]
- 32.Schwab F, Blondel B, Chay E, et al. The comprehensive anatomical spinal osteotomy classification. Neurosurgery. 2015;76:S33–41. [DOI] [PubMed] [Google Scholar]
- 33.Zhang Y, Tao L, Hai Y, et al. One-stage posterior multiple-level asymmetrical Ponte osteotomies versus single-level posterior vertebral column resection for severe and rigid adult idiopathic scoliosis: a minimum 2-year follow-up comparative study. Spine (Phila Pa 1976). 2019;44(20):E1196–E1205. [DOI] [PubMed] [Google Scholar]
- 34.Shi B, Zhao Q, Xu L, et al. SRS-Schwab Grade 4 osteotomy for congenital thoracolumbar kyphosis: a minimum of 2 years follow-up study. Spine J. 2018;18(11):2059–2064. [DOI] [PubMed] [Google Scholar]
- 35.Suk SI, Chung ER, Kim JH, Kim SS, Lee JS, Choi WK. Posterior vertebral column resection for severe rigid scoliosis. Spine (Phila Pa 1976). 2005;30(14):1682–1687. [DOI] [PubMed] [Google Scholar]
- 36.Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976). 2005;30(18):2024–2029. [DOI] [PubMed] [Google Scholar]
- 37.Lafage V, Schwab F, Patel A, Hawkinson N, Farcy JP. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976). 2009;34(17):E599–606. [DOI] [PubMed] [Google Scholar]
- 38.Schwab F, Ungar B, Blondel B, et al. Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976). 2012;37(12):1077–1082. [DOI] [PubMed] [Google Scholar]
- 39.Lafage V, Schwab F, Vira S, et al. Does vertebral level of pedicle subtraction osteotomy correlate with degree of spinopelvic parameter correction? J Neurosurg Spine. 2011;14(2):184–191. [DOI] [PubMed] [Google Scholar]
- 40.Bekmez S, Ozhan M, Olgun ZD, et al. Pedicle subtraction osteotomy versus multiple posterior column osteotomies in severe and rigid neuromuscular scoliosis. Spine (Phila Pa 1976). 2018;43(15):E905–E910. [DOI] [PubMed] [Google Scholar]
- 41.Daubs MD, Lenke LG, Cheh G, Stobbs G, Bridwell KH. Adult spinal deformity surgery: complications and outcomes in patients over age 60. Spine (Phila Pa 1976). 2007;32(20):2238–2244. [DOI] [PubMed] [Google Scholar]
- 42.Zeng ZY, Xu ZW, He DW, et al. Complications and prevention strategies of oblique lateral interbody fusion technique. Orthop Surg. 2018;10(2):98–106. [DOI] [PMC free article] [PubMed] [Google Scholar]