Abstract
Objective:
To investigate the amount and pattern of changes of maxillary front teeth 7 years postretention, which previously were retained with a bonded retainer.
Materials and Methods:
The study group consisted of 27 patients. Study models before treatment (T1), at debonding (T2), 1 year after removal of the upper bonded retainer (T3), and 7 years postretention (T4) were present. The irregularity index (sum of contact point displacements) and the rotations of front teeth toward the raphe line were calculated.
Results:
The irregularity index of the maxillary front teeth changes very little or not at all during the first year postretention. Further change long term resulted in an irregularity index of mean 2.0 (range 0.0–5.8). The contact relationship between the laterals and centrals seems to be the most critical. Forty rotated teeth in 21 patients were corrected more than 20°. Mean relapse during the first year postretention was 6.7° (range 0.0°–14.7°). Mean changes during 7 years was 8.2° (range 0.0°–19.3°).
Conclusions:
Relapse of upper front teeth retained with a bonded retainer is minor in both the short and long term. If permanent retention is required after 3 years of retention, it is enough to retain the incisors.
Keywords: Retention, Rotation, Relapse, Irregularity, Long-term
INTRODUCTION
From an esthetic standpoint, alignment of the anterior teeth is of considerable importance as most patients focus on the alignment of incisors and canines.1,2 The problems of lower front stability after treatment has been discussed in several studies3–6 and some information can also be found regarding the severity of maxillary irregularity long term postretention.6–9 In most of these studies a maxillary Hawley retainer has been used for upper retention, but there are no long-term postretention studies after use of bonded upper retainers.
The present study is a follow-up of a previous article where the relapse tendency of the maxillary front, 1 year after removal of upper bonded retainers was reported.10 Minor or no relapse was found. What we do not know is if the short-term stable cases change in the long term, or if slightly displaced contact points or partly relapsed rotations 1 year postretention deteriorate with time. The long-term pattern of relapse concerning rotations and contact point displacements (CPDs) for canines, laterals, and centrals is unknown.
The objectives of this study therefore are to:
Study the amount of changes in alignment of the upper front teeth long-term after retention with a bonded retainer.
Study the relapse pattern of corrected rotations.
Investigate the pattern of change of contact point displacements due to rotations and labiolingual movements.
Examine the effect of overcorrected contact points.
MATERIALS AND METHODS
The 45 patients described in a previous study10 were invited to participate in the follow-up study. In spite of several attempts to contact the patients, only 27 agreed to participate. The reason for this was mainly that they lived far away from the clinic, and in some cases there was a lack of interest to participate in the follow-up.
The present group of 27 patients is, considering treatment and duration of retention, similar to the former group of 45. Mean irregularity index at T1 (pretreatment), T2 (posttreatment), and T3 (1 year postretention) was also of the same magnitude. The mean age of patients was 25.3 years (range 21.7–30.4 years); there were 10 male and 17 female patients.
The patients in the present study, including 19 treated with extraction and eight with nonextraction, who had initial upper front irregularity had been treated with fixed edgewise appliances at the County Orthodontic Clinic in Mariestad, Sweden. Their maxillary arches were retained with bonded retainers only. The mean duration of the retention period was 34.3 months (range 25–48 months).
Study models were collected at mean 7.6 years (range 6.7–10.9 years) out of retention (T4). Models from (T1), (T2), and (T3) were available. The method of retention with a bonded wire has been previously described.11
Labiolingual CPDs of the five contacts between the mesial of the upper right canine and the mesial of the upper left canine were measured with a digital caliper with 0.1 mm accuracy. CPDs less than 0.5 mm were noted as 0 mm. The sum of the five CPDs on each model (irregularity index) was calculated according to Little.12 All models were scanned and measured as described in the 1-year follow-up.10 Intercanine distance and rotations of the upper front teeth in relation to the raphe line were measured with a modified computer program (Scion Image) (Figure 1).
Figure 1.
