Abstract
Background/Objectives:
State-specific obesity prevalence data are critical to public health efforts to address the childhood obesity epidemic. However, few states administer objectively-measured BMI surveillance programs. This study reports state-specific childhood obesity prevalence by age and sex correcting for parent-reported child height and weight bias.
Subjects/Methods:
As part of the Childhood Obesity Intervention Cost Effectiveness Study (CHOICES), we developed childhood obesity prevalence estimates for states for the period 2005–2010 using data from the 2010 U.S. Census and American Community Survey (ACS), 2003–2004 and 2007–2008 National Survey of Children’s Health (NSCH) (n=133,213), and 2005–2010 National Health and Nutrition Examination Surveys (NHANES) (n=9,377; ages 2–17). Measured height and weight data from NHANES were used to correct parent-report bias in NSCH using a non-parametric statistical matching algorithm. Model estimates were validated against surveillance data from five states (AR, FL, MA, PA, and TN) that conduct censuses of children across a range of grades.
Results:
Parent-reported height and weight resulted in the largest overestimation of childhood obesity in males ages 2–5 years (NSCH: 42.36% vs. NHANES: 11.44%). The CHOICES model estimates for this group (12.81%) and for all age and sex categories were not statistically different from NHANES. Our modeled obesity prevalence aligned closely with measured data from five validation states, with a 0.64 percentage point mean difference (range: 0.23–1.39) and a high correlation coefficient (r=0.96, p=0.009). Estimated state-specific childhood obesity prevalence ranged from 11.0% to 20.4%.
Conclusion:
Uncorrected estimates of childhood obesity prevalence from NSCH vary widely from measured national data, from a 278% overestimate among males aged 2–5 years to a 44% underestimate among females aged 14–17 years. This study demonstrates the validity of the CHOICES matching methods to correct the bias of parent-reported BMI data and highlights the need for public release of more recent data from the 2011–2012 NSCH.
Background
Despite decades of effort to address the childhood obesity epidemic, public health practitioners often must plan and evaluate prevention and treatment strategies in the absence of accurate state-specific child BMI surveillance data. Although the number of states collecting child BMI data has grown in recent years, currently only one quarter of U.S. states conduct ongoing, objectively-measured BMI surveillance programs.1 These data are of critical importance for targeting limited national obesity prevention resources and planning clinical staffing to meet expected increases in obesity-related co-morbidities.
The Pediatric Nutrition Surveillance System (PedNSS) provided state-level, measured BMI data on 8 million 0–5 year old children participating in federal maternal and child health programs for three decades, but was not representative of the total population, and was discontinued in 2012.2 The Youth Risk Behavior Surveillance System (YRBSS) collects state-representative self-reported estimates of BMI from high school students, which have been shown to be biased compared to measured data and cannot be used to estimate prevalence in younger ages.3–5 NHANES provides unbiased demographic-specific childhood obesity data, but the sample is too small for state-level estimation.
Previous studies have estimated state-specific childhood obesity prevalence using parent-reported height and weight for children participating in the National Survey of Children’s Health (NSCH).6 In adults, self-report bias leading to an underestimation of BMI and obesity prevalence has been characterized for all ages.7 However, bias in parent-reported child height and weight varies qualitatively by the age and sex of the children. Compared to objectively measured data from the National Health and Nutrition Examination Survey (NHANES), parents overestimate their children’s BMI when children are young and underestimate BMI during adolescence, leading to substantially biased estimates of obesity prevalence.8, 9 Using uncorrected estimates from NSCH would lead to biased estimates of the state-specific prevalence of childhood obesity. Due to the lack of national datasets that include both parent-reported and measured height and weight, it is not possible to use an individual-level regression-based approach for bias correction, as previously done for adults.10
The objective of this study is to provide bias-corrected state-specific estimates of childhood obesity prevalence across all ages for the period 2005–2010 using statistical matching techniques and to validate these estimates against objectively-measured BMI surveillance data from five states that conducted school-based censes of student height and weight. These methods were developed for use in the Childhood Obesity Intervention Cost Effectiveness Study (CHOICES) project, which is evaluating both national and state-specific cost-effectiveness of a broad range of nutrition and physical activity policies to prevent childhood obesity using a microsimulation model of the U.S. population.11
Methods
Data
State-specific parent-reported height and weight are from the 2003–2004 and 2007–2008 waves of the NSCH, which is a national and state-representative telephone survey covering a range of children’s health data conducted by the Centers for Disease Control and Prevention’s National Center for Health Statistics. Additional detail on the sampling methodology has been reported previously.12, 13 Data from both waves of the surveys were available for a combined 213,900 responses. After excluding observations with missing demographic variables needed for the matching process (n=29,234) and those missing parent-reported height and weight (n=51,453), 133,213 responses were used in this study’s analysis. Sample weights were pooled across survey rounds. Data on younger children (<10 years of age) were only available from the 2003–2004 wave of data collection. Data on height and weight were not available in the 2011–2012 NSCH public use datasets, although derived BMI categories are available based on parent self-reported height and weight for participants aged 10–17 years.
