Abstract
Purpose
The aim of this study was to evaluate the prevalence of clinically relevant anatomical variations of the ethmoid sinuses and their potential association with ethmoid and maxillary sinus pathologies on cone-beam computed tomography (CBCT) scans. Additionally, potential associations with different sides and demographic factors, including age and sex, were evaluated.
Materials and Methods
In total, 273 CBCT scans with complete ethmoid and maxillary sinuses were analyzed to determine the prevalence of Agger nasi cell, supraorbital ethmoid cell, Haller cell, Onodi cell, and ethmomaxillary sinus. In addition, the health or pathology of the ethmoid and maxillary sinuses was also recorded to assess correlations with the aforementioned variations.
Results
The prevalence of Agger nasi cell was found to be the highest (95.6%) in this study, followed by Onodi cell (60.4%), Haller cell (29.3%), and supraorbital ethmoid cell (19.4%). Ethmomaxillary sinus was the least common finding (16.5%). Males and persons above 61 years of age had a significantly higher frequency of supraorbital ethmoid cell and Onodi cell, respectively. However, no significant relationships were noted between anatomical variations of the ethmoid sinus and pathologies of the ethmoid or maxillary sinus.
Conclusion
There was a high prevalence of ethmoid sinus variations in this Southern Chinese population. The prevalence of Agger nasi cell and Onodi cell was higher than that of other anatomical variations of the ethmoid sinuses. Anatomical variations of the ethmoid sinuses were not associated with ethmoid or maxillary sinus pathologies in this patient cohort.
Keywords: Cone-Beam Computed Tomography, Maxillary Sinus, Ethmoid Sinus
Introduction
The ethmoid bone is an unpaired intricate and delicate bone, which is centrally located in the skull. It comprises the cribriform plate, a median perpendicular plate, and 2 ethmoidal labyrinths.1 Within these labyrinths are 2 groups of air cells (anterior and posterior) that are generally known as ethmoid sinuses or ethmoidal air cells. These are essential for warming and humidifying the air flow, adjusting speech resonance, and can also influence drainage pathways of the paranasal sinuses.1,2
The ethmoid sinuses are already present at birth, and continue to develop up to the age of 12 years.3 The number of air cells varies considerably, with an average of 9 (ranging from 4 to 17) in each ethmoidal labyrinth.4 Anatomical variations of the ethmoid sinuses may occur when pneumatization of the ethmoid sinuses extends to the proximate paranasal sinuses, such as the frontal, maxillary, and sphenoid sinuses, or when the first ethmoturbinal of the nose remains.1 The most relevant anatomical variations for daily clinical practice are Agger nasi cell (ANC), supraorbital ethmoid cell (SOEC), Haller cell, Onodi cell, and ethmomaxillary sinus (EMS). Some of these variations may affect the drainage of the ostiomeatal complex and consequently could cause pathological changes of the maxillary sinuses.5 For dental surgeons, the maxillary sinus status should be thoroughly assessed prior to sinus-related surgery, such as sinus floor elevation procedures.6 Moreover, with the advent of functional endoscopic surgery (FESS), otolaryngologists who do not detect anatomical variations of the ethmoid sinuses beforehand risk damaging adjacent structures like the internal carotid artery, optic nerve, brain tissue, and orbits, potentially leading to carotid artery-cavernous sinus fistula, orbital hematoma, and even death.7 Hence, it is of the utmost importance to fully understand the anatomy of the ethmoid sinuses, as well as their anatomical variations, and assess potential pathologies before sinus-related surgery or FESS.
Cone-beam computed tomography (CBCT) provides 3-dimensional (3D) images with high spatial resolution and relatively low radiation dose compared to traditional computed tomography (CT) in the craniofacial region.8 In the literature, anatomical variations of the ethmoid sinuses have been frequently reported on CT,3,9,10 as well as their correlation with pathologies of the paranasal sinuses.11 However, to the best of our knowledge, no previous research has comprehensively described anatomical variations of the ethmoid sinuses and their associations with ethmoid and maxillary sinus pathologies using CBCT in a Southern Chinese population. Therefore, this study aimed to examine the prevalence of clinically relevant anatomical variations of the ethmoid sinuses and evaluate their potential correlation with ethmoid and maxillary sinus pathologies on CBCT scans. Additionally, potential associations with different sides and demographic factors, including age and sex, were evaluated.
