ABSTRACT
Introduction:
Low back pain (LBP) is ranked as the first musculoskeletal disorder considering years lived with disability worldwide. Despite numerous guidelines promoting a bio-psycho-social (BPS) approach in the management of patients with LBP, many health care professionals (HCPs) still manage LBP patients mainly from a biomedical point of view.
Objective:
The purpose of this pilot study was to evaluate the feasibility of implementing an interactive e-learning module on the management of LBP in HCPs.
Methods:
n total 22 HCPs evaluated the feasibility of the e-learning module with a questionnaire and open questions. Participants filled in the Back Pain Attitude Questionnaire (Back-PAQ) before and after completing the module to evaluate their attitudes and beliefs about LBP.
Results
The module was structured and easy to complete (91%) and met the expectations of the participants (86%). A majority agreed that the module improved their knowledge (69%). Some participants (77%) identified specific topics that might be discussed in more detail in the module. HCPs knowledge, beliefs and attitudes about LBP significantly improved following module completion (t = −7.63, P < .001) with a very large effect size (ds = −1.63).
Conclusion
I The module seems promising to change knowledge, attitudes and beliefs of the participants. There is an urgent need to develop and investigate the effect of educational interventions to favor best practice in LBP management and this type of e-learning support could promote the transition from a biomedical to a bio-psycho-social management of LBP in HCPs.
KEYWORDS: Distance education, musculoskeletal pain, physicians, physical therapists, guideline adherence
Introduction
Low back pain (LBP) represents a major health issue worldwide and is one of the leading causes of disability [1–3]. In most cases the pain cannot be attributed to a specific underlying pathology, hence the term nonspecific LBP [3,4]. LBP is often defined as a multidimensional condition, involving biological, social and psychological factors. Despite the recommended biopsychosocial (BPS) approach in the management of patients with LBP [5–8], many healthcare professionals (HCPs) still manage patients mainly from a biomedical point of view [7]. Their search for a biomedical explanation for LBP is reflected by overuse of medical imaging and medication [9], advice to restrict work and activities [10], and insufficient attention toward psychosocial risk factors during actual consultations [11], which is all guideline discordant. HCPs’ beliefs and attitudes might influence patient’s beliefs [12] and negatively affect their prognosis [13]. Interestingly HCPs can also have a positive influence on patient’s beliefs. For example, explaining the multidimensional cause of pain, reassuring the patient about the prognosis, giving advice to stay active and return to work as fast as possible, will help the patient understand his condition and to better cope with it [14–18]. A first step in the process of change is to make sure that HCPs’ beliefs and attitudes are in line with the evidence-based guidelines.
Different interventions with a purpose to change HCPs’ beliefs and attitudes have been carried out but with marginal effects only [19–22]. These interventions most often consisted of passive e-learning modules, lectures and/or information brochures [19–22]. One study asked HCPs to attend a traditional lecture regarding the BPS approach of LBP. After the study the patients did not perceive a difference in HCPs’ clinical behavior [23]. This lack of effectiveness can be attributed to the fact that listening to a lecture or reading a brochure is a rather passive method, which seems not helpful to change the HCP’s behavior. A change in used methodology to train the HCPs is needed. Growing evidence confirms the complexity of LBP which explains the disappointing progress of LBP research and defies researchers to think more broadly and creatively [24].
Active strategies seem necessary to change the behavior of a professional and the used methodology should include interaction and feedback [25]. Using e-learning is an easy way to promote interactivity (e.g. questions with feedback), repetition and spacing between the different activities, or controllable navigation [26]. The latter allows participants to control the progression in their learning [27]. Besides, the use of role-plays, standardized patients and interactive demonstrations of key skills in action are recommended as they increase this interactivity [28,29]. For example a study integrated in their e-learning several clinical scenarios and case descriptions for which the participant needed to give a clinical evaluation [30]. The authors observed significant improvement on HCPs’ attitudes, knowledge and comprehension of communication skills following the intervention [30]. Another study used mixed training activity integrating traditional lectures and practical lessons (functional exercise and communication skills). The results showed that these active methods significantly improved attitudes and beliefs of physiotherapy students about LBP after the module [31].
E-learning modules have already been used in several healthcare domains [32–36] with positive results, sometimes even better than face-to-face instruction [27]. Some HCPs have difficulties to follow continued education to update their knowledge and skills because of lack of time [37]. E-learning modules allow HCPs to complete them with a certain flexibility in the time and location [38–40].
We developed an interactive e-learning module to enhance HCPs’ knowledge, attitudes and beliefs regarding the management of patients with LBP from a BPS approach. This pilot study will investigate the feasibility of an interactive e-learning module by examining its content, structure and presentation, length and access, and the change regarding HCP’s knowledge and beliefs.
Methods
Study design and ethical aspects
A pilot study was conducted to investigate the feasibility of an interactive e-learning module about the knowledge, beliefs and attitudes in the management of LBP in a sample of HCPs. The study was approved by the ethical commission of the University Hospital Saint-Luc (CEHF) in Brussels, Belgium on 13 January 2020.
Participants
A small sample of convenience of HCPs (n = 17) and medical or physiotherapy students (n = 5) was recruited (see Table 1). The module was open to several health care professions such as general physicians, orthopedists, physiotherapists, psychologists, nurses and occupational therapists. The students included were in their last year of physiotherapy or medicine.
Table 1.
