Abstract
Background
Doctors’ organisations in the UK have reported worrying levels of work-related stress and burnout in the GP workforce for some time, and the COVID-19 pandemic has presented clear new challenges.
Aim
To synthesise international evidence exploring the impact of COVID-19 on primary care doctors’ mental health and wellbeing, and identify risk factors associated with their psychological wellbeing during this time.
Design and setting
Mixed-methods systematic review.
Method
Six bibliographic databases, Google Scholar, and MedRxiv were searched on 19 November 2020 and 3 June 2021 to identify studies of GP psychological wellbeing during the pandemic. Reference checking was also conducted. Two reviewers selected studies, extracted data, and assessed the quality of studies using standardised tools. Heterogeneity in outcomes, setting, and design prohibited statistical pooling; studies were combined using a convergent integrated thematic synthesis.
Results
Thirty-one studies were included. Multiple sources of stress were identified including changed working practices; risk, exposure, and inadequate personal protective equipment (PPE); information overload; pandemic preparedness; and cohesion across sectors. Studies demonstrated an impact on psychological wellbeing, with some GPs experiencing stress, burnout, anxiety, depression, fear of COVID-19, lower job satisfaction, and physical symptoms. Studies reported gender and age differences: women GPs had poorer psychological outcomes across all domains, and older GPs reported greater stress and burnout. Use of outcome measures and reporting practice varied greatly.
Conclusion
This review of international evidence demonstrates that the COVID-19 pandemic has adversely affected GPs’ wellbeing around the world. Further research could explore gender and age differences, identifying interventions targeted to these groups.
Keywords: coronavirus, COVID-19, general practice, mental health, systematic review, wellbeing
INTRODUCTION
Doctor burnout has been described as a global crisis1 affecting the quality of patient care2–4 and the sustainability of healthcare systems.5 International literature highlights growing problems with chronic stress and burnout that threatened the mental health of doctors working in primary care settings before the COVID-19 pandemic.6–12 In the UK, 37% of GPs surveyed in 2019 reported an intention to leave direct patient care,13 and researchers have estimated a shortage of 2500 GPs, projected to increase to 7000 within 5 years if current trends continue.14
The COVID-19 pandemic has presented additional challenges for primary care doctors around the world, including rapid change, risks of infection, remote working, pent-up demand, reductions in face-to-face patient care, and vaccination delivery. Research from earlier epidemics and emerging during the COVID-19 pandemic demonstrates a negative impact on clinician psychological wellbeing.15–19 A 40% increased use of mental health support services has been reported during the pandemic (across UK health professional groups).20
While there has been a tendency for research to focus on hospital roles,21 there is now a need to synthesise evidence and explore factors associated with primary care doctors’ mental health and wellbeing during the pandemic.
METHOD
Cochrane guidance for conducting systematic reviews22 was followed and the study was registered and a protocol published (PROSPERO ID: CRD42020225680).23 The PRISMA checklist24 was used to ensure the transparency of reporting.
Search strategy
Six bibliographic databases (MEDLINE, Embase, PsycINFO, Science Citation Index, Social Science Citation Index, and Emerging Sources) were searched for GP wellbeing during the COVID-19 pandemic. Owing to the current nature of the topic, Google Scholar and MedRxiv, a preprint service for health research, were also searched (see Supplementary Appendix S1 for full searches). No date or language limits were applied at the search stage. A date limit (2019 onwards) was applied once the records were entered into Endnote (version 20) to capture studies measuring outcomes during the pandemic. Reference lists of included studies were also searched. The initial search was undertaken on 19 November 2020; this was updated on 3 June 2021.
Inclusion criteria
Studies in any country examining the impact of the COVID-19 pandemic on measures of primary care doctors’ psychological wellbeing, stress, and burnout, with absenteeism and markers of workforce retention as secondary outcomes, were included. Studies solely exploring doctors’ infection rates were excluded. International variations in terminology, for example, doctors working in general practice/family practice/primary care were used; for simplicity, in this article all are referred to as ‘GPs’. Non-English language studies and those including multiple health professional groups that did not present the results for GPs separately were excluded. Searches were not limited by study design in this mixed-methods systematic review, but only empirical research was included; editorials and purely descriptive articles were excluded. Studies rated as high risk of bias were excluded from the synthesis.
How this fits in
| Many GPs have reported stress and burnout over recent years, which is potentially damaging not just to doctors themselves but also to patients and healthcare systems. The COVID-19 pandemic has presented new challenges and there is a need to evaluate the impact on GP wellbeing. This review synthesises the international evidence base exploring primary care doctors’ psychological wellbeing during the pandemic. Studies have highlighted multiple sources of stress during this time and report experiences of stress, burnout, anxiety, depression, fear of COVID-19, reduced job satisfaction, and physical symptoms. Gender and age differences may warrant further research to identify interventions targeted to the needs of specific groups. |
Selection of studies
The results of each search were entered into an Endnote Library and duplicates removed. Two independent reviewers screened resulting records using titles and abstracts. Two of four reviewers screened the full text of all studies deemed potentially relevant and any disagreements were resolved by a third reviewer.
