Abstract
Background and Objectives
To review treatments for reducing the risk of recurrent stroke or death in patients with symptomatic intracranial atherosclerotic arterial stenosis (sICAS).
Methods
The development of this practice advisory followed the process outlined in the American Academy of Neurology Clinical Practice Guideline Process Manual, 2011 Edition, as amended. The systematic review included studies through November 2020. Recommendations were based on evidence, related evidence, principles of care, and inferences.
Major Recommendations
Clinicians should recommend aspirin 325 mg/d for long-term prevention of stroke and death and should recommend adding clopidogrel 75 mg/d to aspirin for up to 90 days to further reduce stroke risk in patients with severe (70%–99%) sICAS who have low risk of hemorrhagic transformation. Clinicians should recommend high-intensity statin therapy to achieve a goal low-density lipoprotein cholesterol level <70 mg/dL, a long-term blood pressure target of <140/90 mm Hg, at least moderate physical activity, and treatment of other modifiable vascular risk factors for patients with sICAS. Clinicians should not recommend percutaneous transluminal angioplasty and stenting for stroke prevention in patients with moderate (50%–69%) sICAS or as the initial treatment for stroke prevention in patients with severe sICAS. Clinicians should not routinely recommend angioplasty alone or indirect bypass for stroke prevention in patients with sICAS outside clinical trials. Clinicians should not recommend direct bypass for stroke prevention in patients with sICAS. Clinicians should counsel patients about the risks of percutaneous transluminal angioplasty and stenting and alternative treatments if one of these procedures is being contemplated.
Symptomatic intracranial atherosclerotic arterial stenosis (sICAS) is one of the most common causes of stroke worldwide and is associated with a high risk of recurrent stroke.1-4 The global burden of stroke associated with sICAS is expected to rise as the population ages and as Asian, Black, and Hispanic populations, which have a higher prevalence of sICAS, increase, as major contributors to global population growth.5
Over the past 2 decades, evidence has accumulated informing the treatment of sICAS, with 2 general approaches emerging: (1) aggressive medical management (AMM) with dual antiplatelet therapy (DAPT) plus intensive control of vascular risk factors and (2) medical therapy plus endovascular procedures. Given the high risk of recurrent stroke reported in many studies,6,7 clinical trials also focused on identifying and quantifying modifiable and nonmodifiable risk factors that may place patients at a particularly high risk of recurrent stroke. Knowledge of predictors of recurrent stroke is crucial for risk stratification, effect modification, and identifying therapeutic targets in future clinical trials.
This practice advisory seeks to answer the following clinical questions:
-
For patients with a history of sICAS, which medical therapies, as compared with no therapy or an alternative therapy, reduce the risk of recurrent stroke/death or increase the risk of major hemorrhage (therapeutic scheme)?
Anticoagulation vs antiplatelet therapy
Specific antiplatelet therapy regimens vs alternative regimens
Antihypertensive agents or blood pressure (BP) control targets
Statin therapy or lipid targets
Ischemic preconditioning
For patients with a history of sICAS, do endovascular or extracranial to intracranial (EC/IC) bypass procedures, as compared with no procedure, reduce the risk of recurrent stroke or death (therapeutic scheme)?
-
For patients with a history of sICAS, what modifiable and nonmodifiable risk factors predict an increased risk of recurrent stroke or death (prognostic scheme)?
Degree of stenosis
Length of stenosis
Tandem lesions
Vascular bed
Degree of collateral circulation
Demographics including sex, race, and ethnicity of patient
Medical comorbidities
Time from index event
Physical activity level
Lack of use of aggressive medical therapy
This article is a summary of the key findings of the practice advisory. The complete practice advisory, including evidence tables, is available at aan.com/Guidelines/home/GuidelineDetail/1067.
Description of the Analytic Process
This practice advisory follows the 2011 edition of the American Academy of Neurology's (AAN) guideline development process manual.8 In September 2014, a multidisciplinary panel was recruited to develop the protocol for this practice advisory. The authors include content experts (T.N.T., L.B.G., M.I.C., A.C., A.J.F., J.G.L., M.J.S., A.B.S., L.R.W., O.O.Z., R.S.S., N.R.G, T.N.N., A.A.R.), a methodology expert (G.S.G.), and Guidelines Subcommittee members (J.J.F., S.R.M.). All authors were required to submit the AAN's relationship disclosure forms and copies of their curriculum vitae, which were reviewed by panel leadership. The full author panel was solely responsible for final decisions about the design, analysis, and reporting of this practice advisory, which was submitted for approval to the Guidelines Subcommittee.
Inclusion and exclusion criteria for article selection were chosen to be rated for risk of bias on the basis of a priori criteria. Consistent with prior AAN stroke-related guidelines, the primary outcome of interest was recurrent stroke or recurrent stroke and death. sICAS is defined as TIA or ischemic stroke attributed to 50%–99% atherosclerotic stenosis of a major intracranial artery. Therapeutic clinical trials of sICAS were primarily limited to stenosis of the middle cerebral, intracranial carotid, basilar, and vertebral arteries.
For therapeutic questions, only studies that randomly allocated patients with sICAS to different treatment groups and followed patients to compare their subsequent risks of recurrent stroke or death were included in the systematic review and intention-to-treat analyses were used to inform conclusions. The author panel determined a priori that the effect measure used would be risk differences (RDs), with a change of 5% considered clinically meaningful. Generic inverse variance random effects meta-analytic models were used to pool effect sizes as we expected substantive heterogeneity based on patient selection, time from qualifying event, medical management, duration of follow-up, or inclusion and exclusion criteria. For the primary analysis, we utilized studies with the lowest risk of bias and greatest generalizability to inform conclusions.
For the prognostic question, only cohort studies or case-control studies that compared recurrent stroke risk in patients with sICAS with and without a putative risk factor were included in the systematic review. The author panel determined a priori that the primary effect measure used would be the odds ratio (OR), and if no OR was reported or calculable, the hazard ratio would be considered equivalent to the risk ratio and would be used to estimate the OR.9-11 An increased risk ratio of 0.5 (i.e., OR >1.5) was considered clinically meaningful. When determining risk of bias in prognostic studies, we did not downgrade a study's contribution if baseline risk factors were ascertained prior to the determination of the outcome.
Confidence in the evidence was anchored by the number and class of studies included in the synthesis. Generalizability and study precision were also considered, but studies were not downgraded for generalizability based on race or ethnicity. Evidence was downgraded when the CI for a statistically insignificant effect measure included a clinically meaningful effect (e.g., an OR >1.5) indicating poor precision. Evidence was not downgraded for imprecision when CIs around effect measures were consistent with statistical significance but contained values of uncertain clinical importance (e.g., an OR of 1.05); however, the evidence could not be upgraded. All CIs were presented transparently for individual interpretation and use in the modified Delphi process. Confidence in the evidence was downgraded by 2 levels for imprecision. Confidence in the evidence was only downgraded by 1 level in indirect studies with good precision. The magnitude of effect was considered when upgrading the confidence in evidence supported by studies with direct evidence and low risk of bias (Class I evidence).
The overall confidence in the evidence was determined using a modified Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach.8,12,13 Recommendations were derived by the author panel utilizing an iterative modified Delphi process after considering the evidence strength, risks and benefits, cost, availability, and patient preference variations.
