Abstract
Purpose:
When seeking treatment for male SUI (mSUI), patients are faced with weighing complex risks and benefits in making treatment decisions within their individual context. We sought to quantify the frequency of decisional regret among this population and to determine factors associated with regret.
Materials & Methods:
A cohort of 130 males aged ≥65 seen for initial mSUI consultation at the University of California, San Francisco Medical Center and the San Francisco Veterans Affairs Medical Center between June 2015 – March 2020 was developed. Using retrospective chart review and telephone interviews, we ascertained decisional regret as well as other patient-, disease-, and treatment-related characteristics. Decisional regret was analyzed by treatment type and patient-, disease-, and treatment-related factors. Multivariable logistic regression models were built to examine the factors most associated with decisional regret.
Results:
Among the entire cohort, 22% reported moderate to severe decisional regret. Regret was highest among those electing conservative management, with 34.7% having decisional regret (vs. with surgery: 8.3% sling, 8.2% sphincter, p < 0.001). In multivariable analysis, depression, lower rating of shared decision-making, and higher current incontinence scores were significantly associated with decisional regret.
Conclusions:
Recognition of depression, improved efforts at shared decision-making, and more individualized treatment counseling have the potential to improve patient satisfaction with treatment choice. In addition, given high levels of regret among those electing conservative treatment, we may be underutilizing mSUI surgery in this population.
Keywords: male stress urinary incontinence, geriatric urology, decision-making, shared decision-making, treatment decisions
Introduction:
Rates of male stress urinary incontinence (mSUI) after prostatectomy vary, with studies showing that anywhere from 8–29% of men will have moderate to severe distress or leakage at 18–24 months depending on how incontinence is defined and assessed, though even single pad leakage can cause significant decrements in quality of life (QOL).1–3 Fortunately, treatment options do exist, including conservative measures and surgical treatment. Given that there is no imperative for treatment of mSUI other than improvement of QOL, it is especially important that patients understand the risk-benefit tradeoffs of various treatment options and how treatment fits into their goals and values.
Treatment options for mSUI vary significantly in terms of risks, benefits, and leakage-related outcomes.4 Though it is suggested as first-line therapy and has virtually no risks, pelvic floor muscle training has not shown good success in improving long-term continence rates.5 Surgery has been shown to result in near-term quality of life improvements, with 85–95% satisfaction after undergoing artificial urinary sphincter (AUS) or sling surgery.6–8 Sphincters are considered the gold standard for mSUI given the high success rates for even severe leakage, but do require manual dexterity and have higher rates of short- and long-term complications compared to slings.5 Slings allow for physiologic voiding, but have lower success rates in men with higher grade incontinence and/or prior radiation.5 Adding to the complexity of treatment decisions, data show that patients and their providers are faced with weighing these risks and benefits within the context of existing multi-morbidity, frailty and functional limitations, and limited life expectancy.9
Guidelines and studies tend to focus primarily on incontinence outcomes after treatment and less on eliciting the patient’s individual goals and values around treatment. One study that evaluated patient choice found that 25% of patients who were counseled by their urologist to choose an AUS would still choose a sling, even though this was not what was recommended or what is considered “gold standard” in their situation, with the most common rationale being the desire to avoid a mechanical device.6 Given that most patients adhere to treatment recommendations made by the urologist, it becomes essential that urologists are making tailored, individualized recommendations that take into account patient context and values.6 To move towards improved decision-making for mSUI treatment, we aimed to quantify the frequency of decisional regret among this patient population and to determine factors associated with regret.
Materials & Methods:
Participants and Data Collection
Methods have been described in detail previously and are summarized here.9 A total of 186 men age ≥65 at University of California San Francisco (UCSF) and the San Francisco Veterans Affairs Healthcare System underwent consultation for mSUI between June 2015 and March 2020 and were recruited to participate in the study. We recruited participants by phone, using electronic medical record review and a telephone survey to assess various characteristics among those who consented. Participants were provided a $20 Amazon gift certificate after completion of the interview. Institutional Review Board approval for the study was obtained at UCSF.
Measures
Our primary outcome of interest was decisional regret, as measured by the validated Decisional Regret Scale which results in a score between 0 (no regret) and 100 (high regret) and has been previously used in elderly patient populations.10–12 An established cut-point of >25 was selected a priori and used to indicate “moderate to severe regret”, while a score of ≤ 25 was used to indicate “none to minimal regret”.13,14 The Decisonal Regret Scale user manual provides detail about the questions and scoring: https://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_Regret_Scale.pdf.