Materials and Methods
This study was conducted in full accordance with the Declaration of Helsinki 2013 (www.wma.net). The study protocol was submitted to and approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (approval number: UW 20-549).
CBCT scans with a large field of view (20 cm×17 cm) obtained between February 2016 and June 2020 at Oral and Maxillofacial Radiology of Dentistry, the University of Hong Kong were screened. These scans were all obtained using a CBCT device (ProMax 3D Mid; Planmeca Oy, Helsinki, Finland). Indications for the scans varied from orthognathic pre-surgical planning and obstructive sleep apnea syndrome airway assessment to the analysis of temporomandibular joint-related pathology.
Only scans exhibiting a complete view of the ethmoid and maxillary sinuses were included. As the adult appearance of the ethmoid sinus becomes apparent on CBCT scans at about 12 years old, any scans obtained from individuals 12 years and above were included.3 CBCT scans were excluded in this study if severe motion and/or metal artifacts were noticed or if patients had a known history of surgical intervention/trauma in the ethmoid and maxillary sinus region.
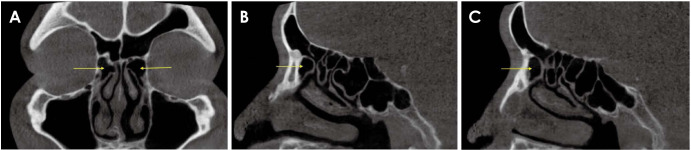
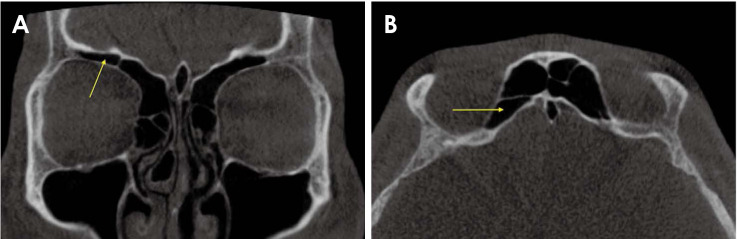
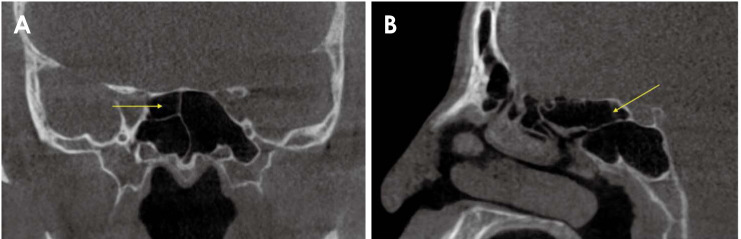
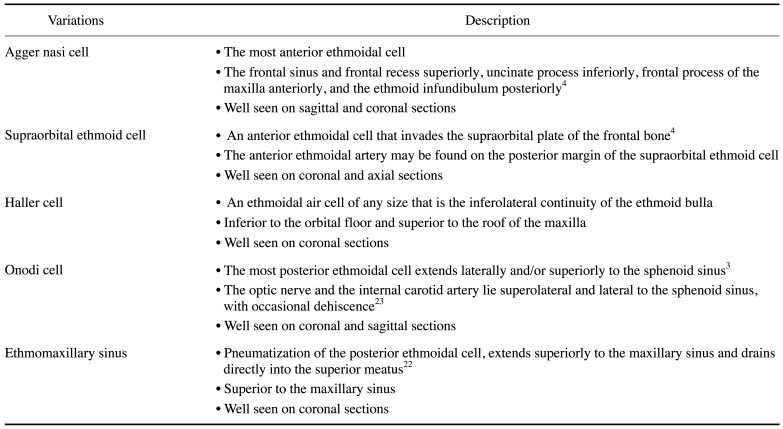
The variations of the ethmoid sinuses assessed include ANC (Fig. 1), SOEC (Fig. 2), Haller cell (Fig. 3), Onodi cell (Fig. 4), and EMS (Fig. 5). In CBCT images, ANC is the most anterior ethmoidal cell with the frontal sinus and frontal recess superiorly, SOEC is an anterior ethmoidal cell that invades the supraorbital plate of the frontal bone, Haller cell is the inferolateral continuity of the ethmoid bulla superior to the roof of the maxilla, Onodi cell is the most posterior ethmoidal cell that extends laterally and/or superiorly to the sphenoid sinus, and EMS is the pneumatization of the posterior ethmoidal cell, which extends superiorly to the maxillary sinus and drains directly into the superior meatus (Table 1).