Analysis of Evidence
The panel searched the MEDLINE, Cochrane, and Science Citation Index databases from database inception to February 2016 for relevant peer-reviewed articles that met inclusion criteria. The panelists reviewed the titles and abstracts of 2,325 articles for relevance, which resulted in 505 obtained for full-text review. Independent review of the 505 articles by 2 panel members resulted in 45 articles for inclusion in the analysis and evidence rating. An updated literature search following the same process was conducted in November 2020, yielding 1,233 articles. Of the reviewed abstracts, 54 were identified for full-text review and 11 new articles were ultimately selected to inform conclusions.
1a. For patients with a history of sICAS, does anticoagulation, as compared with antiplatelet therapy, reduce the risk of recurrent stroke or death?
For patients with sICAS, there is insufficient evidence to support or refute the effectiveness of warfarin, as compared with aspirin, in reducing the recurrent risk of stroke or death (RD –0.3%, 95% CI –7.2% to 6.5%; very low confidence in the evidence, 1 Class I trial,7 confidence downgraded due to imprecision).
For patients with sICAS, it is likely that warfarin, as compared with aspirin, increases the risk of major hemorrhage (RD 5.1%, 95% CI 1.2%–9.1%) and death (RD 5.4%, 95% CI 1.2%–9.8%). This conclusion is based on 1 Class I trial7 and confidence in the evidence is moderate.
For patients with sICAS, there is insufficient evidence to support or refute the effectiveness of short-term nadroparin calcium (low molecular weight heparin [LMWH]), as compared with aspirin, for reducing the composite of early neurologic decline and recurrent stroke (RD 0.2%, 95% CI –6.3% to 6.5%) or death (RD 0.4%, 95% CI –4.5% to 5.2%; very low confidence in the evidence, 1 Class I study,14 confidence downgraded due to imprecision and indirectness).
For patients with sICAS, there is insufficient evidence to support or refute the effect of short-term nadroparin calcium (LMWH), as compared with aspirin, on hemorrhagic adverse events (RD 4.7%, 95% CI –3.3% to 10.3%; very low confidence in the evidence, 1 Class I study,14 confidence downgraded due to imprecision and indirectness).
1b. For patients with a history of sICAS, do specific antiplatelet therapy regimens, as compared with alternative antithrombotic regimens, reduce the risk of recurrent stroke or death?
Cilostazol Regimens
For patients with sICAS, there is insufficient evidence to support or refute the effectiveness of cilostazol plus aspirin or clopidogrel (DAPT), as compared with monotherapy (aspirin or clopidogrel), for reducing the risk of recurrent stroke or death (RD –3%, 95% CI –8% to 3%; I2 = 57%; very low confidence in the evidence, 1 Class I study15 and 1 Class II study,16 confidence downgraded for insufficient precision). The risk of serious hemorrhagic complications is likely not different between DAPT with cilostazol compared with monotherapy (RD 0%, 95% CI –1% to 0%; I2 = 0%; moderate confidence in the evidence, 1 Class I study15 and 1 Class II study16).
For patients with sICAS, there is insufficient evidence to support or refute the effectiveness of DAPT with cilostazol plus aspirin, as compared with clopidogrel plus aspirin, in reducing recurrent stroke or death (RD 1.7%, 95% CI –2.4% to 5.7%; very low confidence in the evidence, 1 Class 1 study,17 confidence downgraded due to imprecision). DAPT with cilostazol plus aspirin is likely not associated with any difference in hemorrhagic complications compared with clopidogrel plus aspirin (RD –1.8%, 95% CI –4.9% to 0.8%; moderate confidence in the evidence, 1 Class I study17).
DAPT With Aspirin and Clopidogrel Regimens
For patients with sICAS, there is insufficient evidence to support or refute the effectiveness of DAPT with clopidogrel plus aspirin, compared with aspirin monotherapy, initiated soon after high-risk TIA or stroke in reducing the risk of recurrent stroke or death (RD –3%, 95% CI –7% to 1%; I2 = 0%; very low confidence in the evidence, 1 Class I study18 and 1 Class II study,19 confidence downgraded due to imprecision and indirectness).
For patients with sICAS, it is possible that short-term DAPT with clopidogrel plus aspirin does not increase the risk of hemorrhagic complications compared with aspirin monotherapy in patients with TIA or minor stroke (RD –1%, 95% CI –2% to 1%; I2 = 7%; low confidence in the evidence, 1 Class I study20 and 1 Class II study,19 confidence downgraded due to indirectness).
1c. For patients with a history of sICAS, which antihypertensive agents or BP control targets, as compared with alternative agents or targets, reduce the risk of recurrent stroke or death?
For patients with sICAS, there is insufficient evidence to support or refute the effectiveness of intensive vs modest BP control in reducing the risk of recurrent stroke or death (RD 0%, 95% CI –8.5% to 7.2%; very low confidence in the evidence, 1 Class IV study21 with insufficient precision).
1d. For patients with a history of sICAS, do statin therapy or lipid targets, as compared with alternative management, reduce the risk of recurrent stroke or death?
For patients with sICAS, there is insufficient evidence to support or refute the effectiveness of any statin therapy or other lipid-lowering regimens in reducing the recurrent risk of stroke or death (very low confidence in the evidence, 2 Class IV studies22,23).
1e. For patients with a history of sICAS, does ischemic preconditioning, as compared with sham therapy, reduce the risk of recurrent stroke or death?
In patients with sICAS, bilateral arm ischemic preconditioning (BAIPC) is likely effective in reducing the risk of recurrent stroke (RD –15%, 95% CI –27% to −2%; I2 = 0%; moderate confidence in the evidence, 2 Class II studies24,25).
2a. For patients with a history of sICAS, do EC/IC bypass procedures, as compared with no procedure, reduce the risk of recurrent stroke or death?
For patients with symptomatic severe middle cerebral artery (MCA) stenosis, EC/IC direct bypass, as compared with medical therapy alone, is highly likely to increase the risk of recurrent stroke or death (RD 20.3%, 95% CI 2.5%–36.7%; high confidence in the evidence, 1 Class I study,26 confidence upgraded due to magnitude of effect).
2b. For patients with a history of sICAS, do endovascular procedures, as compared with no procedure, reduce the risk of recurrent stroke or death?
For patients with recent TIA or nondisabling stroke attributed to sICAS, it is highly likely that percutaneous transluminal angioplasty and stenting (PTAS) plus AMM, compared with AMM alone, increases the early risk of recurrent stroke and death (RD 13%, 95% CI 3%–24%; I2 = 59%; high confidence in the evidence, 2 Class I studies27-29 with large magnitude of effect).
For patients with recent TIA or nondisabling stroke attributed to sICAS, it is possible that PTAS plus AMM, compared with AMM alone, does not reduce the long-term risk of recurrent stroke or death (RD 3%, 95% CI –3% to 8%; I2 = 86%; low confidence in the evidence, 2 Class I studies,27-29 confidence downgraded due to imprecision).
