Abstract
Salter osteotomy is widely used to improve acetabular coverage in the treatment of developmental dysplasia of the hip. Herein we describe angulated Salter osteotomy (ASO) as the modified Salter osteotomy, which creates a two-point contact between the proximal and distal fragments and better stabilizes the fixation of the fragments. We reported our results of ASO and compared it with that of Salter osteotomy performed previously by us. We retrospectively reviewed 41 unilateral hips that underwent ASO, with no other accompanying procedures, between 2012 and 2018. We investigated the radiographic measurements included the preoperative values of the acetabular index and center-edge angle (CEA), immediate postoperative values of distance d (lateral displacement of the distal fragment), lateral rotation angle (LRA), the ratio of the obturator height (ROH), pelvic height increase percentage (PHIP) and the values of acetabular index and CEA during the last follow-up. Measurements were compared with 20 unilateral hips that underwent Salter osteotomy. The mean age at the time of surgery was 5.4 years, and the mean follow-up duration was 3.3 years. Immediately after surgery, the mean distance d, LRA, ROH and PHIP were 8 mm, 19°, 70 and 1%, respectively. The last follow-up values of acetabular index and CEA significantly improved from the preoperative values by 18° and 21°, respectively. Patients treated with ASO showed significantly larger distance d, more improvement in CEA, and lesser PHIP than those treated with Salter osteotomy. The short-term outcomes of ASO are favorable. ASO was as effective as or better than Salter osteotomy in pulling out and stabilizing the distal fragment anterolaterally. ASO prevents elongation of the ilium, which causes pelvic obliquity.
