Abstract
Objective
To estimate the surgical burden of malignant disease in the Eastern Region of Ghana.
Design
Descriptive cross-sectional study.
Setting
Regional hospital in the eastern region of Ghana.
Participants
Patients treated by the surgery department at Eastern Regional Hospital in Koforidua, Ghana.
Interventions
None.
Primary and secondary outcome measures
Primary outcome was incidence of malignancy and secondary outcome descriptive differences between patients who had a benign indication for surgery compared with those with a malignant indication for surgery.
Results
A total of 1943 inpatient surgical procedures were performed from 2015 to 2017 with 13.4% (261) of all procedures ultimately performed for malignancy. Of all breast procedures performed, 95.2% of procedures resulted in a malignant diagnosis. The remaining subtypes of procedures had rates ranging from <1% to 41.2% of procedures performed for malignant disease. Additionally, this study found over 13% of patients admitted to the surgical service for breast cancer ultimately did not undergo a surgical procedure.
Conclusion
This is the first study investigating the burden of malignant disease in the Eastern Region of Ghana. We found a substantial prevalence of malignant disease in the surgical population in this region. This information can be used to aid in future medical resource planning in this region.
Keywords: oncology, surgery, pathology
Strengths and limitations of this study.
The burden of malignant disease in the eastern region of Ghana is currently unknown and this study represents the first study to characterise the incidence, distribution and demographics of patients with malignant disease in this region.
This study represents a novel method to estimate cancer burden in low-resource communities without comprehensive cancer registries using surgical log books and pathology records.
This study contains important results that can be used for resource allocation and capacity building of oncologic care programmes.
Given the lack of cancer registries, there is no way to characterise detailed oncologic, treatment and overall survival data in this population.
This study includes only patients treated by general surgery given limited records of other specialties and does not include patients with obvious advanced or metastatic disease who are not considered surgical candidates.
Background
Cancer is a major cause of morbidity and mortality worldwide with low and middle-income countries (LMIC) such as those in Sub-Saharan Africa shouldering a majority of the burden of cancer-related mortality.1 In 2016, out of 9 million cancer-related deaths, 70% occurred in LMIC.2 Historically, the burden of cancer has been overshadowed in LMIC countries by infectious and neonatal mortalities. However, as life expectancy has been progressively increasing in countries such as Ghana, attention has been shifted towards preventing cancer-related deaths.3 4 In Ghana, cancer-related disease is currently the fifth leading cause of death at 58 deaths per 100 000 population annually.5 While the current burden of cancer in Ghana is significant, the International Agency for Cancer Research estimates that cancer incidence and mortality to double by 2040,6 reinforcing the importance of understanding and addressing burden of cancer-related mortality in this region.
Contributing to this disproportionate burden of cancer in Ghana and other parts of Sub-Saharan Africa is inadequate data and lack of centralised cancer registries. Cancer registries are a basic but essential tool for understanding patterns of cancer and developing effective programmes regarding resource utilisation.7 High-quality cancer registries such as the Cancer Incidence in Five Continents have provided valuable information for high-income continents such as North America, where over 95% of the population is included in existing cancer databases. Data are inadequate for continents such as Africa, where the proportion of population covered is less than 2%.8 While attempts have been made to develop sustainable population-based cancer registries (PBCRs) in Ghana, inadequate funding, lack of personnel, insufficient coordination of reporting sources and the lack of available census data have made it difficult to implement.9 10 Currently, the only existing PBCR in Ghana is the Kumasi Cancer Registry, which was established in 2012 and collects cancer data from Komfo Anokye Teaching Hospital and Kumasi South Regional Hospital.11 In the absence of PBCRs, the majority of cancer incidence estimates for Ghana are based on mathematical modelling, which includes prevalence of risk factors and the use of data from other countries in Sub-Saharan Africa.12
Despite the known growing burden of cancer in Sub-Saharan Africa, the lack of cancer registries along with limited understanding of the incidence and distribution of different tumour types makes it difficult to allocate resources for early detection and treatment.10 13 Limited existing research has shown that a majority of patients with cancer in Ghana present with advanced disease14–16 and often require surgical intervention. In fact, an existing cancer registry found that over 50% of cancers treated at Komfo Anokye Teaching Hospital in Kumasi were treated by surgical resection only and never received medical or radiation oncology treatments.10 17 This is concerning as the cancer registry initially collected information only from the medical oncology department, resulting in a majority of the cancer cases inadvertently being left out of the registry.