Data on measured height and weight were from the 2005–2010 NHANES. Data were pooled across survey waves to allow for sufficient sample sizes within precisely defined demographic strata to capture the population height and weight distributions for each group. There were 9,957 individuals aged 2–17. After excluding individuals with missing demographic data (n=356) and those with missing height and weight (n=224), data were analyzed from 9,377 individuals aged 2–17. Sample weights were calculated for all individuals based on NHANES analytic guidelines.
Population counts and demographic characteristics representative at the state level were sampled from the 2010 U.S. Census using a simple random sample. Sampled individuals included information on census tract age, sex, and race/ethnicity. Data on household income are from the 5-year aggregated 2010 American Community Survey.
In order to validate our model estimates, data from all available state BMI census systems were identified through a staged search process.1 Data were included for model validation from five states (AR, FL, MA, PA, and TN) that conducted and published results from a census of all students across three or more grades.14–18 The use of school-based census data eliminates sampling error from child BMI surveillance, but may not include children in private schools and does not include children not attending school. For validation purposes, the use of multiple grade levels reduces uncertainty around model estimates for a single age group within specific states, which are based on smaller sample sizes from 2003–2008 NSCH. Data from these five states include observations on 3 million participants per year with the latest data reported from each state ranging from 2012–2014.
Statistical Matching Process
We developed a non-parametric statistical matching algorithm to correct for parent-report bias in the state-specific National Survey of Children’s Health (NSCH) surveys using measured height and weight data from the National Health and Nutrition Examination Survey (NHANES) in order to generate bias-corrected prevalence estimates.19–22 This method combines demographic data from the U.S. Census and the American Community Survey with data on height and weight from NSCH and NHANES. The method matches children based on their percentile of parent-reported height and weight from NSCH to measured height and weight percentiles within strata based on age, sex, race/ethnicity and household income. The resulting CHOICES model population thus recreates the national distribution of children’s and adolescents’ measured height and weight from NHANES while also capturing state-level variation in parent-reported height and weight from NSCH. State-specific childhood obesity prevalence for youth 2–17 years of age was calculated based on the matched population.
Statistical Analysis
The validity of our method was evaluated in two ways. First, we compared national estimated obesity prevalence within age and sex categories from the uncorrected NSCH pooled sample and our bias-corrected model to estimates of measured obesity prevalence from NHANES 2005–2010 using χ2 tests. Second, we compared our modeled estimates of obesity prevalence within age strata to the most recently published data (2012–2014) from five states with statewide measured obesity prevalence across a range of ages. Pearson correlation coefficients and mean differences between modeled and observed obesity prevalence were estimated using SAS version 9.4.
Additional detail on the methods used to generate the CHOICES model population and discussion of the process for model replication are available in the appendix. All matching analyses and comparisons between populations were performed using Java, a compiled programming language. Data used in the analysis are publicly available. Code is not publicly available. No protocol approval was needed for this study because it uses only publicly-available, de-identified data.
Results
Parent-reported height and weight led to overestimates of mean BMI until age ten and underestimates at later ages, particularly amongst adolescent females, leading to substantial errors in obesity prevalence estimates (Table 1). Comparison of mean height, weight, and BMI from unadjusted 2003–2008 NSCH national sample and measured data from the 2005–2010 NHANES identified significant differences across almost all age and sex groups (Appendix A and Appendix B). Parent-reported height and weight resulted in the largest overestimation of childhood obesity in males aged 2–5 years (NSCH: 43.26% vs. NHANES: 11.44%), a 278% percent overestimate of obesity prevalence in this group (Table 1). This large difference is due to parental underestimates of children’s height at younger ages (Appendix B). The mean difference in height is relatively small at 4% (3.89 cm), but as a squared term results in a 15.6% overestimate of mean BMI (18.95 vs. 16.39 BMI units). This results in a substantially greater overestimate of obesity prevalence due to the age and sex-specific cut point for childhood obesity and the current distribution of BMI. For adolescent females 10–17 years of age, the average parent-reported BMI is nearly 1 whole unit (0.94) lower than measured data from NHANES, leading to a 5.7 percentage point underestimate (33%) of obesity prevalence in this group nationally (NHANES: 17.23% (15.29%−19.16%) vs. NSCH: 11.53% (10.85%−12.21%)) (data not shown). Among adolescents, parents underreport weight compared to measured data (Appendix B).
Table 1.