Covariates included demographics as well as measures of comorbidities and functional status, mental health and cognition, incontinence and treatment data. Demographics collected included age, race, education, marital status, and health literacy; details on the collection of patient data has been previously reported in detail.9 To assess baseline and follow-up incontinence details, participants were provided with the International Consultation on Incontinence Questionnaire – Urinary Incontinence Short Form (ICIQ-UI-SF), which collects patient-reported incontinence data on frequency of leakage, amount of leakage, and leakage bother.15 An overall score is calculated from these responses which ranges from 0 (no incontinence) to 21 (significant, bothersome incontinence). Shared decision-making (SDM) was assessed during the telephone interview using the validated 9-item Shared Decision Making Questionnaire (SDM-Q-9), which rates SDM on a scale from 0 to 100 where 0 indicates lowest possible extent of SDM and 100 indicates highest extent of SDM.16
Statistical Analysis
Descriptive summary statistics are reported using mean ± standard deviation for continuous variables and count and percentages for categorical variables. Decisional regret was analyzed by treatment type using one-way analysis of variance (ANOVA). Patient-, disease-, and treatment-related factors were then analyzed by presence or absence of decisional regret using Chi-squared or Fisher’s exact test and independent group Student’s t-tests where appropriate. As per our a priori analytic plan, multivariable regression models were created to evaluate decisional regret as both a continuous and binary outcome to examine the combination of factors that are most important in identifying decisional regret, incorporating variables with a p-value of < 0.1 on univariate analysis and adjusting for pre-decision ICIQ leakage score. Additional multivariable linear regression models were constructed to evaluate factors associated with decisional regret score by treatment choice in subgroup analysis. STATA 16.1 was used for analysis with p-value of <0.05 considered significant.
Results:
130 of 186 (70%) eligible participants completed the interview and were included for analysis (mean time since initial consultation of 31.6 ± 15.8 months). (Table 1) Participants were on average 75 years of age, mostly white (87%), college-educated (76%), married (79%), and 4% had low health-literacy. Incontinence was due to surgery alone in 45% of cases and surgery in addition to radiation therapy in 53% of cases, with the vast majority related to an underlying prostate cancer diagnosis. At the time of consultation, the majority of men reported leaking a moderate (55%) or large (25%) amount of urine, with leakage occurring daily (12%), several times per day (32%), or all the time (53%). Leakage was noted to have moderate interference with daily activities, with a mean interference score of 5.7 ± 3.2 on a scale of 0 (not at all) to 10 (a great deal). The mean pre-consultation ICIQ-UI-SF score of the cohort was 14.2 ± 4.4, representing moderate leakage and interference. In terms of treatment, 53% elected conservative management, 9% underwent sling placement, and 38% underwent sphincter placement. The mean SDM score was 72.9 ± 26.1.
TABLE 1:
Characteristics of Older Men Presenting for Stress Urinary Incontinence Consultation by Decisional Regret
| All | None to minimal decisional regret (DRS ≤ 25) | Moderate to severe decisional regret (DRS > 25) | ||
|---|---|---|---|---|
| N = 130 | N = 101 | N = 29 | p-value | |
| DEMOGRAPHICS | ||||
| Age (mean ± SD) | 74.9 ± 4.6 | 75.0 (4.4) | 74.4 (5.0) | 0.509 |
| Race: White (vs. non-white) – n (%) | 113 (86.9) | 87 (86%) | 26 (89%) | 0.245 |
| Education: College grad – n (%) | 99 (76.2) | 23 (23%) | 8 (28%) | 0.592 |
| Marital status: Married/partnered – n (%) | 102 (78.5) | 82 (81%) | 20 (69%) | 0.158 |