Keywords: beta-tricalcium phosphate, developmental dysplasia of the hip, Salter osteotomy
Introduction
Salter osteotomy [1] is widely used for treating acetabular dysplasia and residual subluxation in developmental dysplasia of the hip (DDH). Salter osteotomy uses complete transiliac osteotomy to redirect the entire acetabulum. Good results have been reported so far with Salter osteotomy [1,2], but technical errors such as medial or posterior displacement of the distal fragment and slipping of the bone graft have led to less than ideal correction and inadequate acetabular coverage [3–6]. By its nature, Salter osteotomy increases the pelvic length and adds length to the ipsilateral limb depending on the size of the triangular bone graft used after the osteotomy site is opened (Fig. 1) [3,6–8]. Several authors developed modifications of Salter osteotomy to overcome these problems [3,5,6,9,10].
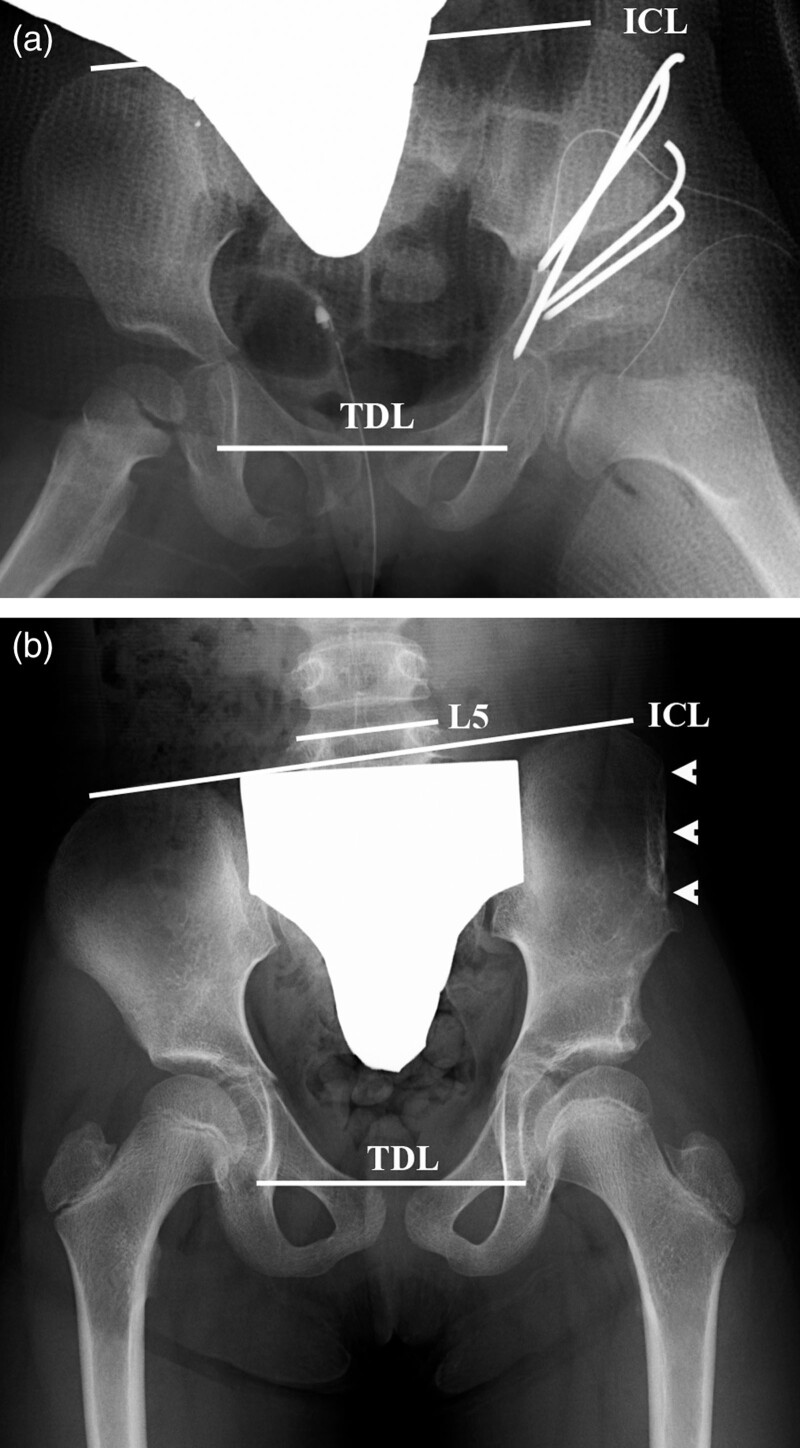
Fig. 1.
Immediate (a) and 4.5-year (b) postoperative anteroposterior radiographs after Salter osteotomy. (a) Salter osteotomy is performed on the left hip at 4.4 years of age. (b) The cephalad end L5 vertebral line (L5) and iliac crest line are greatly inclined towards the tear drop line. SO increases the pelvic length and causes pelvic obliquity and scoliosis. Deformity of the iliac wing is observed at the bone-graft harvesting site (arrowhead). ICL, iliac crest line; TDL, tear drop line.
In 2012, we first proposed the angulated Salter osteotomy (ASO) (Figs. 2 and 3) as the modified Salter osteotomy to avoid the elongation of the ilium. In ASO, a small quadrangular prism-shaped beta-tricalcium phosphate (ß-TCP) bone-graft substitute is used instead of an autologous iliac bone graft, which causes cosmetic problems due to the deformity of the iliac wing.
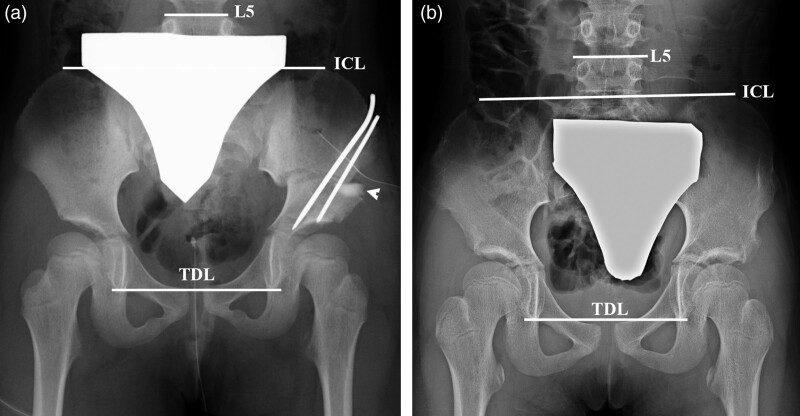
Fig. 2.
