Abstract
Among liver vascular tumours, hepatic small vessel neoplasm (HSVN) has been recently identified as a rare infiltrative vascular neoplasm whose malignant potential is yet to be fully ascertained. About 30 cases of HSVN have been described so far. The most common clinical presentation is an asymptomatic solitary liver lesion. Multifocal disease has been described in literature; however, to date, there are no reports of disease dissemination to other organs. Here we report a case of multifocal HSVN with synchronous spleen secondary lesions.
Keywords: Hepatic cancer, Radiology, Pathology
Background
In recent years, many technological advances have allowed investigators to detect and characterise the molecular genetics of different vascular tumours. Hepatic vascular tumours, in particular, comprise a heterogeneous group of neoplasms with different histology and tumour biology, therefore making the diagnosis challenging.
The most common benign vascular tumour is cavernous hemangioma, which accounts for approximately 70% of all benign liver lesions. It is characterised by well-defined margins and large vascular spaces, surrounded by flat endothelial cells.1 Size may vary from a few millimetres to more than 10 cm, the so-called giant hemangiomas.2 Between cavernous hemangioma and hepatic angiosarcoma (HAS), which stands out as the most aggressive hepatic vascular tumour with a bleak prognosis, there is a wide spectrum of tumours with different histopathology, clinical presentations, radiological behaviours and, of course, biology and genetics. In this plethora of rare neoplasms are included tumours with different degrees of malignant potential such as hepatic perivascular epithelioid cell tumours and hepatic hemangiopericytomas, characterised by a high malignant potential and hepatic epithelioid hemangioendothelioma which is classified as an entity with a variable grade of malignancy.3 HAS is the most common malignant vascular tumour, accounting for approximately 2% of primary hepatic tumours.4
Some authors hypothesise that hepatic vascular tumours may represent a continuum from the most common benign lesion, hemangioma, to the most frequent aggressive one, angiosarcoma. In this context, hepatic small vessel neoplasm (HSVN), recently identified, represents a new diagnostic entity of uncertain malignant potential, as it is characterised by an infiltrative behaviour in the absence of marked cytonuclear atypias. To date, although literature data on this newly defined tumour entity are scarce, HSVN is mostly described as a solitary liver lesion; there is some evidence that suggest that this neoplasm may appear as a multifocal disease. However, no metastatic dissemination to other organs has been described so far. Here we report a case of HSVN characterised by multifocal liver disease and synchronous spleen secondary lesions.
Case presentation
A woman in her 70s with a history of dyslipidaemia, arterial hypertension with history of haemorrhagic stroke, impaired fasting glucose, hyperuricemia, cholelithiasis and past HBV infection with evidence of seroconversion presented for further evaluation following the discovery of multiple hepatic lesions, which were identified in an ultrasonography (US) and in a CT scan performed at an outside facility.
The patient has been treated with atenolol, amlodipin, telmisartan and allopurinol. She initially sought medical attention for mild intermittent pain in the right upper quadrant of the abdomen, which resolved spontaneously with no medical treatment. She also complained of anorexia with weight loss of 10 kg in the last 12 months.
CT scan report described multiple hypodense hepatic lesions, with a maximum diameter of 2 cm, with contrast enhancement in the arterial and portal phase and wash-out in the tardive phase, suspect for metastasis. Focal lesions with the analogous imaging features and the same contrastographic behaviour were detected in the spleen, with a maximum diameter of 4×2.5 cm (figure 1). A positron emission tomography/computed tomography (PET-CT) scan was performed with no evidence of abnormal 18F-fluorodeoxyglucose (18F-FDG) uptake in any district.
Figure 1.
Abdomen CT scan shows multiple hepatic and splenic lesions with contrast enhancement in arterial (A) and portal phase (B) and wash-out in tardive phase (C). Radiological appearance and contrastographic behaviour are identical in both organs.
The patient was admitted to our hospital for clinical and pathological evaluation of the disease.
Investigations
On admission, the performance status of the patient was one per Eastern Co-operative Oncology Group scale. Physical examination revealed mild hepatomegaly. Complete blood count, serum chemistry and liver tests were within the normal ranges. Tumour markers for hepatocellular carcinoma (alpha-fetoprotein) and gastrointestinal tumours (CEA, CA19-9) were negative.
