Abstract
Patient: Male, 35-year-old
Final Diagnosis: Negative-pressure pulmonary edema
Symptoms: Difficult airway management
Medication:—
Clinical Procedure: —
Specialty: Anesthesiology • Critical Care Medicine
Objective:
Unusual clinical course
Background:
Difficult tracheal intubation (DTI) is common in patients with rheumatoid arthritis (RA) because of the subluxation of atlas and axis, the fusion of the cervical spine as a result of arthritis. We report a case of negative-pressure pulmonary edema (NPPE) caused by DTI in a patient with juvenile RA (JRA) who underwent surgery for spigelian hernia.
Case Report:
A 35-year-old man was referred to our department for repeated abdominal pain and a left-lower quadrant mass. Spigelian hernia was diagnosed with abdominal computed tomography (CT), and surgery was scheduled. Despite careful preoperative preparation and intubation strategy, fiber-optic intubation and laryngeal mask ventilation failed; nasal fiber-optic tracheal intubation was subsequently successfully performed. During induction, upper airway obstruction caused NPPE. CT findings showed bilateral infiltration and diffuse ground-glass opacity suggestive of pulmonary edema. Surgery for the spigelian hernia was canceled as the patient required intensive care as a result of NPPE. After 48 h of initiating treatment, the patient’s respiratory condition gradually improved. Seven days after DTI, he underwent laparoscopy-assisted surgery for the spigelian hernia. The patient was discharged after 2 weeks of hospitalization. Four years have passed since the surgical procedure; the outcome has remained favorable and there has been no recurrence.
Conclusions:
Normal ventilation may be the most important factor for preventing NPPE. It is vital that patients with RA receive treatment in an environment with advanced airway equipment and staff fully trained in its use. Similarly, the necessary staff and equipment for emergency cricothyroidotomies should also be readily available.
Keywords: Airway Management; Hernia, Abdominal; Pulmonary Edema; Rheumatoid Arthritis, Systemic Juvenile
Background
Difficult tracheal intubation (DTI) is common in patients with juvenile rheumatoid arthritis (JRA) because of the subluxation of the atlas and axis, the fusion of the cervical spine as a result of arthritis, glottis stenosis caused by inflammation of the cricoarytenoid cartilage, and a defect in the palate [1]. Spigelian hernia, which accounts for less than 2% of all hernias, is a spontaneous abdominal hernia caused by a defect in the spigelian fascia [2], which is located between the semi-lunar line and the lateral edge of the rectus abdominis muscle. However, spigelian hernia in association with JRA has not been previously reported. Also, negative-pressure pulmonary edema (NPPE), recognized as a serious consequence of severe hypoxia, is rare. NPPE is caused by forceful inspiration against the upper airway obstruction, which causes significant negative-pressure on the lung and results in pulmonary edema [3]. We herein report a case of NPPE that resulted from DTI in a patient with JRA who underwent surgery for spigelian hernia. This case report was reviewed and approved by the Ethics Committee of Kurume University School of Medicine (no. 2021–033). Written informed consent for publication was obtained from the patient.
Case Report
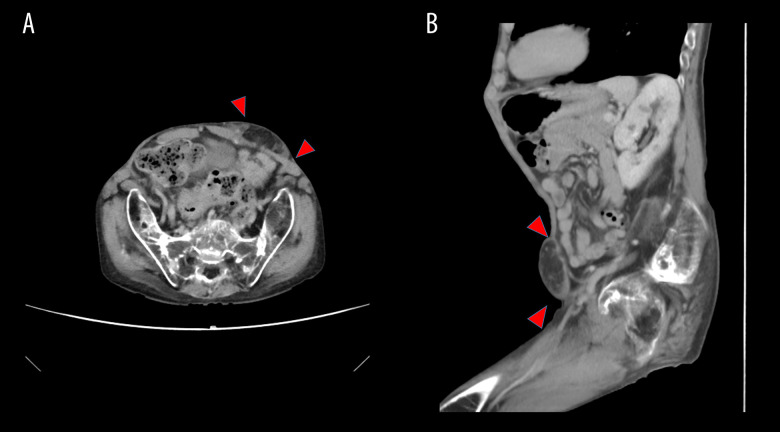
A 35-year-old man (height, 110 cm; weight, 19.5 kg) presented with a 6-year history of abdominal pain and a left-lower quadrant mass and was referred to our department because his symptoms became frequent. JRA was diagnosed when he was 2 years old, and he used a wheelchair because of the deformity of his limbs. Clinical examination revealed a mass of approximately 5×5 cm in the left lower abdomen. Abdominal wall ultrasonography showed a mass with mixed echoic signals under the muscle layer of the left lower abdominal wall. Abdominal contrast medium-enhanced computed tomography (CT) revealed that the mass had low signal attenuation, which suggested that mesenteric fat was present between the thin ventral muscles in the left lower abdominal wall. Therefore, spigelian hernia was diagnosed (Figure 1).
