ABSTRACT
Background
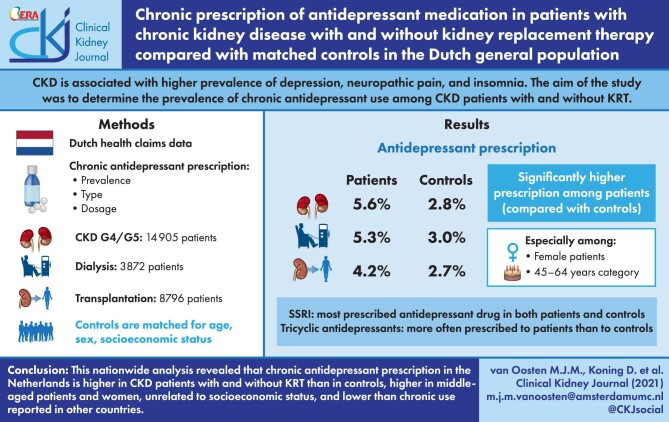
Chronic kidney disease (CKD) is associated with a higher prevalence of depression, neuropathic pain and insomnia. These conditions are often treated pharmaceutically. In this study we aimed to determine the prevalence of chronic antidepressant use among CKD patients with and without kidney replacement therapy (KRT).
Methods
By using the Dutch health claims database, we were able to determine the prevalence, type and dosage of chronic antidepressant prescriptions in patients with CKD Stage G4/G5 without KRT (n = 14 905), patients on dialysis (n = 3872) and patients living on a functioning graft (n = 8796) and compared these to age-, sex- and socio-economic status (SES)-matched controls from the general population.
Results
Our data show that the prevalence of chronic antidepressant prescription is 5.6%, 5.3% and 4.2% in CKD Stage G4/G5, dialysis and kidney transplant patients, respectively, which is significantly higher than in matched controls. Although our data revealed more prescriptions in female patients and in the age category 45–64 years, our data did not show any association between antidepressant prescriptions and SES. Selective serotonin reuptake inhibitors were the most prescribed drugs in all patient groups and controls. Tricyclic antidepressants were more often used in patients compared with controls.
Conclusion
This nationwide analysis revealed that chronic antidepressant prescription in the Netherlands is higher in CKD patients with and without KRT than in controls, higher in middle-aged patients and women, unrelated to socio-economic status and lower than chronic use reported in other countries.
Keywords: antidepressant medication, chronic kidney disease, depression, dialysis, kidney transplantation
Graphical Abstract
Graphical Abstract.
INTRODUCTION
Chronic kidney disease (CKD) is associated with substantial comorbidity. In addition to well-known cardiovascular pathology, CKD is associated with a number of neuropsychiatric conditions, including neuropathic pain, sleeping disorders, depressive mood disorder and anxiety [1–3]. Various non-pharmaceutical therapies are available for these conditions, such as lifestyle modification or cognitive behavioural therapy. If these prove ineffective or when disease burden is high, pharmaceutical intervention by prescribing antidepressant medication can be considered. The results of several studies suggest that in CKD, the use of antidepressants is associated with higher mortality [4, 5], although this is not consistently demonstrated [6].
Current literature suggests that antidepressant use in CKD with and without kidney replacement therapy (KRT) varies between 5.2% and 29.1% [4, 6–8]. In CKD patients without KRT, antidepressant use appears to be substantially higher than in age- and sex-matched controls without CKD [8]. However, in studies on antidepressant use in dialysis-dependent and kidney transplant patients, a control group has been lacking. Moreover, previous studies were restricted to samples and did not use comprehensive, nationwide data [9, 10]. Our study aims to examine chronic antidepressant use in patients with CKD stage G4/G5 without KRT, patients on dialysis treatment and patients with a functioning kidney transplant compared with matched controls from the general population. To this end we analysed data derived from a national health insurance database that covers the entire Dutch CKD population.
MATERIALS AND METHODS
Vektis database
For this study we used Dutch health claims data from the Vektis database. Since health insurance is mandatory in the Netherlands, ∼99% of Dutch residents are insured, of whom 99% are included in the database. This database contains all reimbursement data for healthcare products covered by the Dutch Health Insurance Act, as well as demographic data such as an individual's year of birth, sex, postal code, socio-economic status (SES) and date of death (if applicable) [11]. The SES of each individual is based on a person's postal code and is a reflection of the average income, education level and position in the labour market in that area of residence [12]. The mean SES score in the Netherlands has been set at 0 and ranges from −6.75 to +3.06, where a lower score indicates a lower SES and a higher score indicates a higher SES [12].
