Abstract
Objectives
Few studies have evaluated the prevalence of psychiatric disorders among treatment-seeking elite athletes (EA) or high-performance coaches (HPC) in psychiatric outpatient settings.
Methods
Descriptive overview of EA and HPC with psychiatric disorders at two publicly funded psychiatric outpatient treatment clinics in Stockholm and Malmö, Sweden. Co-occurring psychiatric disorders were illustrated using Venn diagrams for EA and HPC, and male and female EA separately, among patients from the Stockholm clinic (SC) that used standardised diagnostic interviews.
Results
Overall, most patients were EA (n=221) compared with HPC (n=34). The mean age was 23.5 (±5.9) years for EA and 42.8 (±8.8) for HPC. Anxiety disorders were most common at the SC in EA and HPC (69% vs 91%, respectively). Stress-related disorders were found in 72% of HPC compared with 25% of EA. Affective disorders were found in 51% of EA and 52% of HPC. Eating disorders were common among EA (26%), especially females (37%). Substance use disorders were found in 17% of HPC. Comorbidity was generally common between affective and anxiety disorders.
Conclusion
Stress and adjustment disorders were found in nearly three of the four HPC compared with one in four EA. Eating disorders were prevalent in around one in four athletes and about one in six HPC had a substance use disorder.
Keywords: anxiety, depression, eating disorders, psychiatry, stress
Key messages.
What is already known on this topic
Elite athletes (EA) suffer from mental health problems and psychiatric disorders largely to the same extent as the general population. The prevalence in high-performance coaches (HPC) has not been evaluated.
The prevalence of psychiatric diagnosis and comorbidity among treatment-seeking EA and HPC in open psychiatric care is unknown.
Few studies have examined EA and HPC with psyciatric disorders assessed by a licensed caregiver.
What this study adds
Anxiety disorders were the most prevalent diagnostic group in EA and HPC in psychiatric care found in 69% of EA and 93% of HPC. Affective disorders were present in around half of all patients, 50% of EA and 52% of HPC. Comorbidity between these two diagnostic groups was common.
Eating disorders were frequently found in EA (26%), especially in females (37%). In HPC, 17% presented with a substance use disorder compared with 6% of the EA. Eating disorders among EA were generally found with concurrent anxiety and/or affective disorder.
How this study might affect research, practice or policy
Our results support the development of, and further research on, transdiagnostic prevention strategies and treatment for EA and HPC.
The results contribute to preventing and treating psychiatric disorders in these populations.
Introduction
Research involving elite athletes (EA), high-performance coaches (HPC) and mental health has increased in the last 10 years, especially regarding EA. However, most research on mental ill health in elite sport has been conducted by screening presumingly healthy populations of EA,1 presenting symptoms of psychiatric disorders with the use of questionnaires, and not on clinical cohorts of EA or HPC with psychiatric disorders assessed by a licensed caregiver according to the International Statistical Classification of Diseases and Related Health Problems version 10 (ICD-10).2 3
In Sweden, 17.2% of the general population experienced clinical levels of depression and 10.8% of the general population experienced clinical levels of anxiety in 2013, and of those, nearly 50% had symptoms of a comorbid psychiatric disorder.4 Furthermore, 5.2% of the Swedish population had at least one contact with specialised psychiatric care and a psychiatric medical record in 2020,5 and in Stockholm, 16.5% of the population used some form of psychiatric service in 2017.6
From a lifetime perspective, a longitudinal cohort study following individuals in New Zeeland from birth to age 45 years over time using three versions of the Diagnostic and Statistical Manual of Mental Disorders for diagnosis (versions 3–5) found that 86% were diagnosed with at least one psychiatric disorder7 and only 17% had enduring mental health,8 indicating that episodes of psychiatric disorders may be more the norm than the exception.
EA are as vulnerable to psychiatric disorders in sport as the general population.2 9 The female over-representation for many psychiatric disorders is also present among EA and includes, for example, affective, anxiety and eating disorders.10 11 The prevalence of HPC is unknown.3 For EA, specific risk factors include injury and overtraining, sport-related stressors and stigma towards help-seeking. Generic risk factors also apply to EA and HPC, such as genetics, low social support, poor general health, ineffective coping, history of violence and/or abuse and maladaptive personality traits.2 11–13 Compared with EA, HPC are usually older, and females are under-represented. For HPC, sport-related risk factors include performance-related pressure, job insecurity, excessive workload, feelings of isolation and challenges connected to work-life balance.3 14 15
In Sweden, 8.1% of EA (at the national team level) reported a lifetime prevalence of psychiatric disorders (females 10.7%, males 4.4%). Most common were depressive disorders, eating disorders and stress-related disorders.16 In France, all EA undergo annual psychiatric evaluations, and 16.9% had at least one ongoing or recent psychiatric disorder (females 20.2%, males 15.1%).17 A prospective study (12 months) with Dutch EA found symptoms of psychiatric disorders, that is, reaching the established clinical cut-off using validated questionnaires but without a psychiatric evaluation by a licensed caregiver, ranging from 6% for adverse alcohol use to 57% for symptoms of anxiety/depression.9
Regarding specific diagnoses, eating disorders are over-represented among EA18 19 and substance use disorders may be more prevalent than in the normal population.20 Most research that targets mental health among HPC has addressed coaching stress and/or burnout,3 but anecdotal reports of harmful alcohol use have also been reported.21
To our knowledge, no study has evaluated psychiatric disorders and comorbidity among EA or HPC in psychiatric outpatient treatment. Therefore, this study describes comorbidities between psychiatric disorders and clinical characteristics among EA and HPC in a consecutive clinical cohort.