Comparison of obesity prevalence estimates for 2005–2010 by sex and age group from NHANES, NSCH, and CHOICES model
| Obesity Prevalence (%) | NHANES v NSCHa | NHANES v CHOICES Modela | |||||
|---|---|---|---|---|---|---|---|
| Age Group | NHANES | NSCH | CHOICES Model | χ2 | p | χ2 | p |
| Males | |||||||
| 2–5 | 11.44 (9.40–13.49) | 43.26 (41.49–45.03) | 12.81 (12.70–12.89) | 505.12 | <0.001 | 2.29 | 0.130 |
| 6–9 | 17.75 (15.18–20.32) | 32.38 (30.72–34.03) | 17.63 (17.52–17.76) | 102.46 | <0.001 | 0.01 | 0.912 |
| 10–13 | 20.36 (17.46–23.27) | 21.59 (20.36–22.81) | 20.92 (20.81–21.02) | 0.95 | 0.330 | 0.21 | 0.646 |
| 14–17 | 18.78 (15.96–21.61) | 14.81 (13.64–15.98) | 18.36 (18.29–18.44) | 13.86 | <0.001 | 0.14 | 0.711 |
| Females | |||||||
| 2–5 | 10.48 (8.35–12.60) | 37.79 (36.03–39.56) | 12.23 (12.15–12.31) | 357.34 | <0.001 | 3.55 | 0.060 |
| 6–9 | 15.90 (13.32–18.48) | 29.93 (28.09–31.78) | 16.42 (16.28–16.53) | 96.81 | <0.001 | 0.23 | 0.633 |
| 10–13 | 18.88 (16.08–21.68) | 14.35 (13.22–15.47) | 20.38 (20.30–20.49) | 17.55 | <0.001 | 1.56 | 0.211 |
| 14–17 | 15.70 (13.02–18.38) | 8.75 (8.01–9.50) | 15.75 (15.63–15.86) | 59.62 | <0.001 | 0.00 | 0.960 |
Sources: National Health and Nutrition Examination Survey (NHANES) 2005–2010 (n=9,377). National Survey of Children’s Health (NSCH) 2003–2004 and 2007–2008 (n=133,213). CHOICES Model incorporates data from NSCH, NHANES, 2010 U.S. Census and 2010 5-year American Community Survey.
Chi-square independent sample test of equality of proportions between NHANES and NSCH or CHOICES estimates.
In contrast to the unadjusted NSCH obesity prevalence estimates, there were no significant differences in estimated obesity prevalence within age and sex strata between the CHOICES model and estimates using measured data from NHANES (Table 1). CHOICES model estimates within age and sex strata were on average within 6% (0.79 percentage points) of estimated prevalence from NHANES. BMI distributions by age and sex were similar for the 2005–2010 NHANES sample and the synthesized U.S. population (Appendix C).
At the state level, our bias-adjusted obesity prevalence estimates matched well to age-specific obesity prevalence data obtained from the five measured state BMI surveillance systems. The model-derived obesity prevalence estimates aligned closely with measured data, with a mean difference of 0.64 percentage points (range: 0.23–1.39) and a high correlation coefficient (r=0.96, p=0.009) (Table 2).
Table 2.
Validation of adjusted obesity prevalence estimates to BMI census data from five states
| State | Arkansas | Florida | Massachusetts | Pennsylvania | Tennessee |
|---|---|---|---|---|---|
| Year | 2013–2014 | 2013–2014 | 2013–2014 | 2012–2013 | 2012–2013 |
| Population (N) | 182,640 | 548,665 | 243,240 | 1,803,689 | 327,487 |
