Abstract
Pigmented villonodular synovitis is a rare proliferative process, especially in children. Pigmented villonodular synovitis can affect the synovial joint, tendon sheaths, and bursa membranes. Within synovial joint involvement, it is commonly seen in the knee joint but hip, ankle, shoulder, wrist, and other joints can be involved. The appearance characteristic is found on a magnetic resonance imaging scan. Complete excision and synovectomy are the usual treatment. In this article, we report a case of pigmented villonodular synovitis of the knee in a 12- year-old girl who underwent total synovectomy after the diagnosis was confirmed by biopsy. Three years after surgery, neither recurrence nor joint degeneration was found. The osteochondral defect at the tibial plateau was filled with calcium phosphate bone paste.
Keywords: Pigmented villonodular, Child; Knee; Synovitis
Introduction
Pigmented villonodular synovitis (PVNS) is a rare proliferative disease of synovial membranes, with characteristics of villonodular synovial hyperplasia and hemosiderin deposition [1]. At present, the standard treatment for pigmented villonodular synovitis has been surgical excision with total synovectomy of the affected joint [2]. If left untreated, the affected joint can become severe deformity, degenerative articular change, and articular destruction and finally lead to the risk of arthrodesis or amputation [2].
This thing leads to the need for early recognition of the clinical presentation and using imaging diagnosis to make an early and accurate diagnosis. Especially, due to the low incidence rates in pediatric populations, PVNS often is misdiagnosed with other diseases of synovial membranes leading to late diagnosis and severe articular destruction. Magnetic resonance imaging (MRI) plays an important role in early diagnosis and improving treatment outcomes, protecting joint function as well as the quality of life for children. In imaging diagnosis, MRI is the most appropriate imaging modality for detection and assessment of disease extent, biopsy guide, and PVNS treatment [1].
In this article, we describe a case of diffuse PVNS in a 12-year-old girl who was not properly diagnosed after going to several hospitals within 8 months. The patient was treated in several hospitals with the diagnosis of right knee effusion but the symptoms became worsened. When coming to our hospital, the patient underwent imaging examinations of the right knee joint including ultrasound, CT-scanner, and MRI. The features found on imaging suggested the diagnosis of diffuse PVNS. Then the patient was sent to a surgeon for appropriate treatment. This is a rare case of diffuse PVNS in children and misdiagnosed for a long time. Therefore, we report this case to emphasize the diffuse PVNS lesions that can occur in children, and we would like to share our experience in diagnosing PVNS and differentiating it from other lesions of the knee joint.
Case report
This study follows the case of a 12-year-old girl with recurrent pain and swelling in the right knee for 8 months. The patient was treated with knee joint aspiration many times with the diagnosis of right knee effusion - a rather vague diagnosis, but the symptoms became worsened. This time, she was admitted to National E hospital because the knee pain became more severe. She had no familial history of rheumatological conditions.
A physical examination of the patient revealed swelling and a limited range of motion in the knee. Laboratory investigations were normal.
The ultrasound of the right knee showed joint effusion measured 20 mm in thickness, hypoechoic and irregular thickening of the synovium (Fig. 1). On CT-scanner imaging of the right knee joint, there was the formation of subchondral bone cysts of the medial tibial plateau (Fig. 2A). The MRI imaging showed diffuse irregular thickening of the synovium, slightly hypointense in T1W, hypointense in T2W due to hemosiderin deposition, strong enhancement of the synovium after contrast-agent infusion, with knee effusion (Figs. 3A, 3B). We made the diagnosis of diffuse pigmented villonodular synovitis (diffuse PNVS) of the right knee joint.
Fig. 1.
Ultrasound.
Joint effusion (green arrow), with hypoechoic and irregular thickening of the synovium (red arrow).
Fig. 2.
Computed tomography.
Joint effusion (red arrow), diffuse irregular thickening of the synovium (yellow arrow), associated with the formation of subchondral bone cysts (blue arrow).
