Abstract
Aims
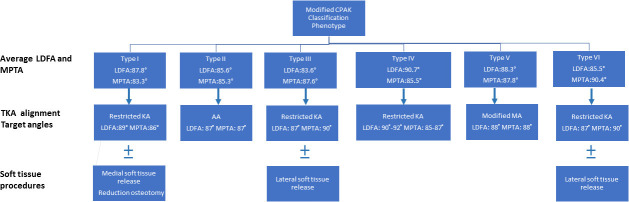
The Coronal Plane Alignment of the Knee (CPAK) classification is a simple and comprehensive system for predicting pre-arthritic knee alignment. However, when the CPAK classification is applied in the Asian population, which is characterized by more varus and wider distribution in lower limb alignment, modifications in the boundaries of arithmetic hip-knee-ankle angle (aHKA) and joint line obliquity (JLO) should be considered. The purposes of this study were as follows: first, to propose a modified CPAK classification based on the actual joint line obliquity (aJLO) and wider range of aHKA in the Asian population; second, to test this classification in a cohort of Asians with healthy knees; third, to propose individualized alignment targets for different CPAK types in kinematically aligned (KA) total knee arthroplasty (TKA).
Methods
The CPAK classification was modified by changing the neutral boundaries of aHKA to 0° ± 3° and using aJLO as a new variable. Radiological analysis of 214 healthy knees in 214 Asian individuals was used to assess the distribution and mean value of alignment angles of each phenotype among different classifications based on the coronal plane. Individualized alignment targets were set according to the mean lateral distal femoral angle (LDFA) and medial proximal tibial angle (MPTA) of different knee types.
Results
A very high concentration, 191 from 214 individuals (89.3%), were found in knee types with apex distal JLO when the CPAK classification was applied in the Asian population. By using aJLO as a new variable, the high distribution percentage in knee types with apex distal JLO decreased to 125 from 214 individuals (58.4%). The most common types in order were Type II (n = 70; 32.7%), Type V (n = 55; 25.7%), and Type I (n = 46; 21.5%) in the modified CPAK classification.
Conclusion
The modified CPAK classification corrected the uneven distribution when applying the CPAK classification in the Asian population. Setting individualized TKA alignment targets according to CPAK type may be a practical method to recreate optimal LDFA and MPTA in KA-TKA.
Cite this article: Bone Jt Open 2022;3(3):211–217.
Keywords: Kinematic alignment, Total knee arthroplasty, Phenotype of the knee, Total knee replacement, Kinematically aligned, CPAK classification, knees, medial proximal tibial angle, lateral distal femoral angle, joint line obliquity, hip-knee-ankle angle, total knee arthroplasty (TKA), limb alignment, arthritic knee, varus deformity, distal femur
Introduction
Kinematically aligned (KA) total knee arthroplasty (TKA) aims to restore native (pre-arthritic) alignment and has shown improved soft-tissue balance, with excellent long-term surgical outcomes in long-term follow-up. 1 However, uncertainty still exists in estimating an individual’s pre-arthritic alignment and setting an acceptable alignment target. 2-5
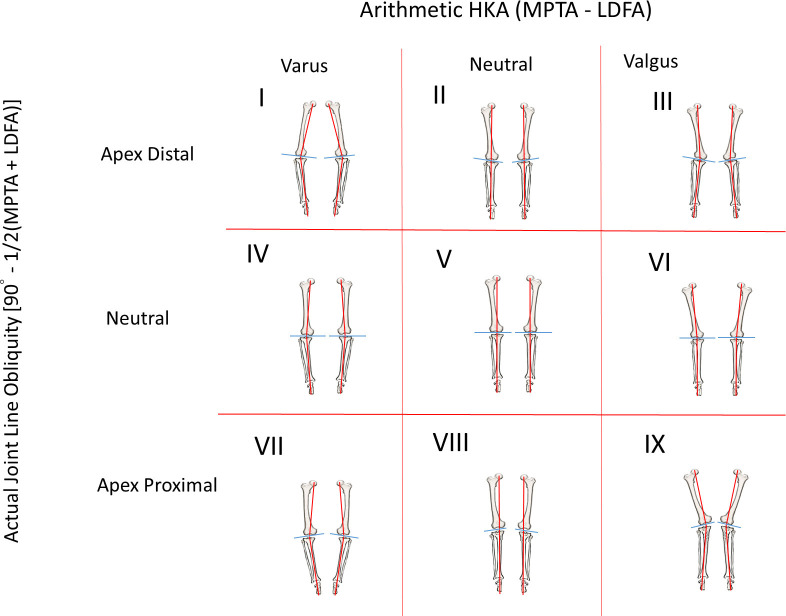
Though categorizing knee type in the coronal plane is a straightforward way of determining the pre-arthritic alignment, only a few papers have mentioned the classification system. In 2018, Lin et al 6 used the mechanical hip-knee-ankle angle (mHKA), lateral distal femoral angle (LDFA), and medial proximal tibial angle (MPTA) as the main variables to classify five knee coronal alignment phenotypes. 6 This is the first paper to classify lower limb alignment by independent femoral and tibial alignment parameters, rather than mHKA alone. In the following year, Hirschman et al 7 proposed another classification system based on CT imaging from 160 nonarthritic individuals. They used the combination of mHKA, LDFA, and MPTA to construct 125 theoretical functional phenotypes and found the most common phenotypes in each sex. Griffiths-Jones et al 8 and MacDessi et al 9 found that the arithmetic HKA (aHKA) was relatively equivalent to mHKA, which is an ideal variable for estimating the constitutional limb alignment after the development of significant arthritis. In 2021, MacDessi et al 10 proposed the Coronal Plane Alignment of Knee (CPAK) classification, which simplified categorization