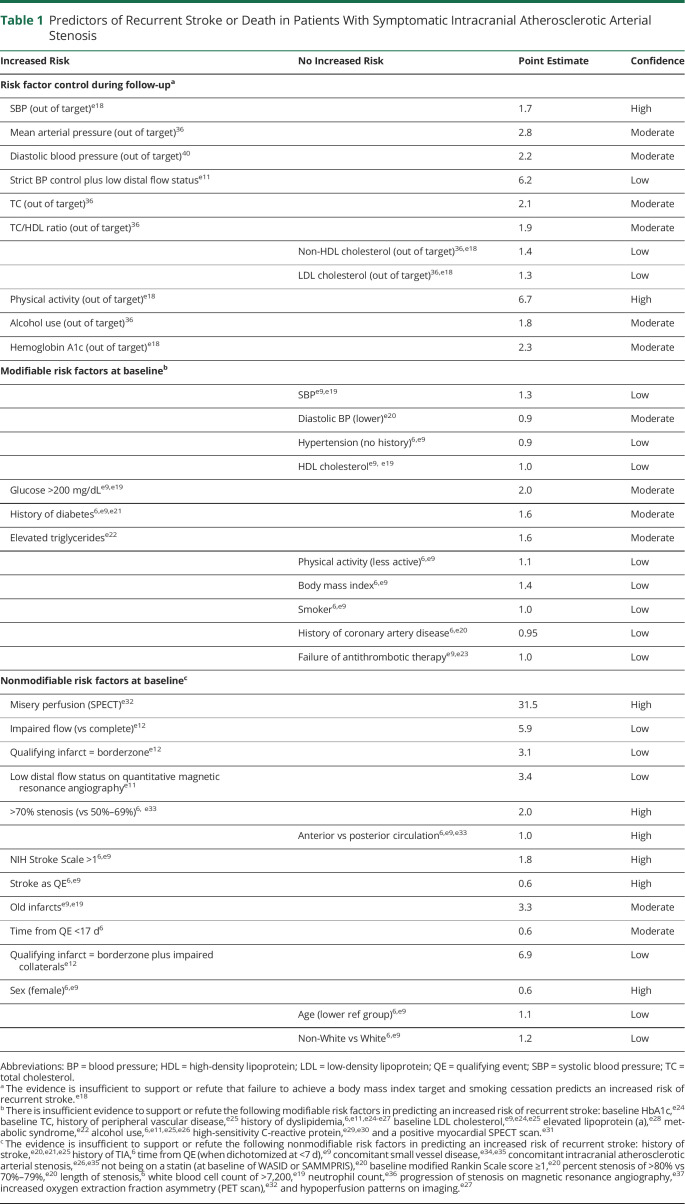
3. For patients with a history of sICAS, what modifiable and nonmodifiable risk factors predict an increased risk of recurrent stroke or death?
Evidence supporting factors that did or did not predict an increased risk of recurrent stroke or death is summarized in Table 1.
Table 1.
Predictors of Recurrent Stroke or Death in Patients With Symptomatic Intracranial Atherosclerotic Arterial Stenosis
Practice Recommendations
Diagnosis
Rationale for Recommendation 1
sICAS is one of the most common causes of stroke worldwide, responsible for 10%–50% of strokes depending on racial and ethnic factors,2,4,30 and can coexist with other stroke etiologies such as extracranial atherosclerosis or atrial fibrillation.31,32 There is no diagnostic gold standard for diagnosing sICAS and various noninvasive and invasive techniques (e.g., magnetic resonance angiography, CT angiography, transcranial Doppler, and catheter cerebral angiography) are used with varying sensitivity and specificity.33,34 Intracranial artery luminal stenosis may be due to a variety of vasculopathies and atherosclerosis may be differentiated clinically in most cases.5 It is important to identify sICAS as the etiology of stroke to optimize secondary prevention strategies. Expeditious evaluation is reasonable as the highest risk of recurrent stroke is soon after the incident event.
Recommendation 1 Statement
Clinicians should utilize diagnostic modalities to diagnose sICAS and distinguish it from other intracranial vasculopathies if the results would be expected to change management or provide important prognostic information (Level B).
Antithrombotic Medication Therapy
Rationale for Recommendations 2, 3, and 4
The WASID trial (Warfarin–Aspirin Symptomatic Intracranial Disease) showed that in patients with sICAS, aspirin 650 mg twice daily was safer and as effective as warfarin for preventing the combined endpoint of stroke, intracerebral hemorrhage, and vascular death. Whereas the optimal aspirin dose for sICAS has not been determined, patients in the medical arm of the SAMMPRIS trial (Stenting and Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis) were treated with aspirin alone 325 mg/d after the first 90 days. Other antiplatelet agents used for stroke prevention (e.g., ticagrelor or combination dipyridamole and aspirin) and other doses of aspirin have not been specifically studied in sICAS. The safety and efficacy of novel oral anticoagulants for prevention of stroke in sICAS are not established. Similarly, the safety and efficacy of adding aspirin to anticoagulation in patients with sICAS who require anticoagulation for another condition (e.g., atrial fibrillation) have not been established. However, given that warfarin was equally effective as aspirin for stroke prevention in WASID, the utility of adding aspirin to warfarin does not seem warranted in light of bleeding concerns.
Combination short-term clopidogrel and aspirin use in sICAS was not directly supported by this systematic review but is supported by related evidence.19,35 The CLAIR study (Clopidogrel Plus Aspirin Versus Aspirin Alone for Reducing Embolisation in Patients With Acute Symptomatic Cerebral or Carotid Artery Stenosis) showed that patients randomized to clopidogrel plus aspirin had significantly decreased microemboli in the territory of the stenotic artery when compared with aspirin alone.19 When combined with the CARESS trial (Clopidogrel and Aspirin for Reduction of Emboli in Symptomatic Carotid Stenosis), a similar study of patients with carotid atherosclerosis, patients treated with clopidogrel and aspirin had a significant reduction in recurrent stroke compared with patients treated with aspirin monotherapy.35 In addition, patients with sICAS in the CHANCE trial (Clopidogrel in High-Risk Patients With Acute Nondisabling Cerebrovascular Events) who were randomized to clopidogrel and aspirin had a numerically lower rate of stroke at 90 days compared with those on aspirin alone, albeit not statistically significant. Additional support for combined short-term clopidogrel and aspirin comes from analyses comparing patients in the medical arm of SAMMPRIS treated with 90 days of clopidogrel plus aspirin, who had a lower primary endpoint rate, with similar patients from WASID treated with aspirin alone at 1 month (5.8% vs 10.5%) and 6 months (8.9% vs 17.9%).27,36 This analysis of WASID patients who met SAMMPRIS entry criteria was adjusted for confounding factors and still showed almost double the risk of stroke in the WASID patients, despite the higher burden of poor prognostic features in the SAMMPRIS patients. The optimal duration of combined clopidogrel and aspirin in sICAS has not been tested in randomized controlled trials (RCTs) and remains unknown, but the high rate of stroke beyond the first few months on aspirin alone in the medical arm of the SAMMPRIS trial suggests further study is needed to determine whether extending clopidogrel use beyond 3 months is warranted.
Trials of cilostazol combined with other antiplatelet agents for stroke prevention in sICAS have had mixed results. TOSS (Trial of Cilostazol in Symptomatic Intracranial Arterial Stenosis) and TOSS-2 found cilostazol plus aspirin was not better for stroke prevention than aspirin alone or clopidogrel plus aspirin. However, the CATHARSIS study (Cilostazol-Aspirin Therapy Against Recurrent Stroke with Intracranial Artery Stenosis) demonstrated that cilostazol plus aspirin prevented the combined secondary endpoint of all vascular events and new silent brain infarcts when compared with aspirin alone. A subgroup analysis of patients with sICAS in CSPS (Cilostazol Stroke Prevention Study for Antiplatelet Combination), which included heterogeneous causes of stroke, showed a lower rate of stroke when randomized to cilostazol plus either aspirin or clopidogrel compared with those on aspirin or clopidogrel alone. Generalizability of these cilostazol studies is limited in that they were conducted in a primarily Asian population and low-dose aspirin (≤150 mg/d) was used.