In the Netherlands, all hospital procedures are reimbursed via physician claims called Diagnosis Treatment Combinations (DBC) [13]. Every DBC corresponds to a given medical diagnosis in a given medical discipline. Furthermore, Vektis contains pharmacy dispensing data with information regarding the World Health Organization's (WHO's) Anatomical Therapeutic Chemical (ATC) classification system, the daily defined dose (DDD) and the annual quantity of a supplied medication [14]. The DDD reflects the assumed average maintenance dose per day for a medication used for its main indication. The annual quantity of a specific medication is a product of the DDD and the number of days a medication was dispensed. For example, an annual DDD of 180 may indicate the use of a medication in its routine dose during 180 days or half of the routine dose during 360 days. Vektis has no information on medication administered in intramural settings, such as during a hospital admission, a dialysis treatment or a nursing home stay. Furthermore, Vektis does not include data on over-the-counter drugs.
Since the Vektis database lacks detailed clinical information, we used proxies to assess the prevalence of chronic conditions in our study population. The variables diabetes mellitus, macrovascular disease [including coronary artery disease, peripheral artery disease and cerebrovascular accident (CVA)/transient ischemic attack (TIA)], and malignancies were based on combinations of DBC codes, primary care codes and medication use [15]. The variables chronic obstructive pulmonary disease (COPD) and Parkinson's were based on medication profiles, i.e. Pharmaceutical Cost Groups, which have been shown to provide reliable estimates of chronic disease burden [16–19]. The variables hospitalization and intensive care unit (ICU) admission were based on operational codes, an element of the DBC code. See Supplementary data, Section S1 for the variable definitions.
Study population
We identified adults (i.e. ≥20 years of age) with CKD Stage G4/G5 [estimated glomerular filtration rate (eGFR) <30 mL/min/1.73 m2] without KRT, patients on dialysis treatment (regardless of dialysis modality) and patients with a functioning kidney transplant. Patients were identified and allocated to the patient groups by a DBC for CKD Stage G4/G5, dialysis or kidney transplantation on 1 January 2017 [20]. Patients with CKD Stage G4/G5 without KRT who started KRT in 2017 and patients switching KRT modality in 2017 (from dialysis to kidney transplantation or vice versa) were excluded from the study (n = 7229). Furthermore, individuals were excluded in case of incomplete data, if they died during the study year or if we were unable to match them to controls.
A control group was created for each patient group separately by randomly selecting two controls per patient out of all individuals in the Vektis database provided that they had no CKD-related healthcare claim in 2017. Controls were matched for age, sex and SES score.
Antidepressant prescription
Antidepressant prescription was defined by drugs listed in the WHO's ATC classification system, code N06A Antidepressants (see Supplementary data, Section S2 for drugs listed to code N06A) [14]. We selected antidepressants with a cumulative annual DDD ≥180 to define chronic antidepressant use as our main outcome. In addition, total antidepressant prescription was defined as a DDD >0.
Statistical analyses
Baseline characteristics were described using medians and percentiles for continuous variables that were not normally distributed and frequency distributions with percentages for categorical variables. For the variable age, which was not normally distributed, we also presented the mean and standard deviation (SD). We calculated antidepressant prescription in all patient (sub)groups and controls and expressed it as a percentage. Baseline characteristics and antidepressant prescription in subgroups were compared using a Student's t-test for normally distributed continuous variables, Mann–Whitney U-test for not normally distributed continuous variables and chi-squared test for categorical variables. We considered P-values <0.05 as statistically significant. Analyses were performed in SAS, version 9.4 (SAS Institute, Cary, NC, USA).
RESULTS
Patient characteristics
In total, 14 905 CKD G4/G5, 3872 dialysis and 8796 transplant patients were included. Baseline characteristics are shown in Table 1. The mean age ranged from 56.5 years in transplant patients to 75.6 years in CKD G4/G5 patients, whereas the percentage of males ranged from 52.8% in the CKD G4/G5 patients to 59.8% in transplant patients. The median SES ranged from −0.1 (kidney transplantation) to −0.4 (dialysis). The percentage of patients suffering from diabetes mellitus, macrovascular disease and COPD was significantly higher in patients compared with controls (P < 0.001). Furthermore, the percentage of patients with malignancy, hospitalization or ICU admission was higher in all patients compared with controls (P < 0.001).
Table 1.