Immediate (a) and 4.3-year (b) postoperative anteroposterior radiographs after angulated Salter osteotomy (ASO). (a) ASO is performed on the left hip at 5.5 years of age. A beta-tricalcium phosphate bone-graft substitute (arrowhead) is placed between the fragments. (b) The cephalad end L5 vertebral line (L5) and iliac crest line are much less inclined towards the tear drop line as compared to that after SO. The ß-TCP bone-graft substitute is completely reabsorbed. ICL, iliac crest line; TDL, tear drop line.
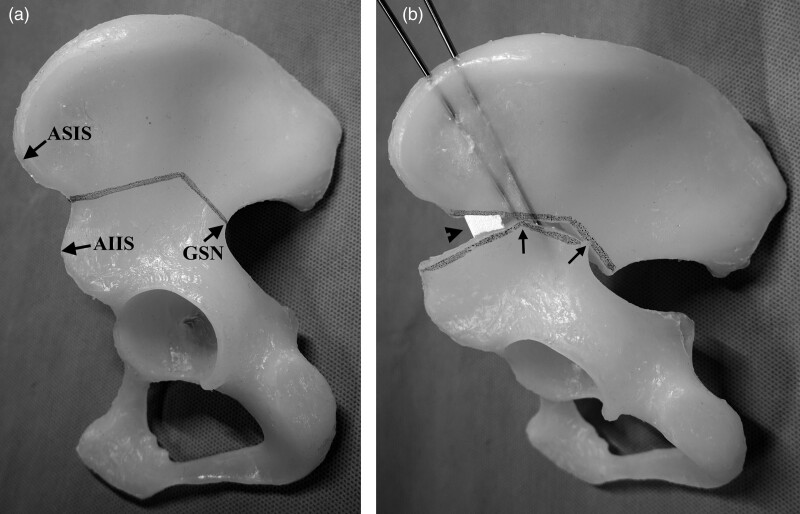
Fig. 3.
Angulated Salter osteotomy. (a) The first osteotomy line is raised 30° or more proximal to the straight osteotomy line of the Salter osteotomy. The apex of the osteotomy is set at a depth of approximately one-third of the ilium. (b) Angular osteotomy creates a 2-point contact (arrows) between the proximal and distal fragments. A beta-tricalcium phosphate bone-graft substitute (arrowhead) is placed between the fragments. AIIS, anterior inferior iliac spine; ASIS: anterior superior iliac spine; GSN, greater sciatic notch.
We reported our results of ASO and compared it with that of Salter osteotomy performed previously by us.
Patients and methods
We performed ASO for the treatment of 60 hips of patients with DDH in our hospital from January 2012 to December 2018. Our study included 41 unilateral hips (10 right and 31 left hips of 2 boys and 39 girls) that were followed up for at least over a year after surgery and had not undergone any other concomitant procedures. The initial reduction methods used were Pavlik harness (11 hips), gradual traction followed by closed reduction (24 hips) and open reduction after unsuccessful nonoperative treatment (2 hips). The remaining four hips had acetabular dysplasia without dislocation.
Surgical procedure for angulated Salter osteotomy
A 4-cm skin incision was marked 3 cm proximal and 1 cm distal to the superior anterior iliac spine. Sartorius muscle was detached from the superior anterior iliac spine, reflected, and later reattached to the original portion. We combined the iliopsoas tenotomy in Salter osteotomy according to the technique described by Salter, but we omitted the iliopsoas tenotomy in the present ASO. The greater sciatic notch was exposed subperiosteally. A Gigli saw was passed beneath the greater sciatic notch and used for iliac osteotomy.