Recommendation 2 Statement
Clinicians should recommend aspirin 325 mg/d over warfarin for long-term prevention of stroke and death in patients with sICAS (Level B).
Recommendation 3 Statement
Clinicians should recommend adding clopidogrel 75 mg/d to aspirin for up to 90 days to further reduce stroke risk in patients with severe (70%–99%) sICAS who have low risk of hemorrhagic transformation of ischemic stroke (Level B).
Recommendation 4 Statement
Clinicians may recommend adding cilostazol 200 mg/d to aspirin for up to 90 days to further reduce stroke risk in patients with sICAS and low risk of hemorrhagic complications as an alternative to clopidogrel or in Asian patients (Level C).
Lipid and Hypertension Vascular Risk Factor Modification
Rationale for Recommendations 5 and 6
Support for the management of vascular risk factors in patients with sICAS comes from prespecified, post hoc analyses of sICAS clinical trials and other clinical practice guidelines for patients with stroke and vascular disease. Evidence for the use of high-intensity statins in patients with symptomatic atherosclerotic disease is well established and is applicable to patients with sICAS.37 In addition, a lower rate of cerebrovascular events was seen in patients with sICAS randomized to high-intensity statin therapy compared with other dosages. A target low-density lipoprotein (LDL) level <70 mg/dL among patients with stroke and atherosclerotic disease was found to reduce major cardiovascular events compared with patients with a target LDL <100 mg/dL.38 Post hoc analyses from WASID and SAMMPRIS also show lower rates of vascular events with lower LDLs in sICAS. The use of other lipid-lowering agents (e.g., PCSK9 inhibitors or omega-3) has not been specifically studied in sICAS but may be supported by studies of symptomatic atherosclerotic disease.37
Historically, there was concern for targeting normal BP in the setting of an intracranial stenosis resulting in hypoperfusion and contrasting concern for worsening atherosclerosis due to uncontrolled hypertension.39 Analyses from WASID, SAMMPRIS, and the CICAS registry (Chinese Intracranial Atherosclerosis) have demonstrated that among clinically stable patients with sICAS, a mean systolic BP (SBP) <140 mm Hg during follow-up was associated with a lower risk of stroke and vascular events, even in patients with posterior circulation or severe stenosis.e18,40,41 Although the current American Heart Association guideline–recommended target of SBP <130 mm Hg has not been studied in patients with sICAS, an RCT of patients with sICAS comparing SBPs <120 mm Hg vs <140 mm Hg found that the more intensive group (which had a mean SBP of 124.6 mm Hg) had a higher rate of new ischemic lesions on imaging and larger stroke volume than the standard group.21,42 Some subgroups of patients with sICAS may be at higher risk of stroke with lower BPs, including those with hemodynamic impairment43,44 or those with a large reduction in BP from baseline.
Recommendation 5 Statement
Clinicians should recommend high-intensity statin therapy to achieve a goal LDL <70 mg/dL in patients with sICAS to reduce the risk of recurrent stroke and vascular events (Level B).
Recommendation 6 Statement
Clinicians should recommend a long-term BP target of <140/90 mm Hg in clinically stable patients with sICAS to reduce the risk of recurrent stroke and vascular events (Level B).
Physical Activity
Rationale for Recommendation 7
In the general population, moderate physical activity reduces incidence of stroke.45 Among patients with sICAS, a post hoc analysis of SAMMPRIS showed that not performing moderate physical activity at least 3–5 times per week was associated with a higher risk of recurrent stroke and vascular events (OR 6.7, 95% CI 2.5–18.1).e18
Recommendation 7 Statement
Clinicians should recommend at least moderate physical activity in patients with sICAS who are safely capable of exercise to reduce the risk of recurrent stroke and vascular events (Level B).
Other Modifiable Vascular Risk Factors
Rationale for Recommendation 8
Benefits on morbidity and mortality from maintaining a healthy lifestyle and management of other vascular risk factors are well established for patients with atherosclerotic disease and are applicable to patients with sICAS.46
Recommendation 8 Statement
Clinicians must recommend treatment of other modifiable vascular risk factors in patients with sICAS to reduce the risk of recurrent stroke and vascular events (Level A).
Bilateral Arm Ischemic Preconditioning
Rationale for Recommendation 9
Based on 2 RCTs done in patients with sICAS, 5 cycles of BAIPC twice daily appears to reduce the risk of recurrent stroke and death. However, the evidence is derived from only 2 centers in China, the studies had small sample sizes, and the studies were not blinded. These methodologic issues limit conclusions about efficacy in a multiethnic population. Whereas the risk of the procedure appears low, the BAIPC device does not have approval for use in the United States, limiting its application. These methodologic issues limit confidence in conclusions about efficacy and there are no data in a multiethnic population.
Recommendation 9 Statement
The authors could not achieve consensus on a recommendation for BAIPC in patients with sICAS.
Endovascular and Surgical Therapy
Rationale for Recommendations 10–13
Percutaneous Transluminal Angioplasty and Stenting
Recommendations related to PTAS are informed by several randomized trials that showed no benefit of PTAS (with either self-expanding or balloon-mounted stents) over medical therapy. Three RCTs have shown a higher rate of periprocedural cerebrovascular events and death from PTAS and no benefit of stroke prevention during follow-up compared with medical therapy in patients with sICAS.
Single-arm, uncontrolled registries assessing subpopulations of patients with sICAS, including medical failures (i.e., stroke or TIA while on antithrombotic medications) or those with progressive neurologic symptoms, have reported conflicting rates of periprocedural complications.47,48 In a Food and Drug Administration (FDA)–mandated postmarket surveillance study of the Wingspan stent, the stroke or death rate was 23.9% within 72 hours among those who did not meet criteria for FDA-approved use, many of whom had not failed medical therapy or were treated recently after stroke.49,50 In post hoc analyses of RCTs, no studied subgroups have been shown to benefit from PTAS, including those with intracranial vertebral segment location or those taking antithrombotic medications at the time of the initial cerebrovascular event. PTAS has not been systematically compared with medical therapy in patients with moderate (50%–69%) sICAS, but the low risk of stroke in these patients and the high risk of periprocedural complications, which do not depend on severity of stenosis, makes PTAS unwarranted.7,51
Angioplasty Alone
In light of safety issues related to PTAS, balloon angioplasty alone (i.e., without placement of an intracranial stent) has been considered a possible alternative for endovascular therapy.52 However, no RCTs have compared angioplasty alone with medical therapy for stroke prevention in patients with sICAS. A systematic review and meta-analysis of 25 studies of angioplasty alone compared event rates in patients treated with angioplasty to events in the SAMMPRIS medical group and found no benefit of angioplasty due to high periprocedural morbidity and mortality.53 Balloon angioplasty alone may be performed with a submaximal staged approach, which may have a lower rate of morbidity and mortality.54
Optimal stroke prevention for patients with sICAS who have recurrent strokes despite antiplatelet therapy and intensive treatment of risk factors is unknown. However, given the lack of efficacy data, the use of PTAS or angioplasty alone for stroke prevention in any subpopulation of patients with sICAS is investigational.52-54
Recommendation 10 Statement
Clinicians should not recommend PTAS as the initial treatment for stroke prevention in patients with severe (70%–99%) sICAS (Level B) (Figures 1 and 2).