Baseline characteristics of CKD Stage G4/G5 without KRT, dialysis and kidney transplant patients and matched controls
| CKD | Dialysis | Kidney transplantation | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristics | Patients (n = 14 905) | Matched controls (n = 29 810) | P-value | Patients (n = 3872) | Matched controls (n = 7744) | P-value | Patients (n = 8796) | Matched controls (n = 17 592) | P-value |
| Age (years), mean (SD) | 75.6 (11.2) | 75.6 (11.2) | 1.00 | 70.8 (13.2) | 70.8 (13.2) | 1.00 | 56.5 (13.6) | 56.5 (13.6) | 1.00 |
| Age (years), median (25th–75th percentile) | 78.0 (70.0–84.0) | 78.0 (70.0–84.0) | 1.00 | 74.0 (64.0–80.0) | 74.0 (64.0–80.0) | 1.00 | 58.0 (48.0–67.0) | 58.0 (48.0–67.0) | 1.00 |
| 20–44 (%) | 1.8 | 1.8 | 1.00 | 4.5 | 4.5 | 1.00 | 19.6 | 19.6 | 1.00 |
| 45–64 (%) | 12.2 | 12.2 | 22.5 | 22.5 | 48.4 | 48.4 | |||
| 65–74 (%) | 25.0 | 25.0 | 25.7 | 25.7 | 24.5 | 24.5 | |||
| ≥75 (%) | 61.0 | 61.0 | 47.3 | 47.3 | 7.5 | 7.5 | |||
| Sex (male), % | 52.8 | 52.8 | 1.00 | 58.8 | 58.8 | 1.00 | 59.8 | 59.8 | 1.00 |
| SES, Median (quartile 1–quartile 3) | −0.2 (−1.0–0.5) | −0.2 (−1.0–0.5) | 1.00 | −0.4 (−1.2–0.3) | −0.3 (−1.2–0.4) | 1.00 | −0.1 (−1.0–0.6) | −0.1 (−1.0–0.6) | 1.000 |
| Quartile 1 (%) | 28.1 | 28.1 | 1.00 | 33.6 | 33.6 | 1.00 | 27.6 | 27.6 | 1.00 |
| Quartile 2 (%) | 26.5 | 26.5 | 26.6 | 26.6 | 24.9 | 24.9 | |||
| Quartile 3 (%) | 25.2 | 25.2 | 22.4 | 22.4 | 23.7 | 23.7 | |||
| Quartile 4 (%) | 20.2 | 20.2 | 17.4 | 17.4 | 23.9 | 23.9 | |||
| Diabetes mellitus (%) | 32.3 | 8.9 | <0.001 | 29.6 | 8.8 | <0.001 | 27.8 | 4.4 | <0.001 |
| Macrovascular disease (%) | 17.7 | 5.4 | <0.001 | 29.2 | 4.8 | <0.001 | 11.3 | 2.4 | <0.001 |
| Coronary artery disease (%) | 8.7 | 4.6 | <0.001 | 13.2 | 4.5 | <0.001 | 5.9 | 2.3 | <0.001 |
| Peripheral artery disease (%) | 8.4 | 1.9 | <0.001 | 16.9 | 1.8 | <0.001 | 4.9 | 0.7 | <0.001 |
| CVA/TIA (%) | 2.5 | 1.7 | <0.001 | 3.6 | 1.4 | <0.001 | 1.6 | 0.8 | <0.001 |
| COPD (%) | 7.1 | 3.1 | <0.001 | 5.6 | 2.7 | <0.001 | 2.1 | 1.2 | <0.001 |
| Parkinson's (%) | 0.6 | 0.6 | 0.832 | 0.6 | 0.5 | 0.789 | 0.4 | 0.2 | 0.001 |
| Malignancies (%) | 13.7 | 7.5 | <0.001 | 16.4 | 7.9 | <0.001 | 19.2 | 3.6 | <0.001 |
| Hospitalization (%) | 28.7 | 8.7 | <0.001 | 52.3 | 7.6 | <0.001 | 28.8 | 4.3 | <0.001 |
| ICU admittance (%) | 2.6 | 0.7 | <0.001 | 8.4 | 0.5 | <0.001 | 2.5 | 0.4 | <0.001 |
Chronic antidepressant prescription
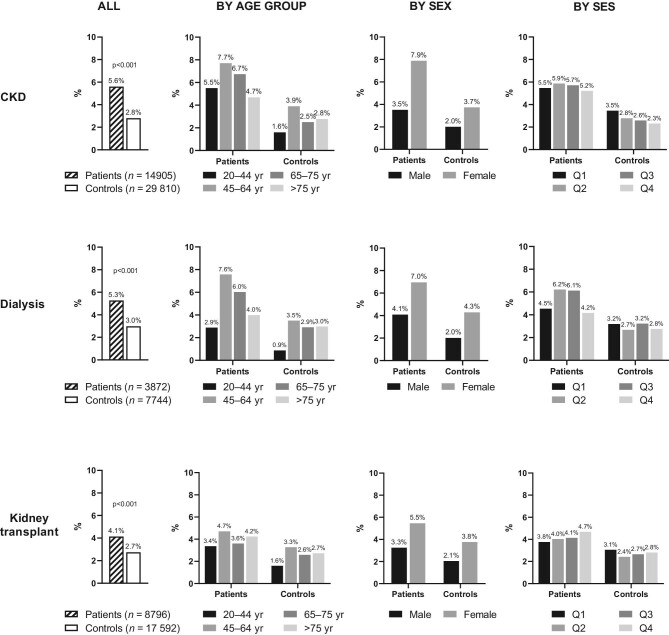
Figure 1 shows the percentage of chronic antidepressant prescription in patients and controls. Overall, antidepressant prescription was higher in patients than in controls; i.e. CKD G4/G5 patients (5.6% versus 2.8%; P < 0.001), dialysis patients (5.3% versus 3.0%; P < 0.001) and transplant patients (4.1% versus 2.7%; P < 0.001). In both patients and controls, antidepressant prescription was highest between 45 and 64 years of age and lowest in patients and controls ages 20–44 years, with the exception of CKD G4/G5 patients, where prescription was lowest in patients ≥75 years of age. In both patients and controls, women were prescribed antidepressants more often than men (Figure 1). Frequencies ranged from 5.5% to 7.9% in female patients and from 3.3% to 4.1% in males, while in controls this was 3.7–4.3% in women and 2.0%–2.1% in men (Figure 1). Variation in prescriptions between the different SES groups was small.
