Abstract
Following the first report of COVID-19 infection in December 2019 as a respiratory illness, it has proven to be a multisystem disease. There are few reported cases of ischemic colitis with COVID-19 infection in the medical literature to date and we have limited understanding of its pathophysiology. We report 2 cases of ischemic colitis as the only manifestation of COVID-19. In addition, we review the current limited literature regarding COVID-19-associated ischemic colitis.
Keywords: COVID-19, coronavirus, gastrointestinal manifestation, ischemic colitis, colonic ischemia
Introduction
In December 2019, the first case of coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was reported in Wuhan, China. 1 The infection rapidly spread across the world and was declared a pandemic by the World Health Organization (WHO) on March 11, 2020. 2 As of July 19, 2021, the Centers for Disease Control and Prevention (CDC) has reported >600 000 deaths due to COVID-19 infection in the United States. 3 Patients with COVID-19 infection predominantly have respiratory symptoms, but gastrointestinal (GI) symptoms such as nausea, vomiting, abdominal pain, and diarrhea have been reported in up to 60% of these patients.4-12 In this article, we are reporting 2 cases of ischemic colitis as the only manifestation of COVID-19.
Case Description
Case 1
A 62-year-old man with hypertension, well-controlled type 2 diabetes, and gastroesophageal reflux disease presented to the hospital with multiple episodes of hematochezia for 1 day. He was hemodynamically stable and afebrile. He had mild left lower abdominal tenderness. Laboratory data revealed white blood cell count (WBC) 13 300/mm3, hemoglobin 13.2 g/dL, hematocrit 41.2%, and lactic acid 2.1 mmol/L. Stool culture and Clostridium difficile polymerase chain reaction (PCR) testing were negative. The SARS-CoV-2 PCR was positive. Patient did not have any respiratory compromise or hemodynamic instability throughout the hospitalization. Computed tomography (CT) of the abdomen and pelvis with intravenous contrast demonstrated inflammatory changes extending from the rectum to the splenic flexure with patent celiac, superior mesenteric, and inferior mesenteric arteries. Patient underwent flexible sigmoidoscopy that revealed severely edematous, ulcerated, friable mucosa extending 25 cm from the anal verge proximally to the splenic flexure (Figure 1). Colonic biopsies demonstrated small crypts, loss of goblet cells, hyalinization of lamina propria, and mucosal hemorrhage (Figure 2). Based on endoscopic and biopsy findings, he was diagnosed with ischemic colitis. He was given intravenous antibiotics. He was discharged home on day 3 of admission after resolution of leukocytosis and hematochezia.
Figure 1.
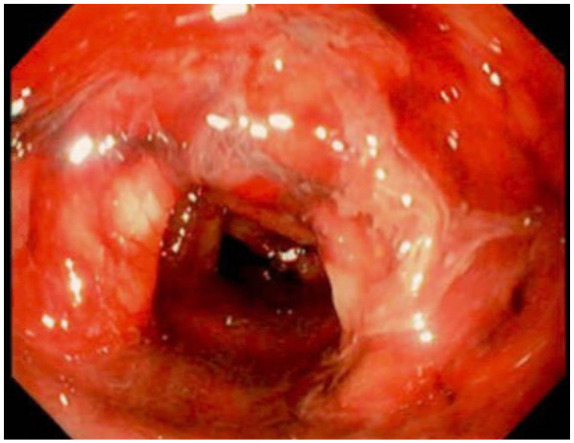
Flexible sigmoidoscopy—severely edematous, friable, ulcerated descending colon.
Figure 2.
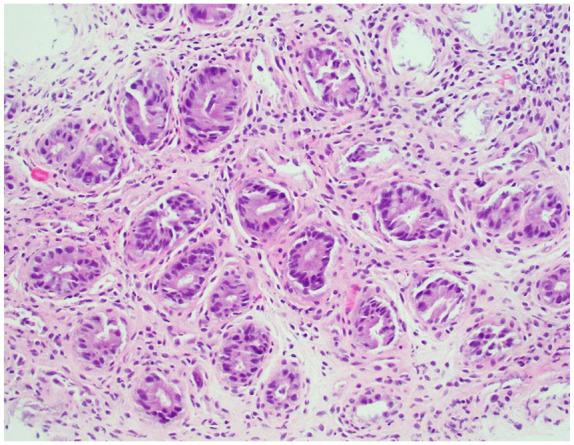
Colonic biopsy—loss of goblet cells and hyalinization of lamina propria.