| Health literacy (low) – n (%) | 5 (3.9) | 3 (3%) | 2 (6%) | 0.332 |
| COMORBIDITIES & FUNCTIONAL STATUS | ||||
| Charlson Comorbidity Index (mean ± SD) | 5.2 ± 2.0 | 5.2 (2.0) | 5.1 (2.2) | 0.676 |
| 10-year mortality risk1 > 50% – n (%) | 93 (71.5) | 74 (73%) | 19 (65%) | 0.415 |
| Functional status: help with 1+ ADL – n (%) | 13 (10.0) | 9 (9%) | 4 (14%) | 0.440 |
| TUG score2 in seconds (mean ± SD) | 9.6 ± 2.4 | 9.1 (2.3) | 10.0 (2.9) | 0.274 |
| Prefrail/Frail: TUG2 > 10 seconds – n (%) | 29 (22.3) | 20 (26%) | 9 (36%) | 0.316 |
| Upper extremity function score3 (mean ± SD) | 52.9 ± 3.6 | 52.8 (3.8) | 53.3 (2.7) | 0.519 |
| Physical QOL4 (mean ± SD) | 51. 3 ± 9.1 | 52.0 (8.8) | 48.9 (9.8) | 0.099 |
| MENTAL HEALTH & COGNITION | ||||
| Anxiety5 – n (%) | 5 (3.9) | 3 (3%) | 2 (7%) | 0.332 |
| Depression6 – n (%) | 13 (10.0) | 6 (6%) | 7 (24%) | 0.004 |
| Cognitive impairment7 – n (%) | 0 | 0 (0%) | 0 (0%) | 1.000 |
| Mental QOL4 (mean ± SD) | 55.6 ± 8.4 | 56.8 (8.1) | 52.3 (8.7) | 0.015 |
| INCONTINENCE CHARACTERISTICS | ||||
| Etiology | ||||
| H/o surgery only – n (%) | 58 (44.6) | 83 (82%) | 26 (90%) | 0.335 |
| H/o surgery + XRT – n (%) | 69 (53.1) | 57 (56%) | 14 (48%) | 0.437 |
| Other etiology – n (%) | 3 (2.3) | 1 (1%) | 0 (0%) | 0.591 |
| Prior radiation – n (%) | 71 (54.6) | 57 (56%) | 14 (48%) | 0.437 |
| Prior hormone therapy – n (%) | 30 (23.1) | 25 (25%) | 5 (17%) | 0.397 |
| Amount of leakage – n (%) | 0.527 | |||
| Small amount | 25 (19.2) | 18 (18.0) | 7 (24.1) | |
| Moderate amount | 72 (55.4) | 55 (55.0) | 17 (58.6) | |
| Large amount | 32 (24.6) | 27 (27.0) | 5 (17.1) | |
| Frequency of leakage – n (%) | 0.621 | |||
| 2–3 times per week | 3 (2.3) | 3 (3.0) | 0 (0.0) | |
| Daily | 15 (11.5) | 10 (10.0) | 5 (17.2) | |
| Several times a day | 42 (32.3) | 31 (31.0) | 11 (37.9) | |
| All the time | 69 (53.1) | 56 (56.0) | 13 (44.8) | |
| Leakage interference, 0–10 (mean ± SD) | 5.7 ± 3.2 | 5.8 ±3.2 | 5.3 ± 3.2 | 0.117 |
| Pre-decision leakage ICIQ score8 (mean ± SD) | 14.2 ± 4.4 | 14.4 (4.5) | 13.4 (4.3) | 0.324 |
| Urgency symptoms at presentation – n (%) | 29 (22.3) | 23 (25%) | 6 (21%) | 0.720 |
| TREATMENT CHARACTERISTICS | ||||
| Treatment type | 0.001 | |||
| Conservative (no surgery) – n (%) | 69 (53) | 45 (44%) | 24 (83%) | |
| Sling – n (%) | 12 (9) | 11 (11%) | 1 (3%) | |
| Sphincter – n (%) | 49 (38) | 45 (45%) | 4 (14%) | |
| Shared decision-making score (mean (SD)) | 72.9 (26.1) | 77.4 (4.7) | 56.9 (4.5) | 0.002 |
| Any complication – n (%) | 17 (28) | 15 (27%) | 2 (40%) | 0.528 |
| Post-decision leakage ICIQ score8 (mean (SD)) | 8.90 (5.1) | 7.80 (4.7) | 13.10 (4.5) | <0.001 |
| Time since consultation, in months (mean (SD)) | 31.6 (1.4) | 31.8 (1.5) | 30.6 (3.3) | 0.710 |
| Time since surgery, in months (mean (SD)), where relevant | 28.6 (2.0) | 28.8 (2.1) | 26.3 (6.8) | 0.740 |
10-year mortality determined by the Lee Index
TUG – Timed Up and Go Test. TUG score of > 10 seconds indicates prefrail or frail.
Upper extremity function determined by Neuro-QOL Short Form v1.0 - Upper Extremity Function: Fine Motor ADL. Raw scores are transformed into a standardized T-score where 50 represents the mean of the reference population with a standard deviation of 10.
Physical and mental QOL determined by PROMIS Scale v1.2 - Global Health. Raw scores are transformed into a standardized T-score where 50 represents the mean of the reference population with a standard deviation of 10.
Anxiety determined by Generalized Anxiety Disorder 2-item scale (GAD-2)
Depression determined by Patient Health Questionnaire 2-item scale (PHQ-2)
Cognitive impairment determined by Short Portable Mental Status Questionnaire (SPMSQ)
Incontinence score determined by International Consultation on Incontinence Questionnaire – Urinary Incontinence Short Form. Score ranges from 0 (no incontinence) to 21 (significant, bothersome incontinence).