into nine knee phenotypes by incorporating only two critical variables: aHKA and the joint line obliquity (JLO). JLO is a milestone for knee type classification as it adds the degrees and direction of JLO to the characteristic of a knee. 9 By definition, JLO is calculated by MPTA+ LDFA. 10 When the sum of these two angles is greater than 180°, it indicates an apex proximal joint line, while a sum of less than 180° indicates that the joint line is apex distal. However, JLO is not the angle of the joint line that deviates from the horizontal line. It also does not reflect the certain degree of JLO to the ground (Figure 1). To provide a better understanding of the actual JLO to the ground, we herein propose a new variable termed “actual JLO” (aJLO), which reflects the certain degree of the JLO parallel to the ground. The equation of aJLO is described as aJLO = 90° – (LDFA+ MPTA)/2. Taking the illustration depicted in Figure 1 as an example, in a knee with LDFA of 88° and MPTA of 87°, the JLO is the sum of LDFA and MTPA, i.e. 175°, while the aJLO is 2.5°, which is a more straightforward way of expressing the degree of JLO to the ground.
Fig. 1.
The calculation of the actual joint line obliquity (aJLO) in the case of a neutral knee with an apex distal JLO, which has its mechanical axis (MA) vertical to the ground. α angle = 90° - lateral distal femoral angle (LDFA). β angle = 90° - medial proximal tibial angle (MPTA). Both α angle and β angle each contributes to half of the apex distal JLO, so the aJLO to the ground should be calculated as aJLO = (α+β)/2, which is 90° - (LDFA+ MPTA)/2.
The aHKA is determined by MPTA-LDFA to predict constitutional pre-arthritic alignment. 9 In the original CPAK classification, the boundaries of neutral alignment were set as 0° ± standard deviation (SD) 2°. However, applying CPAK classification in the Asian population, which has more varus and wider distribution of lower limb alignment, 6,11 means that wider boundaries for neutral aHKA should be considered. Thus, the boundaries of neutral aHKA were enlarged to 0° ± SD 3° in the modified CPAK classification.
In addition to helping provide information about different knee types and their features, another important function of an ideal classification is to guide treatment. Since each CPAK type has its own specific alignment, the mean LDFA and MPTA of each CPAK type could be a valuable reference to recreate optimal LDFA and MPTA. The purposes of this study were as follows: first, to propose a modified CPAK classification based on the aJLO and the wider range of neutral aHKA in the Asian population; second, to test this classification in a cohort of Asians with healthy knees and to compare it to other coronal plane classifications; and third, to propose individual alignment targets for different CPAK types in KA-TKA.
Methods
Study groups
Approval for the current study was provided by a local institutional review board (approval number CE20008B).
The data were obtained from a healthy cohort consisting of 214 adults aged between 20 and 70 years from a previous cross-sectional study of knee alignment conducted by two blinded observers, which was used to validate the CPAK classification. 6 The exclusion criteria were as follows: previous complaint of knee or hip pain mentioned in the chart, osteoarthritis of the knee or hip on plain film (Kellgren-Lawrence classification 12 grade 1 or above), history of lower limb trauma, deformity, or surgery history, and rotation or poor image quality.
The mean age of the 214 subjects was 41.3 (SD 18.6) years; 52% were male (n = 111) and 48% were female. The radiological data of the 214 subjects, who all had healthy knees, are shown in Table I. No significant differences were noted between aHKA (-1.5° (SD 3.2°)) and mHKA (-1.2° (SD 3.1°)).
Table I.
Radiological measurement data for 214 subjects with healthy knees.
| Variable | Mean (SD) | p-value* |
|---|---|---|
| aHKA, ° | -1.5 (3.2) | 0.265 |
| mHKA, ° | -1.2 (3.1) | |
| LDFA, ° | 87.3 (2.4) | |
| MPTA, ° | 85.8 (2.2) | |
| AA-MA, ° | 4.7 (1.5) | |
| JLO, ° | 173.1 (3.3) | |
| aJLO, ° | 3.4 (1.7) |
Independent-samples t-test.