Data extraction
One of three reviewers extracted data using a pre-piloted data extraction form, cross-checking a 20% sample to ensure consistency. Information was extracted regarding study design, sample size, sample characteristics, and primary and secondary outcomes.
Quality assessment
The quality of identified reviews was assessed using the Joanna Briggs Institute (JBI) Checklist for Analytical Cross Sectional Studies25 and the Critical Appraisal Skills Programme (CASP) quality checklist26 for observational and qualitative studies. Two researchers independently quality assessed the included studies, with disagreements resolved by a third reviewer. Studies were excluded if ≥4 categories were rated as inadequate on the JBI tool25 or if qualitative studies were rated as being ‘invaluable’ using the CASP tool26 because of significant issues in the design and conduct of the study.
Data synthesis
Pooled analysis (random effects) was used to summarise age and gender data across studies. Where age groups were reported, the average age was estimated using the midpoint and frequency of the age groups. Data did not meet the requirements for statistical pooling of outcomes because of heterogeneity in outcome measures, study designs, and healthcare settings.
As this mixed-methods systematic review included both quantitative and qualitative study designs covering broadly similar topics, a convergent integrated approach was undertaken based on the JBI guidance for mixed-methods systematic reviews.27 This involved a form of narrative synthesis whereby quantitative data are described alongside qualitative findings under common themes or categories.27 NVivo (version 12) software was used to manage and sort data, following a process of thematic qualitative synthesis that moves from initial ‘free coding’ through to descriptive and then more analytical themes.28 This process was iterative, with codes and themes refined and developed throughout the analysis process, through consultation among the wider research team.
RESULTS
Search results
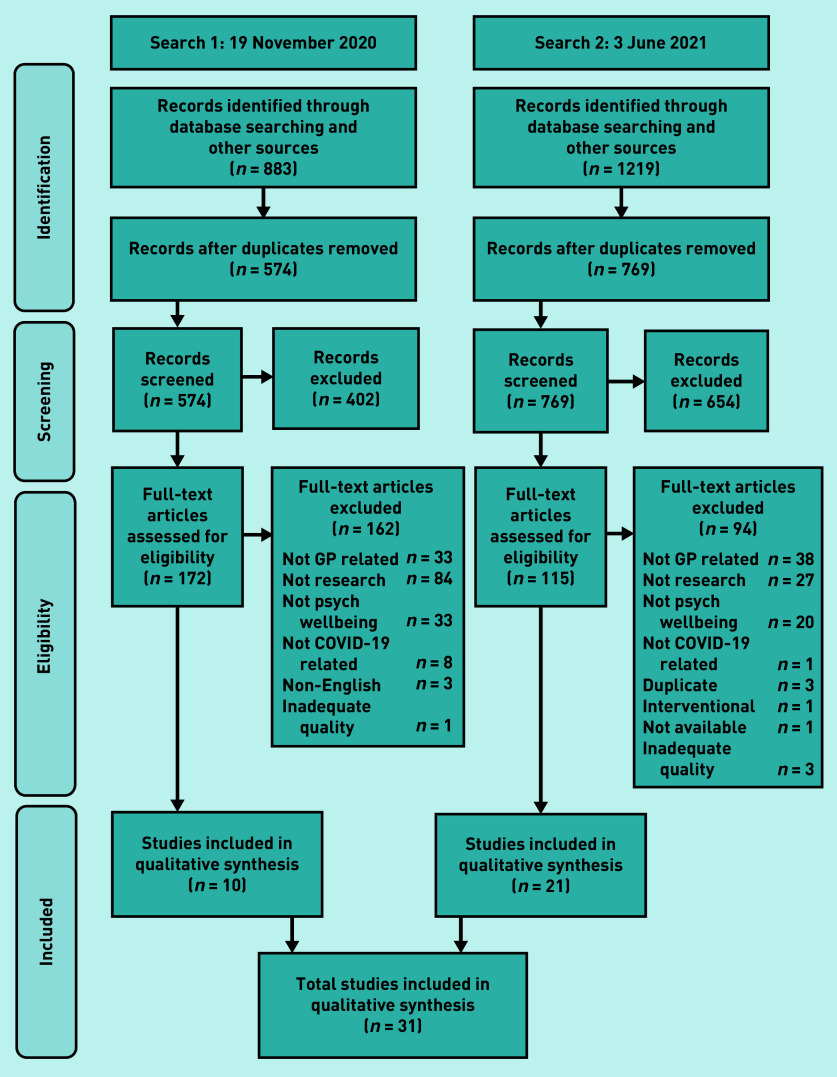
In total, 2102 studies were retrieved from databases and hand searching. There were 759 duplicates that were removed, and 1056 studies were excluded by screening the titles and abstracts. This resulted in 287 full texts being screened and 31 studies29–59 being included overall (Figure 1).
Figure 1.
Flow diagram for included studies. Psych = psychological.
Description of studies
Characteristics of the included studies are presented in Supplementary Table S1. Studies were dispersed geographically, with the largest numbers undertaken in Italy32,42,46,52 and China35,50,51,59 (Table 1).
Table 1.
