ABSTRACT
Background
Physician trainee research collaboratives (TRCs) help trainees develop research skills and establish peer networks. We aimed to identify the structure, activity and views of physician TRCs in the UK.
Methods
Representatives from physician TRCs in the UK were invited to complete an online survey and participate in a focus group.
Results
Representatives from 23 physician TRCs completed the survey. There was wide variation in collaborative structure, senior input and funding resources. Seventy-four per cent of physician TRCs had published peer-reviewed articles, with 70% reporting ongoing projects at the time of the survey. The survey and focus group identified improved patient care, research and leadership skills as benefits of collaborative work; while institutional and consultant support, limited time for research, funding opportunities and restrictions on group authorship were cited as challenges to collaborative success.
Conclusion
Physician TRC activity continues to grow and demonstrates a dynamic approach to research for all trainees.
KEYWORDS: trainee research collaboratives, physician trainees, research skills, widening access to research
Introduction
The General Medical Council requires all postgraduate medical curricula to include training in research.1 Trainee research collaboratives (TRCs; networks of doctors in training based on geographical location or specialty who collaborate to deliver multicentre quality improvement or research) are seen as a means of developing research skills and fostering networks between trainees within and between specialties in medicine and surgery. Surgical TRCs started in the UK in 2008 with the formation of the West Midlands Research Training Collaborative.2 This model has disseminated around the UK over the past 13 years, with establishment of numerous national and international collaboratives.3,4 Outputs from these surgical collaboratives include audits and quality improvement studies, as well as randomised clinical trials (such as the Reduction of Surgical Site Infection Using Several Novel Interventions (ROSSINI) trial, which involved 760 study subjects from 21 research sites) directly influencing patient care.6 Collaborative research can facilitate the collection of extensive datasets that can inform clinical practice, such as the COVIDSurg and GlobalSurg collaboratives’ recent publication of data on timing of surgery following COVID-19 infection, which involved over 140,000 patients and a record-breaking 15,025 contributors from around the world.7,8 These and other international research collaboratives have included participants from lower-income countries and those in the global south, demonstrating the reach and power of collaborative research, particularly during the COVID-19 pandemic.
Recently, the Royal College of Physicians (RCP) in the UK has outlined its strategy to develop and support the physician workforce to become more research active and innovative as part of improving patient care.9 However, there is little information on the current state of physician TRCs and the research outputs from these networks.
The aim of this study was to survey the representatives of the current physician TRCs in the UK in order to identify the factors that influence the development, governance and outputs of these networks.
Methods
Physician TRCs were identified in August 2020 via the RCP trainees committee regional representatives, specialty societies and their trainee representatives, specialty trainee groups, PubMed and social media searches, and the National Research Collaborative database.10 The selection process is described in Fig 1.
Fig 1.
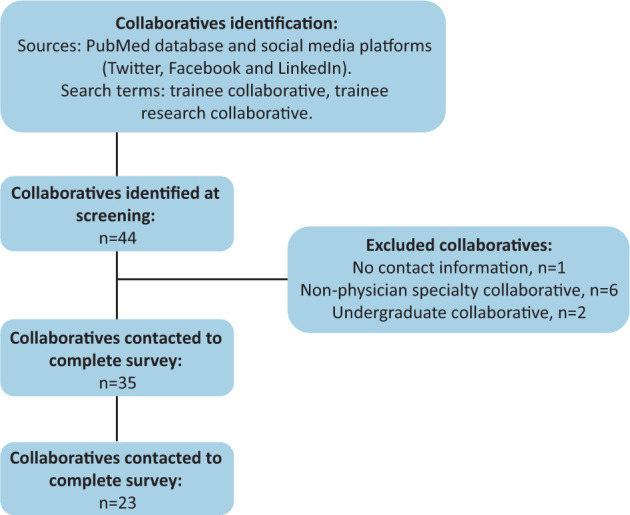
Selection process for identifying physician trainee research collaboratives.
All physician TRCs in the UK were included, including medical ophthalmology and paediatric cardiology, which fall under the auspices of the Joint Royal Colleges of Physicians Training Board (JRCPTB) and were therefore included in this study. Non-physician trainee research collaboratives (including surgery, anaesthetics, emergency medicine, intensive care, general practice, obstetrics and gynaecology, and paediatrics (except paediatric cardiology)) were excluded. Undergraduate research collaboratives were also excluded.