Results of socio-demographic data
| Participants | Age (year) | Gender (Man or Woman) | Nationality | Healthcare Professionals | Years of practice | LBP patients per week | |
|---|---|---|---|---|---|---|---|
| 1 | 46 | M | Belgian | Physiotherapist | 20 | 6 | |
| 2 | 44 | W | Belgian | Nurse | 22 | 5 | |
| 3 | 43 | M | Belgian | Physiotherapist | 20 | 30 | |
| 4 | 50 | M | Belgian | Back surgeon | 20 | 80 | |
| 5 | 59 | W | Belgian | General practitioner | 34 | 18 | |
| 6 | 61 | M | Belgian | Physiotherapist | 38 | 100 | |
| 7 | 44 | W | Belgian | Physiotherapist | 20 | 5 | |
| 8 | 31 | W | Belgian | Physiotherapist | 2 | 10 | |
| 9 | 23 | W | Belgian | Physiotherapist | 2 | 6 | |
| 10 | 22 | W | Belgian | Physiotherapist | 2 | 3 | |
| 11 | 54 | W | Belgian | Physiotherapist | 30 | 20 | |
| 12 | 24 | M | Belgian | Physiotherapist | 1 | 15 | |
| 13 | 24 | W | Belgian | Student in physiotherapy | 0 | 5 | |
| 14 | 48 | W | French | General practitioner | 25 | 4 | |
| 15 | 24 | W | French | Student in physiotherapy | 0 | 0 | |
| 16 | 29 | W | Belgian | Physiotherapist | 4 | 8 | |
| 17 | 23 | W | Belgian | Student in physiotherapy | 0 | 0 | |
| 18 | 44 | M | Belgian | General practitioner | 18 | 3 | |
| 19 | 50 | M | Belgian | General practitioner | 25 | 5 | |
| 20 | 25 | M | Belgian | General practitioner | 2 | 7 | |
| 21 | 23 | W | Belgian | Medical student | 0 | 0 | |
| |
22 |
23 |
M |
Belgian |
Student in physiotherapy |
0 |
0 |
| Mean (SD) or n (%) | 22 (100%) | 37 (13.5) |
Men: 9 (40.9%) |
Belgian: 20 (90.9 %) |
Physicians: 6 (27.3%) |
13 (13) | 15 (25.6) |
| Women: 13 (59.1 %) |
French: 2 (9.1 %) |
Physiotherapists: 10 (45.5 %) | |||||
|
Students: 5 (22.7%) |
|||||||
| Nurse: 1 (4.5%) |
HCPs and students were eligible if they were aged between 23 and 65 years old and took care of patients suffering from LBP in their daily clinical practice or internships.
The exclusion criteria were: not being in possession of an Internet-connected device, or non-French speaking professionals.
Procedure
The enrollment took place between February and April 2020 in Belgium and France. HCPs and students were recruited by phone calls. They were told they would be asked to follow an interactive e-learning module on the management of LBP and fill in different questionnaires. A single appointment was planned (one session of one hour) with each participant. Participants were aware that no financial compensation was provided for their time and effort spent in the study.
For the nine first participants a physical appointment was made with the researcher in a location chosen by the participant (e.g. clinical practice). The participants first filled in a written informed consent and the Back-PAQ questionnaire on an online platform (see Appendix 1). The researcher installed the e-learning module on the personal device of the participant. Then the researcher explained how to navigate in the e-learning. The researcher was available in case of technical difficulties. After completing the module, participants were asked to fill in the Back-PAQ for post-evaluation and a feasibility questionnaire on the same online platform (see Appendix 2). Because of the COVID-19 pandemic physical appointments with the next participants were not possible. After the phone recruitment, the next thirteen participants received a link by e-mail to fill in the online questionnaires and follow the interactive e-learning module remotely on an online platform and in a personal location.
Interactive e-learning module
The main objective of this pilot study is to examine the feasibility of an e-learning intervention regarding the management of LBP. The e-learning intervention included written parts, voice-overs and clinical encounter videos.
Development process
The interactive e-learning module has been jointly developed by a multidisciplinary team of researchers and clinicians with complementary expertise. This international team (Belgium and France) involved professions such as physiotherapists, physicians (both general practitioners and specialized physicians), sociologists and professors in prevention of musculoskeletal disorders. Its content is based on recent guidelines from different countries for the management of LBP (e.g. Belgium, United Kingdom) [8,41,42].
Access
The interactive e-learning module, the Back-PAQ and the feasibility questionnaire were available in French. The module could be completed from home, work or any other place with an internet connected device of participant’s choice. The module was only available for the duration of the study.
Structure and content
The interactive e-learning module consisted of one session structured on 4 topics (see Figure 1). The planned duration was 60 minutes. In total, it included 61 slides with written information, voice-overs, 4 face-cam videos explanations, and 2 clinical encounter videos of respectively 6 and 8 minutes.
Figure 1.
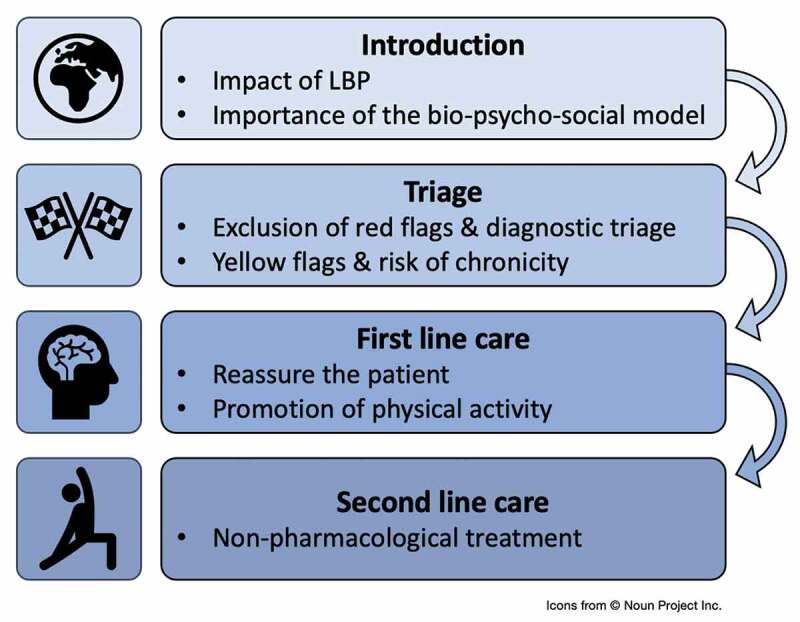
Structure of the interactive e-learning module.
The interactive e-learning module provided information about the adequate management of the LBP patient. The e-learning module was structured around four main themes:
1) Introduction
The module provided an introduction of the burden of LBP and the need for a multidimensional and patient-centered approach for the management of LBP [43–45].
2) Triage and evaluation
In this part, the assessment of a patient suffering from LBP was discussed with as main focus a diagnostic triage (to differentiate between specific spinal pathologies, radicular symptoms and nonspecific LBP), and a yellow flag screening and risk stratification according to the STarT Back Tool [46,47].