Summary characteristics of studies
| Characteristic | n |
|---|---|
| Location of study | |
| Italy | 4 |
| China | 4 |
| Singapore | 3 |
| France | 2 |
| Colombia | 2 |
| UK | 2 |
| US | 2 |
| Australia | 1 |
| Croatia | 1 |
| Indonesia | 1 |
| Jordan | 1 |
| Oman | 1 |
| Portugal | 1 |
| Romania | 1 |
| Saudi Arabia | 1 |
| Spain | 1 |
| Turkey | 1 |
| Multiple countries | 2 |
|
| |
| Demographic, mean (95% CI), range | |
| Age, years | 42.4 (39.6 to 45.2),a 26–55 |
| Gender, % male | 41.3 (34.6 to 48.5), 15–100 |
Based on 23 studies reporting sufficient information.
There were 25 cross-sectional surveys,30–33,36–50,52,54,55,57–59 five qualitative studies,34,35,51,53,56 and one mixed survey and qualitative study.29 Several validated and some non-validated measures were used to assess outcomes. Sample sizes ranged from 86 to 1040 participants (median 330) for the studies with survey designs, and 11 to 80 for the qualitative interview studies (median 14). Demographic characteristics commonly reported by studies included age and gender (Table 1), with mixed reporting of other characteristics such as years of experience (Supplementary Table S1).
Quality assessment
The quality of included studies was generally good (Boxes 1 and 2).
Box 1.
Quality appraisal of cross-sectional surveys using the JBI toola
| Author (year) | 1. Were the criteria for inclusion in the sample clearly defined? | 2. Were the study subjects and the setting described in detail? | 5. Were confounding factors identified? | 6. Were strategies to deal with confounding factors stated? | 7. Were the outcomes measured in a valid and reliable way? | 8. Was appropriate statistical analysis used? |
|---|---|---|---|---|---|---|
| Amerio et al (2020)52 | Yes | Yes | No | No | Yes | Yes |
| Alrawashdeh et al (2021)29 | Yes | Yes | Yes | Yes | Yes | Yes |
| Baptista et al (2021)41 | Yes | Yes | No | No | Yes | Yes |
| Castelli et al (2021)46 | Yes | Yes | No | No | Yes | Yes |
| Di Monte et al (2020)42 | Yes | Yes | No | No | Yes | Yes |
| Dutour et al (2021)30 | Yes | Yes | Yes | Yes | Yes | Yes |
| Filfilan et al (2020)49 | Yes | Yes | No | No | Yes | Yes |
| Gold et al (2021)57 | Yes | No | No | No | Unclear | Yes |
| Gokdemir et al (2020)33 | No | Yes | Partly | Partly | Yes | Yes |
| Jahan et al (2021)40 | No | Yes | No | No | Yes | Yes |
| Lange et al (2022)36 | Yes | Yes | No | No | Yes | Yes |
| Lau et al (2021)31 | Yes | Yes | Yes | Yes | Unclear | Yes |
| Lau et al (2021)54 | Yes | Yes | No | No | No | Yes |
| Lee et al (2020)37 | Yes | Yes | No | No | Yes | Yes |
| Ortega-Galán et al (2020)38 | Yes | Yes | No | No | Yes | Yes |
| Monterrosa-Castro et al (2020)48 | Yes | Yes | No | No | Partly | Yes |
| Monterrosa-Castro et al (2021)44 | Yes | Yes | No | No | Yes | Yes |
| Rossi et al (2020)32 | Yes | Yes | Yes | Yes | Yes | Yes |
| Sitanggang et al (2021)43 | Yes | Yes | No | No | Yes | Yes |
| Sotomayor-Castillo et al (2021)58 | Yes | No | No | No | No | Yes |
| Stafie et al (2021)47 | Yes | Yes | No | No | Yes | Yes |
| Taş et al (2021)45 | Yes | Yes | No | No | Partly | Yes |
| Trivedi et al (2021)55 | Yes | Yes | No | No | Yes | Yes |
| Tse et al (2020)59 | No | Yes | No | No | Yes | Yes |
| Vilovic et al (2021)39 | Yes | Yes | No | No | Yes | Yes |
| Zeng et al (2021)50 | Yes | Yes | No | No | Yes | Yes |
Questions 3 and 4 on the JBI were not applicable and are excluded here. JBI = Joanna Briggs Institute.
Box 2.
Quality appraisal of qualitative studies using the CASP tool
| Author (year) | Section A: Are the results valid? | Section B: What are the results? | Section C: Will the results help locally? | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Was there a clear statement of the aims of the research? | 2. Is a qualitative methodology appropriate? | 3. Was the research design appropriate to address the aims of the research? | 4. Was the recruitment strategy appropriate to the aims of the research? | 5. Were the data collected in a way that addressed the research issue? | 6. Has the relationship between researcher and participants been adequately considered? | 7. Have ethical issues been taken into consideration? | 8. Was the data analysis sufficiently rigorous? | 9. Is there a clear statement of findings? | 10. How valuable is the research? | |
| Alrawashdeh et al (2021)29 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Valuable |
| Gomez et al (2021)34 | Yes | Yes | Yes | No | Yes | No | Yes | Yes | Yes | Valuable |
| Taylor et al (2021)53 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Valuable |
| Wanat et al (2021)56 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Valuable |
| Xu et al (2020)35 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Partly | Valuable |
| Yin et al (2021)51 | Yes | Yes | Unclear | Yes | Yes | No | Yes | Yes | Yes | Valuable |
CASP = Critical Appraisal Skills Programme.