Given both the unknown burden of cancer outside of large cities in Ghana as well as the likely significant surgical burden of cancer-related disease, the aim of this study was to investigate the surgical cancer burden in the suburban/rural setting of Ghana’s eastern region. We hypothesised that there is a high burden of cancer-related disease affecting the population of Ghana’s eastern region, and that a substantial proportion of general surgery resources is currently being used to treat malignant disease. By using data obtained from the inpatient general surgical service at Eastern Regional Hospital (ERH), a large referral centre for the eastern region of Ghana, our study aims to estimate the incidence and burden of cancer-related surgeries from 2015 to 2017 at this institution.
Methods
Data source
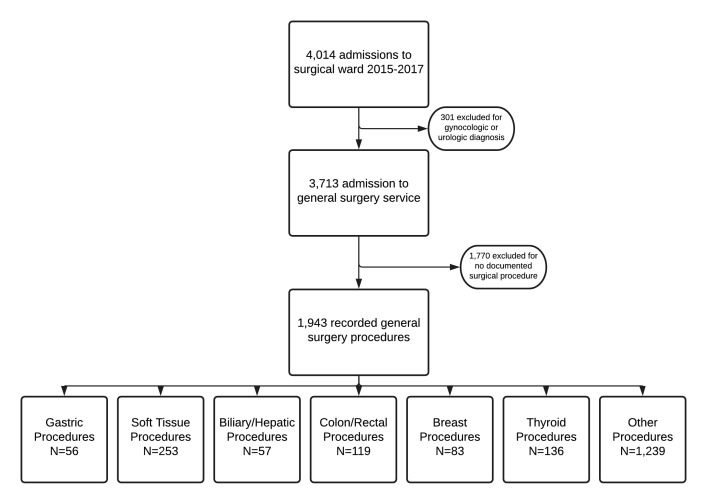
Surgical logbooks and the electronic medical record at ERH in Koforidua, Ghana were reviewed for all surgical admissions from 2015 to 2017 to create a database of surgical patients. Demographic information including age, sex, admitting diagnosis and surgical procedure performed was available within the database. Primary surgical procedures for potentially malignant disease were grouped into one of seven categories, including gastric, soft tissue, biliary/hepatic, colon/rectal, breast, thyroid or other. Any patient admitted to the inpatient surgical service at ERH between 2015 and 2017 and who had a procedure with general surgery was included in the database. Men, women and children were included in this study. Patients having gynaecological or urologic surgery were excluded. Patients who did not have surgery or if the procedure was not recorded were excluded (figure 1).
Figure 1.
Flowchart of patients included in study.
Data regarding pathologic information were obtained directly from pathology records. All pathology for ERH is performed at the neighbouring hospital, St. Joseph Orthopaedic Hospital. After any surgical procedure that results in a specimen that is appropriate for pathologic evaluation, patients are asked to transport the specimen and must pay an additional fee to St. Joseph Orthopaedic Hosptial. Pathologic results are then given directly to the patient or family member and must be physically brought to their subsequent follow-up appointment with the operating surgeon at ERH. There is inconsistent inclusion of pathology reports in medical records, thus all pathology reports recorded at St. Joseph Orthopaedic hospital for procedures performed at ERH were examined from 2015 to 2017. Any pathologic reports of malignancy were obtained and included in this study except for gynaecological and urologic tumours. Only patients admitted to the surgical ward were included in this study, with all outpatient procedures and patients admitted to medical, gynaecological and paediatric wards excluded from this study. Approval for use of the data was given by the institutional review board at The Pennsylvania State University College of Medicine (STUDY00011242) as well as by ERH ethical review board.
Patient and public Involvement
It was not appropriate or possible to involve patients or the public in the design, or conduct, or reporting or dissemination plans of our research
Statistics
Descriptive statistics including mean and SD or median and IQR for normally distributed and skewed continuous data were reported. Categorical variables were expressed as frequencies and percentages. The incidence of cancer diagnosis by type of procedure was calculated by determining the number of malignancies identified by pathology report divided by the overall number of surgical procedures performed during the same time period.