3) First line care
First line management consists of reassurance about the symptoms and giving advice about the importance of staying active. This must be proposed to all patients (low, medium and high risk). HCPs were briefly informed about the neurophysiology of pain (e.g. the difference between nociception and pain, etc.), how to communicate and reassure their patients (e.g. the benign aspect of LBP) (4 face-cam videos).
4) Second line care
This last part of the module explored the non-pharmacological management of LBP. Additional therapies (exercises, manual treatments and psychological interventions oriented by the physiotherapist) were discussed for patients at low risk for developing chronic/persistent pain not responding to education and to medium risk patients. In case of failure, a multidisciplinary approach is recommended. This last approach is also suggested for high-risk patients.
At the end, the module consisted of two short clinical encounter videos summarizing the content of the full module. The first video displayed a consult between a general practitioner and a patient suffering from acute LBP. The second one presented the same consult with a patient suffering from chronic LBP. The two videos included examples of how to reassure patients about their condition.
Human involvement, co-interventions and prompts
An investigator was present for the nine first participants during the completion of the module for technical support but no other support or intervention (involving information about the content) was provided. The thirteen other participants could contact the investigator by mail or by phone for any technological issues. There were no co-interventions or prompts.
Feasibility questionnaire
A questionnaire was developed to assess the feasibility of this module. In total, 20 items were included based on previous feasibility studies [22,30,33,34,37,48–54]. Likert Scales (n = 15) and open questions (n = 5) were both used to record HCPs’ opinions (see Appendix 2). The open questions were audio recorded for the first nine participants and the thirteen others gave written answers online.
The focus of this feasibility study was to investigate HCPs’ opinions about the module, including their suggestions about how to improve this module. Therefore, most of the items were related to the participants satisfaction about the content, structure and presentation, length and access of the module. Demographic data was also collected through this questionnaire.
Back pain attitudes questionnaire (Back-PAQ)
Before and after the module, participants filled in the validated French version of the Back-PAQ questionnaire (34 items version) [55]. This questionnaire assesses attitudes and underlying beliefs about back pain on a 5-point Likert scale. The scoring of the answers ranges from −2 to +2. A negative score reflects beliefs that are unhelpful and vice-versa [56]. All items were written in the second person to personalize the questionnaire. The purpose of this personalization is that HCPs or students present their own beliefs rather than projecting their beliefs onto people with LBP or presenting their beliefs about people with LBP [56]. It allowed us to investigate the potential change of beliefs about their own back induced by the interactive e-learning module (see Appendix 1).
Statistical analysis
All statistical analysis were computed with Microsoft Excel 16.43 and RStudio 1.3.959–1 (RStudio Team 2020).
Sociodemographic data
Means and standard deviations (SD) were calculated for continuous variables and counts (age, years of practice, number of patients with LBP per week) and percentages for categorical variables (gender, nationality, work).
Feasibility data
Data were retrieved from the feasibility questionnaire. The Likert scales were analyzed using median and minimum – maximum or counts and percentages. Open questions were used to support the results obtained from the Likert scales.
Back-PAQ
Changes between pre- and post-module measures were compared using a 2-sided paired Student t-test with a significance level of .05. The effect size between pre- and post-module measures was calculated using Cohen’s ds [57]. Interpretation of effect size was: small (ds = 0.2), medium (ds = 0.5), large (ds = 0.8), very large (ds = 1.2), and huge (ds = 2.0) [58]. A negative Cohen’s ds indicate an improvement of the Back-PAQ score after the module.
Results
Socio-demographic results
In total, 22 participants (9 men and 13 women) took part in this pilot study. Mean age ± SD was 37 ± 13.5 years old. Regarding the health disciplines, 45.5% were physiotherapists, 27% physicians, 23% last year students in medicine or physiotherapy and 4.5% nurses. Participant’s experience ranged from 0 (i.e. the students) to 38 years with a mean of 13.5 ± 13 years. They treated a mean of 15 ± 26 patients suffering from LBP per week (see Table 1).
Feasibility results
Changes in knowledge and beliefs
About 69% of the participants agreed that the module improved their knowledge while 23% strongly disagreed. A total of 54% agreed that their beliefs changed whereas 41% disagreed. Up to 86% of the participants intend to use their new skills in their clinical practice (see Table 2 and Figure 2).
Table 2.
Results of the feasibility questionnaire
| Possible range | Mean (SD) | Median (min-max) | Mode | |
|---|---|---|---|---|
| Content | ||||
| Sufficiency | 1–5 | 4.5 (1) | 5 (1–5) | 5 |
| Attractiveness | 1–5 | 4.1 (1) | 4.5 (1–5) | 5 |
| Meetings of expectations | 1–5 | 4.3 (1) | 5 (1–5) | 5 |
| Structure and Presentation | ||||
| Attractiveness | 1–5 | 4.4 (0.7) | 4.5 (3–5) | 5 |
| Clarity | 1–5 | 4.8 (0.4) | 5 (4–5) | 5 |
| Structure | 1–5 | 4.6 (0.8) | 5 (2–5) | 5 |
| Changes in knowledge and beliefs | ||||
| Improvement in knowledge | 1–5 | 3.8 (1.4) | 4 (1–5) | 5 |
| Change in beliefs | 1–5 | 3.1 (1.6) | 4 (1–5) | 5 |
| Time (minutes) | ||||
| 37.6 (9.6) | 39.5 (20–60) | 40 |
Figure 2.
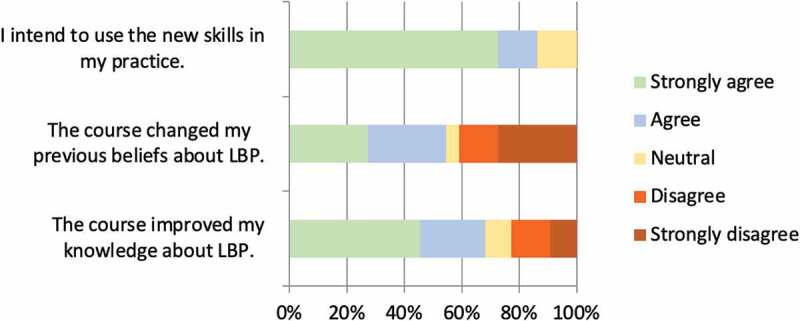
Feasibility results about the change in knowledge and beliefs.