Methods
Study population
To meet the need for psychiatric treatment in elite sports, different models of service provision have been established worldwide.22 In Sweden, two psychiatric outpatient clinics specialising in elite sport, Mottagningen för Elitidrott och Hälsa, in Stockholm and Malmö, opened in early 2015 and late 2017, respectively. These two clinics are each located within a larger psychiatric clinic specialised in addiction open to the general population in Sweden. Substance use disorders can therefore be treated within the sport specialised clinics. Eating disorders are also evaluated and treated at the two clinics, but more severe cases can be referred to specialised eating disorder treatment centres after evaluation. Neuropsychiatric screenings, including assessment of attention deficit hyperactivity disorder (ADHD), are also performed. Both clinics represent a collaboration between the Swedish Sports Federation (Riksidrottsförbundet) and the public healthcare system in Sweden and have a nationwide intake of patients. The Swedish Sports Federation governs sports in Sweden. It incorporates the majority of all sports, including team sports, for example, soccer and ice hockey, and individual sports, such as swimming and gymnastics.
Patients contact the clinics using the webpage for the Swedish healthcare system (Vårdguiden www.1177.se). This electronic self-referral system was not in use during the first year, thus it is not possible to present the total number of EA and HPC contacting the clinics. After self-referral, a medical secretary generally contacts the EA or HPC to book a first appointment. During this conversation, potential patients can be referred to contact other care providers or a sport psychologist if performance enhancement strategies were their sole reason for help-seeking. All patients who after self-referral visited either of the two clinics for a psychiatric evaluation from February 2015 to May 2021 were included in a retrospectively analysed clinical cohort. All data were pseudonymised before analysis and no direct or indirect identification of specific individuals was possible based on the dataset.
It is possible for patients <18 years to seek psychiatric treatment without their guardians being informed. This is rarely the case in practice, and if it happens, the treating psychologist encourages the patient to involve the parents in their treatment. All patients fulfilling the inclusion criteria were therefore included. Inclusion criteria were (a) either a history of national team representation (as an athlete or coach) during the preceding 2 years or seeking psychiatric treatment within 1 year of retirement from elite sport defined as a history of national team representation during the preceding 2 years, (b) assessed with a standardised diagnostic interview at admission and at least one current psychiatric disorder according to the ICD-1023 and (c) no longer in treatment at any of the two clinics. Reasons for no longer being active in treatment were that the treatment was completed, being referred to other psychiatric clinics or treatment closer to home, moving or difficulties in attending the treatment sessions.
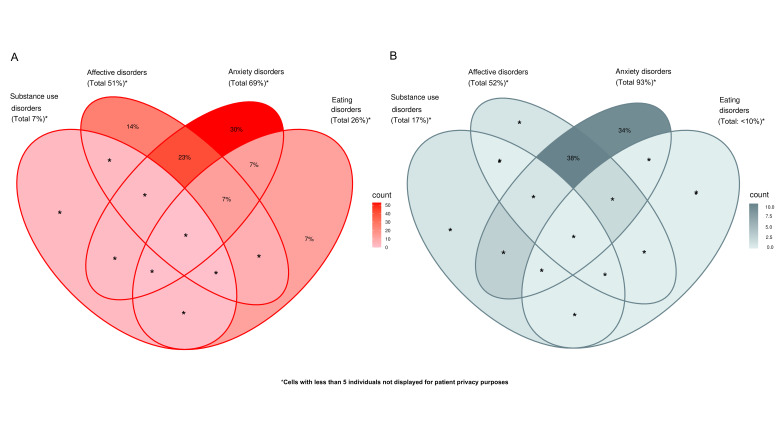
Design and procedure
At the Stockholm clinic (SC), all patients underwent standardised diagnostic interviews using the Mini-International Neuropsychiatric Interview (MINI) 7.0.0 Swedish version24 by a psychiatrist at admission. Only psychiatric diagnoses assessed in connection to the index treatment episode, defined as the time of treatment at the specialised sports clinic, are included (ie, any prior history of mental health disorders previously given by other caregivers was not considered). Diagnostic assessments at the Malmö Clinic were performed by a licensed psychiatrist according to ICD-10 criteria but did not include a standardised diagnostic interview. Based on this notable difference, only patients from the SC are included in the presentation of prevalence and comorbidity. In the demographical description (age, sex, role), athletes from both clinics are included (figure 1).