US described both the hepatic and the splenic lesions as characterised by a mixed echogenicity with an alternance of solid and liquid areas.
A CT-guided liver biopsy was performed, with multiple samplings from the same nodule.
Histological examination showed a vascular neoplasm with anastomosing small thin channels lined by plump and hobnail endothelial cells, with bland nuclear atypias; no necrosis was observed. Immunohistochemistry was positive for CD34, ERG, CD31 and vimentin, while pankeratin and Hep-Par1 were negative. There was no significant expression of p53, and Ki-67 index was <5% (figures 2A, B and 3). A diagnosis of HSVN was made and confirmed after a review by a soft-tissue tumour reference institution.
Figure 2.
Histological specimen (H&E stained tissue) shows a vascular proliferation with anastomising vascular channels surrounded by rounded endothelial cells are observed (A). Immunohistochemistry demonstrates diffuse positivity for the vascular marker ERG (B).
Figure 3.
H&E stained tissue. Further magnification (40x) showing bland nuclear atypias and hobnail cells surrounding the vascular channels.
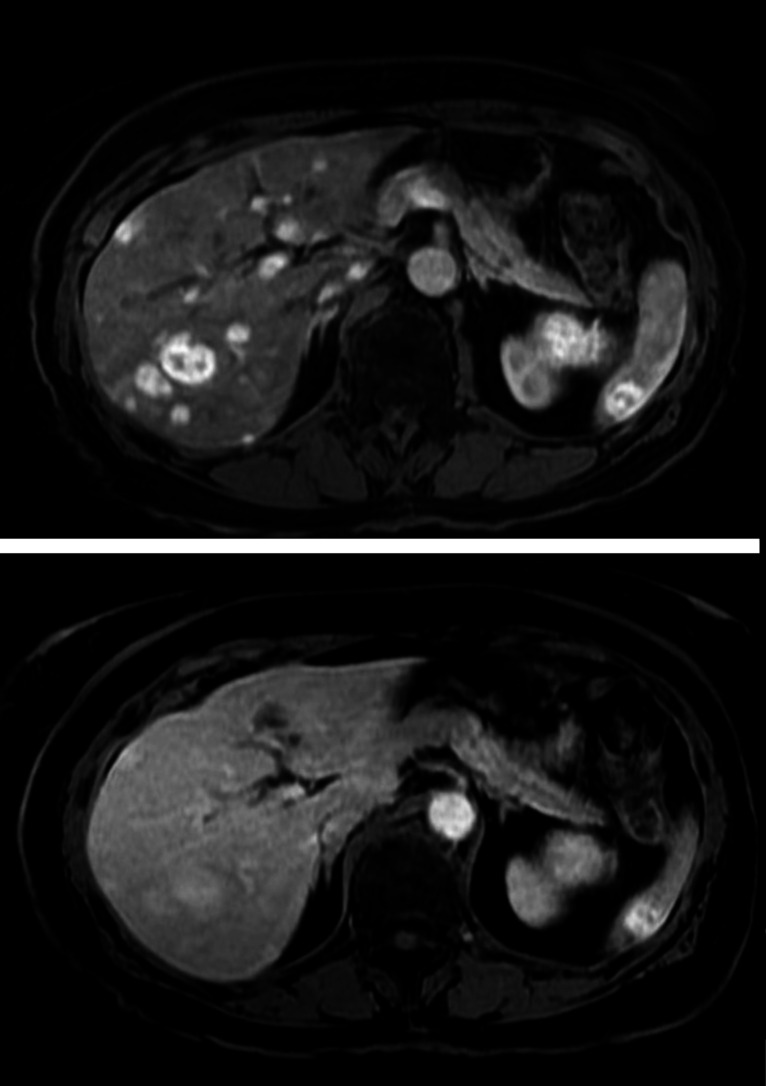
Abdominal MRI was performed during the radiological follow-up. Hepatic and splenic lesions showed the same MRI appearance with hyperintensity in T2-weighted images with no diffusion coefficient restriction. Moreover, the lesions had the same contrastographic behaviour with a strong and early homogeneous enhancement in the arterial phase, which persisted in the portal phase, with a central area characterised by an irregular morphology and a late and gradual enhancement (figure 4).
Figure 4.
