Adverse pregnancy outcomes are associated with long-term risk for cardiometabolic disease in both women and their offspring.1 Individual cardiovascular risk factors (e.g. obesity and hypertension) present before pregnancy have been associated with higher risk for maternal and neonatal morbidity and mortality;2 however, the presence of multiple co-occurring risk factors may be associated with greater risk for adverse pregnancy outcomes than any single risk factor alone. Given the rising prevalence of cardiovascular risk factors in women of reproductive age,3,4 identifying the association between the total burden of pre-pregnancy cardiovascular risk factors and adverse maternal and offspring outcomes can help inform comprehensive prevention strategies that move beyond targeting any single risk factor.
We conducted a cross-sectional analysis of maternal and foetal data from the National Center for Health Statistics (NCHS), which collects data on all live births and foetal deaths (after 20 weeks’ gestation) in the USA. Data are reported to the NCHS by healthcare professionals present at delivery according to a standard protocol that includes a chart review, medical record abstraction, and maternal self-report.5,6 We pooled individual-level data from births to women aged 15–44 years from 2014 to 2018 to allow for adequate power to examine rare outcomes. Four pre-pregnancy cardiovascular risk factors were assigned 1 point if present and 0 points if absent, including body mass index (BMI) <18.5 kg/m2 or >24.9 kg/m2 and smoking by maternal self-report, and hypertension and diabetes ascertained by the medical professional at delivery, to construct a risk factor score ranging from 0 to 4. Pre-pregnancy hypertension and diabetes were defined by diagnosis prior to pregnancy and excluded diagnoses made during pregnancy.6 In a secondary analysis, we examined all four risk factors individually. We excluded records missing data on any of the pre-pregnancy risk factors or pregnancy outcomes of interest (3.9%). We used modified Poisson regression to estimate relative risks for maternal ICU admission, preterm birth (<37 weeks), low birthweight (<2500 g), and foetal death associated with greater risk factor burden (1, 2, 3, or 4) compared with no risk factors (0). Women with foetal death (0.5%) were included only in the analysis for this outcome. All analyses were adjusted for maternal age at delivery, race/ethnicity, education, receipt of prenatal care, parity, and birth plurality. We conducted a complete case analysis due to low missingness in covariates (3.7%). We completed a sensitivity analysis in nulliparous women to minimize bias related to repeat pregnancies included in the de-identified dataset. This study was exempt from IRB review due to the de-identified, publicly available dataset.
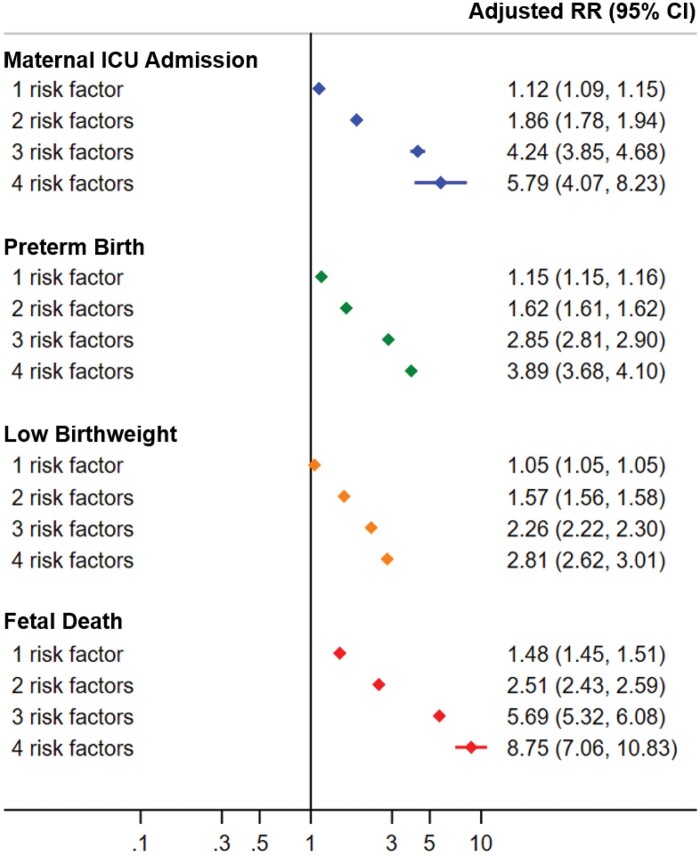
Of 18 646 512 pregnancies included, mean (SD) maternal age was 28.6 (5.8) years, and 53.6% of women were non-Hispanic White, 14.8% non-Hispanic Black, 23.0% Hispanic, 6.8% non-Hispanic Asian, and 1.9% other race/ethnicity. More than 60% of women had one or more pre-pregnancy cardiovascular risk factors (52.5%, 7.3%, 0.3%, and 0.02% had 1, 2, 3, and 4 risk factors, respectively). Compared with women with no risk factors, women with one or more risk factors had on average lower educational attainment (79.5-85.3% vs. 88.7% graduated high school), less receipt of prenatal care (97.8–98.5% vs. 98.7%), higher prevalence of multiparity (64.4–69.3% vs. 56.9%), and higher prevalence of prior spontaneous or induced pregnancy loss (27.4–46.0% vs. 