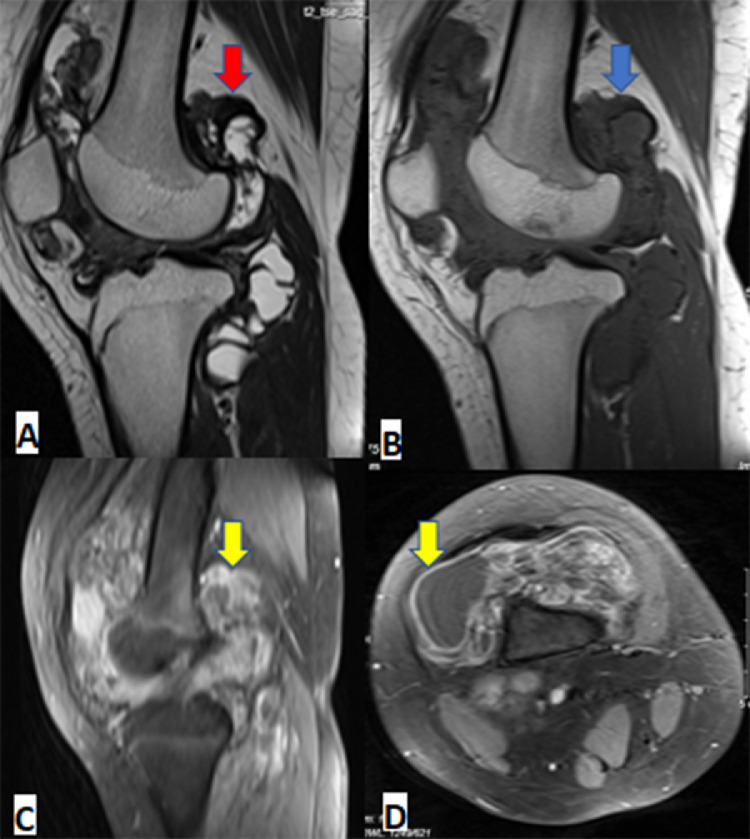
Fig. 3.
Magnetic resonance imaging.
Diffuse irregular thickening of the synovium in the knee joint, slightly hypointense in T1W (blue arrow), hypointense in T2W due to hemosiderin deposition (red arrow), after contrast the synovium show strong enhancement (yellow arrow).
Then the patient underwent laparoscopic surgery for total synovectomy (Fig. 4).
Fig. 4.
Knee arthroscopy: The knee synovial membrane is thickened, villonodular synovial hyperplasia throughout the posterior patellar space and the knee joint space. Nodular proliferation (green arrow), villous proliferation (red arrow).
The final diagnosis confirmed by the pathologist was diffuse pigmented villonodular synovitis (diffuse PNVS) of the right knee joint (Fig. 5). After surgery, the patient was given rehabilitation exercises at the Department of Rehabilitation of E hospital. After 3 years, the patient has recovered an almost complete range of motion of the knee joint without any pain.
Fig. 5.
Histopathology.
Microscopic sections show mononuclear cells admixed with osteoclast – like multinucleated giant cells and inflammatory cells
(HE A – 40x, B-100x).
Discussion
PVNS is a subtype of tenosyvial giant cell tumors that affect the soft tissue lining of joints and tendons. PVNS was first described in 1941 by Jaffe et al [3], who considered it as a benign disease with characteristics of focal or diffuse proliferative of villonodular synovial membranes and hemosiderin deposition. Only a small number of malignant transformation was reported. Nevertheless, the expansion of the tumor will cause moderate to severe range of motion limitations, maybe lead to joint stiffness and joint destruction at the late stage [2]. Translocations of chromosome 1p13 are present in the majority of PVNS cases. These translocations lead to overexpress colony-stimulating factor 1. The endpoint effect is clusters of aberrant cells form to create focal areas of soft tissue hyperplasia in the synovial cells lining joints [2].
PVNS is an uncommon disease with about 2 new cases per million population are diagnosed each year, statistically [4]. PVNS usually occurs between the 2nd and 5th decade of life [4]. This disease has been shown to have a lower incidence in children, hence the reason why cases of PVNS in children often go undiagnosed at the early stage [4]. Our patient is also a 12-year-old child who was initially misdiagnosed with knee bursitis and had a poor response to internal medicine treatment. The patient then was admitted to National E hospital and underwent a knee MRI with typical images of PVNS. The patient was satisfactorily treated with knee arthroscopy.
PVNS is classified into 2 types: localized and diffuse PNVS. Localized PVNS just involves the tendons that support the joint, or occurs in just one area of the joint. Diffuse PVNS is more widespread and involves an entire joint. Diffuse PVNS is more common and more difficult to treat [5]. The frequency of affected joints in descending order: knee joint (accounting for 66%-80%), hip, ankle, shoulder, and elbow [3]. The disease is most commonly monoarticular, rarely it can be oligoarticular [6]. In our case, the patient also showed a lesion to only the right knee joint.
