Abstract
Essential to responsible practice and progress in neurology and neuroscience research is robust engagement with associated ethical dimensions and challenges. By virtue of the privileged relationship between personhood and the brain, and the importance of properties of the nervous system to what for most makes life worth living, conditions that affect neurologic function introduce a growing host of novel ethical and philosophical issues. Rather than serving a reactionary role, it is important for neurologists to anticipate such issues and develop familiarity with ethical analysis to inform quality medical practice and to safeguard neuroscience research. The field of neuroethics is an emerging career path devoted to identifying and evaluating such issues with the aim of informing optimal clinical practice and responsible neuroscience research. This article describes the past, present, and future of neuroethics, informed by an interview with one of the field's key founders and luminaries, Dr. James Bernat, with specific focus on training and career opportunities for neurologists in training.
Introduction
Responsible neurology practice and neuroscience research requires robust engagement with associated ethical issues and challenges.1-4 Neuroethics is an emerging career path devoted to evaluating such issues with the aim of informing optimal practice and progress. We describe the past, present, and future of neuroethics, focusing on training and career opportunities for neurologists. As opportunities for ethics engagement grow for clinicians, neurologists are especially well positioned to impactfully contribute due to unique arrays of consequential normative issues raised by neuroscience research, practice and policy, growing public interest, and emerging funding opportunities.
Toward Ethics-Informed Neuroscience Research and Practice
Neuroethics is the ethics of research and clinical neuroscience, that is, normatively what is right or wrong in evaluating or manipulating the nervous system when conducting neuroscience research or clinical care.5-8 Neuroethics also includes inquiry into neural correlates of moral cognition and behavior (neuroscience of ethics).9,10 Normative challenges posed by experiences of patients with neurologic illnesses and caregivers underscore the pragmatic importance of neuroethics inquiry.8,11,12 Disparities in access to and outcomes of neurologic care are of growing and crucial neuroethics concern.13 Knowledge of ethics also guides responsible neuroscience research, including managing concerns surrounding appropriate, equitable use of emerging neurotechnologies.
Over the past 2 decades, neuroethics has matured as a discipline with its own professional society (International Neuroethics Society), conferences, journals, faculty positions, textbooks, National Institutes of Health (NIH) Brain Research Through Advancing Innovative Neurotechnologies (BRAIN) Initiative committee, and scholarship.14,15 Most of this disciplinary organization has centered on research neuroethics. Neurologists should partner with research neuroethics scholars to advance clinical neuroethics. As neurologist and neuroethics researcher Winston Chiong (UCSF) presciently remarked, “…an integrated neuroethics must engage with ethical and social controversies that are direct working concerns of those in neuroscience, including the clinical neurosciences… a more inclusive conception of neuroethics would cohere with neuroscience's own self-conception as an interdisciplinary field… A more broadly engaged neuroethics would not only be a more useful partner to neuroscientists—particularly to those working with clinical populations.”14 Neuroethics may also be successfully combined with other neurology subspecialty training, particularly synergistic subspecialties include neurocritical care, cognitive behavioral neurology, stroke, neurorecovery, neurogenetics, global neurology, neurophysiology, and neuropalliative care.
Lessons From Dr. James Bernat, A Pioneering Leader in Neuroethics
What Drew You to Neuroethics, and How Did You Successfully Pursue This Career Path?
As a medical student at Cornell in the 1970s, I became interested in coma, consciousness, and brain death under the teachings of my professors Fred Plum and Jerome Posner. I intensively studied their classic textbook The Diagnosis of Stupor & Coma. During neurology residency at Dartmouth, I became interested in many topics now encompassed in critical care neurology, although no fellowship programs in that field then existed. I grew interested in learning more about bioethics, but no clinical fellowships in that field existed either. In my final year of training (1977), I identified mentors to learn from.
I began collaborating with philosopher Bernard Gert and psychiatrist-bioethicist Charles Culver at Dartmouth. We analyzed definitions and criteria of death and wrote several articles, one of which was cited by the President's Commission as the conceptual basis for brain death in Defining Death (1981). Gert & Culver taught the bioethics course to Dartmouth medical students and invited me to join. Over our years of collaboration, I learned moral philosophy from Gert and bioethics from Culver.
In the 1980s, I met Ronald Cranford, a neurologist-bioethicist (University of Minnesota) and chair of the AAN Ethics & Humanities Subcommittee. Ron invited me to join the committee, beginning my 26-year tenure on that committee with 10 as chair (1993–2003). We published 15 practice advisories in Neurology on various ethical problems in neurology and wrote AAN's Code of Professional Conduct. Our committee was promoted to AAN full committee status (AAN Ethics, Law & Humanities Committee). Committee members taught ethics courses at AAN meetings beginning in the 1980s. Later, our committee initiated AAN's Ethics Interest Section.