Case 2
A 66-year-old woman with well-controlled type 2 diabetes and hyperlipidemia presented to the hospital with left lower abdominal pain, intermittent hematochezia, and nonbloody emesis for 2 days. She was diagnosed with asymptomatic COVID-19 infection 3 weeks prior to presentation based on positive SARS-CoV-2 PCR. Patient was afebrile and hemodynamically stable. She had mild left lower abdominal tenderness and examination was otherwise normal. Laboratory data revealed hemoglobin 13.9 g/dL, hematocrit 42.8% and lactic acid 2.4 mmol/L, and negative stool culture, C difficile PCR, and SARS-CoV-2 PCR. CT of abdomen and pelvis with intravenous contrast demonstrated inflammatory changes extending from hepatic flexure to sigmoid with patent celiac and mesenteric arteries. Patient underwent flexible sigmoidoscopy and this revealed cratered, clean-based, nonbleeding ulcers with surrounding mucosal erythema, edema, and friable mucosa involving the sigmoid and descending colon (Figure 3). Colonic biopsies demonstrated crypts with loss of goblet cells, hyalinization of lamina propria, and focal hemorrhage (Figure 4). Based on endoscopic and biopsy findings, patient was diagnosed with ischemic colitis. She was administered antibiotics and managed conservatively. She was discharged home on day 4 of admission, after resolution of hematochezia.
Figure 3.
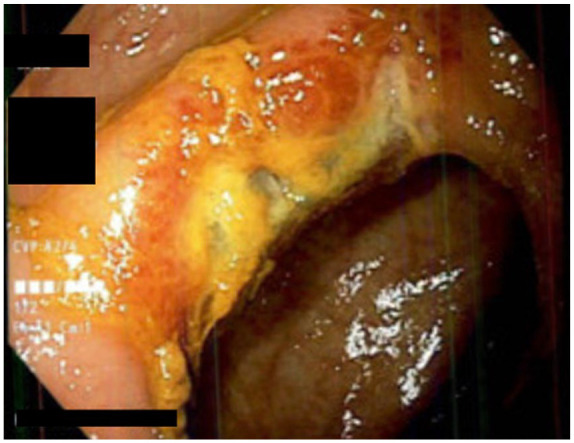
Flexible sigmoidoscopy—cratered, clean-based, nonbleeding ulcer in the descending colon.
Figure 4.
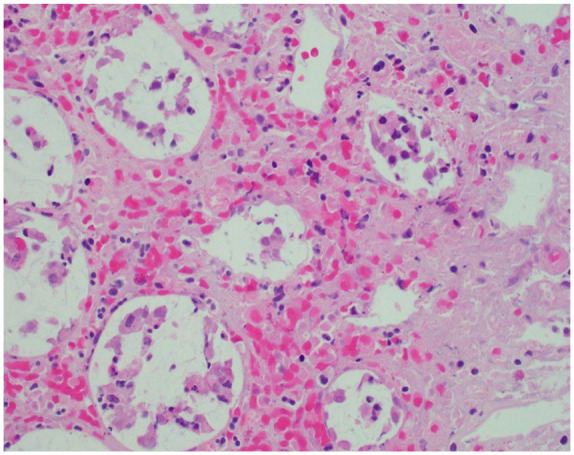
Colonic biopsy—loss of goblet cells, hyalinization of lamina propria and focal hemorrhage.
Discussion
With the evolution of the COVID-19 pandemic and growing recognition of various manifestations of the disease, there are an increasing number of reports in the medical literature about the rare and lesser understood extrapulmonary manifestations of the disease. One of the less frequently encountered GI manifestations of COVID-19 infection is ischemic colitis.
We searched the medical literature for reports of COVID-19-associated ischemic colitis and identified 15 patients from 9 publications with COVID-19-associated ischemic colitis and their characteristics are summarized in Table 1.13-21 Among the 15 patients, the outcome of 1 patient was not reported, 13 8 patients died, and 6 patients survived the illness. Among the survivors, 2 patients were managed medically19,20 and 4 patients required surgical management. We excluded 4 patients with ischemic enteritis,16,20,22 2 patients with incidentally found pneumatosis intestinalis,23,24 and cross-sectional studies published by Vanella et al and Bhayana et al on mucosal damage (6 patients with left-sided and 3 patients with diffuse ischemic colitis) and abdominal imaging findings in COVID-19 patients, respectively, due to limited availability of patient information (age, sex, preexisting condition[s], GI symptom[s], vasopressor requirement, presence of intravascular thrombus, treatment, and outcomes).25,26
Table 1.