PVNS usually progresses slowly. In the beginning, the patient has swelling and pain in the joints but the cause is unknown. The average time from the onset of symptoms to the time of diagnosis is about 18 months. The damage is gradual, leading to stiffness and articular destruction that limits the range of motion of the joint. Metastatic lesions of PVNS are extremely rare, however, there are some case reports of metastases to the lungs, muscles, and lymph nodes [8].
Features on plain radiographs are nonspecific. Bone density and joint space are preserved until the late stages. In the late stage, there is the sign of bone erosion creating subchondral bone defects and joint margin defects, osteoarthritis. Bone erosion is common in the hip because the joint space is smaller than the knee joint, with no space to decompress. Nevertheless, these features are nonspecific to distinguish PVNS from other synovial lesions such as synovial chondromatosis [1]. CT images show joint effusion, synovial thickening, and better assessment of bone lesions than plain radiograph [7]. Ultrasound is helpful in determining joint effusion, thickening, and hypoechoic of the synovial bursa and increased blood flow in the synovial membrane [3]. MRI has many advantages in the diagnosis and treatment of PVNS [9]. MRI is well suited for evaluating musculoskeletal structures like tendons, ligaments, synovial fluid, cartilage, and bone, thereby determining the extent of the damage. MRI also helps to provide detailed information of the lesions preoperatively and control disease recurrence [10].
With diffuse PVNS type, MRI shows diffuse irregular thickening of the synovial bursa (nodular or villiform). The synovial membrane is low to intermediate signal on T1-weighted image, low signal on T2-weighted image due to hemosiderin deposition, and is more prominent on the Gradient Echo (GE) sequence. In PVNS, the synovial membrane is strongly enhanced after contrast injection, which helps to distinguish from other diseases that also have low signal on T2W and GE due to intra-articular bleeding such as hemophilia, synovial hemangioma. In addition, MRI also helps to well evaluate erosive bone lesions, subchondral bone cysts, bone marrow edema, soft-tissue edema, and articular cartilage damage [1,11].
Histopathology is the gold standard for diagnosis [2]. On the macroscopic appearance, the joint fluid is usually dark brown or blood-colored due to hemosiderin deposition, the synovium is diffusely thickened with multiple villous and nodular projections. Microscopically, 2 typical cell types are monocytes and macrophages containing hemosiderin (a breakdown product of erythrocytes after recurrent bleeding and multinucleated osteoclasts) [2,3].
Biopsy should be performed under ultrasound guidance or during knee arthroscopy. The histological features of diffuse PVNS in the joint may simulate malignant proliferative lesions such as synovial sarcoma, rhabdomyosarcoma, or epithelial sarcoma. Therefore, the combination of histological features with clinical presentation and imaging characteristics helps to make an accurate diagnosis [2]. Ultrasound-guided biopsy is recommended, especially in patients who cannot completely exclude the possibility of malignancy in the joints [1,2].
Differential diagnoses of PVNS include rheumatoid arthritis, septic arthritis, synovial chondroma, synovial hemangioma, intra-articular fatty sarcoma, synovial sarcoma [2]. Rheumatoid arthritis is chronic bilateral symmetrical polyarthritis. The synovial membrane is irregularly thickened and enhanced after contrast injection. Rice bodies with intermediate signals may be seen, which are small, multiple, and free-floating rather than attached to the synovial bursa [12]. Synovial hemangioma (Venous malformation) is an uncommon intra - or extra-articular lesion. Lesions are strongly hyperintensity on fat-sat sequences and hypointensity on T1W. Venous malformations have low-flow blood vessels. Venous calcifications may be present [13]. In synovial chondromatosis, hyalinized cartilage shows an intermediate signal on T1W. There may be central calcifications in the hyaline cartilage which show the same shape, same size, well-defined, and low signal intensity on all pulse sequences [14]. In intra-articular liposarcoma, 2 main types can be seen: the low-differentiated myxoid liposarcoma in young adults and less commonly the well-differentiated pleomorphic liposarcoma in older adults. Liposarcomas are typically found near the knee or elbow; while highly differentiated forms are found in the buttocks, abdomen, or groin [15]. Synovial sarcoma is common in young patients. Soft tissue lesions around the knee are hyperintense on T1W, T2W and show strong enhancement after injection of magnetic contrast agent. On T2W, a triple sign was observed: the necrotic area is strongly hyperintense, the soft tissue area is moderate hyperintense, and the fibrosis area is hypointense [16].