Among the entire cohort, the mean decisional regret score was 14.0 ± 23.1, with 22% having moderate or high regret. (Table 1). Regret scores were highest among those who elected conservative management (19.5 ± 23.4) compared to those who underwent sling (10.0 ± 28.5) and sphincter (7.3 ± 19.4) surgery, with 34.7% of those conservatively managed having moderate to severe decisional regret (vs. 8.3% sling and 8.2% sphincter, p < 0.001).(Figure 1) Those with decisional regret were significantly more likely to report depression (24% vs. 6%, p < 0.004) and have lower mental QOL scores (mean 52.3 vs. 56.8, p = 0.015) compared to those with none to minimal regret. Decisional regret strongly correlated with SDM scores, as those with decisional regret had a mean SDM score of 56.9 vs. 77.4 in those without regret (p = 0.002). Finally, current leakage scores were also significantly associated with decisional regret, with a mean score of 13.1 in those with regret vs. 7.8 in those with none to minimal regret (p < 0.001).
Figure 1: Distribution of Decisional Regret Score by Treatment Choice.
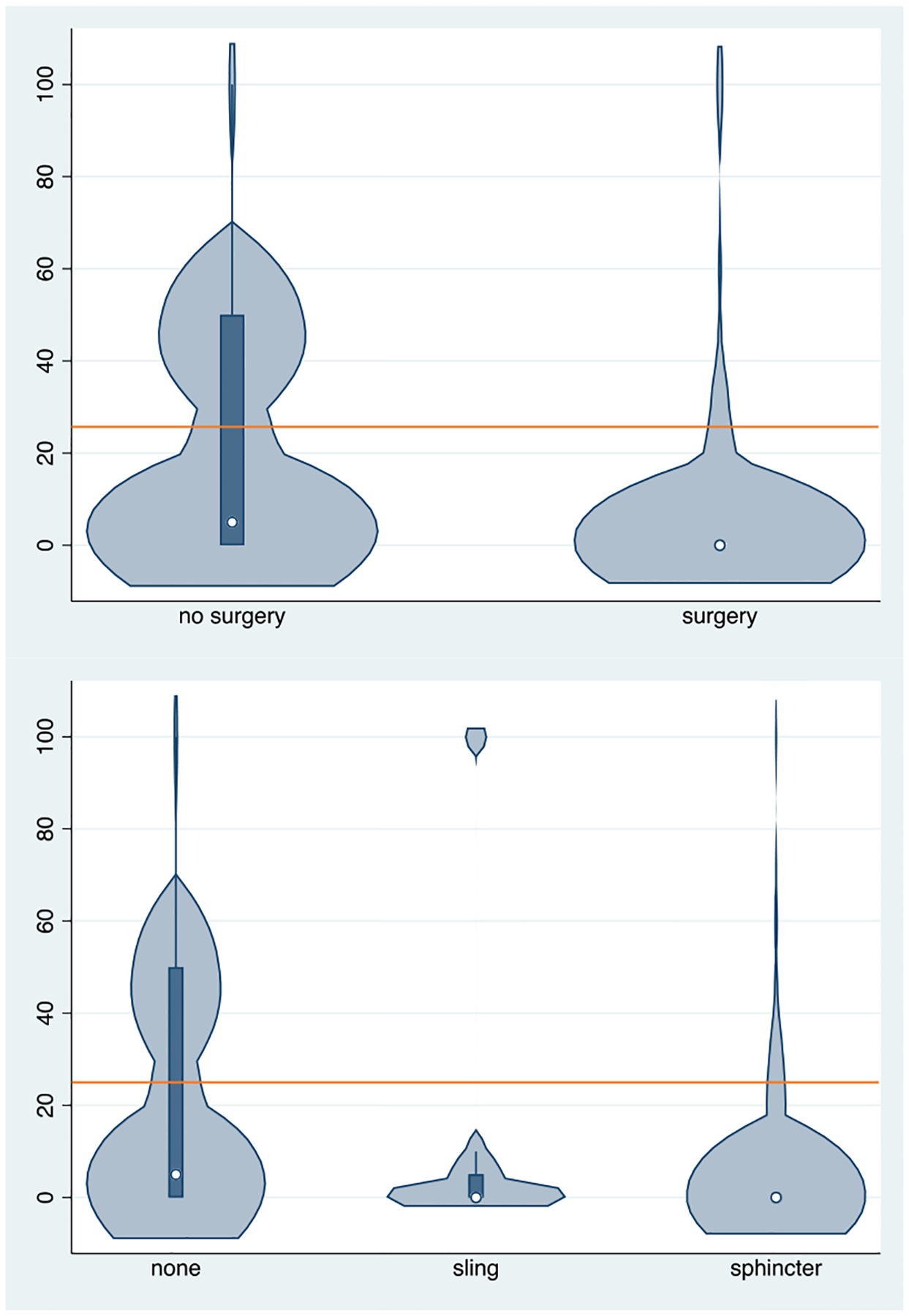
Decisional Regret Score 0 – 100; orange line indicates a cut-point of 25.