Content of the module
About 73% of the participants agreed that the content of the module was attractive and stimulating. A total of 86% agreed that the module met their expectations. Most of the participants (91%) found that this interactive e-learning module was able to enhance knowledge of HCPs (see Table 2 and Figure 3). According to the participants, a beneficial aspect of the module was its capacity ‘to re-contextualize and to look at LBP from a different point of view’ . However, up to 77% of the participants identified some topics such as the psychological aspects of LBP or the type of exercises to prescribe that might be discussed more in detail in a revised version of the module. The opinions about the clinical encounter videos content diverged. While 25% of the participants mentioned that the short clinical encounter videos ‘were too long and theoretical’ or found them ‘a waste of time’, other participants said that it was ‘a nice way to summarize the module and to see practically how to interact with a patient.’
Figure 3.
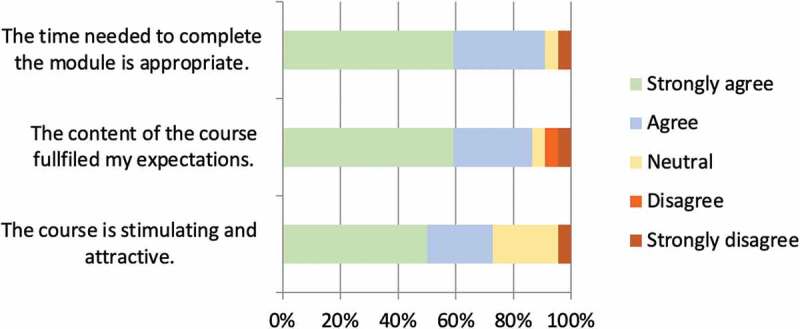
Feasibility results about the content and time.
Structure and presentation of the module
A total of 78% of the participants agreed that the presentation sustained their learning. Indeed, 91% of the participants found the module structured and easy to complete. About 91% of the participants agreed with the appeal of the presentation (see Table 2 and Figure 4).
Figure 4.
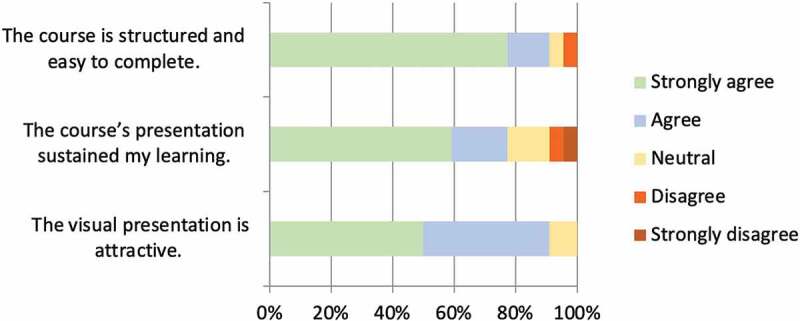
Feasibility results about the structure and presentation.
Length of the module
Participants took 36.6 ± 10 minutes to complete the module. A total of 91% of the participants found the time frame adequate (see Table 2 and Figure 3).
Access
A total of 76% did not encounter technical problems and 91% of the participants were comfortable with the use of a computer (see Figure 5). Some participants mentioned that one of the most beneficial aspects of the interactive e-learning was ‘the freedom offered to complete it whenever or wherever you want’.
Figure 5.
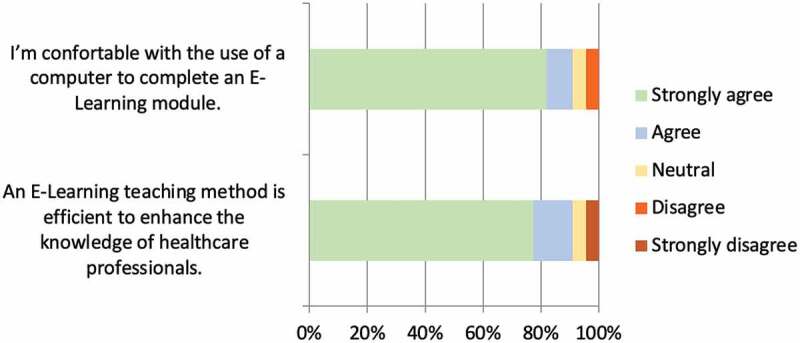
Feasibility results about the access.
Back-PAQ
A significant improvement was seen in the Back-PAQ scores (see Figure 6) after the participation in the module (t = −7.63, P < .001) with a very large effect size (ds = −1.63). Participants have been sub-grouped according to the years of practice experience (Student with no years of experience (n = 5); < 20 years (n = 7); between 20 and 29 years (n = 7); ≥ 30 years (n = 3)). All sub-groups showed a significant difference in their pre- and post-module scores (See Figure 7): the student’s group with no years of experience (t = −6.12, P = 0.003), the group < 20 years (t = −3.12, P = 0.02), the group between 20 and 29 years (t = −5.16, P = 0.01) and the group ≥ 30 years (t = −8.32, P = 0.01). A very large effect size was observed in the group < 20 years (ds = −1.18) while a huge effect size was observed in the student’s group (ds = −2.74), the group between 20 and 29 years (ds = −1.95) and the group ≥ 30 years (ds = −4.8).
Figure 6.
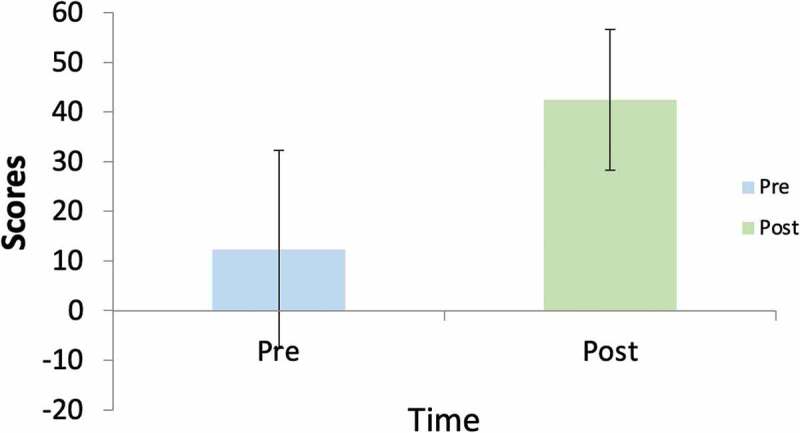
Back-PAQ results before and after the completion of the e-learning module.