A web-based survey was designed, with questions categorised into eight sections: about you; about your collaborative; collaborative structure; support for your collaborative; output from your collaborative; benefits and challenges; final comments; and consent to follow-up interview.
An invitation to complete the survey was sent to the chairs and co-chairs of all suitable collaboratives identified at screening in September 2020. Contact was made via publicly available information. The survey was open to respondents for 28 days with reminders sent at day 14. Data were collated and analysed using MS Excel 16.0 (Microsoft Corporation, Redmond, USA). Permission to publish collaborative details was requested separately to the survey.
Survey respondents who had consented to a follow-up interview were invited to attend a virtual focus group. Three study team members took part in the focus group, with two facilitating the session and one observing and recording. The focus group was conducted in a semi-structured format, with pre-planned probing questions derived from themes identified from the survey responses. Interviewers were free to explore responses with follow-up questions where this was felt appropriate. Participants were asked to give their views based on their personal experiences as well as the experiences of wider members from the collaboratives they led. Key challenges to TRC success as well as proposed solutions were identified contemporaneously and agreed upon by the participants. The study was determined not to require ethical approval by the Health Research Authority online tool.11
Results
Web survey results
Overview
In total, 44 TRCs were identified at screening, of which, nine were excluded (one due to lack of contact information, six non-physician-based specialty collaboratives and two undergraduate collaboratives). Trainees in leadership positions in the remaining 35 collaboratives were invited to undertake the survey, of which, 28 individual responses from 23 collaboratives were received (66% response rate; Fig 1). Thirty collaboratives gave permission to publish their details on the RCP Research and Innovation Hub.12
Of the 23 collaboratives who responded to the survey, there were two international, six national and 15 regional collaboratives (six northern, four Midlands, two London, two south west and one Wales). All but one were specialty-based (six gastroenterology, three respiratory, three palliative medicine, two ophthalmology, two geriatric medicine, one acute medicine, one nephrology, one neurology, one non-malignant haematology, one oncology and one pancreatology), and one was condition-specific (breast cancer). These collaboratives were established between 2010 and 2019, with the majority (87%) established after 2014 (Fig 2). The size of collaboratives ranged from fewer than 10 members to greater than 50 members, with the majority having more than 20 members. All but one collaborative was structured with a central steering committee along with wider trainee membership.
Fig 2.
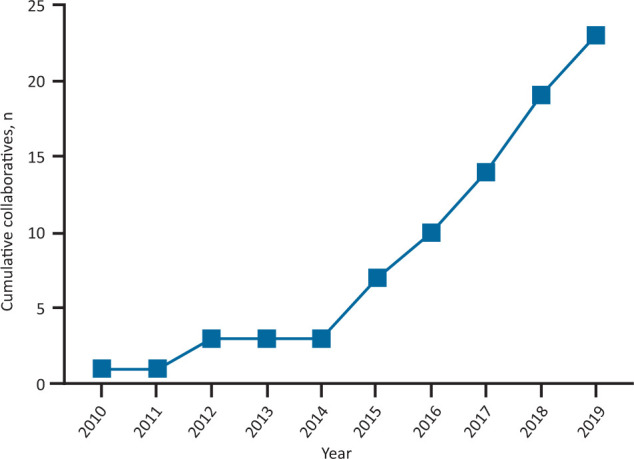
Establishment of trainee research collaboratives over time.
Provision of support for trainee research collaboratives
All collaboratives were supported by a consultant: 11 reported nominal support and 18 reported regular support (email and/or face-to-face) from one or more consultants. Consultant input was reported by 13 (57%) collaboratives during project planning (ethics applications and funding procurement), five (22%) collaboratives during project progression (data collection) and 13 (57%) collaboratives during project completion (manuscript drafting/editorial input; Fig 3). Seven (30%) collaboratives did not receive funding support for their research activity. The remainder procured funding through various sources including charitable organisations (nine; 39%), National Institute for Health Research (NIHR) (five; 22%), private industry (six; 26%), NHS trusts (one; 4%) and specialty societies (one; 4%).
Fig 3.