Figure 1.
Flowchart of inclusion. Basic demographic description of the cohort is based on patients from both Stockholm clinic (SC) and Malmö clinic (n=255). To assess prevalence of specific diagnostic groups (table 1) and comorbidities, only patients from SC (n=209) are included based on their use of standardised diagnostic interviews at admission. EA, elite athletes; HPC, high-performance coaches.
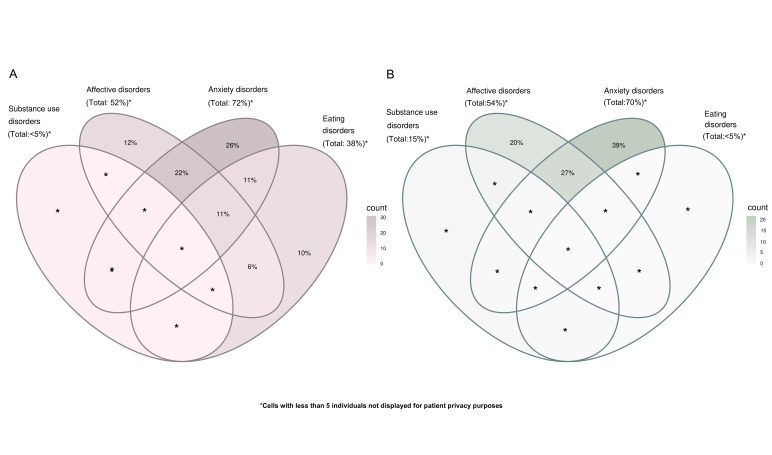
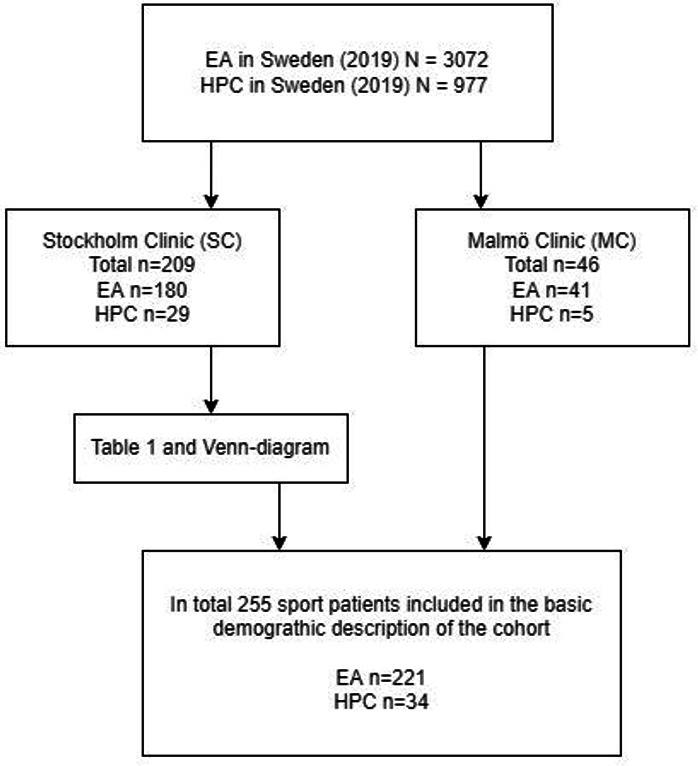
Assessment of comorbidity between specific disorders was based on four diagnostic ICD-10 categories:23 disorders due to psychoactive substance use (ICD-10: F10–F19, Z721), affective disorders (ICD-10: F30–F39), anxiety disorders (ICD-10: F40–F43) and eating disorders (ICD-10: F50). These ICD-10 categories were chosen based on being the most common diagnostic groups. All HPC (n=29) and 97% of the EA (n=175) from the SC had at least one disorder encompassed by these four groups. Venn diagrams were used to display the comorbidities between disorders within these four main diagnostic groups. A small number of uncommon disorders (n<5) were labelled ‘other disorders’ (table 1), such as ADHD and/or premenstrual dysphoric disorder.
Table 1.