AA-MA, angle between femoral anatomical axis and mechanical axis; aHKA, arithmetic hip-knee-ankle angle; aJLO, actual joint line obliquity; JLO, joint line obliquity; LDFA, lateral distal femoral angle; mHKA, mechanical hip-knee-ankle angle; MPTA, medial proximal tibial angle; SD, standard deviation.
Radiological measurements
All participants underwent standard digital long leg radiographs. The mHKA was the angle subtended by the mechanical axes of the femur and tibia. The LDFA was defined as the lateral angle formed between the femoral mechanical axis and the joint line of the distal femur. The MPTA was defined as the medial angle formed between the tibial mechanical axis and the joint line of the proximal tibia.
All films were reviewed and measured by two observers, using the above methodology, which has been shown to have high inter- and intraobserver reliability. The α value of intraclass correlation coefficients of the two observers for mHKA, LDFA, and MPTA, were 0.991, 0.912, and 0.918, respectively. The result indicated excellent interobserver reliability.
The aHKA was determined as described in a previous publication: aHKA = MPTA - LDFA to predict constitutional alignment. 9 CPAK boundaries for neutral aHKA were determined to be one SD (rounded to the nearest whole number) for the mean mHKA of all 214 knees in our study group (SD 3.1°). 6 Hence, the boundaries for neutral aHKA were 0° ± 3°, inclusive. A varus aHKA is less than -3°, while a valgus aHKA is greater than 3°.
The aJLO is calculated by the equation: 90° – (LDFA + MPTA)/2. Boundaries for the neutral aJLO were 0° ± 3°, inclusive. An apex distal JLO is greater than 3°, while an apex proximal JLO is less than -3°. The knee was classified into type I to type IX, according to the modified CPAK (Figure 2).
Fig. 2.
The modified coronal plane alignment of the knee classification with nine theoretical types of knee. HKA, hip-knee-ankle angle; LDFA, lateral distal femoral angle; MPTA, medial proximal tibial angle.
Outcome measures
Frequencies, mean aHKA, mHKA, LDFA, MPTA, JLO, and aJLO for each knee type for the CPAK classification, and modified CPAK classification were analyzed and compared.
Statistical analysis
Scatterplots were created to demonstrate alignment distribution for the original CPAK classification and the modified classification. Normality of data distribution was assessed for continuous variables using Q-Q plots and the Shapiro-Wilk test. Continuous variables are expressed as mean (SD) and were compared using the independent-samples t-test. Statistical significance was set at a p-value ≤ 0.05. Statistical analyses were performed using SPSS Statistics v. 22 (IBM, USA).
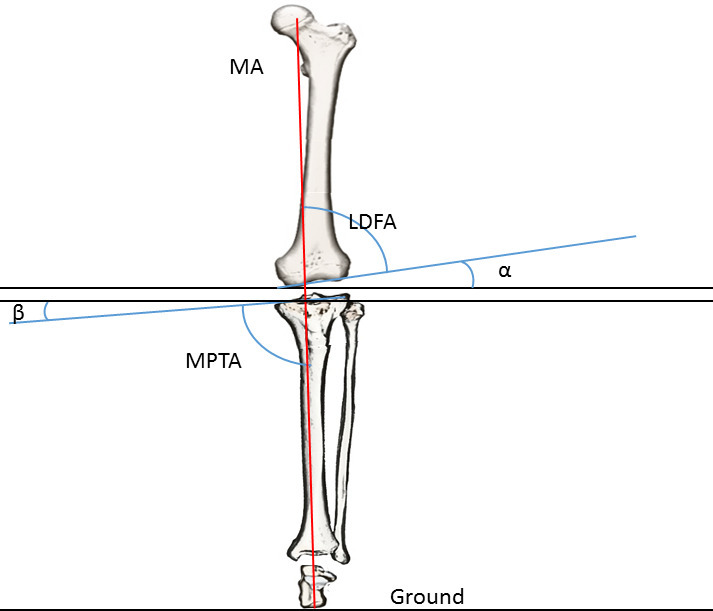
Results
Table II shows the distribution and the mean knee alignment angles of each type classified according to the CPAK classification. The most common CPAK types in order were Type II (neutral aHKA, apex distal JLO: n = 84; 39.3%), Type I (varus aHKA, apex distal JLO: n = 78; 36.4%), and Type III (neutral aHKA, apex distal JLO: n = 29; 13.6%). The distribution plot of the CPAK classification is shown in Figure 3. In total, 191 patients (89.3%) were concentrated in Type I, Type II, and Type III, which have an apex distal JLO. No subjects were classified into types VII, VIII, or IX, which have an apex proximal JLO.
Table II.
