ABSTRACT
Introduction
Hospital at Home (@Home) services bring the ward to the patient, providing acute care in the home. The @Home team adapted to support the care of patients with COVID-19 in the community who would otherwise have required hospitalisation.
Methods
An evidence-based guideline and treatment bundle (dexamethasone, oxygen, intravenous fluids and thromboprophylaxis) for managing severe COVID-19 was developed. Data were retrospectively extracted from notes of patients with COVID-19 admitted between 16 December 2020 to 14 February 2021, and service users contacted for feedback.
Results
One-hundred and twenty-five adults with COVID-19 were treated by @Home; 42 severe (34%) and 83 non-severe (66%) infections; average length of stay was 7 days (interquartile range 4–8). Eight-hundred and seventy-five hospital-occupied bed days were saved. Service users emphasised the importance of being with loved ones and the value of respecting peoples’ wishes to be at home.
Conclusion
@Home gave people with COVID-19 a choice of active treatment at home, thereby extending available healthcare capacity beyond the acute hospital setting.
KEYWORDS: COVID-19, hospital at home, patient choice, admission avoidance and urgent care response, older people
Introduction
Hospital at Home (@Home) services are a relatively new concept in healthcare provision aimed at providing acute and semi-acute level-1 hospital care to people in their own homes. This consists of ward based multidisciplinary care with medical interventions including intravenous treatments, oxygen and nebulisers, but not single organ support such as renal haemofiltration or mechanical ventilation.1 They reduce the demand on hospital beds by offering an alternative place of care to people who otherwise would either need to be admitted to hospital for treatment or would need to stay longer in hospital to complete their treatment. In healthcare systems with @Home, these services fill the gap between primary and secondary care acute services. @Homes exist throughout the world but are predominantly found in higher-income countries. Some are specific to a single disease entity (such as oncology and stroke), whereas many others manage a mixture of medical conditions.2,3 These services are particularly helpful for older adults living with frailty for whom hospital admission might lead to hospital-associated secondary issues, such as nosocomial infections, worsening mobility, delirium and institutionalisation. Outcomes are similar whether care is delivered by @Home or in hospital, and there is evidence of a reduction in subsequent admission to long-term institutional care for those who receive @Home care.4
The COVID-19 pandemic has led to two surges in demand for hospital care. Hospitals have a finite capacity, so alternatives to hospital care were vital to ensure patients received evidence-based treatment in the right place at the right time. Many systems for remote support and monitoring of patients in their own homes with COVID-19 were set up to cope with the surge in demand but for frailer adults and those with more complex needs, face-to-face support was needed. Here, we describe how a well-established @Home service supported pathways of care for patients with COVID-19, particularly older adults living with frailty, including a unique severe COVID-19 treatment pathway.
Aims
To describe the development and implementation of pathways of care for patients with COVID-19 by @Home who would otherwise have required inpatient hospital care.
To describe the development, implementation and outcome of a treatment bundle for managing severe COVID-19 by @Home.
To investigate the experiences of patients and those close to them receiving treatment for severe COVID-19 by @Home.
Methods
Setting
Guy's and St Thomas’ NHS Foundation Trust (GSTT) @Home was established in 2013. It is within the integrated care directorate that provides both acute medical inpatient and community services to two inner London boroughs. These boroughs (Lambeth and Southwark) have a population of 650,000 and are ethnically and economically diverse; 60% and 37%, respectively, describe their ethnicity as other than White British, and both boroughs describe wide ranges in household income, with 20% having an income under £15,000 and another 20% having an income over £60,000 in Southwark.5,6 These factors put these populations at particular risk of COVID-19.7,8 Within the boroughs, there are 63 care homes and three large teaching hospital trusts (GSTT, King's College Hospital NHS Foundation Trust, and South London and Maudsley NHS Foundation Trust).9
@Home operates as a mobile ward in the community providing acute and semi-acute care 7 days a week by doctors, nurses and allied healthcare professionals. Prior to the COVID-19 pandemic, all common level 1 ward treatments were offered in the home except oxygen.