Figure 7.
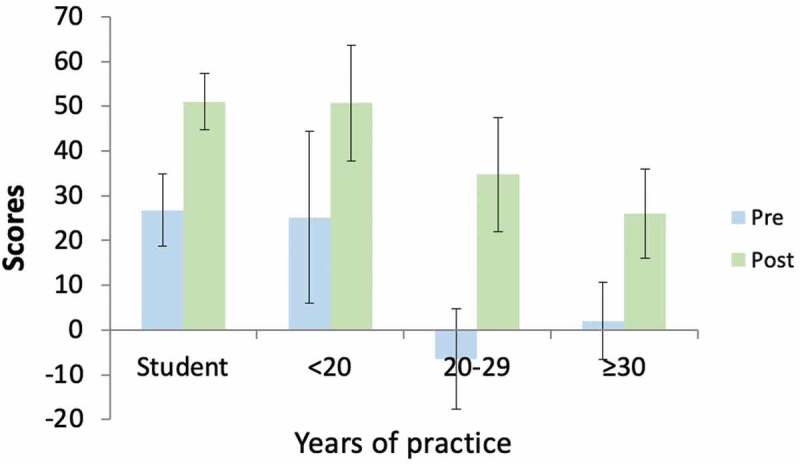
Back-PAQ results sub-grouped by years of practice before and after the completion of the e-learning module.
Discussion
The results of this pilot study reveal that the interactive e-learning module was highly appreciated by the majority of the participants.
Participants found the content of the intervention sufficient and clear. They estimated the module to be efficient to explore the management of LBP. ‘Patient’s reassurance about the benign aspect of LBP is essential’, ‘Clear explanations that medical imagery does not correlate with the symptoms’, ‘Reconsidering our absolute truths’, ‘Promoting conservative care management and movement’ were the principal strengths. Some suggestions were made to improve the module. For example, some participants suggested to discuss the psychological aspects of LBP more in detail as well as the role of psychologists. ‘The psychological and emotional aspects of LBP often play a primordial role in the development of LBP; it might be interesting to explore it more deeply’. These results confirm previous research revealing that physiotherapists may lack confidence to deliver a psychologically informed approach to their patients [59] and that this approach should be better integrated into the physiotherapy training curriculum, at least in French-speaking Belgium and France. Other participants highlighted the importance of exercise and wondered whether information regarding the type of exercises could be more elaborated in the module. The type and examples of exercises are not elaborated in the guidelines and the recommendation is to use a time-contingent approach [8,41,42].
Participants were satisfied by the module’s presentation and structure. Participants said: ‘the structure was very clear’, ‘the module was interactive, clear and interesting’. We believe therefore that it sustained their learning process.
The majority of the participants was satisfied with the length and the time to complete the interactive e-learning module. Participants took less than one hour (time originally estimated) to complete it.
Effectiveness
The results of the feasibility questionnaire suggest that a majority of HCPs found an e-learning teaching method able to enhance their knowledge. Similar results have been found in several studies. It is known that e-learning is an effective way to improve knowledge in health care area [22,38,49,60]. Participants mentioned that its accessibility and flexibility were its greatest advantages. Indeed, they had the control of the time and location of the module’s completion. Those results have been reported in other studies [22,38,49].
According to the Back-PAQ questionnaire, the interactive e-learning module might be promising to change HCPs’ or students’ knowledge and beliefs about their back. These results are in accordance with studies who report a significant change in beliefs about back pain following an educational intervention [31,61–63]. Interactive e-learning modules have already been used to improve HCPs’ knowledge and self-confidence in their communication skills [39,49,60]. Furthermore, it has been suggested that biopsychosocial-based content are more effective in reducing negatives beliefs in HCPs than biomedical ones [7,64,65]. However, a Cochrane review on e-learning modalities showed little or no difference in HCPs’ knowledge compared to traditional learning [66]. This pilot study did not compare the e-learning module with other learning modalities. The results of the Back-PAQ questionnaire showed that clinicians with less years of clinical practice had better scores pre- and post-module. It could indicate an enhancement in the teaching of the BPS management of LBP in higher education. Nonetheless, even though the Back-PAQ scores showed a significant improvement after the intervention, half of the participants did not have the feeling that their beliefs had changed after completing the module. It might be explained by two different phenomena: confirmation bias and cognitive dissonance [67,68]. Confirmation bias is the tendency to search for information that confirms or strengthens prior personal beliefs opposed to looking for data that challenge those beliefs [68]. Cognitive dissonance is a well-known psychosocial theory. It is experienced in situations involving conflicting attitudes, beliefs or behaviors. When confronting conflicting beliefs, we feel a mental discomfort leading to an alteration in one of the attitudes, beliefs or behaviors to reduce the discomfort [67]. In our case, participants may have been confronted to beliefs that contradicted their previous ones. It created discomfort that led them to adjust their prior personal beliefs unconsciously. The difference between the HCPs perception of change and the quantitative results from the Back-PAQ could also be explained by the sensitivity of the measurement tools. The perception of the change in beliefs of HCPs was measured by using a question rated on a Likert scale, probably not as sensitive as the validated Back-PAQ questionnaire.
Strengths and limitations
This study had a small sample size, as only 22 participants were recruited. Because of the COVID-19 pandemic, nine participants followed the module in presence of an experimenter whilst thirteen completed it online without assistance. For the first nine participants we were able to record their answers for the open questions. It allowed more complete answers and feedbacks to enhance the module, which was not the case for the other participants. Because of the pandemic the recruitment has been limited and some professions are not represented in our sample (e.g. psychologists and occupational therapists). Selection bias due to convenient sampling could also influence the results. The results concerning the change in attitude and beliefs of the participants regarding the effectiveness of this e-learning module are preliminary and should be interpreted with caution. Further studies should evaluate the updated version of this e-learning module in a large randomized controlled trial.