| Grades a | K,2,4,6,8,10 | 1,3,6 | 1,4,7,10 | K-12 | K,2,4,6,8–12 |
| Reported Obesity Prevalence (%) | 21.5 | 19.1 | 15.3 | 17.12 | 21.5 |
| CHOICES Model Obesity Prevalence (%) | 22.38 | 19.33 | 16.69 | 16.85 | 21.09 |
| Difference (%) | 0.88 | 0.23 | 1.39 | 0.27 | 0.41 |
A map of the CHOICES model estimated prevalence of obesity by state is presented in Figure 1, the prevalence of overweight and obesity in Appendix D, and point estimates and uncertainty for both overweight and obesity in Table 3. Estimated state-specific obesity prevalence ranged from 11.0% (Utah) to 20.4% (Tennessee). Estimated state-specific overweight prevalence ranged from 12.7% (Utah) to 18.1% (Louisiana).
Figure 1.
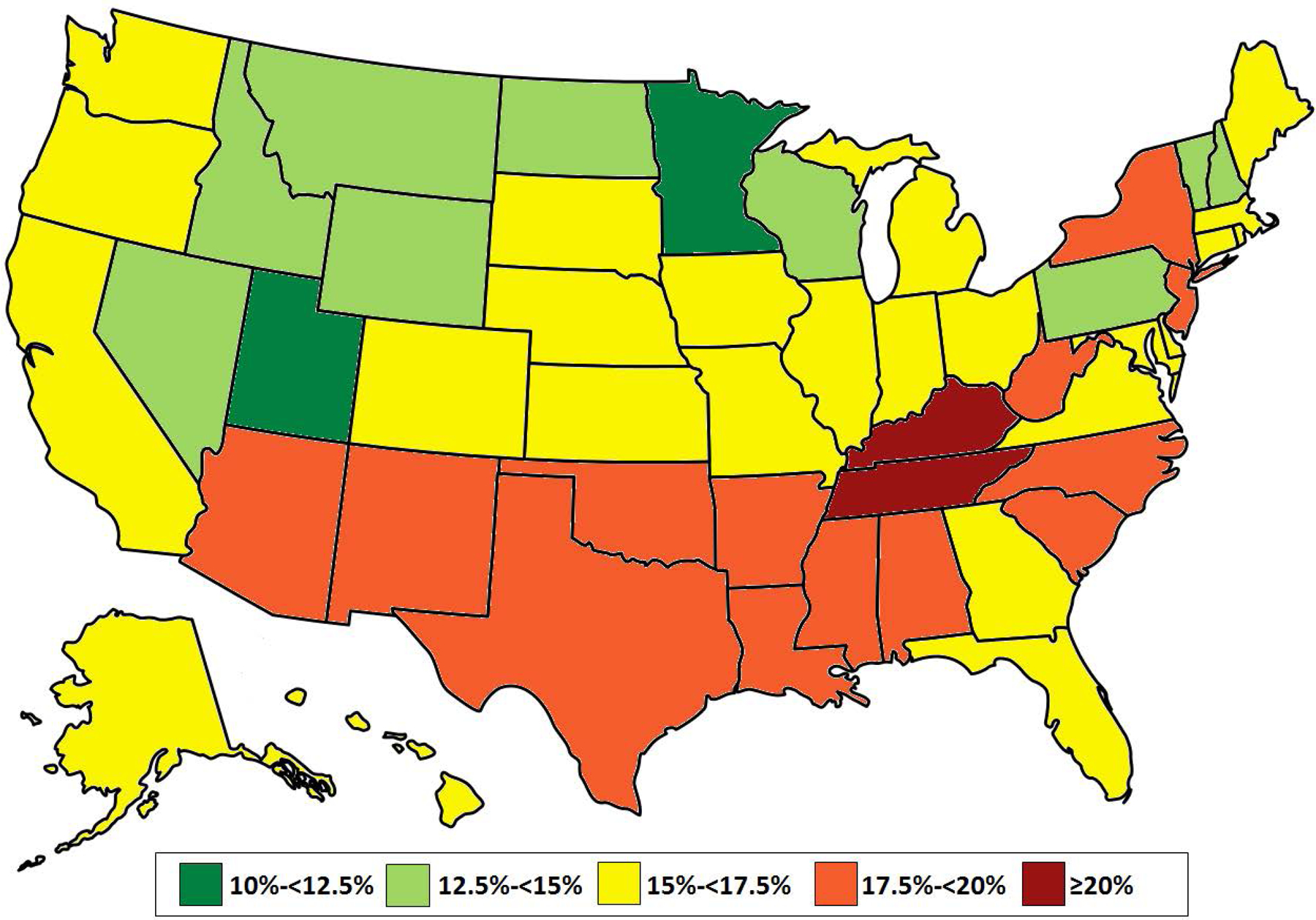
Childhood obesity prevalence by state in 2005–2010 estimated by CHOICES model
Table 3.
CHOICES model estimated childhood (2–17 years of age) overweight and obesity prevalence for 2005–2010 by state and sex
| Overweight prevalence (Range)a | Obesity prevalence (Range) | |||||
|---|---|---|---|---|---|---|
| State | Total | Male | Female | Total | Male | Female |
| NATIONAL | 15.7 (15.7–15.7) | 16.1 (16.1–16.1) | 15.3 (15.2–15.3) | 17.0 (17.0–17.1) | 17.6 (17.6–17.7) | 16.4 (16.3–16.4) |
| Alabama | 16.2 (16.0–16.5) | 15.0 (14.6–15.3) | 17.4 (17.1–17.8) | 18.8 (18.5–19.0) | 20.1 (19.7–20.5) | 17.4 (16.9–17.8) |
| Alaska | 16.7 (16.2–17.7) | 19.6 (18.5–21.0) | 14.0 (13.3–15.1) | 15.5 (14.9–16.3) | 13.1 (12.0–13.9) | 17.9 (16.6–19.1) |
| Arizona | 15.2 (15.0–15.4) | 17.0 (16.7–17.3) | 13.5 (13.2–13.7) | 19.4 (19.1–19.6) | 18.7 (18.4–19.1) | 20.0 (19.6–20.3) |
| Arkansas | 15.4 (15.2–15.7) | 15.1 (14.5–15.7) | 15.6 (15.3–16.2) | 19.6 (19.2–19.9) | 19.3 (18.9–19.6) | 19.9 (19.5–20.3) |
| California | 15.2 (15.1–15.4) | 15.3 (15.1–15.5) | 15.2 (15.0–15.3) | 17.0 (16.9–17.1) | 19.3 (19.1–19.5) | 14.8 (14.7–15.0) |
| Colorado | 13.8 (13.4–14.0) | 13.1 (12.7–13.5) | 14.4 (14.1–14.7) | 15.3 (14.9–15.6) | 16.3 (15.9–16.7) | 14.4 (13.7–14.7) |
| Connecticut | 15.1 (14.8–15.3) | 15.5 (15.1–15.9) | 14.7 (14.3–15.1) | 16.6 (16.2–16.9) | 16.6 (16.2–16.9) | 16.6 (16.1–17.0) |
| Delaware | 16.0 (15.5–16.6) | 16.2 (15.6–17.2) | 15.8 (14.7–16.8) | 16.3 (15.7–17.1) | 14.3 (13.7–15.5) | 18.2 (17.2–19.1) |
| District of Columbia | 14.4 (13.4–15.1) | 13.8 (12.9–15.2) | 15.0 (13.8–16.1) | 18.9 (17.9–19.9) | 16.5 (14.7–17.5) | 21.2 (19.2–22.7) |
| Florida | 16.4 (16.3–16.6) | 16.2 (16.0–16.4) | 16.7 (16.4–16.9) | 17.0 (16.9–17.2) | 19.0 (18.8–19.2) | 15.1 (14.9–15.3) |
| Georgia | 15.9 (15.7–16.1) | 16.7 (16.4–16.9) | 15.0 (14.8–15.3) | 16.1 (15.9–16.2) | 15.7 (15.5–15.8) | 16.5 (16.3–16.7) |
| Hawaii | 14.0 (13.7–14.5) | 15.0 (14.5–15.5) | 13.1 (12.3–13.8) | 15.7 (15.2–16.4) | 16.1 (15.4–17.1) | 15.3 (14.5–16.0) |