Guideline development
A consensus group of medical consultants with expertise in infectious disease, general medicine, geriatrics and respiratory medicine was formed. They used their experience in the first wave of the pandemic and results from national trials to create a series of COVID-19 treatment action cards and a severe COVID-19 treatment bundle to ensure consistent application of evidence-based treatment. As part of this process, it was recognised that there was a group of patients who might benefit more from treatment in their own homes than from transfer to hospital for the same treatment ‘bundle’. The severe treatment bundle was therefore adapted for @Home. A live guideline developed at speed to operationalise the delivery of this care in people's own homes was jointly agreed with @Home clinicians, infectious disease consultants and respiratory teams from both acute hospitals. This guideline was first used in mid-December 2020 at the start of the second wave of COVID-19 in London. Subsequently, a national consensus statement was produced for community treatment that was similar.10 As experience grew and new evidence on treatment emerged, the local guideline was revised.
Severe COVID-19 guideline and bundle
The COVID-19 @Home guideline operationalises the WHO criteria for diagnosis of severity of COVID-19 infection and directs the pathway of care for patients according to this categorisation.11 Consequently, three pathways of care emerged: severe COVID-19, non-severe COVID-19 and hospital discharged COVID-19 with ongoing care needs.
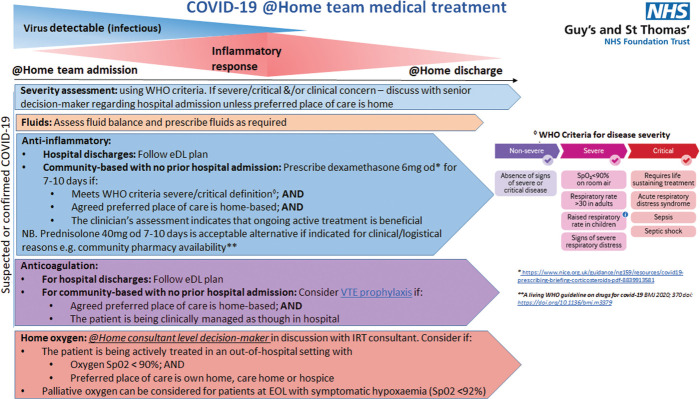
At initial assessment by @Home, those diagnosed with severe COVID-19 were asked their preferred place of care (hospital vs home), for those that lacked capacity, the Mental Capacity Act was followed with those close to them consulted for a best interest decision.12 If home treatment was agreed, then the severe COVID-19 @Home treatment bundle commenced involving intravenous fluids, oxygen, dexamethasone, venous thromboembolism (VTE) prophylaxis and advance care planning using the principles of the AMBER care bundle, a tool to assist teams in managing patients with uncertain prognosis.13 As in hospital, patients received a minimum of one medical review daily with treatment plan revision according to their improvement or deterioration. Pathways for ongoing care were included as per hospital inpatients; palliative care support for deteriorating patients and respiratory outpatient care for improving patients (Fig 1).
Fig 1.
Pathways for ongoing care. Reproduced with permission from Anne Goodman on behalf of the GSTT COVID Guideline Development Group. @Home = Hospital at Home; eDL = electronic discharge letter; EOL = end of life; IRT = integrated respiratory team; od = once per day; SpO2 = oxygen saturation; VTE = venous thromboembolism; WHO = World Health Organization.
A treatment pack consisting of the first doses of dexamethasone, VTE prophylaxis and intravenous fluids with a drug chart, blood glucose chart and fluid chart was created, and available to all doctors to take to initial visits. Oxygen concentrators were obtained and kept in the cars for initial visits to enable rapid oxygen initiation prior to arrival of ongoing oxygen supply.
There was an ongoing risk of COVID-19 infection to those living with and caring for the patient. Most were already aware of this risk and taking sensible precautions preceding @Home input, such as wearing personal protective equipment and keeping a suitable physical distance from the patient. Verbal advice was given by @Home staff to all patients and those supporting them concerning infection control measures and self-isolation rules.
