Abstract
Aim:
To test the null hypothesis that there are no significant differences in the reusability of debonded brackets with regard to debonding technique and adhesive used.
Method:
Ninety-six osteotomed third molars were randomly assigned to two study groups (n = 48) for bonding of a 0.018-inch bracket (Ormesh, Ormco) with either a composite adhesive (Mono-Lok2; RMO) or a glass ionomer cement (GIC; Fuji Ortho LC;GC). Each of these two groups were then randomly divided into four subgroups (n = 12) according to the method of debonding using (1) bracket removal pliers (BRP; Dentaurum), (2) a side cutter (SC; Dentaurum), (3) a lift-off debracketing instrument (LODI; 3M-Unitek), or (4) an air pressure pulse device (CoronaFlex; KaVo). The brackets were subsequently assessed visually for reusability and reworkability with 2× magnification and by pull testing with a 0.017- × 0.025-inch steel archwire. The proportions of reusable brackets were individually compared in terms of mode of removal and with regard to adhesives using the Fisher exact test (α = 5%).
Results:
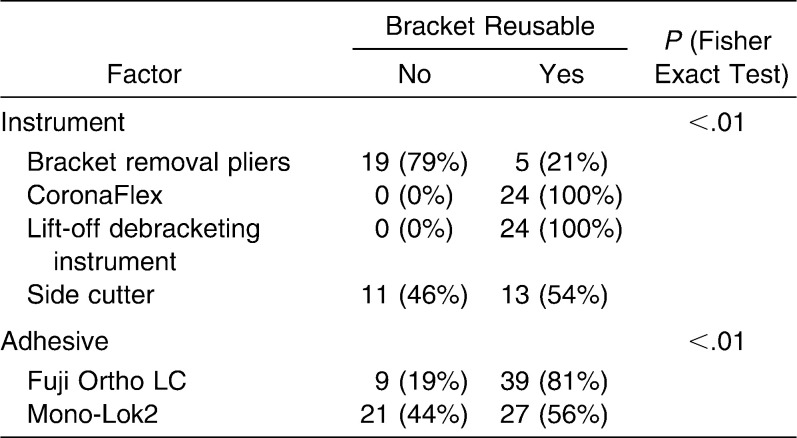
The null hypothesis was rejected. Not taking into account the debonding method, brackets bonded with GIC were judged to a significant extent (81%; n = 39; P < .01) to be reworkable compared with those bonded with composite (56%; n = 27). All brackets in both adhesive groups removed with either the LODI or the CoronaFlex were found to be reusable, whereas 79% (46%) of the brackets removed with the BRP (SC) were not. The proportion of reusable brackets differed significantly between modes of removal (P < .01).
Conclusion:
With regard to bracket reusability, the SC and the BRP cannot be recommended for debonding brackets, especially in combination with a composite adhesive.
Keywords: Debonding, Rebonding, Bracket reusability, CoronaFlex
INTRODUCTION
The bracket adhesive technique is an important and routine part of contemporary orthodontics because it provides the basis for ensuring a controlled force and torque transmission from the archwire on the teeth. The enamel-adhesive-bracket interface has to provide both aspects of reliable attachment of the bracket during treatment and also easy and quick removal following treatment with the least possible amount of damage to the enamel surface.
Another important aspect is that of economics. The cost factor can be significantly reduced if the bracket debonding is carried out in such a way that it does not damage the brackets during removal; that is, the brackets can be reused following different forms of processing, for either rebonding incorrectly positioned brackets or recycling, requiring only a fraction of the price for a new bracket.
Matasa1 investigated differences in the damage to brackets as a result of different debonding techniques. Damage can be done to the wings of the bracket, in addition to deformation of the bracket base or slot. If these occur, it will no longer be possible to reuse or rework the bracket.
Orthodontic bracket recycling, which is perhaps more appropriately referred to as bracket processing or bracket reworking, as brackets are not reshaped but only separated from stains and adhesive remnants using heat and chemical agents, followed by cleaning and polishing results in brackets that reach standards of quality comparable to those shown by unused brackets2 and are able to withstand the same draw-off strengths.3
Because of the increasing importance of the economic aspect of orthodontics, the use of reworked brackets has been adopted by a growing number of orthodontists. In a questionnaire distributed among 300 members of the British Orthodontic Society, 48% said they used processed brackets for economic reasons.4
Another rationale for using a bracket-preserving method of debonding is the intentional removal and rebonding of incorrectly positioned brackets,5 a challenge orthodontists regularly face. Even the slightest deformations of the bracket slot can result in lowered fitting accuracy of the inserted archwire, producing unwanted friction.6
Therefore, in addition to the enamel-preserving aspect of debonding, it is important for many orthodontists to choose a method of bracket removal that does not deform or damage the bracket and allows for instant rebonding.