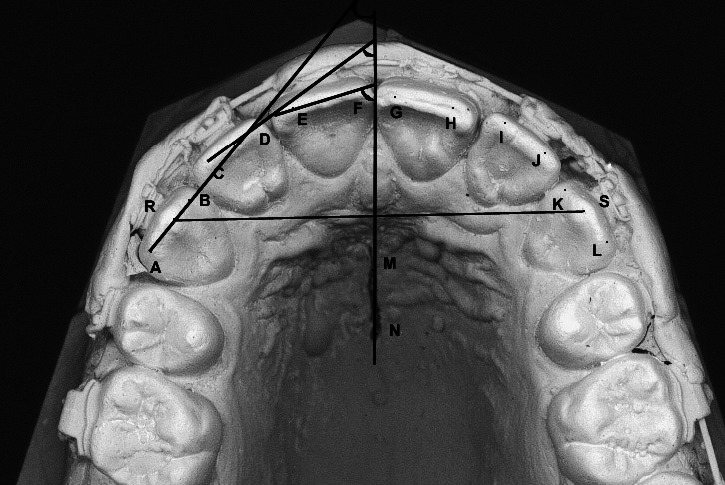
Teeth angles on the right side to the raphe line and intercanine distance.
Measurement Error
The measurement error was calculated from double measurements of 27 models (T4), using Dahlberg's formula.13 The error for CPD measurements was 0.2 mm.
The measurement errors for rotation were 3.1° for canines, 2.8° for laterals, and 2.4° for centrals.
Statistical Analysis
Pearson's product-moment correlation coefficients were calculated to test for associations between irregularity index at T1/T3, T1/T4, and T3/T4. The same analysis was also used to test for correlations between correction of rotations/relapse of rotations and the change in mean CPD T2/T4 for the canine/lateral contact, the lateral/central contact, and the central/central contact.
RESULTS
Contact Point Discrepancies
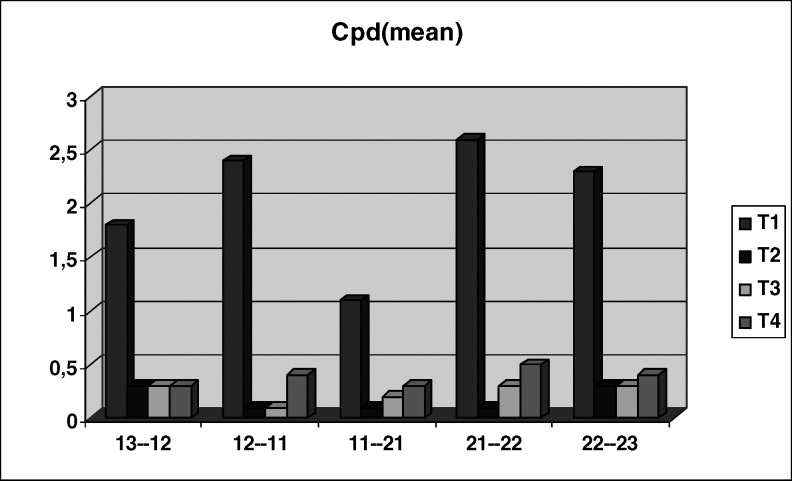
CPDs (mean) for each of the five contact points in the maxillary front are presented in Figure 2. There was no statistically significant difference between the change in mean CPD for the contacts canines/laterals, laterals/centrals, or centrals/centrals. The irregularity index of the upper front teeth is seen in Table 1. No correlations were found between the pretreatment and postretention irregularity T1/T3 and T1/T4. There was a significant association between the irregularity index at T3 and T4 (R = 0.938, P < .0001).
Figure 2.
Contact point displacement (CPD) before treatment (T1), after treatment (T2), 1 year postretention (T3), and 7 years postretention (T4).
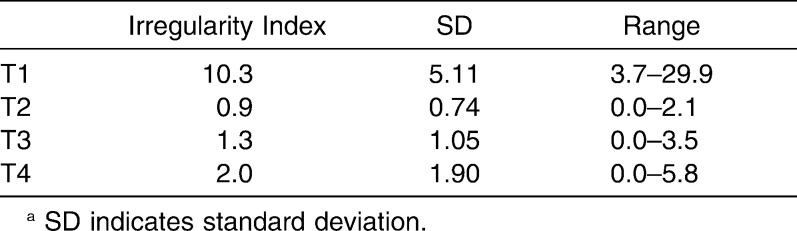
Table 1.