Quality of cross-sectional surveys
Using the criteria outlined in the JBI tool,25 sampling was well defined, as were study participants and settings in most studies (Box 1). Studies reported age and gender inconsistently or lacked reporting of wider characteristics. This was more common for studies reporting GP outcomes alongside other professional groups. Most studies used objective and validated measures, although some also developed measures specifically to answer novel research questions around the impact of COVID-19,39,59 which had not been validated owing to the timeframes.
Although statistical analyses were appropriately conducted across studies, very few studies considered confounders or used strategies to deal with these. Four studies did this29–32 and one study partly explored confounders.33 Inadequacies in reporting were problematic, for example, the most commonly used measure was the Perceived Stress Scale (PSS), measured in seven studies,30,33,36–39,55 but this was poorly reported at times and different versions were used.
Quality of qualitative studies
Assessment using the CASP tool26 found all studies involving qualitative methods provided a clear statement of aims and study methodology, and the methods were deemed appropriate to address the aims of the research (Box 2). All but one study34 used suitable recruitment strategies, and all studies were rated as collecting data appropriately and conducting sufficiently rigorous analyses to address the research questions. No studies described consideration for the effect of the relationship between interviewee and researcher. There was some ethical review in all studies, although for the majority there was limited discussion of the issues considered. One qualitative study35 met the CASP quality criteria, but lacked clear information about which type of health professional the quotations related to (since multiple health professional groups were included). The study authors provided this information on request.
Thematic findings
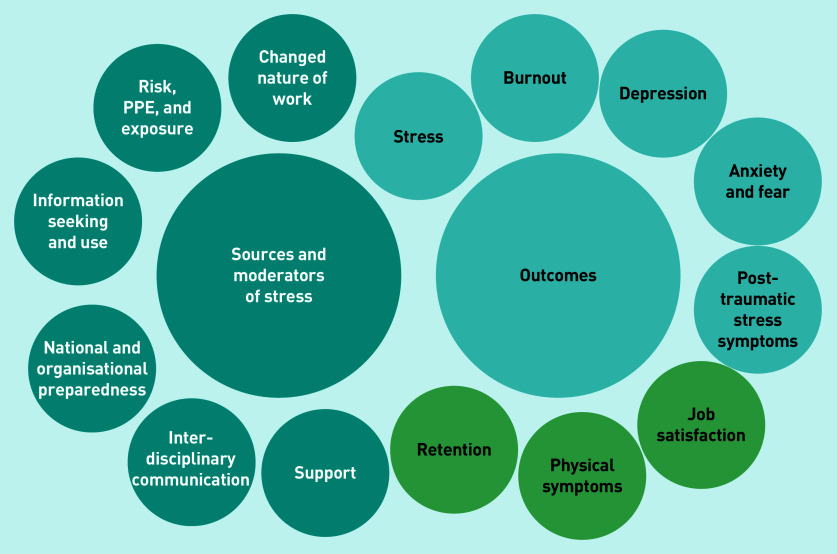
Findings were grouped into two overarching categories: 1) stressors and moderators; and 2) psychological wellbeing outcomes (Figure 2 and Supplementary Table S2).
Figure 2.
Stressors, moderators, and outcomes relating to GP wellbeing during the COVID-19 pandemic. a
a Light blue circles indicate psychological outcomes, while green circles indicate other outcomes. PPE = personal protective equipment.
Stressors and moderators
Both qualitative and quantitative studies assessed sources of stress during the pandemic and these were grouped thematically as factors associated with the changing nature and quantity of GP work, risk and exposure, information seeking and use, organisational and national preparedness, and interdisciplinary communication. Support was seen as a moderator of stress. Further descriptions can be found in Supplementary Table S2.
Psychological wellbeing outcomes
Reporting and measurement of psychological outcomes varied across studies, making comparisons across settings difficult.
Studies measuring stress placed GPs, on average, into ‘borderline’ or ‘stressed’ categories of the PSS30,36–39 and, using other stress scales, moderate-to-severe stress was reported in between 9.5% of GPs in Oman40 and 24.7% of GPs in Portugal.41 In terms of burnout, studies found the greatest difficulties related to emotional exhaustion, with 24.5% to 46.1% of GPs reporting high burnout symptoms relating to the emotional exhaustion components of the scale.36,42
Rates of anxiety ranged from 20% in Indonesia43 to 95% in Turkey and Colombia.44,45 Symptoms of depression were reported to a lesser extent, and ranged from 13% in Indonesia43 to 37% in Italy.46 Post-traumatic stress symptoms were reported in 10.6% of GPs in France,36 moderate-to-severe symptoms were reported in 45.2% of GPs in Croatia,39 and 32% of GPs in Italy presented with significant post-traumatic stress symptoms.46
Occupational groups
Among five studies of mixed groups of healthcare workers, primary care doctors reported higher levels of personal perceived stress,37,38 worse burnout scores (relating to lower ‘compassion satisfaction’ and higher ‘compassion fatigue’),38 worse depression scores,39 greater reporting of post-traumatic stress symptoms,32 and lower job satisfaction than other specialty groups.29
Gender
Seven studies report statistically significant differences in outcomes for female GPs, including higher stress levels,30,36,38,39,47 greater reporting of burden and burnout,36,41,47 greater reporting of anxiety,48 and higher mean post-traumatic stress symptom scores.36
Age
Older age was associated with higher stress levels in three studies,39,49,50 but in GPs in Colombia younger age predicted anxiety,48 and in Portugal greater levels of depression were reported in GPs aged <40 years.41 In this study of Portuguese GPs, increased length of time working as a doctor predicted higher burnout on items of the burnout scale relating to patient interactions.41
Other outcomes
Four studies explored future intentions, reporting wide variations in plans to leave medicine, which were associated with general anxiety, particularly around infection risk.30,31,48,51 Two studies report that 7% of GPs considered leaving practice,30,31 and another48 found that these intentions were associated with anxiety around protecting family members.