Service evaluation
Data collection
Information was retrospectively extracted from electronic notes (Carenotes, electronic patient record and local care record) of all patients with COVID-19 admitted to @Home between 16 December 2020 and 14 February 2021 by one researcher and then independently validated by a second. Where not documented in contemporaneous clinical notes, Clinical Frailty Scores (CFSs) were calculated retrospectively using clinical judgement based on the status of the patient 2 weeks prior to their admission to @Home, with the assistance of the ‘Clinical Frailty Scale App’.14 A consultant geriatrician resolved any disagreements. Patients were considered on the severe COVID-19 bundle if any element of the treatment bundle was started by @Home for a patient with severe COVID-19. Outcomes were extracted on the day of discharge and 30 days following discharge.
Service user feedback
A retrospective telephone questionnaire was designed by the researchers to obtain feedback on the severe COVID-19 pathway from patients and those close to them. It contained five questions to ascertain satisfaction and areas for improvement (supplementary material S1).
The researchers attempted to contact all the patients or those close to them that were treated on the severe COVID-19 pathway whether the patient was alive or dead. Patients who were alive and had capacity to answer the questionnaire were contacted directly. Those close to them were contacted in all other circumstances. All those contacted were reassured that their responses were anonymous.
The questionnaire was carried out between 14 June 2021 and 15 June 2021 and responses transcribed at the time of interview onto an online survey hosted on Google Forms. Responses were reviewed qualitatively and common themes were identified.
Outcomes
All patients
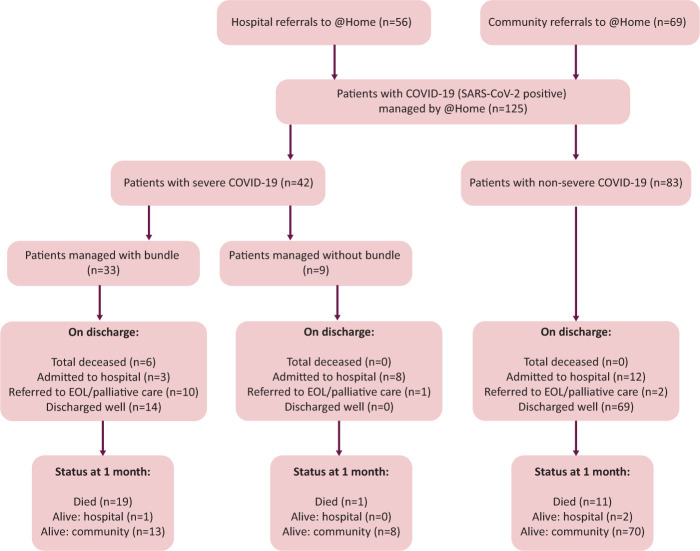
One-hundred and twenty-five COVID-19 patients were treated by @Home during the second wave of the pandemic in London between 16 December 2020 and 14 February 2021 (Fig 2).
Fig 2.
Patients treated by Hospital at Home service during the second wave of the pandemic in London between 16 December 2020 and 14 February 2021. @Home = Hospital at Home; EOL = end-of-life.
Sixty-nine (55%) patients were referred directly from the community and 56 (45%) from hospital. This represented 30% (125/420) of all patients seen by @Home during this period. COVID-19 patients’ care requirements were subdivided across the three pathways: severe COVID-19 (n=42; 34%), non-severe (n=35; 28%) and hospital discharged COVID-19 with ongoing care needs (n=56; 45%). Median age was 81 years (interquartile range 67–87), with 69 patients (55%) over 80-years-old. Seventy-four (59%) patients were women and 51 (41%) were men.
Average length of stay with @Home for all 125 patients with COVID-19 was 7 days (range 1–25). This translates to 875 occupied bed days, which would have been the equivalent of the use of a 28 bedded ward for 31 days. During this time, @Home also admitted a further 295 non-COVID-19 patients with a related further reduction in hospital bed requirement.