Mean Irregularity Index T1, T2, T3, T4 (n = 27)a
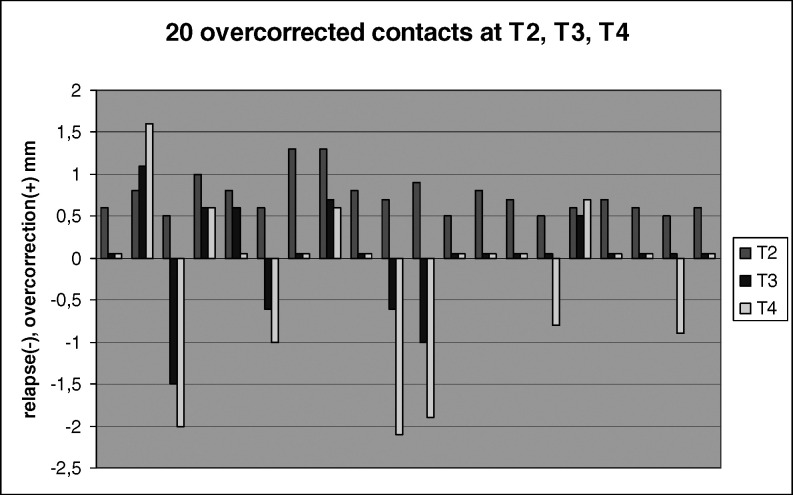
Most of the posttreatment irregularity of 0.9 (T2) was because of overcorrections. When overcorrections were excluded, the mean irregularity index was 0.4. Twenty overcorrected contacts were noted. Of the 20 overcorrected CPDs, 10 showed perfect contacts at T4 and four were to some degree still overcorrected. Six contacts had relapsed 0.8–2.1 mm (Figure 3).
Figure 3.
Twenty overcorrections at T2, T3, and T4.
Rotations
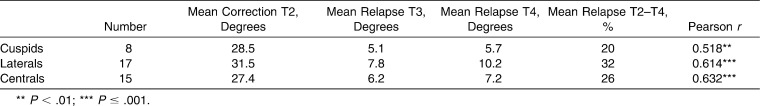
A total of 40 rotated teeth in 21 patients were corrected more than 20° during treatment (range 20.3°–51.9°). Mean relapse during the first year postretention (T2–T3) was 6.7° (range 0.0°–14.7°). Seven years postretention (T2–T4) the mean relapse was 8.2° (range 0.0°–19.3°). Mean for the different tooth groups are seen in Table 2. Most of the changes were seen at 1 year postretention (T3). Positive correlation between rotational correction in treatment and long-term relapse was significant for centrals (P = .0004), laterals (P = .0007), and canines (P = .0056).
Table 2.
Teeth Derotated More Than 20.0° (n = 40)
Circumferential supracrestal fiberotomy was performed on seven incisors in four patients (initially corrected mean 34°). Mean rotational relapse (T2–T4) in this group was 9.1° (range 1.2°–17.6°).
Intercanine Distance
During treatment the upper intercanine distance increased 1.5 mm or more in nine patients (range 1.5–6.4 mm). Five of these showed relapse of 1 mm or more at T4 (range 1.1–2.3). Among the patients, without increased intercanine distance during treatment, three showed a decreased intercanine distance of 1.5–2.3 mm. In these cases, there was a tendency for small changes during both the first year postretention and long term, but no obvious influence on the irregularity.
DISCUSSION
This study shows that the irregularity index of the maxillary front teeth changes very little or not at all during the first year postretention. Further change long term resulted in an irregularity index of less than 3 for 70% of the patients. A weakness in our material is the relatively small number of patients (n = 27) with records 1 year postretention and long-term postretention. The 27 patients we could examine long term were in all aspects similar to the larger group10 (initial irregularity, treatment, duration of retention). A strength with this study is that the original 45 patients reported in the 1-year study10 were selected at the appointment when the retainer was removed. Other studies7–9,14–17 are based on retrospective materials selected from larger collections. All our patients had the same method of retention, ie, upper bonded retainer, and we can specify the length of the retention period and the postretention period. These variables have a wider range in many studies or are not reported at all.6–8,14–17
Difficulty in locating the raphe line on all four casts, variation of quality of plaster casts, and changes in arch form causing relatively large measurement errors have been discussed in the previous paper.10 Although using implants as fixed reference points is the most stable way to measure rotations, the raphe line is a useful and relatively easy tool to find reference to measure rotations of upper front teeth.