Figure 1.
Abdominal contrast-enhanced computed tomography scan showing a spigelian hernia in a patient with juvenile rheumatoid arthritis. (A, B) Abdominal contrast-enhanced computed tomography (CT) scan. Abdominal contrast medium-enhanced CT revealed a mass of low signal attenuation, which suggested the presence of mesenteric fat between the thin ventral muscles in the left-lower abdominal wall (red arrow).
The patient had never had an operation or intubation before presenting to our department. He had a short neck with very limited movement. The maximum opening of his mouth was 3 cm in interincisional distance. The patient belonged to class II of the Mallampati classification because his soft palate, posterior palatine arch, and partial uvula were visible (Figure 2). When breathing spontaneously, the patient’s oxygen saturation (SpO2) level was 100%. Therefore, we expected that endotracheal intubation would not be easy. After the hernia was diagnosed, our team considered counseling this patient on simple expectant management. However, the patient wanted to undergo surgery because of his symptoms. One week before the scheduled spigelian hernia surgery, we referred him to an anesthesiologist. The patient’s spinal deformity was so pronounced that he could not be positioned for spinal anesthesia, and he wanted a general anesthetic. The anesthesiologist considered that endotracheal intubation could be accomplished via fiber-optic bronchoscopy or laryngoscopy or that endotracheal intubation could be performed while the patient was awake.
Figure 2.
(A, B) The patient’s neck was short and had very limited movement. The maximum mouth opening was 3 cm in interincisional distance.
On the day of the surgery, before administering 40 mg of propofol, the patient was administered oxygen for 5 min by an anesthesiologist. With spontaneous breathing, his vital signs were blood pressure 128/68 mmHg, heart rate 82 beats/min, and SpO2 100%. The patient was ventilated using a bag valve mask, and 12 mg of rocuronium was injected to relax the trachea in preparation for intubation. At this point, the patient’s ventilation abruptly failed. The patient had difficulty moving his jaw, and his airway became obstructed. Although i-gel (Intersurgical Ltd, Wokingham, UK) was inserted to facilitate ventilation, it was obstructed by the patient’s lockjaw, and ventilation was not possible. An emergency call was made, and we prepared for emergency surgical airway creation. Fiber-optic intubation and the subsequent laryngeal mask ventilation were attempted by 2 anesthesiologists for 5 min, but the attempts were unsuccessful owing to high airway resistance. This led to bradycardia (40 beats/min) and a drop in SpO2 to 60%. Cardiac massage was performed for 20 s, and the heart rate was recovered. The otolaryngologist prepared the emergency cricothyroidotomy. At the same time, 3 anesthesiologists advanced a 6.5-F tracheal tube into the oral cavity through the right nasal passage using a fiberoptic bronchoscope. Nasotracheal intubation was successfully achieved. After intubation, the bronchoscope showed no airway abnormalities, such as stenosis or obstruction. However, the patient’s SpO2 was only 93% with the fraction of inspired oxygen (FiO2) at 100%. NPPE was suspected owing to the presence of pink-colored foamy bloody secretion. Therefore, the surgical procedure for spigelian hernia was canceled. Thirty minutes after intubation, the patient was transferred to the Intensive Care Unit.