FIGURE 1:
Percentage of chronic antidepressant prescription (DDD ≥180) in CKD stage G4/G5 without KRT, dialysis and kidney transplant patients versus matched controls and by age, sex and SES. yr: years; Q: quartile.
In Supplementary data, Figure S1 and Table S3, we present the percentage of total antidepressant prescriptions (DDD >0) in patients and controls. Similar patterns were observed as in chronic antidepressant prescription, albeit at higher prescription frequencies. Total antidepressant prescriptions were higher in patients than in controls [CKD G4/G5: 10.6% versus 5.6% (P < 0.001); dialysis: 12.1% versus 5.4% (P < 0.001); transplantation 7.8% versus 4.4% (P < 0.001)].
Type of antidepressants
Among patients who were prescribed antidepressant medication, selective serotonin reuptake inhibitors (SSRIs) were the most prevalent type of antidepressant medication, ranging from 55.1% in CKD G4/G5 to 65.1% in transplant patients (Table 2). SSRI prescription was consistently lower in patients compared with controls, although this difference was only statistically significant in the CKD group (55.1% versus 62.0%; P = 0.004). The frequency of tricyclic antidepressant (TCA) prescription was 23.4%, 23.0% and 18.7% in CKD G4/G5, dialysis and transplant patients, respectively, and was significantly higher in all patient groups compared with controls. Citalopram and paroxetine were the most often prescribed SSRIs (Table 2). Regarding TCAs, amitriptyline was significantly more often prescribed in all three patient groups compared with their control groups (P < 0.01). In transplant patients, nortriptyline was more often prescribed than in controls (P = 0.034). Mirtazapine (tetracyclic antidepressant) and venlafaxine (selective noradrenalin reuptake inhibitor) were the most commonly prescribed ‘other’ types of antidepressants.
Table 2.
Prescription rates of the different classes of antidepressants and individual antidepressants in CKD Stage G4/G5, dialysis and kidney transplantation patients and matched controls using antidepressants
| CKD | Dialysis | Kidney transplantation | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Antidepressants | Patients | Controls | P-value | Patients | Controls | P-value | Patients | Controls | P-value |
| SSRI (%) | 55.1 | 62.0 | 0.004 | 61.3 | 67.1 | 0.206 | 65.1 | 69.7 | 0.156 |
| Citalopram | 19.6 | 21.5 | 0.334 | 26.0 | 19.0 | 0.083 | 21.7 | 21.0 | 0.792 |
| Paroxetine | 19.0 | 22.8 | 0.056 | 20.6 | 28.1 | 0.068 | 20.6 | 25.1 | 0.125 |
| Sertraline | 6.5 | 5.9 | 0.640 | 4.4 | 8.7 | 0.076 | 10.7 | 8.9 | 0.383 |
| Escitalopram | 4.1 | 5.8 | 0.103 | 4.9 | 4.8 | 0.946 | 5.8 | 6.6 | 0.605 |
| Othera | 6.6 | 7.5 | n.d. | 5.9 | 7.4 | n.d. | 7.4 | 9.8 | n.d. |
| TCA (%) | 23.4 | 19.5 | 0.048 | 23.0 | 14.7 | 0.026 | 18.7 | 11.0 | 0.002 |
| Amitriptyline | 13.1 | 8.3 | 0.002 | 17.7 | 7.8 | 0.002 | 11.3 | 4.8 | <0.001 |
| Nortriptyline | 7.3 | 7.4 | 0.980 | 4.9 | 4.3 | 0.776 | 4.7 | 2.1 | 0.034 |
| Otherb | 3.5 | 3.9 | n.d. | 2.0 | 3.0 | n.d. | 3.3 | 4.2 | n.d. |
| Other (%) | 30.4 | 28.9 | 0.489 | 27.9 | 26.4 | 0.720 | 26.4 | 28.4 | 0.509 |
| Mirtazapine | 16.8 | 15.8 | 0.568 | 20.6 | 14.3 | 0.083 | 12.6 | 10.8 | 0.405 |
| Venlafaxine | 8.8 | 10.0 | 0.399 | 7.8 | 8.7 | 0.758 | 8.2 | 13.1 | 0.026 |
| Otherc | 6.1 | 5.3 | n.d. | 3.9 | 5.6 | n.d. | 5.6 | 6.4 | n.d. |
n.d.: not determined.