Summary of COVID-19-Associated Ischemic Colitis Cases Reported in the Medical Literature.
| Patient number | Publication | Age/sex | Preexisting diseases | GI symptoms | Vasopressor requirement | Intravascular thrombi | Diagnostic tests | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Lakshmanan and Toubia | 72/Male | Multiple comorbidities (details NA) | Diffuse abdominal pain, rectal bleeding | No | NA | CT: thickening of descending and sigmoid colon, mid ascending colon, pneumatosis without portal venous gas | Medical | NA |
| 2 | Singh et al | 82/Female | HTN, DM | Abdominal distension, tenderness | No | CT angiogram: no evidence of atherosclerosis; pathology: microvascular thrombosis | CT: PI of ascending colon and cecum; intraoperative findings: gangrenous ascending colon, marked distension from cecum to rectosigmoid junction | Surgical ileostomy | Alive |
| 3 | Almeida et al | 76/Male | HTN | Rectal bleeding | NA | No | Endoscopy: erythema, edema and fragile mucosa; CT: signs of colonic ischemia such as wall thickening, absence of wall enhancement, mesenteric stranding of sigmoid | Medical | Death |
| 4 | Almeida et al | 68/Male | HTN, DM, dyslipidemia | Abdominal distension, paralytic ileus, signs of peritoneal irritation | NA | No | CT: cecal perforation, pneumatosis of left colon; intraoperative findings: fecaloid peritonitis, gangrenous perforation of cecum, diffuse ischemia of colon | Surgical ileostomy and peritoneal lavage | Death |
| 5 | Almeida et al | 56/Male | HTN, DM, COPD, dyslipidemia, obesity | Abdominal distension, tenderness, guarding | NA | No | CT: small bowel distension, colonic pneumatics, pneumoperitoneum | Medical | Death |
| 6 | Norsa et al | 85/Male | NA | Lower GI bleeding | NA | NA | CT and endoscopy: ischemic colitis | NA | Alive |
| 7 | Norsa et al | 71/Female | NA | Loss of appetite, vomiting, lower GI bleeding | NA | NA | Endoscopy: ischemic colitis | NA | Alive |
| 8 | Norsa et al | 69/Male | NA | Diarrhea, fever, dyspnea | NA | NA | CT: ischemic colitis (right colon) | NA | Death |
| 9 | Norsa et al | 63/Male | NA | GI symptom not specified | NA | NA | CT: right and transverse colon ischemia, splenic infarcts | NA | Death |
| 10 | Norsa et al | 83/Female | NA | Dyspnea, abdominal pain | NA | NA | CT: small bowel and colon ischemia | NA | Death |
| 11 | Chan et al | 73/Male | HTN, ESRD | Bloody diarrhea | No | NA | CT: mucosal hyperenhancement with mass-like thickening of distal sigmoid colon and regional air within mesenteric vessels concerning for ischemic colitis | Medical | Death |
| 12 | González Lázaro et al | 53/Male | DM, hypercholesterolemia | Abdominal pain, vomiting | NA | NA | CT: mucosal hypoenhancement of ascending colon concerning for ischemic colitis | Surgical resection of 148 cm of small bowel and 32 cm of right colon and end ileostomy | Alive |
| 13 | Paul et al | 66/Male | None | Diarrhea, melena | Yes | NA | Endoscopy: multiple ulcerations of sigmoid colon | Medical | Alive |
| 14 | Kinjo et al | 45/Male | None | Hematochezia | NA | No | CT: thickening of descending colon, engorgement of mesenteric vessels | Medical | Alive |
| 15 | Varshney et al | 50/Female | HTN, hospitalization for COVID-19 pneumonia 2 weeks prior to current hospitalization | Abdominal pain, constipation | Yes | CT: larger sized arteries were patent with no apparent atherosclerotic disease; pathology: thickened intima with compromised lumen | CT: grossly distended distal segment of descending and sigmoid colon, imperceptible posterior wall of sigmoid possibly due to ruptured diverticulum; intraoperative finding: gangrenous sigmoid, ischemic descending colon with multiple perforations | Surgical drainage of collection, left colectomy, transverse colectomy, and rectal stump closure (Hartmann procedure) | Death |
| 16 | Case 1 | 62/Male | HTN, DM, GERD | Hematochezia | No | No | CT: inflammatory changes extending from rectum to splenic flexure | Medical | Alive |
| 17 | Case 2 | 66/Female | DM, hyperlipidemia | Left lower quadrant pain, hematochezia, nonbloody emesis | No | No | CT: inflammatory changes extending from hepatic flexure to sigmoid | Medical | Alive |
Abbreviations: GI, gastrointestinal; NA, not available; CT, computed tomography; HTN, hypertension; DM, diabetes; PI, pneumatics intestinalis; COPD, chronic obstructive pulmonary disease; ESRD, end-stage renal disease; GERD, gastroesophageal reflux disease.