Figure 1. Summary Estimate of the Effects of PTAS + AMM Compared to AMM Alone on 30-Day Risk of Recurrent Stroke or Death.
AMM = aggressive medical management; PTAS = percutaneous transluminal angioplasty and stenting; SAMMPRIS = Stenting and Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis; VISSIT = Vitesse Intracranial Stent Study for Ischemic Therapy
Figure 2. Summary Estimate of the Effects of PTAS + AMM Compared to AMM Alone on Recurrent Stroke or Death Beyond 30 Days.
AMM = aggressive medical management; PTAS = percutaneous transluminal angioplasty and stenting; SAMMPRIS = Stenting and Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis; VISSIT = Vitesse Intracranial Stent Study for Ischemic Therapy
Recommendation 11 Statement
Clinicians should not recommend PTAS for stroke prevention in patients with moderate (50%–69%) sICAS (Level B).
Recommendation 12 Statement
Clinicians should not routinely recommend angioplasty alone for stroke prevention in patients with sICAS outside clinical trials (Level B).
Recommendation 13 Statement
Clinicians should counsel patients about the risks of PTAS and alternative treatments if one of these procedures is being contemplated (Level B).
Surgical Treatment
Rationale for Recommendations 14 and 15
Direct Bypass
Recommendations related to the use of direct surgical bypass for stroke prevention in patients with sICAS are informed by 1 RCT. The EC/IC bypass trial included patients with sICAS and found that bypass was not associated with a decrease in recurrent stroke and death as compared with medical therapy alone. For subgroups with severe MCA stenosis or occlusion, there was an increased risk of recurrent stroke or death with direct bypass. Similar to the EC/IC bypass study, COSS (Carotid Occlusion Surgery Study), which studied patients with symptomatic ICA occlusion, found that direct bypass increases the risk of stroke and death predominantly due to early periprocedural complications.55 For patients with posterior circulation vertebral artery disease, a single-center case series reported that surgical revascularization decreased recurrent stroke and death as compared with medical therapy alone, but no RCTs have been performed to establish efficacy and the procedure is considered investigational.56,57
Indirect Bypass
In patients with anterior circulation sICAS, indirect bypass with encephaloduroarteriosynangiosis (EDAS) is an emerging investigational surgery for stroke prevention.58-60,e1,e2 A small initial study of indirect revascularization without standardized medical management showed a high rate of recurrent stroke in patients with sICAS.59 Four nonrandomized studies, including 2 small case series,58,e1 1 single-center prospective study,e2 and 1 two-center prospective trial with independent outcomes assessment,e3 suggested that there may be benefit of EDAS over medical therapy when applied with standardized medical treatment. Well-designed and well-conducted randomized trials have not been completed.
Recommendation 14 Statement
Clinicians should not recommend direct bypass for stroke prevention in patients with sICAS (Level B).
Recommendation 15 Statement
Clinicians must not routinely recommend indirect surgical revascularization for stroke prevention in patients with sICAS outside clinical trials (Level A).
Suggestions for Future Research
Medical Research
Randomized trials are needed to optimize type and duration of antithrombotic therapy for patients with sICAS. The most promising candidate therapies for future studies are combinations of antithrombotic therapy that have been shown in prior trials to reduce the risk of stroke in patients with (1) large artery cerebrovascular disease (ticagrelor plus aspirin),e4 (2) coronary or peripheral vascular disease (low dose factor Xa inhibitor plus aspirin),e5 and (3) stroke (cilostazol plus aspirin or clopidogrel).15 Novel factor XIa inhibitors alone or in combination with aspirin and clopidogrel are being evaluated in Phase II stroke prevention trials and could also be considered for future trials in patients with sICAS. Because clopidogrel is a prodrug that may be ineffective in patients who carry genetic single-nucleotide loss-of-function (LOF) polymorphisms for the CYP2C19 cytochrome P450 enzyme necessary to metabolize clopidogrel to its active form,e6 trials that include clopidogrel should determine the effect of CYP2C19 LOF allele carrier status on clinical outcomes.
Randomized therapeutic trials of patients with sICAS should incorporate intensive risk factor management in all arms, including the intraoperative and perioperative periods for surgical and endovascular interventions. Consideration should be given to encouraging lifestyle management including exercise, stopping smoking, and weight reduction,e7 the use of a PCKS9 inhibitor in patients with raised LDL despite a maximum tolerated dose of a statin,37 and icosapent ethyl for patients with elevated triglycerides.e8
Endovascular and Surgical Research
Phase I and II trials are needed to develop safe and durable endovascular treatments (e.g., submaximal balloon angioplasty alone52 or new intracranial stents) that could subsequently be compared with AMM in high-risk sICAS. Randomized controlled clinical trials (Phase III) are needed to compare surgical treatments (e.g., EDAS)e1 with AMM in these patients.
Other Areas of Future Research
Adequately powered studies are needed to validate clinical,e9 genetic (e.g., ring finger protein 213 variant),e10 and imaging biomarkerse11-e14 that identify high-risk patients with sICAS for enrollment in future therapeutic trials. Other promising novel therapeutic approaches that should be considered for evaluation are ischemic preconditioning,e15 continuous positive airway pressure in patients with sleep apnea, and anti-inflammatory agents such as colchicine or canakinumab.e16,e17
Disclaimer
Clinical practice guidelines, practice advisories, systematic reviews, and other guidance published by the American Academy of Neurology (AAN) and its affiliates are assessments of current scientific and clinical information provided as an educational service. The information (1) should not be considered inclusive of all proper treatments, methods of care, or as a statement of the standard of care; (2) is not continually updated and may not reflect the most recent evidence (new evidence may emerge between the time information is developed and when it is published or read); (3) addresses only the question(s) specifically identified; (4) does not mandate any particular course of medical care; and (5) is not intended to substitute for the independent professional judgment of the treating provider, as the information does not account for individual variation among patients. In all cases, the selected course of action should be considered by the treating provider in the context of treating the individual patient. Use of the information is voluntary. AAN provides this information on an “as is” basis, and makes no warranty, expressed or implied, regarding the information. AAN specifically disclaims any warranties of merchantability or fitness for a particular use or purpose. AAN assumes no responsibility for any injury or damage to persons or property arising out of or related to any use of this information or for any errors or omissions.
Conflict of Interest
The American Academy of Neurology (AAN) is committed to producing independent, critical, and truthful clinical practice guidelines (CPGs). Significant efforts are made to minimize the potential for conflicts of interest to influence the recommendations of this CPG. To the extent possible, the AAN keeps separate those who have a financial stake in the success or failure of the products appraised in the CPGs and the developers of the guidelines. Conflict of interest forms were obtained from all authors and reviewed by an oversight committee prior to project initiation. AAN limits the participation of authors with substantial conflicts of interest. The AAN forbids commercial participation in, or funding of, guideline projects. Drafts of the guideline have been reviewed by at least 3 AAN committees, a network of neurologists, Neurology peer reviewers, and representatives from related fields. The AAN Guideline Author Conflict of Interest Policy can be viewed at aan.com. For complete information on this process, access the 2011 AAN process manual.8
Acknowledgment
The authors thank former AAN staff members Thomas S.D. Getchius and Shannon A. Merillat, MLIS, for their assistance during the guideline development process.