Prevalence of psychiatric disorders among elite athletes (EA) and high-performance coaches (HPC) from the Stockholm Clinic between February 2015 and May 2021
| EA | HPC | ||||||
| Total (n=180) | Females (n=122) |
Males (n=58) |
Total (n=29) |
Females (n=9) |
Males (n=20) |
||
| Anxiety disorders | Any anxiety disorder | 69% | 70% | 67% | 93% | 100% | 90% |
| Phobic anxiety disorders (F40) | 31% | 33% | 26% | n<5 | 100% | n<5 | |
| Other anxiety disorders (F41) | 29% | 27% | 33% | 28% | n<5 | 35% | |
| Obsessive-compulsive disorder (F42) | 8% | 7% | 9% | n<5 | n<5 | n<5 | |
| Reaction to severe stress and adjustment disorders (F43) | 25% | 28% | 19% | 72% | 89% | 65% | |
| Affective disorders | Any affective disorder | 51% | 50% | 52% | 52% | 78% | 40% |
| Major depressive disorder, single episode or recurrent (F32, F33) | 37% | 37% | 36% | 28% | n<5 | n<5 | |
| Bipolar disorder (F31) | n<5 | n<5 | n<5 | n<5 | n<5 | n<5 | |
| Eating disorders | Any eating disorder (F50) | 26% | 37% | n<5 | n<5 | n<5 | n<5 |
| Anorexia nervosa (F50.0) | 7% | 11% | n<5 | n<5 | n<5 | n<5 | |
| Bulimia nervosa (F50.2) | 3% | 5% | n<5 | n<5 | n<5 | n<5 | |
| Eating disorder, unspecified (F50.9) | 20% | 29% | n<5 | n<5 | n<5 | n<5 | |
| Mental and behavioural disorders due to psychoactive substance use | Any disorders due to psychoactive substance use | 6% | n<5 | 14% | 17% | n<5 | n<5 |
| Alcohol-related disorders (F10, Z721) | 6% | n<5 | 14% | n<5 | n<5 | n<5 | |
| Other substance-related disorders | n<5 | n<5 | n<5 | n<5 | n<5 | n<5 | |
| Other disorders | Any other disorder | 7% | 6% | 10% | n<5 | n<5 | n<5 |
Cell counts with fewer than five individuals are displayed as n<5 for data protection purposes.
Absolute numbers, proportions and means, by sex and separately for EA and HPC, were used to summarise the data. The distribution of psychiatric diagnoses was compared by sex using a χ2 test or Fisher’s exact tests (for expected contingency table cell counts smaller than 5). Two-sample t-tests were used to investigate if the patients’ age at first contact with the clinic and the number of psychiatric diagnoses differed by sex. Due to the small group of HPC (n=29) and hence lack of power, formal statistical analyses were only performed for the EA dataset. The ggVennDiagram package in R was used to illustrate and contrast psychiatric comorbidity graphically, and the statistical programme SPSS V.2625 was used for data management and the statistical analyses.
Patient and public involvement
Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Results
In total, 255 EA and HPC fulfilled the inclusion criteria of the cohort between February 2015 and April 2021. A majority (n=221) were EA, of which 69% were females and 31% were males, compared with the HPC (n=34), of which 32% were females and 68% were males. The mean age at index admission for EA was 23.5 (±5.9, corresponding to 1 SD) years and 42.4 (±8.8) years for HPC. No significant difference in treatment-seeking age was found by sex for EA (females: 23.5 years (±5.4) years, males: 24.5 (±6.9) years, p value=0.12). The mean age for female and male HPC was 43.3 (±6.9) years and 41.9 (±9.7) years, respectively. As the SC used standardised diagnostic interviews at admission, only patients from this clinic are included in presenting the prevalence of psychiatric disorders among EA and HPC (table 1).
Elite athletes
Of all patients (n=209) from the SC, 66% were diagnosed with more than one psychiatric disorder (two diagnoses 26%, >2 diagnoses 39%). Of the EA, 69% (n=180) had an anxiety disorder. No significant sex difference in anxiety disorders was observed overall (females: 70%, males: 67%, p value χ2=0.89). Within this group, phobic disorders were most common (31%) and mostly represented social anxiety disorders. Other anxiety disorders, including, for example, generalised anxiety disorder, panic disorder and other unspecified anxiety disorders, were found in 29% of the EA. For example, stress-related disorders, including, for example, acute stress reactions, adjustment disorder, other reactions to severe stress and post-traumatic stress disorder, were observed in 25% of the EA.
Affective disorders, including major depression episodes, were found in 51% of the EA, with no significant sex difference (females: 50%, males: 52%, p value χ2=0.95). Eating disorders were present in 26% and more common in females (females: 37%, males n<5, p value χ2<0.001). Of the eating disorders, non-specified were most common (20%), followed by anorexia nervosa (7%) and bulimia nervosa (3%). Disorders due to psychoactive substance use were observed in 6% of the EA and more often in males (females n<5; males 14%, p value=0.01).
High-performance coaches
Similarly to the EA, the most common diagnostic category in HPC was an anxiety disorder, with 93% having at least one such diagnosis (females: 100%, males 90%). Stress-related disorders were most frequent (72%), followed by other anxiety disorders (28%). In HPC, 52% had been diagnosed with an affective disorder (females: 78%, males: 40%) and disorders due to psychoactive substance use were found in 17% (females: n<5, males: n<5). Eating disorder diagnoses were uncommon (n<5).