Both cases 1 and 2 reported by us do not have any risk factors for intestinal ischemia but had clinical features consistent with ischemic colitis. Neither of the 2 patients had hemodynamic instability or imaging evidence of intravascular thrombosis. Case 1 had positive COVID-19 PCR during the admission, whereas case 2 had recent asymptomatic COVID-19 infection preceding the admission for ischemic colitis. There is no definitive proof of causation; however, given the diagnosis of ischemic colitis during/recent infection with COVID-19, we diagnosed both patients with COVID-19-associated ischemic colitis.
Human-to-human transmission of COVID-19 infection is mainly through respiratory droplets. The hallmark of COVID-19 infection is severe respiratory illness; however, other organs, including GI tract, are also affected. Angiotensin-converting enzyme 2 (ACE2) receptor that plays a key role in the viral entry is expressed in the gastric, duodenal, and rectal epithelia. 27 The most common GI symptoms are diarrhea (34%), nausea (27%), vomiting (16%), and abdominal pain (11%). 28 In a retrospective study conducted by Laszkowska et al, patients with GI symptoms had an indolent course with lower rates of intubation and death. 29
In patients with COVID-19, coagulopathy is suspected to be related to the high inflammatory state and is associated with increased mortality and morbidity.30,31 Most common thromboembolic complications are pulmonary embolism, deep vein thrombosis, and, rarely, mesenteric ischemia. Acute mesenteric ischemia is associated is very high morbidity and mortality. Following prompt diagnosis, patients with mesenteric ischemia should be treated with fluid resuscitation and surgical resection of necrotic bowel with restoration of blood flow to the ischemic intestine.14,15
The reduced blood flow state in colonic ischemia (CI) is insufficient to maintain cellular metabolic function. 32 The CI is the cause of 9% to 24% of all hospitalizations for acute lower GI bleeding.33-35 There is higher incidence of CI after age 49 and has a female predilection.36,37 CI results from alterations in the systemic circulation or from anatomic or functional changes in the mesenteric vasculature. 32 Typical clinical presentation is sudden onset abdominal pain, urge to defecate, and rectal bleeding within 24 hours. 37 These symptoms resolve in 2 to 3 days and colon usually heals in 1 to 2 weeks. 32 Left colon is most commonly affected and includes the watershed areas—splenic flexure and sigmoid colon. Early colonoscopy (less than 48 hours) with minimum insufflation is recommended in suspected cases to confirm the diagnosis.38-40
The pathophysiological mechanism in COVID-19 resulting in ischemic colitis is poorly understood. None of the patients with COVID-19 ischemic colitis had mesenteric arterial occlusion detectable in imaging, but 2 patients had microthrombi in pathology specimen.14,21 Patients with severe COVID-19 infection have nonocclusive CI due to intense vasoconstriction and decreased mesenteric blood flow secondary to hemodynamic compromise and use of inotropic agents. 14
In cases 1 and 2, there was no hemodynamic instability or radiographic evidence of thrombosis. We suspect that our patients developed ischemic colitis, most likely due to SARS-CoV-2-induced endotheliitis or direct bowel damage due to expression of ACE-2. Given the limited information available on COVID-19-associated ischemic colitis, further research is needed to better understand this condition.
Footnotes
Author Contributions: Each author contributed substantially to the work, worked on the drafting of the manuscript, and was involved in its final approval.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: Our institution does not require ethical approval for reporting individual cases or case series.
Informed Consent: Verbal informed consent was obtained from the patients for their anonymized information to be published in this article.