Ten studies explored impact on physical symptoms and general quality of life.41,44–46,48,50–53,58 GPs reported migraines and headaches, tiredness and exhaustion, sleep disorders,45,50 and increased eating, drinking, and smoking.44,48,51 More severe insomnia was associated with depressive symptoms in GPs in Italy.52
GPs in the UK with symptoms of long COVID felt ‘let down’ and expressed frustration at the lack of support and recognition for the condition.53
DISCUSSION
Summary
The COVID-19 pandemic has necessitated substantial changes in primary care around the world; GPs rapidly changed working practices and managed evolving guidelines amid uncertainty and personal risk. This review of international literature highlights the difficulties that GPs have experienced across healthcare settings during the pandemic and shows there are high levels of work-related stress and burnout.30,32,33,36–42,47,55 Rates of anxiety and depression varied considerably across international settings, as did the use of tools to measure such outcomes. Studies also lack longitudinal or ‘pre-pandemic’ comparators, which makes drawing firm conclusions regarding the impact of COVID-19 difficult.
Studies found gender differences, with female GPs reporting worse outcomes on all facets of psychological wellbeing.30,36,38,39,41,47,48 Similar findings have been reported in other physician groups in China,60 and greater job strain has been reported among female doctors in dual-doctor marriages during the pandemic.61 Experiences according to age varied across studies, with higher stress reported in older groups but more anxiety and depression in younger groups.
Studies included in this review highlight GPs’ plans to leave medicine,30,31,44 both to protect family members from risk of infection and because of the effects on their psychological wellbeing. Understanding the key sources of stress for GPs could enable an evidence-based approach to the development of future policy as the pandemic progresses, which may help to protect the future wellbeing of the workforce.
Strengths and limitations
To the authors’ knowledge, this is the first systematic review exploring GPs’ psychological wellbeing during the COVID-19 pandemic. A rigorous methodology was used, and the combination of qualitative and quantitative literature generates an in-depth understanding of stressors and outcomes. Issues faced during the first year of the pandemic may be over-represented because of time-lags in publishing studies; further research may be needed to explore later experiences. There are limitations to these findings relating to their context, for example, non-English language studies were excluded.
Although the quality of the evidence was generally good, there were some limitations in consideration of confounders and in reporting across studies, with results pertaining to GPs often not disentangled from other healthcare workers, limiting the pool of research. Furthermore, most studies used cross-sectional survey designs so there may be selection bias in the types of GPs responding. The lack of longitudinal cohort designs limits the ability to assess the impact of the pandemic, and one study55 relied on participants’ retrospective judgement, which may be flawed because of potential recall bias. There is a need to standardise tools across studies, particularly around workplace stress and burnout.
Comparison with existing literature
Although GP mental health and wellbeing has been the focus of a growing international debate, this current review is, to the authors’ knowledge, the first evidence synthesis on this topic.
Policymakers may wish to consider the strength of evidence from their particular settings, with potential need for further research reflecting variations in government and population responses to the pandemic, infection rates, and healthcare systems. For example, further research is needed from the US, India, and Brazil, which have had the highest absolute numbers of confirmed COVID-19 deaths as of March 2022.62 To the authors’ knowledge, just two studies exist from the US,34,57 both focused only on the uptake of telemedicine during the pandemic. Although three studies included GPs in the UK, these were limited to one geographical area,55 focused on GPs’ experiences of long COVID,53 or formed part of international evidence from different settings.56 Further UK evidence is needed.
Implications for research and practice
COVID-19 has presented many challenges and created additional pressures for the GP workforce. The present study provides an international overview of the sources of stress and psychological outcomes, and highlights the need for policy and practice to support GPs.
Gender and age differences are noteworthy and may warrant further exploration. Although women may be more open in discussing difficulties and seeking support because of socialised gender norms,63 women may also have experienced greater pressures during the pandemic because of wider caring responsibilities.61 Increasing stress with age may result from seniority and additional roles including practice management. Policymakers and researchers may wish to consider these gender and age differences to design tailored interventions. Despite the increased risk of COVID-19 among some ethnic minority groups in the UK,64 there was a lack of evidence exploring the impact of ethnicity on measures of psychological wellbeing.