This study has several strengths as well. First, the heterogeneity of participants’ health disciplines allowed us to record diversified feedbacks. Second, none of the participants dropped out during the module’s completion. Third, the module used role-modeling videos and interactivity, which was mostly appreciated by the participants and could participate in a change in knowledge and beliefs. Finally, the module was developed based on several recent evidence-based guidelines for LBP management.
Conclusion
This interactive e-learning module seems feasible and promising to change knowledge and beliefs in a majority of HCPs or last year students in medicine or physiotherapy. Participants evaluated it positively: it was attractive, structured and clear. Moreover, the module was accessible and easy to follow. The content was sufficient and met the expectations of the participants. Some suggestions have been made to improve it such as investigate more deeply the emotional and psychological impact of LBP. There is an urgent need to develop and investigate the effect of educational interventions to favor best practice in LBP [31,69] and this type of e-learning support could promote the transition from a biomedical to a bio-psycho-social management of LBP in HCPs. Future studies should evaluate the effects of a revised version of the e-learning on larger samples and with experimental designs that will reveal the relative effectiveness of different e-learning modalities.
Acknowledgments
The authors would like to thank Isaline Demeure and Sebastiaan Naessens (University of Antwerp) for their input and critical reflection regarding the creation of the e-learning module.
Funding Statement
With the financial support of the European Regional Development Fund (Interreg FWVl NOMADe - N° 4.7.360);
Abbreviations
Back-PAQ: Back Pain and Attitudes Questionnaire
BPS: Biopsychosocial
HCPs: Healthcare professionals
LBP: Low back pain
Disclosure Statement
No potential conflict of interest was reported by the author(s).
References
- [1].Sullivan PO, and Caneiro JP.. Unraveling the complexity of low back pain Journal of Orthopaedic & Sports Physical Therapy . 2016;46(11):932–937. [DOI] [PubMed] [Google Scholar]
- [2].Buchbinder R, Van Tulder M, Öberg B, et al. Low back pain: a call for action. Lancet. 2018. Jun;391(10137):2384–2388. PMID: 29573871 [DOI] [PubMed] [Google Scholar]
- [3].Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet. 2018. Jun;391(10137):2356–2367. [DOI] [PubMed] [Google Scholar]
- [4].Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet. 2017. Feb;389(10070):736–747. [DOI] [PubMed] [Google Scholar]
- [5].Kamper SJ, Yamato TP, Williams CM. The prevalence, risk factors, prognosis and treatment for back pain in children and adolescents: an overview of systematic reviews. Best Pract Res Clin Rheumatol. 2016. Dec;30(6):1021–1036. [DOI] [PubMed] [Google Scholar]
- [6].Nielens H, Zundert J, Mairiaux P, et al. Chronic low back pain. Good clinical practice (GCP). 2006. Dec 1; [Google Scholar]
- [7].Foster NE, Anema JR, Cherkin D, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet. 2018. Jun;391(10137):2368–2383. [DOI] [PubMed] [Google Scholar]
- [8].Van Wambeke Leuven PU, President G, and Desomer A. (2nd edition; 1st edition: 19 May 2017) , et al. KCE REPORT 287Cs SUMMARY LOW BACK PAIN AND RADICULAR PAIN: ASSESSMENT AND MANAGEMENT. 2017. accessed 27 November 2017; Available from: www.kce.fgov.be
- [9].Mafi JN, McCarthy EP, Davis RB, et al. Worsening trends in the management and treatment of back pain. JAMA Intern Med. 2013. Sep 23;173(17):1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Darlow B, Fullen BM, Dean S, et al. The association between health care professional attitudes and beliefs and the attitudes and beliefs, clinical management, and outcomes of patients with low back pain: a systematic review: the association between health care professional attitudes and outcomes of patients with low back pain. Eur J Pain. 2012. Jan;16(1):3–17. [DOI] [PubMed] [Google Scholar]
- [11].Roussel NA, Neels H, Kuppens K, et al. History taking by physiotherapists with low back pain patients: are illness perceptions addressed properly? Disabil Rehabil. 2016. Jun 18;38(13):1268–1279. [DOI] [PubMed] [Google Scholar]
- [12].Gardner T, Refshauge K, Smith L, et al. Physiotherapists’ beliefs and attitudes influence clinical practice in chronic low back pain: a systematic review of quantitative and qualitative studies. J Physiother Korea Inst Orient Med. 2017;63(3):132–143. [DOI] [PubMed] [Google Scholar]
- [13].Hayden JA, Wilson MN, Riley RD, et al. Individual recovery expectations and prognosis of outcomes in non-specific low back pain: prognostic factor review. Cochrane Database Syst Rev. 2019. Nov 25. DOI: 10.1002/14651858.CD011284.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Darlow B. Beliefs about back pain: the confluence of client, clinician and community. Int J Osteopath Med. 2016;20:53–61. [Google Scholar]
- [15].Louw A, Zimney K, Puentedura EJ, et al. The efficacy of pain neuroscience education on musculoskeletal pain: a systematic review of the literature. Physiother Theory Pract. 2016;32(5):332–355. PMID: 27351541 [DOI] [PubMed] [Google Scholar]
- [16].O’Keeffe M, O’Sullivan PB, O’Sullivan K. Education can “change the world”: can clinical education change the trajectory of individuals with back pain? Br J Sports Med. 2019;53(22):1385–1386. [DOI] [PubMed] [Google Scholar]
- [17].Puentedura EJ, Flynn T. Combining manual therapy with pain neuroscience education in the treatment of chronic low back pain: a narrative review of the literature. Physiother Theory Pract. 2016. Jul 3;32(5):408–414. [DOI] [PubMed] [Google Scholar]
- [18].Watson JA, Ryan CG, Cooper L, et al. Pain neuroscience education for adults with chronic musculoskeletal pain: a mixed-methods systematic review and meta-analysis. J Pain. 2019;20(10):1140.e1–1140.e22. PMID: 30831273 [DOI] [PubMed] [Google Scholar]
