ABSTRACT
Delirium is an acute confusional state due to physical illness and is a frequent cause of hospital admission. In this article, we describe the development and outcomes for a community delirium toolkit pilot across Greater Manchester during the COVID-19 pandemic. We conclude that delirium can be safely managed in the community by using a toolkit that incorporates structured assessment and management. Carers and patients benefited from the use of a co-designed information leaflet.
KEYWORDS: delirium, community, pilot, assessment, management
Introduction
Delirium affects one in eight medical inpatients and is associated with poor outcomes including prolonged hospital stays and increased mortality.1 It is a frequent reason for hospital admission. There are less data around the prevalence in community settings.2 de Lange et al studied delirium in the community and showed a prevalence of 1%–2% for those aged over 65 years, 10% for those aged over 85 years and higher in groups such as those with dementia.3 While efforts have been made to implement a standardised process for delirium assessment in secondary care settings, there are no publications that mirror this activity in the community.4–6
Dementia United (DU) is the Greater Manchester (GM) Health and Social Care Partnership programme to improve dementia care. In 2017, it was established that there were no pathways or standardised assessment tools for managing delirium in the community in GM. Following a World Delirium Awareness Day event in 2018, which had engagement with stakeholders from across primary and secondary care, an evidence-based ‘GM approach to delirium’ was developed. This included key standards focused on early detection of delirium, standardised assessment and education and information for patients and family members. DU were aware of a community delirium pathway utilised by NHS Ayrshire and Arran (supplementary material S1) and this was used as an initial template for pathway development building on National Institute for Health and Care Excellence (NICE; 2019) and Health Improvement Scotland (2019) standards.1,7 Development of the community delirium toolkit was expedited by the COVID-19 pandemic as it was felt it would add value due to the pressure on acute services.8 DU shared draft versions of the community toolkit and leaflet, as part of the World Delirium Awareness Day event in 2020 with 80 delegates, consisting of stakeholders from across health and social care and carers of people with dementia, who all provided feedback. A patient delirium leaflet was included in the toolkit on which system-wide engagement and feedback was gathered.9 The toolkit was approved by DU governance and GM primary care cell with support for a 6-month pilot.
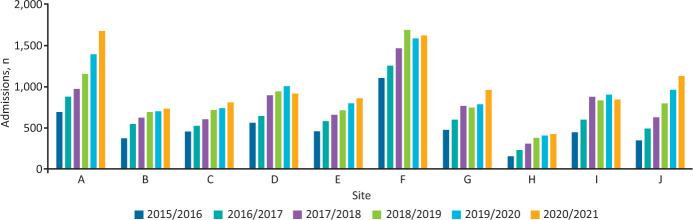
The overarching aims of the toolkit were to introduce standardised assessment, improve patient outcomes, reduce hospital admissions (known to be high in GM; Fig 1) and to provide information to patients and caregivers. Herein, we describe the feasibility of the pilot, resources required and progress achieved in meeting the overarching aims.
Fig 1.
Hospital admissions for Greater Manchester with coded delirium per year (April to March).
Methods
DU adopted the following prerequisites for teams to participate in the pilot:
use the 4AT screening tool and diagnose delirium10
be able to determine the cause of delirium including access to venepuncture
skills to act on the results from the blood tests/investigations.
Supplementary material S2 highlights the timeline of the development and piloting of the toolkit and pilot. From June 2020 onwards, expressions of interest to participate in the pilot were received from five locality sites (A, D, F, G and I) and five different teams (see supplementary material S3 for team details). DU offered each team support with launch and feasibility, governance and accountability, and data collection.
Staff in the community teams had varying levels of expertise in delirium. The COVID-19 pandemic prevented DU from accessing in-person training as had been initially planned. Alternatives were offered including collation of resources on the DU website. Fortnightly drop-in sessions were offered with the DU team including a consultant geriatrician, a mental health nurse and peer support.
Each community team adopted their own approach to preparing staff for using the toolkit. An urgent care team (site I) and an intermediate care team (site D) spent time training all staff before going live with the toolkit, an admission avoidance team (site A) trained some staff and then went live with a plan to train more staff at a later date. Using plan, do, study, act cycles, the toolkit was reviewed at intervals and amended. Teams collected a minimal anonymised dataset.