Comorbidity
The mean number of co-occurring psychiatric diagnoses in females (n=122) was 2.5 (±1.6) and in males (n=58) the corresponding number was 2.4 (±1.3). No significant sex difference in diagnoses was observed (p=0.60). Comorbidities across diagnostic groups are presented for those EA and HPC diagnosed in at least one of the four investigated diagnostic groups: substance use disorders, affective disorders, anxiety disorders and eating disorders (figure 2). All HPC (n=29) and 97% of the EA (n=175) from SC had at least one disorder encompassed by these four groups. Figure 2A shows the comorbidity of mental health disorders in the EA. Anxiety disorders alone were most common (30%), followed by accompanying anxiety and affective disorders (23%) and affective disorders alone (14%). Eating disorders tended to co-occur with an anxiety disorder (7%) or with both anxiety and affective disorder (7%) rather than manifesting as the sole disorder (7%).
Figure 2.
Venn diagrams showing the comorbidity of (A) elite athletes (n=175) and (B) high performance coaches (n=29) with at least one disorder in the four main categories (substance use disorders, affective disorders, anxiety disorders and eating disorders) in patients from the Stockholm Clinic. Darker color equals a higher prevalence for this group or overlap of groups.
Among HPC, figure 2B, anxiety disorders occurred both alone (34%) or concurrently with an affective disorder (38%). Figure 3A, B presents comorbidity for female and male EA.
Figure 3.
Comorbidity in (A) female elite athletes (n=119) and (B) male elite athletes (n=56) from the Stockholm Clinic that were diagnosed with at least one disorder in the four main categories (substance use disorders, affective disorders, anxiety disorders and eating disorders). Darker color equals a higher prevalence for this group or overlap of groups.
Figure 3A highlights that 10% of female EA with at least one disorder in the four diagnostic groups had sole eating disorders and 28% had eating disorders comorbid with anxiety and/or affective disorders.
Discussion
Based on the total EA (n=3072) and HPC (n=977) in Sweden 2019,26 27 this study comprises 7% of all EA and 3.5% of HPC. In comparison, 5.2% of the general population in Sweden had a least one contact with specialised psychiatric care in 2020.5 As any patient may also seek treatment from private caregivers or other parts of the public healthcare system (eg, primary care), direct comparisons of care utilisation should be interpreted with caution.
Gender and age
Overall, more female than male EA are included in the cohort (n=153 vs n=68) despite a slight male dominance in national team representation among EA in Sweden in 2019 (n=1651, 53.7% vs n=1421, 46.3%). This finding is consistent with the female over-representation regarding the prevalence of most psychiatric disorders in the general population.28 In addition, female EA have previously been reported at a 30% higher lifetime risk of having a psychiatric disorder than their male counterparts.17
The mean age for EA at first contact with the clinics was 23.5 years. Previous research has found that self-reported first onset of mental health problems among Swedish EA peaked at age 19 years, with 50% of onsets between 17 and 21 years16, and in longitudinal research on psychiatric disorders, 59% of onsets had occurred by adolescence.7 EA in this study might likely have had symptoms some time before seeking help or seeking treatment for a recurring episode.
Psychiatric diagnosis and comorbidity
The average number of psychiatric diagnoses in EA was 2.38 (±1.5) in the SC sample. French EA had a lifetime prevalence of 1.46 (±0.7) psychiatric disorders.17 As comorbidity is associated with more severe symptoms and lower quality of life,4 it is expected that athletes actively seeking psychiatric treatment have more severe symptoms compared with those found by the screening of presumably healthy EA. This finding also highlights the need for specialised psychiatric care for EA and HPC. These clinics play an important role as more complex mental health problems should always be assessed and treated by a licensed professional.
More than one-third of female EA had an eating disorder. In Europe, 1%–4% of women have been found to suffer from anorexia nervosa during their lifetime.29 Previous research found eating disorders to be significantly more prevalent in EA than in the general population.2 18 Together, this points towards an unmet treatment need for eating disorders in this group. Therefore, it is advisable to screen for eating disorders among EA expressing psychological distress, even if this is not the main indication for help-seeking as symptoms of eating disorders are often under-reported or hidden.2
Around two-thirds of EA had one or more anxiety disorders. In comparison, 10.8% of the general Swedish population have been found to suffer from clinical levels of anxiety.4 Interestingly, in EA almost one-third had a phobic anxiety disorder, and most of these patients, in turn, met diagnostic criteria for a social anxiety disorder. Social anxiety disorder shares many elements with performance anxiety commonly described in sports psychology. The aetiology of social anxiety disorders is explained by a complex interplay between genetic and environmental influences,30 and this is yet to be explored in the present patient population. Investigating how anxiety disorders and other disorders in EA interact may also lead to a better understanding of psychiatric symptoms in individuals with significant performance anxiety levels.