The table shows the percentages of (type of) antidepressant prescribed in individuals with an antidepressant prescription. The prescription rates of SSRIs, TCAs and other add up to >100%, which indicates that some individuals were prescribed more than one antidepressant from different classes.
Fluvoxamine and fluoxetine.
Clomipramine, imipramime, doxepine, maprotiline and dosulepine.
Bupropion, duloxetine, trazodone, agomelatine, vortioxetine and mianserine.
DISCUSSION
We conducted the first nationwide study assessing chronic antidepressant prescription in patients with CKD Stage G4/G5 with and without KRT compared with age-, sex- and SES-matched controls. In this study, the percentage of prescribed antidepressants was higher in CKD patients than in the matched general population without CKD. Around 6% of CKD Stage G4/G5 patients, 5% of dialysis patients and 4% of transplant patients were chronically prescribed antidepressants compared with ∼3% in the control groups. Antidepressant prescription was highest in patients ages 45–64 years. In both patients and controls, women were more likely to be prescribed antidepressant medication. Furthermore, antidepressant prescribing in CKD patients was comparable across SES categories, which suggests that there is no association between education level and chronic antidepressant prescribing. SSRIs were the antidepressant of choice in patients being prescribed antidepressants; with 55% of CKD, 61% of dialysis and 65% of kidney transplant patients using a drug from this class of antidepressants. Interestingly, TCAs were prescribed significantly more often in patients compared with controls.
Strengths and limitations
In this study we used a comprehensive data source of routinely collected health claims data comprising ∼98% of all Dutch inhabitants. This enabled us to study CKD Stage G4/G5 patients with and without KRT in the same study cohort and to select a matched control group from the general population. Pharmacy dispensing data, which was used to determine antidepressant prescription in this study, is generally considered the most accurate way to determine medication use in large populations as opposed to medication reviews from patient interviews or medical charts that are vulnerable to recall bias or incomplete registration [21]. Furthermore, our data allowed for the selection of chronically prescribed antidepressant medication representing a group of patients with clinically significant depressive symptoms present for a prolonged period of time. An additional advantage of pharmacy dispensing data is that they only represent prescribed medication that is truly dispensed by the pharmacy and accordingly collected by the patient. Although medication adherence remains difficult to quantify, regular medication dispensing by a pharmacy is a strong indicator that this medication was routinely used by the patient.
Several limitations of this study must also be acknowledged. First, the validity of study results must be discussed when health claims codes are being used to identify a study population. Previously we showed that Dutch health claims data from the Vektis database provide reliable estimates of the Dutch dialysis and kidney transplantation population since the correspondence between the Dutch renal registry data and the Vektis data was very high (99%) [20]. The overall sensitivity to identify patients with CKD Stage G4/G5 (eGFR <30 mL/min/1.73 m2) using Dutch health claims data was low (51%), although sensitivity was higher in younger patients. The relatively low validity can be explained by the fact that patients solely treated in primary care cannot be identified using hospital claims data. As a result, especially elderly patients and patients with limited comorbidities are underrepresented in the CKD Stage G4/G5 group [22]. Consequently there is a chance that unidentified CKD patients in our study were selected as controls.
Second, we were unable to determine the indication for the prescription of antidepressants. Besides the treatment of depressive symptoms, antidepressants can be prescribed for other diagnoses such as neuropathic pain or anxiety, which are both more common among CKD patients than in the general population [1–3].