Multiphasic abdomen MRI demonstrates multiple hepatic and splenic lesions with a strong and early contrast enhancement in the arterial phase (top), with a central area displaying irregular morphology and gradual enhancement; contrast enhancement persisted in the portal phase with a tendency to the wash-out in the late portal one (bottom).
Given the undefined malignant potential of the lesion and the multifocality of the disease and taking into account the patient’s age and comorbidities, we decided to adopt a wait-and-see strategy with close clinical and radiological follow-up. To date, the 15-months follow-up of our patient was uneventful and the hepatic and splenic lesions are numerically and dimensionally stable.
Outcome and follow-up
To date, the 15-months follow-up of our patient was uneventful and the hepatic and splenic lesions are numerically and dimensionally stable.
At the time of writing this report, there is no evidence of recurrence or progressive disease in any of the patients for which follow-up was available. Longer follow-up is needed to establish the potential recurrence or metastases of this entity.
Discussion
HSVN is a rare infiltrative vascular neoplasm of the liver of undetermined malignant potential. It can mimic HAS because of its infiltrative behaviour, but lacks the marked cytological and nuclear atypias that are typical of the HAS. HSVN was originally described by Gill et al, who analysed 17 cases collected in a 5years period.5
Less than 30 HSVN cases have been described so far.5–11 In the vast majority of the cases, HSVN presented as a single lesion in the liver. However, in four patients included in our literature review, there was evidence of a second hepatic lesion, thus suggesting that HSVN may occur as a multifocal disease;6 moreover, in one case a suspect splenic lesion had been detected although no histological examination was carried out. In our patient, the radiological appearance and the contrastographic behaviour of the splenic lesions was very similar to that of the hepatic nodules, as shown in figure 2A, B. Therefore, it is very likely that both the spleen and liver lesions represent multiple foci of the same disease, although spleen biopsy was not performed due to the patient’s age and comorbidities, taking into account the risks of such procedure.
In immunohistochemical assays, HSVN is characterised by a strong expression of vascular markers, namely CD31, CD34 and FLI-1 or ERG, while pancytokeratines staining is negative.5 All HSVN cases show a Ki-67 index <10%; Gill et al suggest that this Ki-67 cut-off may be useful in differentiating this disease from the more aggressive angiosarcoma, which is normally characterised by higher levels of Ki-67 staining. On the other hand, Ki-67 expression in HSVN could also be helpful in differentiating this tumour from cavernous hemangioma, which usually shows no proliferative activity. In addition, morphological examination by an experienced pathologist could be able to discriminate an HSVN from a hemangioma; for example, HSVN lacks the typical fibrous walls of cavernous hemangioma and it does not present spindle cells, which are commonly found in capillary hemangioma.
Molecular characterisation of the HSVN cases described so far demonstrated recurrent activating hotspot mutations of GNAQ and GNA14, which occurred in a mutually exclusive fashion; two cases had missense mutations in GNAQ.7 Activating mutations in gene encoding the alpha subunit of the GTP-binding protein (GNAQ and its paralogues GNA14, GNA11 and GNA15) have been described in hepatic vascular malformations and benign vascular neoplasm such as congenital hemangioma and anastomosing hemangioma but not in their malignant counterpart, HAS; therefore, identification of these molecular alterations, along with histological features and immunohistochemical analysis, may be useful in the distinction between HSVN and HAS.
Radiological findings of HSVN described to date are inconclusive because of the different techniques used in the case reported in literature.8 9 It has been suggested that contrast-enhanced ultrasonography (CEUS) may raise suspicion of HSVN because its contrastrographic behaviour may differ to that of typical hemangiomas or high-flow hemangiomas.8 Paisant et al, who analysed four cases combining CEUS, CT scan and MRI of the liver, recognise the same enhancement pattern in all lesions, with a thick continuous rim enhancement in the arterial phase and radial enhancement septa configuring a ‘flower-petal’ shape in MRI.6 Our radiological findings are in line with those described in literature, with a strong and early peripheral tumour enhancement in the arterial phase associated with a late and gradual enhancement in the central area. The identical appearance and contrastographic pattern displayed in the imaging techniques performed corroborate the hypothesis that both hepatic and splenic lesions belong to the same disease.