To ensure the reusability of a bracket, it is important to choose both an appropriate adhesive and the right instrument for debonding. Current bracket adhesives are mostly based on diacrylates. Their bonding strength has been tested in numerous studies, and they have produced good results,7,8 which to a substantial extent is due to the conditioning of the enamel surface by etching and subsequent mechanical retention to microporosity.9
Apart from composites, glass ionomeric cements (GIC) are in common use in orthodontics. In contrast to composite adhesives, they do not work by using mechanical retention but instead by acid-base interaction between GIC and enamel.10 Compton et al.11 reported that light-cured GIC had a higher bonding strength compared with chemically hardened GIC and suggested the use of GIC with prior conditioning of the enamel surface with a weak acid to enhance cohesion as an alternative to conventional orthodontic composites. However, later studies confirmed the assumption that composites produce significantly higher bond strengths during bracket fixation than light-cured GIC.12
The aim of this in vitro study was therefore to optimize bracket removal to enable their reusability with rebonding after incorrect bonding and for reworking, by testing four different debonding instruments (side cutter, bracket removal pliers, lift-off debracketing instrument, and an air pressure crown remover; CoronaFlex, Kavo, Biberach/Riss, Germany) used in prosthodontics for the removal of crowns and bridges) and two different types of orthodontic adhesives (a composite adhesive and a GIC).
The null hypothesis was that there are no significant differences in terms of the reusability of debonded brackets in relation to the debonding technique and adhesive used.
MATERIALS AND METHODS
Teeth
Ninety-six third molars that were freshly osteotomed due to a lack of space were included in the study. The exclusion criteria of enamel damage (fractures, demineralization, or decay) were assessed by visual inspection using a 2× magnifier. The patients or their guardians gave informed consent for donation of the extracted third molars for study purposes. Both for better handling and a simulation of the viscoelastic cushioning and elastic dental fiber suspension, the cleaned teeth were each embedded in small blocks of silicon (Silaplast; Detax, Ettlingen, Germany; Figure 1) and stored in physiological saline at 20°C, which was renewed every second day.
Figure 1.
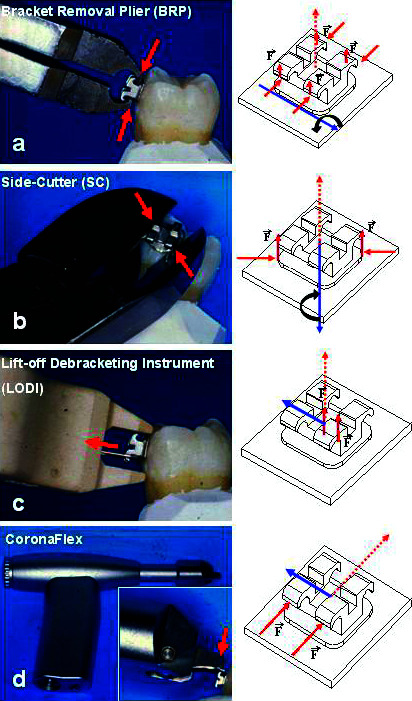
Instruments used for debonding with the corresponding force systems generated (red), moments (blue), and effective force (dotted) on the bracket base. Please see the online version of this article for the color version of figure 1.
The teeth were randomly assigned to one of two study groups (n = 48) for either bonding with composite adhesive or with GIC. Then the two groups were each once more randomly divided into four subgroups (n = 12), and these were allocated one of the four bracket-debonding methods described in the following sections.