Fig. 1. Agger nasi cells (arrows) are shown on both the left and right sides on coronal (A), left-side sagittal (B), and right-side sagittal (C) cone-beam computed tomography views.
Fig. 2. A supraorbital ethmoid cell (arrows) is noted on the right side on coronal (A) and axial (B) CBCT views.
Fig. 3. Coronal view of Haller cells (arrows) are shown on both the left and right sides.

Fig. 4. An onodi cell (arrows) is noted on the right side on coronal (A) and sagittal (B) cone-beam computed tomography views.
Fig. 5. Coronal view of ethmomaxillary sinuses are shown on both the left and right sides (arrows).
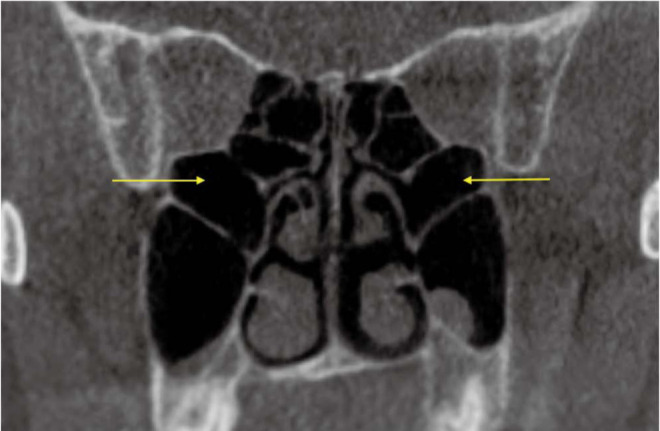
Table 1. Details and summary of the anatomical variations of the ethmoid sinuses that were assessed.
The health status of the ethmoid and maxillary sinuses was assessed according to the radiographic mucosal morphology.12,13,14,15 Only CBCT scans presenting criterion 1) in the following list were considered healthy: 1) inconspicuous or up to 2 mm thickening of the sinus membrane, 2) flat mucosal thickening more than 2 mm, 3) semispheric thickening of the membrane (suspected mucous retention cyst), 4) complete opacification of the sinus, 5) mixed flat and semispherical thickenings, 6) others (e.g., cyst, suspected neoplasia).
The presence (yes or no) and type of the anatomical variations of the ethmoid sinuses, as well as the ethmoid and maxillary sinus status, were assessed on the selected CBCT scans. The frequency of anatomical variations of the ethmoid sinuses was further calculated. To evaluate the potential association between these anatomical variations and ethmoid or maxillary sinus pathologies, the selected CBCT scans were divided into 2 groups according to the presence or absence of ethmoid or maxillary sinus pathologies (yes or no). Regarding age, CBCT scans were divided into adolescent (12-18 years), adult (19-60 years) and elderly (61 years and above) groups.
Prior to the assessment, 2 authors (LH and KFH) were calibrated by reviewing CBCT scans not pertinent to the study. All CBCT scans were then assessed by 2 calibrated observers. LH evaluated the scans twice with a wash-out period of 2 weeks, and KFH analyzed the same scans once to determine inter- and intra-rater reliability (repeatability and reproducibility). Disagreements encountered in the evaluation of a scan were resolved via consensus between both observers.
The CBCT readings were done on a Philips 223 V LED monitor (Philips, Amsterdam, Netherlands) with a resolution of 1,920×1,080 pixels. The smallest slice thickness of 0.4 mm was recommended based on the 0.4-mm voxel size used for the scans. Both observers were allowed to employ the available tools to adjust image brightness, contrast, and zoom mode using the software included in the device (Romexis, Planmeca Oy, Helsinki, Finland).
All collected data were initially analyzed descriptively. For inter- and intra-rater reliability, the Cohen’s kappa (κ) coefficient was calculated. The Chi-square test was used to detect associations between the presence of ethmoid sinus variations and different sides, ethmoid or maxillary sinus pathologies (at the sinus level), and age and sex (at the patient level). The Fisher exact test was used when more than 20% of cells had expected frequencies less than 5 or the subgroup sample size was small.
All statistical analyses were performed using SPSS version 26.0 (IBM Corp., Armonk, NY, USA) at a confidence level of 95%. A P value of <0.05 was considered to indicate statistical significance.