Antidepressant use
CKD Stage G4/G5 without KRT
Antidepressant use in CKD patients without KRT has been described in previous studies originating from the USA and UK [4, 7, 8, 23, 24]. The 2020 United States Renal Data System (USRDS) report describes SSRI prescription drug coverage, based on 6-month prescriptions, in CKD Stage 4 and 5 patients being 22.4% and 21.8%, respectively (of note: this USRDS report only described patients >65 years of age and coverage of other antidepressants is not reported) [23]. Two studies by Fischer et al. [7, 24] report antidepressant use, derived from patient interviews, in CKD patients (eGFR <60 mL/min/1.73 m2) using data from two different US cohorts among patients with a mean age of ∼60 years. Antidepressant use of 18.2% was reported in the Chronic Renal Insufficiency Cohort and 5.4% in the African American Study of Kidney Disease and Hypertension Cohort [7, 24]. Finally, Balogun et al. [4] reported antidepressant use of 29.1% using Medicare pharmacy dispensation data from the national Veterans Affairs Health System database, a cohort of elderly (mean age 74 years) CKD patients (eGFR <60 mL/min/1.73 m2) [4]. The study by Iwagami et al. [8] is the only one comparing antidepressant use in CKD patients (eGFR <60 mL/min/1.73 m2) with matched controls from the general population. This UK study reported that 16.3% of CKD patients with a mean age of 76 years were taking antidepressants, defined as a prescription for a period of at least 6 months, compared with 11.9% in the controls.
The chronic antidepressant prescription in CKD Stage G4/G5 patients in the Netherlands, being 5.6% as reported in this study, is considerably lower than that described in literature with the exception of the African American Study of Kidney Disease and Hypertension cohort. It is unknown why this African American cohort reported such low rates of antidepressant use, although it has been suggested that depression is undertreated in African American populations. The low antidepressant prescription rates in our study cannot likely be explained by the age of the included participants, as these were comparable across the different studies. Furthermore, the fact that we only included patients with an eGFR <30 mL/min/1.73 m2 is unlikely to be related to the observed differences in antidepressant prescription, since other studies describe no clear relationship between the level of eGFR and antidepressant use [7, 8, 24]. Indeed, the percentage of prescribed antidepressants in our study might be lower due to the selection of chronic prescriptions. Nevertheless, antidepressant prescription in the Netherlands seems to be remarkably lower than reported by the USRDS (although only reporting SSRI prescriptions) and the UK study, both based on 6-month prescriptions [8, 23]. Furthermore, we report a 10.6% prevalence of total antidepressant prescription that is still remarkably lower than previously reported.
Dialysis
The 2020 USRDS report describes the percentage of patients undergoing haemodialysis and peritoneal dialysis using SSRIs in the USA, which is 21.5% and 19.3%, respectively [23]. Guirguis et al. [25] report that 11% of haemodialysis patients use antidepressants, based on a small set of UK patients who were interviewed. Finally, Lopes et al. [26] report antidepressant use, derived from medical charts, of ∼13% in a cross-sectional analysis of the Dialysis Outcomes and Practice Patterns Study II cohort including haemodialysis patients from 12 different countries [26]. Again we find a lower prevalence of chronic antidepressant prescriptions in dialysis patients compared with other studies. Where the USRDS reports chronically prescribed medication, the duration of prescriptions is not known for the other two studies where antidepressant use was based on patient interview and chart review [23, 25, 26]. The results of these latter studies are in concordance with our reported total antidepressant prescription rate of 12.1% in dialysis patients [25, 26].
Kidney transplantation
Information on antidepressant use in kidney transplant patients is scarce. The 2020 USRDS report described SSRI use of 19.6% in transplant patients [23]. Lentine et al. [5] studied antidepressant prescriptions in the year before and after transplantation using US pharmacy claims data. Antidepressant prescriptions were 12.8% in the year before transplantation, of which 51.8% of the patients continued use after transplantation and 13.2% started use after transplantation. Among transplant patients, we found a lower prevalence of both chronic (4.1%) and total (7.8%) prescriptions of antidepressants in comparison with other studies.
Prescribing patterns
The Dutch clinical practice guideline advises SSRIs for treatment of patients with depressive disorders, because of their lower risk of side effects compared with TCAs, and prefers the prescription of SSRIs citalopram and sertraline and the TCA nortriptyline in older individuals [27]. In line with this guideline, the results of our study show that most older patients were prescribed citalopram. However, the results of our study do not show a preference for nortriptyline over amitriptyline in older individuals. This may change in the coming years as prescribers may gradually become aware of the beneficial effects of nortriptyline [28]. Our data are broadly consistent with previously conducted studies in CKD patients describing the preference of SSRIs over TCAs [5, 7, 8, 25]. Data on the specific type of antidepressant are scarce, but two studies by Iwagami et al. [8] and Guirguis et al. [25] report that citalopram is the most commonly prescribed antidepressant in CKD and dialysis patients.
Prescription of antidepressants in the general population
The antidepressant prescription of ∼3% in our matched control groups is lower compared with data from the general population in the Netherlands showing that ∼6% of all Dutch inhabitants were prescribed antidepressants in 2019 [29]. This difference might be explained by the older age of the matched control groups, as our results suggest that antidepressant use decreases with age. Antidepressant use in adults seems to be higher in the USA (13.2%) compared with Europe (7.2%) [9]. Of note, the percentage of antidepressant use in Europe varies widely per country, from 15.7% in Portugal to 2.7% in Greece [9].