Distribution and mean alignment angles of 214 healthy knees for each type in the original coronal plane alignment of the knee classification.
| CPAK | n, (%) | Mean mHKA, ° (SD) | Mean LDFA, ° (SD) | Mean MPTA, ° (SD) | Mean AA-MA, ° (SD) | Mean aHKA, ° (SD) | Mean JLO, ° (SD) | Mean aJLO, ° (SD) |
|---|---|---|---|---|---|---|---|---|
| I | 78 (36.4) | -3.8 (1.7) | 88.4 (1.6) | 84.0 (1.6) | 5.2 (1.4) | -4.5 (2.1) | 172.3 (2.8) | 3.8 (1.4) |
| II | 84 (39.3) | -0.0 (1.2) | 86.4 (1.6) | 86.1 (1.4) | 4.2 (1.2) | -0.3 (1.8) | 172.5 (2.8) | 3.7 (1.4) |
| III | 29 (13.6) | 3.5 (1.1) | 84.4 (1.5) | 87.9 (1.8) | 3.4 (1.7) | 3.9 (1.0) | 172.3 (3.1) | 3.8 (1.5) |
| IV | 12 (5.6) | -4.9 (3.0) | 91.9 (1.7) | 86.6 (1.3) | 6.2 (2.2) | -5.2 (2.2) | 178.5 (0.9) | 0.8 (0.5) |
| V | 10 (4.7) | 0.2 (1.2) | 89.4 (0.7) | 89.1 (0.8) | 4.4 (1.1) | -0.5 (1.4) | 178.5 (1.1) | 0.7 (0.6) |
| VI | 1 (0.5) | 5.5 | 86.5 | 93.2 | 5.4 | 6.7 | 179.7 | 0.15 |
aHKA, arithmetic hip-knee-ankle angle; aJLO, actual joint line obliquity; CPAK, Coronal Plane Alignment of the Knee; JLO, joint line obliquity; LDFA, lateral distal femoral angle; MA-AA, angle between femoral anatomical axis and mechanical axis; mHKA, mechanical hip-knee-ankle angle; MPTA, medial proximal tibial angle; SD, standard deviation.
Fig. 3.
The percentage distributions of the 214 patients in each type using the coronal plane alignment of the knee classification. aHKA, arithmetic hip-knee-ankle angle; JLO, joint line obliquity; LDFA, lateral distal femoral angle; MPTA, medial proximal tibial angle.
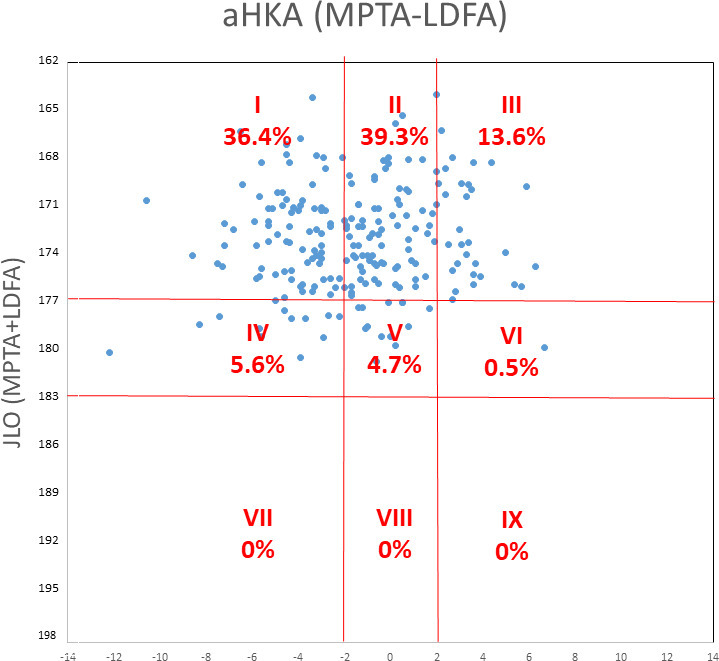
Table III shows the distribution and the mean knee alignment angles of each type classified according to the setting of the modified CPAK classification. The most common CPAK types in order were Type II (neutral aHKA, apex distal JLO: n = 70; 32.7%), Type V (neutral aHKA, neutral JLO: n = 55; 25.7%), and Type I (varus aHKA, apex distal JLO: n = 46; 21.5%). The distribution plot of the modified CPAK classification is shown in Figure 4. The distribution in types I, II, and III was 125 from 214 individuals (58.4%). No subjects were classified into types VII, VIII, or IX.
Table III.