In Salter osteotomy, the ilium was cut in a straight line from the greater sciatic notch to the point between the anterior superior iliac spine and anterior inferior iliac spine. Meanwhile, in ASO, the first osteotomy line was raised ≥30° proximal to the straight osteotomy line of the Salter osteotomy (Fig. 3a). This osteotomy angle usually amounts to 30° and is set to >30° if more rotation is needed. The apex of the osteotomy was set at a depth of approximately one-third of the ilium. An angulated osteotomy was performed distal to the point between the anterior superior iliac spine and anterior inferior iliac spine from the apex. After the osteotomy, the distal fragment was rotated anteriorly and laterally as performed in Salter osteotomy. Unlike Salter osteotomy, where the antero-laterally displaced distal bone fragment contacts the proximal bone fragment at one point, ASO creates a two-point contact between the proximal and distal fragments and improves the stability of the fixation of the fragments (Fig. 3b).
The fragments were fixed with two or three 2.4-mm nonthreaded Kirschner wires. The gap between the proximal and distal fragments was smaller in ASO than that in Salter osteotomy, and we did not use any bone grafts in three hips. In the other 38 hips, we placed a small quadrangular prism-shaped ß-TCP bone-graft substitute (8–10 mm long, 5–6 mm high and 10 mm wide). The ß-TCP bone-graft substitute was placed after Kirschner wire fixation because the Kirschner wires could not be inserted into the block.
We investigated the patient’s age at the time of surgery, duration of follow-up and time required for bone union (time until removal of internal Kirschner wire fixation).
We evaluated the anteroposterior radiographs of the hip taken in the supine position preoperatively, immediately after surgery and during the last follow-up. The acetabular index and the center-edge angle (CEA) were measured preoperatively and during the last follow-up. The effectiveness of surgery was evaluated by a decrease in acetabular index and an increase in CEA after surgery. The movement of the distal fragment was assessed by measuring distance d, lateral rotation angle (LRA), and the ratio of the obturator heights (ROH) immediately after surgery as described by Kitoh et al. [4] (Fig. 4). Distance d, the distance between the distal inner edge of the proximal bone fragment and the proximal inner edge of the distal bone fragment, represents the lateral displacement of the distal bone fragment. LRA, an open-wedge angle between the proximal and distal bone fragments, represents the abduction angle of inclination of the distal bone fragment. ROH, the ratio of the maximum heights of the obturator foramen on the operated hip relative to that on the contralateral hip, represents the anterolateral rotation of the distal fragment. The elongation of the ilium and pelvic obliquity was assessed by measuring the pelvic height increase percentage (PHIP) immediately after surgery as described by Wang et al. [8] (Fig. 4). PHIP was calculated as the percentage of the difference in pelvic height between the operated and contralateral hips divided by the pelvic height of the contralateral hip.
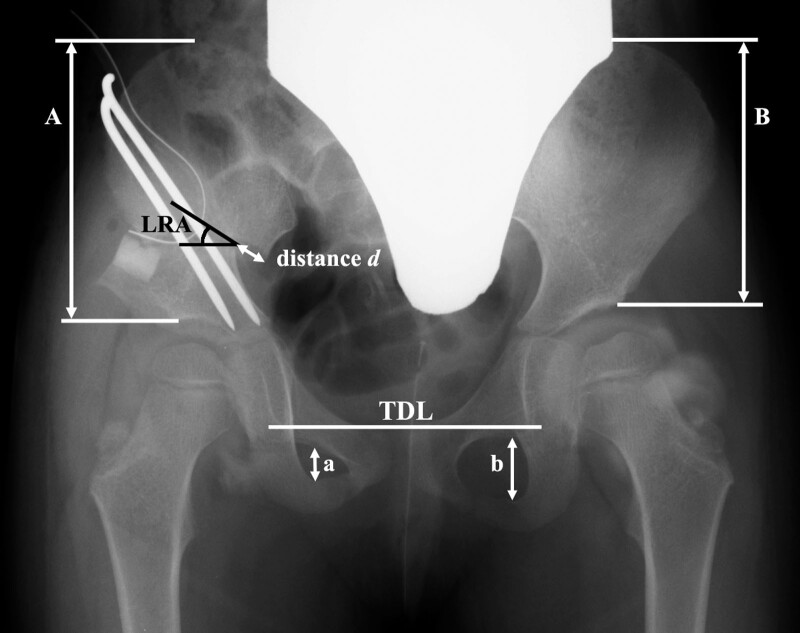
Fig. 4.