Results
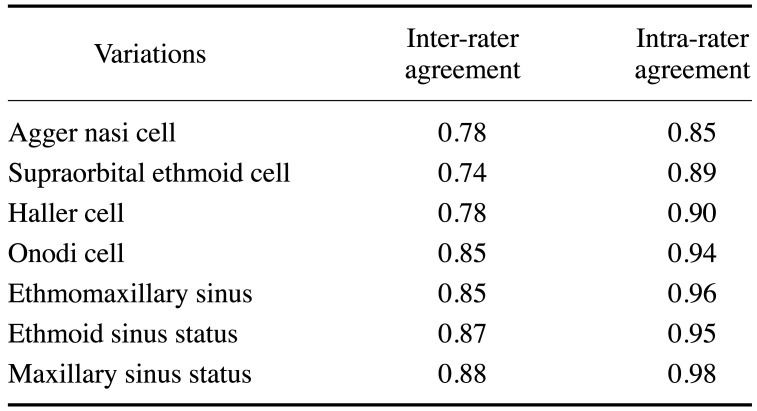
A total of 273 CBCT scans were selected for the final analysis exhibiting complete ethmoid and maxillary sinuses. Intra-rater agreement was excellent (κ values ranging from 0.85 to 0.98) for all anatomical variations and the status (health or pathology) of the ethmoid or maxillary sinus (Table 2). Inter-rater agreement for the detection of the anatomical variations of ANC, SOEC, and Haller cell was substantial (κ=0.78, κ=0.74, κ=0.78, respectively), while the agreement values for the remaining anatomical variations and ethmoid or maxillary sinus status were excellent.
Table 2. Inter- and intra-rater agreement assessed by the Cohen’s kappa coefficient for anatomical variations of the ethmoid sinuses and ethmoid or maxillary sinus status.
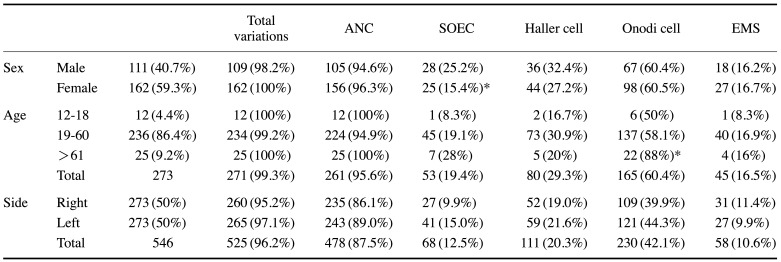
In the 273 CBCT scans (546 sides), the overall prevalence of ethmoid sinus anatomical variations was 99.3% at the patient level (271 out of 273 patients) and 96.2% at the side level (525 out of 546 sides; Table 3). The prevalence of ANC was found to be the highest (95.6%, n=261 patients; 87.5%, n=478 sides), followed by Onodi cell (60.4%, n=165 patients; 42.1%, n=230 sides), Haller cell (29.3%, n=80 patients; 20.3%, n=111 sides), and SOEC (19.4%, n=53 patient; 12.5%, n=68 sides), while EMS was seen with the lowest frequency (16.5%, n=45 patients; 10.6%, n=58 sides).
Table 3. Demographic and analytical data regarding anatomical variations of the ethmoid sinuses, and their association with sex, age, and different sides (number and percentage).
*: P<0.05
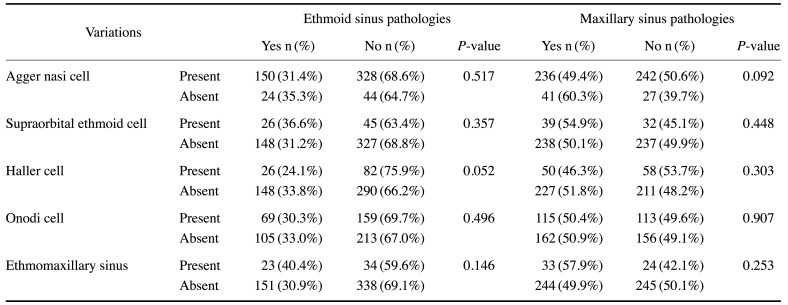
Of all 3 potential influencing factors that were assessed, sex exhibited a significant association with the presence of SOEC (P=0.044; Table 3), which was significantly more frequent in males. Likewise, patient age presented a significant association with the presence of Onodi cell (P=0.011), with the age group of over 61 years exhibiting the highest prevalence. No significant differences were shown for any of the anatomical variations according to different sides. There were also no statistically significant differences between the ethmoid sinus anatomical variations and ethmoid or maxillary sinus pathologies (all P>0.05; Table 4).