Distribution and mean knee alignment angles of 214 healthy knees in the modified coronal plane alignment of the knee classification.
| CPAK | n, (%) | Mean mHKA, ° (SD) | Mean LDFA, ° (SD) | Mean MPTA, ° (SD) | Mean MA-AA, ° (SD) | Mean aHKA, ° (SD) | Mean JLO, ° (SD) | Mean aJLO, ° (SD) |
|---|---|---|---|---|---|---|---|---|
| I | 46 (21.5) | -4.1 (2.0) | 87.8 (1.8) | 83.3 (1.5) | 5.2 (1.4) | -4.5 (2.2) | 170.3 (2.2) | 4.5 (1.2) |
| II | 70 (32.7) | 0.0 (1.6) | 85.6 (1.7) | 85.3 (1.3) | 4.2 (1.2) | -0.3 (1.7) | 170.7 (2.2) | 4.6 (1.2) |
| III | 9 (4.2) | 4.0 (1.0) | 83.6 (1.4) | 87.6 (1.2) | 3.4 (1.7) | 3.9 (1.0) | 172.9 (2.2) | 4.4 (1.9) |
| IV | 26 (12.1) | -4.5 (2.4) | 90.7 (1.6) | 85.5 (1.1) | 6.2 (2.2) | -5.2 (2.1) | 176.2 (1.8) | 1.9 (0.9) |
| V | 55 (25.7) | -0.3 (1.7) | 88.3 (1.1) | 87.8 (1.1) | 4.4 (1.1) | -0.5 (1.5) | 176.0 (1.6) | 2.0 (0.8) |
| VI | 8 (3.7) | 4.6 (1.0) | 85.5 (0.7) | 90.4 (1.3) | 4.6 (1.3) | 4.9 (1.3) | 175.9 (1.6) | 2.0 (0.8) |
aHKA, arithmetic hip-knee-ankle angle; aJLO, actual joint line obliquity; CPAK, Coronal Plane Alignment of the Knee; JLO, joint line obliquity; LDFA, lateral distal femoral angle; MA-AA, angle between femoral anatomical axis and mechanical axis; mHKA, mechanical hip-knee-ankle angle; MPTA, medial proximal tibial angle; SD, standard deviation.
Fig. 4.
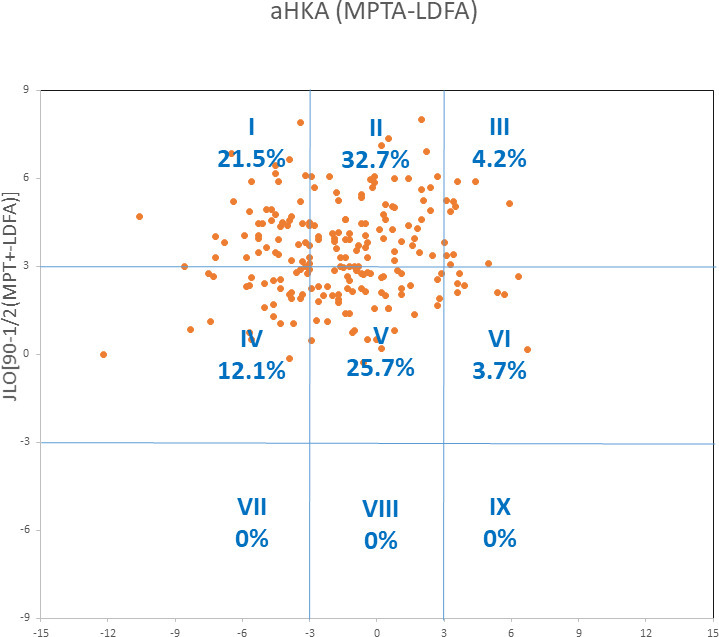
The percentage distributions of the 214 patients in each type using the modified coronal plane alignment of the knee classification. aHKA, arithmetic hip-knee-ankle angle; JLO, joint line obliquity; LDFA, lateral distal femoral angle; MPTA, medial proximal tibial angle.
Discussion
Since the CPAK classification is determined by two critical variables (aHKA = MPTA - LDFA and JLO = MPTA + LDFA) in a population with a smaller MPTA, both the aHKA and JLO tend to become smaller, and the distribution shifts to the left and toward the upper corner in the scatterplot (Figure 3). A significant uneven distribution was noted when the CPAK classification was applied in the Asian population. The high concentration in CPAK type I, type II, and type III may be because the JLO doubles the aJLO. This deviation reduced the distribution within the neutral boundaries of JLO and increased the distribution in types of the apex distal JLO. For example, in a knee with LDFA of 88° and MPTA of 87°, the aHKA is -1°, which falls into neutral aHKA boundaries. The JLO is 175°, which is outside the neutral JLO boundaries. Thus, the knee is characterized as CPAK type II. However, the actual JLO to the ground for this knee is 2.5°, which falls into neutral aJLO boundaries. Combined with the neutral aHKA, the knee belongs to the modified CPAK type V. An important function of the CPAK classification is to guide treatment, i.e. to determine whether a patient should be considered for a MA-TKA (type V), anatomical alignment (AA)-TKA (type II), or KA-TKA (type I, III, IV, VI). 10 However, with the original setting of the CPAK classification, only 4.7% of the Asian population was classified as CPAK type V, and therefore the vast majority of Asians were not candidates for MA-TKA.