Radiographic measurements on immediate postoperative anteroposterior radiograph after angulated Salter osteotomy. Distance d (mm) represents the lateral displacement of distal fragment. Lateral rotation angle (°) is the open-wedge angle between the proximal and distal bone fragments. The ratio of the obturator height (%) is the maximum height of the obturator foramen on the operative side (a) relative to that on the contralateral side (b), calculated as a/b × 100. Parallel lines are drawn to the tear drop line at the superior margin of the iliac crest and the acetabular roof. The pelvic height increase percentage (%) is the pelvic height on the operative side (a) relative to that on the contralateral side (b), calculated as (A–B)/B × 100. LRA, lateral rotation angle; TDL, tear drop line.
For comparison with the ASO group, we analyzed the cases of an additional 20 unilateral hips (8 right hips and 12 left hips) of 2 boys and 18 girls who previously underwent Salter osteotomy without any concomitant procedures and without any major complications at our hospital and whose age at the time of surgery was in the same range as that of the ASO group. A large autologous iliac bone graft was harvested from the ipsilateral iliac wing and used to fill the anterior gap. The proximal and distal fragments and the bone graft were fixed with four nonthreaded Kirschner wires. Similar to the ASO group, we investigated the age at the time of surgery, duration of follow-up and time required for bone union in the Salter osteotomy group. Furthermore, the radiographic measurements included acetabular index and CEA preoperatively, distance d, LRA, ROH and PHIP immediately after surgery, and acetabular index and CEA values 2- to 4-years postoperatively.
The results were analyzed using the independent-sample t-test and paired t-test. Independent-sample t-tests were used to compare the age at the time of surgery, duration of follow-up and time required for bone union between the ASO and Salter osteotomy groups. Additionally, non-paired t-tests were used to compare the preoperative values and improvement in acetabular index and CEA, and immediate postoperative values of distance d, LRA, ROH and PHIP between both groups. Paired t-tests were used to compare the preoperative and last follow-up values of acetabular index and CEA in the ASO group, and the preoperative and 2- to 4-year postoperative values for the same measures in the Salter osteotomy group. Statistical analysis was performed using BellCurve for Excel (Social Survey Research Information Co., Ltd, Tokyo, Japan), and statistical significance was set at P value <0.05.
Results
In the ASO group, the mean age at the time of surgery was 5.4 years (range, 4.2–7.9 years) and the mean duration of follow-up was 3.3 years (range, 1.1–6.7 years). The mean time required for the bone union was 61 days (range, 56–74 days). In one of the three hips in which we did not use any bone grafts, the distal fragment was displaced, and the fragments were re-fixed 1 week after the initial surgery, even though the patient had a hyperactivity disorder. None of the 41 hips have developed avascular necrosis or chondrolysis after ASO. During the last follow-up, none of the patients had any limitation of flexion and were able to deep-squat without pain.
The preoperative values of acetabular index and CEA represented as mean ± standard deviations were 31° ± 3° (range, 25–38°) and 3° ± 3° (range, −8 to 10°), respectively. The mean radiographic immediate postoperative measurements were as follows: distance d, 8 ± 2 mm (range, 3–13 mm); LRA, 19° ± 4° (range, 9–27°); ROH 70% ± 12% (range, 35–89%) and PHIP 1% ± 3% (range, −4 to 7%) (Table 1). The mean acetabular index and CEA values during the last follow-up were 12° ± 4° (range, 5–23°) and 25° ± 6° (range, 9–35°), respectively. The mean last follow-up values of acetabular index and CEA significantly improved as compared to the mean preoperative values by 18° ± 4° (range, 9–29°) (P < 0.001) and 21° ± 6° (range, 12–34°) (P < 0.001), respectively (Table 2).
Table 1.