This review of international evidence demonstrates that the COVID-19 pandemic has adversely affected GPs’ wellbeing around the world. Policy and infrastructure are needed to support GPs during this challenging time.
Acknowledgments
The authors would like to thank the members of their Project Steering Committee meeting for their contributions throughout the design and conduct of this study: Professor Dame Clare Gerada, Professor Michael West, and Professor Michael Holmes; and the patient and public representatives for their contributions throughout: Patricia Thornton, Stephen Rogers, and Emma Williams.
Funding
This report is independent research commissioned and funded by the National Institute for Health Research (NIHR) Policy Research Programme (reference: NIHR202329). The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Ethical approval
Not applicable.
Data
Materials and data used for the conduct of this research are available from the study authors on request.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.The Lancet Physician burnout: a global crisis. Lancet. 2019;394(10193):93. doi: 10.1016/S0140-6736(19)31573-9. [DOI] [PubMed] [Google Scholar]
- 2.West CP, Tan AD, Habermann TM, et al. Association of resident fatigue and distress with perceived medical errors. JAMA. 2009;302(12):1294–1300. doi: 10.1001/jama.2009.1389. [DOI] [PubMed] [Google Scholar]
- 3.Dawson J. Links between NHS staff experience and patient satisfaction: analysis of surveys from 2014 and 2015. 2018 https://www.england.nhs.uk/wp-content/uploads/2018/02/links-between-nhs-staff-experience-and-patient-satisfaction-1.pdf (accessed 3 Mar 2022). [Google Scholar]
- 4.West M, Markiewicz L. Effective team working in health care. In: Ferlie E, Montgomery K, Pedersen AR, editors. The Oxford handbook of health care management. Oxford: Oxford University Press; 2016. pp. 231–252. [Google Scholar]
- 5.Beech J, Bottery S, Charlesworth A, et al. Introduction. Closing the gap: key areas for action on the health and care workforce. 2019 https://www.kingsfund.org.uk/sites/default/files/2019-06/closing-the-gap-full-report-2019.pdf (accessed 11 Feb 2022). [Google Scholar]
- 6.British Medical Association Caring for the mental health of the medical workforce. 2019 https://www.bma.org.uk/media/1365/bma-caring-for-the-mental-health-survey-oct-2019.pdf (accessed 3 Mar 2022). [Google Scholar]
- 7.Kane L. Medscape national physician burnout, depression and suicide report. 2019 https://www.medscape.com/slideshow/2019-lifestyle-burnout-depression-6011056 (accessed 11 Mar 2022). [Google Scholar]
- 8.Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work–life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377–1385. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- 9.Orton P, Orton C, Pereira Gray D. Depersonalised doctors: a cross-sectional study of 564 doctors, 760 consultations and 1876 patient reports in UK general practice. BMJ Open. 2012;2(1):e000274. doi: 10.1136/bmjopen-2011-000274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Imo UO. Burnout and psychiatric morbidity among doctors in the UK: a systematic literature review of prevalence and associated factors. BJPsych Bull. 2017;41(4):197–204. doi: 10.1192/pb.bp.116.054247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.General Medical Council The state of medical education and practice in the UK. 2019 https://www.gmc-uk.org/-/media/documents/somep-2019---full-report_pdf-81131156.pdf (accessed 3 Mar 2022). [Google Scholar]
- 12.McKinley N, McCain RS, Convie L, et al. Resilience, burnout and coping mechanisms in UK doctors: a cross-sectional study. BMJ Open. 2020;10(1):e031765. doi: 10.1136/bmjopen-2019-031765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Walker B, Moss C, Gibson J, et al. Tenth national GP worklife survey. 2019 https://prucomm.ac.uk/assets/uploads/Tenth_GPWLS_2019_Final_version_post-review_corrected_1.pdf (accessed 3 Mar 2022). [Google Scholar]
- 14.Beech J, Bottery S, Charlesworth A, et al. Closing the gap: modelling the impact of reform and funding on nursing and GP shortages. Closing the gap: key areas for action on the health and care workforce. 2019 https://www.kingsfund.org.uk/sites/default/files/2019-06/closing-the-gap-full-report-2019.pdf (accessed 11 Feb 2022). [Google Scholar]
- 15.Badahdah AM, Khamis F, Mahyijari NA. The psychological well-being of physicians during COVID-19 outbreak in Oman. Psychiatry Res. 2020;289:113053. doi: 10.1016/j.psychres.2020.113053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dong Du J, Wang LT, et al. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen Hosp Psychiatry. 2020;67:144–145. doi: 10.1016/j.genhosppsych.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maunder RG, Lancee WJ, Balderson KE, et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. 2006;12(12):1924–1932. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tam CW, Pang EP, Lam LC, et al. Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: stress and psychological impact among frontline healthcare workers. Psychol Med. 2004;34(7):1197–1204. doi: 10.1017/s0033291704002247. [DOI] [PubMed] [Google Scholar]
- 20.British Medical Association Written evidence submitted by the British Medical Association (WBR0069) 2020 https://committees.parliament.uk/writtenevidence/11201/pdf (accessed 3 Mar 2022). [Google Scholar]