Factors related to antidepressant prescription
Variations in antidepressant prescription between countries are the result of a complex interplay of factors such as the prevalence of depression, certain stigmata about depression, a country's healthcare spending and coverage and the availability of other treatment options for depression [9, 10]. The high percentage of antidepressant prescriptions in CKD patients in the USA is in line with the known high antidepressant rates in the US population, which is among the highest in the world [10]. On the other hand, a recent study by Hayward et al. [30] demonstrated that the chance of hyperpolypharmacy in older patients with advanced CKD was twice as high in the Netherlands as in the UK. In light of this study, it is perhaps remarkable that this does not hold true for antidepressants—the prescription of antidepressants in CKD patients with and without KRT seems to be lower in the Netherlands than in the UK. The results of the study by Hayward et al. [30] imply a generally reserved prescribing approach of UK physicians towards patients with CKD, whereas the results of our study suggest a restrictive prescribing approach, particularly antidepressants, in the Netherlands.
CONCLUSION
This nationwide analysis of Dutch pharmacy dispensing data shows that chronic antidepressant prescription was significantly higher in CKD patients with and without KRT compared with their matched controls from the general population. Prescription was lower in elderly patients and in men, yet unrelated to SES. This study reveals an importantly lower prescription rate of antidepressants in Dutch CKD patients than that reported in CKD patient populations elsewhere. It is difficult to assess to what extent the intercountry variation is a result of under- or overprescription.
Supplementary Material
Contributor Information
Manon J M van Oosten, Department of Medical Informatics, Amsterdam UMC, University of Amsterdam, Amsterdam Public Health Research Institute, Amsterdam, The Netherlands.
Dan Koning, Department of Internal Medicine, Diakonessenhuis, Utrecht, The Netherlands.
Susan J J Logtenberg, Department of Internal Medicine, Diakonessenhuis, Utrecht, The Netherlands.
Martijn J H Leegte, Dutch Renal Registry, Nefrovisie Foundation, Utrecht, The Netherlands.
Henk J G Bilo, Department of Internal Medicine, University Medical Center, Groningen, and Faculty of Medicine, Groningen University, Groningen, The Netherlands; Diabetes Research Center and Department of Epidemiology and Statistics, Isala Hospital, Zwolle, The Netherlands.
Marc H Hemmelder, Department of Internal Medicine, Division of Nephrology, Maastricht Universal Medical Center and Cardiovascular Research Institute University Maastricht, Maastricht, The Netherlands.
Kitty J Jager, Department of Medical Informatics, Amsterdam UMC, University of Amsterdam, Amsterdam Public Health Research Institute, Amsterdam, The Netherlands.
Vianda S Stel, Department of Medical Informatics, Amsterdam UMC, University of Amsterdam, Amsterdam Public Health Research Institute, Amsterdam, The Netherlands.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Cukor D, Coplan J, Brown C et al. Depression and anxiety in urban hemodialysis patients. Clin J Am Soc Nephrol 2007; 2: 484–890 [DOI] [PubMed] [Google Scholar]
- 2. Shirazian S, Grant CD, Aina O et al. Depression in chronic kidney disease and end-stage renal disease: similarities and differences in diagnosis, epidemiology, and management. Kidney Int Rep 2017; 2: 94–107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kumar P, Clark M. Kidney and urinary tract diseases. In: Feather A, Randall D, Waterhouse M (eds.). Clinical Medicine. Amsterdam: Elsevier, 2012: 618–621 [Google Scholar]
- 4. Balogun RA, Abdel-Rahman EM, Balogun SA et al. Association of depression and antidepressant use with mortality in a large cohort of patients with nondialysis-dependent CKD. Clin J Am Soc Nephrol 2012; 7: 1793–1800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lentine KL, Naik AS, Ouseph R et al. Antidepressant medication use before and after kidney transplant: implications for outcomes—a retrospective study. Transpl Int 2018; 31: 20–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tuot DS, Lin F, Norris K et al. Depressive symptoms associate with race and all-cause mortality in patients with CKD. Kidney Int Rep 2019; 4: 222–230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fischer MJ, Xie D, Jordan N et al. Factors associated with depressive symptoms and use of antidepressant medications among participants in the Chronic Renal Insufficiency Cohort (CRIC) and Hispanic-CRIC studies. Am J Kidney Dis 2012; 60: 27–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Iwagami M, Tomlinson LA, Mansfield KE et al. Prevalence, incidence, indication, and choice of antidepressants in patients with and without chronic kidney disease: a matched cohort study in UK clinical practice research datalink. Pharmacoepidemiol Drug Saf 2017; 26: 792–801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lewer D, O'Reilly C, Mojtabai R et al. Antidepressant use in 27 European countries: associations with sociodemographic, cultural and economic factors. Br J Psychiatry 2015; 207: 221–226 [DOI] [PubMed] [Google Scholar]