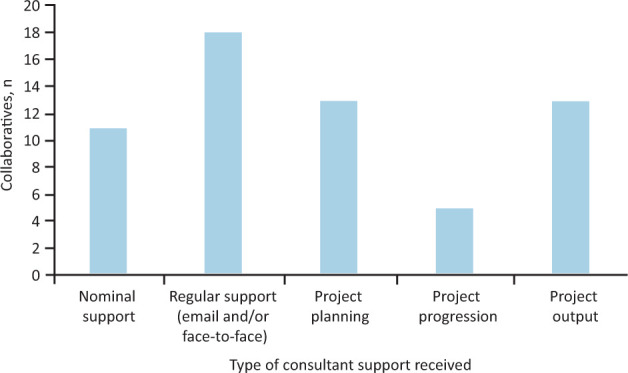
Consultant support for trainee research collaboratives.
Research activities and output of trainee research collaboratives in the last 5 years
All 23 collaboratives conducted audit, quality improvement and/or service evaluation projects. Other major project types included cohort studies (nine collaboratives), qualitative research projects (seven collaboratives), case series (three collaboratives) and one randomised controlled trial (Fig 4a). These projects resulted in both poster and oral presentations from 16 (70%) collaboratives. Twenty-one (91%) collaboratives reported presentations (oral and/or poster) at national or international forums. In total, the physician TRCs reported 136 PubMed-indexed publications: 18 (78%) collaboratives had published abstracts and 17 (74%) had published peer-reviewed journal articles (Fig 4b). At the time of survey, 16 (70%) collaboratives had two or more ongoing projects in progress. Thirteen (57%) collaboratives attained competitive awards or additional funding (two collaboratives from specialty societies, five collaboratives from charitable organisations, two collaboratives from NIHR, one collaborative from private industry and four collaboratives from miscellaneous sources).
Fig 4.
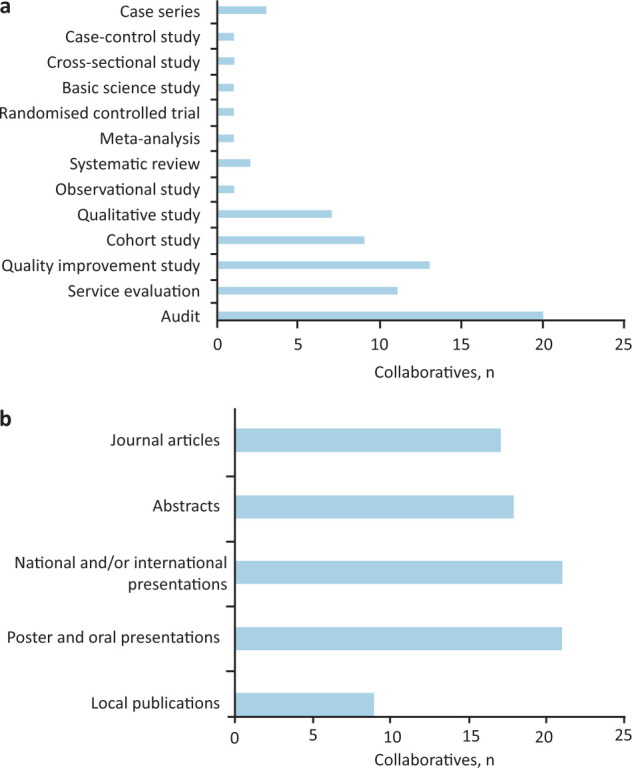
Research activities and output of trainee research collaboratives.
Benefits and challenges of trainee research collaboratives
In the survey, collaborative chairs and co-chairs were asked to indicate personal benefits, perceived benefits to the wider membership and the challenges to the goals of the collaborative (Table 1). Collectively, the common themes of benefit were improved patient care, personal development (leadership, management, and research and presentation skills), career progression and improved wellbeing. The three biggest challenges were time management, logistical support and financial support. Sixteen (70%) collaboratives indicated that ≤20% of their members had protected time to conduct project-related activities, and these were academic or out-of-programme trainees. The other key challenges identified were group authorship restrictions and obtaining support from training programmes, NHS trusts and universities.
Table 1.
Perceived benefits and challenges to collaboratives from the survey and focus group
| Perceived benefits to collaborative members |
|
| Perceived challenges to collaborative governance |
|
Focus group results
Overview
The focus group was held by teleconference in January 2021. Eight survey respondents were invited and five attended.