Results
There were 4014 admissions to the surgical service from 2015 to 2017. After excluding gynaecological and urological procedures, a total of 3713 admissions for the general surgical service occurred during this time period, with 1943 having recorded surgical procedures. The 1943 patients with recorded surgical procedures included 56 gastric procedures, 253 soft tissue procedures, 57 biliary/hepatic procedures, 119 colon/rectal procedures, 83 breast procedures, 136 thyroid procedures and 1239 classified as other, most commonly hernia repair or appendectomy. The mean age, gender and insurance status distribution are seen in table 1.
Table 1.
Demographic features of patients undergoing any surgical procedures
| Gastric procedure (N=56) | Soft tissue procedure (N=253) | Biliary/hepatic procedure (N=57) | Colon/rectal procedure (N=119) | Breast procedure (N=83) | Thyroid procedure (N=136) | Other procedure (N=1239) | |
| Gender | |||||||
| Female | 19 (33.9%) | 94 (37.2%) | 37 (64.9%) | 24 (20.2%) | 80 (96.4%) | 126 (92.6%) | 433 (34.9%) |
| Male | 37 (66.1%) | 159 (62.8%) | 20 (35.1%) | 95 (79.8%) | 3 (3.6%) | 10 (7.4%) | 806 (65.1%) |
| Age | |||||||
| Mean (SD) | 51.4 (20.37) | 47.3 (21.73) | 52.6 (20.24) | 43.5 (18.23) | 54.0 (13.44) | 47.0 (13.10) | 40.6 (20.40) |
| Median | 58.0 | 45.0 | 51.0 | 42.0 | 54.0 | 47.0 | 38.0 |
| IQR | 35.5, 65.5 | 31.0, 66.0 | 40.0, 68.0 | 30.0, 52.0 | 46.0, 61.0 | 38.0, 57.5 | 25.0, 55.0 |
| Range | (0.0–88.0) | (1.0–94.0) | (7.0–96.0) | (5.0–97.0) | (15.0–94.0) | (16.0–83.0) | (0.0–140.0) |
| Insurance status | |||||||
| No | 15 (26.8%) | 45 (17.8%) | 9 (15.8%) | 41 (34.5%) | 15 (18.1%) | 7 (5.1%) | 504 (40.7%) |
| Yes | 41 (73.2%) | 208 (82.2%) | 48 (84.2%) | 78 (65.5%) | 68 (81.9%) | 129 (94.9%) | 735 (59.3%) |
Information obtained from pathology reports is presented in table 2. A total of 261 pathology reports during 2015–2017 revealed a definitive malignant diagnosis. This indicates that 134 per 1000 surgeries performed at EHR during this time period were performed due to a malignant diagnosis with confirmed pathologic evaluation. When including all patients admitted to and treated by the surgical service, with or without documented surgical intervention, this study found that 70 per 1000 surgical admissions had a diagnosis of malignancy that was pathologically confirmed.
Table 2.
Demographic features of all patients with malignant diagnosis
| Gastric | Soft tissue | Biliary/hepatic | Colon/rectal | Breast | Thyroid | Other | Total | |
| Number | 17 | 21 | 5 | 49 | 79 | 14 | 12 | 261 |
| Gender | ||||||||
| Female | 9 (52.9%) | 11 (52.4%) | 2 (40%) | 27 (55.1%) | 77 (97.5%) | 13 (92.9%) | 7 (58.3%) | |
| Male | 8 (47%) | 10 (47.6%) | 3 (60%) | 21 (42.9%) | 2 (2.5%) | 1 (7.1%) | 5 (41.7%) | |
| Age | ||||||||
| Mean (SD) | 58.3 (19.77) | 49.2 (16.3) | 56.6 (6.4) | 55.1 (16.4) | 50.0 (14.7) | 44.7 (14.8) | 54.3 (21.6) | |
| Median | 59.5 | 48.0 | 57 | 58 | 48 | 44 | 53 | |
| Range | (28–97) | (29–80) | (45–63) | (15–85) | (4–79) | (13–68) | (20–94) |
When further investigating categories of surgical procedure, the highest incidence of malignancy was found to be in those undergoing inpatient breast procedures. 95.2% (79/83) of all breast procedures resulted in a diagnosis of breast cancer. Of those with a diagnosis of breast cancer, 97.5% were women with an average age of 54 years old (SD 13.44).