Glossary
- AAN
American Academy of Neurology
- AMM
aggressive medical management
- BAIPC
bilateral arm ischemic preconditioning
- BP
blood pressure
- DAPT
dual antiplatelet therapy
- EC/IC
extracranial to intracranial
- EDAS
encephaloduroarteriosynangiosis
- FDA
Food and Drug Administration
- LDL
low-density lipoprotein
- LMWH
low molecular weight heparin
- LOF
loss of function
- MCA
middle cerebral artery
- OR
odds ratio
- PTAS
percutaneous transluminal angioplasty and stenting
- RCT
randomized controlled trial
- RD
risk difference
- SAMMPRIS
Stenting and Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis
- SBP
systolic blood pressure
- sICAS
symptomatic intracranial atherosclerotic arterial stenosis
- WASID
Warfarin–Aspirin Symptomatic Intracranial Disease
Appendix. Authors
Study Funding
This practice advisory was developed with financial support from the AAN. Authors who have served as AAN subcommittee members (S.R.M., J.J.F., G.S.G.) or who are or were AAN staff (M.D.O., H.S.) were reimbursed by the AAN for expenses related to travel to subcommittee meetings where drafts of manuscripts were reviewed.
Disclosure
T. Turan has received research support from the NIH for the SAMMPRIS, CREST 2, SE-CoAST StrokeNet RCC, and CHAMPION studies, as well as for serving on the event adjudication committee for the VERiTAS clinical trial; has received personal compensation in the range of $10,000–$49,999 for serving as a blinded clinical events adjudicator for Pfizer and Boehringer Ingelheim; has received personal compensation in the range of $500–$4,999 for serving as a blinded clinical events adjudicator for trials unrelated to intracranial stenosis for W.L. Gore & Associates; and has received publishing royalties from a publication relating to health care. O. Zaidat has received personal compensation for consulting work unrelated to intracranial atherosclerosis and research support from Stryker, Cerenovous, Penumbra, and Medtronic; is the co-chair of the endovascular committee for the NIH StokeNet, the co-editor in chief for the Endovascular and Interventional Neurology section of Frontiers in Neurology, and a past president of the Society of Vascular and Interventional Neurology; and is a founder of Galaxy Therapeutics, Inc. G. Gronseth has received personal compensation in the range of $0–$499 for serving as an editor, associate editor, or editorial advisory board member for Brain & Life and has received personal compensation in the range of $10,000–$49,999 for serving as an associate editor of Neurology®; and has received personal compensation in the range of $0–$499 for serving as an evidence-based medicine consultant for the AAN Guidelines Subcommittee. M. Chimowitz has received product support from Stryker Neurovascular, AstraZeneca, Bayer AG, and Bristol Myers Squibb for the NIH-funded SAMMPRIS and WASID trials; has received personal fees from Gore, Medtronic, Merck & Co., Parexel, and NoNO Inc. for participating as a member of a data and safety monitoring board or stroke adjudicator in clinical trials unrelated to intracranial stenosis; has received funding from the NIH for the SAMMPRIS and WASID trials and the NIH Wingspan registry; has received personal compensation in the range of $500–$4,999 for serving on a scientific advisory or data safety monitoring board for NoNO Inc.; and his institution has received research support from the NIH. A. Culebras has served on UpToDate and MedLink Neurology editorial boards. A. Furlan has nothing to disclose. L. Goldstein has served on scientific advisory boards for Daiichi Sankyo and Merz; has received funding for travel from Pfizer, Daiichi Sankyo, and the National Lipid Association to attend scientific meetings to discuss SPARCL studies; has received publishing royalties from UpToDate, Henry Stewart Publications, and Wiley; has received research support from St. Jude Medical, Inc., for the RESPECT trial, from Nexstim for the NICHE trial, and from the NIH; has received intellectual property interests from a publication relating to health care; and his institution has received research support from the NIH; has received compensation for consulting work from Nestlé, Artemida, Roche, Abbott, and Shire; has received compensation for participating in a data safety monitoring board from Artemida and Roche; and has received an honorarium from the American Heart Association (AHA). N. Gonzalez has received research support from the NIH and the AHA. J. Latorre has nothing to disclose. S. Messé has received funding for travel from the AAN; has received publishing royalties from articles written for UpToDate, including articles about antiplatelets for secondary stroke prevention, carotid disease and surgery, and patent foramen ovale (PFO) and stroke; has received compensation from the Yale Cardiovascular Research Group for serving on clinical event committees for trials of embolic protection during valve replacement and a registry of left atrial appendage occluder placement; has received research support from W.L. Gore & Associates for a PFO closure study and a study of proximal aortic repair, from Novartis for a study of medication to reduce inflammation after intracerebral hemorrhage, from Biogen for a study of a medication to reduce edema from malignant infarction, and from the NIH for a study examining an embolic protection in aortic valve replacement, a cohort study examining renal insufficiency, and a study of sleep apnea treatment after acute stroke; and is a cofounder of and has equity in Neuralert Technologies, a company developing monitors to detect in-hospital stroke. T. Nguyen serves as editor of Frontiers in Neurology; has received compensation as a consultant for Avania; and has received research support from Medtronic and the Society of Vascular and Interventional Neurology. R. Sangha has nothing to disclose. M. Schneck has served on the editorial boards of the Journal of Stroke and Cerebrovascular Disease and Frontiers in Neurology and owns mutual funds that include health retail business stock; has received personal compensation in the range of $500–$4,999 for serving on a scientific advisory or data safety monitoring board for HLT; has received personal compensation in the range of $10,000–$49,999 for serving as an expert witness for miscellaneous legal firms; an immediate family member has received personal compensation for serving as an employee of HistoGeneX; and his institution has received research support from the NIH. A. Singhal has received personal compensation for consulting, serving on a scientific advisory board, speaking, or other activities with Omniox, Deck Therapeutics, Proneurotech, MedLink, and UpToDate; and has served as an expert in legal cases, holds stock and/or stock options in Biogen and Zafgen, and has received research support from the NIH-NINDS for serving as deputy principal investigator (PI) of the New England Regional Coordinating Center for the NIH StrokeNet, site PI of the ARCADIA trial, and data safety monitoring board chair of the FEASt trial. L. Wechsler has served on a SanBio Company Limited scientific advisory board and holds stock in Silk Road Medical and Forest Devices; and his institution has received research support from NINDS. A. Rabinstein has received personal compensation in the range of $5,000–$9,999 for serving on a scientific advisory or data safety monitoring board for Boston Scientific and Boehringer-Ingelheim, has received personal compensation in the range of $0–$499 for serving on a scientific advisory or data safety monitoring board for Minnetronix Medical, has received personal compensation in the range of $500–$4,999 for serving as an editor, associate editor, or editorial advisory board member for Neurocritical Care and UpToDate; has received publishing royalties from a publication relating to health care; and his institution has received research support from Oculogica. M. Dolan O'Brien is an employee of the American Academy of Neurology. H. Silsbee is an employee of the American Academy of Neurology. J. Fletcher has nothing to disclose. Go to Neurology.org/N for full disclosures.