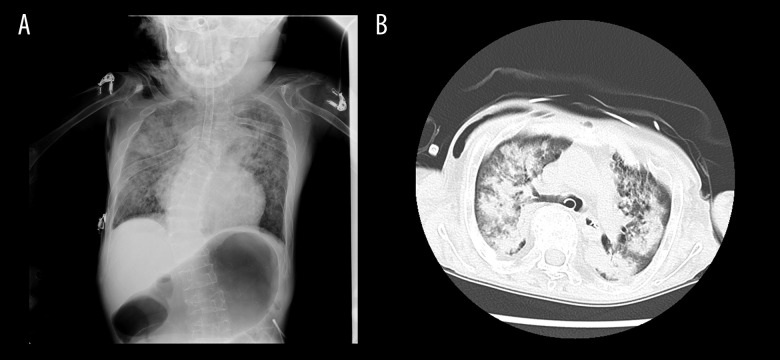
A chest radiograph after intubation showed pulmonary edema in both lobes and no cardiomegaly. The patient’s gastric distension and neck aerodermectasia were likely caused by insufflation of the stomach in response to the attempted positive-pressure ventilation via face mask. A chest CT showed bilateral infiltration and diffuse ground-glass opacity suggestive of pulmonary edema (Figure 3). The patient’s postoperative cardiac enzyme levels were tested, and an ultrasonic cardiogram was performed. We diagnosed NPPE on the basis of the CT findings, because the partial pressure of arterial oxygen (PaO2)/fraction of inspired oxygen (FiO2) ratio was <200 mmHg (68.6 mmHg) and because the FiO2 was <100%. The patient was administered sivelestat sodium hydrate (100 mg/day) and furosemide (20 mg/day). After 48 h, his respiratory condition showed gradual improvement. After 3 days from starting treatment, the PaO2/FiO2 ratio and radiographic findings gradually improved (PaO2/FiO2 increased to >300 mmHg); he was then weaned from mechanical ventilation. Blood gas sample analysis showed a pH of 7.52, partial pressure of oxygen (PO2) of 159 mmHg, and partial pressure of carbon dioxide (PCO2) of 31.7 mmHg. To avoid a further DTI, we planned to extubate the patient after the spigelian hernia surgery.
Figure 3.
Chest computed tomography scan of a patient with juvenile rheumatoid arthritis after difficult endotracheal intubation. (A) Chest radiograph after intubation showed pulmonary edema in both lobes and no cardiomegaly. (B) Chest computed tomography showed bilateral infiltration and diffuse ground-glass opacities, which were suggestive of pulmonary edema.
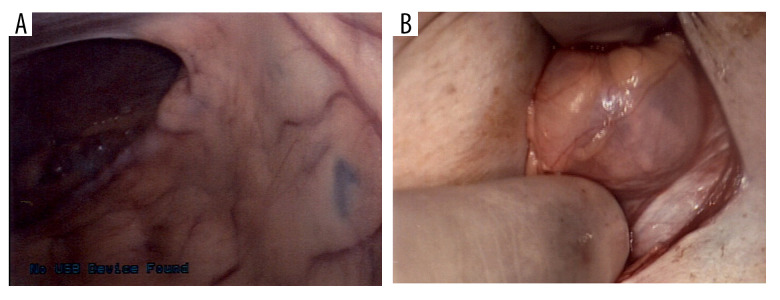
Seven days after the DTI, he underwent laparoscopy-assisted surgery for the spigelian hernia. The hernia content was omentum, and the defect size was 2.0×2.0 cm (Figure 4). Because of the small size of the defect and in view of the comorbidity of JRA, we performed a simple herniorrhaphy to avoid postoperative surgical site infection. The perioperative course was uneventful, and the patient was extubated 4 days after the surgery. The patient had been mechanically ventilated for a total of 10 days. Blood gas sample analysis performed after extubation showed a pH of 7.47, PO2 of 151 mmHg, and PCO2 of 40.3 mmHg. The patient was discharged after 2 weeks of hospitalization. In the 4 years since the surgical procedure, his outcome has been favorable, without recurrence.