≤ 25 = none to minimal regret, > 25 = moderate to severe regret
In multivariable analyses of decisional regret both as a binary and a continuous outcome, depression (p-value 0.026 and 0.004, respectively), SDM (p-value 0.017 and 0.002), and current leakage score (p-value 0.001 and < 0.001) were noted to be significant drivers of regret in both analyses.(Table 2) The inclusion of additional covariates that were not significantly associated with decisional regret on univariate analysis were added to the models sequentially and were not significant predictors and did not change the significance of depression, SDM, or current leakage score.
TABLE 2:
Multivariable Decisional Regret Score (DRS) Analysis
| DRS as a binary outcome | DRS as a continuous outcome | |||
|---|---|---|---|---|
| Covariates included in model | p-value | OR, 95% CI | p-value | β, 95% CI |
| Physical QOL1 | 0.152 | 1.07 (0.97,1.165) | 0.355 | 0.24 (−0.27, 0.75) |
| Depression2 | 0.026 | 14.82 (1.38, 158.99) | 0.004 | 14.12 (0.77, 27.47) |
| Mental QOL1 | 0.213 | 0.094 (0.86, 1.04) | 0.385 | −0.25 (−0.82, 0.32) |
| Pre-decision leakage ICIQ score3 | 0.028 | 0.79 (0.65,0.98) | 0.324 | −0.555 (−1.595, 0.486) |
| Treatment type | 0.116 | 0.351 | ||
| Conservative (no surgery) | Ref | Ref | ||
| Sling | 2.18 (0.14, 3.87) | 6.553 (−8.057, 21.162) | ||
| Sphincter | 0.79 (0.15, 4.27) | 0.347 (−9.805, 10.501) | ||
| Shared decision-making score | 0.017 | 0.97 (0.96, 0.99) | 0.002 | −0.183 (−0.327, −0.039) |
| Post-decision leakage ICIQ score3 | 0.001 | 1.32 (1.13, 1.61) | <0.001 | 1.806 (0.974, 2.638) |
Physical and mental QOL determined by PROMIS Scale v1.2 - Global Health. Raw scores are transformed into a standardized T-score where 50 represents the mean of the reference population with a standard deviation of 10.
Depression determined by Patient Health Questionnaire 2-item scale (PHQ-2)
Incontinence score determined by International Consultation on Incontinence Questionnaire – Urinary Incontinence Short Form. Score ranges from 0 (no incontinence) to 21 (significant, bothersome incontinence).
Additional multivariable linear regression models were constructed to understand factors associated with decisional regret scores by treatment.(Supplementary Table 1) For those electing conservative management, increased leakage scores correlated with higher levels of regret (β 2.35; 95% CI 0.75,4.0). Leakage scores were also found to be significantly associated with decisional regret for those undergoing surgery, though less impactful in the surgery group than in the conservatively treated group (β 1.58; 95% CI 0.54,2.62). In addition within the surgery group, higher SDM scores correlated with lower regret scores (β −0.34, 95% CI −0.57,−0.10). When analyzing sling and sphincter surgeries, the sling group (n = 12) was too small to create valid models. Within the sphincter group, higher SDM scores (β −0.28; 95%CI −0.51,−0.06) and health literacy (β −24.80; 95% CI −46.52, −3.09) were noted to be independent predictors of lower regret.
Discussion:
To our knowledge this is the first study that has evaluated decisional regret amongst this patient population. Our data show that one-fifth of older men who have made mSUI treatment decisions report moderate to high levels of decisional regret. In particular, regret scores are highest among those who elected conservative management, with 35% of men electing conservative management having moderate to severe regret. In addition, incontinence scores, depression, and SDM were found to be significant independent predictors of regret. These data suggest that we need to better understand what is important to patients in making these treatment decisions and incorporate these aspects into treatment counseling to make treatment decisions more individualized and values-directed.