| Idaho | 16.5 (15.9–17.0) | 17.2 (16.5–17.7) | 15.8 (15.1–16.3) | 13.8 (13.4–14.3) | 17.0 (16.3–17.7) | 10.5 (10.1–11.0) |
| Illinois | 16.0 (15.9–16.2) | 17.2 (17.0–17.6) | 14.8 (14.6–15.1) | 16.4 (16.2–16.5) | 17.7 (17.4–18.0) | 15.0 (14.8–15.2) |
| Indiana | 15.6 (15.4–15.9) | 15.1 (14.8–15.3) | 16.2 (15.9–16.4) | 16.8 (16.5–17.0) | 17.4 (17.0–17.8) | 16.1 (15.7–16.4) |
| Iowa | 15.7 (15.3–16.0) | 14.7 (14.2–15.2) | 16.6 (16.2–17.3) | 16.3 (15.9–16.5) | 16.6 (16.1–17.0) | 15.9 (15.4–16.3) |
| Kansas | 16.3 (16.0–16.7) | 17.5 (17.1–18.2) | 15.1 (14.7–15.7) | 17.3 (17.0–17.7) | 17.3 (16.8–17.8) | 17.3 (16.8–17.8) |
| Kentucky | 16.1 (16.0–16.5) | 15.9 (15.6–16.2) | 16.4 (16.1–16.8) | 20.2 (19.7–20.6) | 18.9 (18.4–19.3) | 21.5 (21.0–22.1) |
| Louisiana | 18.1 (17.8–18.5) | 18.2 (17.9–18.6) | 18.0 (17.4–18.4) | 19.0 (18.7–19.3) | 20.3 (19.9–20.7) | 17.8 (17.4–18.2) |
| Maine | 17.2 (16.8–17.6) | 18.8 (18.3–19.7) | 15.5 (14.7–16.2) | 15.5 (15.2–16.1) | 16.2 (15.5–17.1) | 14.8 (14.2–15.4) |
| Maryland | 16.6 (16.3–16.9) | 18.2 (18.0–18.6) | 14.9 (14.5–15.3) | 16.4 (16.2–16.6) | 17.0 (16.7–17.4) | 15.8 (15.5–16.1) |
| Massachusetts | 14.9 (14.7–15.1) | 16.6 (16.3–16.9) | 13.2 (12.8–13.4) | 15.4 (15.0–15.6) | 17.5 (17.0–17.8) | 13.2 (13.0–13.5) |
| Michigan | 15.1 (14.9–15.3) | 15.1 (14.9–15.4) | 15.1 (14.9–15.3) | 15.5 (15.2–15.6) | 16.7 (16.5–17.0) | 14.2 (13.8–14.3) |
| Minnesota | 16.6 (16.3–16.9) | 16.7 (16.4–17.0) | 16.5 (16.1–16.9) | 12.3 (12.1–12.6) | 12.7 (12.4–13.0) | 12.0 (11.6–12.4) |
| Mississippi | 16.9 (16.6–17.2) | 18.9 (18.5–19.4) | 14.8 (14.4–15.4) | 19.8 (19.4–20.1) | 19.9 (19.5–20.4) | 19.7 (19.1–20.3) |
| Missouri | 14.5 (14.3–14.7) | 15.4 (15.1–15.7) | 13.6 (13.3–14.0) | 15.9 (15.5–16.2) | 15.0 (14.6–15.3) | 16.8 (16.5–17.2) |
| Montana | 14.3 (13.6–15.0) | 15.8 (14.8–16.7) | 12.8 (11.9–13.6) | 14.6 (14.0–15.2) | 18.1 (17.2–18.9) | 11.0 (10.2–11.7) |
| Nebraska | 14.8 (14.5–15.1) | 14.3 (13.8–14.7) | 15.3 (14.7–15.7) | 15.5 (15.1–15.8) | 17.5 (17.0–18.2) | 13.5 (12.9–14.1) |
| Nevada | 17.6 (17.3–18.0) | 16.3 (15.9–16.7) | 19.0 (18.4–19.4) | 14.8 (14.4–15.1) | 18.1 (17.6–18.6) | 11.7 (11.3–12.0) |
| New Hampshire | 16.4 (16.0–16.9) | 17.5 (16.8–18.1) | 15.2 (14.7–16.0) | 12.9 (12.6–13.4) | 13.5 (12.7–14.3) | 12.3 (11.7–12.9) |
| New Jersey | 17.5 (17.4–17.8) | 17.9 (17.6–18.1) | 17.2 (17.0–17.5) | 17.9 (17.7–18.1) | 18.9 (18.6–19.1) | 16.9 (16.7–17.2) |
| New Mexico | 15.7 (15.3–16.0) | 16.7 (16.2–17.3) | 14.7 (14.1–15.2) | 19.1 (18.7–19.4) | 24.1 (23.3–25.0) | 14.4 (13.9–15.1) |
| New York | 15.8 (15.6–15.9) | 17.2 (17.0–17.4) | 14.3 (14.2–14.5) | 19.4 (19.3–19.6) | 20.4 (20.2–20.6) | 18.5 (18.3–18.7) |
| North Carolina | 14.7 (14.5–14.9) | 14.4 (14.2–14.6) | 15.0 (14.8–15.3) | 18.6 (18.4–18.8) | 17.3 (17.0–17.5) | 20.0 (19.7–20.3) |