Figure 4.
A spigelian hernia from a patient with juvenile rheumatoid arthritis. (A, B) The hernia content was omentum, and the defect size was 2.0×2.0 cm.
Discussion
Airway management for general anesthesia in patients with RA can be challenging because of the anomalies of the temporomandibular joint and cervical spine. In this case, the patient’s spinal deformity was so pronounced that he could not be positioned for spinal anesthesia. Therefore, general anesthesia was chosen. The intubation techniques for these patients have been under debate. Video laryngoscopy and fiber-optic bronchoscopy are reported to be significantly helpful in securing tracheal intubation in such patients [4]. Alternatively, when a difficulty of airway securement is anticipated, endotracheal intubation via fiber-optic bronchoscopy while the patient is awake is considered the safest. On the other hand, Johnson et al reported that the failure rate of first attempts at endotracheal intubation via fiber-optic bronchoscopy is high (approximately 53.3%), which means that sufficient skill and experience with tracheal intubation are necessary [5].
According to the Japanese Society of Anesthesiologists Airway Management, other medical staff, including a senior anesthesiologist, should be prepared for DTI emergencies [6]. However, in practice, the timing of requesting support for a DTI remains controversial because deciding immediately how to respond in such an emergency is quite difficult for a single anesthesiologist. Several algorithms related to airway management difficulties have been developed. According to the algorithms, if oxygenation cannot be maintained with face-mask ventilation or supraglottic airway after general anesthesia induction, anesthesiologists should prepare for the possible need for an emergency front-of-neck airway. However, there should first be a final attempt at any untried approach (face-mask ventilation, supraglottic airway, or tracheal intubation) for ensuring neuromuscular blockade [7]. Therefore, multiple anesthesiologists, as well as surgeons, must perioperatively share the patient’s clinical information and understand the intubation strategy in case of DTI emergencies. Also, the patient and the family should be informed that intubation can fail. Considering the possibility of a DTI emergency, patient consent should be obtained from the patient for an emergency cricothyroidotomy.
An analysis of closed civil cases involving anesthesiologists reported by the Canadian Medical Protective Association showed that 46 of the 406 cases analyzed (11%) were related to problems with airway management. The outcomes in the majority of these cases were severe, with death or permanent brain damage in 31% of the 46 cases. Inadequate preoperative airway evaluation was the most common error (accounting for 59% of the cases) [8]. Our patient had a short neck with very limited movement, and the maximum interincisional distance with which he could open his mouth was 3 cm. Therefore, surgeons were able to anticipate DTI during the induction of anesthesia and referred the patient to an anesthesiologist 1 week before surgery to ensure that proper preparations were made and the most appropriate approaches selected.
Performing fiberoptic bronchoscopy or laryngoscopy while the patient was still awake was considered, but only 1 anesthesiologist anesthetized the patient. Difficult airway management requires a preformulated strategy. The foremost consideration is an evaluation of the clinical advantages and disadvantages of intubation while the patient is awake versus while he is asleep [9]. Conventional flexible bronchoscopic intubation of conscious patients has been described as the criterion standard for securing the airway in patients at risk of difficult airway intubation. The clinician should be prepared for the potential difficulties specific to every case and should attain and maintain competence in the required techniques. In hindsight, flexible bronchoscopic intubation performed while our patient was awake might have been the best option, but the number of staff available was not sufficient. Anesthetists should share the clinical information of each patient and have an emergency intubation strategy prepared in case of DTI emergencies. We have learned from this experience the importance of consultation with pediatricians and anesthesiologists for high-risk cases, regardless of the airway.