Comparison of radiographic immediate postoperative values between angulated Salter osteotomy and Salter osteotomy
| ASO | Salter osteotomy | Significance | |
|---|---|---|---|
| Distance ‘d’ (mm) | 8 ± 2 (3–13) | 3 ± 1 (0–7) | P < 0.001a |
| LRA (°) | 19 ± 4 (9–27) | 19 ± 3 (14–25) | P = 0.588 |
| ROH (%) | 70 ± 12 (35–89) | 66 ± 12 (38–85) | P = 0.264 |
| PHIP (%) | 1 ± 3 (−4 to 7) | 7 ± 3 (3–14) | P < 0.001a |
The values are represented as mean ± SD, with the range in parentheses.
ASO, angulated Salter osteotomy; LRA, lateral rotation angle; PHIP, pelvic height increase percentage; ROH, ratio of the obturator heights.
Statistically significant.
Table 2.
Comparison of the radiographic improvement between angulated Salter osteotomy and Salter osteotomy
| ASO | Salter osteotomy | Significance | |
|---|---|---|---|
| Acetabular index (°) | 18 ± 4 (9–29) | 15 ± 4 (5–25) | P = 0.075 |
| CEA (°) | 21 ± 6 (12–34) | 17 ± 5 (6–27) | P = 0.003a |
The values are represented as mean ± SD, with the range in parentheses.
ASO, angulated Salter osteotomy; CEA, center-edge angle
Statistically significant.
In the Salter osteotomy group, the mean age at the time of surgery was 5.4 years (range, 2.9–6.8 years) and the mean duration of follow-up was 2.9 years (range, 2.3–3.5 years). The mean time required for the bone union was 61 days (range, 54–77 days). The mean preoperative values of acetabular index and CEA were 32° ± 4° (range, 24–45°) and 4° ± 3° (range, −2 to 12°), respectively. The mean radiographic immediate postoperative measurements were as follows: distance d, 3 ± 1 mm (range, 0–7 mm); LRA, 19° ± 3° (range, 14–25°); ROH 66% ± 12% (range, 38–85%); and PHIP 7% ± 3% (range, 3–14%). The mean 2- to 4-year postoperative values of acetabular index and CEA were 16° ± 4° (range, 6–25°) and 21° ± 6° (range, 8–33°), respectively. The mean 2- to 4-year postoperative values of acetabular index and CEA significantly improved as compared to the preoperative values by 15° ± 4° (range, 5–25°) (P < 0.001) and 17° ± 5° (range, 6–27°) (P < 0.001), respectively.
The age at the time of surgery, duration of follow-up and time required for bone union were not significantly different between the ASO and Salter osteotomy groups (P = 0.937, P = 0.131 and P = 0.733, respectively).
Preoperative acetabular index and CEA values were not significantly different between the ASO and Salter osteotomy groups (P = 0.144 and P = 0.410, respectively). Immediately after the surgeries, the distance d in the ASO group was significantly greater than that of the Salter osteotomy group (P < 0.001), whereas the LRA and ROH values were not significantly different between the ASO and Salter osteotomy groups (P = 0.588 and P = 0.264, respectively). The PHIP in the ASO group was significantly smaller than that in the Salter osteotomy group (P < 0.001). During the last follow-up, there were no significant differences between the ASO and Salter osteotomy groups with respect to the improvement in the acetabular index (P = 0.075), whereas the improvement in CEA was significantly more in the former than the latter (P = 0.003).
Discussion
Several modifications of Salter osteotomy have been reported. Kalamchi removed a triangular bone wedge posteriorly from the proximal fragment and engaged the distal fragment into the created triangular slot to increase stability and prevent the elongation of the ilium [3]. Synder et al. [6] also reported successful results with this modification. Eren et al. [9] performed an oblique straight osteotomy and did not use internal pin fixations when the bone graft was stable. Kremli [5] used biodegradable polyglycolic acid pins for fixing the bone graft and eliminated the need for a second surgery for pin removal. Yoon et al. [10] changed the direction of the osteotomy by cutting the anterior half of the ilium in an oblique direction at 45º. A large autologous iliac bone graft was harvested from the ipsilateral iliac wing and used to fill the anterior gap in these studies.