Brackets
Maxillary premolar metal brackets (0.018-inch slot system; Ormesh; Ormco, Orange, CA), which were identical on both the left and right sides, proved to fit neatly to the buccal surface of the third molars. The brackets had a common meshlike base to provide better adhesive retention.13
Adhesives
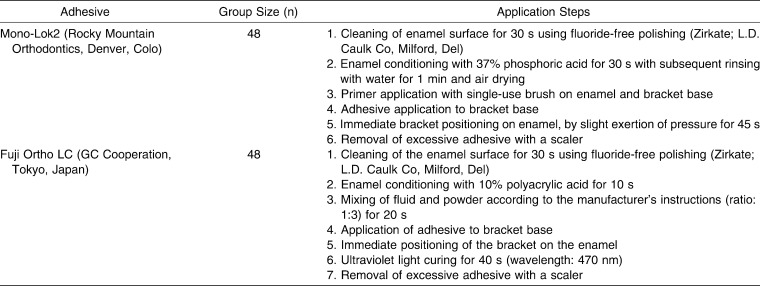
We used two types of adhesive for bracket bonding following the manufacturers' instructions for application. Representative for the composites, Mono-Lok2 (Rocky Mountain Orthodontics, Denver, Colo) was used, a one-paste hybrid composite of methacrylmonomers and polymers, with prior enamel etching using 37% phosphoric acid. For the GIC, we used Fuji Ortho LC (GC Co-operation, Tokyo, Japan), a light-cured, resin-modified GIC that is characterized by enhanced bond strength compared with conventional GIC.11,14 Prior enamel conditioning was achieved by etching with 10% polyacrylic acid. Application steps for both adhesives are shown in Table 1.
Table 1.
Application Steps for Both the Composite Adhesive Mono-Lok2 and the Glass Ionomere Cement Fuji Ortho LC
Debonding
Removal of the brackets was carried out 24 hours after bonding. Four different debonding instruments were employed: (1) a medium-sized side cutter (SC; Dentaurum, Ispringen, Germany), (2) bracket removal pliers (BRP; Dentaurum; Ispringen, Germany), (3) a lift-off debracketing instrument (LODI; 3M Unitek, Monrovia, Calif), and (4) an air pressure pulse device (CoronaFlex; Kavo, Biberach, Germany), which is used in prosthodontics for the removal of crowns and bridges (Figure 1a-d).
Although variations in the use of the debonding instruments are possible, debracketing was performed in the typical, standardized manner. The SC was orientated in such a way that it was inserted diagonally at the bracket base at the cervical and incisor portion of the bracket wing. The bracket was removed by gentle squeezing of the pliers and an additional clockwise rotational movement.
The BRP was used by gripping below the bracket wings. By closing and downward tipping of the pliers, a rotational axis was created at the apical bracket margin, thereby releasing the bracket.
The LODI was positioned by linking its hanger to the upper left bracket wing and simultaneously resting the instrument on the tooth. Compression of the pliers caused the bracket to lift off on application of a pulling force.
The CoronaFlex was used by positioning its toggle parallel to the adhesive-enamel interface. By pulling the trigger, a piston with a weight of 2.5 g was impelled by an air pressure of 2.2 bar along the shaft on the toggle, releasing a short impact pulse of 3000 N for 10 milliseconds, which removed the adhesion.
Criteria and Assessment of Reusability of Debonded Brackets
At first, the brackets were visually inspected using a 2× magnification for deformations to the bracket base, wings, or slot, compared directly with an unused (new) bracket of the same type (Figure 2a), as recovery of brackets with visual deformations cannot be reworked at a reasonable cost.6 Only slight deformations of the slot inhibit the wire insertion, or at least the gliding of the bracket along the archwire (Figures 2b,c). Therefore, brackets were subsequently tested with a straight 0.017- × 0.025-inch archwire (Ormco) for deadlock or crepitation, which are signs of slot deformation. The assessment criterion for being not reworkable and nonreusable was whether the archwire resulted in any noticeable friction or jamming, either during complete manual pulling through the slot (Figure 2c) or by regular insertion into the slot. Both tests were carried out twice by two orthodontists in the Dentistry Centre at the University of Göttingen, Germany. A bracket was judged to be reusable if it passed both tests. Testing was implemented prior to and after debonding: all 96 brackets fresh from the factory were therefore intact at baseline.
Figure 2.
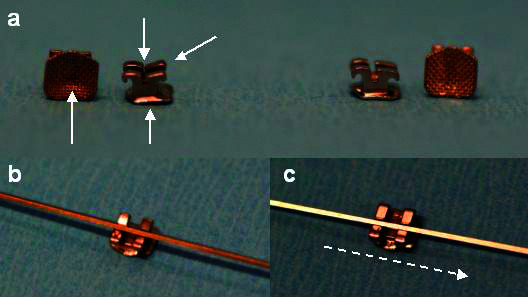
Examples of (a, left) deformed and (a, right) intact brackets. (b) Misfit of archwire due to slot deformation. (c) Pull testing.