Our data showed that incontinence score remained an important independent predictor of regret when stratified by treatment type, wherein the coefficient for incontinence scores was greatest among those who elected conservative management, corresponding to the relatively high level of regret seen among those men. These data suggest that patients who do not elect to have surgery are the most dissatisfied, and this may result from a lack of patients’ clarity of their own goals, or providers’ lack of understanding of what is important to patients. It was surprising to us to find that among our cohort there were quite a few men who were counseled about mSUI treatment but had deferred surgery. We are undertaking qualitative interviews to ascertain why these individuals elected not to undergo surgery and what drives their treatment decisions, given that these patients seem to have the most regret.
These findings suggest that mSUI surgery may be underutilized in older men, which is echoed by existing data; despite the known QOL improvements that mSUI surgery offers, only 3–6% of men treated with prostatectomy undergo mSUI surgery.17–20 This discrepancy could be due to patients themselves not seeking treatment; in one study of older community-dwelling adults with urinary incontinence, only 38% had told their physician about their incontinence.21 Alternatively, one could hypothesize that patients may be reluctant to tell the urologist who performed their prostatectomy about their incontinence or may be concerned about having to undergo another surgery when the last surgery caused their issue to begin with. Thus, we need better ways to encourage patients to share their concerns with urologists and for urologists to better assess mSUI and counsel patients about treatment options.
We also found that higher SDM scores were a significant independent predictor of less decisional regret, in particular among those electing surgery. SDM is at the crux of patient-centered care and requires understanding the best available evidence around risks and benefits across all available treatment options, while ensuring patients’ values and preferences are taken into account. SDM is increasingly advocated for, both as an ethical imperative, and because there is robust evidence that SDM may actually improve health outcomes.22,23 In fact, mSUI treatment guidelines do recognize the complexity of this decision-making and advocate “using the shared decision-making model” to discuss treatment options, yet provide no guidance on how to do this in practice.24 A recent look at SDM in urologic practice was carried out using the 2019 American Urologic Association Census Shared Decision-Making module.25 Of 2,219 respondents, 77% reported regular use of SDM in at least one preference sensitive scenario. SDM can be buoyed by decision support tools, which have been shown in rigorous research to improve patients’ knowledge and accuracy of risk perceptions, increase the likelihood of patients making care choices that are congruent with their values, decrease decisional conflict, have a positive effect on patient-clinician communication, and improve satisfaction with decisions and the decision-making process.26 While there are many models for decisional support tools, one does not yet exist for mSUI.
Importantly, in our cohort depression was also noted to be strongly independently correlated with decisional regret, and 24% of those with regret screened positive for depression. Depression among older adults is estimated at 3–15%, and urinary incontinence is also known to be associated with depression.27–30 Given the high prevalence of depression amongst this patient population, as well as its correlation with decisional regret, this is an important factor to take into account. Addressing patients’ mental wellness could potentially improve their participation in making a treatment choice that is aligned with their goals and/or improve satisfaction with treatment. However, how and whether to do this in practice is challenging given concerns about how receptive patients will be to such screening and what to do with a positive result.
Our study does have limitations. Overall this represents a cohort that is mostly white and college-educated with high health literacy, which means that our results may be less generalizable. In addition, some of the data was collected through a telephone survey after the patient’s initial consultation, which relies on recollection by the patient and is therefore subject to recall bias (for example, reporting the amount and bother of incontinence at the time of consultation). However, we did see significant improvement in pre- to post-incontinence scores among those individuals who received treatment compared to no significant improvement in those who did not undergo surgery, which decreases our concern about recollection bias. Of note, participants were provided a small monetary incentive to participate, though several individuals declined the incentive after completing the study and asked that the funds be used to support more mSUI research instead. Despite these limitations, it is the first study to comprehensively evaluate decisional regret among men making mSUI treatment choices, and in particular allows comparisons between those pursuing conservative treatment versus surgery and uses a validated metric of decisional regret. We believe these data offer valuable insights into what factors play a role in treatment regret and how we might focus our efforts towards improving treatment counseling in the future.
Conclusion:
One-fifth of men with mSUI report decisional regret regarding their initial incontinence management decision. Depression and higher incontinence scores are associated with more regret, while SDM is associated with less. Recognition of depression, improved efforts at SDM, and individualized treatment counseling have the potential to improve patient satisfaction with treatment choice. In addition, given high level of regret among those electing conservative treatment, we may be underutilizing surgery in this population.