23.4%) There were consistent and marked graded associations between greater pre-pregnancy risk factor burden and higher risk of adverse maternal and foetal outcomes (Figure 1); for example, the risk ratios (95% CI) of maternal ICU admission (compared to women with no pre-pregnancy risk factors) were 1.12 (1.09, 1.15) for one risk factor, 1.86 (1.78, 1.94) for two risk factors, 4.24 (3.85, 4.68) for three risk factors, and 5.79 (4.07, 8.23) for four risk factors. Individual components of the risk factor score were directly associated with adverse outcomes, with heterogeneity in effect sizes, except for non-ideal BMI, which was inversely associated with low birthweight (Table 1). Similar patterns were observed in sensitivity analyses in nulliparous women (data not shown).
Figure 1.
Relative risk of pre-pregnancy cardiovascular risk factor burden for adverse maternal and offspring outcomes. There were positive and graded associations of greater cardiovascular risk factor burden, compared with no pre-pregnancy risk factors, for all four outcomes. RR represents relative risk; CI confidence interval.
Table 1.
Relative risk of individual pre-pregnancy cardiovascular risk factors for adverse maternal and offspring outcomes
| Pre-pregnancy risk factor | Adjusted RRa (95% CI) |
|||
|---|---|---|---|---|
| Maternal ICU admission | Preterm birth | Low birthweight | Foetal death | |
| Non-ideal BMI | 1.04 (1.01, 1.07) | 1.08 (1.08, 1.09) | 0.94 (0.94, 0.94) | 1.39 (1.36, 1.41) |
| Smoking | 1.23 (1.18, 1.28) | 1.28 (1.28, 1.29) | 1.64 (1.64, 1.65) | 1.59 (1.55, 1.64) |
| Hypertension | 2.84 (2.70, 2.99) | 1.92 (1.91, 1.93) | 1.98 (1.96, 1.99) | 1.92 (1.84, 2.00) |
| Diabetes | 2.71 (2.53, 2.90) | 2.27 (2.24, 2.29) | 1.36 (1.34, 1.38) | 2.98 (2.84, 3.13) |
Based on modified Poisson regression including all four risk factors coded as 1 if present and 0 if absent. Adjusted for maternal age at delivery, race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, Asian, or Other), education (Less than high school, high school graduate, or any college), receipt of prenatal care (or no prenatal care), parity (nulliparous or multiparous), and birth plurality (singleton or multiple gestation).
BMI, body mass index; CI, confidence interval; RR, relative risk.
In this analysis of nationwide data, we found that pre-pregnancy cardiovascular risk factors are highly prevalent, and there are consistent and graded associations between greater risk factor burden and key adverse maternal and offspring outcomes. Although individual risk factors were generally associated with these outcomes, the cumulative risk factor burden was associated with higher risk than any single risk factor; compared to women with no pre-pregnancy risk factors, those with all four risk factors (3242 women) had approximately 5.8-fold higher risk for ICU admission, 3.9-fold for preterm birth, 2.8-fold for low birthweight, and 8.7-fold for foetal death. Limitations of this analysis include the potential for misclassification of pre-pregnancy risk factor status such as bias related to self-report of BMI, inability to characterize risk factor control and its potential to modify associations with adverse pregnancy outcomes, lack of available data on lifestyle factors, and absence of linkage with maternal mortality. However, the NCHS Birth Data Files represent the most robust and comprehensive surveillance dataset, which captures all pregnancies in the USA resulting in a live birth or foetal death. While the primary sample included repeat pregnancies, data from nulliparous women demonstrated similar findings.