To deal with the left- and up-shifting distribution of our Asian population, we widened the neutral boundaries in aHKA and used aJLO as a new variable (Figure 4). This modification increased the distribution of knee types with neutral aHKA and aJLO. Thus, the distribution of type V increased from 4.7% to 25.7% after the modification. In our study group, SDs of both mHKA and aHKA were more than 3° (3.1° and 3.2°, respectively). Hence, setting a neutral boundary as 0° ± 3° was an appropriate modification to apply CPAK classification in this Asian population. It has been reported that Asian populations have more varus limb alignment and wider distribution compared to Westerners. 11,13
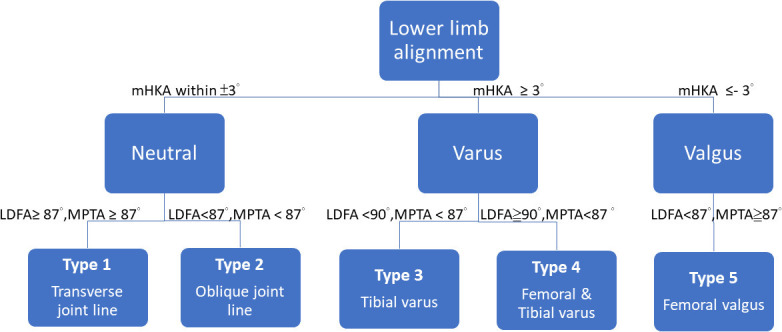
Lin et al’s 6 classification is the first system to categorize knee phenotypes in the coronal plane. In their classification, 214 healthy knees from an Asian population were classified into five phenotypes according to mHKA, LDFA, and MPTA. The classification system is depicted in Figure 5. An algorithm for recreating different LDFA and MPTA according to the mean LDFA and MPTA in different knee types in Lin et al’s 6 classification for KA-TKA was proposed in 2020. 14 Early implant survivorship and functional outcomes of this phenotype-oriented KA-TKA were promising. These result suggests that using the mean LDFA and MPTA of each modified CPAK type to recreate LDFA and MPTA may also be valid.
Fig. 5.
The algorithm of Lin et al’s 6 classification for the lower limb alignment in the coronal plane. LDFA, lateral distal femoral angle; mHKA, mechanical hip-knee-ankle angle; MPTA, medial proximal tibial angle.
KA-TKA aims to restore native pre-arthritic alignment, but the acceptable safe ranges for limb alignment remain uncertain. To avoid extreme alignment, the restricted KA-TKA defines the safe zone as 86° to 93° for recreation of both the LDFA and the MPTA, and -5° varus to +4° valgus for the final mHKA. 15 Restricted KA-TKA balances neutral mechanical alignment and preserves the native pre-arthritic alignment, which is suitable for CPAK types I, III, IV, and VI. 10 However, a detailed account of the method for recreating the target LDFA and MPTA has not been clearly described. Using the mean LDFA and MPTA of each modified CPAK type as the alignment target may avoid significant deviation from the original constitutional alignment. In patients with severe deformity and bony wear, for whom even aHKA cannot precisely predict the pre-arthritic knee alignment angles, the mean LDFA and MPTA of each CPAK type could also be used as a guide for restoring appropriate lower limb alignment. By integrating the concept of aHKA, aJLO from the modified CPAK classification, and the restricted safe zone, the alignment targets can be set more precisely for each modified CPAK type in the preoperative alignment planning.
In type I knees, the major contribution of varus deformity is the tibial varus. The mean LDFA and MPTA were 87.8° and 83.3°. The alignment targets were set according to the following steps. First, the MPTA was set to 86°, as the lowest limits of the restricted safe zone. Then the LDFA was set to 89° to make aHKA and aJLO both within 3°. In this type of knee, medial soft-tissue release and reduction osteotomy is usually needed to balance the extension gap. In type II knees, the mean LDFA and MPTA were 85.6° and 85.3°. The target angles of LDFA and MPTA were both set to 87° to achieve the goal of anatomical alignment (AA) and decrease the JLO. External rotation of about 2° to 3° to the posterior condylar axis may be needed to balance the flexion gap. Usually, no soft-tissue release is necessary. In type III knee, the major contribution of valgus alignment is due to the distal femur deformity. The mean LDFA and MPTA were 83.3° and 87.6°. First, the LDFA was set to 87°, as valgus deformity over 3° should be avoided to prevent patella instability. 16 Then the MPTA was set to 90° to get both aHKA and aJLO within 3°. Lateral release of iliotibial and lateral patella retinaculum may also be necessary to decrease the incidence of patella instability. In type IV knees, both the distal femur and proximal tibia contribute to the varus deformity. The mean LDFA and MPTA were 90.7°and 85.5°. The targets of LDFA and MPTA should be set to 90° to 92° and 85° to 87° so that aHKA and aJLO are both within 3° to 5°. The major cause of large LDFA is coxa varus or femur bowing. In knees with severe femoral lateral bowing, the LDFA may be greater than 94°, and the LDFA could be set at 92° to avoid putting the femoral component into too much varus alignment, which may increase the knee component loosening rate. 17 If the varus deformity is more severe, medial soft tissue release and reduction osteotomy technique are still necessary to achieve a balanced knee. In type V knee, the mean LDFA and MPTA were 88.3° and 87.8°. The target angle of LDFA and MPTA was set at 88° according to the concept of the modified MA-TKA. 18 In type VI knee, the mean LDFA and MPTA were 85.5° and 90.4°. Both the femur and tibia contribute to the valgus deformity. The target angles of LDFA and MPTA were set at 87° and 90°. The algorithm for setting the LDFA and MPTA is shown in Figure 6.