Statistical Analyses
The proportion of reusable brackets was compared between instruments and adhesives, respectively, using the Fisher exact test. The significance level for the tests was chosen to be α = 5%. All analyses were performed using the software R (version 2.8, www.r-project.org).
RESULTS
Adhesive Factor
Leaving the method used for the bracket removal out of the analysis, of those brackets bonded with Fuji Ortho LC, 81% (n = 39) were judged to be reworkable. Of those bonded with Mono-Lok2, 56% (n = 27) were judged to be reworkable (Table 2). Statistically, the proportions of reusable brackets was therefore significant (P < .01), and accordingly, the null hypothesis was rejected. In general, brackets bonded with Fuji Ortho LC were subjectively easier to remove compared with those bonded with MonoLok.
Table 2.
Comparison of Bracket Reusability Between Instruments and Adhesives
Instrument Factor
The proportions of reusable brackets also differed significantly between instruments (P < .01), so that the second element of the null hypothesis was also rejected. All brackets of both adhesive groups removed with the LODI and also those removed with the impulse device were reusable; that is, they were intact according to the standard used in the evaluation. The results of the assessment for bracket reusability for the BRP and the SC were worse (Table 2) and differed significantly when compared with one another (P = .04). Particularly in combination with the MonoLok bonding, the BRP and SC results were discouraging (Table 2).
DISCUSSION
The proportion of reusable debonded brackets may be influenced by three factors: the mode of enamel conditioning, the adhesive used, and the mode of debonding.
The composite adhesive MonoLok2 was used in combination with prior enamel conditioning by etching with 37% phosphoric acid, to enhance the interface area between the adhesive and the enamel by dissolving enamel prisms away to a depth of 22 μm, thereby providing a basis for mechanical adhesive retention.15
Fuji Ortho LC requires enamel conditioning with 10% polyacrylic acid. Its penetration depth can be judged as moderate compared with the use of 37% phosphoric acid.16 Its purpose is not to enhance mechanical retention but to reduce interface (surface) tension, to provide the basis for chemical bonding between the enamel and GIC.17
Contemporary light-cured GIC produces clinically acceptable results for bond strength,14,18 although they are below those for conventional composites.19,20 Moreover, they are easier to handle than are composites such as MonoLok2 as they do not require a completely dry operation area,18 which is of advantage in, for example, the unforeseen necessity of instant rebonding of lost or incorrectly positioned brackets during practice hours or bonding lingual mandibular teeth.
On the subject of enamel damage following debonding, Kusy21 raised the question of whether and when higher bond strengths are necessary and recommended the use of GIC for orthodontic purposes. Our findings indicate that a side effect of these lower bond strengths of GIC appears to be a significantly reduced proportion of brackets that are not reusable after debonding (Table 2). Putting the method of bracket removal to one side and focusing on the adhesive factor, almost half of the brackets bonded with MonoLok2 were not in such a condition as to allow reuse or reworking, whereas in the GIC group, less than 20% of the brackets had corresponding deformations. This result is not only in agreement with previous findings of higher bond strengths for composites than for GIC8,14,18 but also seems to confirm our subjective impression that the brackets used in our study that were bonded with Fuji Ortho LC were easier to flip off compared with those bonded with MonoLok2.
Beyond a diversity of debonding methods and their modifications, variations in the application of the tested devices themselves are possible, with the result of different force influence lines. We therefore propose to base discussions of the effects of debonding methods not only on the type of the instrument but also on a clear description of the way it was applied, as variations may have an influence on bracket deformation.
The equivalent force systems created by the different instruments during removal of the brackets may provide an explanation for the proportions of nonreusable brackets. The use of the BRP produces symmetrical force insertion on all four bracket wings (Figure 1a). These forces are transmitted to bracket base and slot but do not contribute to bracket removal, as they cancel each other, but they do contribute to a deformation of bracket base and especially bracket slot. The equivalent force system created by the BRP is a force perpendicular to enamel surface and bracket base, which creates a moment parallel to the bracket base (Figure 1a). The result is wing and slot deformation, which absorbs forces that would otherwise be transmitted on the enamel. In this context, Benett et al.22 described the BRP method as more enamel preserving than those methods that produce forces on the bracket base, as does the SC, but they also reported that brackets removed with the removal pliers were not suitable for rebonding.