- [19].Henrotin Y, Moyse D, Bazin T, et al. Study of the information delivery by general practitioners and rheumatologists to patients with acute low back pain. Eur Spine J. 2011;20(5):720–730. PMID: 21069543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Bekkering GE, Engers AJ, Wensing M, et al. Development of an implementation strategy for physiotherapy guidelines on low back pain. Aust J Physiother. 2003;49(3):208–214. [DOI] [PubMed] [Google Scholar]
- [21].Stevenson K, Lewis M, Hay E. Does physiotherapy management of low back pain change as a result of an evidence-based educational programme? J Eval Clin Pract. 2006;12(3):365–375. [DOI] [PubMed] [Google Scholar]
- [22].Jacobs ZG, Michael Elnicki D, Perera S, et al. An E-learning module on chronic low back pain in older adults: effect on medical resident attitudes, confidence, knowledge, and clinical skills. Pain Med U S. 2018;19(6):1112–1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Overmeer T, Boersma K, Main CJ, et al. Do physical therapists change their beliefs, attitudes, knowledge, skills and behaviour after a biopsychosocially orientated university course? J Eval Clin Pract. 2009. Aug;15(4):724–732. [DOI] [PubMed] [Google Scholar]
- [24].Pransky G, Borkan JM, Young AE, et al. Are we making progress?: the tenth international forum for primary care research on low back pain. Spine [Internet]. 2011;36(19). Available from https://journals.lww.com/spinejournal/Fulltext/2011/09010/Are_We_Making_Progress___The_Tenth_International.14.aspx [DOI] [PubMed] [Google Scholar]
- [25].Chauhan BF, Jeyaraman M, Mann AS, et al. Behavior change interventions and policies influencing primary healthcare professionals’ practice—an overview of reviews. Implement Sci. 2017. Dec;12(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Cook DA, Levinson AJ, Garside S, et al. Instructional design variations in internet-based learning for health professions education: a systematic review and meta-analysis. Acad Med J Assoc Am Med Coll United States. 2010. May;85(5):909–922. PMID: 20520049 [DOI] [PubMed] [Google Scholar]
- [27].Means B, Toyama Y, Murphy R, et al. Evaluation of evidence-based practices in online learning : a meta-analysis and review of online learning studies. Washington, D.C.: US Dep Educ Off Plan Eval Policy Dev; 2010. [Google Scholar]
- [28].Rees C, Sheard C, McPherson A. Medical students’ views and experiences of methods of teaching and learning communication skills. Patient Educ Couns. 2004. Jul;54(1):119–121. [DOI] [PubMed] [Google Scholar]
- [29].Bosse HM, Schultz JH, Nickel M, et al. The effect of using standardized patients or peer role play on ratings of undergraduate communication training: a randomized controlled trial. Patient Educ Couns. 2012;87(3):300–306. [DOI] [PubMed] [Google Scholar]
- [30].Douma KFL, Aalfs CM, Dekker E, et al. An E-Learning module to improve nongenetic health professionals’ assessment of colorectal cancer genetic risk: feasibility study. JMIR Med Educ. 2017. Dec 18;3(2):e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Christe G, Nzamba J, Desarzens L, et al. Physiotherapists’ attitudes and beliefs about low back pain influence their clinical decisions and advice. Musculoskelet Sci Pract. 2021Jun;53:102382. [DOI] [PubMed] [Google Scholar]
- [32].Cook DA, Levinson AJ, Garside S, et al. Internet-based learning in the health professions. Am Med Assoc. 2008;300(10):1181–1196. [DOI] [PubMed] [Google Scholar]
- [33].Lukaschek K, Schneider N, Schelle M, et al. Applicability of motivational interviewing for chronic disease management in primary care following a web-based E-learning course: cross-sectional study. J Med Internet Res. 2019;21(4). DOI: 10.2196/12540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Beijer LJ, Rietveld TCM, Hoskam V, et al. Evaluating the feasibility and the potential efficacy of e-learning-based speech therapy (EST) as a web application for speech training in dysarthric patients with Parkinson’s disease: a case study. Telemed E-Health. 2010;16(6):732–738. [DOI] [PubMed] [Google Scholar]
- [35].Franchi C, Mari D, Tettamanti M, et al. E-learning to improve the drug prescribing in the hospitalized elderly patients: the ELICADHE feasibility pilot study. Aging Clin Exp Res. 2013;26(4):435–443. [DOI] [PubMed] [Google Scholar]
- [36].Richmond H, Hall AM, Hansen Z, et al. Using mixed methods evaluation to assess the feasibility of online clinical training in evidence based interventions: a case study of cognitive behavioural treatment for low back pain. BMC Med Educ. 2016;16(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Fontaine G, Cossette S, Heppell S, et al. Evaluation of a web-based e-learning platform for brief motivational interviewing by nurses in cardiovascular care: a pilot study. J Med Internet Res. 2016;18(8):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Lukaschek K, Schneider N, Schelle M, et al. Applicability of motivational interviewing for chronic disease management in primary care following a web-based E-learning course: cross-sectional study. J Med Internet Res. 2019. DOI: 10.2196/12540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Weiner DK, Morone NE, Spallek H, et al. E-learning module on chronic low back pain in older adults: evidence of effect on medical student objective structured clinical examination performance. J Am Geriatr Soc. 2014;62(6):1161–1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Sinclair P, Kable A, Levett-Jones T. The effectiveness of internet-based e-learning on clinician behavior and patient outcomes: a systematic review protocol. JBI Database Syst Rev Implement Rep. 2015;13(1):52–64. PMID: 26447007 DOI: 10.11124/jbisrir-2015-1919. [DOI] [PubMed] [Google Scholar]
- [41].Almeida M, Saragiotto B, Richards B, et al. Primary care management of non-specific low back pain: key messages from recent clinical guidelines. Med J Aust. 2018;208(6):272–275. PMID: 29614943 DOI: 10.5694/mja17.01152. [DOI] [PubMed] [Google Scholar]
- [42].NICE . Low back pain and sciatica in over 16s : assessment and management(London: National Institute for Health and Care Excellence (UK)). 2019. NICE guideline [NG59]. [PubMed] [Google Scholar]