- 21.De Kock JH, Latham HA, Leslie SJ, et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health. 2021;21(1):104. doi: 10.1186/s12889-020-10070-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Higgins J, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions version 63. 2022 https://training.cochrane.org/handbook (accessed 11 Mar 2022). [Google Scholar]
- 23.Jefferson L, Golder S, Dale V, et al. Systematic review protocol exploring the impact of the COVID-19 pandemic on the wellbeing of general practitioners. medRxiv. 2021. DOI: . [DOI]
- 24.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Joanna Briggs Institute The Joanna Briggs Institute critical appraisal tools for use in JBI systematic reviews: checklist for analytical cross sectional studies. 2017 https://joannabriggs.org/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Analytical_Cross_Sectional_Studies2017_0.pdf (accessed 3 Mar 2022). [Google Scholar]
- 26.Critical Appraisal Skills Programme CASP checklist: 10 questions to help you make sense of a qualitative research. 2018 https://casp-uk.net/wp-content/uploads/2018/01/CASP-Qualitative-Checklist-2018.pdf (accessed 3 Mar 2022). [Google Scholar]
- 27.Stern C, Lizarondo L, Carrier J, et al. Methodological guidance for the conduct of mixed methods systematic reviews. JBI Evid Synth. 2020;18(10):2108–2118. doi: 10.11124/JBISRIR-D-19-00169. [DOI] [PubMed] [Google Scholar]
- 28.Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8:45. doi: 10.1186/1471-2288-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alrawashdeh HM, Al-Tammemi AB, Alzawahreh MK, et al. Occupational burnout and job satisfaction among physicians in times of COVID-19 crisis: a convergent parallel mixed-method study. BMC Public Health. 2021;21(1):811. doi: 10.1186/s12889-021-10897-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dutour M, Kirchhoff A, Janssen C, et al. Family medicine practitioners’ stress during the COVID-19 pandemic: a cross-sectional survey. BMC Fam Pract. 2021;22(1):36. doi: 10.1186/s12875-021-01382-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lau J, Tan DHY, Wong GJ, et al. Prepared and highly committed despite the risk of COVID-19 infection: a cross-sectional survey of primary care physicians’ concerns and coping strategies in Singapore. BMC Fam Pract. 2021;22(1):22. doi: 10.1186/s12875-021-01370-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rossi R, Socci V, Pacitti F, et al. Mental health outcomes among healthcare workers and the general population during the COVID-19 in Italy. Front Psychol. 2020;11:608986. doi: 10.3389/fpsyg.2020.608986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gokdemir O, Pak H, Bakola M, et al. Family physicians’ knowledge about and attitudes towards COVID-19 — a cross-sectional multicentric study. Infect Chemother. 2020;52(4):539–549. doi: 10.3947/ic.2020.52.4.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gomez T, Anaya YB, Shih KJ, et al. A qualitative study of primary care physicians’ experiences with telemedicine during COVID-19. J Am Board Fam Med. 2021;34(Suppl):S61–S70. doi: 10.3122/jabfm.2021.S1.200517. [DOI] [PubMed] [Google Scholar]
- 35.Xu Z, Ye Y, Wang Y, et al. Primary care practitioners’ barriers to and experience of COVID-19 epidemic control in China: a qualitative study. J Gen Intern Med. 2020;35(11):3278–3284. doi: 10.1007/s11606-020-06107-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lange M, Joo S, Couette PA, et al. Impact on mental health of the COVID-19 outbreak among general practitioners during the sanitary lockdown period. Ir J Med Sci. 2022;191(1):93–96. doi: 10.1007/s11845-021-02513-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee ES, Tan SY, Lee PSS, et al. Perceived stress and associated factors among healthcare workers in a primary healthcare setting: the Psychological Readiness and Occupational Training Enhancement during COVID-19 Time (PROTECT) study. Singapore Med J. 2020 doi: 10.11622/smedj.2020163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ortega-Galán AM, Ruiz-Fernández MD, Lirola M-J, et al. Professional quality of life and perceived stress in health professionals before COVID-19 in Spain: primary and hospital care. Healthcare (Basel) 2020;8(4):484. doi: 10.3390/healthcare8040484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vilovic T, Bozic J, Vilovic M, et al. Family physicians’ standpoint and mental health assessment in the light of COVID-19 pandemic — a nationwide survey study. Int J Environm Res Public Health. 2021;18(4):1–17. doi: 10.3390/ijerph18042093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jahan F, Al Zadjali NMI, Siddiqui M, et al. Mental health status among health care workers in primary care exposed to COVID-19 pandemic in North Batinah, Oman. Eur J Mol Clin Med. 2021;8(3):1268–1280. [Google Scholar]
