This editorial refers to ‘Underperformance of clinical risk scores in identifying imaging-based high cardiovascular risk in psoriasis: results from two observational cohorts’, by A. Gonzalez-Cantero et al., pp. 591–598.
Psoriasis is one of the most common autoimmune disorders that primarily affects the skin and joints.1 However, many patients with psoriasis harbour cardiovascular risk factors including Type 2 diabetes,2 dyslipidaemia,3 hypertension,4 and obesity.5 Notwithstanding the high prevalence of cardiovascular risk factors, psoriasis is independently associated with an increased risk of premature cardiovascular disease (CVD).6 Given the increased risk of CVD in patients with psoriasis, appropriate cardiovascular risk stratification and identification of patients at elevated risk are integral parts of patient care.
The current foundation of primary CVD prevention lies in the use of risk prediction scores that estimate risk of developing incident cardiovascular events in asymptomatic individuals.7 Cardiovascular risk prediction tools are often embedded in electronic medical record systems and allow for rapid estimation of absolute risk.7 This ease of use has led to widespread adoption of these tools in the clinical setting and thus preventive cardiovascular care. The potential benefits of lifestyle interventions and preventive pharmacotherapies can be assessed in real time, assisting both clinicians and patients in collaborative informed decision-making.7 The most commonly used cardiovascular risk estimation tools include the European Systematic COronary Risk Evaluation (SCORE),8 and the American Pooled Cohort Equation (PCE).9 SCORE helps estimate the 10-year risk of CVD death,8 while PCE helps determine the 10-year risk of atherosclerotic CVD (ASCVD) events (defined as coronary death, non-fatal myocardial infarction, fatal or non-fatal stroke).9 It is well-established that both SCORE and PCE are heavily influenced by age and can be inept at predicting long-term cardiovascular risk in younger individuals.10 Thus, risk prediction algorithms that capture the cumulative influence of cardiovascular risk factors over an individual’s lifetime have been promulgated.10 Commonly used long-term cardiovascular risk scores include the European QRISK lifetime score11 and the American ASCVD lifetime score.9
It is important to note that these cardiovascular risk estimation tools utilize population-level cardiovascular risk factors to predict the natural course of CVD.7 While these tools are well-calibrated for general populations, there is divergence between estimated and observed risk in patients with chronic inflammatory conditions including psoriasis,12 systemic lupus erythematosus,13 and rheumatoid arthritis.14 Traditional risk estimation tools tend to underestimate risk in such patients as they fail to account for systemic inflammation, a key driver of atherosclerosis, that can account for up to 20–30% of residual risk for incident CVD.15 In this context, the European League Against Rheumatism has recommended multiplying estimated 10-year cardiovascular risk by 1.5 to allow better alignment of predicted and observed risk in patients with autoimmune diseases.16
In addition to traditional cardiovascular risk factors that comprise risk estimation tools, subclinical atherosclerosis as determined by non-invasive imaging techniques like ultrasonography and computed tomography (CT) is an important ‘non-traditional’ cardiovascular risk factor.17 The evidence of subclinical atherosclerosis reflects the impact of risk factors over an individual’s lifetime and is an independent predictor of cardiovascular risk.17 Furthermore, several studies have demonstrated its ability to refine cardiovascular risk estimation in the general population.18 As such, subclinical atherosclerosis may have a promising role in enhancing cardiovascular risk estimation in patients with autoimmune inflammatory diseases including psoriasis. The first step in answering this important question is determining the alignment of subclinical atherosclerosis with estimated CVD risk in patients with psoriasis. This knowledge gap has now been addressed by Gonzalez-Cantero et al. in the accompanying study published in the Journal19 .
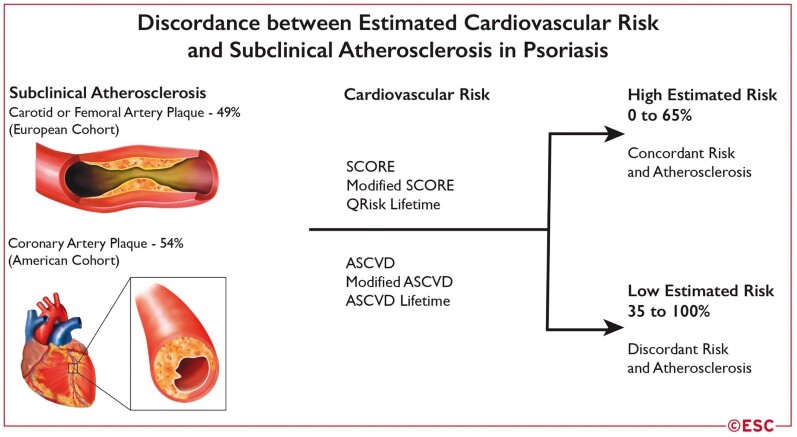
The authors studied the relationship of estimated cardiovascular risk with subclinical atherosclerosis in 238 psoriasis patients recruited in two observational cohorts across the Atlantic. Participants of the European cohort (N = 73) underwent ultrasonographic examination of carotid and femoral arteries, while participants of the American cohort (N = 165) underwent coronary CT angiography to determine the presence of subclinical atherosclerotic plaque. Participants in both cohorts were middle-aged, and subclinical atherosclerotic plaque was seen in 37 European (50%) and 89 American (54%) participants. Cardiovascular risk was estimated using SCORE, modified SCORE (SCORE risk * 1.5), and QRISK-lifetime algorithms in the European cohort; while ASCVD, modified ASCVD (ASCVD * 1.5), and ASCVD-lifetime algorithms were used in the American cohort. When established cut-offs for estimated cardiovascular risk were used in the European cohort, 0%, 5%, and 51% participants were classified as high-risk by SCORE, modified SCORE, and QRISK-lifetime algorithms, respectively. The corresponding proportions were 15%, 30%, and 41% with ASCVD, modified ASCVD, and ASCVD-lifetime algorithms, respectively, in the American cohort.