Table 4. The association between the anatomical variations of ethmoid sinuses and the ethmoid or maxillary sinus pathologies (Chi-square test).
Discussion
The nasoethmoidal region represents one of the most intricate anatomical areas in the head and neck. Identifying and characterizing anatomical variations in this region (especially for the paranasal sinuses) is imperative for making sound radiographic diagnoses, reducing the frequency of pathological misdiagnoses, and improving the success of surgical procedures performed by otorhinolaryngologists or oral and maxillofacial surgeons.1 Since CBCT is considered a precise imaging modality in the preoperative assessment of bony structures,8 this study examined the prevalence of clinically relevant ethmoid sinus variations, as well as their relationship with demographic characteristics, locations, and occurrence of ethmoid or maxillary sinus pathologies using this imaging modality.
This study of 273 CBCT scans found a high prevalence of ethmoid sinus variations at both the subject and location level (left versus right side). While variations such as ANC and Onodi cell occurred commonly, others including Haller cell, SOEC, and EMS had a subject-level prevalence of less than 30%. Generally, anatomical variations are usually classified as frequent (10-100%), infrequent (1-10%), rare (<1%), and sporadic (<100 reported cases) in nature.16 Based on the findings of this study, all ethmoid sinus anatomical variations may be considered as frequent findings among the Hong Kong or Southern Chinese population, with ANC being extremely frequent. This finding is clinically relevant in this population, especially for surgical procedures such as FESS, as inadequate removal of an ethmoid sinus variation such as ANC may result in iatrogenic chronic frontal sinusitis.17
Comparing the prevalence of anatomical variations of the ethmoid sinuses with previous CT or CBCT analyses, the present study displayed marked differences in comparison to other populations.9,10,18,19 Nonetheless, the present study corroborates the high prevalence of ANC when compared to other anatomical variations of the ethmoid sinuses detected in Australian, Turkish, and Iranian populations utilizing similar definition criteria.9,18,19 Previous studies have reported the prevalence of ANC (6.4-98.5%), SOEC (2.6-64.6%), Haller cell (4.6-60.0%), Onodi cell (8.0-65.3%), and EMS (0.7-8.2%), with substantial variation in different populations.18,19,20,21,22,23,24,25,26,27 A comparison of the prevalence of variations in the present cohort showed that the prevalence of ANS, SOEC, Haller cell, and Onodi cell was well within the reported limits of occurrence. Additionally, the prevalence of SOEC (19.4%) corroborates previous findings that SOEC is less frequently detected in East Asians than in Caucasians.27,28 However, this study identified a higher prevalence of EMS (16.5%) than has been previously reported.22 This finding may be due to population differences among studies. Thus, future studies in similar Southern Chinese cohorts are now needed to confirm this observation.
An analysis of the associations between the frequency of ethmoid sinus variations and demographic characteristics yielded significant findings, with a higher prevalence of SOEC among males and a higher prevalence of Onodi cell among elderly patients. Based on these findings, it can be hypothesized that the higher prevalence of Onodi cell in the elderly may represent an age-related variation. However, this issue remains to be evaluated further in future reports. With regard to these findings, this study did not corroborate the findings of Shokri and colleagues19 from Iran, who found no difference in the prevalence of SOEC or Onodi cell when stratified by sex and age, respectively. However, differences in the statistical methods employed in the 2 studies may account for this disparity. Moreover, elderly patients were not included in the previous study. Other studies also found no association between demographic characteristics and the prevalence of ANC or Haller cell.21 Although some anatomical variations may be considered as predisposing factors of sinusitis, this possibility remains a controversial and disputed point.5,25 The present study found no significant association between the presence of an ethmoid sinus variation and ethmoid or maxillary sinus pathologies.
While this study is unique in its objectives and main findings, it is not without limitations. The retrospective nature of the study, and a lack of assessment of the patients’ clinical history may lead to an overestimation or underestimation of the associations between anatomical variations and associated pathologies. Thus, the findings of this study should be interpreted with caution and need to be validated in future prospective studies.