One in four EA experienced a stress-related disorder that may have relevance for potential overtraining syndromes (characterised by the imbalance between training and non-training stressors and recovery)31 since they might benefit from treatment as an adjustment disorder.32 The high prevalence of affective disorders in EA, found in around half of the help-seeking athletes, is in agreement with earlier data indicating a high prevalence of depressive symptoms in elite sport.33 For context, a point prevalence of 17.2% of clinical levels of depression have been found in the general Swedish population.4 Lastly, regarding sex differences, the over-representation of eating disorders among female EA and substance use disorders in males, respectively, reflects previous research in EA.2
In treatment-seeking HPC, psychiatric disorders or symptoms of disorders have seemingly not been evaluated before.3 In this group, the 93% prevalence of anxiety disorders stands out. Among the anxiety disorders, reactions to severe stress and adjustment disorders were observed in 72%. These are high numbers compared with the 25% of the EA sample that shares the same demanding and highly competitive context, suggesting that stress-related disorders in HPC merit further research. In the general population of Sweden in 2016, half of those with a psychiatric diagnosis resulting in sick leave suffered from a stress-related diagnosis.34 Risk factors for mental health problems in HPC suggested by previous research are also typically stress related, such as job insecurity, excessive workload and performance-related pressure.3 14 15
In HPC, 17% presented with a disorder due to psychoactive substance use. This finding signals a need to evaluate further the culture of substance use among HPC since this finding is also in agreement with qualitative research.21 Future research with larger samples should also explore the comorbidity between anxiety disorders, affective disorders and substance use disorders among HPC. Together, more research is needed regarding the mental health of HPC as this group has not gained the same attention as EA3 and, at least in a treatment setting, seems to present with a somewhat different psychiatric symptom spectrum.
Comorbidity between the four main diagnostic categories (substance use disorders, affective disorders, anxiety disorders and eating disorders) was present in 47% of EA and 58% of HPC. Therefore, we advocate for the use of transdiagnostic treatment and prevention, a valuable approach for patients with different psychiatric conditions,7 35 and that this should be explored in future research with elite sports patients. An increased understanding of the overlap of different psychiatric disorders in EA and HPC also contributes to all stakeholders working to counteract mental health problems in elite sports.
Strengths and limitations
This study of psychiatric diagnoses, comorbidity and clinical characteristics of a treatment-seeking cohort of EA and HPC may be the first to evaluate this population. Still, more research is needed from comparable contexts. The study has several important limitations, including the limited number of participants, especially HPC. Since it is a natural observation of those actively seeking psychiatric treatment by self-referral at two elite sport specialised clinics, the generalisability of results is likely limited outside this group. Furthermore, the MINI diagnostic interview does not include neuropsychiatric diagnosis or sleep disorders. In practice, if these disorders were suspected, they were assessed using additional validated questionnaires. Even so, a risk of underdiagnosis of these disorders is possible. It is also possible that patients with more chronic or severe conditions are under-represented due to the inclusion only of patients no longer active in treatment. Patients with more severe psychiatric disorders, such as psychosis or suicidal ideation, are also likely to have their first assessment elsewhere, for example, at a clinic with inpatient psychiatric care. Other disorders, like ADHD, manifest in childhood and are likely to be assessed and treated at a younger age. Overall, psychiatric diagnoses are based on diagnostic criteria combined with clinical judgement; in this study, all psychiatrists responsible for diagnostic assessment were clinicians with broad experience from manual-based psychiatric assessments from different settings of general psychiatry.
Moreover, only disorders assessed in connection to the index treatment episode were included, thus disregarding any life history of comorbidity and diagnoses established during previous contacts with psychiatric care. The use of different admission procedures at the two clinics also limits the possibility to combine datasets outside descriptions of age, sex and role of the patients. There is a free choice of care in Sweden independent of your residence and the clinics included in this study have a nationwide intake of patients. Patients from all over Sweden are treated at the two clinics, increasing generalisability of results outside of the two cities (Stockholm and Malmö). In some psychiatric clinics in Sweden, reimbursement is linked to the number of diagnoses reported in medical records. Because the clinics included in this study did not use this payment structure, it is not prone to systematic over-reporting of diagnoses. A strength of the study is that observations were made in a standard clinical setting which adds to its ecological validity and that all patients between 2015 and 2021 fulfilling the inclusion criteria were included, thereby minimising self-selection bias.
Conclusions
Anxiety and depressive disorders were the most prevalent diagnostic groups in a clinical cohort of EA and HPC. Stress and adjustment disorders were found in nearly three out of four HPC compared with one in four EA. Eating disorders were prevalent in around one in four athletes and about one in six HPC had a substance use disorder. Most of these patients also had comorbid anxiety and/or depressive disorder.