ORCID iDs: Rajarajeshwari Ramachandran  https://orcid.org/0000-0001-5367-869X
https://orcid.org/0000-0001-5367-869X
Swetha Parvataneni  https://orcid.org/0000-0002-5932-2237
https://orcid.org/0000-0002-5932-2237
References
- 1. Archived: WHO Timeline–COVID-19. Who.int. https://www.who.int/news/item/27-04-2020-who-timeline—covid-19. Accessed October 18, 2021.
- 2. WHO Director-General’s opening remarks at the media briefing on COVID-19–11 March 2020. Who.int. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020. Accessed July 19, 2021.
- 3. CDC. COVID data tracker. Cdc.gov. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html. Accessed July 19, 2021.
- 4. Guan W-J, Ni Z-Y, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708-1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jin X, Lian J-S, Hu J-H, et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut. 2020;69(6):1002-1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sultan S, Altayar O, Siddique SM, et al. AGA institute rapid review of the gastrointestinal and liver manifestations of COVID-19, meta-analysis of international data, and recommendations for the consultative management of patients with COVID-19. Gastroenterology. 2020;159(1):320-334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Parasa S, Desai M, Thoguluva Chandrasekar V, et al. Prevalence of gastrointestinal symptoms and fecal viral shedding in patients with coronavirus disease 2019: a systematic review and meta-analysis: a systematic review and meta-analysis. JAMA Netw Open. 2020;3(6):e2011335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. D’Amico F, Baumgart DC, Danese S, Peyrin-Biroulet L. Diarrhea during COVID-19 infection: pathogenesis, epidemiology, prevention, and management. Clin Gastroenterol Hepatol. 2020;18(8):1663-1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Aroniadis OC, DiMaio CJ, Dixon RE, et al. Current knowledge and research priorities in the digestive manifestations of COVID-19. Clin Gastroenterol Hepatol. 2020;18(8):1682-1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Redd WD, Zhou JC, Hathorn KE, et al. Prevalence and characteristics of gastrointestinal symptoms in patients with severe acute respiratory syndrome coronavirus 2 infection in the United States: a multicenter cohort study. Gastroenterology. 2020;159(2):765-767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hajifathalian K, Krisko T, Mehta A, et al. Gastrointestinal and hepatic manifestations of 2019 novel coronavirus disease in a large cohort of infected patients from New York: clinical implications. Gastroenterology. 2020;159(3):1137-1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lakshmanan S, Toubia N. Pneumatosis intestinalis in COVID-19. Clin Gastroenterol Hepatol. 2021;19(10):e99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Singh B, Mechineni A, Kaur P, et al. Acute intestinal ischemia in a patient with COVID-19 infection. Korean J Gastroenterol. 2020;76(3):164-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Almeida Vargas A, Valentí V, Sánchez Justicia C, et al. Severe colon ischemia in patients with severe coronavirus-19 (COVID-19). Rev Esp Enferm Dig. 2020;112(10):784-787. [DOI] [PubMed] [Google Scholar]
- 16. Norsa L, Bonaffini PA, Indriolo A, Valle C, Sonzogni A, Sironi S. Poor outcome of intestinal ischemic manifestations of COVID-19. Gastroenterology. 2020;159(4):1595-1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chan KH, Lim SL, Damati A, et al. Coronavirus disease 2019 (COVID-19) and ischemic colitis: an under-recognized complication. Am J Emerg Med. 2020;38(12):2758e1-2758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. González Lázaro P, Lomas Meneses A, Del Val Zaballos F, Morandeira Rivas A. Ischemic colitis and short bowel disease due to choronavirus disease 2019 (COVID 19). Clin Nutr ESPEN. 2020;40:406-407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Paul T, Joy AR, Alsoub Parambil JV. Case report: ischemic colitis in severe COVID-19 pneumonia: an unforeseen gastrointestinal complication. Am J Trop Med Hyg. 2021;104(1):63-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kinjo T, Hokama A, Nakamura H, et al. Case report: ischemic enterocolitis associated with coronavirus disease 2019: two case reports and a review of the literature. Am J Trop Med Hyg. 2021;104(5):1655-1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Varshney R, Bansal N, Khanduri A, Gupta J, Gupta R. Colonic gangrene: a sequela of coronavirus disease 2019. Cureus. 