Based on the findings of the present study, there is a high prevalence of ethmoid sinus variations in a Southern Chinese population. The prevalence of ANC and Onodi cell was higher than that of other anatomical variations of the ethmoid sinuses. SOEC and Onodi cells were more common among males and elderly persons, respectively. Anatomical variations of the ethmoid sinuses were not associated with ethmoid or maxillary sinus pathologies in this patient cohort.
Acknowledgments
The authors wish to thank Dr. Tanaka Ray, Applied Oral Sciences & Community Dental Care, Faculty of Dentistry, The University of Hong Kong, for the assistance regarding the relevant radiographic anatomy in this study. The authors also express their gratitude towards Ms. Kar Yan Li, Centralized Research Lab, The University of Hong Kong, for her support of the statistical analysis.
Footnotes
This study was supported by departmental funds only.
Conflicts of Interest: None
References
- 1.von Arx T, Lozanoff S, Bornstein MM. Extraoral anatomy in CBCT - a literature review. Part 1: nasoethmoidal region. Swiss Dent J. 2019;129:804–815. doi: 10.61872/sdj-2019-10-01. [DOI] [PubMed] [Google Scholar]
- 2.Stammberger HR, Kennedy DW Anatomic Terminology Group. Paranasal sinuses: anatomic terminology and nomenclature. Ann Otol Rhinol Laryngol Suppl. 1995;167:7–16. [PubMed] [Google Scholar]
- 3.Vaid S, Vaid N. Normal anatomy and anatomic variants of the paranasal sinuses on computed tomography. Neuroimaging Clin N Am. 2015;25:527–548. doi: 10.1016/j.nic.2015.07.002. [DOI] [PubMed] [Google Scholar]
- 4.Van Alyea OE. Ethmoid labyrinth: anatomic study, with consideration of the clinical significance of its structural characteristics. Arch Otolaryngol. 1939;29:881–902. [Google Scholar]
- 5.Ali IK, Sansare K, Karjodkar FR, Vanga K, Salve P, Pawar AM. Cone-beam computed tomography analysis of accessory maxillary ostium and Haller cells: prevalence and clinical significance. Imaging Sci Dent. 2017;47:33–37. doi: 10.5624/isd.2017.47.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bornstein MM, Chappuis V, von Arx T, Buser D. Performance of dental implants after staged sinus floor elevation procedures: 5-year results of a prospective study in partially edentulous patients. Clin Oral Implants Res. 2008;19:1034–1043. doi: 10.1111/j.1600-0501.2008.01573.x. [DOI] [PubMed] [Google Scholar]
- 7.Mafee MF, Chow JM, Meyers R. Functional endoscopic sinus surgery: anatomy, CT screening, indications, and complications. AJR Am J Roentgenol. 1993;160:735–744. doi: 10.2214/ajr.160.4.8456654. [DOI] [PubMed] [Google Scholar]
- 8.Hayashi T, Arai Y, Chikui T, Hayashi-Sakai S, Honda K, Indo H, et al. Clinical guidelines for dental cone-beam computed tomography. Oral Radiol. 2018;34:89–104. doi: 10.1007/s11282-018-0314-3. [DOI] [PubMed] [Google Scholar]
- 9.Earwaker J. Anatomic variants in sinonasal CT. Radiographics. 1993;13:381–415. doi: 10.1148/radiographics.13.2.8460226. [DOI] [PubMed] [Google Scholar]
- 10.Gibelli D, Cellina M, Gibelli S, Cappella A, Oliva AG, Termine G, et al. Anatomical variants of ethmoid bone on multidetector CT. Surg Radiol Anat. 2018;40:1301–1311. doi: 10.1007/s00276-018-2057-6. [DOI] [PubMed] [Google Scholar]
- 11.Kaya M, Çankal F, Gumusok M, Apaydin N, Tekdemir I. Role of anatomic variations of paranasal sinuses on the prevalence of sinusitis: computed tomography findings of 350 patients. Niger J Clin Pract. 2017;20:1481–1488. doi: 10.4103/njcp.njcp_199_16. [DOI] [PubMed] [Google Scholar]
- 12.Rak KM, Newell JD, 2nd, Yakes WF, Damiano MA, Luethke JM. Paranasal sinuses on MR images of the brain: significance of mucosal thickening. AJR Am J Roentgenol. 1991;156:381–384. doi: 10.2214/ajr.156.2.1898819. [DOI] [PubMed] [Google Scholar]