Acknowledgments
The authors thank the staff at the two clinics for their help with conducting this study.
Footnotes
Twitter: @the_sportpsych
Contributors: All authors made significant contributions to the research and interpretations of findings, contributed to interpretations and presentations of findings and made significant contributions to the text. CÅ, GK, AH and JF were responsible for data collection. SE made important contributions regarding statistical analyses. CÅ wrote the major part of the paper and are responsible for the overall content as the guarantor.
Funding: The study was funded by the Swedish School of Sport and Health Sciences and Region Stockholm.
Competing interests: CÅ and GK had a part-time employment at the Stockholm Clinic and AH had a part-time employment at the Malmö Clinic.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
In Sweden, the National Ethics Review Authority (file number 2020-05345) approved a descriptive overview of the clinical cohort regarding four variables (sex, age, role and psychiatric diagnosis) without informed consent. Patients were not routinely informed about this study, as informed consent was waived for the purposes of this descriptive overview.
References
- 1.Currie A, Blauwet C, Bindra A, et al. Athlete mental health: future directions. Br J Sports Med 2021;55:1243–4. 10.1136/bjsports-2021-104443 [DOI] [PubMed] [Google Scholar]
- 2.Reardon CL, Hainline B, Aron CM, et al. Mental health in elite athletes: international Olympic Committee consensus statement (2019). Br J Sports Med 2019;53:667–99. 10.1136/bjsports-2019-100715 [DOI] [PubMed] [Google Scholar]
- 3.Kenttä G, Olusoga P, Bentzen M. Wellbeing and Burnout. In: Hackfort D, Schinke RJ, eds. The Routhledge international Encylopedia of sport and exercise psychology, 2020: 154–65. [Google Scholar]
- 4.Johansson R, Carlbring P, Heedman Åsa, et al. Depression, anxiety and their comorbidity in the Swedish general population: point prevalence and the effect on health-related quality of life. PeerJ 2013;1:e98. 10.7717/peerj.98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Malm W. Psykiatri I siffor Vuxenpsykiatri -Kartläggning 2020. In: Regioner SKo, ed, 2021. https://www.uppdragpsykiskhalsa.se/wp-content/uploads/2021/05/Psykiatrin_i_siffror_VUP_2020_2.pdf [Google Scholar]
- 6.Forslund T, Kosidou K, Wicks S, et al. Trends in psychiatric diagnoses, medications and psychological therapies in a large Swedish region: a population-based study. BMC Psychiatry 2020;20:1–9. 10.1186/s12888-020-02749-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Caspi A, Houts RM, Ambler A, et al. Longitudinal assessment of mental health disorders and comorbidities across 4 decades among participants in the dunedin birth cohort study. JAMA Netw Open 2020;3:e203221–e21. 10.1001/jamanetworkopen.2020.3221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schaefer JD, Caspi A, Belsky DW, et al. Enduring mental health: prevalence and prediction. J Abnorm Psychol 2017;126:212–24. 10.1037/abn0000232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gouttebarge V, Jonkers R, Moen M, et al. A prospective cohort study on symptoms of common mental disorders among Dutch elite athletes. Phys Sportsmed 2017;45:426–32. 10.1080/00913847.2017.1370987 [DOI] [PubMed] [Google Scholar]
- 10.Riecher-Rössler A. Sex and gender differences in mental disorders. Lancet Psychiatry 2017;4:8–9. 10.1016/S2215-0366(16)30348-0 [DOI] [PubMed] [Google Scholar]
- 11.Kuettel A, Larsen CH. Risk and protective factors for mental health in elite athletes: a scoping review. Int Rev Sport Exerc Psychol 2019:1–35. 10.1080/1750984x.2019.1689574 [DOI] [Google Scholar]
- 12.Sullivan PF, Daly MJ, O'Donovan M. Genetic architectures of psychiatric disorders: the emerging picture and its implications. Nat Rev Genet 2012;13:537–51. 10.1038/nrg3240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Timpka T, Spreco A, Dahlstrom O, et al. Suicidal thoughts (ideation) among elite athletics (track and field) athletes: associations with sports participation, psychological resourcefulness and having been a victim of sexual and/or physical abuse. Br J Sports Med 2021;55:198–205. 10.1136/bjsports-2019-101386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thelwell RC, Weston NJV, Greenlees IA, et al. Stressors in elite sport: a coach perspective. J Sports Sci 2008;26:905–18. 10.1080/02640410801885933 [DOI] [PubMed] [Google Scholar]