References
- 1.De Silva DA, Woon FP, Lee MP, Chen CP, Chang HM, Wong MC. South Asian patients with ischemic stroke: intracranial large arteries are the predominant site of disease. Stroke. 2007;38:2592-2594. [DOI] [PubMed] [Google Scholar]
- 2.Wong LK. Global burden of intracranial atherosclerosis. Int J Stroke. 2006;1(3):158-159. [DOI] [PubMed] [Google Scholar]
- 3.White H, Boden-Albala B, Wang C, et al. Ischemic stroke subtype incidence among whites, blacks, and Hispanics: the Northern Manhattan Study. Circulation. 2005;111(10):1327-1331. [DOI] [PubMed] [Google Scholar]
- 4.Gorelick PB, Wong KS, Bae HJ, Pandey DK. Large artery intracranial occlusive disease: a large worldwide burden but a relatively neglected frontier. Stroke. 2008;39(8):2396-2399. [DOI] [PubMed] [Google Scholar]
- 5.Banerjee C, Chimowitz MI. Stroke caused by atherosclerosis of the major intracranial arteries. Circ Res. 2017;120(3):502-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kasner SE, Chimowitz MI, Lynn MJ, et al. Predictors of ischemic stroke in the territory of a symptomatic intracranial arterial stenosis. Circulation. 2006;113(4):555-563. [DOI] [PubMed] [Google Scholar]
- 7.Chimowitz MI, Lynn MJ, Howlett-Smith H, et al. Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med. 2005;352(13):1305-1316. [DOI] [PubMed] [Google Scholar]
- 8.American Academy of Neurology. Clinical Practice Guideline Process Manual. American Academy of Neurology; 2011. [Google Scholar]
- 9.Grant RL. Converting an odds ratio to a range of plausible relative risks for better communication of research findings. BMJ. 2014;348:f7450. [DOI] [PubMed] [Google Scholar]
- 10.VanderWeele TJ. Optimal Approximate Conversions of Odds Ratios and Hazard Ratios to Risk Ratios. Biometrics; 2019. [DOI] [PubMed] [Google Scholar]
- 11.Symons MJ, Moore DT. Hazard rate ratio and prospective epidemiological studies. J Clin Epidemiol. 2002;55(9):893-899. [DOI] [PubMed] [Google Scholar]
- 12.Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011;64(4):380-382. [DOI] [PubMed] [Google Scholar]
- 13.Guyatt GH, Oxman AD, Sultan S, et al. GRADE guidelines: 9: rating up the quality of evidence. J Clin Epidemiol. 2011;64(12):1311-1316. [DOI] [PubMed] [Google Scholar]
- 14.Wong KS, Chen C, Ng PW, et al. Low-molecular-weight heparin compared with aspirin for the treatment of acute ischaemic stroke in Asian patients with large artery occlusive disease: a randomised study. Lancet Neurol. 2007;6(5):407-413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Toyoda K, Uchiyama S, Yamaguchi T, et al. Dual antiplatelet therapy using cilostazol for secondary prevention in patients with high-risk ischaemic stroke in Japan: a multicentre, open-label, randomised controlled trial. Lancet Neurol. 2019;18(6):539-548. [DOI] [PubMed] [Google Scholar]
- 16.Kwon SU, Cho YJ, Koo JS, et al. Cilostazol prevents the progression of the symptomatic intracranial arterial stenosis: the multicenter double-blind placebo-controlled trial of cilostazol in symptomatic intracranial arterial stenosis. Stroke. 2005;36(4):782-786. [DOI] [PubMed] [Google Scholar]
- 17.Kwon SU, Hong KS, Kang DW, et al. Efficacy and safety of combination antiplatelet therapies in patients with symptomatic intracranial atherosclerotic stenosis. Stroke. 2011;42(10):2883-2890. [DOI] [PubMed] [Google Scholar]
- 18.Liu L, Wong KS, Leng X, et al. Dual antiplatelet therapy in stroke and ICAS: subgroup analysis of CHANCE. Neurology. 2015;85(13):1154-1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wong KS, Chen C, Fu J, et al. Clopidogrel plus aspirin versus aspirin alone for reducing embolisation in patients with acute symptomatic cerebral or carotid artery stenosis (CLAIR study): a randomised, open-label, blinded-endpoint trial. Lancet Neurol. 2010;9(5):489-497. [DOI] [PubMed] [Google Scholar]
- 20.Wang Y, Wang Y, Zhao X, et al. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. N Engl J Med. 2013;369(1):11-19. [DOI] [PubMed] [Google Scholar]
- 21.Park JM, Kim BJ, Kwon SU, et al. Intensive blood pressure control may not be safe in subacute ischemic stroke by intracranial atherosclerosis: a result of randomized trial. J Hypertens. 2018;36(9):1936-1941. [DOI] [PubMed] [Google Scholar]
- 22.Zhou P, Lu Z, Gao P, et al. Efficacy and safety of intensive statin therapy in Chinese patients with atherosclerotic intracranial arterial stenosis: a single-center, randomized, single-blind, parallel-group study with one-year follow-up. Clin Neurol Neurosurg. 2014;120:6-13. [DOI] [PubMed] [Google Scholar]
- 23.Zhou P, Cao Z, Wang P, et al. The effect of intensive statin therapy on symptomatic intracranial arterial stenosis. Iran J Public Health. 2018;47(2):231-236. [PMC free article] [PubMed] [Google Scholar]
- 24.Meng R, Asmaro K, Meng L, et al. Upper limb ischemic preconditioning prevents recurrent stroke in intracranial arterial stenosis. Neurology. 2012;79(18):1853-1861. [DOI] [PubMed] [Google Scholar]
- 25.Meng R, Ding Y, Asmaro K, et al. Ischemic conditioning is safe and effective for octo- and nonagenarians in stroke prevention and treatment. Neurotherapeutics. 2015;12(3):667-677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.EC/IC Bypass Study Group. Failure of extracranial-intracranial arterial bypass to reduce the risk of ischemic stroke: results of an international randomized trial. N Engl J Med. 1985;313(19):1191-1200. [DOI] [PubMed] [Google Scholar]
- 27.Chimowitz MI, Lynn MJ, Derdeyn CP, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011;365(11):993-1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Derdeyn CP, Chimowitz MI, Lynn MJ, et al. Aggressive medical treatment with or without stenting in high-risk patients with intracranial artery stenosis (SAMMPRIS): the final results of a randomised trial. Lancet. 2014;383(9914):333-341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zaidat OO, Fitzsimmons BF, Woodward BK, et al. Effect of a balloon-expandable intracranial stent vs medical therapy on risk of stroke in patients with symptomatic intracranial stenosis: the VISSIT randomized clinical trial. JAMA. 2015;313:1240-1248. [DOI] [PubMed] [Google Scholar]
- 30.Sacco RL, Kargman DE, Zamanillo MC. Race-ethnic differences in stroke risk factors among hospitalized patients with cerebral infarction: the Northern Manhattan Stroke Study. Neurology. 1995;45(4):659-663. [DOI] [PubMed] [Google Scholar]
- 31.Kim YD, Cha MJ, Kim J, et al. Increases in cerebral atherosclerosis according to CHADS2 scores in patients with stroke with nonvalvular atrial fibrillation. Stroke. 2011;42(4):930-934. [DOI] [PubMed] [Google Scholar]
- 32.Marzewski DJ, Furlan AJ, St Louis P, Little JR, Modic MT, Williams G. Intracranial internal carotid artery stenosis: longterm prognosis. Stroke. 1982;13:821-824. [DOI] [PubMed] [Google Scholar]