- 10. Brody DJ, Gu Q. Antidepressant use among adults: United States, 2015–2018. NCHS Data Brief 2020; 377: 1–8 [PubMed] [Google Scholar]
- 11. de Boo A. Vektis: information centre for healthcare. Tijdschr Gezondheidswetenschappen 2011; 89: 358–359 [Google Scholar]
- 12. Knol F. Statusontwikkeling van wijken in Nederland 1998–2010. Den Haag: Sociaal en Cultureel Planbureau, 2012 [Google Scholar]
- 13. Westerdijk M, Zuurbier J, Ludwig M et al. Defining care products to finance health care in the Netherlands. Eur J Health Econ 2012; 13: 203–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. WHO Collaborating Centre for Drug Statistics Methodology . Guidelines for ATC Classification and DDD Assignment 2020. 23rd ed. Oslo: 2019. http://www.whocc.no/filearchive/publications/2020_guidelines_web.pdf (August 2021, date last accessed) [Google Scholar]
- 15. van Oosten MJM, Logtenberg SJJ, Hemmelder MH et al. Polypharmacy and medication use in patients with chronic kidney disease with and without kidney replacement therapy compared to matched controls. Clin Kidney J. 2021; 14: 2497–2523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chini F, Pezzotti P, Orzella L et al. Can we use the pharmacy data to estimate the prevalence of chronic conditions? A comparison of multiple data sources. BMC Public Health 2011; 11: 688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lamers LM. Pharmacy costs groups: a risk-adjuster for capitation payments based on the use of prescribed drugs. Med Care 1999; 37: 824–830 [DOI] [PubMed] [Google Scholar]
- 18. Slobbe LCJ, Füssenich K, Wong A et al. Estimating disease prevalence from drug utilization data using the Random Forest algorithm. Eur J Public Health 2019; 29: 615–621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tamblyn R, Lavoie G, Petrella L et al. The use of prescription claims databases in pharmacoepidemiological research: the accuracy and comprehensiveness of the prescription claims database in québec. J Clin Epidemiol 1995; 48: 999–1009 [DOI] [PubMed] [Google Scholar]
- 20. Mohnen SM, van Oosten MJM, Los J et al. Healthcare costs of patients on different renal replacement modalities—analysis of Dutch health insurance claims data. PLoS One 2019; 14: e0220800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Schneeweiss S, Avorn J. A review of uses of health care utilization databases for epidemiologic research on therapeutics. J Clin Epidemiol 2005; 58: P323–337 [DOI] [PubMed] [Google Scholar]
- 22. van Oosten MJM, Logtenberg SJJ, Leegte MJH et al. Age-related difference in health care use and costs of patients with chronic kidney disease and matched controls: analysis of Dutch health care claims data. Nephrol Dial Transplant 2020; 35: 2138–2146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. United States Renal Data System . 2020 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2020 [Google Scholar]
- 24. Fischer MJ, Kimmel PL, Greene T et al. Sociodemographic factors contribute to the depressive affect among African Americans with chronic kidney disease. Kidney Int 2010; 77: 1010–1019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Guirguis A, Chilcot J, Almond M et al. Antidepressant usage in haemodialysis patients: evidence of sub-optimal practice patterns. J Renal Care 2020; 46: 124–132 [DOI] [PubMed] [Google Scholar]
- 26. Lopes AA, Albert JM, Young EW et al. Screening for depression in hemodialysis patients: associations with diagnosis, treatment, and outcomes in the DOPPS. Kidney Int 2004; 66: 2047–2453 [DOI] [PubMed] [Google Scholar]
- 27. Nederlands Huisartsen Genootschap . NHG Richtlijn Depressie. 2019. https://richtlijnen.nhg.org/standaarden/depressie (31 December 2021, date last accessed)
- 28. Stichting Farmaceutische Kengetallen . Apotheken scoren beter op nortriptyline-indicator. https://www.sfk.nl/publicaties/PW/2019/apotheken-scoren-beter-op-nortriptyline-indicator (31 December 2021, date last accessed) [Google Scholar]
- 29. Central Bureau of Statistics . Persons with dispensed medicines. 2019. http://opendata.cbs.nl/#/CBS/en/ (August 2021, date last accessed) [Google Scholar]
- 30. Hayward S, Hole B, Denholm R et al. International prescribing patterns and polypharmacy in older people with advanced chronic kidney disease: results from the European quality study. Nephrol Dial Transplant 2021; 36: 503–511 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.