The pulling force exerted by the SC is generated by the wedge effect of the pliers' cutting end (Figure 1b). Compression of the pliers creates a deformation of the bracket base. As these forces are identical in magnitude but opposite in direction, they cancel each other out and do not contribute to the release of the bracket. The insertion at two points of the bracket generates a force couple (ie, a moment with an initial axis of rotation at the center of the bracket and a force that is perpendicular to the enamel surface). Therefore, regardless of the adhesive used, the SC resulted in a majority of the brackets' having deformations at the base or at the slot. We can therefore conclude that the compression of brackets by an insertion of opposite forces, as described for the BRP and the SC method, may be decisive in excluding brackets as being suitable for rebonding.
The equivalent force system generated by the LODI is a pull-off force perpendicular to the bracket base, which creates a moment that is parallel to the enamel surface (Figure 1c). There was no compression of the bracket, and although there was a pulling force insertion at one bracket wing, all brackets debonded with the LODI remained intact afterward. This result is in accordance with findings from previous studies.23,24
The equivalent force system created by the CoronaFlex is a force and a moment that are both parallel to the enamel surface and to the bracket base (Figure 1d). In combination with the immediate elimination of the adhesive layer, the absence of compressive forces and the moment parallel to the enamel provide an explanation for the preservation of all brackets during debonding.
Clinical Implications
Irrespective of the adhesive used, the LODI and the CoronaFlex provided the best results in relation to the reusability of debonded brackets. If conventional debonding techniques (BRP, SC) are used, the use of a GIC is favored, since its lower bond strength compared with composite adhesives18 seems to result in a significantly higher portion of reusable brackets. In addition, the insertion of a gauge or archwire matching the slot width during debonding may be considered a useful step to prevent the slot from collapsing.
CONCLUSIONS
The proportions of reusable or reworkable brackets differed significantly depending on the mode of removal and the adhesive used (P < .01).
In the case of those bonded with the GIC Fuji Ortho LC, a significantly higher number of brackets could be recovered or reused compared with those bonded with the composite MonoLok2 (P < .01).
All brackets removed with the LODI and with the impulse device were reusable, that is, intact according to the evaluation criterion, regardless of the adhesive used, whereas 79% (46%) of the brackets removed with the removal pliers (SC) were not.
When assessed in terms of bracket reusability, especially in combination with the MonoLok2 composite adhesive, the SC and the BRP cannot be recommended for debonding brackets.
REFERENCES
- 1.Matasa G. C. Pros and cons of the reuse of direct-bonded appliances. Am J Orthod Dentofacial Orthop. 1989;96:72–76. doi: 10.1016/0889-5406(89)90232-1. [DOI] [PubMed] [Google Scholar]
- 2.Eliades T, Zinelis S, Eliades G, Athanasiou A. E. Characterization of as-received, retrieved, and recycled stainless steel brackets. J Orofac Orthop. 2003;64:80–87. doi: 10.1007/s00056-003-0216-8. [DOI] [PubMed] [Google Scholar]
- 3.Postlethwaite K. M. Recycling bands and brackets. Br J Orthod. 1992;19:157–164. doi: 10.1179/bjo.19.2.157. [DOI] [PubMed] [Google Scholar]
- 4.Coley-Smith A, Rock W. P. Bracket recycling—who does what? Br J Orthod. 1997;24:172–174. doi: 10.1093/ortho/24.2.172. [DOI] [PubMed] [Google Scholar]
- 5.Mui B, Rossouw P. E, Kulkarni G. V. Optimization of a procedure for rebonding dislodged orthodontic brackets. Angle Orthod. 1999;69:276–281. doi: 10.1043/0003-3219(1999)069<0276:OOAPFR>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Machen D. E. Orthodontic bracket recycling. Am J Orthod Dentofacial Orthop. 1993;104:618–619. doi: 10.1016/S0889-5406(05)80447-0. [DOI] [PubMed] [Google Scholar]