As expected, the absolute cardiovascular risk estimated using all risk prediction tools listed above was higher among psoriasis patients with subclinical atherosclerosis as compared to those without. However, the authors observed that cardiovascular risk scores did not perform well at identifying subclinical atherosclerosis when risk categories were considered. In the European cohort, none of the participants with carotid or femoral atherosclerotic plaque were classified as high risk by SCORE and only 11% were classified as high risk by modified SCORE. Similarly, in the American cohort, 20% of the participants with coronary atherosclerotic plaque were classified as high risk by ASCVD and 45% were classified as high risk by modified ASCVD. Lifetime risk prediction tools performed better at aligning with subclinical atherosclerosis, such that 65% Europeans with subclinical atherosclerosis were in the high-risk QRISK-lifetime group. The corresponding proportion in Americans was 54% with ASCVD-lifetime risk prediction approach. Overall, a significant proportion of European and American psoriasis patients with subclinical atherosclerotic plaque were classified as non-high risk by traditional cardiovascular risk estimation tools (Figure 1).
Figure 1.
Discordance between estimated cardiovascular risk and subclinical atherosclerosis in psoriasis.
These observations are highly relevant when considered under these two tenets of the current paradigm of primary CVD prevention: (i) categories of estimated cardiovascular risk are the yardstick for guiding cardiovascular prevention strategies including statin use in high-risk patients, and (ii) evidence of subclinical atherosclerotic plaque has now been recognized as a marker of increased cardiovascular risk that should prompt clinician-patient discussion regarding statin initiation.20 Thus, the discordance between estimated cardiovascular risk and presence of subclinical atherosclerotic plaque highlights the potential utility of incorporating non-invasive atherosclerosis imaging as a decision making aid for guiding primary cardiovascular prevention strategies in patients with psoriasis. Furthermore, this study also demonstrates that nearly 50% of asymptomatic patients with psoriasis have evidence of subclinical atherosclerosis, lending support to the notion that autoimmune inflammatory conditions such as psoriasis be regarded as ‘risk-enhancing’ factors in primary prevention.7 That being said, it is important to understand that evidence of subclinical atherosclerosis is a surrogate marker for ASCVD and cannot be misconstrued as a cardiovascular event. Furthermore, the current study is limited by the modest sample size of both cohorts and the lack of a control group that could facilitate comparisons with the general population. Taken together, this report is an important first step in enhancing our understanding of the role of subclinical atherosclerosis imaging for improving risk stratification in patients with psoriasis, a patient population that harbours a high CVD risk.
Funding
S.J.I. is supported by Bryon Williams Jr, MD Fellowship Fund and the National Institutes of Health (T32 HL130025 and T32 HL007745-26A1). A.M. is supported by American Heart Association (19POST34400057) and Abraham J. & Phyllis Katz Foundation.
Conflict of interest: none declared.
The opinions expressed in this article are not necessarily those of the Editors of the European Journal of Preventive Cardiology or of the European Society of Cardiology.