Severe COVID-19
The demographics and outcomes at discharge from @Home for the patients treated on the severe pathway are shown in Table 1. Of the 42 severe patients seen, six were referred as they didn't wish to go to hospital but were persuaded to go as they would have benefited from critical care support had they deteriorated and, for two patients, palliation rather than active treatment was more appropriate; one further patient was escalated to hospital on initial assessment having been erroneously referred for home treatment. Therefore, 33 patients were treated for severe COVID-19. More patients lived in their own homes than care homes (58% vs 42%, respectively), most were severely frail with mean CFS of 7. Forty-two per cent were discharged well and alive at 1 month after discharge.
Table 1.
Patients on severe COVID-19 bundle, total n=33
| Demographics | |
|---|---|
| Age, years, mean (range) | 85 (61–95) |
| Men, n (%) | 12 (36) |
| Women, n (%) | 21 (64) |
| Nursing home, n (%) | 14 (42) |
| Own home, n (%) | 19 (58) |
| Clinical frailty score, mean (range) | 7 (3–9) |
| Outcome at discharge | |
| Length of stay for those discharged, days, mean (range) | 8 (4–25) |
| Died, n (%) | 6 (18) |
| Admitted to hospital from @Home, n (%) | 3 (9) |
| Discharged to EOL community care with palliative care team, n (%) | 10 (30) |
| Recovered, n (%) | 14 (42) |
| Outcome at 1 month | |
| Alive, n (%) | 14 (42) |
| Died, n (%) | 19 (58) |
@Home = Hospital at Home; EOL = end-of-life.
Non-severe COVID-19
Patients with non-severe COVID-19 were monitored as clinically appropriate and non-COVID-19 medical issues addressed. Once stable, these patients were triaged according to their length of COVID-19 illness and either discharged without specific COVID-19 follow-up or referred to an appropriate monitoring service to detect and manage deterioration during the known peak risk timeframe.
Patients on the ‘hospital discharged COVID-19 with ongoing care needs’ pathway mainly required blood sugar monitoring and insulin adjustment due to dexamethasone-induced hyperglycaemia, ongoing respiratory monitoring due to COVID-19 pneumonitis or delirium support. Due to comorbidity resulting in issues such as poor cognition, poor dexterity, reduced mobility and inability to use IT or telephone, these patients could not be supported by the existing non-face-to-face virtual pathways of care that were in place.
Feedback
Feedback was obtained for 16 of the 33 episodes of severe COVID-19 treatment, three patients and 13 people close to patients. Service user feedback was largely very positive with 100% of service users stating that the patient was well supported by @Home, and 14 of the 16 (88%) service users stating that those close to the patient were also well supported.
Key themes elicited from patients and those close to them were the importance of being able to be with loved ones, the benefits of being treated in a familiar environment for older, frailer patients and the value of respecting patients’ wishes to be at home. One patient reported, ‘I was determined to be treated at home as I didn't want to go to hospital. I was certain I would not survive if I went to hospital,’ and another said the main benefit of being treated by the @Home team was ‘being surrounded by my family at a time when I needed them the most.’ One relative reported that the care ‘was much more individualised. It meant I could be with him as he faded, and that I was there when he took his last breath.’ While another said, ‘Having his family around him was the most important thing for him, and Hospital at Home allowed that to happen.’ The main disadvantages reported were regarding oxygen delivery, either not being able to access oxygen fast enough or feeling that the ‘hospital was better equipped to handle the oxygen cylinder.’
Discussion
Having an established @Home as part of our integrated care pathways put us in a unique position to develop and deliver new COVID-19 treatment pathways rapidly in a person's own home. We provided three novel COVID-19 pathways, two for direct community referrals to treat both severe and non-severe COVID-19, and the third for early hospital discharge of those with COVID-19. These pathways reduced the need for acute hospital beds at a time of unprecedented demand amid a well-publicised concern that there would be insufficient hospital beds to cope with a second pandemic surge in COVID-19 cases.15 To date, hospital at home services in the USA and Spain have also described using their services to help with COVID-19 patients in the first wave of the pandemic by providing hospital discharge and community support.16–20 However, to our knowledge, this is the first report of severe COVID-19 treatment of community-referred patients in the UK. As we understand it, our service is also the first to describe the use of a formalised bundle of treatment for the management of severe COVID-19 in the community.