Time for research
Participants agreed that limitations on time represented one of the biggest challenges to trainee research collaborative success, particularly in the context of an already packed curriculum and limited time for higher specialty training. There was commonly a small group of more active members who would do the majority of the work for a collaborative project. For those out-of-programme for research (OOPR), it was perceived by trainees, and sometimes voiced by supervisors, that they were ‘stealing’ time from their main academic programme. Trainees without dedicated academic time did not feel supporting professional activities (SPA) time was sufficient for the work of TRCs and collaborative projects. However, participants emphasised that their collective view that the benefits outweighed the challenges, including opportunities for networking, publications and introducing trainees to academic career pathways. Proposed solutions included clearly identified sources of support, ranging from affiliation with a charitable, research or learning institution as well as a culture of support from consultant colleagues and supervisors.
Funding support for collaboratives
Participants sought funding from various sources, including the NIHR, national cancer research institute and other specialty- or disease-specific charities. Participants reported that previous unsuccessful funding applications were rejected due to concerns around accountability and sustainability of TRCs. Where funding had been secured, it was typically between £400 and £5,000. Participants agreed that most projects required small budgets to support them, however, larger sums would be useful for resources such as statistical and data management support. Nevertheless, access to funding was agreed as essential to optimise opportunities. Proposed solutions included competitive small grant funding opportunities from institutions such as the RCP and NIHR.
Senior support, mentorship and publication
All participants agreed dedicated consultant support for TRCs was essential. Experienced consultants were able to provide advice and guidance on study design and manuscript production without needing to give direct input. It was helpful to have access to at least one consultant with a formal academic affiliation. Participants desired additional support with data management and statistics for collaborative projects.
Authorship of research publications was a contentious issue. The approach to authorship is not standardised between collaboratives. Several collaboratives have adopted a collaborative authorship approach, yet reported receiving pushback from journals whose authorship policy does not account for corporate authorship models. On one occasion, a collaborative was invited to submit a paper to a journal, however, the journal significantly restricted the maximum number of authors and, therefore, the publication did not proceed. Collaborative chairs also described difficulty balancing the varied opinions of members with respect to the ethos of collaborative authorship.
Perceived benefits of collaboratives to the patient and public
Participants agreed that one of the key benefits of trainee research collaboratives was the opportunity to collect large multi-centre datasets (‘big data’), as trainees working across many organisations could contribute results to a single project. This meant that studies with accessible methodology (for example, audits) were more likely to achieve high levels of reliability and validity, and improve the potential for positive impact on patient care. Participants also expressed a view that trainees who worked ‘on the ground’ were more likely to conceptualise projects with real-world applicability. In addition, participants felt that collaboratives improved accessibility to academic training pathways and were capable of driving forward training in research, which all agreed would ultimately benefit patient care. All participants felt that collaborative working contributed towards the abolition of a culture of academics working in silos. Participants were hopeful for opportunities for improved collaboration between specialties.
Other skills developed as part of working in a collaborative (eg leadership and teamwork) were felt likely to benefit patient care in the long term. It was agreed that a culture of participating in research during training (without necessarily completing a formal qualification) encouraged trainees to make evidence-based medicine the norm.
Discussion
Our initial mapping exercise revealed that there are at least 35 physician TRCs active in the UK. This is in comparison with 34 known surgical collaboratives.10 The majority were established in the last 7 years. Surgical specialty curricula commonly require trainees to have achieved publication on completion of training.13 This is suggested to be a motivator to formation of surgical trainee research collaboratives. Despite there not being a publication requirement for physician trainees, it is clear that there remains a substantial motivation for establishment of physician TRCs.
For the first time, we have been able to describe the structure and scope of physician TRCs, which cover a diverse range of specialties and geographical regions. Not all physician specialties or geographical regions in the UK are represented. Gastroenterology, in particular, is over-represented in the TRCs nationally. This may be due to the large size of the specialty with several subspecialty areas, the close relationships between general surgery and gastroenterology facilitating the transfer of TRCs to the specialty at an earlier stage, and the TRC-specific support from the British Society of Gastroenterology, United European Gastroenterology, pharmaceutical companies and the UK gastroenterology charity Guts UK.14
In order to support networking opportunities, the RCP have published, with consent, the details of the identified collaboratives on the RCP Research and Innovation Hub.12
The survey and focus group allowed us to examine in detail the support received and desired by those in a leadership position in the collaboratives. This included consultant and institutional level support, financial support and authorship requirements.