| North Dakota | 16.4 (15.7–17.2) | 16.4 (15.1–17.7) | 16.4 (15.5–17.6) | 13.8 (13.1–14.6) | 14.9 (13.3–15.8) | 12.6 (11.3–13.9) |
| Ohio | 15.7 (15.6–15.9) | 16.0 (15.7–16.2) | 15.5 (15.3–15.7) | 16.1 (15.9–16.3) | 14.7 (14.4–14.9) | 17.5 (17.2–17.8) |
| Oklahoma | 15.5 (15.2–15.7) | 16.1 (15.7–16.6) | 14.8 (14.4–15.2) | 18.6 (18.1–18.9) | 21.0 (20.5–21.4) | 16.3 (15.8–16.7) |
| Oregon | 16.7 (16.5–17.0) | 16.5 (16.0–17.0) | 17,0 (16.6–17.3) | 15.1 (14.8–15.4) | 17.3 (16.7–17.8) | 13.0 (12.7–13.4) |
| Pennsylvania | 15.7 (15.6–15.9) | 15.5 (15.3–15.8) | 15.9 (15.7–16.1) | 14.7 (14.6–14.8) | 14.3 (14.1–14.5) | 15.1 (14.9–15.3) |
| Rhode Island | 14.8 (14.1–15.4) | 15.1 (14.0–15.8) | 14.5 (13.7–15.4) | 16.1 (15.4–16.6) | 16.8 (15.9–17.6) | 15.3 (14.7–15.9) |
| South Carolina | 16.6 (16.4–16.9) | 15.9 (15.5–16.3) | 17.3 (17.0–17.7) | 17.8 (17.5–18.2) | 17.9 (17.4–18.3) | 17.6 (17.2–18.1) |
| South Dakota | 15.7 (15.0–16.3) | 16.4 (15.5–17.2) | 15.0 (14.0–15.7) | 15.8 (15.2–16.4) | 16.4 (15.5–17.4) | 15.3 (14.3–16.4) |
| Tennessee | 17.1 (16.9–17.3) | 19.0 (18.6–19.3) | 15.2 (14.8–15.6) | 20.4 (20.2–20.6) | 20.8 (20.4–21.2) | 20.0 (19.6–20.3) |
| Texas | 14.8 (14.7–15.0) | 15.2 (15.0–15.3) | 14.5 (14.3–14.7) | 18.8 (18.7–19.0) | 17.7 (17.5–17.8) | 20.0 (19.8–20.2) |
| Utah | 12.7 (12.4–12.9) | 11.8 (11.4–12.1) | 13.5 (13.2–14.0) | 11.0 (10.6–11.2) | 11.9 (11.4–12.2) | 10.1 (9.7–10.4) |
| Vermont | 14.4 (13.7–15.3) | 13.7 (12.9–14.7) | 15.1 (14.1–16.0) | 13.6 (12.8–14.2) | 15.0 (13.5–15.8) | 12.1 (11.2–13) |
| Virginia | 14.9 (14.7–15.2) | 14.5 (14.2–14.8) | 15.2 (14.9–15.6) | 17.0 (16.8–17.2) | 17.7 (17.4–18.0) | 16.4 (16.0–16.6) |
| Washington | 18.0 (17.8–18.2) | 20.0 (19.7–20.2) | 16.1 (15.8–16.4) | 16.2 (16.0–16.4) | 18.6 (18.1–19.0) | 13.8 (13.6–14.2) |
| West Virginia | 16.0 (15.3–16.4) | 16.4 (15.9–17.2) | 15.5 (14.6–16.0) | 17.5 (17.1–18.0) | 17.6 (16.9–18.1) | 17.5 (16.9–18.3) |
| Wisconsin | 15.3 (15.1–15.6) | 16.7 (16.2–17.1) | 13.9 (13.6–14.2) | 14.3 (14.0–14.5) | 13.8 (13.5–14.1) | 14.7 (14.4–15.0) |
| Wyoming | 14.7 (13.6–15.8) | 15.6 (14.1–17.0) | 13.8 (12.5–14.8) | 13.1 (12.3–13.9) | 14.2 (13.2–15.4) | 11.9 (11.0–12.9) |
Range of estimates generated from 50 separate model populations.
Discussion
Although BMI surveillance is critical to planning the clinical and public health response to the childhood obesity epidemic at the state level, very few states collect and publish statewide BMI census data across a range of ages. This is the first study to estimate bias-corrected state-specific childhood obesity prevalence. This study generated valid estimates of obesity prevalence within demographic strata at the national level and closely matched state-level estimates among five states that conducted a school-based census of student BMI.