Most of the patients who showed minor irregularity 1 year postretention were more irregular at long-term follow-up resulting in that 14% of the contacts were displaced more than 1 mm, maximum 2.2 mm. There was a strong correlation between irregularity 1 year postretention and long-term, but we could not confirm the finding of Surbeck et al.14 that pretreatment irregularity is a significant risk factor for postretention relapse. However, half of the group of 27 patients did not change at all and they were stable during the whole postretention period.
Concerning corrected rotations, almost all relapse was seen 1 year postretention with very small further changes long term. The laterals showed more rotational mean relapse than centrals and canines, and of the 12 rotations that relapsed more than 10°, eight were laterals. Some of the severely corrected rotations were perfectly stable at T4 as can be seen from the range of relapse, 0.0°–19.3°. Our data confirm the findings of Surbeck et al.14 that the majority of rotational relapse of the maxillary incisors is approximately 10°. Half of the overcorrected contacts were nicely aligned at T4. The overcorrections that started to relapse 1 year postretention, deteriorated in the long term.
The irregularity index is not always reflecting the esthetic impression of the teeth; evenly distributed small CPDs are obviously better than one or two major displaced contacts with the lateral/central contact often being the most critical (Figures 4 and 5). Our experience is that rotations of about 10° are not visible. A relapse in the range of 15° to 20° can be detected at close examination. Of the 40 severe rotations in this study, 15% relapsed within that range (15.6°–19.3°; Figure 6).
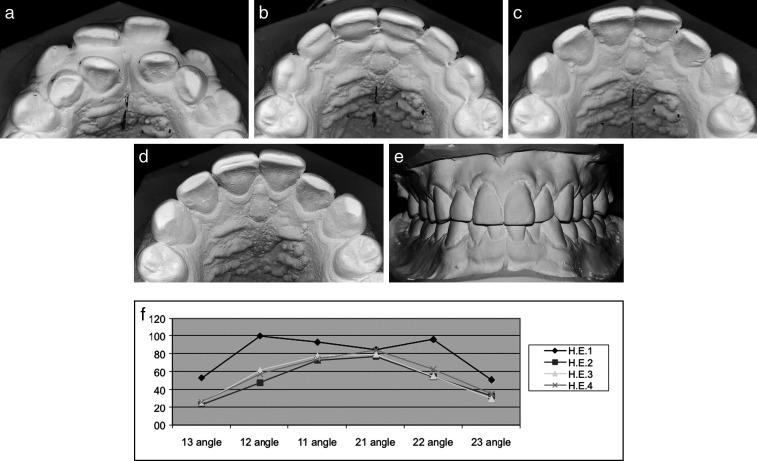
Figure 4.
Patient HE at T1 (a), T2 (b), T3 (c), T4 (d,e), and diagram of rotations (f) (angle to raphe line in degrees); 22 angle is almost the same as T2–T4, but there is a CPD between 22 and 21.
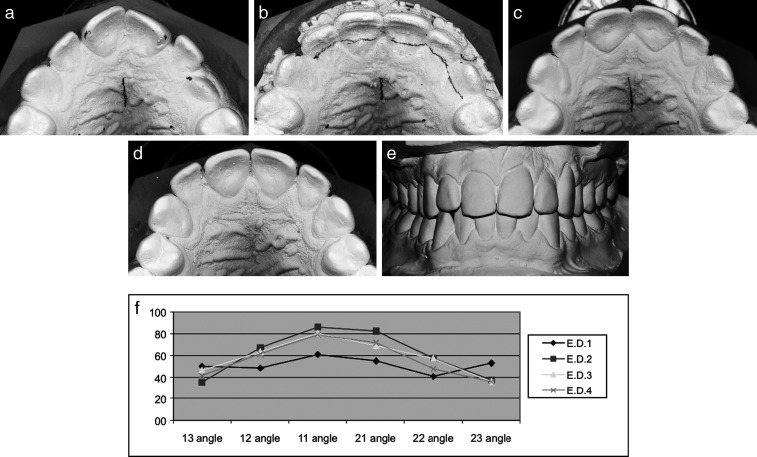
Figure 5.
Patient ED at T1 (a), T2 (b), T3 (c), T4 (d,e), and diagram of rotations (f) (angle to raphe line in degrees); 21 has relapsed between T2 and T4 about 13°, but there is no CPD between 21 and 11. Irregularity index 5.1 (T4).