A total of 119 colon, rectal and anal procedures were performed from 2015 to 2017, resulting in 49 with a confirmed malignant diagnosis. This means that 41.2% of all colon, rectal and anal procedures were ultimately performed for malignant disease. The majority of these cancers were determined to be colon adenocarcinoma (29/49), 15/49 were for adenocarcinoma located in the rectum, 3/49 were performed for squamous cell carcinoma of the anus and 2/49 were indeterminant rectoanal malignancy. Colorectal cancers were evenly distributed between men and women with a slight female predominance (42.9% and 55.1%, respectively). Those who were diagnosed with colorectal malignancy were on average older with a mean age of 55.1 years (SD 16.4) compared with the mean age of 43.5 years (SD 18.23) of all those undergoing colon and rectal surgical procedures.
Another surgical procedures found to have high rates of final malignant diagnosis were gastric procedures, with 30.4% (17/56) of all gastric procedures performed during this time period, resulting in malignant diagnosis. Of the 17 patients with pathologic evidence of gastric malignancy, there was similar incidence in male and female patients. The mean age of patients diagnosed with gastric malignancy was 58.3 (SD 19.77) compared with 51.4 (SD 20.37) in those undergoing all gastric surgical procedures.
The remaining types of procedures had malignancy rates of 10.3% (14/136) for all thyroid procedures, 8.8% (5/57) of all biliary procedures, 8.3% (21/253) of all soft tissue procedures and less than 1% (12/1,239) of all other procedures, resulting in a malignant diagnosis. Demographic information regarding age and gender is seen in table 2.
Further investigation into patients with an admitting diagnosis of breast disease, including individuals with breast cancer, breast abscess, breast cyst and breast lumps, is presented in table 3. There were 145 patients admitted with a diagnosis related to breast disease with 57.2% (83/145) known to have breast cancer or suspected to have breast cancer based on physical examination, resulting in an admitting diagnosis of ‘breast cancer’. Of the 83 patients with an admitting diagnosis of breast cancer, 81.0% (68/83) had surgical treatment with mastectomy. No documented surgical procedure was performed in 13.1% (11/84) of those admitted with a diagnosis of breast cancer.
Table 3.
Details of those with admitting diagnosis related to breast disease
| Admitting diagnosis | 145 |
| Breast abscess | 29 |
| Breast cyst | 5 |
| Breast lump | 28 |
| Breast cancer | 83 |
| Surgical procedure performed for those with breast cancer | 83 |
| Mastectomy | 68 (81.0%) |
| Chest tube placement | 1 (1.2% |
| Emergency tracheostomy | 1 (1.2%) |
| Palliative excisional procedure | 3 (3.8%) |
| No surgical procedure | 11 (13.1%) |
Discussion
The findings from this study represent important data that can be used locally, regionally and nationally to better identify and treat patients with oncologic disease and allocate limited medical resources. Specifically, at ERH, the results from this study can be used by physicians treating individual patients as well as by administration for resource planning. Given that a majority of patients with final malignant disease were suspected to have benign disease preoperatively based on admitting diagnosis, the knowledge of incidence of malignancy and demographic information presented in this study could be used to guide surgeon decision-making about operative intervention on possible malignant disease. For example, awareness that currently greater than 30% of all gastric procedures that are performed at ERH are for malignancy and that malignant diagnosis was found more often in older patients allow for consideration of further diagnostic work-up or referral to oncology prior to surgical intervention. On a larger health system scale, given the high burden of cancer at ERH demonstrated by this study, future development of local chemotherapy and radiation therapy programmes should be considered a priority.