The NSCH provides one of the richest state-specific sources of ongoing data regarding the health and well-being of children in the United States. However, the telephone survey can only collect self- (or parent-) reported height and weight, which have been shown to be biased estimates compared to objectively-measured data. Recognizing this bias as particularly important among younger children, the 2011–2012 NSCH does not report BMI or obesity and overweight prevalence for children younger than 10 years of age. The currently published 2011–2012 NSCH estimates of categorical obesity prevalence among children 10–17 years of age underestimate obesity prevalence in this age group compared to measured data from 2011–2012 NHANES,23 do not provide continuous height and weight data needed to estimate bias-corrected state-specific obesity prevalence, and miss critical growth periods of early childhood.
The statistical matching methods utilized in this paper offer a validated and meaningful alternative to discarding useful state-specific parent-reported height and weight from the ongoing NSCH surveys. The method also provides a flexible framework for updating estimates as new state and national data inputs become available. In addition to estimating obesity prevalence, the method also provides BMI, height, and weight for individuals, which may be useful to researchers interested in analyzing these variables in NSCH or other datasets.
Estimates in this study are important for four reasons. First, this study provides age- and gender-specific obesity prevalence estimates for states that do not currently operate statewide BMI surveillance systems. Second, although a number of states conduct statewide surveillance programs, few states conduct surveillance across the entire age range during childhood. Results from this model validated against reported BMI surveillance data can be used to supplement information from more limited surveillance systems. Third, emerging efforts to guide obesity prevention policymaking through the use of policy evaluation simulation models require state- and demographic-specific information on BMI distributions and how they vary by individual characteristics.11 The methods in the current study provide rich state-level data that can be used to project morbidity and healthcare costs. Using similar methods, we found that current estimates of state-level adult obesity using self-reported height and weight from the Behavioral Risk Factor Surveillance System (BRFSS) underestimate the prevalence of adult obesity.22 Fourth, the methods developed for this project can also be applied to other studies using parent or self-reported data among adolescents. For example, biased data on middle and high school self-reported height and weight from YRBSS could be corrected to provide more accurate obesity prevalence estimates in these populations.3–5
Limitations
Although statistical matching is a powerful method, it does require some assumptions and we do face important data limitations. The most important assumption is that variables that are not jointly observed in the matched dataset are independent conditional on the matching variables. For this study, we included state-level variation in parent-reported height and weight conditional on household income and race/ethnicity, but did not assume that county, city, or smaller geographic level variables are independent of the imputed BMI conditional on these matching variables. As such, we could not fully capture geographic variation below the state level. However, differences within states due to these compositional factors are accounted for in the analysis.
Another limitation is that the measured height and weight data are drawn from a relatively small sample of youth who participated in NHANES 2005–2010. Because the data needed to be pooled across multiple years to provide sufficient sample size, the study cannot capture shifts in BMI distribution occurring during this period. However, measured childhood obesity prevalence remained relatively stable during this period.23 In contrast, as Singh et al. have shown, parent-reported childhood obesity prevalence increased somewhat across the 2003–2004 and 2007–2008 NSCH sample waves.6 As such, pooling data across these waves in order to increase sample size within demographic strata obscures the secular changes observed in the parent-reported data. However, because NSCH data were only used to capture relative state-level variation, the estimates from this study represent more recent absolute prevalence data from 2005–2010 NHANES. The limited sample available in NHANES makes it difficult to accurately represent the tails of the BMI distribution important for estimating health effects from severe obesity.24 Most importantly, the lack of publicly-available data from the most recent 2011–2012 NSCH limits our ability to represent recent changes in state-level variation in childhood obesity prevalence.
Conclusion
This study provides the first bias-corrected state-specific estimates of childhood obesity prevalence across all ages, which we validated against objectively-measured BMI surveillance data from five states. In the absence of national state-specific surveillance systems, this method provides a critical source of local data for clinicians, public health practitioners, and policymakers. This analysis highlights the importance of releasing more recent height and weight data from the 2011–2012 NSCH so that researchers can use bias-correction techniques to provide updated estimates of state-level variation in childhood obesity prevalence. While this model provides important new information, estimating local-area changes in childhood obesity due to policy and environmental changes will require additional investment in state or federal surveillance systems.
Supplementary Material
Acknowledgments
This work was supported in part by grants from The JPB Foundation, the Robert Wood Johnson Foundation (Grant No. 66284), the Donald and Sue Pritzker Nutrition and Fitness Initiative, and the Centers for Disease Control and Prevention (Grant No. U48DP001946), including the Nutrition and Obesity Policy Research and Evaluation Network. YC Wang is partly supported by a grant from the National Cancer Institute (1R01CA172814-01A1). This work is solely the responsibility of the authors and does not represent the official views of the Centers for Disease Control and Prevention or any of the other funders.
Footnotes
Conflict of interest.
The authors declare no conflict of interest.
Supplementary information is available at IJO’s website.