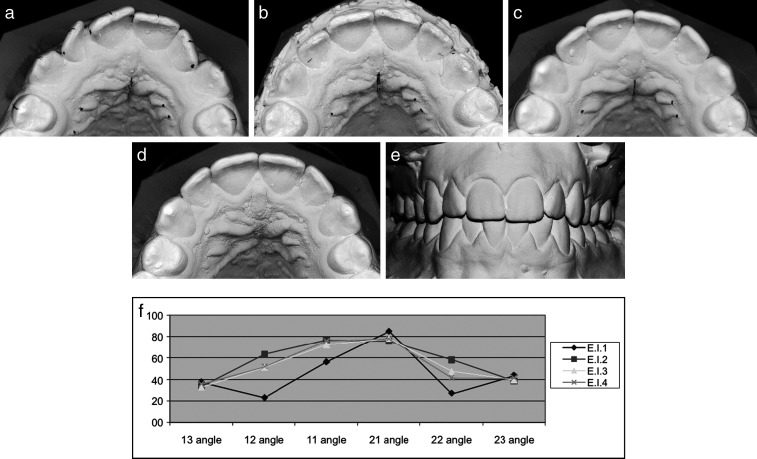
Figure 6.
Patient EI at T1 (a), T2 (b), T3 (c), T4 (d,e), and diagram of rotations (f) (angle to raphe line in degrees). It shows some rotational relapse on 12 and 22 but almost no effect on CPD of those teeth.
From an esthetic point of view, a slightly rotated upper canine is seldom disturbing due to the curved buccal surface, especially if the distal aspect of the lateral is located buccal to the mesial aspect of the canine. A rotation of a lateral or central that causes a broken contact is more displeasing (Figure 7). Our clinical impression is that the contact between lateral and central is the most critical concerning correction and stability. If after a 3-year period of retention a decision is made to use permanent retention of the maxillary front teeth, a retainer bonded to only the incisors seems to be a relevant choice.
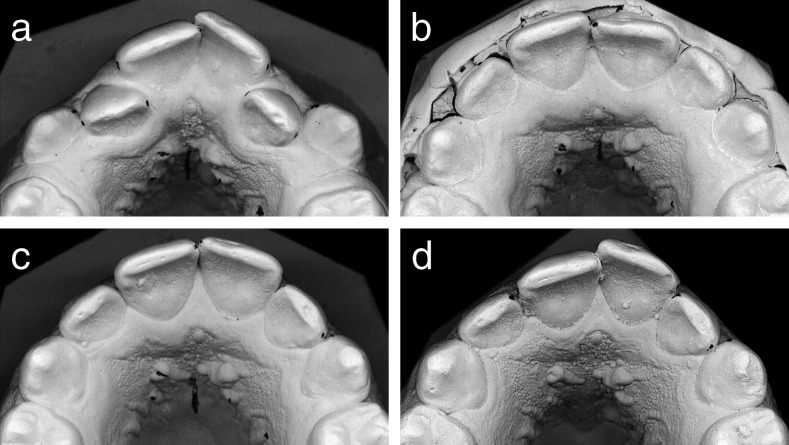
Figure 7.
Patient K at T1 (a), T2 (b), T3 (c), and T4 (d) shows overcorrection of tooth 21 between T1 and T2. Relapse continues T3 to T4.
CONCLUSIONS
The irregularity index of the maxillary front was <3 in 70% of the patients long term with 14% of the contact relationships displaced >1 mm.
Pretreatment irregularity was not correlated to long-term outcome.
There was a strong correlation between irregularity 1 and 7 years postretention.
Most of the rotational relapse was seen 1 year postretention with small changes long-term, 15% of corrections more than 20° relapsed within a range of 15°–20°. This amount of rotation is normally not visible for the patient.
Of the overcorrected contacts, 50% returned to perfect alignment.