Without an existing uniform PBCR system in Ghana,11 distribution of resources and development of medical infrastructure to enhance access to treatment of cancer is challenging. Unfortunately, formal PBCRs are associated with significant cost and time to develop. Because of this, LMIC countries such as Ghana must often rely on basic estimates of cancer burden when developing plans for the distribution and development of systems focused on cancer treatment.18 While there have been significant advancements regarding planned development of cancer registries in primarily large, urban hospitals9 such as those in Kumasi10 and Accra,19 the burden of malignancy faced by smaller suburban and rural hospitals, with extremely limited resources, is unknown and is unlikely to be captured by formal cancer registries for the foreseeable future. With this in mind, this study demonstrates the current need for cancer resources in the Eastern Region of Ghana. Today, patients who require specialised oncologic care must travel to another region for care, with a majority of patients from ERH referred to Korle Bu for treatment. These facilities are hours away from the patient’s home and treatment is often delayed due to the high volume of patients that are referred to these limited specialised centres. With no regional access to oncology care, many patients are treated with systemic chemotherapy prescribed and managed by the operating surgeon at ERH, which likely accounts for the patients admitted to the surgical service with a diagnosis of breast cancer who then did not undergo any surgical procedure observed in this study. This study demonstrates that small, regional hospitals have a substantial and diverse oncologic burden and are in dire need of infrastructure, resources, and specialised personnel to treat patients diagnosed with cancer.
While this study contains important data regarding the burden of malignancy in this geographic area, there are limitations that must be considered when interpreting this data. As there is currently no existing cancer registry capturing malignancies treated in this region, we do not have access to many demographic, oncologic, treatment and overall survival data. This additional information would be helpful for further planning and resource utilisation. Additionally, while a majority of patients presenting with malignancy are admitted to and treated by the surgical service, this study does not capture patients with cancer treated by other specialties, most notably gynaecological cancers. Because this is a hospital-based study and not a population study, this study cannot account for patients in the region who did not seek care at ERH for their malignancy. This has the potential to bias our results in unpredictable ways, especially if the decision to not seek medical care was different among different groups. For example, if elderly patients were less likely to seek care compared with younger patients or if uninsured patients were less likely to seek care compared with patients with health insurance, this could lead to lower estimation of median age or under estimation of incidence of cancer diagnoses. In addition, patients admitted to the surgical service with obvious advanced or metastatic disease are not considered surgical candidates and are not accounted for in these data. Finally, because patients must transport and pay additional fees in order to obtain pathology results, there are pathologic specimens that are never examined and recorded. Currently, it is estimated that about 20% of all specimens that surgeons request pathologic evaluation do not undergo pathologic evaluation due to patient non-compliance or inability to afford the extra associated fee. Missing pathologic results could lead to underestimation of the true incidence of malignancy treated surgically at ERH.
Conclusion
This is the first study to investigate the cancer burden in Ghana’s Eastern Region. This study reveals that over 13% of all surgical interventions were performed in patients with malignant disease. Rates of malignant diagnosis vary by type of procedure performed but are very high in patients undergoing breast, colorectal and gastric procedures. This study is a preliminary evaluation demonstrating the substantial cancer burden in the eastern region of Ghana and the burden of oncologic disease on general surgeons. Information from this study can be used to improve access to oncologic-directed treatments in this region and plan future studies to further evaluate the burden of cancer and cancer-related diseases at local and regional healthcare facilities in Sub-Saharan Africa.
Supplementary Material
Footnotes
Contributors: EJO was involved in study design, data collection, data analysis, interpretation of data, majority of manuscript authorship and critical review and editing of manuscript. PS was involved in study design, data collection, data analysis, interpretation of data, and critical review and editing of manuscript. JD was involved in study design, data collection, data analysis, critical review and editing of manuscript. WGW was involved in study design, data collection, data analysis, critical review and editing of manuscript. KAS was involved in study design, data collection, data analysis, critical review and editing of manuscript. RO-A was involved in interpretation of data, critical review and editing of manuscript. FA-M was involved in study design, interpretation of data, critical review and editing of manuscript, and supervised the entirety of the project. CP was involved in study design, interpretation of data, critical review and editing of manuscript and supervised the entirety of the project. CP is responsible for the overall content as the guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request. All data relevant to the study are included in the article. Raw, deidentified data is available after reasonable request from eolecki@pennstatehealth.psu.edu; orcid ID: https://orcid.org/0000-0002-6204-8654.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and approval for use of the data was given by the institutional review board at The Pennsylvania State University College of Medicine (STUDY00011242) as well as by ERH ethical review board. This was a retrospective, deidentified database and patients could not be identified to obtain consent.