Consultant-level support was identified as vital, yet, it is not consistent. It was noted that participation of academic trainees was important to the success of collaboratives, however, academic trainees in particular felt that they were not always supported to participate by their supervisors, and that they were struggling to justify time spent contributing to collaborative activity. A cultural shift in the relative worth of clinical collaborative research would be needed to address this, which would require key institutions including the RCP, NIHR, universities and research funders. Support mechanisms could be broad, comprising components such as mentorship schemes and specific opportunities for collaboratives to network and showcase their work.
Few respondents had protected time within their training for delivering research within their TRCs. This is despite JRCPTB physician trainee quality criteria recommending regular protected time for educational and research activities.15 While the COVID-19 pandemic has demonstrated the power of collaborative clinical research, it has also placed considerable burdens on trainees’ working lives, with time for educational and research activities reduced, and trainees missing out on required experiences for their clinical training. This may compromise the ability of trainees to engage in TRC activities, which are seen as extra to their curriculum requirements. Further support and time for carrying out research activity built into the curriculum will go a long way to encourage more clinical trainees to get involved with this TRC research activity. In the absence of this support, it falls to the few academic trainees who are not constrained by the arguably inflexible clinical working rota to invest more of their own time into keeping the research activity of TRCs on track.
Financial support for TRCs with access to small grants was identified as an important prerequisite for successful collaborative research. However, currently, there are considerable challenges and barriers to obtaining funding for TRCs, with anecdotal reports of academic and charitable institutions concerned about the accountability and sustainability of newly established TRCs. Developing formal senior support mechanisms for trainee collaboratives may mitigate this issue. In addition, wider access to dedicated, competitive funding sources would be of great benefit. The focus group participants emphasised that these resources would not need to be large, suggesting that a small investment may lead to large gains in the long term. It is noteworthy that the registered charity Guts UK was the most commonly cited small grant funding source for gastroenterology collaboratives, while gastroenterology had the greatest number of research collaboratives of any specialty.
Support of academic journals with respect to acknowledging a collaborative authorship approach was also desired. Having a clear set of regulations specifically targeted at trainee collaboratives could be one solution, as well as clear authorship guidelines for large groups of authors. This would also ease potential tensions within the collaboratives themselves, who could adapt their terms of reference accordingly.
We also examined the benefits of participation in TRCs. This included direct and indirect benefits to patient care, which is inclusive of personal and professional trainee development.
Despite the challenges faced, our findings suggest that physician TRCs are successfully producing useful and beneficial research and audit outputs. Meaningful output is arguably that which is most likely to contribute to improvement in patient care. During the focus group, it was discussed that trainees have a unique patient-centred perspective when conceptualising studies. Furthermore, the collaborative model collection of large volume data may improve validity and reliability of findings of relatively accessible methodological approaches, which come with the advantage of quicker turnaround compared with randomised control trials. This does not diminish the importance of high-quality methodology; participation in trainee research collaboratives (even on audit and quality improvement work) was felt to open doors to higher academic training pathways and, therefore, engage more clinicians in research activity as their careers progress.
Personal and professional development of physician trainees was identified, with skills learned that extend beyond academia, yet, are essential to providing excellent patient care; for example, leadership and teamworking. Survey respondents indicated a perception that participation improved the overall wellbeing of doctors in training, again a factor that can indirectly benefit patient care.
Royal colleges, specialty societies, funding bodies and charities are well-placed to nurture the development of physician TRCs. Royal colleges and specialty societies can establish training and mentorship for nascent TRCs, allowing them to learn from established TRCs and researchers who have delivered successful projects. Conferences can support and showcase the work of TRCs, while royal college and specialty society journals can examine their authorial policies to support corporate authorship models that fit better with collaborative research. Finally, these bodies can create specific ‘seed corn’ grants to support TRC research.
Limitations
Our methodology targeted trainees who held a leadership position in physician TRCs. These individuals are likely to have the requisite experience and insight required to accurately describe the benefits and challenges faced, however, their responses may not fully represent the views of the wider membership of TRCs, which we did not evaluate directly. Trainees engaged in TRCs, and those who took part in the focus group, are likely to be a self-selecting group whose views may not represent those of all trainees. The perspective of consultants involved in TRCs was not surveyed.
Conclusion
This project has established the scope and activity of physician TRCs in the UK. Physician TRCs have the potential to improve patient care both directly through their quality improvement and research projects, and indirectly through the development of improved research, leadership and collaborative working skills in the trainees involved. Physician TRCs will benefit from targeted long-term support to contribute to the wider UK research agenda. Key items for consideration include consultant-level support, institutional support, access to small volume funding opportunities and support for collaborative authorship models. Relatively modest investments in support and funding for physician TRCs has the potential to yield great benefits for UK medical research and patient care.