We used an angular osteotomy in ASO by applying the angular iliac osteotomy used in the single-incision extraperiosteal triple osteotomy [11]. The angular osteotomy creates a two-point contact between the proximal and distal fragments, and it stabilizes the osteotomy site better than a one-point contact with the straight osteotomy in Salter osteotomy (Fig. 3b). The gaps between the proximal and distal fragments were smaller in the present ASO cases than that in Salter osteotomy, and the fragments were fixed with two or three 2.4-mm nonthreaded Kirschner wires without placing a bone graft.
In one of the three hips in which we did not use any bone grafts, the distal fragment was displaced and re-fixed, even though the patient had a hyperactivity disorder. Subsequently, a small quadrangular prism-shaped ß-TCP bone-graft substitute was placed between the fragments after Kirschner wire fixation to improve the stability and prevent loss of correction. Even with the use of a β-TCP bone-graft substitute in the present ASO group, the time required for the bone union (i.e. the time until the removal of the internal Kirschner wire fixation) did not differ significantly between the ASO and Salter osteotomy groups.
In the Salter osteotomy group, the bone graft was harvested from the ipsilateral iliac wing, which caused the deformity of the iliac wing postoperatively (Fig. 1b). The use of a β-TCP bone-graft substitute has the advantage of avoiding postoperative deformity of the iliac wing. Morita et al. [7] started a similar angular osteotomy with our technique from 2014 and reported successful short-term outcomes. They did not use any bone grafts, but they used one 3-mm threaded Kirschner wire and two or three nonthreaded Kirschner wires to fix the fragments. Threaded Kirschner wire fixation could obviate the need for the use of a β-TCP bone-graft substitute at the osteotomy site in ASO.
We combined the iliopsoas tenotomy in Salter osteotomy according to the technique described by Salter, but we omitted the iliopsoas tenotomy in the present ASO. Vengust et al. [12] suggested that the acetabulum was not corrected to the maximum degree to eliminate the increase in the hip joint pressure when leaving the iliopsoas muscle intact. However, we did not have difficulty in obtaining satisfactory correction in ASO, and none of the patients has developed avascular necrosis or chondrolysis after ASO, which is probably because ASO prevents the elongation of the ilium. The results of our study demonstrated that a tenotomy of the iliopsoas muscle is unnecessary in ASO.
In their study of 90 hips treated with Salter osteotomy, Kitoh et al. [4] reported that the distance d and the LRA had a strong positive correlation, whereas the ROH had a negative correlation with the improvement in the acetabular index and CEA values. Herein we observed that the LRA and ROH values and the improvement in acetabular index were not significantly different between the ASO and Salter osteotomy groups, and the values of distance d and the improvement of CEA in the ASO group were significantly greater than those of the Salter osteotomy group.
The importance of the amount of lateral displacement of the distal fragment in Salter osteotomy is well known. Salter and Dubos [2] reported that it is important to avoid posterior or medial displacement of the distal fragment. Kaneko et al. [13] noted that their cases with poor outcomes following Salter osteotomy had a significantly smaller distance d; in contrast, all hips with a d ≥3.5 mm had a good outcome at skeletal maturity, and Kaneko et al. thus concluded that sufficient lateral displacement of the distal bone fragment was a factor related to good long-term outcomes. The mean value of distance d in our Salter osteotomy group was 3 mm, which is similar to 4 mm in the study conducted by Kitoh et al. [4]. The mean value of distance d in the ASO group was 8 mm, which is significantly larger than the 3 mm of the Salter osteotomy group in our present study. ASO was as effective as or better than Salter osteotomy in pulling out and stabilizing the distal fragment anterolaterally.
The mean postoperative PHIP value in our ASO group was only 1%, which is significantly smaller than the 7% of the Salter osteotomy group. ASO was effective in preventing the elongation of the ilium (Fig. 2).