- 41.Baptista S, Teixeira A, Castro L, et al. Physician burnout in primary care during the COVID-19 pandemic: a cross-sectional study in Portugal. J Prim Care Community Health. 2021;12:21501327211008437. doi: 10.1177/21501327211008437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Di Monte C, Monaco S, Mariani R, et al. From resilience to burnout: psychological features of Italian general practitioners during COVID-19 emergency. Front Psychol. 2020;11:567201. doi: 10.3389/fpsyg.2020.567201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sitanggang FP, Wirawan GBS, Wirawan IMA, et al. Determinants of mental health and practice behaviors of general practitioners during COVID-19 pandemic in Bali, Indonesia: a cross-sectional study. Risk Manag Healthc Policy. 2021;14:2055–2064. doi: 10.2147/RMHP.S305373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Monterrosa-Castro A, Buelvas-de-la-Rosa C, Ordosgoitia-Parra E. Probable generalized anxiety disorders in the COVID-19 pandemic: assessment in general practitioners in the Colombian Caribbean. Duazary. 2021;18(1):7–19. [Google Scholar]
- 45.Taş BG, Ozceylan G, Ozturk GZ, et al. Evaluation of job strain of family physicians in COVID-19 pandemic period — an example from Turkey. J Community Health. 2021;46(4):777–785. doi: 10.1007/s10900-020-00950-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Castelli L, Di Tella M, Benfante A, et al. The psychological impact of COVID-19 on general practitioners in Piedmont, Italy. J Affect Disord. 2021;281:244–246. doi: 10.1016/j.jad.2020.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stafie CS, Profire L, Apostol MM, et al. The professional and psycho-emotional impact of the COVID-19 pandemic on medical care — a Romanian GPs’ perspective. Int J Environ Res Public Health. 2021;18(4):1–14. doi: 10.3390/ijerph18042031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Monterrosa-Castro A, Redondo-Mendoza V, Mercado-Lara M. Psychosocial factors associated with symptoms of generalized anxiety disorder in general practitioners during the COVID-19 pandemic. J Investig Med. 2020;68(7):1228–1234. doi: 10.1136/jim-2020-001456. [DOI] [PubMed] [Google Scholar]
- 49.Filfilan NN, Alzhrani EY, Algethamy RF, et al. Psychosocial impact of COVID-19 on family physicians in the Kingdom of Saudi Arabia. Middle East J Fam Med. 2020;18(12):91–97. [Google Scholar]
- 50.Zeng X, Peng T, Hao X, et al. Psychological distress reported by primary care physicians in China during the COVID-19 pandemic. Psychosom Med. 2021;83(4):380–386. doi: 10.1097/PSY.0000000000000939. [DOI] [PubMed] [Google Scholar]
- 51.Yin Y, Chu X, Han X, et al. General practitioner trainees’ career perspectives after COVID-19: a qualitative study in China. BMC Fam Pract. 2021;22(1):18. doi: 10.1186/s12875-020-01364-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Amerio A, Bianchi D, Santi F, et al. Covid-19 pandemic impact on mental health: a web-based cross-sectional survey on a sample of Italian general practitioners. Acta Biomed. 2020;91(2):83–88. doi: 10.23750/abm.v91i2.9619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Taylor AK, Kingstone T, Briggs TA, et al. ‘Reluctant pioneer’: a qualitative study of doctors’ experiences as patients with long COVID. Health Expect. 2021;24(3):833–842. doi: 10.1111/hex.13223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lau J, Tan DHY, Wong GJ, et al. The impact of COVID-19 on private and public primary care physicians: a cross-sectional study. J Infect Public Health. 2021;14(3):285–289. doi: 10.1016/j.jiph.2020.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Trivedi N, Trivedi V, Moorthy A, Trivedi H. Recovery, restoration, and risk: a cross-sectional survey of the impact of COVID-19 on GPs in the first UK city to lock down. BJGP Open. 2021. DOI: . [DOI] [PMC free article] [PubMed]
- 56.Wanat M, Hoste M, Gobat N, et al. Transformation of primary care during the COVID-19 pandemic: experiences of healthcare professionals in eight European countries. BJGP Open. 2021. DOI: . [DOI] [PMC free article] [PubMed]
- 57.Gold KJ, Laurie AR, Kinney DR, et al. Family physician experiences with uptake during the COVID-19 pandemic. Fam Med. 2021;53(3):207–210. doi: 10.22454/FamMed.2021.613099. [DOI] [PubMed] [Google Scholar]
- 58.Sotomayor-Castillo C, Nahidi S, Li C, et al. General practitioners’ knowledge, preparedness, and experiences of managing COVID-19 in Australia. Infect Dis Health. 2021;26(3):166–172. doi: 10.1016/j.idh.2021.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tse DMS, Li Z, Lu Y, et al. Fighting against COVID-19: preparedness and implications on clinical practice in primary care in Shenzhen, China. BMC Fam Pract. 2020;21(1):271. doi: 10.1186/s12875-020-01343-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhang WR, Wang K, Yin L, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. 2020;89(4):242–250. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Soares A, Thakker P, Deych E, et al. The impact of COVID-19 on dual-physician couples: a disproportionate burden on women physicians. J Womens Health. 2021;30(5):665–671. doi: 10.1089/jwh.2020.8903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chatmon BN. Males and mental health stigma. Am J Mens Health. 2020;14(4):1557988320949322. doi: 10.1177/1557988320949322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Johns Hopkins University COVID-19 dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU) 2022. https://coronavirus.jhu.edu/map.html (accessed 3 Mar 2022).
- 64.Public Health England Disparities in the risk and outcomes of COVID-19. 2020 https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/908434/Disparities_in_the_risk_and_outcomes_of_COVID_August_2020_update.pdf (accessed 3 Mar 2022). [Google Scholar]