The severe COVID-19 pathway was particularly utilised for individuals with advanced frailty and comorbidity who would have been extremely unlikely to benefit from hospital critical care interventions.21 Many of these patients and their families were fearful of hospital admission, aware that visitors were not allowed, resulting in isolation during a period of extreme vulnerability and in the knowledge that, if the patient did deteriorate, they were very likely to die without family and friends by their side. Consequently, there was a possibility that some patients would not access evidence-based treatment unless there was a viable alternative to hospital admission. By providing severe COVID-19 treatment in people's homes via @Home, a real alternative to hospital was offered. Patients and their families had a true choice of place of care without compromising the quality of care they received.
Despite advanced frailty and uncertainty of survival from COVID-19 for those treated for severe COVID-19, over half survived to discharge, with 42% alive at 1 month. There was no control group, so we do not know whether this was due to the active treatment or not, but it does suggest that it would have been inappropriate not to offer active treatment.
The logistical challenges of providing timely acute care for severe COVID-19 patients were considerable. Oxygen provision was new to our service and its use was supported by respiratory specialists. Initially, oxygen was provided via a centralised ordering system, but it rapidly became evident that the 4-hour wait was too long, with an ambulance on one occasion waiting with the patient to provide temporary oxygen. This issue was also reflected in our patient feedback. Acquiring short-term portable concentrators in each urgent response car resolved this issue. It was anticipated that demand might outstrip the capacity of community palliative care services that usually takes over the care of patients in the last days of life. Staff were, therefore, upskilled with the help of our palliative care team to support patients, particularly in prescribing anticipatory medications and syringe driver set-up.
Operationally, the initial visit to a patient with COVID-19 was longer than is usually required for visits, often taking over 2 hours. Assessing severity, administering the severe COVID-19 bundle, and discussing place of care and advance care planning required a significant time investment to carry out effectively. To accommodate these increased patient needs, additional medical, nursing and transport resources were sourced via redeployment of staff from predominantly outpatient specialties. Compared with pre-COVID-19 experiences, delivery of care was made simpler as the national lockdown tended to ensure patients and those close to them were in their home when @Home visited. Travel times were also much shorter due to lack of traffic compared with pre-pandemic levels, making visiting much easier.22
A major advantage to the local healthcare system was the ability of @Home to reduce the need for inpatient beds, helping the whole system cope with the surge in demand. To give context, in the same time period as our data collection, one large local acute hospital trust treated 1,114 patients presenting with COVID-19.23 The 125 patients with COVID-19 seen by @Home was equivalent to 11% of the COVID-19 inpatients at this trust. Sixty-nine patients aged 80 years or over were seen by @Home, compared with 176 seen by the trust. Our @Home service, therefore, saw the equivalent of 39% of patients in this age group. Thus, @Home was a significant contributor to local health system capacity, especially in the provision of care for older adults. This reduction in bed usage has also been described by other @Home services of comparable size when they provided services for COVID-19, and that this translates to significant cost savings.17,19
In addition to the occupied bed days saved for COVID-19 patients, @Home continued to admit non-COVID-19 patients who otherwise would have required hospitalisation, thereby further reducing the demand on hospital beds during this period. Furthermore, the number of occupied bed days saved may well be an underestimate due to the nature of the patients cared for. Discharging complex frail patients from hospital is challenging as their usual support networks are interrupted. Those caring for them in hospital are not always fully aware of previous functional levels and assessments to reduce perceived risk on discharge can be lengthy. Additionally, rules concerning discharge of patients with COVID-19 home and to care homes have altered throughout the pandemic, often increasing length of stay for this group.