NPPE is a type of noncardiogenic pulmonary edema mainly caused by high negative intrathoracic pressure that has resulted from upper airway obstruction. It is reported to occur in 0.1% of cases of general anesthesia with tracheal intubation, mostly as a result of laryngospasm [10]. Furthermore, specific characteristics, especially a short neck, difficulty in intubation, endotracheal tube obstruction, history of obstructive sleep apnea, obesity, acromegaly, and history of upper aerodigestive tract surgery, can increase the susceptibility to this condition [11]. NPPE is of 2 types: type 1 develops after sudden and intense obstruction of the airway, such as postextubation laryngospasm and epiglottitis, and type 2 develops after the surgical release of chronic airway obstruction, such as the resection of laryngeal tumor, adenoids/tonsils, or intrathoracic goiters [3]. In the present case, none of these criteria for either NPPE type were identified in advance. However, the mild collapse of the suprasternal fossa and a rigid jaw during the induction phases predicted the possibility of upper airway obstruction. Most cases of NPPE resolve within 24 to 48 h when properly treated [3]. The rate of mortality from NPPE was previously described as ranging from 11% to 40%, but a more recent literature review revealed a 2% mortality rate [12].
The primary treatment for NPPE includes positive-pressure ventilation and supplemental oxygenation, according to prior studies [13]. The most common adjunct treatment is the use of diuretics [14]. However, the use of medicines such as diuretics and steroids is heavily debated, and there are, as yet, no definitive guidelines on their use [15]. To the best of our knowledge, 1 patient with RA had acute pulmonary edema as a result of a DTI [16]. In that case, laryngeal mask airway-guided fiber-optic intubation was succeeded after failure of direct tracheal intubation and fiber-optic intubation. In our patient, after failure of fiber-optic intubation and subsequent laryngeal mask oxygenation, nasal fiber-optic intubation successfully secured the airway. In the situation of a DTI in patients with RA, fiber-optic intubation guided through a laryngeal mask [17] or glide scope-assisted fiber-optic bronchoscopy [18] was also reported to have been successfully accomplished. According to those reports, the combination of the 2 devices to facilitate intubation seems to be useful for patients with RA. In our patient, even with careful preoperative assessment, such as prior evaluation by an anesthesiologist, we encountered severe difficulty with securing the airway, although we were able to avoid emergency tracheostomy. NPPE may be well recognized by anesthesiologists and intensivists, but it may not be familiar to other medical specialists. Therefore, it is important for surgeons to recognize NPPE as a potential complication in all patients who develop hypoxia in the perioperative period, and perioperative strategies are improved by close collaboration and sharing of patient’s clinical information among surgeons, pediatricians, and anesthesiologists.
Conclusions
A DTI occurred in a patient with JRA who was to undergo surgery for spigelian hernia. Fortunately, subsequent NPPE was successfully managed with mechanical ventilation. According to the findings of previous reports and our experience, for patients with JRA who require surgery, both extra intubation equipment and a sufficient number of skilled backup staff should be prepared for DTI, as well as for preoperative management and intubation strategies. Normal ventilation may be the most important factor for preventing NPPE. It is vital that patients with RA receive treatment in an environment with advanced airway equipment and staff fully trained in its use.
Similarly, the necessary staff and equipment for emergency cricothyroidotomies should also be readily available.
Acknowledgments
We would like to thank Enago (https://www.enago.jp) for English language editing.
Footnotes
Declaration of Figures; Authenticity
All figures submitted have been created by the authors who confirm that the images are original with no duplication and have not been previously published in whole or in part.