Results
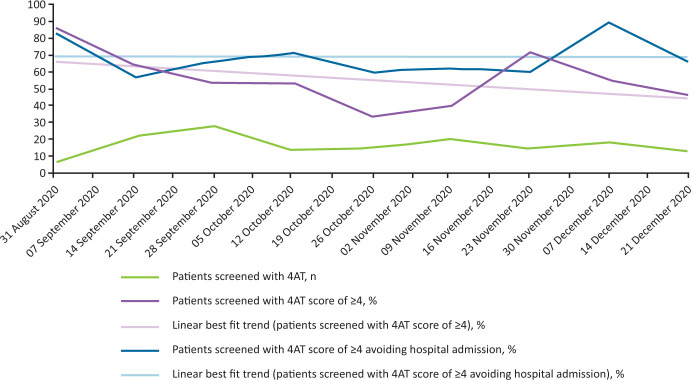
Data from the pilot of the community delirium toolkit was collected fortnightly from a total of four teams from August 2020 to January 2021. There were data for 156 consecutive patients, between 31 August 2020 and 21 December 2020, who presented with new confusion screened using the 4AT. Of those screened, 87 (56%) had a score ≥4. Sixty-one of the 87 (70%) patients who had a 4AT screening score of ≥4 avoided hospital admission and remained at home. Where patients were not able to remain at home, 13 were admitted to hospital, four were admitted into intermediate care units, one into temporary placement, one to a hospice, one patient died and the remaining six had an uncertain outcome. Collated values for number of patients screened, percentage of patients screened with a 4AT of ≥4 and the percentage of those with a 4AT score of ≥4 who avoided hospital admission are shown in Fig 2.
Fig 2.
Collated patient data from four teams.
Causes of delirium included dehydration, urinary tract infection, pain, hypernatraemia, hyponatraemia, high calcium, head injury, respiratory tract infection, COVID-19, cholecystitis, cellulitis, stroke and change in environment. A cause was identified for 67/87 (77%). Forty of the 87 patients (46%) had their bloods taken. Onward referrals outside of the team were made for 13 patients with delirium: three to therapy, two to mental health services, two to therapy for intermediate care, one to a dietitian, one to adult social care, two to bladder and bowel services, one to the hospice and one to district nurses. The caveat is that some teams had therapy services within them that they could access without onward referral. There were occasions that therapy was needed outside of these teams, for example, for intermediate care assessment and then placement. One site (site G) noted that mental health services were already involved with three patients.
Anonymous staff questionnaires were sent out, although only four were completed. Of those who responded, all stated that they agreed or strongly agreed that they understood the difference between delirium and dementia; felt confident in using key documents in the toolkit, such as the 4AT screening tool and the TIME bundle to identify and manage cases of delirium; and had gained confidence and competence through participating in the pilot.
A more detailed case study can be found for one site (site I) in supplementary material S4. In one site (site G), staff reported that they were more likely to recognise delirium and seek help in its management, they had improved recognition of delirium and causes with enhanced knowledge of the correct investigations required and when to seek help; the team also requested roll out to other teams in that area. Staff members from another site's intermediate care unit (site F) designed a lanyard card that prompts for symptoms of delirium and causes using the established acronym PINCH ME (pain, infection, nutrition, constipation, hydration, medication/metabolic and environment). Community teams continued to connect with other linked services (such as emergency departments, ambulance services and intermediate care units) through their involvement with the pilot.
The community teams reported positive feedback from people with delirium and from family members and carers in relation to the GM delirium leaflet. Families reported that the leaflet was invaluable as it ‘made sense’ of what their relative had experienced.
Discussion and conclusion
The community delirium toolkit was successfully implemented by community teams in GM. Standardised training for staff members was not delivered due to COVID-19 restrictions, though teams concluded that delivering training in preparation for implementing the toolkit was useful.
The total number of patients who were screened as part of the pilot were low, which may reflect the low prevalence of delirium in community settings. The pilot showed bloods were taken in 46% of patients and, as 77% of patients had a cause identified, this confirmed that venepuncture was not always required. This indicates, for a wider rollout of the toolkit, that blood tests should be listed as optional and not mandated. The teams reported it was essential to establish at the start which healthcare professional would act on any results.
The majority of patients were managed safely at home. Teams implemented the 4AT screening tool and applied it to all relevant patients who entered their care, enabling cases of delirium to be identified at the earliest possible opportunity. We heard that teams were able to focus on the prevention of delirium in patients who were at higher risk, which was a whole new focus for them.
The TIME bundle provided a standardised way to manage patients with delirium, though not all teams applied it to all patients in their care. Teams that trained all staff members with a detailed review of the key documents in the toolkit were most likely to use all documents in the toolkit. All teams engaged in the pilot have continued to raise awareness of delirium in their site.