References
- 1.Shah SC, Kayamba V, Peek RM, et al. Cancer control in low- and middle-income countries: is it time to consider screening? J Glob Oncol 2019;5:1–8. 10.1200/JGO.18.00200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Cancer Society . The global cancer burden, 2020. Available: https://www.cancer.org/health-care-professionals/our-global-health-work/global-cancer-burden.html
- 3.National policy for the prevention and control of chronic non-communicable disease in Ghana Ministry of Health, 2012. Available: https://www.iccp-portal.org/sites/default/files/plans/national_policy_for_the_prevention_and_control_of_chronic_non-communicable_diseases_in_ghana(1).pdf
- 4.de-Graft Aikins A, Addo J, Ofei F, et al. Ghana’s burden of chronic non-communicable diseases: future directions in research, practice and policy. Ghana Med J 2012;46:1–3. [PMC free article] [PubMed] [Google Scholar]
- 5.Institute for Health Metrics and Evaluation . Global burden of disease cause patterns, 2016. Available: https://vizhub.healthdata.org/gbd-compare/
- 6.Ferlay JSI, Ervik M. Cancer incidence and mortality worldwide. Available: https://gco.iarc.fr/tomorrow/home
- 7.Control CfD . National program of cancer registries cancer surveillance system rationale and approach 1999.
- 8.Bray F, Ferlay J, Laversanne M, et al. Cancer incidence in five continents: inclusion criteria, highlights from volume X and the global status of cancer registration. Int J Cancer 2015;137:2060–71. 10.1002/ijc.29670 [DOI] [PubMed] [Google Scholar]
- 9.Yarney J, Ohene Oti NO, Calys-Tagoe BNL, et al. Establishing a cancer registry in a resource-constrained region: process experience from Ghana. JCO Glob Oncol 2020;6:610–6. 10.1200/JGO.19.00387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O'Brien KS, Soliman AS, Awuah B, et al. Establishing effective registration systems in resource-limited settings: cancer registration in Kumasi, Ghana. J Registry Manag 2013;40:70–7. [PMC free article] [PubMed] [Google Scholar]
- 11.Laryea DO, Awuah B, Amoako YA, et al. Cancer incidence in Ghana, 2012: evidence from a population-based cancer registry. BMC Cancer 2014;14:362. 10.1186/1471-2407-14-362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Amoako YA, Awuah B, Larsen-Reindorf R, et al. Malignant tumours in urban Ghana: evidence from the city of Kumasi. BMC Cancer 2019;19:267. 10.1186/s12885-019-5480-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paul Opoku BA, Nyarko K. Cancer registration in low-resourced settings: practice and recommendations. Afr J Haematol Oncol 2010;1:129–37. [Google Scholar]
- 14.Kitcher E, Yarney J, Gyasi R, et al. Laryngeal cancer at the Korle BU teaching hospital Accra Ghana. Ghana Med J 2006;40:45–9. 10.4314/gmj.v40i2.36016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Clegg-Lamptey J, Hodasi W. A study of breast cancer in Korle BU teaching hospital: assessing the impact of health education. Ghana Med J 2007;41:72–7. 10.4314/gmj.v41i2.55305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martei YM, Vanderpuye V, Jones BA. Fear of mastectomy associated with delayed breast cancer presentation among Ghanaian women. Oncologist 2018;23:1446–52. 10.1634/theoncologist.2017-0409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Espina C, McKenzie F, Dos-Santos-Silva I. Delayed presentation and diagnosis of breast cancer in African women: a systematic review. Ann Epidemiol 2017;27:659–71. 10.1016/j.annepidem.2017.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hanna TP, Kangolle ACT. Cancer control in developing countries: using health data and health services research to measure and improve access, quality and efficiency. BMC Int Health Hum Rights 2010;10:24. 10.1186/1472-698X-10-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Calys-Tagoe BNL, Yarney J, Kenu E, et al. Profile of cancer patients' seen at Korle BU teaching hospital in Ghana (a cancer registry review). BMC Res Notes 2014;7:577. 10.1186/1756-0500-7-577 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request. All data relevant to the study are included in the article. Raw, deidentified data is available after reasonable request from eolecki@pennstatehealth.psu.edu; orcid ID: https://orcid.org/0000-0002-6204-8654.