- [43].Darlow B, Dean S, Perry M, et al. Easy to Harm, hard to heal: patient views about the back. Spine (Phila Pa 1976). 2015. Jun;40(11):842–850. DOI: 10.1097/BRS.0000000000000901. [DOI] [PubMed] [Google Scholar]
- [44].Deyo RA, Mirza SK, Turner JA, et al. Overtreating chronic back pain: time to back off? J Am Board Fam Med. 2009;22(1):62–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356–2367. [DOI] [PubMed] [Google Scholar]
- [46].Suri P, Delaney K, Rundell SD, et al. Predictive validity of the start back tool for risk of persistent disabling back pain in a U.S. primary care setting. Arch Phys Med Rehabil. 2018. Aug;99(8):1533–1539.e2. DOI: 10.1016/j.apmr.2018.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Hill JC, Dunn KM, Lewis M, et al. A primary care back pain screening tool: identifying patient subgroups for initial treatment. Arthritis Rheum. 2008. May 15;59(5):632–641. DOI: 10.1002/art.23563. [DOI] [PubMed] [Google Scholar]
- [48].Clayton J. The validation of the online learning environment survey. ASCILITE 2007 - Australas Soc Comput Learn Tert Educ. 2007;159–167. [Google Scholar]
- [49].Hurley DA, Keogh A, Ardle DM, et al. Evaluation of an e-learning training program to support implementation of a group-based, theory-driven, self-management intervention for osteoarthritis and low-back pain: pre-post study. J Med Internet Res. 2019;21(3):e11123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Kobewka D, Backman C, Hendry P, et al. The feasibility of e-learning as a quality improvement tool. J Eval Clin Pract. 2014;20(5):606–610. [DOI] [PubMed] [Google Scholar]
- [51].Leong S, Mc Laughlin P, O’Connor OJ, et al. An assessment of the feasibility and effectiveness of an E-learning module in delivering a curriculum in radiation protection to undergraduate medical students. J Am Coll Radiol. 2012;9(3):203–209. [DOI] [PubMed] [Google Scholar]
- [52].Trinidad S, and Pearson J. Implementing and evaluating e-learning environments. Beyond the comfort zone: Proceedings of the 21st ASCILITE Conference 5-8 Dec 2004;(2002. R. Atkinson, C. McBeath, D. Jonas-Dwyer & R. Phillips):895–903 http://www.ascilite.org.au/conferences/perth04/procs/trinidad.htm. [Google Scholar]
- [53].Wilroy JD, Ginis KAM, Rimmer JH, et al. E-learning program for increasing physical activity associated behaviors among people with spinal cord injury: usability study. J Med Internet Res. 2019;21(8). DOI: 10.2196/14788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Yu S, Chen IJ, Yang KF, et al. A feasibility study on the adoption of e-learning for public health nurse continuing education in Taiwan. Nurse Educ Today. 2007;27(7):755–761. [DOI] [PubMed] [Google Scholar]
- [55].Demoulin C, Halleux V, Darlow B, et al. Traduction en français du « back pain attitudes questionnaire » et étude de ses qualités métrologiques. Kinésithérapie Rev Elsevier Masson SAS. 2017;17(184):22–23. [Google Scholar]
- [56].Darlow B, Perry M, Mathieson F, et al. The development and exploratory analysis of the back pain attitudes questionnaire (Back-PAQ). BMJ Open. 2014;4(5):e005251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol [Internet]. 2013. cited 2021 Aug 27;4. DOI: 10.3389/fpsyg.2013.00863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Sawilowsky SS. New Effect Size Rules of Thumb. J Mod Appl Stat Methods. 2009. Nov 1;8(2):597–599. [Google Scholar]
- [59].Young D, Callaghan M, Hunt C, et al. Psychologically informed approaches to chronic low back pain: exploring musculoskeletal physiotherapists’ attitudes and beliefs. Musculoskeletal Care. 2019;17(2):272–276. [DOI] [PubMed] [Google Scholar]
- [60].Chance-Larsen F, Chance-Larsen K, Divanoglou A, et al. The use of an e-learning module on return to work advice for physiotherapists – a prospective cohort study. Physiother Theory Pract. 2018;1–9. DOI: 10.1080/09593985.2018.1485193. [DOI] [PubMed] [Google Scholar]
- [61].Buchbinder R, Jolley D, Wyatt M. Population based intervention to change back pain beliefs and disability: three part evaluation. Br Med J. 2001;322(7301):1516–1520. PMID: 11420272 DOI: 10.1136/bmj.322.7301.1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Buchbinder R, Jolley D. Population based intervention to change back pain beliefs: three year follow up population survey. BMJ. 2004. Feb 7;328(7435):321. DOI: 10.1136/bmj.328.7435.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Slater H, Briggs AM, Smith AJ, et al. Implementing evidence-informed policy into practice for health care professionals managing people with low back pain in Australian rural settings: a preliminary prospective single-cohort study. Pain Med. 2014. Oct;15(10):1657–1668. [DOI] [PubMed] [Google Scholar]
- [64].Domenech J, Sánchez-Zuriaga D, Segura-Ortí E, et al. Impact of biomedical and biopsychosocial training sessions on the attitudes, beliefs, and recommendations of health care providers about low back pain: a randomised clinical trial. Pain Int Assoc Study Pain. 2011;152(11):2557–2563. [DOI] [PubMed] [Google Scholar]
- [65].Nijs J, Roussel N, Paul van Wilgen C, et al. Thinking beyond muscles and joints: therapists’ and patients’ attitudes and beliefs regarding chronic musculoskeletal pain are key to applying effective treatment. Man Ther Elsevier Ltd. 2013;18(2):96–102. Doi: 10.1016/j.math.2012.11.001. [DOI] [PubMed] [Google Scholar]
- [66].Vaona A, Banzi R, Kwag KH, et al. E-learning for health professionals. Cochrane effective practice and organisation of care group, editor. Cochrane Database Syst Rev [Internet]. 2018. Jan 22. cited 2020 Apr 2 DOI: 10.1002/14651858.CD011736.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Festinger L. A Theory of cognitive dissonance (Printed in the United States of America: Row, Peterson and Company, 1957 Reissued by Stanford University Press in 1962; ). 1957. [Google Scholar]
- [68].Nickerson RS. Confirmation bias: a ubiquitous phenomenon in many guises. Rev Gen Psychol. 1998. Jun;2(2):175–220. [Google Scholar]
- [69].Buchbinder R, Underwood M, Hartvigsen J, et al. the lancet series call to action to reduce low value care for low back pain: an update. Pain. 2020. Sep;161(Supplement1):S57–S64. [DOI] [PMC free article] [PubMed] [Google Scholar]