- 7.Miguel J. A, Almeida M. A, Chevitarese O. Clinical comparison between glass ionomer cement and a composite for direct bonding of orthodontic brackets. Am J Orthod Dentofacial Orthop. 1995;107:484–487. doi: 10.1016/s0889-5406(95)70115-x. [DOI] [PubMed] [Google Scholar]
- 8.Valente R. M, de Rijk W. G, Drummond J. L, Evans C. A. Etching conditions for resin-modified glass ionomer cement for orthodontic brackets. Am J Orthod Dentofacial Orthop. 2002;121:516–520. doi: 10.1067/mod.2002.122165. [DOI] [PubMed] [Google Scholar]
- 9.Bishara S. E, Gordon V. V, Von Wald L, Jakobsen J. R. Shear bond strength of composite, glass ionomer and acid primer adhesive systems. Am J Orthod Dentofacial Orthop. 1999;115:24–28. doi: 10.1016/s0889-5406(99)70312-4. [DOI] [PubMed] [Google Scholar]
- 10.Wilson A. D, Kent B. E. A new translucent cement for dentistry. Br Dent J. 1972;132:133–135. doi: 10.1038/sj.bdj.4802810. [DOI] [PubMed] [Google Scholar]
- 11.Compton A. M, Meyers C. E, Hondrum S. O, Lorton L. Comparison of the shear bond strength of a light-cured ionomer and a chemically cured glass ionomer for use as an orthodontic bonding agent. Am J Orthod Dentofacial Orthop. 1992;101:138–144. doi: 10.1016/0889-5406(92)70005-U. [DOI] [PubMed] [Google Scholar]
- 12.Cook P. A, Youngson C. C. An in vitro study of the bond strength of a glass ionomer cement in the direct bonding of orthodontic brackets. Br J Orthod. 1988;15:247–253. doi: 10.1179/bjo.15.4.247. [DOI] [PubMed] [Google Scholar]
- 13.Maijer R, Smith D. C. Variables influencing the bond strength of metal orthodontic bracket bases. Am J Orthod. 1981;79:20–33. doi: 10.1016/0002-9416(81)90098-1. [DOI] [PubMed] [Google Scholar]
- 14.Cacciafesta V, Jost-Brinkmann P. G, Süßenberger U, Miethke R. R. Effects of saliva and water contamination on the enamel shear bond strength of light-cured glass ionomer cement. Am J Orthod Dentofacial Orthop. 1998;113:402–407. [PubMed] [Google Scholar]
- 15.Shinchi M. J, Soma K, Nakabayashi N. The effect of phosphoric acid concentration on resin tag length and bond strength of a photo-cured resin to acid-etched enamel. Dent Mater. 2000;16:324–329. doi: 10.1016/s0109-5641(00)00024-5. [DOI] [PubMed] [Google Scholar]
- 16.Farquhar R. B. Direct bonding comparing a polyacrylic acid and a phosphoric acid technique. Am J Orthod. 1986;90:187–194. doi: 10.1016/0889-5406(86)90064-8. [DOI] [PubMed] [Google Scholar]
- 17.Attin T, Buchalla W, Hellwig E. Influence of enamel conditioning on bond strength of resin-modified glass-ionomer restorative materials and polyacid-modified composites. J Pros Dent. 1996;76:29–33. doi: 10.1016/s0022-3913(96)90342-x. [DOI] [PubMed] [Google Scholar]
- 18.Fricker J. P. A new self-curing resin-modified glass ionomer cement for direct bonding of orthodontic brackets in vivo. Am J Orthod Dentofacial Orthop. 1998;113:384–386. [PubMed] [Google Scholar]
- 19.Bishara S. E, Von Wald L, Laffon J. F, Jakobsen J. R. Effect of altering the type of enamel conditioner on the shear bond strength of a resin-reinforced glass ionomer adhesive. Am J Orthod Dentofacial Orthop. 2000;118:288–294. doi: 10.1067/mod.2000.104903. [DOI] [PubMed] [Google Scholar]
- 20.Toledano M, Osorio R, Osorio E, Romeo A, de la Higuera B, Garcia-Godoy F. Bond strength of orthodontic brackets using different light and self-curing cements. Angle Orthod. 2003;73:56–63. doi: 10.1043/0003-3219(2003)073<0056:BSOOBU>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 21.Kusy R. Letter to the editor. Am J Orthod Dentofacial Orthop. 1994;106:17A. [PubMed] [Google Scholar]
- 22.Bennett C. G, Shen C, Waldron J. H. The effects of debonding on the enamel surface. J Clin Orthod. 1984;18:330–334. [PubMed] [Google Scholar]
- 23.Oliver R. G. The effect of different methods of bracket removal on the amount of residual adhesive. Am J Orthod Dentofacial Orthop. 1988;93:196–200. doi: 10.1016/s0889-5406(88)80003-9. [DOI] [PubMed] [Google Scholar]
- 24.Coley-Smith A, Rock W. P. Distortion of metallic orthodontic brackets after clinical use and debond by two methods. Br J Orthod. 1999;26:135–139. doi: 10.1093/ortho/26.2.135. [DOI] [PubMed] [Google Scholar]