2021;13(4):e14687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kielty J, Duggan WP, O’Dwyer M. Extensive pneumatics intestinalis and portal venous gas mimicking mesenteric ischaemia in a patient with SARS-CoV-2. Ann R Coll Surg Engl. 2020;102(6):e145-e147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Meini S, Zini C, Passaleva MT, et al. Pneumatosis intestinalis in COVID-19. BMJ Open Gastroenterol. 2020;7(1):e000434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Aiello P, Johnson S, Ramos Mercado A, Hussein S. Pneumatosis intestinalis in a patient with COVID-19. BMJ Case Rep. 2020;13(9):e237564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Vanella G, Capurso G, Burti C, et al. Gastrointestinal mucosal damage in patients with COVID-19 undergoing endoscopy: an international multicentre study. BMJ Open Gastroenterol. 2021;8(1):e000578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bhayana R, Som A, Li MD, et al. Abdominal imaging findings in COVID-19: preliminary observations. Radiology. 2020;297(1):E207-E215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020;158(6):1831-1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Elmunzer BJ, Spitzer RL, Foster LD, et al. Digestive manifestations in patients hospitalized with coronavirus disease 2019. Clin Gastroenterol Hepatol. 2021;19(7):1355-1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Laszkowska M, Faye AS, Kim J, et al. Disease course and outcomes of COVID-19 among hospitalized patients with gastrointestinal manifestations. Clin Gastroenterol Hepatol. 2021;19(7):1402-1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Spiezia L, Boscolo A, Poletto F, et al. COVID-19-related severe hypercoagulability in patients admitted to Intensive Care Unit for acute respiratory failure. Thromb Haemost. 2020;120(6):998-1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Panigada M, Bottino N, Tagliabue P, et al. Hypercoagulability of COVID-19 patients in intensive care unit: a report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost. 2020;18(7):1738-1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Brandt LJ, Feuerstadt P, Longstreth GF, Boley SJ, American College of Gastroenterology. ACG clinical guideline: epidemiology, risk factors, patterns of presentation, diagnosis, and management of colon ischemia (CI). Am J Gastroenterol. 2015;110(1):18-44; quiz 45. [DOI] [PubMed] [Google Scholar]
- 33. Hreinsson JP, Gumundsson S, Kalaitzakis E, Björnsson ES. Lower gastrointestinal bleeding: incidence, etiology, and outcomes in a population-based setting. Eur J Gastroenterol Hepatol. 2013;25(1):37-43. [DOI] [PubMed] [Google Scholar]
- 34. Arroja B, Cremers I, Ramos R, et al. Acute lower gastrointestinal bleeding management in Portugal: a multicentric prospective 1-year survey. Eur J Gastroenterol Hepatol. 2011;23(4):317-322. [DOI] [PubMed] [Google Scholar]
- 35. Longstreth GF. Epidemiology and outcome of patients hospitalized with acute lower gastrointestinal hemorrhage: a population-based study. Am J Gastroenterol. 1997;92(3):419-424. [PubMed] [Google Scholar]
- 36. Suh DC, Kahler KH, Choi IS, Shin H, Kralstein J, Shetzline M. Patients with irritable bowel syndrome or constipation have an increased risk for ischaemic colitis. Aliment Pharmacol Ther. 2007;25(6):681-692. [DOI] [PubMed] [Google Scholar]
- 37. Longstreth GF, Yao JF. Epidemiology, clinical features, high-risk factors, and outcome of acute large bowel ischemia. Clin Gastroenterol Hepatol. 2009;7(10):1075-1080. [DOI] [PubMed] [Google Scholar]
- 38. Montoro MA, Brandt LJ, Santolaria S, et al. Clinical patterns and outcomes of ischaemic colitis: results of the Working Group for the Study of Ischaemic Colitis in Spain (CIE study). Scand J Gastroenterol. 2011;46(2):236-246. [DOI] [PubMed] [Google Scholar]
- 39. Brandt LJ, Boley SJ, Sammartano R. Carbon dioxide and room air insufflation of the colon. Gastrointest Endosc. 1986;32(5):324-329. [DOI] [PubMed] [Google Scholar]
- 40. Kozarek RA, Earnest DL, Silverstein ME, Smith RG. Air-pressure-induced colon injury during diagnostic colonoscopy. Gastroenterology. 1980;78(1):7-14. [PubMed] [Google Scholar]