The association between risk factor counting and cardiovascular and non-cardiovascular outcomes has been examined extensively outside of pregnancy.7,8 Our data extend prior findings by validating the importance of the pre-pregnancy cardiovascular risk factor profile for risks of several key adverse maternal and offspring outcomes, which are known to influence the risk of subsequent cardiovascular disease.1 Future studies should seek to incorporate measures of cholesterol and lifestyle factors, as well as important non-modifiable risk factors such as family history of cardiovascular disease, which has been associated with pregnancy loss9 and may warrant increased attention to optimizing pre-pregnancy cardiovascular health. Assessment of cardiovascular risk factors on the individual level could be applied before pregnancy, when prevention may have a greater benefit than during pregnancy when the time period to intervene is limited.
Acknowledgements
The funding sponsor did not contribute to design and conduct of the study, collection, management, analysis, or interpretation of the data or preparation, review, or approval of the manuscript. The authors take responsibility for decision to submit the manuscript for publication.
Funding
The National Institutes of Health (P30AG059988 and P30DK092939) and the American Heart Association (#19TPA34890060) to S.K. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest: none declared.
References
- 1. Lane-Cordova AD, Khan SS, Grobman WA, Greenland P, Shah SJ.. Long-term cardiovascular risks associated with adverse pregnancy outcomes. J Am Coll Cardiol 2019;73:2106–2116. [DOI] [PubMed] [Google Scholar]
- 2. Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Cheng S, Delling FN, Elkind MSV, Evenson KR, Ferguson JF, Gupta DK, Khan SS, Kissela BM, Knutson KL, Lee CD, Lewis TT, Liu J, Loop MS, Lutsey PL, Ma J, Mackey J, Martin SS, Matchar DB, Mussolino ME, Navaneethan SD, Perak AM, Roth GA, Samad Z, Satou GM, Schroeder EB, Shah SH, Shay CM, Stokes A, VanWagner LB, Wang N-Y, Tsao CW; On behalf of the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics–2021 update: a report from the American Heart Association. Circulation 2021;143:e439–e455. [DOI] [PubMed] [Google Scholar]
- 3. Driscoll AK, Gregory EC.. Increases in prepregnancy obesity: United States, 2016-2019. NCHS Data Brief 2020;392:1–8. [PubMed] [Google Scholar]
- 4. Cameron NA, Molsberry R, Pierce JB, Perak AM, Grobman WA, Allen NB, Greenland P, Lloyd-Jones DM, Khan SS.. Pre-pregnancy hypertension among women in rural and urban areas of the United States. J Am Coll Cardiol 2020;76:2611–2619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Center for Health Statistics. Birth Edit Specifications for the 2003 Proposed Revision of the U.S. Standard Certificate of Birth. https://www.cdc.gov/nchs/data/dvs/birth_edit_specifications.pdf(17 June 2021).
- 6.National Center for Health Statistics. Guide to completing the facility worksheets for the certificate of live birth and report of fetal death (2003. revision). https://www.cdc.gov/nchs/data/dvs/GuidetoCompleteFacilityWks.pdf(17 June 2021).
- 7. Stamler J, Stamler R, Neaton JD, Wentworth D, Daviglus ML, Garside D, Dyer AR, Liu K, Greenland P.. Low risk-factor profile and long-term cardiovascular and noncardiovascular mortality and life expectancy findings for 5 large cohorts of young adult and middle-aged men and women. JAMA 1999;282:2012–2018. [DOI] [PubMed] [Google Scholar]
- 8. Perak AM, Ning H, Khan SS, Bundy JD, Allen NB, Lewis CE, Jacobs DR, Van Horn LV, Lloyd-Jones DM.. Associations of late adolescent or young adult cardiovascular health with premature cardiovascular disease and mortality. J Am Coll Cardiol 2020;76:2695–2707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ranthe MF, Diaz LJ, Behrens I, Bundgaard H, Simonsen J, Melbye M, Boyd HA.. Association between pregnancy losses in women and risk of atherosclerotic disease in their relatives: a nationwide cohort study. Eur Heart J 2016;37:900–907. [DOI] [PubMed] [Google Scholar]