References:
- 1.Takenaka I, Aoyama K, Iwagaki T, et al. Fluoroscopic observation of the occipitoatlantoaxial complex during intubation attempt in a rheumatoid patient with severe atlantoaxial subluxation. Anesthesiology. 2009;111(4):917–19. doi: 10.1097/ALN.0b013e3181b31e41. [DOI] [PubMed] [Google Scholar]
- 2.Webber V, Low C, Skipworth RJE, et al. Contemporary thoughts on the management of Spigelian hernia. Hernia. 2017;21(3):355–61. doi: 10.1007/s10029-017-1579-x. [DOI] [PubMed] [Google Scholar]
- 3.Udeshi A, Cantie SM, Pierre E. Postobstructive pulmonary edema. J Crit Care. 2010;25(3):508. doi: 10.1016/j.jcrc.2009.12.014. e1–5. [DOI] [PubMed] [Google Scholar]
- 4.Niforopoulou P, Pantazopoulos I, Demestiha T, et al. Video-laryngoscopes in the adult airway management: A topical review of the literature. Acta Anaesthesiol Scand. 2010;54(9):1050–61. doi: 10.1111/j.1399-6576.2010.02285.x. [DOI] [PubMed] [Google Scholar]
- 5.Johnson DM, From AM, Smith RB, et al. Endoscopic study of mechanisms of failure of endotracheal tube advancement into the trachea during awake fiberoptic orotracheal intubation. Anesthesiology. 2005;102(5):910–14. doi: 10.1097/00000542-200505000-00008. [DOI] [PubMed] [Google Scholar]
- 6.JSA airway management guideline 2014: To improve the safety of induction of anesthesia. J Anesth. 2014;28(4):482–93. doi: 10.1007/s00540-014-1844-4. [DOI] [PubMed] [Google Scholar]
- 7.Heidegger T. Management of the difficult airway. N Engl J Med. 2021;384(19):1836–47. doi: 10.1056/NEJMra1916801. [DOI] [PubMed] [Google Scholar]
- 8.Crosby ET, Duggan LV, Finestone PJ, et al. Anesthesiology airway-related medicolegal cases from the Canadian Medical Protection Association. Can J Anesth. 2021;68(2):183–95. doi: 10.1007/s12630-020-01846-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Apfelbaum JL, Hagberg CA, Caplan RA, et al. Practice guidelines for management of the difficult airway: An updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013;118(2):251–70. doi: 10.1097/ALN.0b013e31827773b2. [DOI] [PubMed] [Google Scholar]
- 10.Deepika K, Kenaan CA, Barrocas AM, et al. Negative pressure pulmonary edema after acute upper airway obstruction. J Clin Anesth. 1997;9(5):403–8. doi: 10.1016/s0952-8180(97)00070-6. [DOI] [PubMed] [Google Scholar]
- 11.Halow KD, Ford EG. Pulmonary edema following post-operative laryngospasm: A case report and review of the literature. Am Surg. 1993;59(7):443–47. [PubMed] [Google Scholar]
- 12.Westreich R, Sampson I, Shaari CM, Lawson W. Negative-pressure pulmonary edema after routine septorhinoplasty: Discussion of pathophysiology, treatment, and prevention. Arch Facial Plast Surg. 2006;8(1):8–15. doi: 10.1001/archfaci.8.1.8. [DOI] [PubMed] [Google Scholar]
- 13.Lemyze M, Mallat J. Understanding negative pressure pulmonary edema. Intensive Care Med. 2014;40(8):1140–43. doi: 10.1007/s00134-014-3307-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Din Lovinescu C, Trivedi U, Zhang K, et al. Systematic review of negative pressure pulmonary edema in otolaryngology procedures. Ann Otol Rhinol Laryngol. 2021;130(3):245–53. doi: 10.1177/0003489420938817. [DOI] [PubMed] [Google Scholar]
- 15.Liu R, Wang J, Zhao G, Su Z. Negative pressure pulmonary edema after general anesthesia: A case report and literature review. Medicine. 2019;98(17):e15389. doi: 10.1097/MD.0000000000015389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jeong JS, Jun JH, Song HJ, Choi SH. Acute pulmonary edema due to hypoxia during a difficult intubation in a rheumatoid arthritis patient. Korean J Anesthesiol. 2014;67:S74–76. doi: 10.4097/kjae.2014.67.S.S74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lim BG, Lee MK, Kong MH, et al. Fiberoptic intubation through a laryngeal mask airway as a management of difficult airwary due to the fusion of the entire cervical spine – a report of two cases. Korean J Anesthesiol. 2012;62(3):272–76. doi: 10.4097/kjae.2012.62.3.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gu J, Xu K, Ning J, et al. GlideScope-assisted fiberoptic bronchoscope intubation in a patient with severe rheumatoid arthritis. Acta Anaesthesiol Taiwan. 2014;52(2):85–87. doi: 10.1016/j.aat.2014.04.002. [DOI] [PubMed] [Google Scholar]