Fig. 6.
Total knee arthroplasty (TKA) alignment targets for lateral distal femoral angle (LDFA) and medial proximal tibial angle (MPTA) and soft-tissue procedure in each knee type of the modified coronal plane alignment of the knee classification. AA, anatomically aligned; KA, kinematically aligned; MA, mechanically aligned.
The modified CPAK classification inherits advantages of the CPAK classification, which allows individualized preoperative alignment planning according to the knee types. Secondly, it adopts the aJLO variable, which is straightforward and precisely describes the actual joint line obliquity to the ground. Using aJLO in the modified CPAK classification also successfully resolved the problem of small sample size in type IV, V, and VI when the CPAK classification was applied in our Asian population. The boundaries of neutral aHKA and aJLO were set at 0° ± 3°, which is also easy to remember and is likely to be readily accepted in clinical practice. Thirdly, using the mean LDFAs and MPTAs in each knee type as a guide for restricted KA-TKA technique is helpful to avoid extreme alignment and determine the target LDFA and MPTA more easily.
This study has several limitations. First, the age of our study group was relatively older and the age range was wider than in other studies, which may have affected the percentage distribution of knee types, although the accuracy of aHKA is less affected by age or early osteoarthritis change. 8 Secondly, although the targets of LFDA and MPTA for each knee type were proposed according to the mean LDFA and MPTA of healthy knees and within traditionally accepted boundaries, the intercompartmental pressure and clinical outcomes were not investigated. These should be validated in future studies, though excellent short-term outcomes have been reported in the phenotype-oriented KA-TKA technique according to Lin et al’s 6 classification. 14 Thirdly, the sample size in our study group was relatively small, so the findings in distribution percentage and the mean alignment angles should be validated in larger-scale studies, especially in type III and type VI, which had the lowest case numbers in the present study.
In summary, modification of the CPAK classification by changing the neutral boundaries of aHKA to 0° ± 3° and using the aJLO as a new variable corrects the uneven distribution when applying CPAK classification in the Asian population. Setting individualized TKA alignment targets according to knee phenotype may be a practical method to recreate optimal LDFA and MPTA in KA-TKA.
Take home message
- Modification of the Coronal Plane Alignment of the Knee (CPAK) classification by changing the neutral boundaries of arithmetic hip-knee-ankle angle to 0° (standard deviation 3°) and using the actual joint line obliquity as a new variable corrects the uneven distribution when applying CPAK classification in the Asian population.
- Setting individualized total knee arthroplasty (TKA) alignment targets according to knee phenotype may be a practical method to recreate optimal lateral distal femoral angle and medial proximal tibial angle in kinematically aligned TKA.
Acknowledgements
We thank Y-S Lin and F-S Chang for the measurement of the radiographic parameters. We appreciate the help from editors and anonymous referees for the critical review.
Footnotes
Author contributions: C-E. Hsu: Investigation, Software, Data curation, Formal analysis, Writing – original draft, Writing – review & editing.
C-P. Chen: Supervision, Resources, Validation.
S-P. Wang: Supervision, Resources, Software, Validation.
J-T. Huang: Methodology, Project administration.
K-M. Tong: Supervision, Resources.
K-C. Huang: Conceptualization, Funding acquisition, Project administration, Supervision, Writing – review & editing
Funding statement: The authors received no financial or material support for the research, authorship, and/or publication of this article.
Ethical review statement: The study design was approved by the Research Ethics Committee China Medical University & Hospital (IRB number: CMUH108-Rec1-088). All methods were performed in accordance with the relevant guidelines and regulations.
Open access funding: The open access fee was supported by the Asia University Hospital.
Contributor Information
Cheng-En Hsu, Email: jacobhe2001@gmail.com.
Chao-Ping Chen, Email: cpchen@vghtc.gov.tw.
Shun-Ping Wang, Email: wsp0120@yahoo.com.tw.
Jen-Ting Huang, Email: maffucci1234@gmail.com.
Kwok-Man Tong, Email: tongkwokman@gmail.com.
Kui-Chou Huang, Email: kuichouhuang@gmail.com.