My clinical career began in 1977, directing neurology at V.A. Hospital in White River Junction, Vermont, serving on their ethics committee and later cofounding the Northeast Regional V.A. Ethics Center, which provided protected research time. With my colleague, William Nelson, we won the contract for the V.A. National Ethics Center, which I codirected before moving to Dartmouth-Hitchcock Medical Center in 1994 to chair the Bioethics Committee, run the ethics consultation service, and direct ethics teaching at Dartmouth Medical School, which I did for 20 years.
What Motivated You to Write Ethical Issues in Neurology?
No textbook of ethics in neurology existed. In the 1990s, Susan Pioli, acquisitions editor of Butterworth–Heinemann, proposed that I write a monograph on ethical issues in neurology. Writing that book made me systematically study each subject discussed because I tried to make the book a map of the developing field.
What Obstacles Did You Encounter While Pursuing This Path, and How Did You Overcome Them?
Two major issues for neurologists studying ethics are finding mentors in ethics and philosophy and obtaining protected scholarship time. Hospitals may grant protected time for ethics consultation service or obtaining a grant. During my career at the VA I recruited a prominent neurologist (Maurice Victor) to our medical center. He assisted me in running clinical and teaching services, which freed up time for scholarship. Later grants added additional protected time.
How Might Neurologists Inform Philosophical Inquiry?
Neurophilosophy is an emerging branch of philosophy centering on questions of personhood, personal identity, consciousness, and free will. Although many neurophilosophical questions are somewhat removed from neurologic practice, others are more relevant, such as the relationship of brain functioning to the definition of death. This area of neurophilosophy is highly relevant to neurologic practice because it comprises the conceptual basis for brain death determination.
What Advice Do You Have for Trainees Interested in This Field?
For trainees interested in learning about neuroethics, Neurologist-in-Training Clinical Ethics Elective and other resources are available through the AAN. Self-study should be conducted under direction of a mentor if available. Many residencies schedule regular case-based ethics rounds, studying and discussing cases from reference works. Trainees with goals of making it a dedicated career should consider postresidency clinical ethics fellowship. Clinical ethics fellowship provides academic learning in moral philosophy, bioethics, and related law and clinical experience in ethics consultations ideal to begin one's career with. Neurologists may also obtain Healthcare Ethics Consultation Certification.
What Concrete Steps Might a Trainee Take to Build a Strong Foundation For Embarking on a Similar Career Pathway?
Once fellowship training is complete and the neurologist is searching for a position, an ideal job would combine clinical care with ethics consultations, service on the ethics committee, and teaching. The early-career neurologist should become active in AAN's Ethics Section with an eye toward Ethics, Law & Humanities Committee membership. In both roles, the neurologist could initiate projects studying important questions in neuroethics, permitting scholarly literature contributions.
What Are Some Emerging Research Areas in This Field of Growing Importance?
Neuroethics has grown considerably with the proliferation of ethics committees, consultation services, publication of scholarly articles, conferences, growing public interest, and prominence in public sectors (e.g., NIH BRAIN Initiative ethics committee; Defense Advanced Research Projects Agency/Department of Defense funding exploring ethical aspects of neuroenhancement and electrical stimulation). Growth will continue because of greater public interest in ethical aspects of health care and neuroscience.
Emerging neuroethics research areas can be classified by category. The largest category is ethical aspects of neurotechnologies, including neuroimaging, electrodiagnostics, brain stimulation, pharmacologic stimulation, neural implants, brain organoids, cognitive enhancement, mobile health technologies, brain-computer interfaces, and robotics, many of which were not imaginable generations ago. Other categories include managing incidental findings, psychosurgery, neuroresuscitation, neurogenetics, environmental neuroethics, neurophilosophy, interfaces of neuroethics and law (such as personal responsibility in states of brain damage and using neuroimaging in legal cases), equity, and human rights. The breadth of these areas is expanding rapidly with new advances.
What Career Opportunities Are Enabled by Specialized Training in Ethics?
Specialized ethics training can lead to chairing an ethics committee, ethics consultation service, or directing clinical ethics education. This background also facilitates publication of ethics articles resulting from empirical or conceptual studies. The neurologist can collaborate with nurse-ethicists, bioethicists, neuroscientists, philosophers, legal scholars, and others to study emerging topics.