The goals of PVNS treatment are to prevent disease progression and maintain and protect joint function. Surgical resection is the main treatment for this lesion [1, 17]. Knee arthroscopy is the first choice, with the advantage of allowing observation and intervention in deep areas of the joint, reducing the extent of damage to nearby organs [5]. Open reduction can be used when diffuse lesions affect both the anterior and posterior aspect of the joint and require total synovial resection [5]. Arthroscopy combined with minimally open reduction when the large mass is located behind the knee helps to eliminate lesions while allowing faster recovery [18]. Total joint replacement is performed in patients with end-stage lesions, extensive joint destruction [5]. Radiotherapy is usually reserved for patients in whom standard surgery has failed, such as those with diffuse involvement of vascular, nerve, and tendon structures. Two methods of radiation therapy are applied: external and internal radiation therapy [5,8]. Colony-stimulating factor 1R-targeting agents are effective in some cases [2, 19]. After surgery, physical therapy plays an important role in helping patients return to normal activities. Exercises can help regain joints’ strength and range of motion [5].
Conclusion
Pigmented villonodular synovitis is a rare disease of the synovial membrane. The vast majority are benign, slowly progressing to joint destruction if left untreated. Early detection of clinical symptoms and MRI play an important role in the early diagnosis and successful treatment of the disease. Ultrasound-guided biopsy is recommended in cases in which the diagnosis is in doubt.
Patient consent
Informed consent for patient information to be published in this article was obtained.
Ethical statement
Appropriate written informed consent was obtained for publication of this case report and accompanying images.
Author contributions
All authors contributed to this article as co-first authors. All authors have read the manuscript and agree to the contents.
Footnotes
Acknowledgments: Self-financed
Competing interests: The authors do not report any conflicts of interest.
REFERENCES
- 1.Sullivan CJ, Eustace SJ, Kavanagh EC. Pigmented villonodular synovitis of the hip joint: three cases demonstrating characteristic MRI features. Radiol Case Rep. 24 Jun 2020;15(8):1335–1338. doi: 10.1016/j.radcr.2020.05.067. PMID: 32617126; PMCID: PMC7322487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fecek C, Carter KR. StatPearls [Internet] StatPearls Publishing; Treasure Island (FL): 7 Nov 2021. Pigmented villonodular synovitis. 2022 Jan–. PMID: 31751040. [PubMed] [Google Scholar]
- 3.Tritschler P, Baudrez V, Mutijima E. Diffuse pigmented villonodular synovitis of the subtalar joint. J Belg Soc Radiol. 31 Jan 2018;102(1):11. doi: 10.5334/jbsr.1477. PMID: 30039025; PMCID: PMC6032406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fałek A, Niemunis-Sawicka J, Wrona K, Szczypiór G, Rzepecka-Wejs L, Cięszczyk K, et al. Pigmented villonodular synovitis. Folia Med Cracov. 2018;58(4):93–104. PMID: 30745604. [PubMed] [Google Scholar]
- 5.Bernthal NM, Ishmael CR, Burke ZDC. Management of Pigmented villonodular synovitis (PVNS): an orthopedic surgeon's perspective. Curr Oncol Rep. 4 Jun 2020;22(6):63. doi: 10.1007/s11912-020-00926-7. PMID: 32494892. [DOI] [PubMed] [Google Scholar]
- 6.Zhao L, Zhou K, Hua Y, Li Y, Mu D. Multifocal pigmented villonodular synovitis in a child: a case report. Medicine (Baltimore) Aug 2016;95(33):e4572. doi: 10.1097/MD.0000000000004572. PMID: 27537585; PMCID: PMC5370811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen EL, de Castro CM 4th, Hendzel KD, Iwaz S, Kim MA, Valeshabad AK, et al. Histologically benign metastasizing tenosynovial giant cell tumor mimicking metastatic malignancy: a case report and review of literature. Radiol Case Rep. 2019 May 24;14(8):934-940. doi: 10.1016/j.radcr.2019.05.013. PMID: 31193787; PMCID: PMC6542375. [DOI] [PMC free article] [PubMed]
