Sir,
A 55-year-old male, farmer by occupation, who is nonalcoholic and nonsmoker with no comorbidities was admitted to the emergency department with a history of multiple bee stings and presented with swelling and itching over face and neck. His vitals were normal. He was treated with antihistamines and steroids. Symptoms got subsided over 2 h. During the observation period, about 6.5 h after bee sting, he developed sudden onset slurring of speech along with weakness of left upper limb and lower limb. His blood pressure was 140/90 mmHg and pulse rate was 96/min. ECG showed sinus rhythm.
On examination, he was conscious, oriented. He had left lower facial weakness and left hemiparesis with the power of 3 to 4-MRC (Medical research council) grade in pyramidal distribution. Sensory and cerebellar examinations were normal. Examination of other systems was unremarkable. Noncontrast computed tomography (NCCT) brain did not show any abnormality. Diagnosis of acute ischemic stroke was made. His NIHSS score was 7. As there were no contraindications for thrombolysis, he was treated with alteplase 50 mg as per protocol. No complications developed during and after thrombolysis.
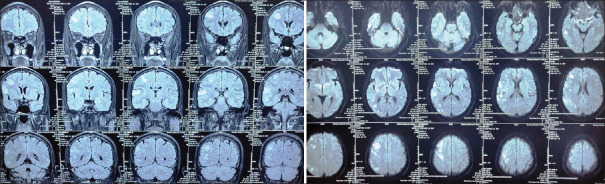
MRI brain after 24 h showed acute infarct in left frontal, parietal, occipital cortical and subcortical regions with no midline shift or mass effect [shown in Figure 1]. His blood investigations were within normal limits. Echocardiography showed normal ejection fraction with no evidence of clot. Carotid and vertebral Doppler study revealed normal blood vessel flow. After 48 h of bee sting, computed tomography cerebral angiography (CTA) performed did not show any evidence of vasospasm, stenosis, or occlusion of blood vessels. Patient was treated with antiplatelets and statins. After 1 week, his power improved to 4+ MRC grade with an NIHSS score of 2. He was discharged after 10 days. Modified Rankin scale was 0 at the time of discharge.
Figure 1.
MRI BRAIN Showing Hyperintense signals on T2 flair sequence in right frontal, parietal, temporal and occipital region with diffusion restriction in the same regions
THROMBOLYSIS IN ISCHEMIC STROKE 2
Hymenoptera are a group of membrane-winged insects which include bees, sawflies, and wasps. Envenomation by hymenoptera sting is a common occurrence with self-limiting local reactions in most cases. Though we know it can cause both local and systemic reactions due to vasoactive peptides and amines released from the venom, incidence of ischemic stroke following bee sting is rare and majority of strokes occurs within 24 h of bee sting.[1] Various mechanisms of stroke following bee sting are as follows: 1) vasospasm of blood vessels due to vasoactive peptides and sympathetic activation; 2) leukotrienes and thromboxane which are prothrombotic and proinflammatory can cause platelet aggregation and can lead to thrombus formation in the blood vessels; 3) cardioembolic stroke following paroxysmal atrial fibrillation; 4) anaphylaxis causing severe hypotension resulting in decreased cerebral hypoperfusion leading to watershed infarct.[2]
Kounis described myocardial infarction following bee and wasp sting by different pathophysiological mechanisms. He postulated 2 variants: type 1 variant has preexisting normal blood vessels with vasospasm secondary to venom and type 2 variant due to rupture of preexisting atheromatous plaque as a result of allergic reaction of envenomation causing acute Myocardial infarction.[3] As similar mechanisms can also operate in cerebral blood vessels, thrombolysis in this setting appears reasonable, especially in view of type 2 kounis syndrome.
Our patient did not have vasospasm or occlusion in CT angiography (CTA). Thrombus formation could be either due to envenomation or kounis type 2 variant and its clearance with thrombolysis could be possible in our patient. However, the possibility of a transient vasospasm could not be completely ruled out as we performed cerebral angiogram after 48 h of bee sting besides treating with early antihistamines and steroids. We ruled out hypotension and arrhythmia-induced ischemic stroke by continuous hemodynamic and ECG monitoring. To the best of our knowledge, we could find only one case report of thrombolysis in the setting of ischemic stroke after wasp sting described by Kulhari et al. in the year 2016. In their case, CT angiography showed multiple areas of vasospasm in the bilateral middle cerebral artery regions.[2]
As there were no clear guidelines for the management of stroke following bee and wasp sting till date, we propose that thrombolysis with tissue-plasminogen activator can be done for ischemic strokes after hymenopterans sting. Patients with hymenoptera sting should be observed for at least 24 h in view of cerebrovascular and cardiovascular complications. We suggest that specific treatment strategies can be devised in future according to emergency CT angiogram abnormalities in this scenario. If vasospasm is clearly demonstrable, intra-arterial vasodilators like milrinone could be considered to reverse vasospasm[4] and instead if thrombotic occlusion is detected by imaging, thrombolysis and thrombectomy in appropriate settings may be the line of management. Future case experiences might further enlighten us about these treatment aspects in such case scenarios.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We would like to thank the entire team of Neurology Department, Emergency Department, and Radiology Department from Stanley medical college for their help in managing this patient. We also extend our thanks to Prof. Dr. V. Natarajan, former director, Madras Institute of Neurology, for his valuable suggestions in editing this case report.
REFERENCES
- 1.Moein P, Zand R. Cerebral Infarction as a rare complication of wasp sting. J Vasc Interv Neurol. 2017;9:13–6. [PMC free article] [PubMed] [Google Scholar]
- 2.Kulhari A, Rogers A, Wang H, Kumaraswamy VM, Xiong W, DeGeorgia M. Ischemic stroke after wasp sting. J Emerg Med. 2016;51:405–10. doi: 10.1016/j.jemermed.2016.06.016. [DOI] [PubMed] [Google Scholar]
- 3.Aminiahidashti H, Laali A, Samakoosh AK, Gorji AM. Myocardial infarction following a bee sting: A case report of Kounis syndrome. Ann Card Anaesth. 2016;19:375–8. doi: 10.4103/0971-9784.179626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fraticelli AT, Cholley BP, Losser MR, Saint Maurice JP, Payen D. Milrinone for the treatment of cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Stroke. 2008;39:893–8. doi: 10.1161/STROKEAHA.107.492447. [DOI] [PubMed] [Google Scholar]
- 5.Rajendiran C, Puvanalingam A, Thangam D, Ragunanthanan S, Ramesh D, Venkatesan S, et al. Stroke after multiple bee sting. J Assoc Physicians India. 2012;60:122–4. [PubMed] [Google Scholar]
- 6.Viswanathan S, Muthu V, Singh AP, Rajendran R, George R. Middle cerebral artery infarct following multiple bee stings. J Stroke Cerebrovasc Dis. 2012;21:148–50. doi: 10.1016/j.jstrokecerebrovasdis.2010.06.003. [DOI] [PubMed] [Google Scholar]