References
- 1.Blondin K, Giles CM, Gortmaker SL, Cradock AL, Resch SC, Wang YC, et al. Improving state childhood obesity surveillance: A review of current practice and recommendations for change. Prev Chronic Dis (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dietz WH. Letter re PedNSS and PNSS: U.S. Centers for Disease Control and Prevention; 2011. Available from: http://www.nj.gov/health/fhs/shapingnj/news/newsletter/documents/Letter%20re%20PedNSS%20and%20PNSS.pdf. [Google Scholar]
- 3.Youth Risk Behavior Surveillance System (YRBSS): U.S. Centers for Disease Control and Prevention; 2015. [cited 2015 July 15]. Available from: http://www.cdc.gov/healthyyouth/data/yrbs/index.htm. [Google Scholar]
- 4.Gosse MA. How accurate is self-reported BMI? Nutrition Bulletin 2014;39(1):105–14. [Google Scholar]
- 5.Brener ND, McManus T, Galuska DA, Lowry R, Wechsler H. Reliability and validity of self-reported height and weight among high school students. The Journal of adolescent health : official publication of the Society for Adolescent Medicine 2003;32(4):281–7. [DOI] [PubMed] [Google Scholar]
- 6.Singh GK, Kogan MD, van Dyck PC. Changes in state-specific childhood obesity and overweight prevalence in the United States from 2003 to 2007. Archives of pediatrics & adolescent medicine 2010;164(7):598–607. [DOI] [PubMed] [Google Scholar]
- 7.Connor Gorber S, Tremblay M, Moher D, Gorber B. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obesity reviews : an official journal of the International Association for the Study of Obesity 2007;8(4):307–26. [DOI] [PubMed] [Google Scholar]
- 8.Akinbami LJ, Ogden CL. Childhood overweight prevalence in the United States: the impact of parent-reported height and weight. Obesity 2009;17(8):1574–80. [DOI] [PubMed] [Google Scholar]
- 9.Weden MM, Brownell PB, Rendall MS, Lau C, Fernandes M, Nazarov Z. Parent-reported height and weight as sources of bias in survey estimates of childhood obesity. American journal of epidemiology 2013;178(3):461–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cawley J, Burkhauser R. Beyond BMI: The Value of More Accurate Measures of Fatness and Obesity in Social Science Research. NBER Working Paper Series 2006;Working Paper 12291. [DOI] [PubMed] [Google Scholar]
- 11.Gortmaker SL, Wang YC, Long MW, Giles CM, Ward ZJ, Barrett JL, et al. Three Interventions That Reduce Childhood Obesity Are Projected To Save More Than They Cost To Implement. Health Aff (Millwood) 2015;34(11):1932–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blumberg SJ, Foster EB, Frasier AM, Satorius J, Skalland BJ, Nysse-Carris KL, et al. Design and operation of the National Survey of Children’s Health, 2007. Vital and health statistics Ser 1, Programs and collection procedures 2012(55):1–149. [PubMed] [Google Scholar]
- 13.Blumberg SJ, Olson L, Frankel MR, L. O, Srinath KP, Giambo P. Design and operation of the National Survey of Children’s Health, 2003. Vital Health Stat 2005;1(43):1–124. [PubMed] [Google Scholar]
- 14.Assessment of Childhood and Adolescent Obesity in Arkansas: Year Eleven (Fall 2013-Spring 2014). Little Rock, AR: Arkansas Center for Health Improvement, 2014. [Google Scholar]
- 15.State of Florida 2013–2014 Summary of School Health Services. Tallahassee, FL: School Health Services Program, Florida Department of Health., 2015. [Google Scholar]
- 16.Results from the Body Mass Index Screening in Massachusetts Public School Districts, 2014. Boston, MA: School Health Unit, Bureau of Community Health and Prevention, Massachusetts Department of Public Health., 2015. [Google Scholar]
- 17.Growth Screens/BMI-For-Age Percentiles by Health District and County, 2012–2013 School Year. Harrisburg, PA: Division of School Health, Bureau of Community Health Services, Pennsylvania Department of Health,, 2015. [Google Scholar]
- 18.A Summary of Weight Status Data: Tennessee Public Schools, 2012–2013 School Year. Nashville, TN: Division of Policy, Planning, and Assessment, Tennessee Department of Health., 2013. [Google Scholar]
- 19.D’Orazio M. Statistical Matching and Imputation of Survey Data with StatMatch. StatMatch R package vignette [Internet]. 2014. Available from: http://cran.r-project.org/web/packages/StatMatch/vignettes/Statistical_Matching_with_StatMatch.pdf. [Google Scholar]
- 20.D’Orazio M, Di Zio M, Scanu M. Statistical matching : theory and practice. Chichester, England; Hoboken, NJ: Wiley; 2006. x, 256 p. p. [Google Scholar]
- 21.Vantaggi B. Statistical matching of multiple sources: A look through coherence. International Journal of Approximate Reasoning 2008;49:701–11. [Google Scholar]
- 22.Ward ZJ, Long MW, Resch SC, Gortmaker SL, Cradock AL, Giles CM, et al. Redrawing the US obesity landscape: Bias-corrected estimates of state-specific adult obesity prevalence. PLoS ONE 2016;11(3):e0150735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311(8):806–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kelly AS, Barlow SE, Rao G, Inge TH, Hayman LL, Steinberger J, et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation 2013;128(15):1689–712. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