- 13.Soikkonen K, Ainamo A. Radiographic maxillary sinus findings in the elderly. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:487–491. doi: 10.1016/s1079-2104(05)80375-0. [DOI] [PubMed] [Google Scholar]
- 14.Yeung AW, Colsoul N, Montalvao C, Hung K, Jacobs R, Bornstein MM. Visibility, location, and morphology of the primary maxillary sinus ostium and presence of accessory ostia: a retrospective analysis using cone beam computed tomography (CBCT) Clin Oral Investig. 2019;23:3977–3986. doi: 10.1007/s00784-019-02829-9. [DOI] [PubMed] [Google Scholar]
- 15.Whyte A, Boeddinghaus R. The maxillary sinus: physiology, development and imaging anatomy. Dentomaxillofac Radiol. 2019;48:20190205. doi: 10.1259/dmfr.20190205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kachlík D, Varga I, Báča V, Musil V. Variant anatomy and its terminology. Medicina (Kaunas) 2020;56:713. doi: 10.3390/medicina56120713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wormald PJ. The agger nasi cell: the key to understanding the anatomy of the frontal recess. Otolaryngol Head Neck Surg. 2003;129:497–507. doi: 10.1016/S0194-59980301581-X. [DOI] [PubMed] [Google Scholar]
- 18.Özdemir A, Arslan S. Incidence of agger nasi and frontal cells and their relation to frontal sinusitis in a Turkish population: a CT study. Anatomy. 2018;12:71–75. [Google Scholar]
- 19.Shokri A, Faradmal MJ, Hekmat B. Correlations between anatomical variations of the nasal cavity and ethmoidal sinuses on cone-beam computed tomography scans. Imaging Sci Dent. 2019;49:103–113. doi: 10.5624/isd.2019.49.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bolger WE, Butzin CA, Parsons DS. Paranasal sinus bony anatomic variations and mucosal abnormalities: CT analysis for endoscopic sinus surgery. Laryngoscope. 1991;101:56–64. doi: 10.1288/00005537-199101000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Kayalioglu G, Oyar O, Govsa F. Nasal cavity and paranasal sinus bony variations: a computed tomographic study. Rhinology. 2000;38:108–113. [PubMed] [Google Scholar]
- 22.Liu J, Dai J, Wen X, Wang Y, Zhang Y, Wang N. Imaging and anatomical features of ethmomaxillary sinus and its differentiation from surrounding air cells. Surg Radiol Anat. 2018;40:207–215. doi: 10.1007/s00276-018-1974-8. [DOI] [PubMed] [Google Scholar]
- 23.Tomovic S, Esmaeili A, Chan NJ, Choudhry OJ, Shukla PA, Liu JK, et al. High-resolution computed tomography analysis of the prevalence of Onodi cells. Laryngoscope. 2012;122:1470–1473. doi: 10.1002/lary.23346. [DOI] [PubMed] [Google Scholar]
- 24.Şirikçi A, Bayazıt YA, Bayram M, Kanlıkama M. Ethmomaxillary sinus: a particular anatomic variation of the paranasal sinuses. Eur Radiol. 2004;14:281–285. doi: 10.1007/s00330-003-1993-6. [DOI] [PubMed] [Google Scholar]
- 25.Mathew R, Omami G, Hand A, Fellows D, Lurie A. Cone beam CT analysis of Haller cells: prevalence and clinical significance. Dentomaxillofac Radiol. 2013;42:20130055. doi: 10.1259/dmfr.20130055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jones NS, Strobl A, Holland I. A study of the CT findings in 100 patients with rhinosinusitis and 100 controls. Clin Otolaryngol Allied Sci. 1997;22:47–51. doi: 10.1046/j.1365-2273.1997.00862.x. [DOI] [PubMed] [Google Scholar]
- 27.Cho JH, Citardi MJ, Lee WT, Sautter NB, Lee HM, Yoon JH, et al. Comparison of frontal pneumatization patterns between Koreans and Caucasians. Otolaryngol Head Neck Surg. 2006;135:780–786. doi: 10.1016/j.otohns.2006.05.750. [DOI] [PubMed] [Google Scholar]
- 28.Jang DW, Lachanas VA, White LC, Kountakis SE. Supraorbital ethmoid cell: a consistent landmark for endoscopic identification of the anterior ethmoidal artery. Otolaryngol Head Neck Surg. 2014;151:1073–1077. doi: 10.1177/0194599814551124. [DOI] [PubMed] [Google Scholar]