References
- 1. Armstrong AW, Read C.. Pathophysiology, clinical presentation, and treatment of psoriasis: a review. JAMA 2020;323:1945–1960. [DOI] [PubMed] [Google Scholar]
- 2. Armstrong AW, Harskamp CT, Armstrong EJ.. Psoriasis and the risk of diabetes mellitus: a systematic review and meta-analysis. JAMA Dermatol 2013;149:84–91. [DOI] [PubMed] [Google Scholar]
- 3. Ma C, Harskamp CT, Armstrong EJ, Armstrong AW. The association between psoriasis and dyslipidaemia: a systematic review. Br J Dermatol 2013;168:486–495. [DOI] [PubMed] [Google Scholar]
- 4. Armstrong AW, Harskamp CT, Armstrong EJ.. The association between psoriasis and hypertension: a systematic review and meta-analysis of observational studies. J Hypertens 2013;31:433–442; discussion 442–443. [DOI] [PubMed] [Google Scholar]
- 5. Armstrong AW, Harskamp CT, Armstrong EJ.. The association between psoriasis and obesity: a systematic review and meta-analysis of observational studies. Nutr Diabetes 2012;2:e54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Prodanovich S, Kirsner RS, Kravetz JD, Fangchao M, Martinez L, Federman DG. Association of psoriasis with coronary artery, cerebrovascular, and peripheral vascular diseases and mortality. Arch Dermatol 2009;145:700–703. [DOI] [PubMed] [Google Scholar]
- 7. Lloyd-Jones DM, Braun LT, Ndumele CE, Smith SC, Sperling LS, Virani SS, Blumenthal RS. Use of risk assessment tools to guide decision-making in the primary prevention of atherosclerotic cardiovascular disease: a special report from the American Heart Association and American College of Cardiology. Circulation 2019;139:e1162–e1177. [DOI] [PubMed] [Google Scholar]
- 8. Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney MT, Corra U, Cosyns B, Deaton C, Graham I, Hall MS, Hobbs FDR, Lochen ML, Lollgen H, Marques-Vidal P, Perk J, Prescott E, Redon J, Richter DJ, Sattar N, Smulders Y, Tiberi M, van der Worp HB, van Dis I, Verschuren WMM, Binno S, E. S. C. Scientific Document Group. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts)Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 2016;37:2315–2381.27222591 [Google Scholar]
- 9. Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, Greenland P, Lackland DT, Levy D, O’Donnell CJ, Robinson JG, Schwartz JS, Shero ST, Smith SC, Sorlie P, Stone NJ, Wilson, PWF 2013 ACC/AHA Guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;63:2935–2959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Berry JD, Dyer A, Cai X, Garside DB, Ning H, Thomas A, Greenland P, Horn LV, Tracy RP, Lloyd-Jones DMet al. Lifetime risks of cardiovascular disease. N Engl J Med 2012;366:321–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hippisley-Cox J, Coupland C, Robson J, Brindle P. Derivation, validation, and evaluation of a new QRISK model to estimate lifetime risk of cardiovascular disease: cohort study using QResearch database. BMJ 2010;341:c6624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Eder L, Chandran V, Gladman DD.. The Framingham Risk Score underestimates the extent of subclinical atherosclerosis in patients with psoriatic disease. Ann Rheum Dis 2014;73:1990–1996. [DOI] [PubMed] [Google Scholar]
- 13. Drosos GC, Konstantonis G, Sfikakis PP, Tektonidou MG. Underperformance of clinical risk scores in identifying vascular ultrasound-based high cardiovascular risk in systemic lupus erythematosus. Eur J Prev Cardiol 2020;doi:10.1177/2047487320906650. [DOI] [PubMed] [Google Scholar]
- 14. Arts EEA, Popa C, Den Broeder AA, Semb AG, Toms T,Kitas GD, van Riel PL, Fransen J. Performance of four current risk algorithms in predicting cardiovascular events in patients with early rheumatoid arthritis. Ann Rheum Dis 2015;74:668–674. [DOI] [PubMed] [Google Scholar]
- 15. Harrington RA. Targeting inflammation in coronary artery disease. N Engl J Med 2017;377:1197–1198. [DOI] [PubMed] [Google Scholar]
- 16. Agca R, Heslinga SC, Rollefstad S, Heslinga M, McInnes IB, Peters MJL, Kvien TK, Dougados M, Radner H, Atzeni F, Primdahl J, Södergren A, Wallberg Jonsson S, van Rompay J, Zabalan C, Pedersen TR, Jacobsson L, de Vlam K, Gonzalez-Gay MA, Semb AG, Kitas GD, Smulders YM, Szekanecz Z, Sattar N, Symmons DPM, Nurmohamed MT. EULAR recommendations for cardiovascular disease risk management in patients with rheumatoid arthritis and other forms of inflammatory joint disorders: 2015/2016 update. Ann Rheum Dis 2017;76:17–28. [DOI] [PubMed] [Google Scholar]
- 17. Kozakova M, Palombo C.. Imaging subclinical atherosclerosis in cardiovascular risk stratification. Eur J Prev Cardiol 2020;doi:10.1177/2047487320916589. [DOI] [PubMed] [Google Scholar]
- 18. Mehta A, Blaha MJ, Miller III J, et al. Coronary artery calcium scoring: a valuable aid in shared decision making among non-traditional risk markers. Curr Cardiovasc Imaging Rep 2017;10;doi:10.1007/s12410-017-9431-3. [Google Scholar]
- 19.Gonzalez-Cantero, AS Reddy, AK Dey, J Gonzalez-Cantero, E Munger, J Rodante, AI Sanchez-Moya, C Perez-Hortet, JL Gonzalez-Calvin, MP Playford, MG Barderas, A Ballester, N Jimenez-Gomez, P Jaén, MY Chen, JM Gelfand, and NN Mehta. Underperformance of clinical risk scores in identifying imaging-based high cardiovascular risk in psoriasis: results from two observational cohorts. Eur J Prev Cardiol 2022;29:591–598. [DOI] [PubMed] [Google Scholar]
- 20. Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J 2020;41:111–188. [DOI] [PubMed] [Google Scholar]