- 33.Feldmann E, Wilterdink JL, Kosinski A, et al. The stroke outcomes and neuroimaging of intracranial atherosclerosis (SONIA) trial. Neurology. 2007;68(24):2099-2106. [DOI] [PubMed] [Google Scholar]
- 34.Duffis EJ, Jethwa P, Gupta G, Bonello K, Gandhi CD, Prestigiacomo CJ. Accuracy of computed tomographic angiography compared to digital subtraction angiography in the diagnosis of intracranial stenosis and its impact on clinical decision-making. J Stroke Cerebrovasc Dis. 2013;22(7):1013-1017. [DOI] [PubMed] [Google Scholar]
- 35.Markus HS, Droste DW, Kaps M, et al. Dual antiplatelet therapy with clopidogrel and aspirin in symptomatic carotid stenosis evaluated using Doppler embolic signal detection: the Clopidogrel and Aspirin for Reduction of Emboli in Symptomatic Carotid Stenosis (CARESS) trial. Circulation. 2005;111(17):2233-2240. [DOI] [PubMed] [Google Scholar]
- 36.Chaturvedi S, Turan TN, Lynn MJ, et al. Risk factor status and vascular events in patients with symptomatic intracranial stenosis. Neurology. 2007;69(22):2063-2068. [DOI] [PubMed] [Google Scholar]
- 37.Grundy SM, Stone NJ, Bailey AL, et al. . 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart association Task Force on clinical practice guidelines. Circulation. 2019;139:e1082-e1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Amarenco P, Kim JS, Labreuche J, et al. A Comparison of Two LDL cholesterol targets after ischemic stroke. N Engl J Med. 2020;382(1):9. [DOI] [PubMed] [Google Scholar]
- 39.Flemming KD, Brown RD Jr.. Secondary prevention strategies in ischemic stroke: identification and optimal management of modifiable risk factors. Mayo Clin Proc. 2004;79(10):1330-1340. [DOI] [PubMed] [Google Scholar]
- 40.Turan TN, Cotsonis G, Lynn MJ, Chaturvedi S, Chimowitz M, Warfarin-Aspirin Symptomatic Intracranial Disease Trial Investigators. Relationship between blood pressure and stroke recurrence in patients with intracranial arterial stenosis. Circulation. 2007;115(23):2969-2975. [DOI] [PubMed] [Google Scholar]
- 41.Yu DD, Pu YH, Pan YS, et al. High blood pressure increases the risk of poor outcome at discharge and 12-month follow-up in patients with symptomatic intracranial large artery stenosis and occlusions: subgroup analysis of the CICAS study. CNS Neurosci Ther. 2015;21(6):530-535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Correction to: systematic review for the 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart association Task Force on clinical practice guidelines. Hypertension. 2018;71:e145. [DOI] [PubMed] [Google Scholar]
- 43.Amin-Hanjani S, Turan TN, Du X, et al. . Higher stroke risk with lower blood pressure in hemodynamic vertebrobasilar disease: analysis from the VERiTAS study. J Stroke Cerebrovasc Dis. 2017;26:403-410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Feng X, Chan KL, Lan L, et al. Translesional pressure gradient alters relationship between blood pressure and recurrent stroke in intracranial stenosis. Stroke. 2020;51(6):1862-1864. [DOI] [PubMed] [Google Scholar]
- 45.Lee CD, Folsom AR, Blair SN. Physical activity and stroke risk: a meta-analysis. Stroke. 2003;34(10):2475-2481. [DOI] [PubMed] [Google Scholar]
- 46.Kleindorfer DO, Towfighi A, Chaturvedi S, et al. . Guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021;52:e364-e467. [DOI] [PubMed] [Google Scholar]
- 47.Alexander MJ, Zauner A, Chaloupka JC, et al. WEAVE trial: final results in 152 on-label patients. Stroke. 2019;50(4):889-894. [DOI] [PubMed] [Google Scholar]
- 48.Aghaebrahim A, Agnoletto GJ, Aguilar-Salinas P, et al. Endovascular recanalization of symptomatic intracranial arterial stenosis despite aggressive medical management. World Neurosurg. 2019;123:e693-e699. [DOI] [PubMed] [Google Scholar]
- 49.US Food and Drug Administration. Use of the Stryker Wingspan stent system outside of approved indications leads to an increased risk of stroke or death: FDA Safety Communication [online]. Accessed December 20, 2020. fda.gov/medical-devices/medical-device-safety/use-stryker-wingspan-stent-system-outside-approved-indications-leads-increased-risk-stroke-or-death
- 50.US Food and Drug Administration. 522 Postmarket surveillance studies database: rates of stroke and death [online]. accessdata.fda.gov/scripts/cdrh/cfdocs/cfPMA/pss.cfm?t_id=297&c_id=762
- 51.Gröschel K, Schnaudigel S, Pilgram SM, Wasser K, Kastrup A. A systematic review on outcome after stenting for intracranial atherosclerosis. Stroke. 2009;40(5):e340-7. [DOI] [PubMed] [Google Scholar]
- 52.Stapleton CJ, Chen YF, Shallwani H, et al. Submaximal angioplasty for symptomatic intracranial atherosclerotic disease: a meta-analysis of peri-procedural and long-term risk. Neurosurgery. 2020;86(6):755-762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kadooka K, Hagenbuch N, Anagnostakou V, Valavanis A, Kulcsár Z. Safety and efficacy of balloon angioplasty in symptomatic intracranial stenosis: a systematic review and meta-analysis. J Neuroradiol. 2020;47(1):27-32. [DOI] [PubMed] [Google Scholar]
- 54.Dumont TM, Sonig A, Mokin M, et al. Submaximal angioplasty for symptomatic intracranial atherosclerosis: a prospective phase I study. J Neurosurg. 2016;125(4):964-971. [DOI] [PubMed] [Google Scholar]
- 55.Powers WJ, Clarke WR, Grubb RL Jr., Videen TO, Adams HP, Derdeyn CP. Extracranial-intracranial bypass surgery for stroke prevention in hemodynamic cerebral ischemia: the Carotid Occlusion Surgery Study randomized trial. JAMA. 2011;306(18):1983-1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wang X, Tong X, Shi M, Shang Y, Wang H. Occipital artery to extradural vertebral artery bypass for posterior circulation ischemia. Oper Neurosurg. 2019;16(5):527-538. [DOI] [PubMed] [Google Scholar]
- 57.Rennert RC, Steinberg JA, Strickland BA, et al. Extracranial-to-intracranial bypass for refractory vertebrobasilar insufficiency. World Neurosurg. 2019;126:552-559. [DOI] [PubMed] [Google Scholar]
- 58.Dusick JR, Liebeskind DS, Saver JL, Martin NA, Gonzalez NR. Indirect revascularization for nonmoyamoya intracranial arterial stenoses: clinical and angiographic outcomes. J Neurosurg. 2012;117(1):94-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Komotar RJ, Starke RM, Otten ML, et al. The role of indirect extracranial-intracranial bypass in the treatment of symptomatic intracranial atheroocclusive disease. J Neurosurg. 2009;110(5):896-904. [DOI] [PubMed] [Google Scholar]
- 60.Zhang M, Horiuchi T, Nitta J, et al. Intraoperative test occlusion as adjustment of extracranial-to-intracranial bypass strategy for unclippable giant aneurysm of the internal carotid artery. World Neurosurg. 2019;122:129-132. [DOI] [PubMed] [Google Scholar]
- Additional references e1–e37 available in the supplemental document, links.lww.com/WNL/B803