At a time of rapid change and uncertainty, @Home offered patients a choice regarding their place of treatment. Patients valued being able to stay at home and those close to them valued being able to support a patient's wishes, including supporting end-of-life care at home. However, staying at home could have resulted in an excess burden on caregivers.24 During the pandemic, caregivers often changed; family members living with patients were present more and often cancelled external carers to reduce potential COVID-19 exposure.25 @Home supported with therapy input and provision of carers for functional support. This may explain why patients and those close to them felt well supported by @Home. In instances when patients deteriorated, it was clear that those close to them valued the individualised palliative approach that @Home offered and their ability to be present to ‘say goodbye’ in stark contrast with hospital.26
The experience of using @Home to provide severe COVID-19 treatment for those living with frailty, where there is uncertainty of survival, can be extrapolated to other acute illnesses in this patient group. Frailty trajectories are relatively unpredictable with considerable uncertainty as to whether someone will improve or die. @Home offers a choice for those whose preferred place of care and death is at home to have active treatment and a chance at improvement in their own homes, with many @Home teams working closely with or run by geriatricians and with strong links to other medical specialists and community palliative care and psychiatric services.
Limitations
Patients and those close to them were contacted for feedback several months after receiving care, which may have led to some loss of recall of the experience. However, evidence suggests it is best to contact bereaved families at least 3 months after a bereavement.27 The questionnaire was administered by a clinician researcher which might have influenced responses. A postal questionnaire might have avoided this potential bias but could have had a lower response rate.
Conclusion
@Home was able to rapidly adapt and provide medical care for COVID-19 patients including severe COVID-19 treatment for those living with frailty and multimorbidity in their own homes. This reduced the demand for acute hospital beds during the second wave of the COVID-19 pandemic but ensured all patients received the care they would benefit from in the place of their choice. @Home is an essential part of any healthcare system, plugging the gap between chronic disease management in the community and acute care in the hospital. Lessons learnt from new COVID-19 @Home pathways will have an enduring legacy on future acute care pathways provided by @Home and should encourage other areas to develop hospital at home services to future proof their care pathways especially in light of The NHS Long Term Plan and urgent care response work.28
Supplementary material
Additional supplementary material may be found in the online version of this article at www.rcpjournals.org/fhj:
S1 – Telephone questionnaire to obtain feedback on the severe COVID-19 pathway.
References
- 1.Department of Health . Comprehensive critical care: a reviewof adult critical care services. DH, 2000. https://webarchive.nationalarchives.gov.uk/+/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4006585 [Accessed 20 July 2021]. [Google Scholar]
- 2.Mooney K, Titchener K, Haaland B, et al. Evaluation of oncology hospital at home: unplanned health care utilization and costs in the huntsman at home real-world trial. J Clin Oncol 2021;39:2586–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gonçalves-Bradley DC, Iliffe S, Doll HA, et al. Early discharge hospital at home. Cochrane Database Syst Rev 2017;6:CD000356. www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000356.pub4/full [Accessed 06 October 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shepperd S, Butler C, Cradduck-Bamford A, et al. Is comprehensive geriatric assessment admission avoidance hospital at home an alternative to hospital admission for older persons?: a randomized trial. Ann Intern Med 2021;174:889–98. [DOI] [PubMed] [Google Scholar]
- 5.Lambeth Council . Demography factsheet. Lambeth Council, 2017. www.lambeth.gov.uk/sites/default/files/ssh-demography-factsheet-2017.pdf [Accessed 07 October 2021]. [Google Scholar]
- 6.Southwark Council . Annual public health report 2019: statistical appendix. Southwark Council, 2019. www.southwark.gov.uk/assets/attach/12094/APHR-2019-Statistical-appendix.pdf [Accessed 06 October 2021]. [Google Scholar]