References
- 1. Howell SM, Shelton TJ, Hull ML. Implant survival and function ten years after kinematically aligned total knee arthroplasty. J Arthroplasty. 2018;33(12):3678–3684. 10.1016/j.arth.2018.07.020 [DOI] [PubMed] [Google Scholar]
- 2. Dossett HG, Estrada NA, Swartz GJ, LeFevre GW, Kwasman BG. A randomised controlled trial of kinematically and mechanically aligned total knee replacements: two-year clinical results. Bone Joint J. 2014;96-B(7):907–913. 10.1302/0301-620X.96B7.32812 [DOI] [PubMed] [Google Scholar]
- 3. Dossett HG, Swartz GJ, Estrada NA, LeFevre GW, Kwasman BG. Kinematically versus mechanically aligned total knee arthroplasty. Orthopedics. 2012;35(2):e160-9. 10.3928/01477447-20120123-04 [DOI] [PubMed] [Google Scholar]
- 4. Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML. Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res. 2013;471(3):1000–1007. 10.1007/s11999-012-2613-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Howell SM, Papadopoulos S, Kuznik K, Ghaly LR, Hull ML. Does varus alignment adversely affect implant survival and function six years after kinematically aligned total knee arthroplasty? Int Orthop. 2015;39(11):2117–2124. 10.1007/s00264-015-2743-5 [DOI] [PubMed] [Google Scholar]
- 6. Lin YH, Chang FS, Chen KH, Huang KC, Su KC. Mismatch between femur and tibia coronal alignment in the knee joint: classification of five lower limb types according to femoral and tibial mechanical alignment. BMC Musculoskelet Disord. 2018;19(1):411. 10.1186/s12891-018-2335-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclerq V, Hess S. Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc. 2019;27(5):1394–1402. 10.1007/s00167-019-05509-z [DOI] [PubMed] [Google Scholar]
- 8. Griffiths-Jones W, Chen DB, Harris IA, Bellemans J, MacDessi SJ. Arithmetic hip-knee-ankle angle (aHKA): an algorithm for estimating constitutional lower limb alignment in the arthritic patient population. Bone Jt Open. 2021;2(5):351–358. 10.1302/2633-1462.25.BJO-2021-0028.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. MacDessi SJ, Griffiths-Jones W, Harris IA, Bellemans J, Chen DB. The arithmetic HKA (aHKA) predicts the constitutional alignment of the arthritic knee compared to the normal contralateral knee: a matched-pairs radiographic study. Bone Jt Open. 2020;1(7):339–345. 10.1302/2633-1462.17.BJO-2020-0037.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. MacDessi SJ, Griffiths-Jones W, Harris IA, Bellemans J, Chen DB. Coronal Plane Alignment of the Knee (CPAK) classification. Bone Joint J. 2021;103-B(2):329–337. 10.1302/0301-620X.103B2.BJJ-2020-1050.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Song MH, Yoo SH, Kang SW, Kim YJ, Park GT, Pyeun YS. Coronal alignment of the lower limb and the incidence of constitutional varus knee in korean females. Knee Surg Relat Res. 2015;27(1):49–55. 10.5792/ksrr.2015.27.1.49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kohn MD, Sassoon AA, Fernando ND. Classifications in Brief: Kellgren-Lawrence Classification of Osteoarthritis. Clin Orthop Relat Res. 2016;474(8):1886–1893. 10.1007/s11999-016-4732-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tang WM, Zhu YH, Chiu KY. Axial alignment of the lower extremity in Chinese adults. J Bone Joint Surg Am. 2000;82(11):1603–1608. 10.2106/00004623-200011000-00014 [DOI] [PubMed] [Google Scholar]
- 14. Hsu CE, Huang JT, Tong KM, Huang KC. Total knee arthroplasty according to the original knee phenotypes with kinematic alignment surgical technique-early clinical and functional outcomes. BMC Musculoskelet Disord. 2020;21(1):839. 10.1186/s12891-020-03862-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. MacDessi SJ, Griffiths-Jones W, Chen DB, et al. Restoring the constitutional alignment with a restrictive kinematic protocol improves quantitative soft-tissue balance in total knee arthroplasty: a randomized controlled trial. Bone Joint J. 2020;102-B(1):117–124. 10.1302/0301-620X.102B1.BJJ-2019-0674.R2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Howell SM, Gill M, Shelton TJ, Nedopil AJ. Reoperations are few and confined to the most valgus phenotypes 4 years after unrestricted calipered kinematically aligned TKA. Knee Surg Sports Traumatol Arthrosc. 2021. 10.1007/s00167-021-06473-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lee BS, Cho HI, Bin SI, Kim JM, Jo BK. Femoral component varus malposition is associated with tibial aseptic loosening after TKA. Clin Orthop Relat Res. 2018;476(2):400–407. 10.1007/s11999.0000000000000012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Vanlommel L, Vanlommel J, Claes S, Bellemans J. Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc. 2013;21(10):2325–2330. 10.1007/s00167-013-2481-4 [DOI] [PubMed] [Google Scholar]