Summary
What is known?
Regional, national and international physician trainee research collaboratives (TRCs) have been established in recent years in many specialties to provides trainees the opportunity to develop research skills.
What is the question?
What are the benefits of physician TRCs and what are the challenges and experiences faced?
What was found?
Physician TRCs produce high-quality academic output through reliance on a select group of motivated trainees and additional consultant support. Benefits identified were improved patient care both directly through quality improvement and research projects, and indirectly through the development of improved research, leadership and collaborative working skills. Challenges include lack of access to consultant-level and institutional-level support, sustainable funding, time constraints, and authorship and contributor recognition difficulties.
What is the implication for practice now?
Physician TRCs continue to produce relevant clinical research and must be supported by academic institutions, NHS trusts, royal colleges and funding bodies in order to produce sustainable networks going into the future.
References
- 1.General Medical Council . Generic professional capabilities framework. GMC, 2017. www.gmc-uk.org/-/media/documents/generic-professional-capabilities-framework–0817_pdf-70417127.pdf [Accessed 12 July 2021]. [Google Scholar]
- 2.West Midlands Research Training Collaboratives. https://wmrtc.org.uk/about [Accessed 12 November 2021].
- 3.Bhangu A, Kolias AG, Pinkney T, et al. Surgical research collaboratives in the UK. Lancet 2013;382:1091–2. [DOI] [PubMed] [Google Scholar]
- 4.Nepogodiev D, Chapman SJ, Kolias AG, et al. The effect of trainee research collaboratives in the UK. Lancet Gastroenterol Hepatol 2017;2:247–8. [DOI] [PubMed] [Google Scholar]
- 5.Jamjoom AAB, Phan PNH, Hutchinson PJ, Kolias AG. Surgical trainee research collaboratives in the UK: An observational study of research activity and publication productivity. BMJ Open 2016;6:e010374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pinkney TD, Calvert M, Bartlett DC, et al. Impact of wound edge protection devices on surgical site infection after laparotomy: multicentre randomised controlled trial (ROSSINI trial). BMJ 2013;347:f4305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.COVIDSurg Collaborative, GlobalSurg Collaborative . Timing of surgery following SARS-CoV-2 infection: an international prospective cohort study. Anaesthesia 2021;76:748–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guinness World Records . Most authors on a single peer-reviewed academic paper. Guinness World Records, 2021. www.guinnessworldrecords.com/world-records/653537-most-authors-on-a-single-peer-reviewed-academic-paper [Accessed 12 November 2021]. [Google Scholar]
- 9.Royal College of Physicians . Research for all: Developing, delivering and driving better research. RCP, 2020. www.rcplondon.ac.uk/;projects/outputs/research-all-developing-delivering-and-driving-better-research [Accessed 12 July 2021]. [Google Scholar]
- 10.National Research Collaborative . The collaboratives. National Research Collaborative. https://nationalresearch.co.uk/the-collaboratives [Accessed 21 July 2021]. [Google Scholar]
- 11.Health Research Authority . Do I need NHS REC review? HRA. www.hra-decisiontools.org.uk/ethics [Accessed 21 July 2021]. [Google Scholar]
- 12.Royal College of Physicians . Trainee research collaboratives. RCP, www.rcplondon.ac.uk/trainee-research-collaboratives [Accessed 12 July 2021]. [Google Scholar]
- 13.Lee MJ, Bhangu A, Blencowe NS, et al. Academic requirements for Certificate of Completion of Training in surgical training: Consensus recommendations from the Association of Surgeons in Training/National Research Collaborative Consensus Group. International Journal of Surgery 2016;36:s24–30. [DOI] [PubMed] [Google Scholar]
- 14.Guts UK . GutsUK/BSG Trainee Awards. Guts UK. https://gutscharity.org.uk/research/grants-and-awards/guts-uk-bsg-trainee-research-grants [Accessed 12 Nov 2021]. [Google Scholar]
- 15.Joint Royal Colleges of Physicians Training Board . Quality criteria for GIM/AIM registrars. JRCPTB. www.jrcptb.org.uk/quality/quality-criteria-gimaim [Accessed 12 November 2021]. [Google Scholar]