Neuroethics: An Emerging Neurology Subspecialty
As ethical and philosophical dimensions of neuroscience research and clinical practice continue to evolve, clinical and research neuroethics are of increasing importance. Opportunities for neurologists to pursue training, research, and leadership in neuroethics are growing. Although neuroethics is a multidisciplinary field populated with practitioners from varied backgrounds, clinicians are especially well positioned to impactfully contribute to the field of neuroethics. All neurologists should be familiar with the neuroethics necessary to guide responsible practice, and those who are interested in neuroethics as a career could develop and apply ethics expertise through studying key references (eTable 1A, http://links.lww.com/WNL/B789), establishing mentors, fellowship training (eTable 1B, http://links.lww.com/WNL/B789), blending ethics committee and consultation involvement, neuroethics research and teaching. Mentorship and support pathways for trainees interested in this emerging field should be recognized and strengthened by professional societies and training programs to ensure that neurologists are well prepared to proactively identify and rigorously appraise ethical issues in neuroscience now and well into the future.
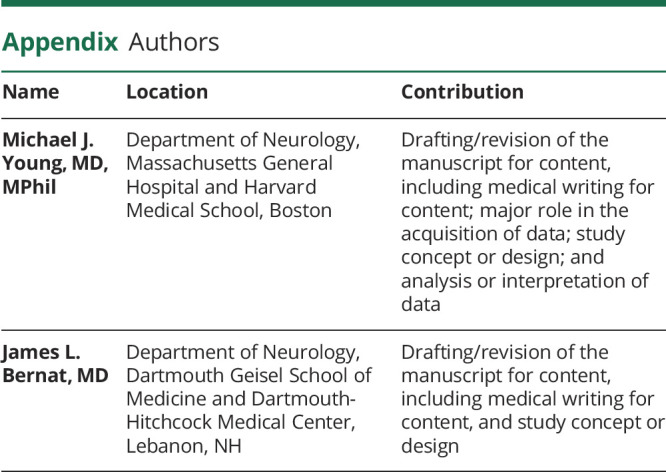
Appendix. Authors
Study Funding
MJY receives support from the NIH BRAIN Initiative (F32MH123001), Tiny Blue Dot Foundation, and American Academy of Neurology (Palatucci Advocacy Grant).
Disclosure
The authors report no disclosures relevant to the manuscript. Go to Neurology.org/N for full disclosures.
References
- 1.Bernat JL. Ethical Issues in Neurology, 3rd ed. : Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 2.Lewis A, Bernat JL, editors. Ethics in neurology. Semin Neurol. 2018;38:493-598. [DOI] [PubMed] [Google Scholar]
- 3.Greely HT, Grady C, Ramos KM, et al. . Neuroethics guiding principles for the NIH BRAIN initiative. J Neurosci. 2018;38(50):10586-10588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Illes J. Neuroethics: Anticipating the Future. Oxford University Press; 2017. [Google Scholar]
- 5.Roskies A. Neuroethics for the new millennium. Neuron. 2002;35(1):21-23. [DOI] [PubMed] [Google Scholar]
- 6.Ramos KM, Grady C, Greely HT, et al. . The NIH BRAIN Initiative: integrating neuroethics and neuroscience. Neuron. 2019;101(3):394-398. [DOI] [PubMed] [Google Scholar]
- 7.Traner CB, Tolchin DW, Tolchin B. Medical ethics education for neurology residents: where do we go from here? Semin Neurol. 2018;38(5):497-504. [DOI] [PubMed] [Google Scholar]
- 8.Fins JJ. Toward a pragmatic neuroethics in theory and practice. In: Racine E, Aspler J, eds. Debates about Neuroethics: Perspectives on its Development, Focus, and Future. Springer; 2017:45-65. [Google Scholar]
- 9.Illes J, Bird SJ. Neuroethics: a modern context for ethics in neuroscience. Trends Neurosciences. 2006;29(9):511-517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kamm FM. Neuroscience and moral reasoning: a note on recent research. Philos Public Aff. 2009;37(4):330-345. [Google Scholar]
- 11.Tolchin B, Conwit R, Epstein LG, Russell JA. AAN position statement: ethical issues in clinical research in neurology. Neurology. 2020;94(15):661-669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tolchin B, Willey JZ, Prager K. Education research: a case-based bioethics curriculum for neurology residents. Neurology. 2015;84(13):e91-e93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saadi A, Himmelstein DU, Woolhandler S, Mejia NI. Racial disparities in neurologic health care access and utilization in the United States. Neurology. 2017;88(24):2268-2275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chiong W. Insiders and outsiders: lessons for neuroethics from the history of bioethics. AJOB Neurosci. 2020;11(3):155-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Farahany N, Ramos KM. Neuroethics: fostering collaborations to enable neuroscientific discovery. AJOB Neurosci. 2020;11(3):148-154. [DOI] [PubMed] [Google Scholar]