Supplementary Material
Funding:
National Institute of Aging GEMSSTAR 1R03AG064372-01 (PI: Hampson)
Doris Duke Charitable Foundation CTSI – UL1 TR001872 (PI: Hampson)
Claude D. Pepper Older Americans Independence Center UCSF Research Education Component Scholar Award (PI: Hampson)
San Francisco Veterans Affairs Medical Center (Hampson, Suskind, Cooperberg, Sudore, Keyhani, Walter)
REFERENCES
- 1.Stanford JL, Feng Z, Hamilton AS, et al. Urinary and sexual function after radical prostatectomy for clinically localized prostate cancer: the Prostate Cancer Outcomes Study. JAMA. 2000;283(3):354–360. doi:doi: 10.1001/jama.283.3.354 [DOI] [PubMed] [Google Scholar]
- 2.Steineck Gunnar, Helgesen Fred, Adolfsson Jan, et al. Quality of life after radical prostatectomy or watchful waiting. N Engl J Med. 2002;347(11):790–796. doi: 10.1056/NEJMoa021483 [DOI] [PubMed] [Google Scholar]
- 3.Cooperberg Matthew R, Master Viraj A, Carroll Peter R. Health related quality of life significance of single pad urinary incontinence following radical prostatectomy. The Journal of Urology. 2003;170(2 Pt 1):512–515. doi: 10.1097/01.ju.0000074941.27370.c4 [DOI] [PubMed] [Google Scholar]
- 4.Alwaal A, Harris CR, Awad MA, Allen IE, Breyer BN. Comparison of complication rates related to male urethral slings and artificial urinary sphincters for urinary incontinence: national multi-institutional analysis of ACS-NSQIP database. Int Urol Nephrol. 2016;48(10):1571–1576. doi: 10.1007/s11255-016-1347-3 [DOI] [PubMed] [Google Scholar]
- 5.Radadia KD, Farber NJ, Shinder B, Polotti CF, Milas LJ, Tunuguntla HSGR. Management of Postradical Prostatectomy Urinary Incontinence: A Review. Urology. 2018;113:13–19. doi: 10.1016/j.urology.2017.09.025 [DOI] [PubMed] [Google Scholar]
- 6.Kumar Angelish, Litt Elana Rosenberg, Ballert Katie N, Nitti Victor W. Artificial urinary sphincter versus male sling for post-prostatectomy incontinence--what do patients choose? The Journal of urology. 2009;181(3):1231–1235. doi: 10.1016/j.juro.2008.11.022 [DOI] [PubMed] [Google Scholar]
- 7.Rehder Peter, Gozzi Christian. Transobturator sling suspension for male urinary incontinence including post-radical prostatectomy. uropean urology. 2007;52(3):860–866. doi: 10.1016/j.eururo.2007.01.110 [DOI] [PubMed] [Google Scholar]
- 8.Gozzi Chrisitan, Becker Armin J, Bauer Ricarda, Bastian Patrick J. Early results of transobturator sling suspension for male urinary incontinence following radical prostatectomy. Eur Urol. 2008;54(4):960–961. doi: 10.1016/j.eururo.2008.04.096 [DOI] [PubMed] [Google Scholar]
- 9.Hampson LA, Suskind AM, Breyer BN, et al. Understanding the Health Characteristics and Treatment Choices of Older Men with Stress Urinary Incontinence. Urology. Published online May 15, 2021. doi: 10.1016/j.urology.2021.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brehaut JC, O’Connor AM, Wood TJ, et al. Validation of a Decision Regret Scale. Med Decis Making. 2003;23(4):281–292. doi: 10.1177/0272989X03256005 [DOI] [PubMed] [Google Scholar]
- 11.Tan EGF, Teo I, Finkelstein EA, Meng CC. Determinants of regret in elderly dialysis patients. Nephrology. 2019;24(6):622–629. doi: 10.1111/nep.13400 [DOI] [PubMed] [Google Scholar]
- 12.Albkri A, Girier D, Mestre A, Costa P, Droupy S, Chevrot A. Urinary Incontinence, Patient Satisfaction, and Decisional Regret after Prostate Cancer Treatment: A French National Study. UIN. 2018;100(1):50–56. doi: 10.1159/000484616 [DOI] [PubMed] [Google Scholar]
- 13.Szymanski KM, Whittam B, Kaefer M, et al. Parental decisional regret and views about optimal timing of female genital restoration surgery in congenital adrenal hyperplasia. Journal of Pediatric Urology. 2018;14(2):156.e1–156.e7. doi: 10.1016/j.jpurol.2017.11.012 [DOI] [PubMed] [Google Scholar]