The results of this study demonstrate that the short-term outcomes of ASO are favorable. As noted above, ASO creates a two-point contact between the proximal and distal fragments and improves the stability of the fixation of the fragments, and it prevents elongation of the ilium, which causes pelvic obliquity. The use of a β-TCP bone-graft substitute also prevents cosmetic problems due to the deformity of the iliac wing.
This study has several limitations, the most important one being that it was a retrospective analysis. The eras of the surgeries differed because Salter osteotomy was changed to ASO, and there were different levels of surgical proficiency in each group. The number of patients in each group was small, and we did not have a long-term follow-up, especially considering the changing nature of the developing acetabulum, which does not fully develop until early adulthood. Considering our present findings, ASO has the potential to show long-term results that are as good as those reported with Salter osteotomy, but further studies are necessary to clarify the long-term results of ASO with larger sample size.
Acknowledgements
None of the authors received financial support for this study.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Salter RB. Innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. J Bone Joint Surg Br 1961; 43-B:518–539. [PubMed] [Google Scholar]
- 2.Salter RB, Dubos JP. The first fifteen years’ personal experience with innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. Clin Orthop Relat Res 1974; 98:72–103. [DOI] [PubMed] [Google Scholar]
- 3.Kalamchi A. Modified Salter osteotomy. J Bone Joint Surg Am 1982; 64:183–187. [PubMed] [Google Scholar]
- 4.Kitoh H, Kaneko H, Ishiguro N. Radiographic analysis of movements of the acetabulum and the femoral head after Salter innominate osteotomy. J Pediatr Orthop 2009; 29:879–884. [DOI] [PubMed] [Google Scholar]
- 5.Kremli M. Bioabsorbable rods in Salter’s osteotomy. J Pediatr Orthop B 2002; 11:104–109. [DOI] [PubMed] [Google Scholar]
- 6.Synder M, Forlin E, Xin S, Bowen JR. Results of the Kalamchi modification of salter osteotomy in the treatment of developmental dysplasia of the hip. J Pediatr Orthop 1992; 12:449–453. [DOI] [PubMed] [Google Scholar]
- 7.Morita M, Kamegaya M, Takahashi D, Kamada H, Tsukagoshi Y, Tomaru Y. Proposal of a new type of innominate osteotomy without the use of bone graft in children: a Preliminary Study. JB JS Open Access 2019; 4:e0016.1–e0016.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang CW, Wang TM, Wu KW, Huang SC, Kuo KN. The comparative, long-term effect of the Salter osteotomy and Pemberton acetabuloplasty on pelvic height, scoliosis and functional outcome. Bone Joint J 2016; 98-B:1145–1150. [DOI] [PubMed] [Google Scholar]
- 9.Eren A, Pekmezci M, Demirkiran G, Cakar M, Guven M, Yazici M. Modified Salter osteotomy for the treatment of developmental dysplasia of the hip: description of a new technique that eliminated the use of pins for internal fixation. J Bone Joint Surg Br 2007; 89:1375–1378. [DOI] [PubMed] [Google Scholar]
- 10.Yoon TR, Rowe SM, Chung JY, Song EK, Mulyadi D, Anwar IB. A new innominate osteotomy in Perthes’ disease. J Pediatr Orthop 2003; 23:363–367. [PubMed] [Google Scholar]
- 11.Sokolovskii AM. Triple osteotomy of the pelvis. Ortop Travmatol Protez 1984; 4:54–58. [PubMed] [Google Scholar]
- 12.Vengust R, Daniel M, Antolic V, Zupanc O, Iglic A, Kralj-Iglic V. Biomechanical evaluation of hip joint after Salter innominate osteotomy: a long-term follow-up study. Arch Orthop Trauma Surg 2001; 121:511–516. [DOI] [PubMed] [Google Scholar]
- 13.Kaneko H, Kitoh H, Mishima K, Matsushita M, Kadono I, Ishiguro N, Hattori T. Factors associated with an unfavourable outcome after Salter innominate osteotomy in patients with unilateral developmental dysplasia of the hip: does occult dysplasia of the contralateral hip affect the outcome? Bone Joint J 2014; 96-B:1419–1423. [DOI] [PubMed] [Google Scholar]