REFERENCES
- 1.Espeland L. V, Stenvik A. Perception of personal dental appearance in young adults: relationship between occlusion, awareness, and satisfaction. Am J Orthod Dentofacial Orthop. 1991;100:234–241. doi: 10.1016/0889-5406(91)70060-A. [DOI] [PubMed] [Google Scholar]
- 2.Shaw W. C. Factors influencing the desire for orthodontic treatment. Eur J Orthod. 1981;3:151–162. doi: 10.1093/ejo/3.3.151. [DOI] [PubMed] [Google Scholar]
- 3.Heiser W, Niederwanger A, Bancher B, Bittermann G, Neunteufel N, Kulmer S. Three-dimensional dental arch and palatal form changes after extraction and nonextraction treatment after extraction and nonextraction treatment. Part 1. Arch length and area. Am J Orthod Dentofacial Orthop. 2004;126:71–81. doi: 10.1016/j.ajodo.2003.05.015. [DOI] [PubMed] [Google Scholar]
- 4.Little R. M, Riedel R. A, Årtun J. An evaluation of changes in mandibular anterior alignment from 10 to 20 years postretention. Am J Orthod Dentofacial Orthop. 1988;93:423–428. doi: 10.1016/0889-5406(88)90102-3. [DOI] [PubMed] [Google Scholar]
- 5.Boese L. R. Fiberotomy and reproximation without lower retention 9 years in retrospect: part II. Angle Orthod. 1980;50:169–178. doi: 10.1043/0003-3219(1980)050<0169:FARWLR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Boley J. C, Mark J. A, Sachdeva R. C, Buschang P. H. Long-term stability of Class I premolar extraction treatment. Am J Orthod Dentofacial Orthop. 2003;124:277–287. doi: 10.1016/s0889-5406(03)00448-7. [DOI] [PubMed] [Google Scholar]
- 7.Sadowsky C, Schneider B. J, BeGole E. A, Tahir E. Long-term stability after orthodontic treatment: nonextraction with prolonged retention. Am J Orthod Dentofacial Orthop. 1994;106:243–249. doi: 10.1016/S0889-5406(94)70043-5. [DOI] [PubMed] [Google Scholar]
- 8.Vaden J. L, Harris E. F, Gardner R. L. Relapse revisited. Am J Orthod Dentofacial Orthop. 1997;111:543–553. doi: 10.1016/s0889-5406(97)70291-9. [DOI] [PubMed] [Google Scholar]
- 9.Edwards J. G. A long-term prospective evaluation of the circumferential supracrestal fiberotomy in alleviation orthodontic relapse. Am J Orthod Dentofacial Orthop. 1988;93:380–387. doi: 10.1016/0889-5406(88)90096-0. [DOI] [PubMed] [Google Scholar]
- 10.Naraghi S, Andrén A, Kjellberg H, Mohlin B. O. Relapse tendency after orthodontic correction of upper front teeth retained with a bonded retainer. Angle Orthod. 2006;76:570–576. doi: 10.1043/0003-3219(2006)076[0570:RTAOCO]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Zachrisson B. U. Clinical experience with direct-bonded orthodontic retainers. Am J Orthod Dentofacial Orthop. 1977;71:440–448. doi: 10.1016/0002-9416(77)90247-0. [DOI] [PubMed] [Google Scholar]
- 12.Little R. M. The irregularity index: a quantitative score of mandibular anterior alignment. Am J Orthod Dentofacial Orthop. 1975;68:554–563. doi: 10.1016/0002-9416(75)90086-x. [DOI] [PubMed] [Google Scholar]
- 13.Dahlberg G. Statistical Methods for Medical and Biological Students. London, UK: George Allen and Unwin Ltd; 1940. [Google Scholar]
- 14.Surbeck B. T, Årtun J, Hawkins N. R, Leroux B. Associations between initial, posttreatment, and postretention alignment of maxillary anterior teeth. Am J Orthod Dentofacial Orthop. 1998;113:186–195. doi: 10.1016/s0889-5406(98)70291-4. [DOI] [PubMed] [Google Scholar]
- 15.Jones M. L. The Barry project-a further assessment of occlusal treatment change in a consecutive sample: crowding and arch dimensions. Br J Orthod. 1990;17:269–285. doi: 10.1179/bjo.17.4.269. [DOI] [PubMed] [Google Scholar]
- 16.Sadowsky C, Sakols E. I. Long-term assessment of orthodontic relapse. Am J Orthod Dentofacial Orthop. 1982;82:456–463. doi: 10.1016/0002-9416(82)90312-8. [DOI] [PubMed] [Google Scholar]
- 17.Ormiston J. P, Huang G. J, Little R. M, Decker J. D, Seuk G. D. Retrospective analysis of long-term stable and unstable orthodontic treatment outcomes. Am J Orthod Dentofacial Orthop. 2005;128:568–574. doi: 10.1016/j.ajodo.2004.07.047. [DOI] [PubMed] [Google Scholar]