- 14.Fowler NR, Shaaban CE, Torke AM, Lane KA, Saba S, Barnato AE. “I’m Not Sure We Had A Choice”: Decision Quality and The Use of Cardiac Implantable Electronic Devices In Older Adults With Cognitive Impairment. Cardiology and cardiovascular medicine. 2018;2(1):10–26. doi:DOI: 10.26502/fccm.92920032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. 2004;23(4):322–330. doi: 10.1002/nau.20041 [DOI] [PubMed] [Google Scholar]
- 16.Kriston Levente, Scholl Isabelle, Hölzel Lars, Simon Daniela, Loh Andreas, Härter Martin. The 9-item Shared Decision Making Questionnaire (SDM-Q-9). Development and psychometric properties in a primary care sample. Patient Educ Couns. 2010;80(1):94–99. doi: 10.1016/j.pec.2009.09.034 [DOI] [PubMed] [Google Scholar]
- 17.Kim Philip H, Pinheiro Laura C, Atoria Coral L, Eastham James A, Sandhu Jaspreet S, Elkin Elena B. Trends in the use of incontinence procedures after radical prostatectomy: a population based analysis. J Urol. 2013;189(2):602–608. doi: 10.1016/j.juro.2012.08.246 [DOI] [PubMed] [Google Scholar]
- 18.Nelson Marc, Dornbier Ryan, Kirshenbaum Eric, et al. Use of Surgery for Post-Prostatectomy Incontinence. J Urol. 2020;203(4):786–791. doi: 10.1097/JU.0000000000000618 [DOI] [PubMed] [Google Scholar]
- 19.Gupta Shubham, Ding Laura, Granieri Michael, Le Ngoc-Bich, Peterson Andrew C. Utilization of surgical procedures and racial disparity in the treatment of urinary incontinence after prostatectomy. Neurourol Urodyn. 2016;35(6):733–737. doi: 10.1002/nau.22790 [DOI] [PubMed] [Google Scholar]
- 20.Berge Viktor, Thompson Trevor, Blackman Donald. Additional surgical intervention after radical prostatectomy, radiation therapy, androgen-deprivation therapy, or watchful waiting. Eur Urol. 2007;52(4):1036–1043. doi: 10.1016/j.eururo.2006.12.012 [DOI] [PubMed] [Google Scholar]
- 21.Burgio KL, Ives DG, Locher JL, Arena VC, Kuller LH. Treatment seeking for urinary incontinence in older adults. J Am Geriatr Soc. 1994;42(2):208–212. doi: 10.1111/j.1532-5415.1994.tb04954.x [DOI] [PubMed] [Google Scholar]
- 22.Légaré France, Adekpedjou Rhéda, Stacey Dawn, et al. Interventions for increasing the use of shared decision making by healthcare professionals. Cochrane Database Syst Rev. 2018;7(7):CD006732. doi: 10.1002/14651858.CD006732.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kaplan SH, Greenfield S, Ware JE Jr. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27(3 Suppl):S110–27. doi: 10.1097/00005650-198903001-00010 [DOI] [PubMed] [Google Scholar]
- 24.Sandhu Jaspreet S, Breyer Benjamin, Comiter Craig, et al. Incontinence after Prostate Treatment: AUA/SUFU Guideline. J Urol. 2019;202(2):369–378. doi: 10.1097/JU.0000000000000314 [DOI] [PubMed] [Google Scholar]
- 25.Lane Giulia Ippolito, Ellimoottil Chad, Wallner Lauren, Meeks William, Mbassa Rachel, Clemens James Quentin. Shared Decision-making in Urologic Practice: Results From the 2019 AUA Census. Urology. 2020;145:66–72. doi: 10.1016/j.urology.2020.06.078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stacey Dawn, Légaré France, Lewis Krystina, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4(4):CD001431. doi: 10.1002/14651858.CD001431.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Volkert Jana, Schulz Holger, Härter Martin, Wlodarczyk Olga, Andreas Sylke. The prevalence of mental disorders in older people in Western countries - a meta-analysis. Ageing Res Rev. 2013;12(1):339–353. doi: 10.1016/j.arr.2012.09.004 [DOI] [PubMed] [Google Scholar]
- 28.Thomas Alan J, O’Brien John T.. Mood disorders in the elderly. Psychiatry. 2009;8(2):56–60. [Google Scholar]
- 29.Blazer Dan G. Depression in late life: review and commentary. The Journals of Gerontology. 2003;58(3):249–265. doi: 10.1093/gerona/58.3.m249 [DOI] [PubMed] [Google Scholar]
- 30.Cheng Shulin, Lin Dong, Hu Tinghui, et al. Association of urinary incontinence and depression or anxiety: a meta-analysis. J Int Med Res. 2020;48(6):300060520931348. doi: 10.1177/0300060520931348 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