- 15.Hill DM, Brown G, Lambert T-L, et al. Factors perceived to affect the wellbeing and mental health of coaches and practitioners working within elite sport. Sport Exerc Perform Psychol 2021;10:504–18. 10.1037/spy0000263 [DOI] [Google Scholar]
- 16.Åkesdotter C, Kenttä G, Eloranta S, et al. The prevalence of mental health problems in elite athletes. J Sci Med Sport 2020;23:329–35. 10.1016/j.jsams.2019.10.022 [DOI] [PubMed] [Google Scholar]
- 17.Schaal K, Tafflet M, Nassif H, et al. Psychological balance in high level athletes: gender-based differences and sport-specific patterns. PLoS One 2011;6:e19007. 10.1371/journal.pone.0019007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Joy E, Kussman A, Nattiv A. 2016 update on eating disorders in athletes: a comprehensive narrative review with a focus on clinical assessment and management. Br J Sports Med 2016;50:154–62. 10.1136/bjsports-2015-095735 [DOI] [PubMed] [Google Scholar]
- 19.Sundgot-Borgen J, Torstveit MK. Prevalence of eating disorders in elite athletes is higher than in the general population. Clin J Sport Med 2004;14:25–32. 10.1097/00042752-200401000-00005 [DOI] [PubMed] [Google Scholar]
- 20.Reardon CL. Psychiatric comorbidities in sports. Neurol Clin 2017;35:537–46. 10.1016/j.ncl.2017.03.007 [DOI] [PubMed] [Google Scholar]
- 21.Roberts SJ, Baker M, Reeves MJ, et al. Lifting the veil of depression and alcoholism in sport coaching: how do we care for carers? Qual Res Sport Exerc Health 2019;11:510–26. 10.1080/2159676X.2018.1556182 [DOI] [Google Scholar]
- 22.Moesch K, Kenttä G, Kleinert J, et al. FEPSAC position statement: mental health disorders in elite athletes and models of service provision. Psychol Sport Exerc 2018;38:61–71. 10.1016/j.psychsport.2018.05.013 [DOI] [Google Scholar]
- 23.World Health Organization . International statistical classification of diseases and related health problems: ICD-10. Geneva: World Health Organization, 2009. [Google Scholar]
- 24.Sheehan DV. The Mini-International neuropsychiatric interview (M.I.N.I) Swedish version 7.0.0, 2015. [Google Scholar]
- 25.I C. Ibm SPSS statistics for windows, version 26.0. Armonk, NY: IBM Corp, 2019. [Google Scholar]
- 26.Science SRCfS . 7 AV 10 landslagstränare är män 2019, 2021. Available: https://idrottsstatistik.se/foreningsidrott/ledare/ [Accessed 7 Aug 2021].
- 27.Science SRCfS . Antal män och kvinnor I svenska landslag 2019, 2021. Available: https://idrottsstatistik.se/foreningsidrott/elitidrott/#antalet-mn-och-kvinnor-i-svenska-landslag [Accessed 7 Aug 2021].
- 28.Diagnostic and statistical manual of mental disorders : DSM-5. Arlington, Va. American Psychiatric Association 2013.
- 29.Keski-Rahkonen A, Mustelin L. Epidemiology of eating disorders in Europe: prevalence, incidence, comorbidity, course, consequences, and risk factors. Curr Opin Psychiatry 2016;29:340–5. 10.1097/YCO.0000000000000278 [DOI] [PubMed] [Google Scholar]
- 30.Spence SH, Rapee RM. The etiology of social anxiety disorder: an evidence-based model. Behav Res Ther 2016;86:50–67. 10.1016/j.brat.2016.06.007 [DOI] [PubMed] [Google Scholar]
- 31.Kenttä G, Hassmén P. Overtraining and recovery. Sports Medicine 1998;26:1–16. 10.2165/00007256-199826010-00001 [DOI] [PubMed] [Google Scholar]
- 32.Jones CM, Tenenbaum G. Adjustment disorder: a new way of conceptualizing the overtraining syndrome. Int Rev Sport Exerc Psychol 2009;2:181–97. 10.1080/17509840903110962 [DOI] [Google Scholar]
- 33.Golding L, Gillingham RG, Perera NKP. The prevalence of depressive symptoms in high-performance athletes: a systematic review. Phys Sportsmed 2020;48:247–58. 10.1080/00913847.2020.1713708 [DOI] [PubMed] [Google Scholar]
- 34.Agency SSI. Psykiatriska diagnoser: lång tId tillbaka till arbete Vid sjukskrivning. In: Försäkringskassan, ed, 2017. https://www.forsakringskassan.se/wps/wcm/connect/d57be02c-46dc-4079-b68d-760739441f11/korta-analyser-2017-1.pdf?MOD=AJPERES&CVID= [Google Scholar]
- 35.Carlucci L, Saggino A, Balsamo M. On the efficacy of the unified protocol for transdiagnostic treatment of emotional disorders: a systematic review and meta-analysis. Clin Psychol Rev 2021;87:101999. 10.1016/j.cpr.2021.101999 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data are available.