As in our case, the most common clinical presentation of HSVN is with a liver mass as an incidental finding on imaging for a different clinical indication; all the patients were asymptomatic. Our patient complained with right upper quadrant abdominal pain which was probably unrelated to the disease, given the relatively small diameter of the lesions and the absence of Glisson’s capsule involvement. Currently, there is no report of symptomatic cases or of disease-related complications, suggesting that HSVN may represent an indolent disease with a slow growth rate. However, since data about the malignant potential are scarce, we planned half-yearly surveillance imaging with contrast-enhanced CT scan/MRI scan alternating with abdominal ultrasound.
Learning points.
Hepatic small vessel neoplasm (HSVN) is a rare vascular tumour of the liver, whose malignant potential remains yet to be fully determined.
Although it most commonly occurs as a solitary liver lesion, HSVN may appear also as multifocal liver disease. Moreover, our case describes for the first time a secondary involvement of the spleen.
Radiological appearance shares some similarities with that of benign hepatic lesions; however, contrastographic behaviour may help raise the suspicion of HSVN. Immunohistochemistry and determination of Ki-67 index are helpful tools for the differential diagnosis.
Follow-up protocols are still not standardised, as longer follow-up will be needed in order to establish the real malignant potential of this entity. Therefore, based on the evidence available so far, we recommend half-yearly surveillance imaging.
Acknowledgments
We would like to thank professor Fabio Maria Vecchio for providing us with the histological specimen.
Footnotes
Contributors: Conceptualisation and investigation: CMC. Data curation and metholodogy: CMC, FM and MCG. Writing: CMC and FM. Supervision: MDS. All authors acquired data, revised and approved the final version of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
References
- 1.Leon M, Chavez L, Surani S. Hepatic hemangioma: what internists need to know. World J Gastroenterol 2020;26:11–20. 10.3748/wjg.v26.i1.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bajenaru N, Balaban V, Săvulescu F, et al. Hepatic hemangioma -review-. J Med Life 2015;8 Spec Issue:4–11. [PMC free article] [PubMed] [Google Scholar]
- 3.Ishak KG, Sesterhenn IA, Goodman ZD, et al. Epithelioid hemangioendothelioma of the liver: a clinicopathologic and follow-up study of 32 cases. Hum Pathol 1984;15:839–52. 10.1016/S0046-8177(84)80145-8 [DOI] [PubMed] [Google Scholar]
- 4.Lazăr DC, Avram MF, Romoșan I, et al. Malignant hepatic vascular tumors in adults: characteristics, diagnostic difficulties and current management. World J Clin Oncol 2019;10:110–35. 10.5306/wjco.v10.i3.110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gill RM, Buelow B, Mather C, et al. Hepatic small vessel neoplasm, a rare infiltrative vascular neoplasm of uncertain malignant potential. Hum Pathol 2016;54:143–51. 10.1016/j.humpath.2016.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paisant A, Bellal S, Lebigot J, et al. Imaging features of hepatic small vessel neoplasm: case series. Hepatology 2021;74:2894–6. 10.1002/hep.31779 [DOI] [PubMed] [Google Scholar]
- 7.Joseph NM, Brunt EM, Marginean C, et al. Frequent GNAQ and GNA14 mutations in hepatic small vessel neoplasm. Am J Surg Pathol 2018;42:1201–7. 10.1097/PAS.0000000000001110 [DOI] [PubMed] [Google Scholar]
- 8.Rangaswamy B, Minervini M, Tublin M, et al. Imaging and pathologic findings of hepatic small vessel hemangioma. Curr Probl Diagn Radiol 2019;48:626–8. 10.1067/j.cpradiol.2018.02.006 [DOI] [PubMed] [Google Scholar]
- 9.Koschny R, Allgäuer M, Pfeiffenberger J, et al. Case report: a rare cause of a hypervascular nodule in a noncirrhotic liver. Z Gastroenterol 2019;57:57–60. 10.1055/a-0755-2478 [DOI] [PubMed] [Google Scholar]
- 10.Walcott-Sapp S, Tang E, Kakar S, et al. Resection of the largest reported hepatic small vessel neoplasm. Hum Pathol 2018;78:159–62. 10.1016/j.humpath.2018.01.013 [DOI] [PubMed] [Google Scholar]
- 11.Mulholland P, Goh IY, Sokolova A, et al. Hepatic small vessel neoplasm case report: a surveillance conundrum. Int J Surg Case Rep 2021;81:105742. 10.1016/j.ijscr.2021.105742 [DOI] [PMC free article] [PubMed] [Google Scholar]