- 7.Pan D, Sze S, Minhas JS, Bangash MN, et al. The impact of ethnicity on clinical outcomes in COVID-19: A systematic review. EClinicalMedicine 2020;23:100404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bambra C, Riordan R, Ford J, Matthews F. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health 2020;74:964–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.carehome.co.uk . Reviews for Care Homes, Residential Homes & Nursing Homes. carehome.co.uk. www.carehome.co.uk [Accessed 20 July 2021]. [Google Scholar]
- 10.British Geriatrics Society . COVID-19: Treatment for older people in the community. BGS, 2021. www.bgs.org.uk/resources/covid-19-treatment-for-older-people-in-the-community [Accessed 20 July 2021]. [Google Scholar]
- 11.World Health Organization . Living guidance for clinical management of COVID-19. WHO, 2021. www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2 [Accessed 20 July 2021]. [Google Scholar]
- 12.Mental Capacity Act 2005. UK Government. www.legislation.gov.uk/ukpga/2005/9/contents [Accessed 10 October 2021]. [Google Scholar]
- 13.Carey I, Shouls S, Bristowe K, et al. Improving care for patients whose recovery is uncertain. The AMBER care bundle: design and implementation. BMJ Support Palliat Care 2015;5:12–8. [DOI] [PubMed] [Google Scholar]
- 14.NHS Acute Frailty Network . Clinical Frailty Scale App. NHS, 2020. www.acutefrailtynetwork.org.uk/Clinical-Frailty-Scale/Clinical-Frailty-Scale-App [Accessed 20 July 2021]. [Google Scholar]
- 15.Campbell D, Davis N. NHS hospitals running out of beds as Covid cases continue to surge. The Guardian 2020. www.theguardian.com/world/2020/dec/17/nhs-hospitals-running-out-of-beds-as-covid-cases-continue-to-surge [Accessed 20 July 2021]. [Google Scholar]
- 16.Heller DJ, Ornstein KA, DeCherrie LV, et al. Adapting a Hospital-at-Home care model to respond to New York City's COVID-19 crisis. J Am Geriatr Soc 2020;68:1915–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pericàs JM, Cucchiari D, Torrallardona-Murphy O, et al. Hospital at home for the management of COVID-19: preliminary experience with 63 patients. Infection 2020;49:327–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nogués X, Sánchez-Martinez F, Castells X, et al. Hospital-at-Home expands hospital capacity during COVID-19 pandemic. J Am Med Dir Assoc 2021;22:939–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Llorens P, Moreno-Pérez O, Espinosa B, et al. An integrated emergency department/hospital at home model in mild COVID-19 pneumonia: feasibility and outcomes after discharge from the emergency department. Intern Emerg Med 2021:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sitammagari K, Murphy S, Kowalkowski M, et al. Insights from rapid deployment of a “virtual hospital” as standard care during the COVID-19 pandemic. Ann Intern Med 2020;174:M20–4076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Institute for Health and Care Excellence . COVID-19 rapid guideline: managing COVID-19: NICE guideline [NG191]. NICE, 2021. www.nice.org.uk/guidance/ng191 [Accessed 20 July 2021]. [Google Scholar]
- 22.Department for Transport . Road traffic estimates: Great Britain 2020. DfT, 2021. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/981967/road-traffic-estimates-in-great-britain-2020.pdf [Accessed 07 October 2021]. [Google Scholar]
- 23.Guy's and St Thomas’ NHS Foundation Trust . Internal Data. Unpublished. [Google Scholar]
- 24.Mäkelä P, Stott D, Godfrey M, et al. The work of older people and their informal caregivers in managing an acute health event in a hospital at home or hospital inpatient setting. Age Ageing 2020;49:856–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carers UK . Caring behind closed doors: six months on. Carers UK, 2020. www.carersuk.org/images/News_and_campaigns/Behind_Closed_Doors_2020/Caring_behind_closed_doors_Oct20.pdf [Accessed 07 October 2021]. [Google Scholar]
- 26.Hanna JR, Rapa E, Dalton LJ, et al. A qualitative study of bereaved relatives’ end of life experiences during the COVID-19 pandemic. Palliat Med 2021;35:843–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Healthy London Partnership . Gathering feedback from families and carers when a child or young person dies - resource launched. Healthy London Partnership, 2019. www.healthylondon.org/gathering-feedback-from-families-and-carers-when-a-child-or-young-person-dies-new-resource [Accessed 07 October 2021]. [Google Scholar]
- 28.NHS England . The NHS Long Term Plan. NHS, 2019. www.longtermplan.nhs.uk/online-version [Accessed 20 July 2021]. [Google Scholar]