- 8.Iakovou I, Symeonidis P, Kotrotsios D, Giannoula E, Sachpekidis C. Radiosynoviorthesis after surgery in the treatment of patients with ankle pigmented villonodular synovitis: a case series. J Clin Med. 22 Feb 2020;9(2):597. doi: 10.3390/jcm9020597. PMID: 32098290; PMCID: PMC7073893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tritschler P, Baudrez V, Mutijima E. Diffuse pigmented villonodular synovitis of the subtalar joint. J Belg Soc Radiol. 31 Jan 2018;102(1):11. doi: 10.5334/jbsr.1477. PMID: 30039025; PMCID: PMC6032406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Willimon SC, Busch MT, Perkins CA. Pigmented villonodular synovitis of the knee: an underappreciated source of pain in children and adolescents. J Pediatr Orthop. Sep 2018;38(8):e482–e485. doi: 10.1097/BPO.0000000000001213. PMID: 29917011. [DOI] [PubMed] [Google Scholar]
- 11.Cheng XG, You YH, Liu W, Zhao T, Qu H. MRI features of pigmented villonodular synovitis (PVNS) Clin Rheumatol. Feb 2004;23(1):31–34. doi: 10.1007/s10067-003-0827-x. Epub 2004 Jan 9. PMID: 14749979. [DOI] [PubMed] [Google Scholar]
- 12.Ranganath VK, Hammer HB, McQueen FM. Contemporary imaging of rheumatoid arthritis: clinical role of ultrasound and MRI. Best Pract Res Clin Rheumatol. Dec 2020;34(6) doi: 10.1016/j.berh.2020.101593. Epub 2020 Sep 26. PMID: 32988757. [DOI] [PubMed] [Google Scholar]
- 13.Mattila KA, Aronniemi J, Salminen P, Rintala RJ, Kyrklund K. Intra-articular venous malformation of the knee in children: magnetic resonance imaging findings and significance of synovial involvement. Pediatr Radiol. Apr 2020;50(4):509–515. doi: 10.1007/s00247-019-04580-5. Epub 2019 Dec 19. PMID: 31853571; PMCID: PMC7067728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boninsegna E, Fassio A, Testoni M, Gatti D, Viapiana O, Mansueto G, et al. Radiological features of knee joint synovial chondromatosis. Reumatismo. 2019 Jul 9;71(2):81–84. doi: 10.4081/reumatismo.2019.1132. PMID: 31309778. [DOI] [PubMed] [Google Scholar]
- 15.Dalla Rosa J, Nogales Zafra JJ. Large intra-articular true lipoma of the knee. BMC Musculoskelet Disord. 2019 Mar 18;20(1):110. doi: 10.1186/s12891-019-2484-5. PMID: 30885187; PMCID: PMC6421673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Al-Mohrej OA, Al-Jarallah SA, Al-Dakhil Allah HH, Pant R, Al-Zayed ZS. Synovial sarcoma presenting as an intra-articular mass in a pediatric patient: a case report. BMC Musculoskelet Disord. 2020 May 7;21(1):283. doi: 10.1186/s12891-020-03312-3. PMID: 32381079; PMCID: PMC7206690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dürr HR, Capellen CF, Klein A, Baur-Melnyk A, Birkenmaier C, Jansson V, et al. The effects of radiosynoviorthesis in pigmented villonodular synovitis of the knee. Arch Orthop Trauma Surg. May 2019;139(5):623–627. doi: 10.1007/s00402-018-3097-4. Epub 2018 Dec 11. PMID: 30539286. [DOI] [PubMed] [Google Scholar]
- 18.Ellsworth B, Kamath AF. Open and arthroscopic with mini-open surgical hip approaches for treatment of pigmented villonodular synovitis and concomitant hip pathology. Case Rep Orthop. 2017;2017 doi: 10.1155/2017/3716360. Epub 2017 Feb 23. PMID: 28326214; PMCID: PMC5343235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Felis-Giemza A, Apanel-Kotarska A, Chojnowski M, Olesińska M. Is intra-articular infliximab therapy a good alternative to radionuclide synovectomy for a patient with refractory pigmented villonodular synovitis? Reumatologia. 2021;59(5):340–345. doi: 10.5114/reum.2021.110601. Epub 2021 Nov 7. PMID: 34819709; PMCID: PMC8609374. [DOI] [PMC free article] [PubMed] [Google Scholar]