In summary, the GM community toolkit pilot was successful in confirming the feasibility of safely managing people with delirium at home and eliciting resources needed in terms of workforce, communication with other specialist teams and requirement for venepuncture. In terms of overarching aims, a standardised assessment for delirium was implemented, use of the structured TIME bundle was variable, and information was provided to patients and carers. The vast majority of patients were cared for at home, but we do not yet have system-wide data translating to reduction of admissions to hospital with delirium. Data may be difficult to interpret given that many hospitals have variable implementation of a robust method for delirium detection on admission.
Caring for patients with delirium in the community is viable. In fact, it is necessary given recent publications linking hospital admission to development of delirium.11,12
Supplementary material
Additional supplementary material may be found in the online version of this article at www.rcpjournals.org/fhj:
S1 – The community delirium pathway utilised by NHS Ayrshire and Arran.
S2 – Community delirium toolkit project timeline.
S3 – Community team components, coverage and scope.
S4 – A detailed case study for an urgent care team.
Acknowledgements
We would like to thank all those people who worked with us over the last four years in supporting the development of the delirium programme of work.
Delirium task and finish group members including people with lived experience and carers.
Delegates who attended the annual World Delirium Awareness Day events in 2018, 2019 and 2020; and to the Greater Manchester and eastern Cheshire strategic clinical networks for their support with these events.
Dementia Carers Expert Reference Group who very kindly provided initial feedback on the delirium leaflet and the wider engagement of carers in the programme of work.
Special thanks to NHS Ayrshire and Arran for their community pathway, Healthcare Improvement Scotland / Scottish Delirium Association for delirium toolkit and TIME bundle.
The community teams who engaged with the pilot: Trafford community enhanced care service, Bolton admission avoidance team, Salford urgent care team, Manchester intermediate care service (Gorton South), Stockport Proactive Victoria primary care network and wider engaging colleagues such as Salford intermediate care service and North West Ambulance Service.
Dementia United delirium team: Emma May Smith and Lyndsey Kavanagh.
References
- 1.Scottish Intercollegiate Guidelines Network . Risk reduction and management of delirium. SIGN, 2019. www.sign.ac.uk/our-guidelines/risk-reduction-and-management-of-delirium [Accessed 08 September 2021]. [DOI] [PubMed] [Google Scholar]
- 2.Andrew MK, Freter SH, Rockwood K. Prevalence and outcomes of delirium in community and non-acute care settings in people without dementia: a report from the Canadian study of health and aging. BMC Med 2006;4:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.de Lange E, Verhaak PF, van der Meer K. Prevalence, presentation and prognosis of delirium in older people in the population, at home and in long term care: a review. Int J Geriatr Psychiatry 2013;28:127–34. [DOI] [PubMed] [Google Scholar]
- 4.Bauernfreund Y, Butler M, Ragavan S, Sampson EL. TIME to think about delirium: improving detection and management on the acute medical unit. BMJ Open Qual 2018;7:e000200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vardy E, Collins N, Grover U, et al. Use of a digital delirium pathway and quality improvement to improve delirium detection in the emergency department and outcomes in an acute hospital. Age Ageing 2020;49:672–8. [DOI] [PubMed] [Google Scholar]
- 6.Gusmao-Flores D, Salluh JI, Chalhub RA, Quarintini LC. The confusion assessment method for the intensive care unit (CAM-ICU) and intensive care delirium screening checklist (ICDSC) for the diagnosis of delirium: a systematic review and meta-analysis of clinical studies. Crit Care 2012;16:R115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Institute for Health and Care Excellence . Delirium: prevention, diagnosis and management: Clinical guideline [CG103]. NICE, 2019. www.nice.org.uk/guidance/cg103 [Accessed 08 September 2021]. [PubMed] [Google Scholar]
- 8.Dementia United . Greater Manchester delirium community toolkit. Dementia United. https://dementia-united.org.uk/delirium-community-toolkit [Accessed 08 September 2021]. [Google Scholar]
- 9.Greater Manchester Health and Social Care Partnership . What is delirium? GMHSCP. https://dementia-united.org.uk/wp-content/uploads/sites/4/2021/03/Greater-Manchester-delirium-Leaflet-long-version.pdf [Accessed 08 September 2021]. [Google Scholar]
- 10.MacLullich A. 4AT Rapid clinical test for delirium. MacLullich A. www.the4at.com
- 11.Richardson SJ, Lawson R, Davis DHJ, et al. Hospitalisation without delirium is not associated with cognitive decline in a population-based sample of older people-results from a nested, longitudinal cohort study. Age Ageing 2021;50:1675–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shepperd S, Butler C, Cradduck-Bamford A, et al. Is comprehensive geriatric assessment admission avoidance hospital at home an alternative to hospital admission for older persons: a randomized trial. Ann Intern Med 2021;174:889–98. [DOI] [PubMed] [Google Scholar]